Abstract
Rationale:
There has been a resurgence of progressive massive fibrosis (PMF) in the United States, particularly among central Appalachian miners.
Objectives:
We characterized the proportion of PMF among former U.S. coal miners applying for Federal Black Lung Program benefits, 1970–2016.
Methods:
Data from the U.S. Department of Labor were used to characterize trends in proportion of PMF cases, defined as an approved black lung claim with a determination of PMF, among all miners who filed for federal benefits between January 1, 1970, and December 31, 2016. Joinpoint, logistic, and linear regression models were used to identify changes in the proportion of claimants with PMF over time.
Results:
There were 4,679 unique PMF cases among claimants for federal black lung benefits between 1970 and 2016, with 2,474 miners determined to have PMF since 1996. The number of PMF cases among Federal Black Lung Program claimants fell from 404 (0.5% of claimants) in 1978 to a low of 18 cases (0.6%) in 1988, and then increased to 353 cases (8.3%) in 2014. The proportion of federal black lung benefits claimants with PMF has been increasing since 1978 (0.06% annual percent change [APC]; 95% confidence interval [CI], 0.05–0.07%; P < 0.0001), and began increasing at a significantly increased rate after 1996 (0.26% APC; 95% CI, 0.25–0.28%; P < 0.0001). Most miners with PMF (84%) last mined in West Virginia, Kentucky, Pennsylvania, or Virginia. Since 1970, the proportion of claimants with PMF has increased significantly among miners who last worked in Kentucky (16.6% APC; 95% CI, 16.5–16.7%), Pennsylvania (4.7% APC; 95% CI, 4.6–4.8%), Tennessee (16.1% APC; 95% CI, 15.7–16.4%), West Virginia (16.8% APC; 95% CI, 16.6–16.9%), and most sharply among miners last working in Virginia (31.5% APC; 95% CI, 31.2–31.7%), where in 2009, more than 17% of claimants received a PMF determination. The proportion of PMF determinations for the rest of the United States has not exceeded 4%.
Conclusions:
There has been a resurgence of PMF, particularly in central Appalachian miners. The resurgence of this preventable disease points to the need for improved primary and secondary prevention of dust-related lung disease in U.S. coal miners.
Keywords: black lung benefits, coal mine dust, coal workers’ pneumoconiosis, progressive massive fibrosis
The United States is experiencing an unprecedented increase in the prevalence of coal workers’ pneumoconiosis, and its most severe form, progressive massive fibrosis (PMF); a debilitating disease responsible for substantial morbidity (1) and mortality among U.S. coal miners (2, 3). Rising prevalence rates of PMF have been observed in national surveillance data of coal miners from the National Institute for Occupational Safety and Health (NIOSH) Coal Workers’ Health Surveillance Program (CWHSP), which primarily targets active coal mine workers (4–7). However, the reported surveillance data do not capture all cases of PMF among U.S. coal miners given that only 25–40% of active miners participate in this voluntary program annually, relatively few former miners are included, and this is a disease of long latency that may not develop or worsen until after the miner has left work (8, 9). A NIOSH survey of former miners between 2009 and 2013 demonstrated a significantly higher prevalence of PMF in former miners compared with active miners (10). In addition, a clinic-based investigation of PMF in Kentucky and Virginia showed a higher burden of PMF among former miners than was detected through the CWHSP (11, 12).
The U.S. Department of Labor, Division of Coal Mine Workers’ Compensation (DOL) operates the Federal Black Lung Program and administers claims filed under the Black Lung Benefits Act of 1969 (13). This Act describes a procedure for coal miners who may be totally disabled by pneumoconiosis due to their coal mine employment to apply for financial and medical coverage benefits. When filing a claim with the DOL, miners provide details of their coal mine employment and are offered a pulmonary evaluation by the DOL including a chest radiograph classified for pneumoconiosis according to the International Labor Office (ILO) system (14) by a NIOSH-certified B Reader, spirometry, and resting and exercise arterial blood gases from a DOL-approved provider (13). Based on these medical test results, the DOL provides an initial determination, indicating their intent to approve or deny the claim based on the presence or absence ofdisabling pulmonary impairment. By definition, PMF is considered totally disabling (15). Miners with other nonmalignant coal mine dust lung diseases, such as chronic obstructive pulmonary disease, silicosis, emphysema, chronic bronchitis, and simple coal workers’ pneumoconiosis, may be eligible for benefits if they have disabling pulmonary impairment due to their coal mine employment.
The aim of this study was to analyze the trends in the number and proportion of former U.S. coal miners with PMF, using data from the Federal Black Lung Program. These data represent an additional source of information, independent of national surveillance data, on the burden of PMF among former U.S. coal miners.
Methods
Data Sources
The DOL has maintained administrative data for all Federal Black Lung Program claimants since 1970, and clinical data associated with these claims since 2000. NIOSH received all DOL claims data for the period between January 1, 1970, and December 31, 2016.
Coal miners as well as their survivors may make a claim for federal benefits. For the DOL to approve a claim, medical evidence must establish the presence of a totally disabling pulmonary impairment to which occupational exposure to coal mine dust is a substantial contributor. Additional medical testing is often obtained leading to subsequent determinations that may or may not uphold the initial finding. These determinations can be disputed and sent for a hearing before an Administrative Law Judge, and further appealed to the DOL’s Benefits Review Board and federal courts. A claimant can receive a determination indicating PMF at any point in this legal process. In the event of an unsuccessful claim, miners may file a subsequent claim with the DOL, which recognizes the progressive nature of the disease and allows that new testing may show evidence of worsening disease.
The DOL administrative data associated with these claims include the claimant’s age at time of filing; state in which the claimant last worked as a coal miner; years of coal mine employment; filing date; and a record of each administrative decision in the claims process. The claims adjudication database included 922,562 records from 341,176 miners applying for federal benefits from 1970 to 2016. Each record contains an administrative step in a miner’s claim that is identified by a determination code.
PMF Case Selection
To identify PMF cases, we selected all records with a DOL determination code of PMF (n = 12,230), excluding those records with a missing determination code. We selected the first record associated with a claim receiving a PMF determination for analysis, excluding subsequent records for the same miner (n = 6,343). For cases with multiple claims, we selected the original living miner claim for analysis. Claims filed by survivors were selected only in cases where there was no living miner claim. A case of PMF was defined as an approved federal black lung claim filed between 1970 and 2016 with a determination of PMF in a miner with between 5 and 60 years of coal mine employment. The first claim associated with all miners applying for federal black lung benefits who did not meet the PMF case criteria were retained for comparison with PMF cases.
We examined ILO classifications (14) of chest radiographs submitted for claims between 2000 and 2016. Radiographic evidence of PMF was defined as a large opacity classification of A (one or more large opacities > 10 mm in diameter, with a combined dimension of ≤50 mm), B (one or more large opacities having the sum of longest dimension(s) exceeding 50 mm but not exceeding the equivalent area of the right upper lung zone), or C (one or more large opacities, that combined exceed the equivalent area of the right upper zone). We characterized the radiographic severity of disease, based on ILO small opacity profusion score (density of small opacities) and large opacity size, among those PMF cases for whom a chest radiograph classification was available.
Data Analysis
We examined miner’s age at time of filing a claim and years of coal mine employment among cases and noncases. We also examined the trends in the number of federal black lung claimants with PMF relative to the number of coal miners employed in the United States, using annual coal mine employment data from the Mine Safety and Health Administration (16). We calculated annual proportions of all federal claims within a year that had a determination of PMF, as well as proportions of miners with PMF by state. The annual proportion of PMF cases was calculated by dividing the number of PMF cases, as defined above, by the total number of miners filing claims within the same year.
We conducted a time-trend analysis of PMF cases from 1970 to 2016, using logistic regression models to test linear and quadratic trends in the odds of PMF over time while controlling for coal mine employment. Before modeling, we centered the year variable and a quadratic term was calculated on the basis of this centered value. We calculated the annual proportion and standard error of claimants with PMF for each year in the data and used the National Cancer Institute software Joinpoint (17, 18) to identify significant (P < 0.05) changes in trend. Linear regression analysis was used to test for trend over time in the proportion of claimants with PMF by state. We calculated the annual percent change (APC) in proportion of Federal Black Lung Program claimants with PMF, using Joinpoint and linear regression results.
All statistical analyses were performed in SAS version 9.4 (19) and Joinpoint version 4.5.0.1 (18). This study was approved by the institutional review boards of both NIOSH and the University of Illinois at Chicago.
Results
Claimant Population
There were 314,176 miners who applied for Federal Black Lung Program benefits from 1970 to 2016. We identified a total of 4,679 unique PMF cases during this time (see Table E1 and Figure E1 in the online supplement), nearly all (93%) from claims made by a living miner (Table 1). The mean age of miners with PMF at time of filing their claim was 61.6 years (median, 61; range, 27–93), which is slightly younger than the mean age of non-PMF claimants (mean, 62.3). The mean duration of coal mine employment of PMF cases (23.0 yr; range, 5–58) was significantly higher than for non-PMF claimants (18.9 yr).
Table 1.
Characteristics of miners applying for Federal Black Lung Program benefits, by PMF determination status, 1970–2016
| Claim Characteristic | PMF Claimants (N = 4,679) |
Non-PMF Claimants (N = 336,497) |
|---|---|---|
| Claim type, n (%) | ||
| Living miner | 4,350 (93.0) | 288,158 (85.6) |
| Living survivor | 329 (7.0) | 48,339 (14.4) |
| Age of miner,* mean (SD) | 61.6 (9.7) | 62.3 (10.3) |
| Coal mine employment,† mean (SD), yr | 23.0 (9.9) | 18.9 (10.3) |
| State/region,‡ n (%) | ||
| West Virginia | 1,327 (28.4) | 67,213 (20.0) |
| Kentucky | 945 (20.2) | 49,266 (14.6) |
| Pennsylvania | 935 (20.0) | 69,445 (20.6) |
| Virginia | 714 (15.3) | 22,791 (6.8) |
| Eastern | 306 (6.5) | 27,135 (8.1) |
| Interior | 109 (2.3) | 25,259 (7.5) |
| Western | 65 (1.4) | 8,387 (2.5) |
| Unknown | 278 (5.9) | 67,001 (19.9) |
Definition of abbreviations: PMF = progressive massive fibrosis; SD = standard deviation.
Age of miner at time of filing a claim for federal black lung benefits.
Coal mine employment, in years, verified by the U.S. Department of Labor.
State is determined by the last state in which the miner was employed as a coal miner. Eastern region includes the states of AL, CT, DC, DE, FL, GA, MA, MD, ME, NC, NH, NJ, NY, OH, TN, RI, SC, and VT. Interior region includes the states of AR, IA, IL, IN, KS, LA, MI, MN, MO, MS, ND, NE, OK, SD, TX, and WI. Western region includes the states of AK, AZ, CA, CO, HI, ID, MT, NM, NV, OR, UT, WA, and WY.
Trends in PMF Claims
The number of PMF cases among Federal Black Lung Program claimants fell from 404 (0.5% of claimants) in 1978 to a low of 18 cases (0.6%) in 1988, and then increased to 353 cases (8.3%) in 2014 (see Table E1). The total number of PMF cases since 1996 through 2016 (n = 2,474; annual average, 118) has surpassed the number of cases during 1970–1996 (n = 2,205; annual average, 85), while overall coal mine employment has declined steadily from 250,226 miners in 1979 to a total of 81,485 miners in 2016 (Figure 1). The number of coal miners filing claims for Federal Black Lung Program benefits peaked in 1978 at 83,252 likely as a result of the 1977 passage of Public Law 95–239, which amended the Federal Coal Mine Health and Safety Act to expand benefit eligibility criteria (20). Miners with previously denied claims were invited to apply again under the new amendment with new claim numbers. There have been 1,564–5,766 claims filed annually with the DOL since 1981.
Figure 1.
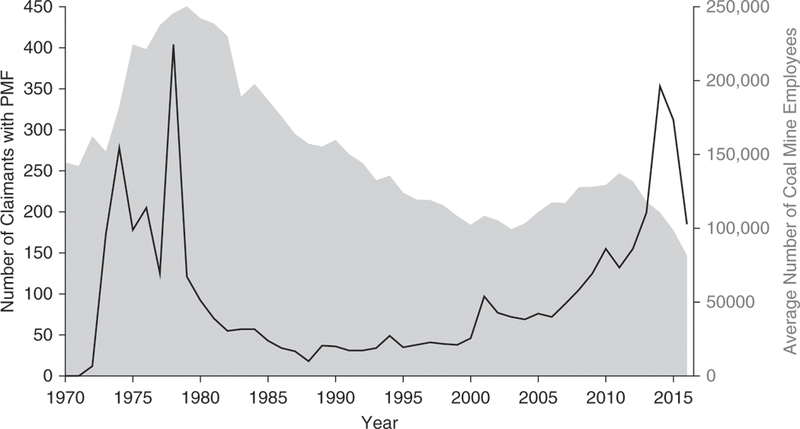
Number of miners filing for Federal Black Lung Program benefits and found to have a determination of progressive massive fibrosis (PMF) compared with average annual coal mine employment, 1970–2016. The number of claimants with PMF from 1970 to 1972 is combined because of small numbers. Office workers are included in employment totals from 1973 to 1977. Data sources: U.S. Department of Labor, Office of Workers’ Compensation Programs, Division of Coal Mine Workers’ Compensation; U.S. Department of Labor, Mine Safety and Health Administration; and the U.S. Energy Information Administration.
The annual proportion of DOL Federal Black Lung Program claimants who received a determination of PMF has increased since 1978 (Figure 2). The odds of a PMF case occurring within a year increased significantly, with evidence of a quadratic association, throughout the study period, controlling for coal mine employment. Joinpoint regression analysis identified four time segments in which the linear change in proportion of PMF cases differed significantly from one another. The proportion of PMF cases significantly increased from 1970 to 1975 (0.29% annual percent change [APC]; 95% confidence interval [CI], 0.28–0.30%; P < 0.0001), decreased from 1975 to 1978 (–0.35% APC; 95% CI, –0.44% to –0.25%; P = 0.27), increased from 1978 to 1996 (0.06% APC; 95% CI, 0.05–0.07%; P < 0.0001), and began increasing at a significantly increased rate after 1996 (0.26% APC; 95% CI, 0.25–0.28%; P < 0.0001). The overall average annual percent change from 1970 to 2016 was 0.14%.
Figure 2.
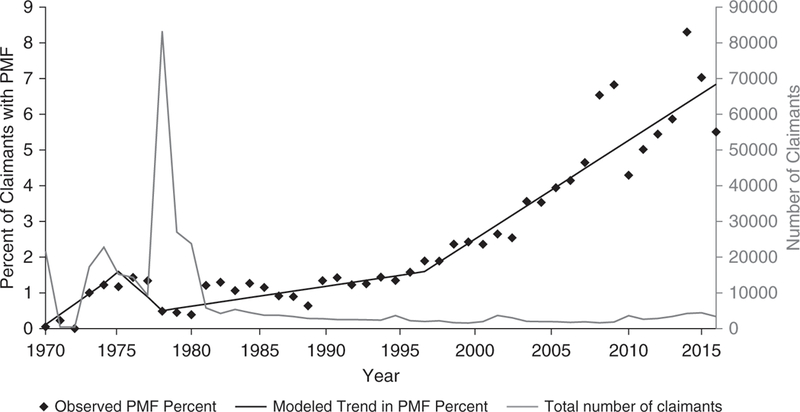
Number of claimants for Federal Black Lung Program benefits and the percentage of these claimants that received a determination of progressive massive fibrosis (PMF) during their claim process, 1970–2016. Observed and Joinpoint regression model results are displayed. Data restricted to those miners with between 5 and 60 years of coal mine employment. Data source: U.S. Department of Labor, Office of Workers’ Compensation Programs, Division of Coal Mine Workers’ Compensation.
Geographic Distribution
The geographic distribution of PMF cases differed significantly from non-PMF cases (Table 1). A large proportion (83.9%) of PMF cases from 1970 to 2016 included claimants who last worked as a miner in West Virginia (n = 1,327, 28.4%), Kentucky (n = 945, 20.2%), Pennsylvania (n = 935, 20.0%), or Virginia (n = 714, 15.3%), despite only 62% of all claims originating from these states (see Figure E2). Results from linear regression models of the proportion all claimants with a determination of PMF from 1970 to 2016 indicate that the annual proportion of PMF cases increased significantly in each of these states (Figure 3). The percentage of PMF cases increased most in Virginia (31.5% APC; 95% CI, 31.2–31.7%; P < 0.0001), where in 2009, over 17% (n = 40) of claimants received a determination of PMF. The percentage of PMF cases also increased in Kentucky (16.6% APC; 95% CI, 16.5–16.7%; P< 0.0001) and West Virginia (16.8% APC; 95% CI, 16.6–16.9%; P < 0.0001), where 5–11% of claimants per year have had a determination of PMF in since 2011. Tennessee has fewer absolute numbers of PMF cases than its central Appalachian neighbors, but has experienced a significant increase in percent of claimants with PMF (16.1% APC; 95% CI, 15.7–16.4%; P = 0.0001), peaking in 2008 with 17.7% (n = 6). The APC in proportion of claimants with PMF in Pennsylvania was 4.7% (95% CI, 4.6–4.8%; P < 0.0001). In contrast, less than 4% ofFederal Black Lung Program claimants from the rest of the United States had a PMF determination annually (Figure 4).
Figure 3.
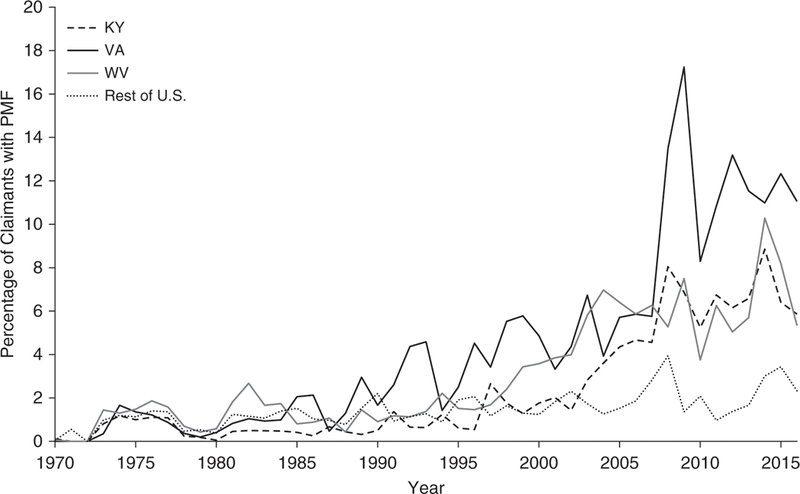
Percentage of claimants for Federal Black Lung Program benefits who received a determination of progressive massive fibrosis (PMF) during their claim process in the central Appalachian states of Kentucky, Virginia, and West Virginia compared with the rest of the United States, 1970–2016. Data restricted to those miners with between 5 and 60 years of coal mine employment. Data source: U.S. Department of Labor, Office of Workers’ Compensation Programs, Division of Coal Mine Workers’ Compensation.
Figure 4.
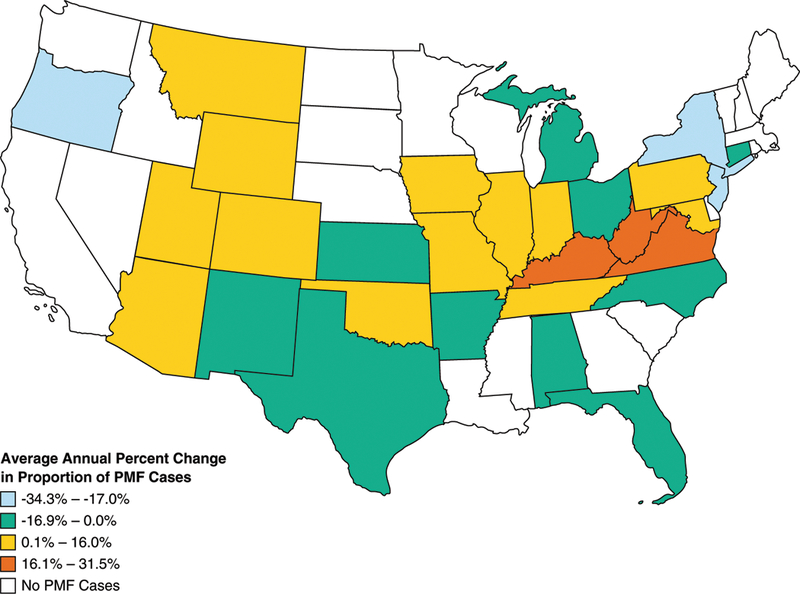
Average annual percent change in the proportion of coal miners with PMF among Federal Black Lung Program claimants by state, 1970–2016. Hawaii and Alaska had no cases of PMF and are not pictured. Data restricted to those miners with between 5 and 60 years of coal mine employment. Data source: U.S. Department of Labor, Office of Workers’ Compensation Programs, Division of Coal Mine Workers’ Compensation.
Pattern of Radiographic Findings
Among cases with a PMF determination, 2,318 were miners who made claims after January 1, 2000. Of the 1,930 claimants with available chest radiograph classifications, data about large opacities were missing for 283 (15%). Of those with data, 1,621 (84%) had a recorded finding of large opacities, indicative of PMF: 915 miners (56%) had category A; 548 (34%) had category B; and 158 (10%) had category C (Table 2). In addition, 26 miners had no large opacity recorded; we do not know how PMF was determined to be present in those cases. Forty percent of PMF cases had low small opacity profusion scores (category one), while the remainder (60%) had category two or higher simple pneumoconiosis.
Table 2.
Distribution of International Labor Office classifications of large and small opacities for miners with a determination of PMF and an available chest radiograph in the Department of Labor clinical data
| Large Opacity Category* | n | % |
| A | 915 | 47 |
| B | 548 | 28 |
| C | 158 | 8 |
| No large opacity | 26 | 1 |
| Missing | 283 | 15 |
| Total: | 1,930 | |
|
Small Opacity Profusion Category† |
n | % |
| 0 | 4 | 0.2 |
| 1 | 645 | 40 |
| 2 | 762 | 47 |
| 3 | 205 | 13 |
| Missing | 5 | 0.3 |
| Total: | 1,621 | |
Definition of abbreviations: ILO = International Labor Office; PMF = progressive massive fibrosis.
Categories shown reflect categories of large opacities according to the ILO Classification of Radiographs for Pneumoconiosis.
Categories shown reflect major categories of small opacity profusion according to the ILO Classification of Radiographs for Pneumoconiosis. Small opacity profusion categories shown only for radiographs with large opacity categories indicating PMF (category A, B, or C; n = 1,621).
Discussion
The frequency and proportion of PMF in former U.S. coal miners applying for Federal Black Lung Program benefits has significantly increased from 1970 to 2016, with a significantly accelerated rate of increase since 1996. We identified 2,474 cases of PMF in the 21 years from 1996 to 2016, which exceeds the number of cases found in the 26 years since the program began in 1970 (n = 2,205). This marked rise in PMF cases has occurred during a period of declining workforce numbers, but cannot simply be attributed to increased numbers of claimants as the number of new claimants has been stable. These findings are consistent with previously published reports showing an increase in the number and severity of this most disabling form of coal workers’ pneumoconiosis.
Most PMF cases were among claimants working in the central Appalachian states of Kentucky, Virginia, and West Virginia. The significant increase since 1996 in the number of miners applying for federal benefits with PMF in the present study mirrors the trend described in national surveillance of active miners in the CWHSP, which has seen PMF in central Appalachia climb to unprecedented levels (11). This analysis indicates that Tennessee has a similar increase in its rate of claims with PMF in recent years and should be targeted for enhanced surveillance and prevention efforts in addition to Kentucky, Virginia, and West Virginia.
Cumulative dust exposure is an important risk factor for the development of PMF (21–23). Mine Safety and Health Administration (MSHA) dust data indicate that dust levels have been in compliance with the appropriate regulations (16). Our findings suggest that miners may have been exposed to higher average dust concentrations than reported (24, 25). Further, changes in mining methods and techniques may have altered the size, shape, and/or mineralogic characteristics of coal mine dust in ways that promote more intense fibrogenic lung responses, such as increased exposure to respirable silica (26–29).
For the most recent period of available data (1996–2016), the number of miners with PMF (n = 2,474) is more than 10 times greater than the number identified in working miners screened by the CWHSP (n = 225) (30). This may be a result of voluntary participation of active coal miners in the CWHSP. Most coal miners file for federal workers’ compensation after their careers have ended when there is greater incentive to file for benefits, which include medical care. This difference may also reflect cases that progress to PMF after a miner leaves mine employment. There is evidence that early-stage coal workers’ pneumoconiosis can progress to PMF even in the absence of continued coal mine dust exposure (10, 31, 32).
We found that 40% of miners with a determination of PMF had low small opacity profusion, a result that has not been frequently reported in the medical literature (33, 34). The conventional notion that a PMF lesion is seen only in cases with high-category simple pneumoconiosis (categories two or greater) is likely incorrect. High-category disease may progress to PMF as the result of coalescence of lesions, therefore reducing small opacity profusion, or may be the result of some individual lesions increasing in size. Uncertainty regarding the pattern of progression underscores the need for continued surveillance of low-profusion pneumoconiosis, even absent further exposure.
These workers’ compensation data were not designed for public health surveillance. Filing for federal black lung benefits is voluntary, and the proportion of coal miners who file for these benefits is unknown. There have been several legislative changes over time that have affected the number of claimants for Federal Black Lung Program benefits. Most notable was expanded eligibility criteria introduced in 1977, which led to a peak in new claimants, but changes limiting the amount of medical evidence that a coal operator and miner can submit (2001) and the passage of the “Byrd Amendment” in 2013, which introduced the 15-year presumption, led to increases in the number of claimants as well. These changes, however, are unlikely to have affected the proportion of claimants with PMF filing for benefits. Benefits application rates may also be affected by a state’s particular workers’ compensation rules as well as by the availability of knowledgeable local benefits counselors and clinics, whose funding has remained unchanged in recent decades, that help miners file black lung claims, and these data likely underestimate the number of miners with PMF. Further, some of our analyses were limited by missing information in the administrative and clinical data available on PMF. Finally, the DOL claims data only record the state in which the miner last worked in the coal industry, precluding a more nuanced geographic analysis of where exposures may have occurred.
The proportion of PMF cases among federal black lung claimants is increasing, and the number of coal miners with this severe and often fatal form of lung disease is substantial. Changes in mining processes associated with increased mechanization, mining of thin-seam coal, and an increase in silica exposure could be contributing to this increase, and additional research is needed to understand how these factors are associated with current disease trends. The exceptionally high number of contemporary cases of PMF identified in this claims database highlights the continuing need for effective primary and secondary prevention of dust-related lung disease in U.S. coal miners.
Supplementary Material
Acknowledgment:
The authors acknowledge the work of Michael Chance, Gerald Delo, Tracey Teague, and Bennett Stewart of the Department of Labor Division of Coal Mine Workers’ Compensation.
Supported by National Occupational Research Agenda intramural funding from the National Institute for Occupational Safety and Health and a grant from the Alpha Foundation for the Improvement of Mining Safety and Health, Inc. The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the National Institute for Occupational Safety and Health, Centers for Disease Control and Prevention. The views, opinions, and recommendations addressed herein are solely those of the authors and do not imply any endorsement by the Alpha Foundation, its directors, and staff.
Footnotes
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Wang ML, Beeckman-Wagner LA, Wolfe AL, Syamlal G, Petsonk EL. Lung-function impairment among US underground coal miners, 2005 to 2009: geographic patterns and association with coal workers’ pneumoconiosis. J Occup Environ Med 2013;55:846–850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kuempel ED, Stayner LT, Attfield MD, BuncherCR. Exposure-response analysis of mortality among coal miners in the United States. Am J Ind Med 1995;28:167–184. [DOI] [PubMed] [Google Scholar]
- 3.Attfield MD, Kuempel ED. Mortality among U.S. underground coal miners: a 23-year follow-up. Am J Ind Med 2008;51:231–245. [DOI] [PubMed] [Google Scholar]
- 4.Antao VC dos Santos, Petsonk EL, Sokolow LZ, Wolfe AL, Pinheiro GA, Hale JM, et al. Rapidly progressive coal workers’ pneumoconiosis in the United States: geographic clustering and other factors. Occup Environ Med 2005;62:670–674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Antao V, Petsonk EL, Attfield MD; Centers for Disease Control and Prevention (CDC). Advanced cases of coal workers’ pneumoconiosis: two counties, Virginia, 2006. MMWR Morb Mortal Wkly Rep 2006;55: 909–913. [PubMed] [Google Scholar]
- 6.Laney AS, Weissman DN. The classic pneumoconioses: new epidemiological and laboratory observations. Clin Chest Med 2012; 33:745–758. [DOI] [PubMed] [Google Scholar]
- 7.Blackley DJ, Halldin CN, Laney AS. Resurgence of a debilitating and entirely preventable respiratory disease among working coal miners. Am J Respir Crit Care Med 2014;190:708–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Laney AS, Attfield MD. Examination of potential sources of bias in the US Coal Workers’ Health Surveillance Program. Am J Public Health 2014; 104:165–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, Respiratory Health Division. Work-Related Lung Disease Surveillance System (eWoRLD). Publication No. 2011–570 [2011; accessed 2017 Aug 17]. Available from:https://wwwn.cdc.gov/eworld/Data/570..
- 10.Halldin CN, Wolfe AL, Laney AS. Comparative respiratory morbidity of former and current US coal miners. Am J Public Health 2015;105: 2576–2577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Blackley DJ, Crum JB, Halldin CN, Storey E, Laney AS. Resurgence of progressive massive fibrosis in coal miners: eastern Kentucky, 2016. MMWR Morb Mortal Wkly Rep 2016;65:1385–1389. [DOI] [PubMed] [Google Scholar]
- 12.Blackley DJ, Reynolds LE, Short C, Carson R, Storey E, Halldin CN, et al. Progressive massive fibrosis in coal miners from 3 clinics in Virginia. JAMA 2018;319:500–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.U.S. Department of Labor, Office of Workers’ Compensation Programs (OWCP), Division of Coal Mine Workers’ Compensation (DCMWC). Guide to filing for black lung benefits: miner’s claim [accessed 2017 Aug 14]. Available from: https://www.dol.gov/owcp/dcmwc/filing_guide_miner.htm.
- 14.International Labour Office. Guidelines for the use of the ILO International Classification of Radiographs of Pneumoconioses., rev. ed., 2011. Geneva, Switzerland: International Labour Office; 2011. [Google Scholar]
- 15.Title 20 C.F.R. Employees’ Benefits §718.304. Irrebuttable presumption of total disability or death due to pneumoconiosis [accessed 2018 Jan 2]. Available from: https://www.ecfr.gov/cgi-bin/retrieveECFR?gp=1&SID= 11539888d27eca5b110ff810692ff280&ty=HTML&h=L&mc=true&r= SECTION&n=se20.4.718_1304.
- 16.Mine Safety and Health Administration. Statistics: Mine Safety and Health Administration (MSHA) [2017; accessed 2017 July 20]. Available from: https://www.msha.gov/data-reports/statistics.
- 17.Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for Joinpoint regression with applications to cancer rates. Stat Med 2000;19: 335–351. [DOI] [PubMed] [Google Scholar]
- 18.Statistical Methodology and Applications Branch, Surveillance Research Program, National Cancer Institute. Joinpoint Regression Program; 2017. [Google Scholar]
- 19.SAS Institute, Inc. SAS. Cary, NC:SAS Institute; 2002. [Google Scholar]
- 20.Black Lung Benefits Reform Act of 1977. Public Law 95–239. 92 Stat. 95. 1 March 1977 [March 1, 1978; accessed 2017 Sept 14]. Available from: https://www.gpo.gov/fdsys/pkg/STATUTE-92/content-detail.html.
- 21.Attfield MD, Morring K. An investigation into the relationship between coal workers’ pneumoconiosis and dust exposure in U.S. coal miners. Am Ind Hyg Assoc J 1992;53:486–492. [DOI] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention (CDC). Pneumoconiosis prevalence among working coal miners examined in federal chest radiograph surveillance programs: United States, 1996–2002. MMWR Morb Mortal Wkly Rep 2003;52:336–340. [PubMed] [Google Scholar]
- 23.Attfield MD, Seixas NS. Prevalence of pneumoconiosis and its relationship to dust exposure in a cohort of U.S. bituminous coal miners and ex-miners. Am J Ind Med 1995;27:137–151. [DOI] [PubMed] [Google Scholar]
- 24.Weeks JL. The fox guarding the chicken coop: monitoring exposure to respirable coal mine dust, 1969–2000. Am J Public Health 2003;93: 1236–1244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Boden LI, Gold M. The accuracy of self-reported regulatory data: the case of coal mine dust. Am J Ind Med 1984;6:427–440. [DOI] [PubMed] [Google Scholar]
- 26.Johann-Essex V, Keles C, Rezaee M, Scaggs-Witte M, Sarver E. Respirable coal mine dust characteristics in samples collected in central and northern Appalachia. Int J Coal Geol 2017;182:85–93. [Google Scholar]
- 27.Suarthana E, Laney AS, Storey E, Hale JM, Attfield MD. Coal workers’ pneumoconiosis in the United States: regional differences 40 years after implementation of the 1969 Federal Coal Mine Health and Safety Act. Occup Environ Med 2011;68:908–913. [DOI] [PubMed] [Google Scholar]
- 28.Cohen RA, Petsonk EL, Rose C, Young B, Regier M, Najmuddin A, et al. Lung pathology in U.S. coal workers with rapidly progressive pneumoconiosis implicates silica and silicates. Am J Respir Crit Care Med 2016;193:673–680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Halldin CN, Reed WR, Joy GJ, Colinet JF, Rider JP, Petsonk EL, et al. Debilitating lung disease among surface coal miners with no underground mining tenure. J Occup Environ Med 2015;57:62–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Laney AS, Blackley DJ, Halldin CN. Radiographic disease progression in contemporary US coal miners with progressive massive fibrosis. Occup Environ Med 2017;74:517–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kimura K, Ohtsuka Y, Kaji H, Nakano I, Sakai I, Itabashi K, et al. Progression of pneumoconiosis in coal miners after cessation of dust exposure: a longitudinal study based on periodic chest X-ray examinations in Hokkaido, Japan. Intern Med 2010;49:1949–1956. [DOI] [PubMed] [Google Scholar]
- 32.Maclaren WM, Soutar CA. Progressive massive fibrosis and simple pneumoconiosis in ex-miners. Br J Ind Med 1985;42:734–740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hodus T, Attfield M. Progressive massive fibrosis developing on a background of minimal simple coal workers’ pneumoconiosis. In: Proceedings of the VIIth International Pneumoconioses Conference [1990; accessed 2018 Sept 11]. U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control, National Institute for Occupational Safety and Health, DHHS (NIOSH) publication No. 90–108, part 1,122–126. Available from: https://www.cdc.gov/niosh/docs/90-108/pdfs/90-108-1pdf. [Google Scholar]
- 34.Hurley JF, Alexander WP, Hazledine DJ, Jacobsen M, Maclaren WM. Exposure to respirable coalmine dust and incidence of progressive massive fibrosis. Br J Ind Med 1987;44:661–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


