Abstract
Background/aims
Preventing and treating proliferative vitreoretinopathy (PVR) remain a serious challenge for vitreoretinal surgeons. PVR is a devastating complication of retinal detachment that results in recurrent detachment and limits visual recovery. At present, there is no effective treatment for PVR.
Materials and methods
A retrospective review was performed on a cohort of five consecutive eyes with severe PVR and recurrent retinal detachment that were treated with relaxing retinectomy, extended perfluorocarbon liquid tamponade (4–5 weeks) and a series of intravitreal methotrexate (MTX) injections (100–200 µg/0.05 mL for 10 weeks).
Results
All five patients remained reattached (100%) with 11–27 months of follow-up (mean = 17.4). 4 eyes recovered ambulatory vision (>20/200) with normal intraocular pressure and non-fibrotic laser scars along with the relaxing retinectomy. The initial patient remained reattached, but only had hand motions vision. The only adverse effect noted was mild superficial punctate keratopathy in one patient.
Conclusion
This small, retrospective study suggests that a series of MTX injections may be beneficial for treating complex retinal detachment caused by PVR. Further study is indicated.
Keywords: retina, treatment medical, treatment surgery, pharmacology, inflammation
Key message.
What is already known?
Methotrexate (MTX) may help treat proliferative vitreoretinopathy (PVR). The rate of anatomical reattachment following retinal reattachment surgery for a patient with PVR is only 60%–80%. Two previous reports found lower than expected rates of recurrent retinal detachment in patients with PVR who received various dosing schedules of intravitreal MTX.
What are the new findings?
Five consecutive eyes with severe PVR and recurrent retinal detachment were treated with relaxing retinectomy, extended perfluorocarbon liquid tamponade and a series of five intravitreal MTX injections. All five patients remained reattached (100%) with 11–27 months of follow-up (mean=17.4). The MTX injections were well tolerated. These results are better than expected for patients with recurrent retinal detachment due to PVR. We hypothesise that the MTX injections suppressed the aberrant cellular proliferation of PVR.
How might these results change the focus of research and clinical practice?
This small, retrospective study suggests that a series of MTX injections may be beneficial for treating complex retinal detachment caused by PVR. Further study is indicated.
Introduction
Preventing and treating proliferative vitreoretinopathy (PVR) remain a serious challenge for vitreoretinal surgeons. PVR is a devastating complication of retinal detachment that results in recurrent detachment and limits visual recovery. This occurs in 5%–10% of all retinal detachment surgeries, but accounts for 75% of subsequent retinal redetachment surgeries.1
Cellular proliferation produces epiretinal and subretinal membranes and intrinsic foreshortening of the retina—the hallmarks of PVR. These changes decrease retinal elasticity, which leads to the tractional elevation of the retina, creation of new retina breaks and recurrent retinal detachment.1 This cellular proliferation continues for 30–90 days after retinal reattachment. Any effective PVR treatment will need to inhibit this process for at least 60–90 days.
Methotrexate (MTX) may have promise for treating PVR. Elliot and Stryjewski treated a group of 10 eyes with either existing PVR (grade C or higher) or were considered to be at high risk for PVR (had undergone repair of a ruptured globe), with a series of 10 intravitreal MTX (400 µg/0.1 mL) injections over a 3-month period. All of these patients required complicated vitrectomy with silicone oil tamponade to reattach their retinas. The silicone oil was removed at 3 months and 80% of eyes remained reattached with a single surgery over 4–39 months (median 25 months) of follow-up. The final visual acuity ranged from 20/70 to HM (median 20/200). The MTX injections were well tolerated. Only one patient developed mild superficial punctate keratopathy.2
Sedaka and associates added 40 mg of MTX (equivalent to 400 µg/0.1 mL) to the infusion fluid at the time of retinal reattachment in a mixed group of 29 eyes presenting with either recurrent retinal detachment (RD) with PVR or severe inflammation associated with RD. In all, 26 of 29 eyes (90%) remained reattached after the intraoperative MTX infusion.3 Ghasemi Falavarjani et al injected a single dose of MTX (250 µg) into 19 silicone oil filled eyes undergoing repair of a diabetic tractional or combined rhegmatogenous retinal detachment and 19 matched control eyes. The single injection of MTX did not reduce the rate of PVR-induced recurrent RD in this study.4
Here, we report our experience using MTX to treat a series of five consecutive eyes with severe PVR (Cp 6 or worse). All of these eyes required required membrane peeling, relaxing retinectomy and extended perfluorocarbon liquid (PFCL) tamponade. They were treated with a series of low-dose intravitreal injections of MTX (100–200 μg/0.05 mL) every 2 weeks for at least 10 weeks after the surgery. We hypothesised that the MTX injections would suppress the aberrant cellular proliferation of PVR.
Materials and methods
Patient and Public Statement: Patients were not directly involved in the design of the study.
We performed a retrospective chart review on a consecutive series of five patients with PVR who were treated with a series of of low-dose MTX injections following retinal reattachment surgery that included a relaxing retinectomy and extended PFCL tamponade. The severity of PVR was graded according to the classification of the Silicone Oil Study Group (1991).1 The institutional review board of University of Maryland at Baltimore reviewed our protocol and determined that this project met the definition of ‘not human subjects research’. Therefore, IRB oversight was not required. All of the patients were treated at the Retinal Consultants of Delmarva in Salisbury, Maryland, USA.
The surgical technique began with a standard 23-gauge pars plana vitrectomy. If there was pre-existing silicone oil, it was removed with a viscous fluid extractor. The retina was carefully inspected and all retina breaks were marked with an intraocular cautery. Any epiretinal membranes were peeled from the surface of the retina. Subretinal membranes were removed through an access retinotomy. If the retina could not be flattened with either air or PFCL, then a relaxing retinectomy was performed to relax the stiffened sections of the retina. The retinectomy was placed as anteriorly as possible. A small bubble of PFCL was placed over the macula to protect it from any migrating subretinal haemorrhage. A cautery was used to draw a line and to cauterise any retinal vessels. The relaxing cut was performed along this line with the vitreous cutter. At each end of the relaxing incision, the cut was redirected anteriorly to the ora serrata. The residual anterior retinal flap was excised. Additional PFCL was added to completely flatten the retina. PFCL was added until the bubble was at the level of the sclerotomies or just behind the plane of the iris. The goal was to achieve a bubble that filled 80% of the vitreous cavity. Continuous duration laser photocoagulation was then used to treat the cut edge of the retinectomy. The PFCL bubble was left in the eye for extended tamponade (4–5 weeks). The microcannulas were removed and sutures were placed as needed. Patients were asked to maintain either supine or upright positioning. Combination steroid and antibiotic eyedrops were administered 3–4 times per day.
MTX was sterilely prepared under a hood in sterile water by a compounding pharmacy at a concentration of either 200 µg/0.05 mL or 100 µg/0.05 mL. Patients 2–5 were given a MTX injection every 2 weeks for a total of five injections. The injections were started within 1 week after the last reattachment surgery (the one that included PFCL tamponade). MTX was injected using sterile technique into the vitreous cavity. The PFCL enters into the aqueous fluid around the bubble, not into the PFCL bubble (personal observation). The intravitreal injections were performed in the office with a standard technique that included the following: topical anaesthesia with lidocaine pledgets, a betadine prep, a lid speculum and no antibiotic drops.
The PFCL was removed when the laser scarring along the retinectomy was completely healed. This was determined in the following manner. Immediately after surgery, the entire laser scar was completely white, due to coagulation necrosis. As the healing progressed, the white colour transitioned into a pigmented scar and was considered fully healed. The process took 4–5 weeks to complete. The PFCL was aspirated through a silicone tip cannula as part of a standard three-port pars plana vitrectomy. A fluid/air exchange was performed to dislodge any residual Patient 1’s vision worsened from count fingers at 2 feet to hand motions. bubbles. At the end of the procedure the vitreous cavity was filled with either air or balanced salt solution.
Results
Tables 1 and 2 summarise our clinical data. Our patients were all Caucasian (three men and two women) ranging in age from 38 to 88 years old (mean=64 years) with severe PVR grade ranging from Cp 6 to Cp 12. They had undergone an average of 1.8 (range 0–3) previous retinal detachment surgeries. All of the patients had undergone previous cataract extraction with intraocular lens placement. Two patients (MTX 1 and 2) had a history of high myopia. Our index patient (MTX 1) was monocular, had a history of ROP, severe panuveitis due to Vogt-Koyanagi-Harada disease, had required three previous retinal detachment surgeries and an initial visual acuity of count finger at 2 feet. The preoperative visual acuity ranged from 20/200 to count fingers at 2 feet. All of the patients were followed for at least 6 months (mean=17.4 months; range 11–27 months).
Table 1.
Baseline patient demographics
| Masked ID | Age | Gender | Race | PVR grade at entry | Other ophthalmic diagnoses | Number of previous RD surgeries |
| MTX 1 | 38 | F | W | Cp 12 | VKH, ROP, previous laser to RT, lattice degeneration and TRD, high myopia, IOL, panuveitis | 3 |
| MTX 2 | 55 | M | W | Cp 12 | RD duration=12 months, high myopia, IOL | 0 |
| MTX 3 | 69 | M | W | Cp 9 | S/P repair MH, IOL, vitelliform dystrophy | 2 |
| MTX 4 | 88 | F | W | Cp 6 | IOL | 2 |
| MTX 5 | 70 | M | W | Cp 11 | IOL | 2 |
IOL, intraocular lens implant; MTX, methotrexate; ROP, Retinopathy of Prematurity; RT, retinal tear; TRD, tractional retinal detachment; VKH, Vogt-Koyanagi-Harada Disease.
Table 2.
Clinical results
| Masked ID | Initial visual acuity | 6-month visual acuity | 6-month IOP | MTX dosage | Number of MTX injections | PFCL duration (weeks) | Redetachment (Y/N) | Duration of follow-up (months) |
| MTX 1 | CF 2 feet | HM | 4 | 200 µg/0.05 mL | 12 | 5 | N | 27 |
| MTX 2 | HM | 20/200 | 12 | 200 µg/0.05 mL | 5 | 5 | N | 22 |
| MTX 3 | 20/400 | 20/400 | 14 | 100 µg/0.05 mL | 5 | 4 | N | 15 |
| MTX 4 | 20/200 | 20/60 | 10 | 100 µg/0.05 mL | 5 | 5 | N | 12 |
| MTX 5 | HM | 20/100 | 10 | 100 µg/0.05 mL | 5 | 4 | N | 11 |
IOP, intraocular pressure; MTX, methotrexate; PFCL, perfluorocarbon liquid.
The last four patients received five intravitreal MTX injections every 2 weeks, whereas the first patient (MTX 1) received 12 injections over an 18-week period. The first two patients were administered a dose of 200 ug/0.05 mL, whereas the last three patients (MTX 3–5) received a lower dose of 100 μg/0.05 mL.
All five eyes (100%) remained reattached with mean follow-up of 13.4 months (range 7–23 months). At 6 months, the visual acuity either improved or remained stable in patients 2–5 (range 20/400 to 20/60). Patient 1 (MTX 1) required reoperation due to dense macular pucker and her vision worsened from count fingers at 2 feet to hand motions.
The appearance of the laser scars in these five MTX-treated eyes was different than other eyes with PVR. All of the laser scars were flat without the usual fibrotic epiretinal or subretinal membrane formation along the retinectomy edges (figures 1–3). No pigmented or white epiretinal membranes (figure 4) were noted along the edge of the retinectomy in any of the five eyes treated with MTX.
Figure 1.

Fundus photograph of the left eye of patient 2 taken methotrexate 14 months after surgery. Note the well-healed laser scar along the 360° retinectomy. There are no fibrotic or pigmented epiretinal membranes along edge of the retinectomy. There is a macular pucker and a few intraretinal haemorrhages.
Figure 2.

Fundus photograph of the right eye of patient 3 taken methotrexate 6 months after surgery. This patient had a history of vitelliform dystrophy associated with foveal atrophy and was status-post macular hole repair. Note the well-healed laser scar along the retinectomy without evidence of proliferative vitreoretinopathy. There is focal fibroglial membrane along with inferior arcade without any significant traction.
Figure 3.

Fundus photograph of the right eye of patient 4 taken methotrexate 7 months after surgery. There is a well-healed laser scar along with the inferior retinectomy and without any fibrotic or pigmented epiretinal membranes.
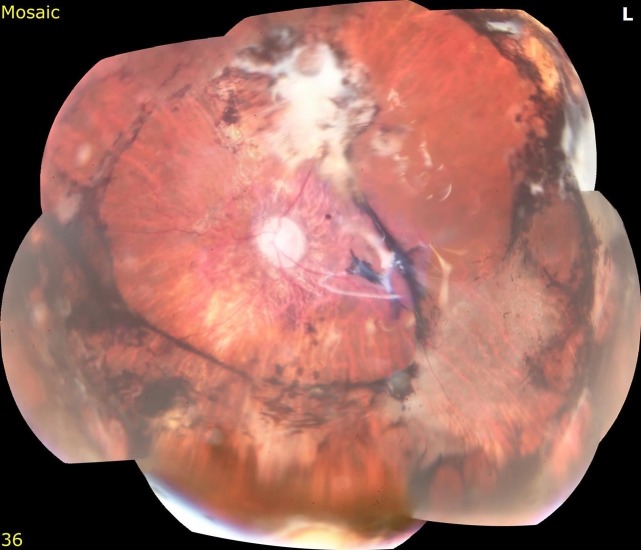
Figure 4.
Fundus photograph of a patient with proliferative vitreoretinopathy (not in this study) that is shown for illustrative purposes. This patient required multiple retinal surgeries and permanent silicone oil tamponade (did not receive intravitreal methotrexate or extended perfluorocarbon liquid tamponade). Note the thick pigmented and white fibrotic membranes (both subretinal and epiretinal) along the retinectomy edge and also extending through the macula. There is a tractional retinal detachment.
The use of PFCL for extended tamponade was well tolerated without any increased inflammation. The PFCL was removed at an average of 4.6 weeks postoperatively (range 4–5 weeks). There was no significant intraocular inflammation (<1+ by Standardization of Uveitis Nomenclature (SUN) grading) noted in eyes of patients 2–5. None of the eyes developed posterior synechiae or fibrin deposition in the anterior chamber. The initial patient had severe panuveitis from her VKH and was taking 60 mg of oral prednisone and prednisolone acetate drops every 2 hours—prior to staring the MTX injections. After starting the MTX injections, her inflammation rapidly controlled, which allowed both the oral prednisone and the prednisolone acetate drops to be tapered. Eventually, the oral prednisone was stopped.
The intravitreal MTX was found to be well tolerated. The only adverse effect noted was mild superficial punctate keratopathy (MTX 5). This resolved without any treatment after 2 weeks.
Hypotony was not seen in patients 2–4 of this series. The mean intraocular pressure (IOP) at 6 months was 10 mm Hg (range 4–14). Patient 1 remained hypotonous.
Discussion
The results of this small, retrospective, consecutive series suggest that low-dose MTX may be useful for treating complex retinal detachment with PVR. All five patients remained reattached (100%) with >6 months of follow-up. The final four eyes had reasonably good vision, normal IOP and non-fibrotic laser scars along the relaxing retinectomy. The combination of a series of five low-dose MTX injections and the use of extended PFCL was well tolerated without toxicity.
All five patients had severe PVR (average grade Cp 10) and remained reattached (100%) with more than 6 months of follow-up. There were no redetachments. These results are much better than the natural history of patients with recurrent retinal detachment due to PVR. The rate of anatomical reattachment following retinal reattachment surgery is only 60%–80%.5 All of our patients remained reattached and four out of five achieved a 6-month visual acuity better than 5/200 (range 20/60 to 20/400). Overall, the series of low-dose MTX injections appears to be effective in these eyes with severe PVR.
The appearance of the reattached retina of the MTX treated eyes was substantially different than that typically seen in other eyes with PVR. All of laser scars in the MTX-treated eyes (especially those along the retinectomy edge) were flat and well-healed (figures 1a–3a). None of the MTX-treated eyes had the thick fibrotic membranes (neither subretinal nor epiretinal) that are typically seen in cases of PVR (figure 4 is shown to illustrate this difference).
The MTX injections were well tolerated. The only untoward effect from the MTX was mild transient superficial punctate keratopathy that was observed in the fifth patient. This resolved spontaneously over a 2-week period. Elliot and Stryjewski also noted punctate keratopathy in 1 of their 10 patients.2 Punctate keratopathy is well known to occur in patients who are receiving frequent MTX injections for central nervous system lymphoma with intraocular involvement. These patients are required to receive a total course of 25 intravitreal injections of 400 µg of MTX over a 12month period.6
MTX is a folic acid antagonist that was derived from aminopterin, the first in class, chemotherapeutic drug used by Farber and associates to treat acute lymphoblastic leukaemia in 1947. At high doses, MTX inhibits DNA/RNA synthesis in rapidly dividing cells through the blockade of dihydrofolate reductase.7 At low doses, MTX works differently. It blocks both cellular proliferation and the inflammatory pathways by enhancing the release of extracellular adenosine, which inhibits macrophage activation, leucocyte recruitment, and neutrophil adhesion.7
Intravitreal MTX can be effective at a range of doses. We observed inhibition of PVR at doses of 100 µg and 200 µg of MTX. Elliot and Stryjewski were successful with a dose 400 µg of MTX. The same authors were also able to inhibit the cellular proliferation of PVR in vitro with concentrations of 100, 200 and 400 µg of MTX. The dosages of 100, 200 or 400 µg of MTX all appear to be effective—if administered for a long enough time.
The duration of treatment seems to be less forgiving. PVR has a prolonged time course and its cellular proliferative response needs to suppressed for at least 60–90 days. We administered our MTX injections over a 10-week period with good results. Elliot and Stryjewski were successful in suppressing the PVR in their patients with a 12-week course of MTX.2 Sadaka introduced the MTX via the infusion fluid flowing into the eye continuously during the retinal reattachment surgery.3 They achieved good results with inhibition of the PVR—without extended dosing. Perhaps the continuous flow of the MTX infusate may have loaded the retina and other intraocular tissues with MTX, creating a depot, which was slowly released over an extended time.
A single injection of MTX is inadequate to control a disease that lasts for 2–3 months.4 A series of intravitreal injections may be the most effective method of delivering MTX at the current time. Perhaps in the future, novel drug delivery systems may be able to reduce the treatment burden of biweekly MTX injections.
Extended tamponade (4–5 weeks) with PFCLs was used in our series. Figueroa and Casas reviewed the literature that described the use of PFCLs to provide short, medium and long duration tamponade (2–12 weeks) following retinal reattachment surgery. They concluded that ‘When used as a tamponade, PFCLs achieve excellent anatomical reattachment results, with a primary average success rate of 97%–100% under PFCLs and 63%–100% after PFCL removal. However, when PFCLs are used as a postoperative tamponade for more than 1 week, an inflammatory reaction develops in up to 30% of cases in clinical studies’.8 Intravitreal MTX (400 µg/0.1 mL) has been reported to reduce intraocular inflammation scores and uveitic cystoid macular oedema in patients with posterior uveitis.9 We hypothesise that the MTX injections suppressed the PFCL-induced inflammatory reaction. The inflammation was mild (<1+ by SUN grading) in patients 2–5 and it actually improved in patient 1.
In conclusion, this small, retrospective, consecutive series suggests that low-dose MTX injections may be beneficial for treating complex retinal detachment caused by PVR. The MTX also suppressed the inflammation normally associated with PFCL tamponade. Additional work is needed to determine whether MTX can help patients afflicted with PVR.
Footnotes
Contributors: JDB, MD* Retinal Consultants of Delmarva, Salisbury, MD, USA. JDB had the idea, planned the combined surgical and medical approach, did most of the surgeries, wrote the majority of the manuscript, tables, figure legends and references, and submitted the manuscript. DD, MD Department of Ophthalmology, University of Maryland School of Medicine, Baltimore, MD, USA. DD did a literature search, wrote and edited parts of the manuscript, figure legends and references, submitted and got approval to perform the study from the institutional review board of the University of Maryland at Baltimore. JWB, MD Retinal Consultants of Delmarva, Salisbury, MD, USA. JWB discussed and influenced many aspects of the combined surgical and medical approach, performed some of the surgeries and edited parts of the manuscript. KIH, COA Retinal Consultants of Delmarva, Salisbury, MD, USA. KIH compiled and extracted the data in HIPPA compliant manner, put it into a spreadsheet, took the montage fundus photos and OCTs.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Khan MA, Brady CJ, Kaiser RS. Clinical management of proliferative vitreoretinopathy. Retina 2015;35:165–75. 10.1097/IAE.0000000000000447 [DOI] [PubMed] [Google Scholar]
- 2. Eliott D, Stryjewski TP. Methotrexate for proliferative vitreoretinopathy. US Patent 2017. [Google Scholar]
- 3. Sadaka A, Sisk R, Osher J, et al. . Intravitreal methotrexate infusion for proliferative vitreoretinopathy. Clin. Ophthalmol 2016;10:1811–7. 10.2147/OPTH.S111893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ghasemi Falavarjani K, Modarres M, Hadavandkhani A, et al. . Intra-silicone oil injection of methotrexate at the end of vitrectomy for advanced proliferative diabetic retinopathy. Eye 2015;29:1199–203. 10.1038/eye.2015.114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Pastor JC, de la Rúa ER, Martín F. Proliferative vitreoretinopathy: risk factors and pathobiology. Prog Retin Eye Res 2002;21:127–44. 10.1016/S1350-9462(01)00023-4 [DOI] [PubMed] [Google Scholar]
- 6. Frenkel S, Hendler K, Siegal T, et al. . Intravitreal methotrexate for treating vitreoretinal lymphoma: 10 years of experience. Br J Ophthalmol 2008;92:383–8. 10.1136/bjo.2007.127928 [DOI] [PubMed] [Google Scholar]
- 7. Jolivet J, Cowan KH, Curt GA, et al. . The pharmacology and clinical use of methotrexate. N Engl J Med 1983;309:1094–104. 10.1056/NEJM198311033091805 [DOI] [PubMed] [Google Scholar]
- 8. Figueroa MS, Casas DR. Inflammation induced by perfluorocarbon liquid: intra- and postoperative use. Biomed Res Int 2014;907816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Taylor SRJ, Habot-Wilner Z, Pacheco P, et al. . Intraocular methotrexate in the treatment of uveitis and uveitic cystoid macular edema. Ophthalmology 2009;116:797–801. 10.1016/j.ophtha.2008.10.033 [DOI] [PubMed] [Google Scholar]