Abstract
Background:
Lorcaserin is a modestly selective agonist for 2C serotonin receptors (5-HT2CR) approved for weight-loss therapy. This class can attenuate cue-induced responding and drug taking in preclinical studies, but effects in humans have not been reported.
Methods and Participants:
We evaluated effects of single 10 mg doses of lorcaserin on the subjective and reinforcing effects of cocaine, using a randomized, double-blind, within-subject, cross-over design. Male, non-treatment-seeking, regular cocaine users received either single doses of oral placebo (n = 9) or lorcaserin (n = 9), followed by low- or high- doses of intravenous cocaine (0.23 or 0.46 mg/kg-injection). They were then allowed to self-administer the lower dose of cocaine.
Results:
Cocaine was well tolerated after lorcaserin pretreatment. Oral lorcaserin did not modify the number of cocaine injections self-administered. However, it prolonged the time over which participants made intravenous choices relative to the duration of monetary (cash) decisions. Lorcaserin increased ratings of ‘high’ and ‘stimulated’ after low-dose cocaine or vehicle, but decreased craving for cocaine after intravenous vehicle. It also caused small but significant increases in heart rate following noncontingent injections of intravenous placebo or cocaine. When active cocaine was self-administered, lorcaserin decreased heart rate after selection of a monetary choice, but increased it following an intravenous choice.
Conclusions:
Combined treatment with cocaine and lorcaserin was safe in a limited number of subjects, but did not diminish cocaine-motivated behavior or drug-induced ‘high’. Some positive subjective effects of cocaine were enhanced by lorcaserin, and it delayed intravenous choices and decreased craving under some conditions. Effects on heart rate depended on the type of reinforcer being self-administered.
Trial Registration:
clinicaltrials.gov Identifier, NCT02680288
Keywords: Cocaine-Related Disorders, Dose-Response Relationship, Drug Interactions, Infusions, Intravenous, Self-Administration, Serotonin Receptor Agonists
Introduction
Cocaine use disorders are an important health problem in the United States, causing significant medical, mental health, and social problems [1]. Although a wide variety of different potential therapeutic classes have been evaluated, no drugs are currently approved for relapse prevention after cocaine abuse or dependence. Serotonin (5-HT or 5-hydroxytryptamine) is one of three monoamine neurotransmitters that play important roles in affect and goal-directed behaviors. Type 2C serotonin receptors (5-HT2CR) exert complex actions on limbic neurons, playing a role in both dopamine release and drug-motivated behaviors.
Lorcaserin is a modestly selective agonist for 5-HT2CR receptors approved by the FDA for weight-loss therapy [2]. This class can attenuate cue-induced responding and drug taking in preclinical studies [3], but effects in humans have not been reported. Lorcaserin is marketed at a dose of 10 mg twice daily in patients with a medical indication for weight loss, such as diabetes or heart disease. Supratherapeutic doses are associated with both ‘high’ and negative subjective effects in liability testing, leading it to be classified as Drug Enforcement Administration schedule IV [4].
Given that lorcaserin is currently clinically available, well-tolerated in humans, and can modify psychostimulant-motivated behavior in animals [5,6]; its potential as a treatment for cocaine use is of interest. Although lorcaserin is currently approved for chronic use in patients with a medical indication for weight loss, supratherapeutic single doses can cause euphoria, hallucinations, and dissociation reactions in humans [4]. There is no data currently available on the potential interaction of lorcaserin and cocaine in humans. Because both agents potentiate serotonergic function, combined dosing may cause the serotonin syndrome. In addition, there may be unanticipated effects of combined dosing. To mitigate potential toxicity, single rather than multiple daily doses of lorcaserin were evaluated in the current study for their effects on cocaine-reinforced behavior, with comparison to monetary-reinforced responding. This approach is also justified by observations that single and multiple doses of lorcaserin have similar effects on cocaine-reinforced behavior in rhesus monkeys [5]. Based on findings of attenuated cocaine self-administration and reinstatement in rodents [7] and non-human primates [3], our hypothesis was that pretreatment with lorcaserin would decrease cocaine self-administration and craving in humans.
Materials and Methods
Participants
The protocol was performed under US Food and Drug Administration IND 117,990, Lorcaserin Treatment of Cocaine Abuse after approval by the Institutional Review Board of the Kansas City Veterans Affairs Medical Center. Subjects were recruited through word-of-mouth and advertisements posted in the community or on the internet. Those interested could receive a $20 stipend for each participant who was referred, for up to 10 potential subjects who met preliminary screening criteria. They were required to be current users of cocaine by rapid route (smoking or intravenous injection) and to supply a cocaine-positive urine collected within six weeks prior to dosing. Although women were not excluded, overnight arrangements were only sometimes available for females. All participants were not seeking medical treatment for cocaine abuse, did not have an active psychiatric condition, and had no clinically significant findings on physical exam. None of the participants had a history of asthma, cardiac disease, seizure disorders, or other medical condition that might make participation hazardous. Screening labs included blood counts, routine chemistry measures, urinalyses, and 12-lead electrocardiograms.
Study Design
A randomized, double-blind, double-dummy, placebo-controlled, within-subject, cross-over design was used to evaluate the safety of intravenous cocaine in participants receiving oral lorcaserin, as well as its effects on the subjective and reinforcing actions of cocaine in a laboratory setting. To prevent unauthorized drug use and allow better monitoring of adverse events, participants were observed during overnight admissions of 5 days duration. They received a stipend of $1,506 for completing the entire protocol.
Cocaine and the Study Medication
The study design is outlined in Table 1. Oral placebo was administered on Overnight Days 1, 2, and 4. These doses were known to be oral placebo to study personnel but not participants. To allow one day of observation and ensure washout of any potential illicit substances, intravenous treatments were initiated on Overnight Day 2. In order to be randomized to double-blind oral treatment, participants were required to report at least 20 mm of cocaine-induced ‘high’ and to self-administer at least two cocaine injections on Overnight Day 2. This ensured a baseline response to cocaine that could be reduced by treatment with the study medication. Double-blind lorcaserin (marketed as Belviq, 10 mg single oral doses) was administered on either Overnight Day 3 or 5 (only one active dose per subject). This design allowed participants to become experienced with laboratory procedures prior to receiving active oral treatment. Lorcaserin tablets were enclosed within size 00 capsules filled with microcrystalline cellulose, administered at approximately 9:00 AM, 20 minutes prior to the start of intravenous dosing. After dosing, electrocardiogram signals were continuously monitored, with blood pressure and heart rate checked at frequent intervals (1, 2, 4, 6, 8, 10, 15, 20, 30, 40, 50 minutes after intravenous dosing). Safety labs were repeated 7 hours after double-blind oral treatments, and included blood counts, routine chemistry measures, urinalyses, and 12-lead electrocardiograms. Participants returned three days after their final overnight day for a health status check.
Table 1.
Overview of the Study Design.
| Overnight Day | Oral Treatment | Intravenous Treatment | Objective |
|---|---|---|---|
| 1 | Placebo | None | First 24-hour washout, to ensure elimination of any medications that may have been taken prior to admission. |
| 2 | Placebo | Cocaine / Placeboa | Test if intravenous dosing tolerated. |
| 3 | Lorcaserin / Placebob | Cocaine / Placebob | First double-blind oral and intravenous dosing |
| 4 | Placebo | Cocaine / Placebob | Second 24-hour washout, to ensure elimination of Day 3 oral treatment. |
| 5 | Lorcaserin / Placebob | Cocaine / Placebob | Second double-blind oral and intravenous dosing |
To facilitate the evaluation of adverse events and the subjective effects of cocaine, study personnel but not participants were aware of cocaine dose.
Double-blind treatment.
Intravenous Self-Administration
The National Institute of Drug Abuse (Bethesda, MD) supplied cocaine hydrochloride which was delivered intravenously at a dose of 0.23 mg/kg in approximately 2.4 ml of saline over one minute using an Alaris 8015 interface and patient-controlled analgesia (PCA) module. A two-fold higher noncontingent dose was administered one hour later, by two activations of the PCA module. Participants were then offered six choices for additional injections of the lower dose or a monetary amount at 20-minute intervals. Active cocaine was administered in either the morning or afternoon, with this order reversed each day. Identical dosing with double-blind intravenous vehicle was administered at alternate times of day, with each different dose paired with a color that was unique across four days of intravenous dosing. This procedure allowed double-blind evaluation of injections that were noncontingent (0.00, 0.23, or 0.46 mg/kg of cocaine) or self-administered (0.00 or 0.23 mg/kg of cocaine) within one day. Although participants were required to distinguish between different sampling doses of cocaine, each was associated with a distinct color that was presented alongside questionnaires, allowing it to be readily identified. Individuals meeting inclusion criteria for the present study routinely described taking multiple consecutive doses of cocaine. Overall, repeated dosing in a laboratory setting allows a more efficient evaluation of cocaine dose and likely resembles its use in a recreational setting. Our design also facilitated more direct comparisons between oral treatments.
Responding on a computer mouse was used to select between intravenous and monetary choices, with five additional mouse clicks required to obtain either reinforcer. If no selection was completed within 2 minutes, the choice was withdrawn with neither reinforcer administered. In preliminary studies, we observed that drug-reinforced responding can be facilitated by limiting the availability of monetary reinforcement according to the amount of cocaine self-administered. Accordingly, amounts of cash offered were adjusted according the number of injections of a given dose that had been self-administered: $0.00 for 0 or 1 injections, $0.05 for 2, $0.50 for 3, $1 for 4, and $2 for 5 earned injections (corresponding to $0.20 to $2 if participants made at least 2 intravenous choices). To ensure participant safety, intravenous dosing was stopped after tachycardia exceeding 130 beats per minute (bpm) or blood pressure greater than 165 mm Hg systolic or 100 mm Hg diastolic.
Assessments
Subjective Drug Effects
Visual analogue scale (VAS) responses were recorded on a 100 mm scroll bar marked from 0 (‘not at all’) to 100 (‘extremely’) at baseline, 3, 6, 10, 15, and 20 minutes after intravenous dosing. Participants were asked to indicate ‘Do you feel ANY IV drug effects’, ‘Does the IV drug have any GOOD effects?’, ‘Does the IV drug have any BAD effects?’, ‘Do you feel STIMULATED from the IV drug?’ ‘How HIGH are you from the IV drug?’ Craving was assessed by asking participants to indicate ‘How much do you WANT TO USE cocaine?’ The Addiction Research Center Inventory (ARCI) was completed 20 minutes after each noncontingent dose, with responses subdivided into scales of 1.) Psychostimulant effects, the Amphetamine and Benzedrine Groups (BG); 2.) Euphoria, the Morphine-Benzedrine Group (MBG), 3.) Sedation, the Pentobarbital-Chlorpromazine-Alcohol Group (PCAG), and 4.) Somatic-dysphoric effects, the lysergic acid diethylamide (LSD) scale.
Cocaine Crossover Value
At 18 minutes after noncontingent doses, participants completed the Multiple Choice Questionnaire (MCQ), which involves a series of hypothetical choices between receiving a second intravenous dose or a series of monetary alternatives of increasing value [8]. The dollar amount at which participants switch from selecting drug to money is the crossover point. Values of $0.5, 1, 2, 4, 6, 10, 15, 20, 25, and 50 were offered.
Data Analysis
Based on preliminary studies, participants were expected to make approximately 5 out of 6 potential cocaine choices during self-administration sessions, with a standard deviation of 1.56 choices (31.2%) [9]. Accordingly, including approximately eight participants per group would be sufficient to provide greater than 72% power to detect a reduction in cocaine self-administration of 50% or more. Participants were randomized by block allocation to four different schedules (lorcaserin on day 3 and oral placebo on day 5 with cocaine in the morning or afternoon for both of these sessions [AA or AB, respectively], or lorcaserin on day 5 and oral placebo on day 3 with cocaine at the same time of day for both sessions [BA or BB, respectively]). A study pharmacist randomly assigned participants to different blocks and concealed the assignment from those recording clinical outcomes.
Primary measures were the number of cocaine injections self-administered, the magnitude of cocaine-induced ‘high’ measured by VAS, and the tolerability of combined lorcaserin and cocaine. Statistical analyses were performed by Systat Inc. software, using the Shapiro-Wilk test to evaluate for normality. Comparisons were made by analysis of variance (ANOVA), with oral dose (placebo or 10 mg of lorcaserin), and intravenous dose (0.0, 0.23, and 0.46 mg/kg of cocaine), and time (if available) as factors. Post hoc comparisons by a single factor were performed by ANOVA simple main effects. Otherwise, post hoc comparisons were performed by Bonferroni t-tests. Using the correction by Sidak [10] for a 40% correlation between interrelated areas, a type I error (alpha) value of 0.026 was applied in these instances. A value of p < 0.05 was used as a criterion for the significance of comparisons by ANOVA. Data on adverse events are presented descriptively.
To compare changes in cardiovascular measures during self-administration of cocaine, all responding in individual participants was averaged for a given category of oral dose (placebo or lorcaserin), intravenous dose (placebo or cocaine), and choice (intravenous or monetary). Comparisons were then made across group means of the averaged data, using oral dose, intravenous dose, and reinforcer type as factors.
Results
Participant Characteristics
During the initial lead-in intravenous dosing, two subjects were excluded because of elevated blood pressure values following cocaine that exceeded stopping criteria, one because of heart rate greater than stopping criteria, and two because they failed to self-administer at least two cocaine injections. An additional subject failed to tolerate cocaine due to nausea and lightheadedness during the lead-in and did not participate further.
As outlined in Table 2, nine male, cocaine-dependent volunteers between and 34 and 49 years of age provided written informed consent and completed the study. One additional participant failed to receive lorcaserin because of a pharmacy error, and another subject left early because of a family problem at home. In total, nine doses of oral placebo and nine doses of lorcaserin were administered under double-blind conditions. All of the nine participants who received lorcaserin met the DSM-V criteria for Cocaine Use Disorder and had ASI values indicating clinically-significant disorders.
Table 2.
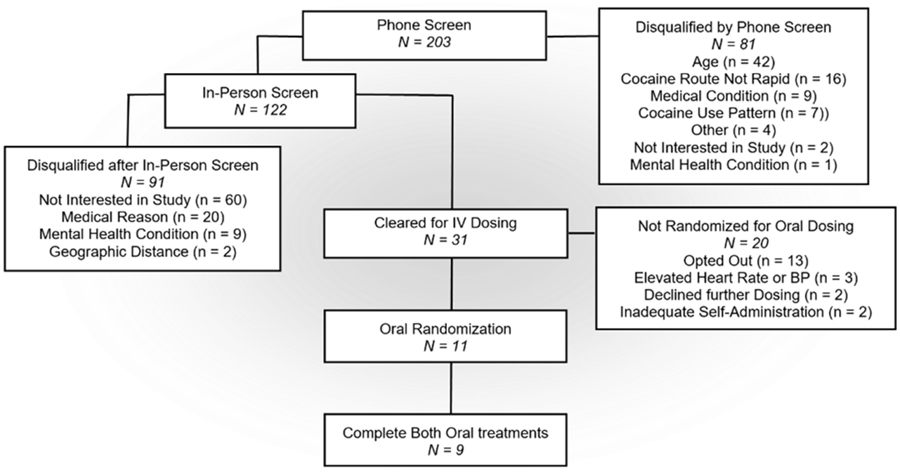
Participant Recruitment and Demographics. The upper flow chart shows results of multi-stage screening of potential subjects using telephone interviews, in-person exams, and intravenous dosing. Demographics of the nine male subjects who received both oral treatments are shown below. ‘?’ describes subjects who received cocaine without purchasing. The randomly assigned order of oral dosing with placebo and lorcaserin is shown in the last column.
 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Number | Racea | Age (years) | Education (years) |
Cocaine Use Daysb |
Years Since First Use |
Cocaine ($ / week) |
Cigarettes (packs / week) |
Drugc | Mental Healthlc |
Familyc | Oral Dose (mg)e |
| 242 | W | 48 | 13 | 20 | 15 | ?d | 4 | 0.269 | 0.091 | 0.329 | 10, 0 |
| 250 | AA | 42 | 10 | 16 | 20 | 1,600 | 20 | 0.058 | 0.000 | 0.282 | 10, 0 |
| 255 | AA | 37 | 13 | 15 | 9 | 600 | 2 | 0.241 | 0.000 | 0.000 | 0, 10 |
| 262 | AA | 37 | 12 | 10 | 6 | ?d | 1 | 0.031 | 0.000 | 0.025 | 10, 0 |
| 264 | AA | 45 | 12 | 15 | 8 | 100 | 3 | 0.131 | 0.000 | 0.000 | 0, 10 |
| 282 | AA | 34 | 10 | 20 | 10 | 150 | 7 | 0.092 | 0.023 | 0.225 | 0, 10 |
| 287 | AA | 41 | 14 | 12 | 6 | 100 | 2 | 0.021 | 0.000 | 0.000 | 10, 0 |
| 289 | AA | 37 | 14 | 20 | 15 | 200 | 6 | 0.182 | 0.000 | 0.000 | 0, 10 |
| 290 | W | 49 | 20 | 20 | 29 | 2,000 | 7 | 0.128 | 0.148 | 0.147 | 0, 10 |
| 2-W7-AA | 41.1±1.67 | 13.1±0.94 | 16.4±1.20 | 13.1±1.98 | 679±224 | 5.78±1.59 | 0.128±0.029 | 0.029±0.017 | 0.112±0.043 | ||
Race: AA (African American), W (Caucasian)
Days of drug use over the last 30 days
Addiction Severity Index composite rating
Not purchasing cocaine
Randomization order is shown left to right
Tolerability of the Study Medication
After receiving oral placebo and cocaine during his second double-blind session, subject 250 became agitated and asked to discontinue participation. Following reassurance, he completed all remaining procedures without incident. Participant 262 reported self-limited gastrointestinal distress with an increased frequency of bowel movements on the evening after receiving oral placebo and cocaine. After receiving lorcaserin and low-dose cocaine, participant 282 had a brief period of mild chest discomfort and eructation.
Cocaine Self-Administration
Numbers of injections chosen during self-administration are shown in Table 3. When intravenous cocaine was available, participants self-administered a greater number of drug injections but fewer monetary reinforcers [F(1, 32) = 11.4 & 9.47, p < 0.02 for either]. Lorcaserin treatment did not modify either cocaine- or monetary- reinforcement [F(1, 32) = 0.27 & 0.46, p > 0.05 for either].
Table 3.
Cocaine Self-Administration during Double-Blind Sessions. Group means and standard error are show for 9 participants who self-administered intravenous placebo and cocaine after both oral placebo and lorcaserin.
| Intravenous Treatment | Oral Treatment | Number or Rein forcers SelfAdministered | |||
|---|---|---|---|---|---|
| Intravenous | Money | ||||
| Placebo | Placebo | 2.00 (0.70) | 3.67 (0.72) | ||
| Lorcaserin | 1.78 (0.73) | 4.11 (0.71) | |||
| Cocaine | Placebo | 4.67 (0.59) | * | 1.33 (0.59) | * |
| Lorcaserin | 4.11 (0.76) | 1.89 (0.76) | |||
Indicates a significant effect of cocaine compared to intravenous placebo, p < 0.01.
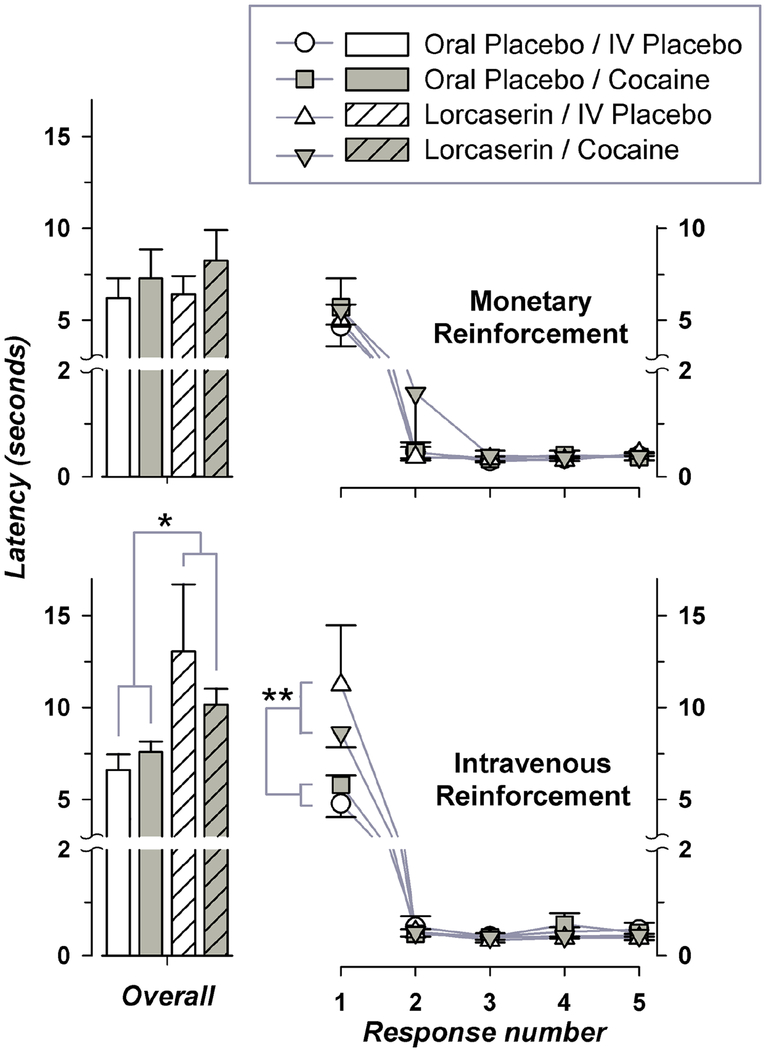
Participants responded more slowly on their first mouse click which initiated either an intravenous or monetary choice, with response rate increasing over subsequent responding (Figure 1). When an intravenous choice was made, overall latency and latency for the first mouse click varied significantly with oral dose (F(1, 22) = 6.61 & 8.80, p < 0.02 for either), but not intravenous dose or the interaction of lorcaserin and cocaine doses. In contrast, latency across monetary choices did not vary significantly with oral dose, intravenous dose, or their interaction. When collapsed across intravenous treatments, active lorcaserin increased overall response latency and latency for the first mouse click when participants were responding for intravenous but not monetary choices. Latency for an initial click to choose intravenous reinforcement was 5.40 ± 0.45 and 9.63 ± 1.38 seconds following oral placebo and lorcaserin, respectively. This corresponded to a prolongation of greater than four seconds after active oral treatment.
Figure 1.
Response Latency during Cocaine Self-Administration. Latency is shown on vertical axes both as overall values to complete five clicks on a computer mouse, and values associated with each individual mouse click, plotted horizontally. Responding during monetary and intravenous reinforcement is shown on the upper and lower graphs, respectively. Group means with standard error are shown for 5 to 9 participants per condition. * indicates a significant simple main effect of lorcaserin, with one and two symbols corresponding to p < 0.03 and p < 0.01, respectively.
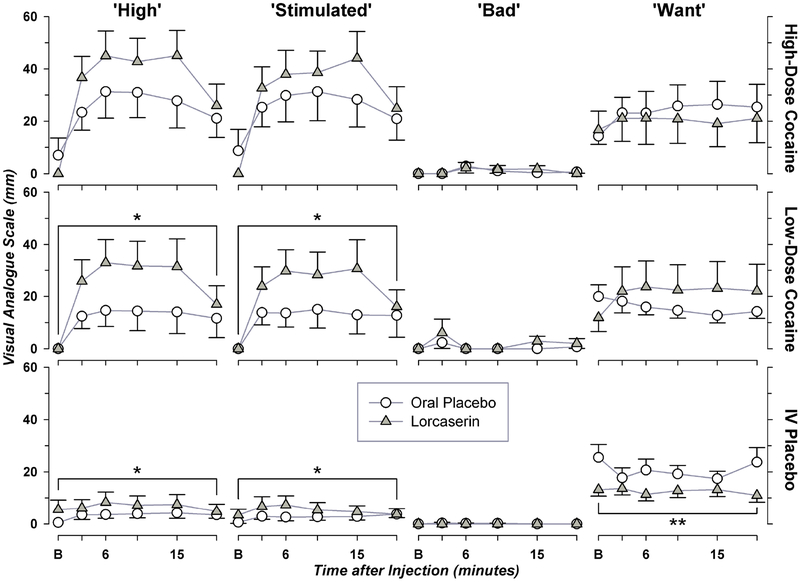
Subjective Effects
Effects of cocaine and lorcaserin on different VAS items are shown in Figure 2. Cocaine produced dose-related increases in ‘High’, ‘Stimulated’, and ‘Good Drug’ ratings [F(2, 396) = 53.8, 56.3, & 40.0; p < 0.001 for all]. Each of these measures varied significantly with oral treatment [F(1, 396) = 16.9, 10.3, & 12.5; p < 0.01 for all]. Treatment with lorcaserin increased all three ratings in participants receiving intravenous placebo, with values for ‘High’ and ‘Stimulated’ also increased by approximately two-fold after low-dose cocaine. In contrast, lorcaserin treatment decreased craving following intravenous placebo [F(1, 214) = 15.8, p < 0.001] but not either dose of cocaine.
Figure 2.
Lorcaserin modifies Visual-Analogue Measures. Participants used a computer mouse to endorse cocaine-induced ‘High’ or other subjective effects, shown on vertical axes. Time after intravenous injection is plotted horizontally. Group means with standard error are shown after treatment with oral placebo (n = 9) or 10 mg of lorcaserin (n = 9). For either oral treatment, each participant received two injections of intravenous placebo and a single injection of low- and high- dose cocaine. * indicates a significant effect of lorcaserin, with 1 and 2 symbols corresponding to p < 0.05 and p < 0.001 by simple main effects.
Injection value measured by the Multiple Choice Questionnaire as well as ratings of ‘Any’ and ‘Bad’ drug effects by VAS varied significantly with dose of cocaine [F(2, 66) = 17.3, p < 0.001; F(2, 396) = 54.3 & 4.47; p < 0.02 for either] but not lorcaserin. As we have previously reported [11], cocaine produced dose-related increases the ARCI morphine-benzedrine subscale [F(2, 66) = 4.39, p < 0.02]. However, there is no effect of lorcaserin on this measure. For most VAS measures, ANOVA showed significant main effects of time.
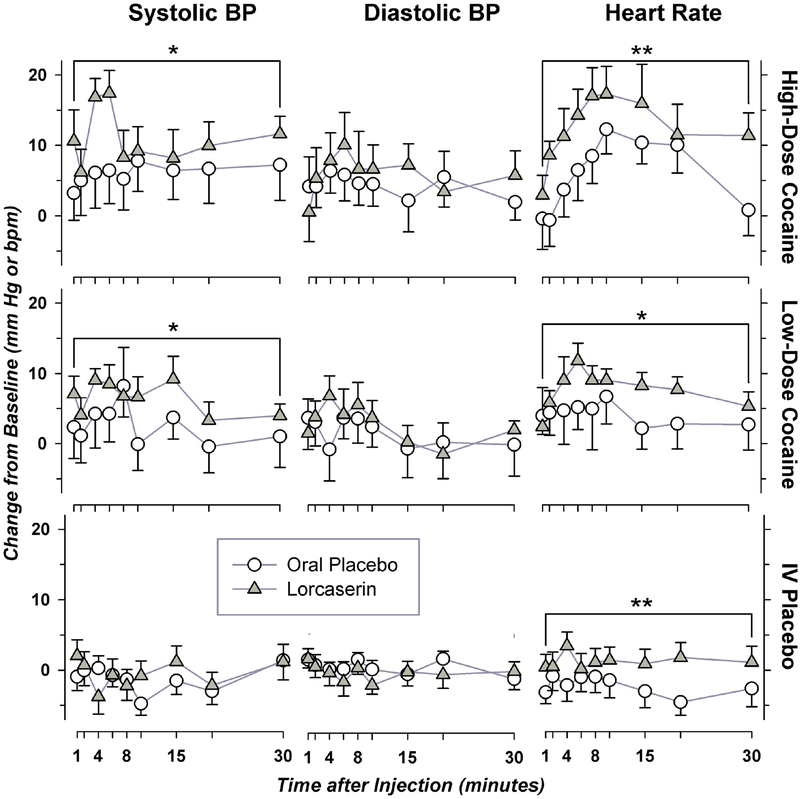
Cardiovascular Measures
ANOVA revealed significant effects of lorcaserin treatment on heart rate and systolic blood pressure [F(1, 594) = 14.4 & 27.9; p < 0.001 for either] (Figure 3). Treatment with lorcaserin potentiated cocaine-induced increases in systolic blood pressure, and also caused small but significant increases in heart rate after noncontingent intravenous placebo or cocaine.
Figure 3.
Cardiovascular Measures after Treatment with Noncontingent Cocaine and Lorcaserin. Group means with standard error for absolute change in blood pressure (mm Hg) and heart rate (beats per minute) after noncontingent cocaine are shown following treatment with oral placebo (n = 9) or lorcaserin (n = 9). * indicates a significant effect of lorcaserin, with 1 and 2 symbols corresponding to p < 0.05 and p < 0.001 by simple main effects.
During self-administration, both systolic and diastolic blood pressure varied significantly with cocaine dose and its interaction with lorcaserin treatment [F(1, 315) = 7.00 & 5.12, p < 0.03 for either]. Treatment with lorcaserin increased both measures during self-administration of cocaine but not intravenous placebo (data not shown).
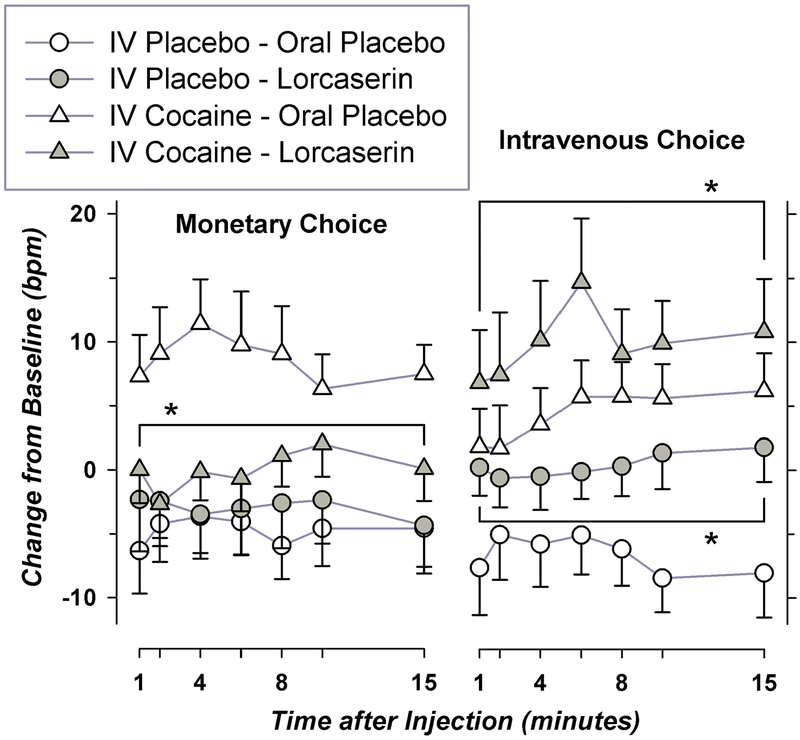
As shown in Figure 4, heart rate during self-administration varied significantly with cocaine dose (0 or 0.23 mg/kg-injection) and its interaction with lorcaserin dose and type of reinforcement [F(1, 315) = 4.91, p < 0.03]. Effects of lorcaserin on heart rate depended on the type of reinforcer chosen and whether active or placebo cocaine was being self-administered. Lorcaserin treatment decreased heart rate after a monetary choice when active cocaine was being self-administered, but increased it after participants selected either intravenous placebo or cocaine. No participant met stopping criteria because of increased blood pressure or heart rate.
Figure 4.
Effects of Lorcaserin and Cocaine on Heart during Self-Administration. Values after monetary and intravenous choices are shown on the left- and right- graphs, respectively. Group means with standard error for absolute change in heart rate (beats per minute) after cocaine self-administration are shown for 5 to 9 participants per condition. * indicates a significant effect of lorcaserin corresponding to p < 0.001.
Discussion
In the present study, active oral treatment with lorcaserin did not decrease either cocaine self-administration or drug-induced ‘high’. Given its negative effects on primary measures, secondary outcome variables were analyzed. We found that lorcaserin treatment delayed early decisions to choose intravenous but not alternative reinforcers, while decreasing craving after intravenous placebo. Delayed responding occurred as participants evaluated a specific color previously paired with noncontingent injections. Lorcaserin did not modify subsequent responding as subjects completed the required four additional mouse clicks. That responding was made rapidly, apparently with minimal further consideration. Previous work has shown that non-intuitive decisions which require greater effort and deliberate reasoning are more prolonged [12,13]. Because lorcaserin potentiated the positive subjective properties of low-dose cocaine and intravenous placebo, motivation for drug may have declined as drug craving was satiated. If so, this may have slowed responding for drug injections as respondents required more effort to evaluate their internal state. Even so, the overall number of cocaine injections chosen by participants was not altered by lorcaserin pretreatment.
Activation of 5-HT2CRs appears to biphasically modulate release of dopamine in brain reward regions. Cocaine-induced dopamine release in the nucleus accumbens shell is increased by delivery of a 5-HT2CR agonist to that brain region at a low dose [14], but attenuated after a higher dose; with opposite effects after treatment with a 5-HT2CR antagonist [15]. Although systemic delivery of 5-HT2CR agonists decreases extracellular dopamine in the nucleus accumbens [16], microinjection to the medial prefrontal cortex augments accumbal dopamine [17]. Biphasic effects of 5-HT2CRs on dopaminergic tone may underlie different effects of lorcaserin in humans and animals. Lorcaserin administered in the present study at a relatively low, clinically relevant-dose on the order of 0.14 mg/kg may have modestly increased accumbal dopaminergic tone, augmenting the positive subjective effects of vehicle or low-dose cocaine. This is consistent with a previous report of dose-related increases drug-induced ‘High’ after supratherapeutic doses of lorcaserin [4]. Although we did not observe an increase in self-administration, this may occur after a lower, otherwise ineffective dose of cocaine.
Preclinical studies have shown that lorcaserin doses of 0.6 mg/kg or more decrease cocaine self-administration in rats [7] or monkeys [5,18,19], with 0.3 mg/kg or greater attenuating cue- or drug- induced reinstatement [7]. These relatively high doses of lorcaserin likely diminish dopaminergic tone in reward regions [16]. When rhesus monkeys responded under a progressive-ratio schedule, intragastric lorcaserin also attenuated self-administration of 0.010 to 0.100 mg/kg-injection of cocaine, but not 0.320 mg/kg-injection [6]. Given these results, a relatively low 0.23 mg/kg-injection dose of cocaine was chosen for the present study. Because the subjective effects of cocaine doses less than 0.23 mg/kg-injection are not easily identified by most participants, lower doses were not evaluated. We also found that lorcaserin decreased craving after intravenous vehicle, with no effect on this measure following different doses of cocaine. It is unclear how this finding relates lorcaserin’s actions in preclinical models of reinstatement, but it would appear more closely linked to cue- rather than drug- induced responding.
We found that lorcaserin caused small but significant increases in the heart rate of participants receiving noncontingent injections of intravenous placebo or cocaine, while augmenting cocaine-induced increases in systolic blood pressure. No significant effects on diastolic blood pressure were observed. In patients using lorcaserin for management of obesity, decreased blood pressure has been reported, with no effect on heart rate [2]. Therefore, effects on cardiovascular measures in the present study may be due to specific characteristics of our subjects, such as expectations of stimulant reward. Consistent with this, lorcaserin increased heart rate after intravenous self-administration of vehicle or cocaine, but caused decreases following selection of a monetary choice while participants were self-administering active cocaine.
Combined treatment with cocaine and lorcaserin appears to be safe, based on evaluation of a limited number of subjects. Because of nonselective decreases in operant responding and its failure to decrease cocaine-versus-food choice in rhesus monkeys, Banks et al. [18] suggested that lorcaserin is unlikely to have clinical utility for treatment of cocaine use disorders. Studies in rodents have shown that lorcaserin diminished opioid self-administration only at doses well above those used clinically [20]. Our own findings also do not support a direct therapeutic benefit on drug-reinforced behavior for the currently marketed dose of lorcaserin. Even so, this dose did selectively slow responding that preceded intravenous choices, implying that greater effort was expended during drug-taking decisions. Decreased craving in participants receiving intravenous placebo could also translate into a therapeutic benefit in abstinent individuals. On the other hand, lorcaserin increased the positive subjective effects of cocaine on some VAS measures.
Cocaine produces robust cardiovascular and subjective effects that can be readily detected in relatively small panels of participants in a laboratory setting [21,22]. Based on an initial power analysis outlined above, sample size for the present study was adequate. Nonetheless, relatively few participants were evaluated with a large number of measures included. Only males were included, with most participants being of African American race. Lorcaserin is rapidly absorbed, reaching peak plasma concentrations within 2 hours of dosing [23]. Initial measures following injections of low-dose cocaine in the present study preceded peak concentrations of lorcaserin. Nonetheless, lorcaserin clearly modified the subjective and cardiovascular effects of low-dose cocaine within 30 minutes of oral dosing, consistent with its rapid effects after supratherapeutic doses in a previous study [4]. Lorcaserin accumulates to approximately 30% higher plasma concentrations after chronic dosing [24], which may have decreased its effects in the present single-dose study relative to chronic dosing. Because our participants were non-treatment seeking, we cannot exclude a therapeutic value on drug taking in patients who are motivated to avoid cocaine use. Further study is needed to determine whether effects of lorcaserin treatment will translate into a clinical benefit in cocaine use disorders.
Conclusions
Double-blind treatment with oral lorcaserin did not decrease primary measures of drug taking and cocaine-induced ‘high’. Changes in secondary outcomes after active treatment included a prolongation of operant responding for intravenous reinforcement and increases in drug-induced ‘high’ and ‘stimulated’ after low-dose cocaine. Pretreatment with lorcaserin augmented cocaine-induced elevations of systolic blood pressure and had complex context-dependent effects on heart rate.
Highlights.
Lorcaserin is a modestly selective agonist for 2C serotonin receptors (5-HT2CR)
It can attenuate drug taking in animals, but effects in humans are unknown
Non-treatment-seeking regular cocaine users received single 10 mg doses of lorcaserin
Neither cocaine self-administration nor ‘high’ were decreased by lorcaserin
Lorcaserin delayed operant responding and diminished craving under some conditions
Acknowledgements
This study was supported by grant R21-DA037556 issued to KG by the National Institutes of Health, Institute on Drug Abuse, Bethesda, MD 20892; and grant 589-KG-0012 issued to KG by the Medical Research Service, Department of Veterans Affairs, Washington, DC, 20420. Neither funding agency was involved in the design of this study. We appreciate editorial assistance by Edward Anselm, MD.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
All authors declare that they have no conflict of interest pertaining to this manuscript.
This protocol followed all applicable regulations for protection of human subjects as outlined by the United States Department of Health & Human Services, including the Food and Drug Administration; and was approved by our local Institutional Review Board.
References
- [1].Center for Behavioral Health Statistics and Quality. Behavioral health trends in the United States: results from the 2014 National Survey on Drug Use and Health. HHS Publication No. SMA 15–4927 ed. Substance Abuse and Mental Health Services Administration; 2015. [Google Scholar]
- [2].Chan EW, He Y, Chui CS, Wong AY, Lau WC, Wong IC. Efficacy and safety of lorcaserin in obese adults: a meta-analysis of 1-year randomized controlled trials (RCTs) and narrative review on short-term RCTs. Obes Rev 2013;14:383–92. [DOI] [PubMed] [Google Scholar]
- [3].Collins GT, Gerak LR, France CP. The behavioral pharmacology and therapeutic potential of lorcaserin for substance use disorders. Neuropharm 2018;142:63–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Shram MJ, Schoedel KA, Bartlett C, Shazer RL, Anderson CM, Sellers EM. Evaluation of the abuse potential of lorcaserin, a serotonin 2C (5-HT2C) receptor agonist, in recreational polydrug users. Clin Pharmacol Ther 2011;89:683–92. [DOI] [PubMed] [Google Scholar]
- [5].Collins GT, Gerak LR, Javors M, France CP. Lorcaserin reduces the discriminative stimulus and reinforcing effects of cocaine in rhesus monkeys. J Pharmacol Exp Ther 2015;356:85–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Gerak LR, Collins GT, France CP. Effects of lorcaserin on cocaine and methamphetamine self-administration and reinstatement of responding previously maintained by cocaine in Rhesus monkeys. J Pharmacol Exp Ther 2016;359:383–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Harvey-Lewis C, Li Z, Higgins GA, Fletcher PJ. The 5-HT receptor agonist lorcaserin reduces cocaine self-administration, reinstatement of cocaine-seeking and cocaine induced locomotor activity. Neuropharm 2015;101:237–45. [DOI] [PubMed] [Google Scholar]
- [8].Griffiths RR, Troisi JR, Silverman K, Mumford GK. Multiple-choice procedure: an efficient approach for investigating drug reinforcement in humans. Behav Pharmacol 1993;4:3–13. [PubMed] [Google Scholar]
- [9].Walsh SL, Geter-Douglas B, Strain EC, Bigelow GE. Enadoline and butorphanol: evaluation of kappa-agonists on cocaine pharmacodynamics and cocaine self-administration in humans. J Pharmacol Exp Ther 2001;299:147–58. [PubMed] [Google Scholar]
- [10].Sankoh AJ, Huque MF, Dubey SD. Some comments on frequently used multiple endpoint adjustment methods in clinical trials. Stat Med 1997;16:2529–42. [DOI] [PubMed] [Google Scholar]
- [11].Grasing K, Mathur D, Newton TF, DeSouza C. Donepezil treatment and the subjective effects of intravenous cocaine in dependent individuals. Drug Alcohol Depend 2010;107:69–75. [DOI] [PubMed] [Google Scholar]
- [12].Kahneman D A perspective on judgment and choice: mapping bounded rationality. Am Psychol 2003;58:697–720. [DOI] [PubMed] [Google Scholar]
- [13].Thinking Kahneman D., Fast and Slow. New York: Farrar, Straus and Giroux; 2011. [Google Scholar]
- [14].Navailles S, Moison D, Cunningham KA, Spampinato U. Differential regulation of the mesoaccumbens dopamine circuit by serotonin2C receptors in the ventral tegmental area and the nucleus accumbens: an in vivo microdialysis study with cocaine. Neuropsychopharm 2008;33:237–46. [DOI] [PubMed] [Google Scholar]
- [15].De DP, Navailles S, Berg KA, Clarke WP, Spampinato U. Constitutive activity of the serotonin2C receptor inhibits in vivo dopamine release in the rat striatum and nucleus accumbens. J Neurosci 2004;24:3235–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Browne CJ, Ji X, Higgins GA, Fletcher PJ, Harvey-Lewis C. Pharmacological modulation of 5-HT2C receptor activity produces bidirectional changes in locomotor activity, responding for a conditioned reinforcer, and mesolimbic DA Release in C57BL/6 mice. Neuropsychopharm 2017;42:2178–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Leggio GM, Cathala A, Moison D, Cunningham KA, Piazza PV, Spampinato U. Serotonin2C receptors in the medial prefrontal cortex facilitate cocaine-induced dopamine release in the rat nucleus accumbens. Neuropharm 2009;56:507–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Banks ML, Negus SS. Repeated 7-day treatment with the 5-HT2C agonist lorcaserin or the 5-HT2A antagonist pimavanserin alone or in combination fails to reduce cocaine vs food choice in male rhesus monkeys. Neuropsychopharm 2017;42:1082–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Gannon BM, Sulima A, Rice KC, Collins GT. Inhibition of cocaine and 3,4-methylenedioxypyrovalerone (MDPV) self-administration by lorcaserin is mediated by 5-HT2C receptors in rats. J Pharmacol Exp Ther 2017;364:359–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Panlilio LV, Secci ME, Schindler CW, Bradberry CW. Choice between delayed food and immediate opioids in rats: treatment effects and individual differences. Psychopharmacology 2017;234:3361–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Lukas SE, Kouri EM, Rhee C, Madrid A, Renshaw PF. Effects of short-term citicoline treatment on acute cocaine intoxication and cardiovascular effects. Psychopharmacology 2001;157:163–7. [DOI] [PubMed] [Google Scholar]
- [22].Hart CL, Haney M, Vosburg SK, Rubin E, Foltin RW. Smoked cocaine self-administration is decreased by modafinil. Neuropsychopharm 2008;33:761–8. [DOI] [PubMed] [Google Scholar]
- [23].Pharmaceuticals Arena. FDA Briefing Document, NDA 22529, Lorcaserin. 2012.
- [24].Smith SR, Prosser WA, Donahue DJ, Morgan ME, Anderson CM, Shanahan WR. Lorcaserin (APD356), a selective 5-HT(2C) agonist, reduces body weight in obese men and women. Obesity (Silver Spring) 2009;17:494–503. [DOI] [PubMed] [Google Scholar]