Abstract
Background
Recently, a stag beetle (SB) knife was introduced to reduce the difficulty of peroral endoscopic myotomy (POEM). The objective of this study was to evaluate the efficacy and safety of the SB knife.
Material/Methods
A total of 71 patients undergoing POEM with the SB knife for esophageal achalasia were included. We used esophagography, manometry, esophagogastroduodenoscopy (EGD), and Eckardt score to assess the utility and safety.
Results
All cases were completed for POEM. The incidence of adverse events during the operation were 2.8%; however, all cases were treated conservatively. There was a vast improvement in clinical symptoms and endoscopic findings. The average Eckardt score was 6.9 before and 0.6 at 1 year after POEM (p<0.05). The average lower esophageal sphincter (LES) pressure before and 6 months after POEM were 44.34±14.83 mmHg and 19.14±6.74 mmHg (p<0.05), respectively. The average LES relaxation pressure before and 6 months after POEM was 12.11±5.02 mmHg and 3.22±2.29 mmHg (p<0.05), respectively.
Conclusions
POEM with the SB Knife is technically efficient and safe in treating achalasia and is associated with favorable short-term outcomes.
MeSH Keywords: Esophageal Achalasia, Follow-Up Studies, Gastroesophageal Reflux
Background
Achalasia is an esophageal motor disorder and a rare disease [1]. It is characterized by the absence of esophageal peristalsis and the ineffective relaxation of the lower esophageal sphincter (LES). Although most of the causes of achalasia remain largely unknown, some believe that it is due to the ineffective inhibitory ganglion cells in the myenteric plexus [2,3]. At present, the main objective of treatment is to confine the pressure of the LES and to relieve symptoms. Inoue et al. developed peroral endoscopic myotomy (POEM) [4]. The procedure is an advanced treatment method for esophageal achalasia, which allows for an ample incision of the muscle layer alone and does not damage the surface. POEM has been widely accepted as an efficient and minimally invasive treatment for esophageal achalasia. There have been many reports on the feasibility and safety of POEM, but the efficacy of POEM on achalasia differs [5–8]. The technical difficulty makes it impossible to be applied more widely, especially by unskilled endoscopists. Since 2010, several devices, such as the Triangle Tip (TT) knife, Hook Knife, Hybrid knife, and dual knife, have been used for POEM. The drawbacks of conventional devices for POEM are that they use single electrodes, and are difficult to manipulate in the target tissue, which results in unintentional incision due to their movement, perforation of the tissue, and mediastinal emphysema. To reduce the incidence of intraoperative complications and the difficulty of POEM, a new stag beetle knife (SB knife) was introduced. The SB knife was also used by Bittinger [9] at the same time, but only 7 patients were treated. The SB knife was designed to prevent unexpected injury by endoscopists [10,11]. Studies have shown that endoscopic submucosal dissection (ESD) with the SB knife was safer than that using a conventional knife for superficial esophageal neoplasms [12]. In addition, ESD with the SB knife was technically efficient and safe in treating early colorectal neoplasms [13]. The aim of this study was to evaluate the efficacy and safety of the SB knife.
Material and Methods
Patients
This was a single-center retrospective study. We collected data from 71 esophageal achalasia patients who underwent POEM with the SB knife at our hospital from September 2015 to March 2018. Patients were diagnosed with esophageal achalasia by either conventional or high-resolution esophageal manometry [14]. Exclusion criteria were: (1) patients with active esophagitis or esophageal ulcer, and (2) patients with severe systemic diseases who are unable to be treated with POEM. The study complied with the principles of the Declaration of Helsinki and was approved by the Institutional Review Board of Renmin Hospital of Wuhan University (approval no. 2014-KYLL-048).
Main equipment used
EGD (GIF-Q260J; Olympus), a stag beetle knife (MD-47704; Sumitomo Bakelite) (Supplementary Figure 1), injection needle (NM-200U-0423), hemostatic forceps (FD-411QR; Olympus), and Resolution clips (Boston Scientific, Natick, MA) were used.
POEM procedure
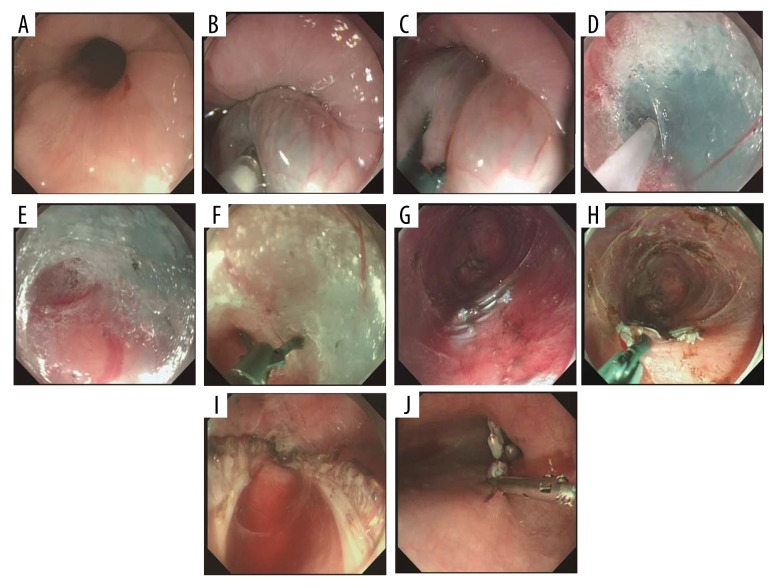
All patients were given second-generation cephalosporins (cefotiam; Harbin Medical) to prevent infection before the procedure. On the day of the operation, patients were nil per os (NPO). POEM was performed as previously described [15], but we made some minor modifications. Residual food in the esophagus was cleared. The POEM procedure is shown in Figure 1, and the tissue was marked with physiological saline and methylene blue about 10 cm above the esophagogastric junction (EGJ) in the posterior of the esophagus (Figure 1A–1C). A submucosal tunnel was created by the SB knife (Figure 1D–1G). A mucosal incision was created and a 1.5–2.0 cm mucosectomy was performed with a stag beetle knife. The last 2 steps are full-thickness myotomy using the SB knife (Figure 1H, 1I) and closure of the mucosal entry with endoscopic clips (Figure 1J).
Figure 1.
POEM procedure (posterior myotomy). (A) preoperative image (B) submucosal injection (C) tunnel entry (D–G) submucosal tunnel (H, I) full-thickness myotomy (J) closure of mucosal entry.
Post-POEM management and follow-up
All patients were maintained NPO the first day after the operation. Intravenous antibiotics and proton pump inhibitor (PPI) therapy were used for 3 days. A post-procedure chest radiograph and barium esophagogram were routinely obtained on the second postoperative day to look for any leaks.
Follow-up data were collected after POEM to assess the effects. The follow-up visit included esophageal manometry, EGD, and evaluation of symptoms using the Eckardt score. The therapeutic success of the Eckardt score was defined as less than or equal to 3 [16]. We used the Los Angeles classification to classify esophagitis [17].
Statistical analysis
SPSS version 21.0 (SPSS, Inc., Chicago) was used for statistical analysis. The paired samples t test and the Wilcoxon signed-rank test were used to compare paired data. The p value of <0.05 was considered statistically significant.
Results
Patient characteristics
Between September 2015 and March 2018, we collected 71 cases that were diagnosed as esophageal achalasia at our hospital and that were followed-up for 1 year after the POEM procedure with the SB knife (Table 1).
Table 1.
Patient demographics and perioperative characteristics.
| Age, years, mean ±SD (range) | 41.2±13.6 (19–77) |
| Sex, Female: Male | 44: 27 |
| Symptoms duration, median (range), months | 59.6±79.7 (3–360) |
| Type of achalasia | |
| Straight type | 59 |
| Sigmoid type | 12 |
| Previous treatment, n (%) | 21 (29.6) |
| EBD | 14 (19.8) |
| Stenting | 1 (1.4) |
| BTI | 4 (5.6) |
| POEM | 2 (2.8) |
| No previous treatment | 50 (70.4) |
| Length of procedure (range), minutes | 53.5±16.4 (40–89) |
| Length of submucosal tunnel, mean (range), cm | 12±2.00 (8–17) |
| Myotomy length (total), mean (range), cm | 9.89±2.26 (6–15) |
| Postoperative stay, mean ±SD (range), days | 8.70±2.48 (3–20) |
SD – standard deviation; EBD – endoscopic balloon dilatation; BTI – botulinum toxin injection; POEM – peroral endoscopic myotomy.
Of the 71 cases (female/male: 44/27), the mean age was 41.2±13.6 (range 19–77) years, and the average time of operation was 53.5 min (range 40–89 min). Their average duration of disease was 59.6±79.7 (range 3–360) months. The average length of the submucosal tunnel was 12.0±2.00 (range 8–17) cm, and the mean myotomy length was 9.9±2.3 (range 6–15) cm.
Twenty-one patients (29.6%) had received prior therapy. Fourteen patients had undergone endoscopic balloon dilatation, 1 patient had undergone stenting and an endoscopic balloon dilatation procedure, 2 patients had undergone the POEM procedure 1 year ago at another hospital, and 4 patients had received one-time botulinum toxin injection. No severe complications were reported, and the mean hospital length of stay was 8.7±2.5 (range 3–20) days.
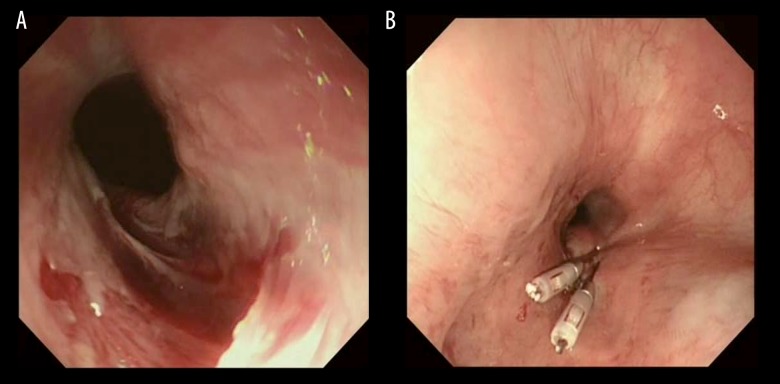
Adverse events
All patients were assessed for adverse events. Mucosal injury occurred in 2 cases (Figure 2). One patient had esophageal perforation, but did not develop into mediastinitis. No patients suffered from substantial bleeding requiring interventions, subcutaneous emphysema, pneumothorax, pneumomediastinum, or pneumoperitoneum. The incidence of complications during the operation was 2.8% (2/71), and all cases were treated conservatively.
Figure 2.
Adverse events. (A) Cardia mucosal perforation appeared and hemostasis was performed with resolution clips (B).
Post-POEM clinical outcomes
Of the 71 cases, LES pressure, barium esophagogram, subjective symptoms, and endoscopic findings were significantly improved.
Of 67 patients with available data on pressure before and 6 months after POEM, the median pre-POEM LES pressure was 44.3±14.8 (23.4–78) mmHg, and the median post-POEM LES pressure was 19.1±6.7 (7.8–35) mmHg. The difference was significant (P<0.05). Furthermore, the median pre-POEM LES relaxation pressure was 12.1±5.0 (5.8–22.9) mmHg, and the median post-POEM relaxation LES pressure was 3.2±2.3 (0.6–8.9) mmHg. There was a significant difference (p<0.05). Compared to before POEM (Figure 3A), the contrast agent smoothly passed through the esophagus 6 months after POEM (Figure 3B).
Figure 3.
Results of barium esophagogram. (A) Barium esophagogram before POEM. Typical bird beak appearance is observed and barium did not pass through the esophagogastric junction for more than a few minutes. (B) Esophagogram at 6 months after POEM. Passage of contrast agent is remarkably improved. No stasis is seen on the post-procedure esophagogram.
Three months after POEM, Eckardt scores were available for 71 patients (100%). At 6 months after POEM, 4 patients were lost to follow-up (1 died due to myocardial infarction and we lost contact with 3 patients); thus, Eckardt scores were available for 67 patients (94%). Twelve months after POEM, Eckardt score were available for 67 patients (94%). The rate of clinical success (Eckardt scores ≤3) was 98.6% (70/71), 97% (65/67), 92.5% (62/67) after POEM at 3 months, 6 months, and 1 year, respectively (Table 2). Three months after POEM, the Eckardt score was equal to 4 in 1 patient, and there was a large amount of residue in the esophagus during endoscopy. The treatment was unsuccessful for this patient. At 6 months after POEM, 2 patients had Eckardt scores 3. Twelve months after POEM, 5 patients had Eckardt scores >3. The mean preoperative and 12-month post-POEM Eckardt scores were 6.9 ±1.9 (3–12) and 0.6±0.8 (0–3), respectively. Therefore, the Eckardt scores decrease remarkably after POEM (p<0.05).
Table 2.
Clinical response after POEM.
| Baseline | 3 months after POEM | 6 months after POEM | 12 months after POEM | |
|---|---|---|---|---|
| No. of patients with available data | 71 | 71 | 67 | 67 |
| Clinical success (Eckard score ≤3),% | 98.6% (70/71) | 97% (65/67) | 92.5% (62/67) | |
| Eckard score (mean ±SD) | 6.9±1.9 | 0.9±1.3 | 0.7±1.1 | 0.6±0.8 |
POEM – peroral endoscopic myotomy; SD – standard deviation.
Reflux and reflux-associated problems
There was a systematic clinical follow-up. All patients were scheduled for a follow-up at 12 months after POEM for clinical assessment using the EGD and symptom questionnaires that included items on reflux and PPI use. Details of post-POEM follow-up are shown in Table 3. In addition, 4 patients had from reflux symptoms without lesions, 15 patients had reflux symptoms with lesions, and there were 2 asymptomatic patients with lesions.
Table 3.
Follow-up clinical data.
| Time points | 12 months |
|---|---|
| Clinical reflux | |
| Heart burn | |
| No. of cases | 19 |
| Daily | 15 |
| Occasionally | 4 |
| PPI consumption | |
| No. of cases | 19 |
| Daily | 15 |
| Occasionally | 4 |
| Esophagitis | |
| A | 10 |
| B | 5 |
| C | 2 |
| D | 0 |
PPI – proton pump inhibitor.
Discussion
At present, all the available treatments for achalasia aim to reduce the pressure of LES, alleviate the patient’s symptoms of dysphagia, and prevent the development of mega-esophagus. POEM is considered a better choice than laparoscopic Heller’s myotomy (LHM) or balloon dilation [18]. Moreover, the safety and efficacy of POEM are not affected by previous endoscopic balloon dilatation (EBD) or botulinum toxin injection (BTI) treatments [19]. POEM may become the first-line treatment [6]. Since 2010, thousands of POEM procedures have been performed; however, there is no standard technique, and the rates of clinical success and adverse events vary widely among centers [12].
The SB knife Jr is already available all over the world, and it is more useful in POEM than the SB knife shown in Supplementary Figure 1. However, a new device to reduce adverse events is important to refine the procedure and make it a safer treatment option. The preliminary experience of POEM using the SB knife has been reported in by Bittinger [9]. However, there is a need for more data. In contrast to Bittinger, we only use the SB knife to complete the operation, without changing the knife to create the submucosal tunnel.
In our research, all cases were completed for POEM. The incidence of adverse events during the operation was low. POEM with the SB Knife appears to be technically efficient and safe in treating achalasia and is associated with favorable short-term outcomes.
The SB knife has 3 significant advantages over other devices. First, the SB knife can precisely control the thickness of the muscle incision, which can effectively maintain the integrity of the esophageal serosa. This knife, which uses a monopole, is a kind of grasping forceps. The outer edge of the scissors is insulated from the surrounding tissue. With an external electrically-insulated coating, it can also maintain a stable operation by grasping the mucosa or muscular fibers. The use of the SB knife also makes the operation easier, even under conditions such as breath movement and heartbeat [20]. Second, the SB knife can coagulate the blood vessels while cutting the muscles, without changing devices [21]. This can effectively control intraoperative bleeding and reduce the incidence of bleeding. Adequate hemostasis also keeps the field of view clean and avoids surgical mistakes due to poor visibility. Third, the shape of the SB knife and its ability to rotate 360° on its axis allows easy and precise positioning in the submucosal tunnel [22]. In the narrow space of the submucosal tunnel, the SB knife can be precisely clamped, separated, and cut. The most important advantage of SB knife is that the ability to grasp the target tissue allows controlled resection without requiring complex endoscopic movements and techniques, as required for conventional ESD devices.
In our center, patients have been treated with the SB knife without any serious adverse events, and the total incidence of adverse events has decreased. Compared with previously reported outcomes of POEM using conventional devices, our results appear promising. A recent meta-analysis of 36 studies, including 2373 patients who underwent POEM, showed that the rates of common perioperative adverse events included mucosal injury, esophageal perforation, substantial bleeding requiring interventions, subcutaneous emphysema, pneumothorax, pneumomediastinum, pneumoperitoneum, and pleural effusion were 4.8% (95%CI 2.0–8.5%), 0.2% (95% CI 0–1.1%), 7.5% (95% CI 3.5–12%), 0.2% (95% CI 0–1.4%), 1.2% (95% CI 0.1–4.3%), 1.1% (95% CI 0.1–4.7%), 6.8% (95% CI 1.9–14%), and 1.2% (95% CI 0–8.3%), respectively [23]. In contrast, we had a 2.8% mucosal injury rate and a 1.4% esophageal perforation rate during the procedure, without any other common perioperative complications.
According to our data, there were significant improvements in both clinical symptoms and endoscopic results. The rate of clinical success was 98.6% and 97% at 3- and 6-month follow-up, respectively. In total, 71 patients completed the POEM full-thickness myotomy treatment with the SB knife. Only 1 patient experienced treatment failure 3 months after POEM, and this case was the eighth in our hospital for POEM surgery. The 54-year-old man had a treatment history of balloon dilatation. A preoperative upper gastrointestinal barium showed this patient to be a non-sigmoid type. The reason for the failure may be attributed to the formation of fibrotic scars that can occur in patients with previous balloon dilation, an intraoperative coagulation injury, and/or the learning curve of the operator [24,25]. We found that the rate of clinical success decreased to 92.5% at 1-year follow-up. This result is similar to that reported by Ngamruengphong [26]. In this paper, the rate of clinical success decreased from 98% at 6 months to 91% at 2-year follow-up. Thus, patients should receive follow-up to monitor for recurrence.
There are several limitations to our study. It was accomplished at a single center and had a moderate sample size. In addition, the study lacked a control group, which is a standard technique. What’s more, this was a retrospective study. However, for the first time, we provide valid information about the feasibility and efficacy of POEM with the SB knife for treating esophageal achalasia.
Conclusions
POEM performed with the SB knife could be a feasible, efficient, and safe therapeutic technique for patients with esophageal achalasia, and it is technically easy to perform compared with conventional knifes. However, further evidence is required to fully evaluate and compare the use of the SB knife in POEM.
Supplementary Figure
The monopolar blades are insulated both externally and on the tip. The blades are isolated to ensure that the electric current used in the monopolar device is applied between the blades. It is a rotatable electrosurgical forceps that can be used like an electrosurgical scissor, thus enabling fast and accurate positioning.
Acknowledgements
We would like to thank Dr Katelyn O’Neill from the University of Nebraska Medical Center for improving the language of this manuscript.
Footnotes
Source of support: Departmental sources
Conflicts of interest
None.
References
- 1.Boeckxstaens GE. Achalasia: From bench to peroral endoscopic myotomy. Dig Dis. 2016;34:476–82. doi: 10.1159/000445222. [DOI] [PubMed] [Google Scholar]
- 2.Boeckxstaens GE, Zaninotto G, Richter JE. Achalasia. Lancet. 2014;383:83–93. doi: 10.1016/S0140-6736(13)60651-0. [DOI] [PubMed] [Google Scholar]
- 3.Kahrilas PJ. Treating achalasia; More than just flipping a coin. Gut. 2016;65:726–27. doi: 10.1136/gutjnl-2015-311016. [DOI] [PubMed] [Google Scholar]
- 4.Inoue H, Minami H, Kobayashi Y, et al. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy. 2010;42:265–71. doi: 10.1055/s-0029-1244080. [DOI] [PubMed] [Google Scholar]
- 5.Sharata AM, Dunst CM, Pescarus R, et al. Peroral endoscopic myotomy (POEM) for esophageal primary motility disorders: Analysis of 100 consecutive patients. J Gastrointest Surg. 2015;19:161–70. doi: 10.1007/s11605-014-2610-5. [DOI] [PubMed] [Google Scholar]
- 6.Inoue H, Sato H, Ikeda H, et al. Per-oral endoscopic myotomy: A series of 500 patients. J Am Coll Surg. 2015;221:256–64. doi: 10.1016/j.jamcollsurg.2015.03.057. [DOI] [PubMed] [Google Scholar]
- 7.Familiari P, Gigante G, Marchese M, et al. Peroral endoscopic myotomy for esophageal achalasia: Outcomes of the first 100 patients with short-term follow-up. Ann Surg. 2016;263:82–87. doi: 10.1097/SLA.0000000000000992. [DOI] [PubMed] [Google Scholar]
- 8.Ramchandani M, Nageshwar Reddy D, et al. Peroral endoscopic myotomy for achalasia cardia: Treatment analysis and follow up of over 200 consecutive patients at a single center. Dig Endosc. 2016;28:19–26. doi: 10.1111/den.12495. [DOI] [PubMed] [Google Scholar]
- 9.Bittinger M, Messmann H. Use of the stag beetle knife for peroral endoscopic myotomy for achalasia: A novel method for myotomy. Gastrointest Endosc. 2015;82:401–2. doi: 10.1016/j.gie.2015.03.1906. [DOI] [PubMed] [Google Scholar]
- 10.Oka S, Tanaka S, Takata S, et al. Usefulness and safety of SB knife Jr in endoscopic submucosal dissection for colorectal tumors. Dig Endosc. 2012;24:90–95. doi: 10.1111/j.1443-1661.2012.01255.x. [DOI] [PubMed] [Google Scholar]
- 11.Honma K, Kobayashi M, Watanabe H, et al. Endoscopic submucosal dissection for colorectal neoplasia. Dig Endosc. 2010;224:307–11. doi: 10.1111/j.1443-1661.2010.01018.x. [DOI] [PubMed] [Google Scholar]
- 12.Kuwai T, Yamaguchi T, Imagawa H, et al. Endoscopic submucosal dissection for early esophageal neoplasms using the stag beetle knife. World J Gastroenterol. 2018;24:1632–40. doi: 10.3748/wjg.v24.i15.1632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Takasago T, Kuwai T, Yamaguchi T, et al. Endoscopic submucosal dissection with a scissors-type knife for post-EMR recurrence tumor involving the colon diverticulum. VideoGIE. 2017;2(8):211–12. doi: 10.1016/j.vgie.2017.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kaindlstorfer A, Pointner R. An appraisal of current dysphagia diagnosis and treatment strategies. Expert Rev Gastroenterol Hepatol. 2016;10:929–42. doi: 10.1586/17474124.2016.1158098. [DOI] [PubMed] [Google Scholar]
- 15.Lv L, Liu J, Tan Y, et al. Peroral endoscopic full-thickness myotomy for the treatment of sigmoid-type achalasia: Outcomes with a minimum follow-up of 12 months. Eur J Gastroenterol Hepatol. 2016;28:30–36. doi: 10.1097/MEG.0000000000000491. [DOI] [PubMed] [Google Scholar]
- 16.Werner YB, Rösch T. POEM and submucosal tunneling. Curr Treat Options Gastroenterol. 2016;14:163–77. doi: 10.1007/s11938-016-0086-y. [DOI] [PubMed] [Google Scholar]
- 17.Armstrong D, Bennett JR, Blum AL, et al. The endoscopic assessment of esophagitis: A progress report on observer agreement. Gastroenterology. 1996;111:85–92. doi: 10.1053/gast.1996.v111.pm8698230. [DOI] [PubMed] [Google Scholar]
- 18.Talukdar R, Inoue H, Nageshwar Reddy D. Efficacy of peroral endoscopic myotomy (POEM) in the treatment of achalasia: A systematic review and meta-analysis. Surg Endosc. 2015;29:3030–46. doi: 10.1007/s00464-014-4040-6. [DOI] [PubMed] [Google Scholar]
- 19.Von Renteln D, Fuchs KH, Fockens P, et al. Peroral endoscopic myotomy for the treatment of achalasia: An international prospective multicenter study. Gastroenterology. 2013;145:309–11.e1–3. doi: 10.1053/j.gastro.2013.04.057. [DOI] [PubMed] [Google Scholar]
- 20.Fujinami H, Hosokawa A, Ogawa K, et al. Endoscopic submucosal dissection for superficial esophageal neoplasms using the stag beetle knife. Dis Esophagus. 2014;27:50–54. doi: 10.1111/dote.12039. [DOI] [PubMed] [Google Scholar]
- 21.Yamashina T, Takeuchi Y, Nagai K, et al. Scissor-type knife significantly improves self-completion rate of colorectal endoscopic submucosal dissection: Single-center prospective randomized trial. Dig Endosc. 2017;29:322–29. doi: 10.1111/den.12784. [DOI] [PubMed] [Google Scholar]
- 22.Battaglia G, Antonello A, Realdon S, et al. Flexible endoscopic treatment for Zenker’s diverticulum with the SB Knife. Preliminary results from a single-center experience. Dig Endosc. 2015;27:728–33. doi: 10.1111/den.12490. [DOI] [PubMed] [Google Scholar]
- 23.Akintoye E, Kumar N, Obaitan I, et al. Peroral endoscopic myotomy: A meta-analysis. Endoscopy. 2016;48:1059–68. doi: 10.1055/s-0042-114426. [DOI] [PubMed] [Google Scholar]
- 24.Kurian AA, Dunst CM, Sharata A, et al. Peroral endoscopic esophageal myotomy: Defining the learning curve. Gastrointest Endosc. 2013;77:719–25. doi: 10.1016/j.gie.2012.12.006. [DOI] [PubMed] [Google Scholar]
- 25.El Zein M, Kumbhari V, Ngamruengphong S, et al. Learning curve for peroral endoscopic myotomy. Endosc Int Open. 2016;4:E577–82. doi: 10.1055/s-0042-104113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ngamruengphong S, Inoue H, Chiu PW, et al. Long-term outcomes of per-oral endoscopic myotomy in achalasia patients with a minimum follow-up of 2 years: An international multicenter study. Gastrointest Endosc. 2017;85:927–33.e2. doi: 10.1016/j.gie.2016.09.017. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The monopolar blades are insulated both externally and on the tip. The blades are isolated to ensure that the electric current used in the monopolar device is applied between the blades. It is a rotatable electrosurgical forceps that can be used like an electrosurgical scissor, thus enabling fast and accurate positioning.