Abstract
Introduction
Kenya’s progress towards reducing maternal and neonatal deaths is at present ‘insufficient’. These deaths could be prevented if the three delays, that is, in deciding to seek healthcare (delay 1), in accessing formal healthcare (delay 2) and in receiving quality healthcare (delay 3), are comprehensively addressed. We designed a mobile phone enhanced 24 hours Uber-like transport navigation system coupled with personalised and interactive gestation-based text messages to address these delays. Our main objective was to evaluate the impact of this intervention on women’s adherence to recommended antenatal (ANC) and postnatal care (PNC) regimes and facility birth.
Methods
We conducted a prospective cohort study. Women were eligible to participate in the study if they were 15 years or older and less than 28 weeks gestation. We defined cases as those who received the standard of care plus the intervention and the control group as those who received the standard of care only. For analysis, we used logistic regression analysis and report crude and adjusted OR (aOR) and 95 % CI.
Results
Cases (women who received the intervention) had five times higher odds of having four or more ANC visits (aOR=4.7, 95% CI 3.20 to 7.09), three times higher odds of taking between 30 and 60 min to reach a health facility for delivery (aOR=3.14, 95% CI 2.37 to 4.15) and four times higher odds of undergoing at least four PNC visits (aOR=4.10, 95% CI 3.11 to 5.36).
Conclusion
An enhanced community-based Uber-like transport navigation system coupled with personalised and interactive gestation-based text messages significantly increased the utilisation of ANC and PNC services as well as shortened the time taken to reach an appropriate facility for delivery compared with standard care.
Keywords: health facility delivery, three delays model, Mhealth, Uber, health services accessibility
Key questions.
What is already known?
Maternal and neonatal deaths can be prevented through addressing the three delays (1): deciding to seek healthcare; (2) accessing formal healthcare and (3) receiving quality healthcare.
Mobile health interventions have been proposed as simple and effective solutions to improve maternal and neonatal health.
What are the new findings?
Timely reminders and information regarding health and transport services available via interactive text messages help women to remember, plan and stay motivated to seek appropriate maternal healthcare services in a timely manner.
An integrated community-based Uber-like transport system can address delay 2 by shortening the time to reach an appropriate facility for delivery.
What do the new findings imply?
The findings can be used to advocate for the integration of community-based Uber-like transport system within existing community maternal and newborn health programme.
Introduction
The Sustainable Development Goal 3 aims to reduce the global maternal mortality ratio (MMR) to less than 70 per 100 000 livebirths before 2030.1 Kenya’s progress towards reducing maternal and neonatal deaths is at present ‘insufficient’ as little progress has been made over the past decade.2 3 According to the WHO, Kenya is among the 10 countries that comprised 58% of the global maternal deaths in 2013, contributing 2% of these deaths.2 Given that the period of highest risk for both the mother and her fetus or neonate is around the time of delivery4; these deaths can be prevented if the three delays, that is, in deciding to seek healthcare (delay 1), in accessing formal healthcare (delay 2) and in receiving quality healthcare (delay 3), are comprehensively addressed.5 The Kenya government has focused on delay 3 and abolished user fees in all public health facilities6 with the aim of promoting health facility delivery service utilisation especially among vulnerable groups.7 There is, therefore, an urgent need to complement this efforts by addressing delay 1 and 2.
In Homa Bay County in western Kenya, the MMR is 583 per 100 000 live births and the leading factors contributing to this are poor access to and low utilisation of skilled birth attendance during pregnancy, childbirth and the postnatal period.3 Although over 90% of pregnant women attend at least one antenatal visit, only about 50% seek institutional deliveries and approximately 50% have access to institutional delivery services within a reasonable travel time. Only half of those women who deliver in a facility (24% of all deliveries) receive full postnatal check-ups before being discharged, which points to critical missed opportunities for assessment of the mother and newborn and the provision of counselling and support for maternal and newborn care practices.
With existing knowledge and technology, it is possible to prevent these maternal deaths. Mobile health (Mhealth) interventions have been proposed as effective solutions to improve maternal and neonatal health.8 The mAccess project was introduced in Homa Bay with an overall aim to contribute to a reduction in maternal and newborn mortality by developing a novel mobile phone-based tool with the following suites: (1) free short message service (SMS)-based service that sends personalised gestation-based text messages to mothers and reminders to utilise antenatal (ANC) and postnatal care (PNC) services; (2) interactive chat service that allows women to chat with a real-life healthcare worker and (3) 24 hours Uber-like transport navigator system, through which women can request transport pickup and the navigator service links her to the nearest, fastest, most reliable and available driver or rider. The system then automatically relays to the woman, the community health worker (CHW) and the link facility, the information about the estimated pickup time and arrival at the health facility.
The specific aims of the mAccess project were to evaluate the impact of this innovation on women’s health-related behavioural outcomes, including adherence to recommended ANC and PNC regimes, and skilled birth delivery. The central hypothesis was that timely reminders and information regarding health and transport services available via interactive text messages will help women to remember, plan and stay motivated to seek appropriate maternal healthcare services as well as provide them with information regarding their babies’ development while pregnant.
Methods
Theoretical framework
The ‘three delays’ model developed by Thaddeus and Maine9 provides a suitable framework for understanding the causes of maternal deaths. These are1 delay in recognising danger signs/decision to seek care,2 delays in reaching a medical facility and3 delay in receiving appropriate care once a facility is reached. We adopted the ‘three delays’ model as a framework to identify the barriers to obstetric care and assess whether a mobile phone-enhanced community-based maternal newborn health intervention that addressed delays 1 and 2 can help women to overcome these barriers. The ‘three delays’ model allows for an objective way to examine the complex interactions that may occur between women’s ability to make decisions to attend antenatal services, choose facility-based delivery services, recognise danger signs, travel to the health facility and ultimately receive quality care at the health facility during pregnancy and childbirth. This model has been applied previously in analyses of newborn death in several countries, including Tanzania and Uganda.10 11
Study design
We conducted a prospective cohort study utilising quantitative methods.
Study setting and participants
The study was done in East Rachuonyo within Homa Bay County, which is located in rural western Kenya beginning from May 2016 to March 2018. Homa Bay County has one of the highest maternal and neonatal mortality rates in the country. Homa Bay’s MMR is estimated at 583, compared with the national average of 488 and Kenya’s least-deprived counties that have rates below 200. East Rachuonyo was selected as it was implementing community maternal newborn health (CMNH) in which CHWs conduct home visits during pregnancy and the postpartum. CHWs in Kenya are unsalaried male and female persons, over the age of 18 years and with at least primary level education. CHWs are selected by local community members and then trained over a period of 6 weeks in basic modules on promotion of maternal, newborn and child health, prevention of preventable diseases, promotion of healthy lifestyle, prevention of injuries and accidents, community support for vulnerable people and addressing sexual-based and gender-based violence.12 CHWs work from community health units, which serve a population of 5000 people. Each community unit is linked to one health facility. One community unit has 6–16 CHWs, with each CHW responsible for approximately 500 people.13 14 Quarterly community dialogue days are in the community units to discuss on the performance of selected indicators and come up with an action plan. CHWs conduct two antenatal home visits at 12–16 and 32–34 weeks to promote birth and newborn care preparedness.15 They also conduct postnatal home visits on day 1, 3 and 7 to reinforce birth and newborn care and provide counselling for breastfeeding difficulties.15 The record of each home visit is entered longitudinally into a WHO-adapted CMNH register. Women registered in this CMNH register comprised the sampling frame for this study.
Eligibility and recruitment
Women were eligible to participate in the study if they were 15 years or older, less than or equal to 28 weeks gestation, planning to remain in the study area (up to 6 weeks postpartum), had access to a mobile phone and reported ability to read or had someone who could read SMS on their behalf.
The recruitment of participant started in the community when CHWs identified eligible women during their routine home visits. All women were enrolled into the CMNH register The CHWs briefly described the study and invited women to receive additional information at the respective Ministry of Health antenatal clinic. At the clinics, eligible women’s phone numbers and SMS preferences were recorded by sending a text message from their phone. This message included date of last normal menstrual period, preferred language (English, Kiswahili or Dholuo), preferred time for receiving SMS and preferred name. This text registered them within the mAccess platform. Participants were followed up to 6 weeks postpartum.
Sampling and intervention allocation
The sampling frame was all pregnant women living in East Rachuonyo during the study period and registered by the CHWs in the CMNH register. Cases were selected using convenience sampling into the study until the sample size was met. To avoid clustering of intervention participants in one region, each location within East Rachuonyo was allocated a weighted number of intervention participants to enrol based on its population density. We defined cases as those who received the standard of care that is, CMNH plus the mAccess intervention and the control group as those who received the standard of care only.
Intervention description
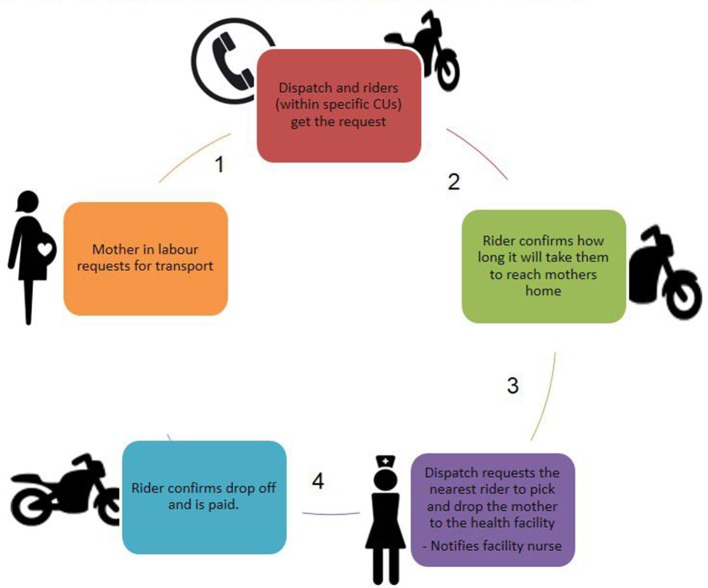
The core of mAccess is a two-way SMS messaging system that coordinates the sending of messages between a pregnant woman and staff. To start, a CHW uses a mobile survey to enrol a woman into the mAccess system during one of her monthly visits, specifying the woman’s estimated gestation. After enrolment, the woman automatically receives weekly messages describing what she can expect during her specific week of pregnancy. Participants received messages updating them how the baby was developing, how their bodies were responding, the different danger signs, need to identify a health facility and/or skilled birth attendant and birth partner of choice, and how to save money and prepare for the birth. After each message, the woman is prompted to ask questions from a live nurse. If she chooses this option, a live nurse is contacted and continues to follow-up with the woman through SMS text messaging until the woman’s questions are resolved. This is known as m-convo. Women participating in m-convo were eligible to receive National Health Insurance Fund (NHIF) yearly premiums, transport to the hospital and mother–baby care packs. M-convo also ensured that women had an interaction with the system and build-up trust in the system before they actually needed a service. The woman is also able to SMS the word ‘mHelp’ to ‘call for help’ if she has questions, feels ill or is in labour. In the case of illness or labour, a central dispatch sends an SMS survey to all trained motorcycle riders in the woman’s area asking a series of questions about their location and availability. Once a rider has been identified and is on his way, dispatch sends an SMS to the woman reassuring her that transport is on the way and to the woman’s preferred health facility notifying them to prepare for her arrival. This transport system is doubly innovative in that as it is not like the regular ‘Uber’ as it is firmly embedded within the national community health strategy. In the same way, CHWs are vetted for selection, the riders apply to the community health committee in charge of community units and undergo a vetting exercise after which they are trained on the importance of a quick response. Transport fares are agreed on on a community level and each community unit has 2–3 motorcycle riders. The riders are, thus, people that the community know and have vetted. Figure 1 summarises the process.
Figure 1.
Twenty-four-hour transport navigation system (Uber redefined).
Patient and public involvement statement
The development and implementation of the mAccess project and research questions was done collaboratively, involving the target population of pregnant and postpartum women, and private and public stakeholders (including mobile phone operators, the Homa Bay transport owners association, national and county health management teams, county communication and transport team, and the Homa Bay NHIF office). The project was in direct response to an existing gap in CMNH in the county. Prior to launching the mAccess project, the investigators on this project had worked with the local community members and the county health management team and launched a mobile phone-enhanced integrated community case management (iCCM) of pneumonia, malaria, diarrhoea and vitamin A supplementation in children aged 2–59 months in Homa Bay County.16 The team trained ~90 County and subcounty healthcare workers to be trainers of trainers in iCCM and CMNH, and further trained a total of 2604 CHWs and 251 community health extension workers in 245 community units across eight subcounties ensuring 100% coverage of the county with essential community child-based interventions.17 Unfortunately, pregnant and postpartum women were not covered by these services and there was a need to address this population while leveraging the existing structures that had been set up. The mAccess project was designed to use this existing framework of mobile phone-enhanced community-based health services and address a community-identified need. The team leveraged the existing CHWs to recruit participants. While participants were not involved in recruitment, they participated in the quarterly community dialogue meetings in which progress on CMNH was discussed and motorcycle vendors vetted and issues raised. Preliminary lay results, including video documentation, were presented to the county health management team as well as to each of the participating community units in which women came from. Final results will be provided to all stakeholders including participants involved in the study.
Sample size
Sample size was estimated based on the assumption that at baseline about 60.4% of women are delivered by a skilled birth attendant18 and hypothesised a 10% increase in the number of women delivered by a skilled birth attendant as a result of mAccess implementation. Using this difference in proportions, uncorrected χ2 test and 80% power to detect a statistically significant difference at 5% significance level, the estimated required sample size was 353 each in control and intervention arm.
Statistical analysis
Frequencies with percentages were used to summarise categorical variables. Means and medians reporting the respective SDs and IQR were used to summarise continuous variables. Logistic regression analysis was used to assess whether mAccess intervention had any impact on cost of transport, time to delivery, number of ANC visits, PNC visits visits and adverse pregnancy outcomes, and control for the effect of confounding variables. A crude OR and 95% CI was determined for each of the outcomes. For all the adjusted analysis, we controlled for age and education level of women, which are known determinants of maternal healthcare seeking.19 Scrutiny of our data revealed that the missing values were randomly distributed across all observations. On the basis of the missing data pattern and critical peer-review of similar data, we assumed that the missing data did not depend on the unobserved data and were missing completely at random. Subsequently, we partitioned the data into two parts, one set containing the missing values and the other containing the non-missing values. A t-test of mean difference was carried out to test whether there existed any difference in the sample between the two data sets. The missing data did not bias the OR implying that the estimated parameters are not biassed by the absenteeism of the data. All analyses were done using STATA V.13.
Variables
The exposure variable of interest was receipt of the mAccess intervention.
The main outcome variables were cost of transport to place of delivery (measured in Kenyan Shillings), time taken to reach facility for delivery (measured in minutes and hours from the time the woman or birth partner makes a call for transport), number of ANC visits, number of PNC visits, pregnancy outcomes (defined as either miscarriage, stillbirth and live) and status of mother after birth (alive, dead and unknown). Potential confounders considered included age and education level of women.
Data sources
Data were derived from the CMNH registers that were compiled by CHWs during the routine implementation of CMNH service delivery. Study nurses abstracted the data collected and entered it into password-protected computers.
Results
Demographic characteristics
Of the total cohort of 1179 pregnant women, 350 women received the intervention and were all followed-up to 6 weeks post partum. Over 50% of the pregnant women enrolled in this study, for both cases and controls, were 15–24 years of age, and over 60% had attained primary education (controls 67.28%, n=549 and cases 61.32%, n=214). The mean age (SDs) of mothers were similar between controls and cases 24.7 (5.8) and 24.9, (5.5) respectively (Table 1).
Table 1.
Sociodemographic characteristics of cases and controls
| Characteristic | Controls n (%) n=817 | Cases n (%) n=349 |
| Mothers age group (years) | ||
| 15–24 | 463 (56.67) | 190 (54.44) |
| 25–34 | 307 (37.58) | 131 (37.54) |
| 35–45 | 47 (5.75) | 28 (8.02) |
| Mean age (SD) | 24.7 (5.8) | 24.9 (5.5) |
| Mothers education level | ||
| Primary | 549 (67.28) | 214 (61.32) |
| Secondary | 247 (30.27) | 111 (31.81) |
| College | 20 (2.45) | 24 (6.88) |
Multivariate analysis
As presented in table 2, cases (women who received the intervention) were five times higher odds of having four or more ANC visits (adjusted OR (aOR)=4.7, 95% CI 3.20 to 7.09), three times higher odds of taking between 30 and 60 min to reach a health facility for delivery (aOR=3.14, 95% CI 2.37 to 4.15) and four times higher odds of undergoing at least four PNC visits (aOR=4.10, 95% CI 3.11 to 5.36). Chances of a pregnant woman having a miscarriage or stillbirth (aOR 2.03, 95% CI 0.83 to 4.95) were not statistically related to being a case or control.
Table 2.
Health behavioural outcomes
| Maternal outcome | Controls (n=826) | Cases (n=350) | OR (95% CI) | aOR (95% CI) |
| No. of ANC visits | ||||
| Less than four ANC visits | 267 (32.32) | 31 (8.86) | Reference | Reference |
| At least four ANC visits | 559 (67.68) | 319 (91.14) | 4.92 (3.31 to 7.31) | 4.8 (3.20 to 7.09) |
| Time taken to reach facility for delivery | ||||
| Less than 30 min | 484 (64.79) | 129 (36.86) | Reference | Reference |
| 30–60 min | 213 (28.51) | 179 (51.14) | 3.15 (2.39 to 4.16) | 3.14 (2.37 to 4.15) |
| 1 hour and above | 50 (6.69) | 42 (12.00) | 3.15 (2.00 to 4.96) | 3.10 (1.95 to 4.90) |
| Adverse pregnancy outcomes | ||||
| Live birth | 784 (98.00) | 341 (97.43) | Reference | Reference |
| Miscarriage/stillbirth | 16 (2.0) | 9 (2.57) | 1.30 (0.57 to 2.96) | 1.97 (0.81 to 4.81) |
| No. of PNC visits | ||||
| Less than four PNC visits | 542 (69.40) | 120 (35.40) | Reference | Reference |
| At least four PNC visits | 239 (30.60) | 219 (64.60) | 4.14 (3.16 to 5.42) | 4.10 (3.11 to 5.36) |
| Status of mother after birth | ||||
| Alive | 790 (99.50) | 348 (99.71) | Reference | Reference |
| Dead | 4 (0.50) | 1 (0.29) | 0.57 (0.06 to 5.20) | 0.61 (0.07 to 5.45) |
aOR, adjusted OR;ANC, antenatal care; PNC, postnatal care.
Women who received the mAccess intervention had significantly higher odds of using a motorcycle during ANC clinic visits (aOR 58.3, 95% CI 23.75 to 143.26) and during the time of delivery (aOR 14.84, 95% CI 5.30 to 41.6) compared with the controls. They also had lower odds of walking to their ANC clinic (aOR 0.02, 95% CI 0.007 to 0.05) or using car taxis during their time of delivery (aOR 0.09, 95% CI 0.03 to 0.26) (Table 2).
Discussion
In this community-based prospective cohort study, we demonstrated that a mobile phone-enhanced 24 hours Uber-like transport navigation system coupled with personalised and interactive gestation-based text messages improved both antenatal and postnatal clinic attendance, and shortened the time taken to reach an appropriate facility for delivery when compared with standard care. This study is among the first Mhealth interventions to successfully demonstrate an integrated Mhealth application addressing both delays 1 and 2 to improve maternal and newborn health service access and utilisation in rural communities.
Participants in the intervention arm were five times more likely to attend more than four ANC visits during the pregnancy and four PNC visits compared with their counterparts in the control arm. The study used gestation-based text messages bidirectional text conversations (m-convo) to convey information to women and support them in decision-making and clearing of myths and misconceptions; thus, addressing delay 1. The delay in seeking healthcare is often attributed to the lack of knowledge of the gravity of the sickness.20 The gestation-based text messages that sent to the women were packed with information regarding danger signs in pregnancy, information as regards to the development of the fetus, what to expect during clinic appointments and general care during pregnancy and delivery. Our m-convo system also allowed the women to request to chat with a healthcare provider in real time. Pregnancy, by its very nature, can be overwhelming and life-changing, demanding change from women physically, emotionally, psychologically and socially.21 The ability of women in mAccess to chat with a healthcare worker in real time did not only help to provide information to assist the women in making decisions to seek care but it also provided the much needed psychological and social support during pregnancy that most women desire. The efficaciousness of the personalised text messages and interactive chats can be attributed to the fact that they allowed for women fill in the gaps in information by healthcare providers and to ask sensitive questions that they were shy to ask in person. Use of text messages reminders has been documented as an effective media to improve uptake in various health interventions especially among pregnant women.22 A study conducted in Malawi showed that the use of text messages led to early ANC attendance among pregnant women, which was vital for malaria prevention.23 A meta-analysis conducted by Guy et al 24 concluded that text messages reminders in healthcare settings substantially increased the likelihood of attending clinic appointments and that SMS reminders appeared to be a simple and efficient option for health services to use to improve service delivery, as well as resulting in health benefits for the patients who receive the reminders.24 Lastly, several studies have also found that bidirectional messages and chats are often more efficacious than generic interventions.25 26
Women receiving the intervention were three times more likely to take between 30 and 60 min to reach a health facility for delivery. This was made possible by our transport navigation system, which ensured that the women could request for transport and the motorbike riders would be available to take them to the hospital at all times regardless of the weather or terrain.27 According to the literature, pregnant women in resource-poor settings delay to reach the health facilities due to the long distance that they have to travel,9 lack of available transport especially at night and when the weather is not conducive, and lack money to pay for the transport.20 The inability of a pregnant woman to access a health facility in times of an emergency has been shown to be a major contributor to maternal mortalities in Kenya. A study conducted in Mozambique to analyse the major contributors to maternal mortality showed that delay 2 (access to healthcare) contributed to 40.4% of maternal mortality.28 Our transport navigation system did not only contribute to the availability of transport but also reduced the amount of time to reach the facilities. This is in keeping with other studies in Malawi and Burundi, which have experimented with using motorcycle ambulances and referral networks. In Malawi, where motorcycle ambulances were stationed in rural health facilities, referral time was reduced by between 35% and 76% and ranged from 78 min to 5 hours referral times.29 Similarly in Burundi, the median referral time (time from maternity calling for an ambulance to the time the patient arrived at the referral facility) was 78 min (IQR 52–130 min).30 Our findings indicate that averagely about 64% of our participants took 30 min from the time they requested for transport to the time they arrived at the clinic represents a significant decrease in this referral time. This is likely because our motorcycles were already stationed in communities where women resided and did not have to make round trips. Our initiative, therefore, is an improvement on both models in Burundi and Rwanda.
The inherent limitation of this study was that selection for women was not random. It is probable that owing to the non-probability sampling that selection bias in this study might have happened at the point of entry into the study when selecting into intervention and non-intervention cohorts resulting in non-differential misclassification of the exposure. Because misclassification of the exposure allocation is likely generally the same irrespective of the outcome, our findings on average are likely to be an underestimate of the true association. While it was not possible to control for all potential confounding factors, any residual confounding is unlikely owing to the fact that the population of East Rachuonyo was small enough to be homogenous.31 In addition, due to the subjective nature in choosing the sample, the selected women may not be a good representation of the population, which limits the generalisability of the intervention. Our study did not find any differences in adverse pregnancy outcomes between cases and controls. These null findings are likely due to the fact that the study was not primarily powered to detect these differences. Given the importance of adverse pregnancy outcomes, future research including scale-up of mAccess should prioritise these outcomes during sample calculation. Another limitation was that we only used quantitative methods in this paper. While quantitative methods are effective in measuring changes over time, they are less effective in providing a deep understanding of the processes and how those changes actually occur. Narratives from in-depth interviews conducted with women using the intervention and navigating pregnancy and delivery are reported in a separate publication.27 A mixed methods approach allowing triangulation of qualitative and quantitative findings including cost-effectiveness would have provided a deeper understanding of the implementation process and its outcomes. While we did not conduct cost-effectiveness studies, studies from similar low-resource settings have shown that ambulance referral networks that also included motorcycles were more cost-effective and had more utility than traditional motor-vehicle networks.30 In our study, the local transport vendors owned the motorcycles and transport prices were negotiated at the community level during quarterly community dialogue meetings. We, therefore, strongly believe that the intervention can be cost-effective and self-sustainable if the existing community health strategy intentionally incorporates local motorcycle riders within their structure.
Conclusion
We demonstrated that delays 1 and 2 could be addressed by a mobile phone-enhanced 24 hours transport navigation system coupled with personalised and interactive gestation-based text messages. Most people in rural Kenya and other parts of low-resource countries now own mobile phones; therefore, application of innovations, such as mAccess, could be a key pillar in the integration of technology to reduce perinatal morbidity and mortality. Moreover, intentionally involving other members of the community, such as local transport vendors, in supporting healthcare in the communities can address delay 2. When viewed as a whole, the findings speak to the fact that reducing perinatal morbidity and mortality must have an integrated approach that addresses all delays simultaneously. Novel integrated local solutions, such as mAccess, can be critical in increasing the utility of maternal and newborn health services with the ultimate goal of reducing maternal and neonatal morbidity and mortality.
Acknowledgments
We thank the Kenyan mothers, fathers and their children, the Homa Bay motorcycle vendors and the community health workers who participated in this study. We recognise M-survey for developing the platform. We acknowledge the technical support of the Kenya Ministry of Health Neonatal, Child and Adolescent Health Unit, the County Health Management Team of Homa Bay County, members of the Kenya Community Maternal Newborn Health Technical Working Group and the Director of the Kenya Medical Research Institute.
Footnotes
Handling editor: Seye Abimbola
Contributors: MAOn designed the intervention, oversaw its implementation, evaluation, data collection and analysis, drafted the first manuscript draft, reviewed subsequent drafts, provided final approval of the version to be published and agrees to be accountable for all aspects of the work. SW was the lead statistical analyst, contributed to the writing of the initial manuscript, revising subsequent drafts, provided final approval of the version to be published and agrees to be accountable for all aspects of the work. PW, CKA, LWW, TS, MAOw and PO contributed to the implementation and collection of data, critical revision of the drafted manuscript, provided final approval of the version to be published and agree to be accountable for all aspects of the work.
Funding: We received financial support from the United Kingdom Department for International Development (DFID) funded County Innovation Challenge Fund.
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: The ethical review committee at AMREF Health Africa approved the study.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available on reasonable request.
References
- 1. Chavane LA, Bailey P, Loquiha O, et al. . Maternal death and delays in accessing emergency obstetric care in Mozambique. BMC Pregnancy Childbirth 2018;18 10.1186/s12884-018-1699-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. World Health Organisation Trends in Maternal Mortality: 1990-2013. Estimates by WHO, UNICEF, UNFPA, The World Bank and the United Nations Population Division. Geneva: World Health Organisation, 2014. [Google Scholar]
- 3. National Council for Population and Development Reducing maternal deaths in Kenya. Nairobi, Kenya: National Council for Population and Development, 2015. [Google Scholar]
- 4. Saleem S, McClure EM, Goudar SS, et al. . A prospective study of maternal, fetal and neonatal deaths in low- and middle-income countries. Bull World Health Organ 2014;92:605–12. 10.2471/BLT.13.127464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mwaniki MK, Baya EJ, Mwangi-Powell F, et al. . ‘Tweaking’ the model for understanding and preventing maternal and neonatal morbidity and mortality in Low Income Countries: “inserting new ideas into a timeless wine skin”. BMC Pregnancy and Childbirth 2016;16 10.1186/s12884-016-0803-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. The presidency Speech by H.E. Hon. Uhuru Kenyatta, C.G.H, president and Commander-in-Chief of the defence forces of the Republic of Kenya during the Madaraka Day celebrations (Nyayo national stadium, June 1,2013). Nairobi: Nation Media group; 2013. [Google Scholar]
- 7. McKinnon B, Harper S, Kaufman JS, et al. . Removing user fees for facility-based delivery services: a difference-in-differences evaluation from ten sub-Saharan African countries. Health Policy Plan 2015;30:432–41. 10.1093/heapol/czu027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sondaal SFV, Browne JL, Amoakoh-Coleman M, et al. . Assessing the effect of mHealth interventions in improving maternal and neonatal care in low- and middle-income countries: a systematic review. Plos One 2016;11:e0154664 10.1371/journal.pone.0154664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Thaddeus S, Maine D. Too far to walk: Maternal mortality in context. Soc Sci Med 1994;38:1091–110. 10.1016/0277-9536(94)90226-7 [DOI] [PubMed] [Google Scholar]
- 10. Waiswa P, Kallander K, Peterson S, et al. . Using the three delays model to understand why newborn babies die in eastern Uganda. Tropical Medicine International Health 2010;15:964–72. 10.1111/j.1365-3156.2010.02557.x [DOI] [PubMed] [Google Scholar]
- 11. Mbaruku G, van Roosmalen J, Kimondo I, et al. . Perinatal audit using the 3-delays model in Western Tanzania. International Journal of Gynecology & Obstetrics 2009;106:85–8. 10.1016/j.ijgo.2009.04.008 [DOI] [PubMed] [Google Scholar]
- 12. MoPHa S, Volunteers CH. CHVs) basic modules Handbook. Nairobi, Kenya: Ministry of Public Health and Sanitation, 2013. [Google Scholar]
- 13. Ministry of Health K Taking the Kenya essential package for health to the community: a strategy for the delivery of level one services. Nairobi, Kenya: Ministry of Health, 2006. [Google Scholar]
- 14. Ministry of Health K Community strategy implementation guidelines for managers of the Kenya essential package for health at the community level. Nairobi, Kenya: Ministry of Health, 2007. [Google Scholar]
- 15. Ministry of Health K Caring for the newborn at home: A training course for community health workers. Nairobi, Kenya: Ministry of Public Health and Sanitation, 2011: 70. [Google Scholar]
- 16. Onono M, Abdi M, Mutai K, et al. . Community case management of lower chest indrawing pneumonia with oral amoxicillin in children in Kenya. Acta Paediatrica 2018;107(5 Suppl):44–52. 10.1111/apa.14405 [DOI] [PubMed] [Google Scholar]
- 17. Onono M, Abdi M, Opondo I, et al. . Using the RE-AIM framework to evaluate the implementation of integrated community case management in Kenya. Acta Paediatrica 2018;107(Suppl 3):53–62. 10.1111/apa.14662 [DOI] [PubMed] [Google Scholar]
- 18. Kenya National Bureau of Statistics KMoH Kenyan national AIDS control Council, Kenya medical research Institute, Kenyan national Council for population and development, the DHS program, ICF international. Kenya Demographic and Health Survey 2014. ICF International, 2015. [Google Scholar]
- 19. Moyer CA, Mustafa A. Drivers and deterrents of facility delivery in sub-Saharan Africa: a systematic review. Reprod Health 2013;10 10.1186/1742-4755-10-40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Killewo J, Anwar I, Bashir I, et al. . Perceived delay in healthcare-seeking for episodes of serious illness and its implications for safe motherhood interventions in rural Bangladesh. Journal of health, population, and nutrition 2006;24:403–12. [PMC free article] [PubMed] [Google Scholar]
- 21. Reblin M, Uchino BN. Social and emotional support and its implication for health. Current Opinion in Psychiatry 2008;21:201–5. 10.1097/YCO.0b013e3282f3ad89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Cole-Lewis H, Kershaw T. Text messaging as a tool for behavior change in disease prevention and management. Epidemiologic Reviews 2010;32:56–69. 10.1093/epirev/mxq004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Nkoka O, Chuang T-W, Chen Y-H. Association between timing and number of antenatal care visits on uptake of intermittent preventive treatment for malaria during pregnancy among Malawian women. Malaria Journal 2018;17 10.1186/s12936-018-2360-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Guy R, Hocking J, Wand H, et al. . How effective are short message service reminders at increasing clinic attendance? A meta-analysis and systematic review. Health Serv Res 2012;47:614–32. 10.1111/j.1475-6773.2011.01342.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kreuter MW, Caburnay CA, Chen JJ, et al. . Effectiveness of individually tailored calendars in promoting childhood immunization in urban public health centers. American Journal of Public Health 2004;94:122–7. 10.2105/AJPH.94.1.122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Odeny TA, Bukusi EA, Cohen CR, et al. . Texting improves testing: a randomized trial of two-way SMS to increase postpartum prevention of mother-to-child transmission retention and infant HIV testing. AIDS 2014;28:2307–12. 10.1097/QAD.0000000000000409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Onono M, Odhiambo G, Congo O. Narratives of women in rural Kenya using a 24-hour ride-hailing transport system to increase access and utilization of maternal and newborn health services in Homa Bay: a qualitative study. American Journal of Tropical Medicine and Hygiene. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Chavane LA, Bailey P, Loquiha O, et al. . Maternal death and delays in accessing emergency obstetric care in Mozambique. BMC Pregnancy and Childbirth 2018;18 10.1186/s12884-018-1699-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hofman JJ, Dzimadzi C, Lungu K, et al. . Motorcycle ambulances for referral of obstetric emergencies in rural Malawi: do they reduce delay and what do they cost? International Journal of Gynecology & Obstetrics 2008;102:191–7. 10.1016/j.ijgo.2008.04.001 [DOI] [PubMed] [Google Scholar]
- 30. Tayler-Smith K, Zachariah R, Manzi M, et al. . An ambulance referral network improves access to emergency obstetric and neonatal care in a district of rural Burundi with high maternal mortality. Trop Med Int Health 2013;18:993–1001. 10.1111/tmi.12121 [DOI] [PubMed] [Google Scholar]
- 31. Etikan I, Ilker Etikan SAM, Alkassim RS. Comparison of convenience sampling and Purposive sampling. American Journal of Theoretical and Applied Statistics 2016;5:1–4. 10.11648/j.ajtas.20160501.11 [DOI] [Google Scholar]