Abstract
Care managers who coordinate care for chronically ill patients in hospitals and outpatient settings use multiple health information technologies for accessing, processing, documenting, and communicating patient-related information. Using a combination of 41 interviews and observations of 15 care managers, we identified a range of technology-related barriers experienced by care managers (total of 163 occurrences). The barriers are related to (lack of) access to information, inadequate information, limited usefulness and usability of the technologies, challenges associated with using multiple health IT, and technical problems. In 43% of the occurrences, care managers describe strategies to deal with the technology barriers; these fit in three categories: nothing/delay (9 occurrences), work-arounds (32 occurrences), and direct action at the individual, team, and organization levels (29 occurrences). Our data show the adaptive capacity of care managers who develop various strategies to deal with technology barriers and are, therefore, able to care for chronically ill patients. This information can be used as input to work system redesigns.
Keywords: work system, barriers, strategies, adaptation, care manager, care coordination, health information technology, usability
1. Introduction
Improving the design of healthcare work systems is key to ensuring safety, productivity, and well-being of healthcare professionals and patients. This can be achieved by identifying barriers in their work systems (Alyousef et al., 2017; Carayon et al., 2011; Carayon, Li, et al., 2014; Hoonakker et al., 2013) and then developing interventions to remove the barriers. Although removing barriers represents a primary intervention for redesigning work systems and achieving positive outcomes, it may not always be possible (Carayon, 2009; Smith & Carayon-Sainfort, 1989). Therefore, we need to further explore the role of workers in adapting their work systems and adapting to their work systems, especially when they face barriers (Carayon, Wetterneck, et al., 2014; R.J. Holden et al., 2013). In this study, we examined strategies used by care managers in dealing with technology barriers.
1.1. Context of the study: Coordinating care for chronically ill patients
Almost half of the U.S. population has one or more chronic conditions, such as heart failure (HF) or chronic obstructive pulmonary disease (COPD) (McDonald et al., 2007). Because patients with chronic conditions are cared for by multiple healthcare providers and hospitalized more often than the general population, they are likely to experience care coordination problems (McDonald et al., 2007). Well-coordinated care helps avoid delays in diagnosis and treatment, and confusion in what needs to be done for the patients (Bodenheimer, 2008); this work is often the responsibility of care managers (Carayon, Hundt, et al., 2015; Maliski, Clerkin, & Litwin, 2004; Oliva, 2010; Steele et al., 2010). In order to coordinate care for patients with chronic conditions, care managers access, process, document, and communicate patient-related information. They use multiple technologies, such as EHR (Electronic Health Record), health information exchange (HIE), documentation systems, the telephone, and fax machines, to perform these coordinating activities. Research has identified various challenges or barriers experienced by care managers who use multiple health information technology (IT) systems when coordinating care for chronically ill patients. These barriers include usability problems (e.g., poor interface design, lack of interoperability between applications) and organizational barriers (e.g., no access to some health IT applications) (Alyousef et al., 2012; Alyousef et al., 2017; Carayon et al., 2012). Some technology barriers may be removed through system redesign (e.g. improving exchange of information between two technologies) while others may not be easily removed because of organizational, technical, or financial constraints. Therefore, it is important to understand how workers experience and deal with work system barriers, that is what type of strategies they develop and use in responding to and managing work system barriers (Durso, Ferguson, Kazi, Cunningham, & Ryan, 2014; Holden, Rivera-Rodriguez, Faye, Scanlon, & Karsh, 2013).
1.2. Conceptual model of strategies
Strategies have been defined and labeled in multiple ways. Different bodies of literature describe strategies or actions taken by individuals when faced with safety hazards, job stressors, and other problems:
resilience engineering (Hollnagel, Woods, & Leveson, 2006),
stress coping theory (Lazarus & Folkman, 1984),
user adaptation to/of technology (Beaudry & Pinsonneault, 2005; Tyre & Orlikowski, 1994),
problem solving (Tucker, Edmondson, & Spear, 2002), and
work-arounds (Blijleven, Koelemeijer, Wetzels, & Jaspers, 2017; Halbesleben, Wakefield, & Wakefield, 2008; Koppel, Wetterneck, Telles, & Karsh, 2008; Patterson, 2018).
The resilience engineering literature has defined three strategies that can be used to deal with safety hazards (Hollnagel et al., 2006): anticipation (i.e., knowing what to expect), attention (i.e. knowing what to look for), and response (i.e., knowing what to do). An example of anticipatory strategy is when a nurse sorts medication orders by name in the bar coding medication administration technology before printing the medication order list (R. J. Holden et al., 2013). These strategies represent resilience behaviors of individuals or organizations when faced with disturbances and safety hazards. Lazarus and Folkman (1984) defined coping as the cognitive and behavioral efforts used to deal with job stressors or demands. Coping strategies either target the emotional response to the stressor or demand, or focus on problem solving, which involves dealing directly with the stressor or demand. The literature on technology user adaptation describes strategies that users develop to deal with “significant information technology events that occur in their work environment” (Beaudry & Pinsonneault, 2005, p. 496). Similar to the stress coping theory (Lazarus & Folkman, 1984), this literature defines strategies that are either emotion-focused or problem-focused. Problem solving strategies have been further identified and characterized by Tucker and colleagues (Tucker, 2004; Tucker et al., 2002; Tucker & Spear, 2006). They described strategies used by nurses when dealing with operational problems, such as doing whatever is necessary to continue patient care. They found that nurses primarily used first-order problem-solving strategies that tackle problems at the individual level of action. An example of first-order problem solving strategy occurred when a nurse has to print security tags for two babies in a row, but does not look for why the security tags were missing (Tucker et al., 2002). Second-order problem solving rarely occurred and involved communicating to the person or department responsible for the problem or bringing it to the managers’ attention; these strategies tackled team and organization levels of action.
Work-arounds, another type of strategy, represent “behaviors of users to overcome perceived limitations (workflow problems) in a technical system” (Friedman et al., 2014). Work-arounds have been found in the hospital environment where “informal temporary practices” are used to manage exceptions to normal workflow (Halbesleben, Savage, Wakefield, & Wakefield, 2010; Halbesleben et al., 2008). Work-arounds often occur when healthcare providers deal with problems created by technologies (Carayon et al., 2007; Ferneley & Sobreperez, 2006; Koppel et al., 2008; Mount-Campbell et al., 2019; Patterson, 2018). For example, nurses felt it was easier to document medication administration using bar code medication administration technology before the medication was given (Carayon et al., 2007). This work-around can represent a safety hazard as the patient may not take the medication, despite the medication having been documented as administered.
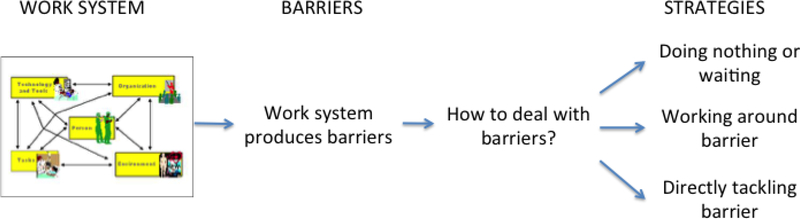
In our research, we defined a strategy as a behavioral or cognitive activity aimed at dealing with a work system barrier. Based on the literature (Durso, Ferguson, et al., 2014; R. J. Holden et al., 2013), we identified three types of strategies in dealing with a work system barrier: (1) doing nothing or waiting and delaying performance (similar to the ‘ignore’ strategy of Durso et al.), (2) working around the barrier either in reaction to or in anticipation of a barrier (similar to the ‘work-around’ strategy of Durso et al.), and (3) tackling the barrier directly and fixing or attempting to fix it [problem-focused] (similar to the ‘mitigate’ and ‘prevent’ strategies of Durso et al.) (see Figure 1). We also recognized that problem-focused strategies (direct action) address various levels of action: the individual, team, or organization levels (Li et al., 2014; Tucker & Edmondson, 2003).
Figure 1 –
Conceptual model of work system, barriers, and strategies
1.3. Study objective
In this research, we applied the conceptual model of strategies displayed in Figure 1 to the domain of care coordination for chronically ill patients. The conceptual model integrates two components of the Systems Engineering Initiative for Patient Safety (SEIPS) model (Carayon et al., 2006; Carayon, Wetterneck, et al., 2014): the work system elements, and the feedback loops; strategies are conceptualized as activities in reaction to strategies created by the work system and are, therefore, examples of the feedback loops in the SEIPS model. We focused on the technology element of the work system (Carayon, 2009; Smith & Carayon-Sainfort, 1989) and technology-related barriers, and described the range of technology barriers experienced by care managers. We then examined care managers’ strategies in dealing with such barriers.
Several studies have described strategies used by healthcare workers in dealing with technology problems or barriers (Durso, Ferguson, et al., 2014; R. J. Holden et al., 2013; Mount-Campbell et al., 2019; Novak, Holden, Anders, Hong, & Karsh, 2013; Tucker & Edmondson, 2003). These studies focus on healthcare workers in the hospitals, such as critical care nurses (Durso, Ferguson, et al., 2014; Durso, Kazi, & Ferguson, 2014). We added to this body of knowledge by studying care managers in both inpatient and outpatient settings. In a manner similar to Durso and colleagues (2014), we also expanded existing research on strategies by examining the specific relationship between barriers and strategies; this is a major innovation of this study. Our study addressed the following research questions:
Do all barriers elicit strategies?
Do certain types of barrier relate to certain types of strategy?
2. Methods
2.1. Setting and sample
Data for this study were collected in the context of a large-scale project funded by the US Department of Health and Human Services. The so-called Keystone Beacon project aimed to expand an existing payor-based outpatient care management model (Maeng, Graf, Davis, Tomcavage, & Bloom, 2012; Steele et al., 2010) and created an integrated system of care managers that were deployed across five counties in central Pennsylvania for about two years. Inpatient care managers (CMs) were located in hospitals, outpatient CMs were assigned to primary care clinics, and transitions of care (TOC) CMs worked in a dedicated telephonic call center (Carayon, Hundt, et al., 2015). CMs relied on health IT-mediated communication of patients’ clinical and psychosocial needs to coordinate care for chronically ill individuals, specifically those with heart failure (HF) and chronic obstructive pulmonary disease (COPD). Technologies used by CMs included electronic health records (EHRs), a health information exchange (KeyHIE), a proprietary care management documentation and reporting system, paper medical records, telephone, and fax.
After receiving an Institutional Review Board (IRB)-approved information sheet, a total of 15 care managers from four hospitals, two primary care clinics and the TOC center volunteered to participate in the study. IRB approval was obtained from the Human Subjects Committee of the lead organization awarded the grant. The IRB for each research partner deferred to the lead organization for approval and oversight.
Summary information and the distribution of interview and observation participants are found in Table 1. The four hospitals in which the inpatient CMs worked included three community hospitals and one regional teaching medical center. Two of the community hospitals were part of the health system led by the regional medical center. The two outpatient clinics were affiliated with community hospitals, both of which had CMs who participated in the study. Most of the care managers in our study are female. Therefore, in the rest of the manuscript we address them with she and her.
Table 1 –
Demographics and summary of interview/observation participants
| Type of Care Manager (CM) | # of CMs (% female) | Mean prior CM experience* | # interviews/observations |
|---|---|---|---|
| Inpatient CM | 5 (100%) | 11 years | 19@ |
| Outpatient CM | 3 (100%) | 3 years | 7 |
| Transition of Care (TOC) CM | 5 (100%) | 8.5 years | 11@ |
| Float CM | 2 (50%) | Not available | 4 |
| Total | 15 (93%) | 41 |
mean reported at data collection 7 months after interviews/observations initiated
one interview included two CMs
2.2. Data collection
Teams composed of two or three senior human factors engineers (the authors), sometimes accompanied by graduate students, conducted a total of 41 combined interviews and observations (12) or interviews alone (29) during 7 rounds of data collection spread over a 21-month period. Data collection occurred over the 21-month period of time during which the Keystone Beacon project was initiated and implemented. During this period, CMs experienced a range of technology barriers, some related to the initiation of the Keystone Beacon project (e.g., not having access yet to all of the necessary health IT systems) and others related to the routine phase of the project. Thirteen of the 15 CMs participated in multiple rounds of data collection (range of participation: 2 to 5 rounds). The data collection resulted in approximately 63 hours of observations and interviews.
2.3. Data collection instrument
Using the SEIPS model (Carayon et al., 2006; Carayon, Wetterneck, et al., 2014) (see Figure 1), we developed a semi-structured interview guide with open-ended questions from which we gained an understanding of CM work. This included questions on all work system elements of the SEIPS model: 1) their past work experience and training, 2) the tools and technology they use, 3) CM-specific tasks they perform including their work schedule, workload and other organizational and environmental characteristics, and 4) work system barriers and facilitators they face. A copy of the interview guide can be found at: https://cqpi.wisc.edu/wp-content/uploads/sites/599/2016/07/Case_Manager_Interview_Guide.pdf. Interviews were conducted in a private room during the workday. Permission was obtained from every participant prior to audio-recording the interview; recordings were later transcribed. During the observations, we watched the CMs perform their work both in their office and, when relevant, on the hospital unit or in the exam room in a primary care clinic, to gain a better understanding of their role, workflow, and how they used the various tools and technologies available to them.
2.4. Data analysis
Content analysis of the transcribed interviews had previously been performed using QSR NVivo® qualitative software (Kianfar, Carayon, Hundt, & Hoonakker, 2014). During that analysis completed by multiple researchers and with an inter-rater reliability of 88%, we captured and coded barriers and facilitators related to multiple facets of the work system, including technology, which is the focus of this study. Through a follow-up coding refinement process, one researcher reviewed the previously identified technology barriers and then coded these data to an inductively-defined node structure. When stated by the interviewee, the researcher also captured the respective strategy(ies) the CM used to address the barriers and coded the corresponding barrier text to a strategy node(s) (i.e., nothing/delay, work-around and/or direct action). Some barriers were not assigned to a strategy whenever the interviewee did not mention an activity aimed at dealing with the barrier. A second researcher reviewed this coding and the node structure of barriers for clarity. Once all initial coding of the technology-related barriers and strategies was complete, the coding was shared with a third researcher. Three researchers then met and, after an iterative process of reviewing and refining the work, agreed upon the final barriers node structure. Three researchers then completed the categorization of strategies independently, using the categorization described earlier (nothing/delay, work-around, direct action). Research team members met and discussed each strategy in light of the barrier(s) to which it was coded. Whenever there was a discrepancy, each researcher explained her/his rationale for how s/he categorized the respective strategy; the researchers then discussed the categorization until agreement was achieved. Throughout this process, any time a question arose concerning a specific barrier or strategy, a researcher returned to the raw data and the research team members discussed the point until they arrived at a consensus. The process used to produce the list of barriers and strategies and to code the data relied on multiple steps, was iterative, and involved significant communication and discussion among the researchers.
A matrix denoting the strategy (when provided by the CM) associated with each barrier was created; rows of the matrix were barriers, and columns were strategies. Cells of the matrix indicated the number of occurrences in which a strategy was mentioned for a specific barrier. Some strategies were used to overcome more than one type of barrier, and some barriers had more than one strategy since different CMs addressed barriers in different ways. This was evident in the matrix. We calculated the percent of barriers with one or more strategy for each category of barriers. This process of quantifying qualitative data fits the mixed methods approach of sequential exploratory design with mixing in the data analysis stage (Carayon, Kianfar, et al., 2015; Creswell & Plano Clark, 2011). This type of mixed methods approach takes advantage of the rich, deep qualitative data (see quotes in the Results section) with quantification to assess linkages between barriers and strategies.
3. Results
3.1. Technology barriers
Through an iterative inductive process, we identified a total of 163 occurrences of technology-related barriers, organized in six categories of barriers (see Table 2). Occurrences of inadequate access to health IT and other tools frequently happened during the initiation of the Keystone Beacon project. For instance, some of the care managers had to wait to get access to the local EHR at their hospital or primary care clinic. Inadequate information in health IT was the technology barrier most frequently reported by CMs (48 occurrences). An example related to the health information exchange as stated by an outpatient CM: “I’m finding KeyHIE to be problematic right now. The only stuff I can see on her [the patient] is from April. There is nothing more recent than that.”
Table 2 –
Technology-related barriers: Definitions, examples and frequency
| Categories | Definitions | Examples | Occurrences |
|---|---|---|---|
| Inadequate access to health IT and other tools | CM is unable or has limited ability to physically or electronically access health IT and other tools. | • No direct/full access to local or external EHR • No access to CM documentation and reporting software when away from workstation • Fax machine located far from workstation |
28 (17%) |
| Inadequate information in health IT | CM does not find or use information in health IT because the information is unavailable, untimely, or incomplete. | • No patient authorization available • Incomplete patient information in EHR • Information not timely in health IT • Progress notes in EHR very long |
48 (29%) |
| Limited usefulness | Health IT has features that interfere with CM’s ability to perform work. | • Discharge instructions pended in EHR are not accessible to CM • Unable to fax directly from EHR • Patient record in CM software cannot be used by multiple CMs |
9 (6%) |
| Poor usability | Design of health IT or tool makes it difficult to use. | • Navigation not easy in EHR • CM software not user friendly • Limited field length for documenting in CM software |
25 (15%) |
| Challenge with use of multiple health IT | Using multiple health IT hinders CM’s work performance. | • Double documentation required in multiple health IT because of lack of inter-operability • Slow computer response due to use of multiple health IT |
20 (12%) |
| Technical problems | Health IT problems interfere with CM’s work. | • Computers are down • Internet connection problems |
33 (20%) |
| Total | 163 (100%) |
Limited usefulness and poor usability of the technologies were two other categories of technology barriers reported in 9 and 25 occurrences, respectively. Usability issues included excessive clicking to access information, documenting activities in the case management software with a field length limit, and listing of medications in non-alphabetical order.
A unique technology barrier experienced by care managers was the challenge of using multiple health IT systems. Because their core function is care coordination, CMs had to use multiple technologies to access and find patient-related information, which created barriers, such as the need to double document the same information in multiple health IT systems. This occurred because of lack of inter-operability between the technologies. Finally, technical problems such as computer slowness and Internet connection problems were reported in 33 occurrences by CMs.
3.2. Strategies
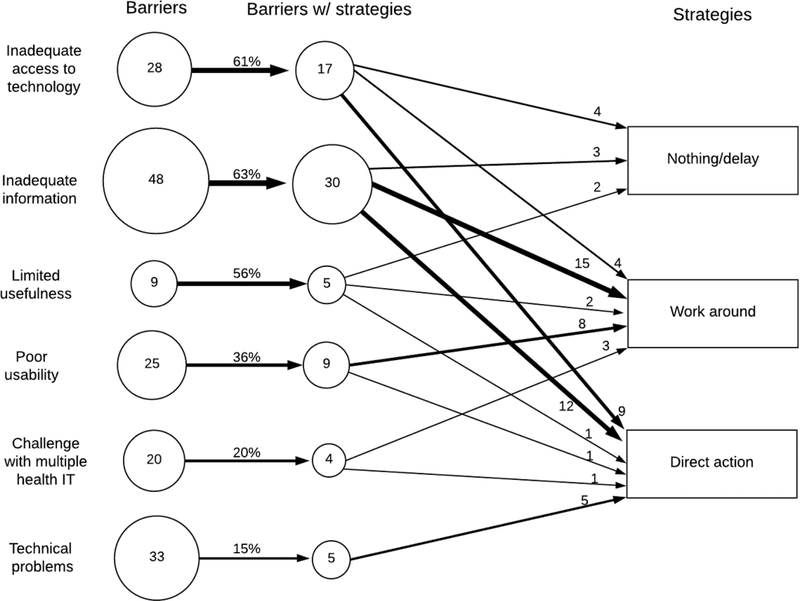
We identified a total of 70 occurrences when CMs described strategies related to technology barriers (43% of occurrences): CMs did nothing or delayed performing an activity (n=9), or used work-around (n=32), and direct action strategies (n=29) (see Table 3 and Figure 2).
Table 3 –
Strategies: Definitions, examples and frequency
| Categories | Definitions | Examples | Occurrences |
|---|---|---|---|
| Nothing/delay | The CM stops or delays her performance because of the presence of barriers. | • Give in; stop task • Discontinue using IT system • Wait for others to get out of IT system |
9 (13%) |
| Work-around | The CM continues to perform her activities and identifies a way to get her job done, despite the presence of the barrier. | • Find patient information in other notes or IT systems • Type notes as free text • Choose option that is closest fit |
32 (46%) |
| Direct action | The CM tackles the barrier directly. | • Create own educational materials for patients • Get help from IT or another CM • Talk to manager about problem |
29 (41%) |
| Total | 70 (100%) |
Figure 2 –
Relationship between technology barriers and strategies
Work-around was the most often reported strategy for almost half of the occurrences of technology barriers. In nine instances, the care manager was not able to resolve a barrier and either had to delay the task or did not take any action. Direct action was the second most reported strategy. The 29 occurrences of the direct action strategy occurred at three levels:
Individual level (9 occurrences): adapting work routines, such as creating own educational materials because of lack of information in EHR.
Team level (14 occurrences): getting help from others, such as IT support and other care managers.
Organization level (6 occurrences): getting the organization involved in fixing the problem, e.g., providing access to EHR, purchasing new software.
3.3. Relationship between technology barriers and strategies
Less than half of the occurrences of technology-related barriers were linked to strategies (see Table 4). Three of the 6 categories of barriers (i.e., inadequate access to technology, inadequate information and poor usability) were linked to strategies in more than 50% of the occurrences. For other barriers, such as technical problems, CMs rarely mentioned strategies regarding how to deal with them.
Table 4 –
Linkages of barriers with strategies
| Barriers | % of barriers with strategies | Strategies | ||
|---|---|---|---|---|
| Nothing/delay | Work-around | Direct action | ||
| Inadequate access to health IT and other tools | 61% (17 of 28) | 4 | 4 | 9 (2 O, 6 T, 1 I) |
| Inadequate information in health IT | 63% (30 of 48) | 3 | 15 | 12 (1 O, 8 T, 3 I) |
| Limited usefulness | 56% (5 of 9) | 2 | 2 | 1 (1 O) |
| Poor usability | 36% (9 of 25) | 8 | 1 (1 O) | |
| Challenge with use of multiple health IT | 20% (4 of 20) | 3 | 1 (1 I) | |
| Technical problems | 15% (5 of 33) | 5 (1 O, 4 I) | ||
| TOTAL | 43% (70 of 163) | 9 | 32 | 29 (6 O, 14 T, 9 I) |
Note: I=individual, T=team, O=organizational [these are levels of action targeted by the direct action strategy.]
Figure 2 displays the relationship between technology-related barriers and strategies. Doing nothing or waiting was a strategy used for 3 of the 6 categories of technology barriers: inadequate access to technology, inadequate information and limited usefulness. Work-arounds were used for all technology-related barriers, except technical problems that were only tackled directly. The strategy of direct action was involved in all 6 categories of technology barriers.
The strategy of doing nothing or waiting was used when, for example, the CM experienced barriers related to some of the technologies, and stopped using them. In other instances, CMs waited for others to enter information in the EHR (e.g. discharge summary) so that they could have access to it.
Work-around was the most frequently reported strategy to deal with technology barriers (32 occurrences). This included “a lot of copy and pasting from [case management software] and putting [one’s] notes over in the [EHR]”. If the technology was not designed appropriately, that is, its usefulness and usability were limited, CMs used various work-arounds such as typing notes as free text: “… the list of disease processes that patients have. I mean, they have this little, tiny list to choose from and otherwise you have to free text everything.” In this instance, the CM also used a direct action strategy by asking that some diseases be added to the list of options.
As indicated above, the direct action strategies occurred at three levels of individual, team and organization. In response to the barrier of inadequate information in the health information exchange, a CM talked about how she developed an individual-level strategy of looking for information in the health information exchange as well as in the other information systems. When encountering technical problems, CMs can get help from health IT technicians as explained by this CM: “… Sometimes I do have problems where I go down with the hospital server… I have to rely on their IT people to bring me up…” This is an example of a strategy at the team level. Organizational strategies frequently involved communication of the CM with their supervisor or manager.
4. Discussion
Using data from 41 interviews and observations of 15 care managers performed over a 21-month period, we identified a large number of technology-related barriers (total of 163 occurrences) that ranged from usability and usefulness, to inadequate access to technology or inadequate information in the technology, to technical problems. Our results are in line with other studies that have found frequent technology-related barriers experienced by healthcare professionals. For instance, Durso et al. (2014) found that technology was the main source of barriers (or threats as called by the authors) experienced by pediatric critical care nurses.
In almost half of the occurrences (43%), care managers mentioned strategies they used to deal with the barriers; the most frequently reported strategies were various types of work-around and direct action at the individual, team and organizational levels. Technology-related barriers, therefore, often involved additional work in the form of strategies (Alyousef et al., 2017), and increase the already high workload of care managers. Therefore, it is important to implement work system changes that can directly address technology barriers and potentially remove extra steps or activities performed by the care managers; therefore, leading to decreased workload. It is also important to recognize that strategies may be used by care managers in order to better manage their workload; strategies may represent efficiencies for the care managers. For instance, strategies aimed at tackling the barriers directly may help remove barriers, and potentially reduce workload associated with the barriers. Our data provide information on the most frequently reported barriers experienced by care managers and can be used to prioritize work system redesign efforts.
4.1. Strategies as job control
Strategies may represent a form of job control where care managers react to the barriers and develop tailoring strategies to determine how to perform their job. Tyre and Orlowski (1994) described two types of individual adaptation activities: “actions intended to modify the technology” to meet users’ needs and “actions intended to modify relevant aspects of the operating context (including users’ skills or procedures)” (page 103). Cook and Woods (1996) also referred to “tailoring strategies”, where technology users may modify the technology (technology tailoring) or modify their behaviors (task tailoring) to accommodate constraints posed by the technology. Tailoring strategies have been found among nuclear control room operators who, for instance, create new graphics to support monitoring during refueling; therefore, compensating for problems with the computerized display of information (Vicente, Roth, & Mumaw, 2001). Our data confirm that care managers indeed developed a range of strategies to deal directly with the technology, such as creating their own educational materials that they share with patients. This adaptive capacity of care managers represents resilience strategies that help care managers perform their care coordination responsibilities and care for their patients, despite the presence of technology barriers.
4.2. Strategy of work-arounds
Work-arounds were the most frequently reported strategies, especially for 2 of the 6 technology barriers: inadequate information in health IT, and limited usefulness. The work of care managers centered around care coordination for chronically ill patients, requiring multiple cognitive activities such as accessing, processing, and documenting patient-related information. Therefore, not being able to access information in the various technologies was a significant barrier that must be addressed: CMs reported strategies in 63% of occurrences of this barrier. In many instances, care managers used a work-around to figure out where and how to find or document information. Work-arounds may represent ‘invisible work’ that care managers need to do in order to perform their job and coordinate care for chronically ill patients. This ‘invisible work’ of work-arounds has been described in a study of technologies used by hospital nurses in treating elderly patients (Dupret, 2017). Dupret (2017) argues that understanding work-arounds in the use of technologies allows this ‘invisible’ work to become visible and, therefore, to be addressed in work system redesign efforts.
Work-arounds may be what allows care managers to provide care in a timely and safe manner; but they can also be potential hazards. For instance, care managers would sometimes choose an option in a menu that was not an exact match, but was the closest fit. In other instances, they typed notes as free text, which may be a hazard if the note is expected to be in another part of the health IT. The use of text fields in health IT was identified as a major theme in a narrative review of work-arounds in the use of health IT (Patterson, 2018).
4.3. Presence or absence of strategies
Our data clearly show that care managers are adaptive and creative in dealing with technology-related barriers; CMs reported doing nothing or delaying performance in only 9 occurrences out of the 70 occurrences when they reported strategies to deal with barriers. It is important to note that doing nothing or delaying performance may also occur in the 93 other occurrences where CMs reported barriers but did not mention strategies. When CMs do not mention strategies during the interviews, one possible explanation is that they do not have strategies for dealing with specific barriers. Another explanation is that CMs may have a hard time in articulating their strategies. The Threat-Strategy Interview technique developed by Durso and colleagues (2014) is a systematic method for identifying strategies and could be used in follow-up research on care managers; this will allow the systematic collection of data on strategies in light of specific barriers experienced by CMs. Data on strategies, in particular work-arounds, can provide valuable information to identify solutions to address technology-related barriers.
4.4. Strategy identification for work system redesign
Strategies developed and used by care managers to deal with technology-barriers provide important insights regarding their work and their ability to adapt their work system or adapt to their work system. They also provide useful information to develop solutions aimed at directly tackling technology barriers. For instance, a work-around may actually become a new work process or procedure. We observed a work-around where care managers ended up finding some important patient-related information in other notes or health IT systems. This may suggest the need to include that information (or a link to it) in the health IT most frequently used by care managers.
For some barriers, care managers reported few strategies. For example, changing the software or hardware may be more difficult to address; therefore, fewer strategies were provided for the barriers of limited usefulness or technical problems. This may be an indication that care managers may not be able to handle or manage those barriers (individual level); therefore, organizational interventions are necessary for these barriers, such as barriers related to the design of the technology. Such barriers would require the designer or implementer of the technology to use human-centered design processes so that the technology fits the work of the care managers (Carayon, Wooldridge, Hose, Salwei, & Benneyan, 2018; Ratwani, Reider, & Singh, 2019). These barriers are important to address in technology or work system redesigns; they may require organizational actions by other people than the care managers.
4.5. Study strengths and limitations
A strength of the study was our evaluation of technology-related barriers throughout the 21 months of the Keystone Beacon project; this allowed us to capture a range of barriers related to the initiation phase (e.g. not having access yet to the technology), as well as the implementation and routine phases. This longitudinal data collection means that we were able to capture technology barriers (and strategies to deal with those barriers) over time. A limitation is that we did not longitudinally analyze the data and therefore did not capture how barriers (and strategies) may have changed over time. In a future study, we can further analyze these possible changes. Because of the longitudinal study design, we collected data by interviewing the same CMs multiple times; but our data analysis did not consider barriers or strategies mentioned by the same interviewee at different times.
The generalizability of the results is limited to this particular case and the small sample of CMs (n=15); however, the general conceptual approach (i.e., the conceptual framework in Figure 1, and the categories of technology barriers and of strategies) may be generalizable to other groups of care managers. This is a topic for future research. Finally, we did not collect data on how effective the different strategies were in overcoming the barriers. Specifically, it would be interesting to examine whether direct action strategies at the organization, team or individual levels were most effective, or whether that is dependent on the type of barrier incurred.
5. Conclusion
Care managers who coordinate care for chronically ill patients face a range of technology barriers and, for about half of the barrier occurrences, describe strategies for dealing with those barriers. Future research should continue to explore strategies developed by workers in dealing with work system barriers, in particular the role of strategies in workload creation and/or management. Because work-arounds were the most frequently reported strategy, we also need to continue examining the benefits and problems (e.g. safety hazard) of work-arounds. This research can provide important information about how to build resilience as organizations find ways to remove or mitigate work system barriers.
Highlights.
Care managers frequently report technology barriers related to information (access and quality) and usability.
About half of the time, care managers report strategies to deal with barriers.
Information on barriers and strategies provides insights for work system redesign.
Acknowledgements
Funding for this research was provided by the US Office of the National Coordinator for Health IT Beacon Community Program [award No. 90BC001301] and was supported by the Clinical and Translational Science Award (CTSA) program, previously through the National Center for Research Resources (NCRR) grant 1UL1RR025011, now by the Center for Advancing Translational Sciences (NCATS), grant 9U54TR000021. The content is solely the responsibility of the authors and does not necessarily represent the official view of NIH.
References
- Alyousef B, Carayon P, Hoonakker P, Hundt AS, Cartmill R, Tomcavage J, … Walker J (2012). Care managers’ challenges in using multiple health IT applications. In The Human Factors and Ergonomics Society (Ed.), Proceedings of the Human Factors and Ergonomics Society 56th Annual Meeting (pp. 1748–1752). Santa Monica, CA: The Human Factors and Ergonomics Society. [Google Scholar]
- Alyousef B, Carayon P, Hoonakker P, Hundt AS, Salek D, & Tomcavage J (2017). Obstacles experienced by care managers in managing information for the care of chronically ill patients. International Journal of Human-Computer Interaction, 33(4), 313–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beaudry A, & Pinsonneault A (2005). Understanding user responses to information technology: A coping model of user adaptation. Mis Quarterly, 29(3), 493–524. [Google Scholar]
- Blijleven V, Koelemeijer K, Wetzels M, & Jaspers M (2017). Workarounds emerging from electronic health record system usage: Consequences for patient safety, effectiveness of care, and efficiency of care. JMIR Hum Factors, 4(4), e27 Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/28982645. doi: 10.2196/humanfactors.7978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodenheimer T (2008). Coordinating care-a perilous journey through the health care system. New England Journal of Medicine, 358(10), 1064–1071. [DOI] [PubMed] [Google Scholar]
- Carayon P (2009). The Balance Theory and the work system model… Twenty years later. International Journal of Human-Computer Interaction, 25(5), 313–327. [Google Scholar]
- Carayon P, Alyousef B, Hoonakker P, Hundt AS, Cartmill R, Tomcavage J, … Walker J (2012). Challenges to care coordination posed by the use of multiple health IT applications. Work: A Journal of Prevention, Assessment and Rehabilitation, 41(0), 4468–4473. Retrieved from 10.3233/WOR-2012-0746-4468. [DOI] [PubMed] [Google Scholar]
- Carayon P, DuBenske LL, McCabe BC, Shaw B, Gaines ME, Kelly MM, … Cox ED (2011). Work system barriers and facilitators to family engagement in rounds in a pediatric hospital In Albolino S, Bagnara S, Bellandi T, Llaneza J, Rosal G, & Tartaglia R (Eds.), Healthcare Systems Ergonomics and Patient Safety 2011 (pp. 81–85). Boca Raton, FL: CRC Press. [Google Scholar]
- Carayon P, Hundt AS, Hoonakker P, Kianfar S, Alyousef B, Salek D, … Tomcavage J (2015). Perceived impact of care managers’ work on patient and clinician outcomes. European Journal of Patient-Centered Healthcare, 3(2), 158–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carayon P, Hundt AS, Karsh B-T, Gurses AP, Alvarado CJ, Smith M, & Brennan PF (2006). Work system design for patient safety: The SEIPS model. Quality & safety in health care, 15(Supplement I), i50–i58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carayon P, Kianfar S, Li Y, Xie A, Alyousef A, & Wooldridge A (2015). A systematic review of mixed methods research on human factors and ergonomics in health care. Applied Ergonomics, 51, 291–321. doi: 10.1016/j.apergo.2015.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carayon P, Li Y, Kelly MM, DuBenske LL, Xie A, McCabe B, … Cox ED (2014). Stimulated recall methodology for assessing work system barriers and facilitators in family-centered rounds in a pediatric hospital. Applied Ergonomics, 45(6), 1540–1546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carayon P, Wetterneck TB, Hundt AS, Ozkaynak M, DeSilvey J, Ludwig B, … Rough SS (2007). Evaluation of nurse interaction with bar code medication administration technology in the work environment. Journal of Patient Safety, 3(1), 34–42. [Google Scholar]
- Carayon P, Wetterneck TB, Rivera-Rodriguez AJ, Hundt AS, Hoonakker P, Holden R, & Gurses AP (2014). Human factors systems approach to healthcare quality and patient safety. Applied Ergonomics, 45(1), 14–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carayon P, Wooldridge A, Hose B-T, Salwei M, & Benneyan J (2018). Challenges and opportunities for improving patient safety through human factors and systems engineering. Health Affairs, 37(11), 1862–1869. Retrieved from https://www.healthaffairs.org/doi/abs/10.1377/hlthaff.2018.0723. doi: 10.1377/hlthaff.2018.0723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook RI, & Woods DD (1996). Adapting to new technologies in the operating room. Human Factors, 38, 593–613. [DOI] [PubMed] [Google Scholar]
- Creswell JW, & Plano Clark VL (2011). Designing and Conducting Mixed Methods Research (2nd ed.). Los Angeles, CA: Sage Publications. [Google Scholar]
- Dupret K (2017). Working around technologies—invisible professionalism? New Technology, Work and Employment, 32(2), 174–187. Retrieved from https://onlinelibrary.wiley.com/doi/abs/10.1111/ntwe.12093. doi: 10.1111/ntwe.12093 [DOI] [Google Scholar]
- Durso FT, Ferguson AN, Kazi S, Cunningham C, & Ryan C (2014). Strategic threat management: An exploration of nursing strategies in the pediatric intensive care unit. Applied Ergonomics. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/25287275. [DOI] [PubMed]
- Durso FT, Kazi S, & Ferguson AN (2014). The Threat-Strategy Interview. Applied Ergonomics. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/25258275. doi: 10.1016/j.apergo.2014.08.001 [DOI] [PubMed]
- Ferneley EH, & Sobreperez P (2006). Resist, comply or workaround? An examination of different facets of user engagement with information systems. European Journal of Information Systems, 15(4), 345–356. [Google Scholar]
- Friedman A, Crosson JC, Howard J, Clark EC, Pellerano M, Karsh BT, … Cohen DJ (2014). A typology of electronic health record workarounds in small-to-medium size primary care practices. Journal of the American Medical Informatics Association, 21(e1), e78–e83. doi: 10.1136/amiajnl-2013-001686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halbesleben JRB, Savage GT, Wakefield DS, & Wakefield BJ (2010). Rework and workarounds in nurse medication administration process: Implications for work processes and patient safety. Health Care Management Review, 35(2), 124–133. [DOI] [PubMed] [Google Scholar]
- Halbesleben JRB, Wakefield DS, & Wakefield BJ (2008). Work-arounds in health care settings: Literature review and research agenda. Health Care Management Review, 33(1), 2–12. Retrieved from <Go to ISI>://000251920800002. [DOI] [PubMed] [Google Scholar]
- Holden RJ, Carayon P, Gurses AP, Hoonakker P, Hundt AS, Ozok AA, & Rivera-Rodriguez AJ (2013). SEIPS 2.0: A human factors framework for studying and improving the work of healthcare professionals and patients. Ergonomics, 56(11), 1669–1686. Retrieved from 10.1080/00140139.2013.838643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holden RJ, Rivera-Rodriguez AJ, Faye H, Scanlon MC, & Karsh B (2013). Automation and adaptation: Nurses’ problem-solving behavior following the implementation of bar coded medication administration technology. Cognition, Technology & Work, 15(3), 283–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollnagel E, Woods DD, & Leveson N (Eds.). (2006). Resilience Engineering - Concepts and Precepts. Burlington, VT: Ashgate. [Google Scholar]
- Hoonakker PL, Carayon P, McGuire K, Khunlertkit A, Wiegmann DA, Alyousef B, … Wood KE (2013). Motivation and job satisfaction of Tele-ICU nurses. Journal of Critical Care, 28(3), 315 e313–315 e321. doi:S0883–9441(12)00328–0 [pii] 10.1016/j.jcrc.2012.10.001 [doi] [DOI] [PubMed] [Google Scholar]
- Kianfar S, Carayon P, Hundt AS, & Hoonakker P (2014). Understanding care coordination for chronically ill patients. In The Human Factors and Ergonomics Society (Ed.), Proceedings of the Human Factors and Ergonomics Society Annual Meeting (pp. 170–174). Santa Monica, CA: The Human Factors and Ergonomics Society. [Google Scholar]
- Koppel R, Wetterneck T, Telles JL, & Karsh B-T (2008). Workarounds to barcode medication administration systems: Their occurrences, causes, and threats to patient safety. Journal of the American Medical Informatics Association, 15, 408–423. Retrieved from http://www.jamia.org/cgi/content/abstract/M2616v1 doi: 10.1197/jamia.M2616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus RS, & Folkman S (1984). Stress, Appraisal and Coping. New York: Springer. [Google Scholar]
- Li Y, Carayon P, Hundt AS, Kianfar S, Hoonakker P, Salek D, & Tomcavage J (2014). Levels of strategies used by care managers to deal with health IT-related barriers. In Broberg O, Fallentin N, Hasle P, Jensen PL, Kabel A, Larsen ME, & Weller T (Eds.), Human Factors in Organizational Design and Management - XI (pp. 469–473). [Google Scholar]
- Maeng DD, Graf TR, Davis DE, Tomcavage J, & Bloom FJ (2012). Can a patient-centered medical home lead to better patient outcomes? The quality implications of Geisinger’s ProvenHealth Navigator. American Journal of Medical Quality, 27(3), 210–216. Retrieved from http://ajm.sagepub.com/content/27/3/210.abstract. [DOI] [PubMed] [Google Scholar]
- Maliski SL, Clerkin B, & Litwin MS (2004). Describing a nurse case manager intervention to empower low-income men with prostate cancer. Oncology Nursing Forum, 31(1), 57–64. Retrieved from 10.1188/04.ONF.57–64 http://ezproxy.library.wisc.edu/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=c9h&AN=11913816&site=ehost-live. [DOI] [PubMed] [Google Scholar]
- McDonald KM, Sundaram V, Bravata DM, Lewis R, Lin N, Kraft SA, … Owens DK (2007). Closing the quality gap: A critical analysis of quality improvement strategies (Vol. 7: care coordination; ). Rockville MD. [PubMed] [Google Scholar]
- Mount-Campbell AF, Evans KD, Woods DD, Chipps EM, Moffatt-Bruce SD, & Patterson ES (2019). Value and usage of a workaround artifact: A cognitive work analysis of “brains” use by hospital nurses. Journal of Cognitive Engineering and Decision Making, 0(0), 1555343418825429 Retrieved from https://journals.sagepub.com/doi/abs/10.1177/1555343418825429. doi: 10.1177/1555343418825429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Novak LL, Holden RJ, Anders SH, Hong JY, & Karsh BT (2013). Using a sociotechnical framework to understand adaptations in health IT implementation. International Journal of Medical Informatics, 82(12), e331–e344. doi:S1386–5056(13)00020–8 [pii] 10.1016/j.ijmedinf.2013.01.009 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliva NL (2010). A closer look at nurse case management of community-dwelling older adults: Observations from a longitudinal study of care coordination in the chronically Ill. Professional Case Management, 15(2), 90–100. Retrieved from http://journals.lww.com/professionalcasemanagementjournal/Fulltext/2010/03000/A_Closer_Look_at_Nurse_Case_Management_of.8.aspx. [DOI] [PubMed] [Google Scholar]
- Patterson ES (2018). Workarounds to intended use of health information technology: A narrative review of the human factors engineering literature. Human Factors, 60(3), 281–292. Retrieved from http://journals.sagepub.com/doi/abs/10.1177/0018720818762546. doi: 10.1177/0018720818762546 [DOI] [PubMed] [Google Scholar]
- Ratwani RM, Reider J, & Singh H (2019). A decade of health information technology usability challenges and the path forward. JAMA. Retrieved from 10.1001/jama.2019.0161. doi: 10.1001/jama.2019.0161 [DOI] [PubMed] [Google Scholar]
- Smith MJ, & Carayon-Sainfort P (1989). A balance theory of job design for stress reduction. International journal of industrial ergonomics, 4(1), 67–79. [Google Scholar]
- Steele GD, Haynes JA, Davis DE, Tomcavage J, Stewart WF, Graf TR, … Shikles J (2010). How Geisinger’s advanced medical home model argues the case for rapid-cycle innovation. Health Affairs, 29(11), 2047–2053. doi:29/1½047 [pii] 10.1377/hlthaff.2010.0840 [doi] [DOI] [PubMed] [Google Scholar]
- Tucker AL (2004). The impact of operational failures on hospital nurses and their patients. Journal of Operations Management, 22(2), 151–169. [Google Scholar]
- Tucker AL, & Edmondson AC (2003). Why hospitals don’t learn from failures: Organizational and psychological dynamics that inhibit system change. California Management Review, 45(2), 55–72. [Google Scholar]
- Tucker AL, Edmondson AC, & Spear S (2002). When problem solving prevents organizational learning. Journal of Organizational Change Management, 15(2), 122–137. [Google Scholar]
- Tucker AL, & Spear SJ (2006). Operational failures and interruptions in hospital nursing. Health Services Research, 41(3 Part 1), 643–662. Retrieved from http://www.blackwell-synergy.com/doi/abs/10.1111/j.1475-6773.2006.00502.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyre MJ, & Orlikowski WJ (1994). Windows of opportunity: Temporal patterns of technological adaptation in organizations. ORGANIZATION SCIENCE, 5(1), 98–188. [Google Scholar]
- Vicente KJ, Roth EM, & Mumaw RJ (2001). How do operators monitor a complex, dynamic work domain? The impact of control room technology. International Journal of Human-Computer Studies, 54(6), 831–856. doi: 10.1006/ijhc.2001.0463 [DOI] [Google Scholar]