Abstract
Background/Aims
18F-fluorodeoxyglucose-positron emission tomography (18F-FDG-PET) reflects biological aggressiveness and predicts prognoses in various tumors. Evaluating the oncologic significance of the preoperative metabolic phenotype might be necessary for planning the surgical strategy in resectable pancreatic cancers.
Methods
From January 2010 to December 2015, a total of 93 patients with pathologic T3 (pT3) pancreatic cancer were included in this study. Clinicopathological parameters and PET parameters were evaluated, and transcriptome-wide analysis was performed to identify the oncologic impact and molecular landscape of the metabolic phenotype of resectable pancreatic cancers.
Results
Preoperative metabolic tumor volume (MTV)2.5 was significantly higher in the pN1 group compared to the pN0 group (11.1±11.2 vs 6.5±7.8, p=0.031). Higher MTV2.5 values (MTV2.5 ≥4.5) were associated with multiple lymph node metastasis (p=0.003), and the lymph node ratio was also significantly higher in resected pT3 pancreatic cancer with MTV2.5 ≥4.5 compared to those with MTV2.5 <4.5 (0.12±0.13 vs 0.05±0.08, p=0.001). Disease-specific survival of patients with MTV2.5 <4.5 was better than that of patients with MTV2.5 ≥4.5 (mean, 28.8 months; 95% confidence interval [CI], 40.1 to 57.0 vs mean, 32.6 months; 95% CI, 25.5 to 39.7; p=0.026). Patients with MTV2.5 ≥4.5 who received postoperative adjuvant chemotherapy showed better survival outcomes than patients with MTV2.5 ≥4.5 who did not receive adjuvant treatment in resected pT3 pancreatic cancers (p<0.001). Transcriptome-wide analysis revealed that tumors with MTV2.5 ≥4.5 demonstrated significantly different expression of cancer-related genes reflecting aggressive tumor biology.
Conclusions
Resectable pancreatic cancer with high MTV2.5 is not only associated with lymph node metastasis but also early systemic metastasis. The molecular background of resectable pancreatic cancer with high MTV2.5 may be associated with aggressive biologic behavior, which might need to be considered when managing resectable pancreatic cancers. Further study is mandatory.
Keywords: Pancreatic neoplasms, Positron-emission tomography, Metabolic phenotype, Transcriptome-wide analysis
INTRODUCTION
In the early 1920s, Otto Warburg reported that cancer cells preferentially metabolize glucose by “aerobic glycolysis,” even in the presence of ample oxygen.1 The increased glucose demand has been considered one of the fundamental features of cancer and has become the foundation of the clinical application of 18F-fluorodeoxyglucose-positron emission tomography (18F-FDG-PET) in oncology.2 Cancer cells show an increased uptake of glucose and FDG.2 Both glucose and FDG are phosphorylated by hexokinase (HK) to prevent their release from cancer cells. In contrast to glucose, FDG cannot be further metabolized due to the lack of the 2′-OH group, resulting in its accumulation in cells proportional to the amount of uptake and HK activity.3 FDG-PET has emerged as an important clinical tool for cancer detection and staging and the monitoring of the response of cancer to therapy.4 However, there are some important critiques of the routine use of FDG-PET in clinical oncology. It has been observed that FDG-PET is not more effective than conventional imaging technology at detecting early pancreatic cancer and small metastatic lesions.5 In addition, FDG-PET is not able to discriminate the oncologic process of pancreatic cancer from inflammatory focal lesions including mass-forming pancreatitis.6
However, with the clinical experiences of using FDG-PET in patients with pancreatic cancer, recent studies have suggested that the characteristics of preoperative FDG-PET images are strongly associated with aspects of tumor biology,7 such as the pathological grade,8 recurrence,9 distant metastasis,10 and long-term oncologic outcomes.11 Several parameters for FDG-PET are being developed to measure the metabolism of cancer lesions and to predict aspects of tumor biology and the resultant oncologic outcomes. Unlike the maximum standard uptake value (SUVmax), which reflects the metabolic activity of a single pixel, the metabolic tumor volume (MTV) and total lesion glycolysis (TLG) can measure the volume-based metabolic activity of the entire tumor lesion.11 In our previous study, the results of the propensity score-matched analysis demonstrated that preoperative MTV2.5 greater than 4.5 can predict tumor recurrence and long-term survival in patients with resected pancreatic cancer.12 In addition, it was shown that high FDG uptake in left-sided pancreatic cancer is strongly associated with loss of SMAD4, subsequently resulting in early systemic metastasis.13 From the viewpoint of the American Joint Committee on Cancer (AJCC) 7th cancer staging system, pathologic T3 (pT3) lesions are the most common type of resected pancreatic cancer, regardless of the tumor size.14 Therefore, small proportions of T1 and T2 are potential confounding factors in the analysis of the oncologic impact of PET/computed tomography (CT)-related parameters in patients with resected pancreatic cancer.
In this study, we focused on patients who underwent potentially curative pancreatectomy for pT3 pancreatic cancer without neoadjuvant treatment. We determined the value of MTV2.5 in predicting the oncologic outcome of resected pancreatic cancer, and investigated the differences in gene expression in patients with pT3 pancreatic cancer to explain the different oncologic outcomes according to the value of MTV2.5. This approach may be a basis for a patient-oriented surgical approach to the treatment of resectable pancreatic cancer in the near future.
MATERIALS AND METHODS
1. Study period and population
From January 2010 to December 2015, 232 patients underwent potentially curative pancreatectomy for pancreatic cancers in Yonsei University Severance Hospital, Seoul, Korea. Of those 232 patients, 93 patients with pT3 pancreatic cancer (AJCC 7th) without neoadjuvant treatment who had undergone preoperative PET/CT imaging were included in this investigation. This study protocol was approved by the Institutional Review Board of Severance Hospital with the waiver of informed consent due to retrospective study (IRB number: 4-2017-0657).
2. Clinicopathological parameters
We retrospectively reviewed the medical records of the patients, and collected information, such as gender, age, tumor location, operation type, tumor size, tumor grade (differentiation), pathologic tumor (pT) stage, presence of lymph node metastasis, lymph node ratio (the total number of metastatic lymph nodes divided by the total number of retrieved lymph nodes), the presence of microscopic perineural invasion, the presence of lymphovascular invasion, the recurrence pattern, and the time to recurrence, which was defined as the time from surgical resection to recurrence or the last clinical follow-up visit at our medical center.
3. PET/CT protocol and PET-related parameters
18F-FDG PET/CT scans were performed with the same protocol described in our previous study.12 The SUVmax and MTV2.5 were measured on PET images using volume viewer software. Each tumor was examined with a spherical-shaped volume of interest (VOI) that included the entire lesion in the axial, sagittal, and coronal planes. By using CT images, the 18F-FDG uptake values of normal organs such as the bowel, stomach, and liver were not included in the VOI. The SUVmax of the VOI was calculated as (decay-corrected activity/tissue volume)/(injected dose/body weight). MTV2.5 was defined as the total tumor volume with an SUV ≥2.5, and the MTV and mean SUV of the VOI were automatically calculated. The tumor to liver ratio (TLG) was calculated as (mean SUV) × (MTV). In patients with SUVmax <2.5, the MTV2.5 and TLG were not measured. The TLG was calculated as the SUVmax/SUVmean of the liver parenchyma to adjust the values of different PET scanners.
4. Sample preparation
In total, six tumor samples from each pancreatic cancer patient were used for the transcriptomics study. Three samples were randomly selected from both the MTV high (MTV2.5 ≥4.5) group and the MTV low (MTV2.5 <4.5) group. Total RNA was extracted from each formalin-fixed paraffin-embedded sample using the TRIzol reagent (Molecular Research Center, Inc., Cincinnati, OH, USA) according to the manufacturer’s instructions. Following homogenization, 1 mL of solution was transferred to a 1.5-mL Eppendorf tube and centrifuged at 12,000 g for 10 minutes at 4°C to remove any insoluble material. The supernatant containing the RNA was collected, mixed with 0.2 mL of chloroform, and centrifuged at 12,000 g for 15 minutes at 4°C. After nucleic acids in the aqueous phase were transferred to a new tube, the RNA was precipitated by adding 0.5 mL of isopropyl alcohol and then recovered by centrifuging the tube at 12,000 g for 10 minutes at 4°C. The RNA pellet was washed briefly in 1 mL of 75% ethanol and centrifuged at 7,500 g for 5 minutes at 4°C. Finally, the total RNA pellet was dissolved in nuclease-free water, and its quality and quantity were assessed on an Agilent Bioanalyzer 2100. Gene expression was analyzed with the GeneChip® Human Genome U133 Plus 2.0 Array (Affymetrix, Santa Clara, CA, USA), which is composed of over 45,000 probe sets representing approximately 38,500 well-characterized human genes. For each gene, eleven pairs of oligonucleotide probes are synthesized in situ on the arrays.
5. Microarray
Biotinylated cRNA was prepared according to the standard Affymetrix protocol from 200 ng of total RNA (Expression Analysis Technical Manual, 2001; Affymetrix). Following fragmentation, 3 μg of RNA were hybridized for 16 hours at 45°C on the GeneChip® Human Genome Array. The GeneChip® was washed and stained in the Affymetrix Fluidics Station 450. The GeneChip® was scanned using the Affymetrix GeneChip® Scanner 3000 7G. The data were analyzed with Robust Multichip Analysis using the Affymetrix default analysis settings and global scaling as the normalization method. The trimmed mean target intensity of each array was arbitrarily set to 100. The normalized and log transformed intensity values were then analyzed using GeneSpring GX 12.6.1 (Agilent Technologies, Santa Clara, CA, USA). Fold change filters included the requirement that the genes be present in at least 150% of the controls for upregulated genes and fewer than 66% of the controls for downregulated genes. Through hierarchical clustering, data were clustered into groups that behaved similarly across experiments using GeneSpring GX 12.6.1 (Agilent Technologies). The clustering algorithm used the Euclidean distance with average linkage.
6. Transcriptomics data analysis
The transcriptomics data obtained from the Affymetrix U133 Plus 2.0 Arrays were used for the calculation of the fold ratio and p-value of gene expression levels between MTV2.5 high and MTV2.5 low tumor samples. Genes showing significantly differential expression between MTV2.5 high and MTV2.5 low tumor samples were selected and included in an integrative analysis with ingenuity pathway analysis software (Qiagen Inc., Valencia, CA, USA). The comprehensive analyses for canonical pathways, upstream elements, diseases and functions, and regulatory effects were performed.
7. Statistics
Continuous variables were described as the means±standard deviation, and categorical variables were described as frequencies (%). The Student t-test, chi-squared tests with Fisher exact tests, and linear regression analyses were performed. The Pearson correlation method was used to calculate the correlation coefficients. Survival curves were estimated using the Kaplan-Meier method to calculate the cumulative recurrence-free survival rates. Statistical analyses were performed using SPSS 20.0 for Windows (IBM Corp., Armonk, NY, USA). p-values <0.05 were considered statistically significant.
RESULTS
1. Characteristics of patients with resected pT3 pancreatic cancer
From January 2010 to December 2015, 232 patients underwent radical resection for pancreatic cancer. The final study population was 93 patients after excluding the patients who underwent neoadjuvant treatment or palliative resection. The mean age of the study population was 63.6±9.4 years; 53 (57%) were males, and 40 (43%) were females.
2. Oncologic outcome of lymph node metastasis in patients with resected pT3 pancreatic cancer
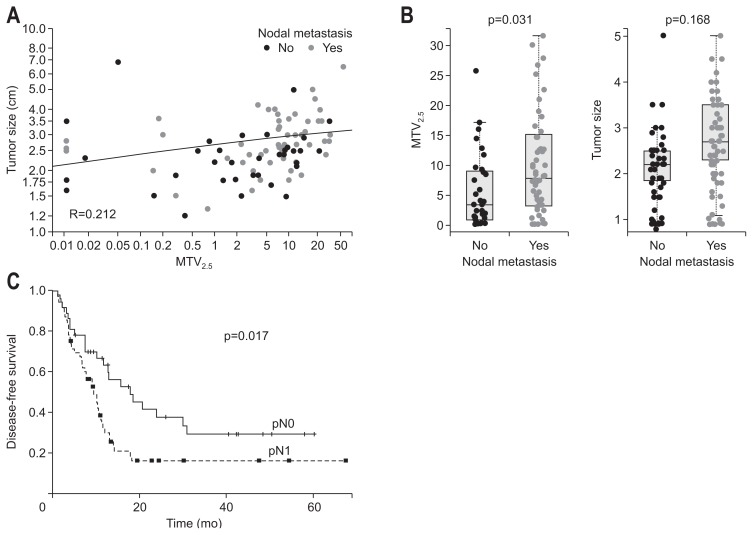
Among the clinically available pathologic variables, such as the tumor size, degree of differentiation, presence of lymphovascular invasion, presence of perineural invasion, presence of lymph node metastasis, and resection margin, the Cox proportional hazard model showed that lymph node metastasis was the strongest prognostic factor predicting tumor recurrence (Exp(β)=1.868, p=0.019). There was a significant difference in disease-free survival (DFS) according to the pN stage (mean, 26.7 months; 95% CI, 18.5 to 34.8 vs mean, 17.7 months; 95% CI, 11.4 to 24.0; p=0.017) (Fig. 1C).
Fig. 1.
Tumor size and MTV2.5 for nodal metastasis. (A) Correlation analysis for tumor size and MTV2.5. (B) Comparison of the difference in tumor size and MTV2.5 according to nodal metastasis. (C) The oncologic outcome of lymph node metastasis in resected pT3 pancreatic cancer.
MTV, metabolic tumor volume; pT3, pathologic T3.
3. Preoperative detectable clinical parameter to predict lymph node metastasis in patients with resected pT3 pancreatic cancer
Only the value of preoperative MTV2.5 was significantly higher in patients with pN1 than in other patients (6.5±7.8 vs 11.1±11.2, p=0.031). SUVmax was also marginally significantly different between the two groups; however, when adjusted by the SUVmean of the liver (tumor to liver ratio), there was no significant difference between two groups (1.9±0.8 vs 2.2±1.1, p=0.231) (Table 1).
Table 1.
Preoperatively Available Parameters to Predict Lymph Node Metastasis in Resected pT3 Pancreatic Cancer
| Clinical variable | pN-stage | p-value | |
|---|---|---|---|
|
| |||
| pN0 (n=37) | pN1 (n=56) | ||
| Age, yr | 64.3±9.2 | 63.2±9.6 | 0.597 |
| Sex, male/female | 23/14 | 30/26 | 0.413 |
| Preoperative CA 19-9 | 575.6±2207.6 | 886.2±2343.4 | 0.58 |
| Radiologic tumor size, cm | 2.4±0.8 | 2.8±1.2 | 0.168 |
| Tumor location, proximal/distal | 23/14 | 38/18 | 0.572 |
| SUVmax | 4.5±2.1 | 5.5±2.6 | 0.055 |
| TLR | 1.9±0.8 | 2.2±1.1 | 0.231 |
| MTV2.5 | 6.5±7.8 | 11.1±11.2 | 0.031 |
Data are presented as mean±SD or number.
pT3, pathologic T3; SUVmax, maximum standard uptake value; TLR, tumor to liver ratio; MTV, metabolic tumor volume.
4. Preoperative MTV2.5 ≥4.5 is significantly associated with lymph node metastasis in patients with resected pT3 pancreatic cancer
The previously determined preoperative PET parameter12 of a value of MTV2.5≥4.5 was again found to have a close relationship with lymph node metastasis in patients with resected pT3 pancreatic cancer (p=0.019). In addition, higher MTV2.5 values (MTV2.5≥4.5) in patients with pancreatic cancer was found to be associated with metastasis to multiple lymph nodes (chi-square, linear-to-linear association, p=0.003), and the lymph node ratio was also significantly higher in patients with resected pT3-pancreatic cancer with MTV2.5 ≥4.5 than in those with MTV2.5 <4.5 (0.05±0.08 vs 0.12±0.13, p=0.001) (Table 2).
Table 2.
Preoperative Positron Emission Tomography Parameters to Predict Pathologic Outcomes in Resected pT3 Pancreatic Cancer
| Pathological variable | MTV2.5 | p-value | |
|---|---|---|---|
|
| |||
| <4.5 | ≥4.5 | ||
| pN-stage | 0.019 | ||
| pN0 | 21 | 18 | |
| pN1 | 16 | 38 | |
| Retrieved LNs | 19.3±9.4 | 19.9±10.9 | 0.76 |
| Metastatic LNs | 0.003 | ||
| 0 | 21 | 14 | |
| 1 | 10 | 15 | |
| ≥2 | 8 | 25 | |
| LNR | 0.05±0.08 | 0.12±0.13 | 0.001 |
Data are presented as number or mean±SD.
pT3, pathologic T3; MTV, metabolic tumor volume; LN, lymph node; LNR, lymph node ratio.
5. Association between MTV2.5 and tumor size according to nodal metastasis
To elucidate the confounding effect of tumor size on MTV2.5, a correlation analysis and statistical comparisons of tumor size and MTV2.5 according to nodal metastasis were performed. There was no marked correlation (Pearson correlation coefficient= 0.212) between MTV2.5 and tumor size (Fig. 1A). Though the difference in tumor size according to nodal metastasis was not statistically significant (p=0.168), the value of MTV2.5 was significantly higher in the nodal metastasis group than in the group without nodal metastasis (p=0.031) (Fig. 1B).
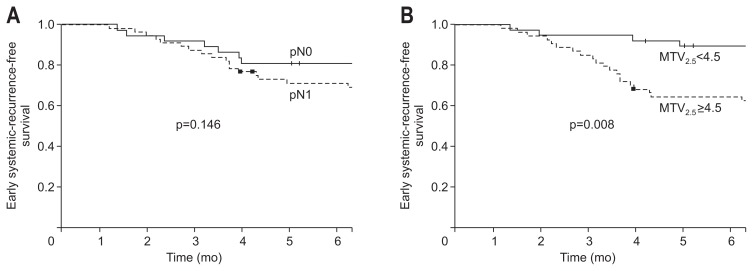
6. Preoperative MTV2.5 ≥4.5 is significantly associated with early systemic metastasis in patients with resected pT3 pancreatic cancer
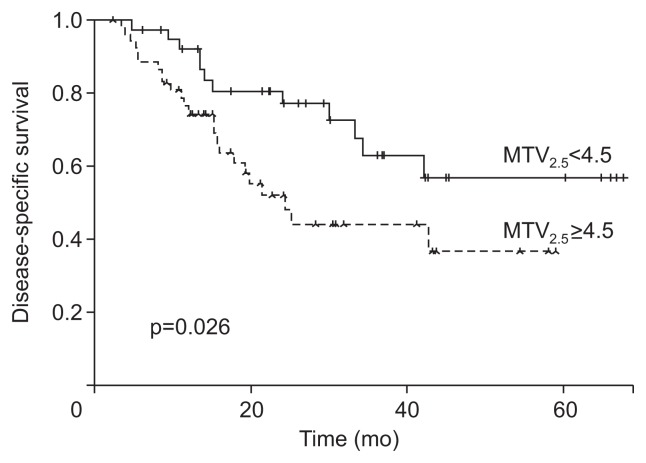
Among the 93 patients with resected pT3 pancreatic cancer, 28 patients (30.1%) experienced early (<6 months after surgery) systemic recurrence. The mean time interval from radical pancreatectomy to early systemic recurrence was 3.9±2.6 months. The most frequent distant metastatic site was found to be the liver (16/28, 57.1%). pN stage could not predict early systemic recurrence in patients with resected pT3 pancreatic cancer (p=0.146) (Fig. 2A). A lymph node ratio cutoff value of 0.07 was shown to determine early systemic recurrence with a sensitivity of 60.7% and a specificity of 71.5%. The same cutoff value could discriminate those with early systemic metastasis from those without with marginal significance in patients with resected pT3 pancreatic cancer (p=0.078). However, significantly more patients with MTV2.5 ≥4.5 than those with MTV2.5 <4.5 had early systemic recurrence after initial radical pancreatectomy (p=0.008) (Fig. 2B). Subsequently, the disease-specific survival of the patients with MTV2.5 <4.5 was much better than those with MTV2.5 ≥4.5 (mean, 28.8 months; 95% CI, 40.1 to 57.0 vs mean, 32.6 months; 95% CI, 25.5 to 39.7; p=0.026) (Fig. 3).
Fig. 2.
Preoperative MTV2.5 parameter and early systemic metastasis in resected pT3 pancreatic cancer. (A) Early systemic recurrence-free survival according to nodal metastasis. (B) Early systemic recurrence-free survival according to MTV2.5 value.
MTV, metabolic tumor volume; pT3, pathologic T3.
Fig. 3.
Disease-specific survival according to the preoperative MTV2.5 parameter in resected pT3 pancreatic cancer.
MTV, metabolic tumor volume; pT3, pathologic T3.
7. Postoperative adjuvant chemotherapy attenuates the adverse oncologic impact of MTV2.5 ≥4.5 in patients with resected pT3 pancreatic cancer
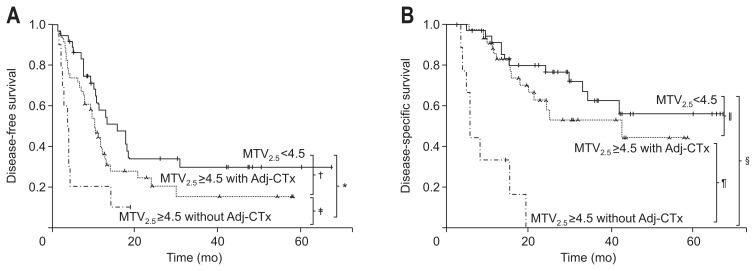
Approximately 80% of patients who underwent curative resection received adjuvant treatment based on gemcitabine or fluorouracil (5-FU). Among them, approximately 15% of patients who received adjuvant treatment after surgery underwent chemotherapy with radiation therapy. There was no significant difference in the proportion of patients receiving adjuvant treatment according to the level of MTV2.5 (Table 3). Postoperative adjuvant chemotherapy could modify the oncologic outcome of patients with resected pT3 pancreatic cancer. There was no significant difference in the oncologic outcomes (log-rank p=0.352 in DFS, p=0.142 in overall survival) between patients who received adjuvant treatment and those who did not in the MTV2.5 low group (MTV2.5 <4.5). However, among patients with MTV2.5 ≥4.5, those who received postoperative adjuvant chemotherapy had longer DFS times than those who did not receive postoperative adjuvant chemotherapy (mean, 5.7 month; 95% CI, 2.2 to 9.2 vs mean, 17.4 month; 95% CI, 11.3 to 23.6; p=0.026) (Fig. 4A); furthermore, the DFS of the former group approached that of patients with MTV2.5 <4.5 (mean, 28.3 months; 95% CI, 18.9 to 37.6; p=0.075). Moreover, the overall disease-specific survival of patients with MTV2.5 ≥4.5 who underwent postoperative chemotherapy became similar to those with MTV2.5 <4.5 (mean, 34.7 months; 95% CI, 29.9 to 45.2 vs mean, 48.4 months; 95% CI, 39.9 to 56.9; p=0.241) (Fig. 4B). In addition, it was found that among the 28 patients who experienced early (<6 months after surgery) systemic recurrence, only 17 patients (60.7%) received postoperative adjuvant chemotherapy, while most patients (58/65 patients, 89.2%) without early systemic recurrence received postoperative adjuvant chemotherapy (p=0.001) (Table 4).
Table 3.
Details of Adjuvant Treatment According to MTV2.5
| Adjuvant treatment | MTV2.5 <4.5 (n=37) | MTV2.5 ≥4.5 (n=56) | p-value |
|---|---|---|---|
| Adjuvant treatment | 29 (78.4) | 45 (80.4) | 0.812 |
| Chemoradiation | 4 (13.8) | 8 (17.8) | 0.788 |
| Chemotherapy only | 25 (86.2) | 48 (82.2) | |
| Radiation dose, range, Gy | 40.3±15.4 | 41.2±12.3 | 0.886 |
| Chemotherapy regimen | |||
| Gemcitabine base | 16 (55.2) | 24 (53.3) | 0.728 |
| 5-Fluorouracil base | 13 (44.8) | 21 (46.7) | |
Data are presented as number (%).
MTV, metabolic tumor volume.
Fig. 4.
The adverse oncologic impact of MTV2.5 ≥4.5 according to postoperative adjuvant chemotherapy in resected pT3 pancreatic cancer. (A) Disease-free survival according to MTV2.5 subgroup with or without adjuvant chemotherapy (*p=0.00, †p=0.075, ‡p=0.026). (B) Disease-specific overall survival according to MTV2.5 subgroup with or without adjuvant chemotherapy (§p<0.001, ||p=0.241, ¶p<0.001).
MTV, metabolic tumor volume; pT3, pathologic T3; Adj-CTx, adjuvant chemotherapy.
Table 4.
Early Systemic Recurrence According to Postoperative Adjuvant Chemotherapy
| Adjuvant chemotherapy | Early systemic recurrence (<6 mo after surgery) | p-value | ||
|---|---|---|---|---|
|
| ||||
| No | Yes | |||
| Postoperative adjuvant chemotherapy | No | 7 | 11 | 0.001 |
| Yes | 58 | 17 | ||
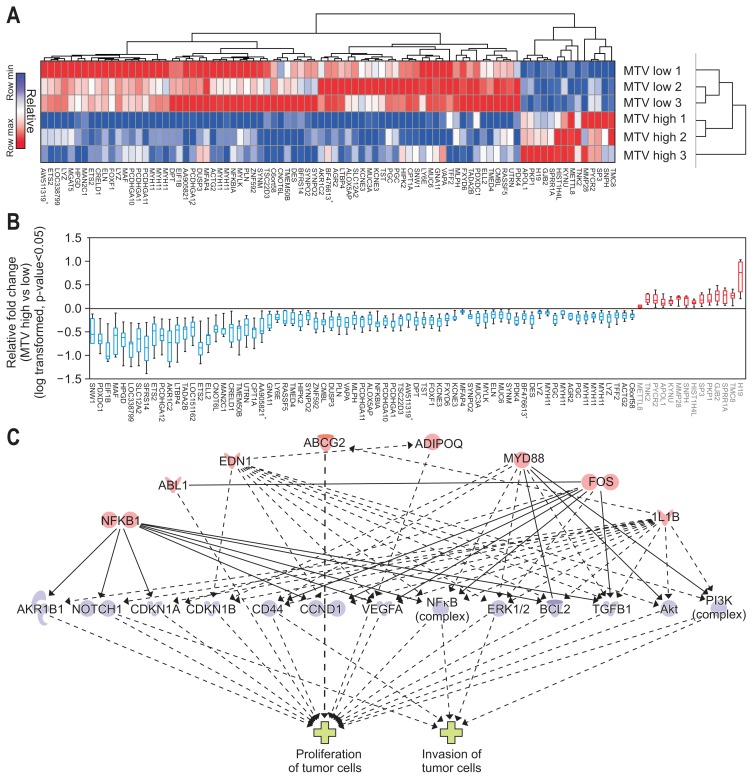
8. Genetic background of resected T3 pancreatic cancer with MTV2.5 ≥4.5 is associated with aggressive biologic behavior; transcriptome-wide analysis discriminating gene expression
In total, 85 genes (upregulated in MTV2.5 high: 14 genes; downregulated: 71) were identified in the transcriptome-wide analysis for differentially expressed genes according to metabolic phenotype (MTV high; MTV2.5 ≥4.5 vs MTV low; MTV2.5 <4.5) (Fig. 5A and B, Supplementary Tables 1 and 2, Supplementary Figs 1 and 2). Causative analyses using regulator effectors associated with the phenotype of the tumors were performed. Master regulators (NFKB1, ABL1, EDN1, ABCG2, ADIPOQ, MYD88, FOS, and IL1B) were associated with the phenotype of the tumor in terms of the proliferation and invasion of tumor cells via several downstream effectors (AKR1B1, NOTCH1, CDKN1A, CDKN1B, CD44, CCND1, VEGFA, NFkB, ERK1/2, BCL2, TGFB1, Akt, and PI3K). These molecular pathways were significantly correlated with the aggressive tumor phenotype (Fig. 5C, data shown in Supplementary Tables 4 and 6).
Fig. 5.
Hierarchical clustering & significant genes heat map comparing metabolic tumor volume (MTV) high versus low (14 upregulated genes and 71 downregulated genes). (A) Hierarchical clustering of significantly expressed genes (fold change >2 or <0.5 with p<0.05). (B) Relative log-transformed fold changes of MTV high versus low. (C) Causative analysis of regulatory effectors and associated tumor phenotype. Master regulators (NFKB1, ABL1, EDN1, ABCG2, ADIPOQ, MYD88, FOS, and IL1B) were associated with the tumor phenotype in terms of the proliferation and invasion of tumor cells via several downstream effectors (AKR1B1, NOTCH1, CDKN1A, CDKN1B, CD44, CCND1, VEGFA, NFkB, ERK1/2, BCL2, TGFB1, Akt, and PI3K) (data shown in Supplementary Tables 4 and 6).
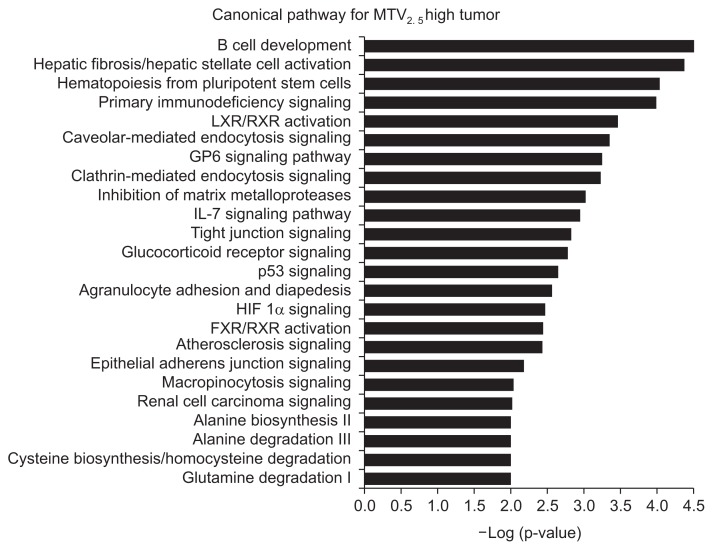
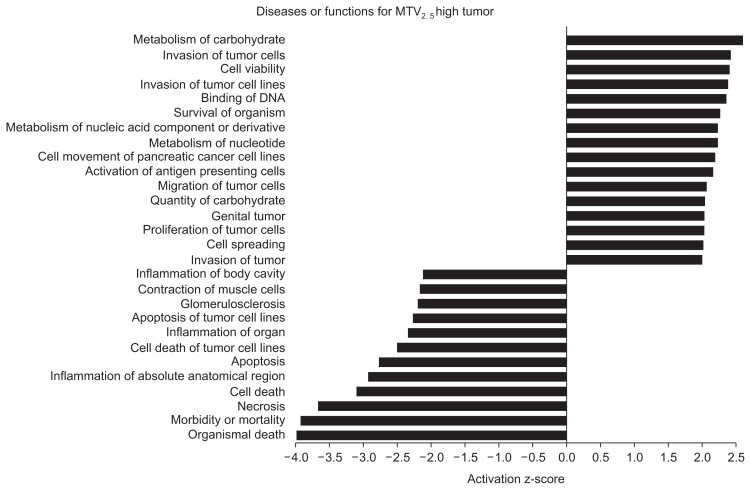
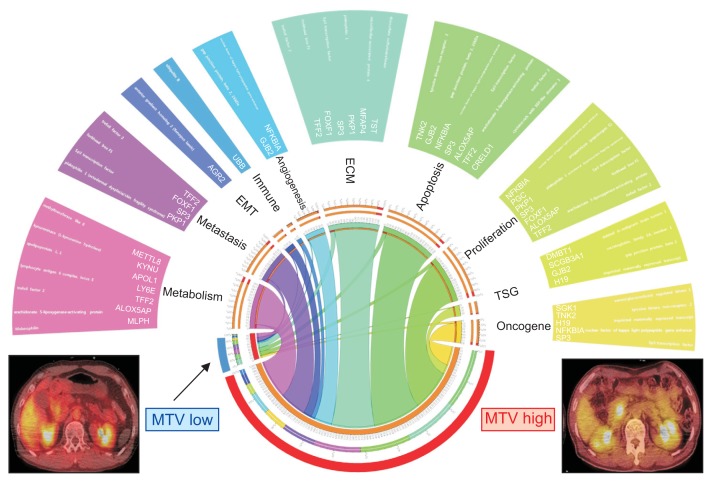
A supervised analysis for cancer-specific genes related to the hallmarks of cancer was performed using gene set analysis with gene sets for oncogenes, tumor suppressor genes, proliferation, apoptosis, extracellular remodeling, angiogenesis, immune escape, epithelial-mesenchyme transition, metastasis, and metabolism obtained from the GeneCards database (Supplementary Figs 2–6).15,16 The upregulated canonical pathways predicted from the gene expression pattern of the MTV high tumors were associated with aberrant immune response, impaired stromal signaling, and alternative metabolic pathways (Fig. 6). MTV high tumors were strongly associated with the aggressive tumor phenotype in terms of the proliferation and invasion of tumor cells, with the predicted correlation with disease and function (Fig. 7). The landscape of discriminating gene expression levels of cancer-specific genes according to metabolic phenotype in resected pT3 pancreatic cancer visualized by Circos plots17 revealed that MTV high tumors had markedly higher expression levels of cancer-specific genes than MTV low tumors, reflecting the biologically aggressive behavior of resectable pancreatic cancer (Fig. 8).
Fig. 6.
Significantly upregulated canonical pathways in MTV2.5 high tumor samples (data shown in Supplementary Table 3).
MTV, metabolic tumor volume; LXR, liver X receptor; RXR, retinoid X receptor; IL, interleukin; HIF, hypoxia-inducible factor 1; FXR, farnesoid X receptor.
Fig. 7.
Diseases or functions associated with gene expression pattern of MTV2.5 high tumor samples (data shown in Supplementary Table 5). MTV, metabolic tumor volume.
Fig. 8.
Circos plot for the landscape of discriminating gene expression related to cancer-specific genes according to metabolic phenotype in resected pT3 pancreatic cancer.
MTV, metabolic tumor volume; pT3, pathologic T3; EMT, epithelial mesenchymal transition; ECM, extracellular matrix; TSG, tumor suppressor gene.
DISCUSSION
Pancreatic cancer is an intractable carcinoma with a dismal prognosis due to early systemic metastasis. Even after marginnegative resection of primary pancreatic cancer, the majority of patients undergo systemic metastasis. Early systemic metastasis is a major feature of pancreatic cancer even after margin-negative resection of a primary cancer lesion. Therefore, the identification of a high-risk group showing aggressive tumor biology even among patients with resectable pancreatic cancer is needed to improve their oncologic outcomes after curative resection.
Current evidence shows that metabolic phenotypes that can be obtained clinically by PET scans before surgical resection can predict the oncologic outcomes of patients with various solid tumors.18 There is a high likelihood that a primary tumor with high metabolic activity has at least a minimal amount of residual disease that cannot be detected on preoperative imaging studies.19,20
In the treatment of pancreatic cancer, systemic chemotherapy is fundamental for improving oncologic outcomes after resection. 19 In fact, in the present study, 15 of 28 patients (53.6%) showing early recurrence were found to have systemic metastasis before adjuvant treatment because of their poor general condition and their refusal of treatment (11 out of 15 patients). Therefore, considering the potential role of systemic chemotherapy in treating pancreatic cancer, even resectable pancreatic cancer, neoadjuvant chemotherapy might be reasonable in patients with pancreatic cancer with high MTV2.5. Our results also showed that high metabolic tumors correlated with higher node positive rate, early systemic recurrence within 6 months after curative resection, and favorable oncologic outcomes in response to systemic chemotherapy. It is thought that this population can be a potential candidate population for neoadjuvant treatment in resectable pancreatic cancer.
In this study, we performed a transcriptome-wide analysis using patients’ tumor tissue to reveal the genetic background of the differences in metabolic phenotypes identified on PET scans preoperatively. The result demonstrated broad enhancement of cancer-related gene expression, especially genes related to cancer progression and metastasis in the MTV high group (MTV2.5 ≥4.5) compared to the low group (MTV2.5 <4.5). To the best of our knowledge, this is rare translational study using clinical samples based on metabolic phenotype measured by preoperative images to reveal differences in the molecular landscape according to metabolic phenotype.
This retrospective observational study was performed in a single institution with a limited study population. The transcriptome-wide analysis was also conducted in small number based on metabolic phenotype. In spite of these limitations, our pilot translational study showed the prognostic value of metabolic phenotype that can be identified by preoperative PET scan. In addition, the potential correlation between gene expression related to aggressive tumor behavior and high metabolism pancreatic cancer can be utilized to suggest neoadjuvant treatment and could be beneficial for patients with “apparently” resectable pancreatic cancer with high FDG uptake.
In conclusion, resectable pancreatic cancer with high MTV2.5 is associated with lymph node metastasis and early systemic metastasis. Nonetheless, postoperative adjuvant chemotherapy attenuated this adverse oncologic impact of high MTV2.5 in resectable pancreatic cancer. The genetic background of resectable pancreatic cancer with high MTV2.5 might be associated with aggressive biologic behavior. Taken together, neoadjuvant treatment can be a potential alternative even in resectable pancreatic cancer with high MTV2.5. A well-designed prospective clinical trial with confirmative mechanism study is needed to confirm the choice of therapeutic strategy according to metabolic phenotype in pancreatic cancer.
Supplementary Material
ACKNOWLEDGEMENTS
This study was supported by Korea Institute of Planning and Evaluation for Technology in Food, Agriculture, Forestry and Fisheries (IPET, 31-316055-3).
Author contributions: Study design: S.H.L., C.M.K. Data collection: H.K.H., W.J.L., M.Y. Data analysis: S.H.L., C.M.K. Article writing: S.H.L., C.M.K. Critical revision: C.M.K., M.Y. Obtaining fund: C.M.K.
Footnotes
See editorial on page 225.
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.Hsu PP, Sabatini DM. Cancer cell metabolism: Warburg and beyond. Cell. 2008;134:703–707. doi: 10.1016/j.cell.2008.08.021. [DOI] [PubMed] [Google Scholar]
- 2.Bares R, Klever P, Hauptmann S, et al. F-18 fluorodeoxyglucose PET in vivo evaluation of pancreatic glucose metabolism for detection of pancreatic cancer. Radiology. 1994;192:79–86. doi: 10.1148/radiology.192.1.8208970. [DOI] [PubMed] [Google Scholar]
- 3.Lindholm P, Minn H, Leskinen-Kallio S, Bergman J, Ruotsalainen U, Joensuu H. Influence of the blood glucose concentration on FDG uptake in cancer: a PET study. J Nucl Med. 1993;34:1–6. [PubMed] [Google Scholar]
- 4.Czernin J, Phelps ME. Positron emission tomography scanning: current and future applications. Annu Rev Med. 2002;53:89–112. doi: 10.1146/annurev.med.53.082901.104028. [DOI] [PubMed] [Google Scholar]
- 5.Kinkel K, Lu Y, Both M, Warren RS, Thoeni RF. Detection of hepatic metastases from cancers of the gastrointestinal tract by using noninvasive imaging methods (US, CT, MR imaging, PET): a meta-analysis. Radiology. 2002;224:748–756. doi: 10.1148/radiol.2243011362. [DOI] [PubMed] [Google Scholar]
- 6.Ahn SJ, Park MS, Lee JD, Kang WJ. Correlation between 18F-fluorodeoxyglucose positron emission tomography and pathologic differentiation in pancreatic cancer. Ann Nucl Med. 2014;28:430–435. doi: 10.1007/s12149-014-0833-x. [DOI] [PubMed] [Google Scholar]
- 7.Kubota K. From tumor biology to clinical PET: a review of positron emission tomography (PET) in oncology. Ann Nucl Med. 2001;15:471–486. doi: 10.1007/BF02988499. [DOI] [PubMed] [Google Scholar]
- 8.Torizuka T, Tamaki N, Inokuma T, et al. In vivo assessment of glucose metabolism in hepatocellular carcinoma with FDG-PET. J Nucl Med. 1995;36:1811–1817. [PubMed] [Google Scholar]
- 9.Chung HH, Jo H, Kang WJ, et al. Clinical impact of integrated PET/CT on the management of suspected cervical cancer recurrence. Gynecol Oncol. 2007;104:529–534. doi: 10.1016/j.ygyno.2006.09.009. [DOI] [PubMed] [Google Scholar]
- 10.Shinoto M, Yamada S, Yoshikawa K, et al. Usefulness of 18F-fluorodeoxyglucose positron emission tomography as predictor of distant metastasis in preoperative carbon-ion radiotherapy for pancreatic cancer. Anticancer Res. 2013;33:5579–5584. [PubMed] [Google Scholar]
- 11.Chong JU, Hwang HK, Lee JH, Yun M, Kang CM, Lee WJ. Clinically determined type of 18F-fluoro-2-deoxyglucose uptake as an alternative prognostic marker in resectable pancreatic cancer. PLoS One. 2017;12:e0172606. doi: 10.1371/journal.pone.0172606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kang CM, Lee SH, Hwang HK, Yun M, Lee WJ. Preoperative volume-based PET parameter, MTV2.5, as a potential surrogate marker for tumor biology and recurrence in resected pancreatic cancer. Medicine (Baltimore) 2016;95:e2595. doi: 10.1097/MD.0000000000002595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kang CM, Hwang HK, Park J, et al. Maximum standard uptake value as a clinical biomarker for detecting loss of SMAD4 expression and early systemic tumor recurrence in resected left-sided pancreatic cancer. Medicine (Baltimore) 2016;95:e3452. doi: 10.1097/MD.0000000000003452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Allen PJ, Kuk D, Castillo CF, et al. Multi-institutional validation study of the American Joint Commission on Cancer (8th Edition) changes for T and N staging in patients with pancreatic adenocarcinoma. Ann Surg. 2017;265:185–191. doi: 10.1097/SLA.0000000000001763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rebhan M, Chalifa-Caspi V, Prilusky J, Lancet D. GeneCards: integrating information about genes, proteins and diseases. Trends Genet. 1997;13:163. doi: 10.1016/S0168-9525(97)01103-7. [DOI] [PubMed] [Google Scholar]
- 16.Stelzer G, Rosen N, Plaschkes I, et al. The GeneCards Suite: from gene data mining to disease genome sequence analyses. Curr Protoc Bioinformatics. 2016;54:1.30.1–1.30.33. doi: 10.1002/cpbi.5. [DOI] [PubMed] [Google Scholar]
- 17.Krzywinski M, Schein J, Birol I, et al. Circos: an information aesthetic for comparative genomics. Genome Res. 2009;19:1639–1645. doi: 10.1101/gr.092759.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim BK, Kang WJ, Kim JK, et al. 18F-fluorodeoxyglucose uptake on positron emission tomography as a prognostic predictor in locally advanced hepatocellular carcinoma. Cancer. 2011;117:4779–4787. doi: 10.1002/cncr.26099. [DOI] [PubMed] [Google Scholar]
- 19.Müller V, Alix-Panabières C, Pantel K. Insights into minimal residual disease in cancer patients: implications for anti-cancer therapies. Eur J Cancer. 2010;46:1189–1197. doi: 10.1016/j.ejca.2010.02.038. [DOI] [PubMed] [Google Scholar]
- 20.Kostakoglu L, Goldsmith SJ. 18F-FDG PET evaluation of the response to therapy for lymphoma and for breast, lung, and colorectal carcinoma. J Nucl Med. 2003;44:224–239. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.