Abstract
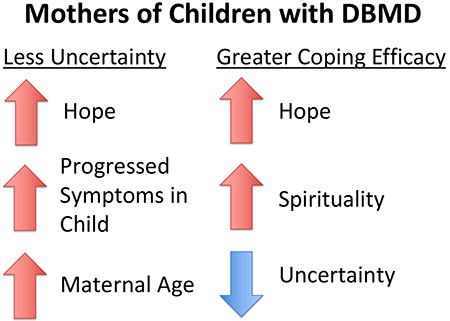
Uncertainty is a challenging aspect of caring for children with Duchenne/Becker Muscular Dystrophies (DBMD). Although uncertainty is often perceived as a state to be avoided, hope may influence caregivers’ perceptions of uncertainty as opportunity. The goal of this cross-sectional quantitative study was to pilot a novel measure of state-based hope, and test relationships among uncertainty, hope, spirituality, and coping efficacy in mothers of children with DBMD. Mothers (n=202) were recruited through DuchenneConnect, Parent Project Muscular Dystrophy, and Cincinnati’s Children Hospital. A one-component solution for the novel Parent Hope Scale explained 44.3% of the variance, and the measure demonstrated high internal consistency. Higher hope (p<0.001), further disease progression (p=0.042), and older mother’s age (p=0.001) were significantly associated with lower perceptions of uncertainty. Mothers reporting less hope (p<0.001), higher perceptions of uncertainty (p<0.001), and less spirituality (p=0.001) reported lower coping efficacy. As such, hope appears to be a key variable in shaping uncertainty appraisals and facilitating coping efficacy. While further research is needed, counseling aimed at bolstering hope, particularly among less-hopeful mothers, and interventions to reappraise uncertainty, may be helpful in promoting coping efficacy.
Keywords: Hope, Uncertainty, Coping Efficacy, Duchenne Muscular Dystrophy
Graphical Abstract
Introduction
Duchenne and Becker Muscular Dystrophy (DBMD) are rare, X-linked recessive, neuromuscular conditions characterized by progressive loss of muscle function. Duchene muscular dystrophy (DMD) presents in childhood, and although interventions aimed at preserving muscle function are increasing survival, death often occurs by the time patients reach their 30s. Becker muscular dystrophy (BMD) is generally milder with a later onset and less severe muscle weakness.1,2 Although the clinical course of most boys with DBMD follows a defined course of progressive deterioration, prognostic variability in these conditions still exists, particularly in the timing of loss of skills and lifespan. Parents’ psychological adaptation is affected by the inherent uncertainty in the progression of the condition, changing nature of caregiving, and the continual losses that these children and parents endure as the disease progresses.3
Research into sources of distress in pediatric chronic illnesses has yielded evidence that uncertainty is “probably the greatest single psychological stressor” faced by the patient and families.4 Uncertainty pervades many aspects of the illness experience and can arise from numerous factors, including prognostic and disease-course ambiguity.5 The persistent uncertainty described by parents of children with chronic and life-limiting medical conditions has been linked to several significant negative and positive outcomes for parents and families. Research has found that uncertainty can negatively affect parental coping and adaptation;6–8 and increase feelings of psychological distress, anxiety, depression, and hopelessness.9–11 Alternatively, parents have reported benefits to uncertainty, including recognizing that uncertainty allows for the possibility for positive outcomes for their child.6,9,11,12 This dichotomization of uncertainty appraisals is further elucidated by Mishel’s Uncertainty in Illness Theory. Mishel argued that uncertainty is classified as neutral until it has been appraised as either a danger or opportunity.13 Therefore, uncertainty is not always a state to be avoided or eliminated. It has been suggested that how an individual appraises uncertainty, in part, determines his or her ability to adapt to both the uncertainty and the stressor leading to it.14
A better understanding of factors that impact uncertainty appraisals can help healthcare providers who work with these families, such as genetic counselors, develop targeted interventions that enhance the adaptation process. Parental hope is one such factor.15,16 The concept of hope has been defined and operationalized in many ways and across a myriad of specialties.17 In the medical setting, hope and uncertainty have been shown to be fundamentally related. A meta-analysis of the hope experience among caregivers of persons with chronic conditions identified one theme as “dynamic possibilities within uncertainty.”16 Additionally, Dufault and Martocchio describe hope as situation and state-dependent and best understood within a context of uncertainty.18
Further, hope has been described as having therapeutic value by affecting coping, coping efficacy (defined as perceived ability to successfully cope), and adaptation in both caregivers and patients,15,19–22 but there is little evidence of the role of hope in influencing perceived uncertainty and the uncertainty appraisal process. One study reported that hope was significantly correlated with lower levels of perceived uncertainty in a population of cancer survivors.23 Additionally, greater uncertainty was associated with less hope and lower adaptation in caregivers of children with Down syndrome.8
Spirituality is another important factor associated with the wellbeing of parents caring for a child with an uncertain medical condition and has conceptual overlap with hope. A qualitative study on the hope experience of parents who have a child with a poor cancer prognosis describes spirituality as a significant facilitator of maintaining hope.24 Spiritual well-being has also been associated with less parental uncertainty.25
Our study contributes to this growing evidence by developing and assessing a novel parent hope scale and testing the relationships among uncertainty, hope, spirituality, and coping efficacy among mothers of children with DBMD.
Methods
This study was approved by the National Human Genome Research Institute IRB (Study ID: T-HG-0108) and the Cincinnati Children’s Hospital Medical Center IRB (Study ID: 2011–1553).
Participants
This cross-sectional study was nested in a longitudinal four-year study involving annual surveys to mothers of children with DBMD. This study includes data from the third survey. Recruitment for the longitudinal cohort was originally conducted through the DuchenneConnect registry (now called the Duchenne Registry), Parent Project Muscular Dystrophy (PPMD), and Cincinnati Children’s Hospital Medical Center Neuromuscular Clinic. To increase sample size for this cross-sectional study, an additional study description was sent out to DuchenneConnect participants. In addition, a notice was posted on the clinicaltrials.gov website. Individuals were eligible to participate if they were the biological mothers of a living child of any age with DBMD residing in the United States, 18 years of age or older, and capable of answering a survey in English.
Procedures
Participants were emailed a link to the survey that was made available from September 6, 2014 to November 4, 2014. Individuals who completed the survey received a $20 Amazon.com gift card.
Measures
Demographic characteristics
Participants reported their age, gender, annual household income, race/ethnicity, marital status, level of education, and employment status. Additionally, they reported characteristics for their oldest child with DBMD including: diagnosis (DMD, BMD, or intermediate phenotype), functional status (a 7-item categorization where a higher score means less ability to ambulate), current age, age at diagnosis, and previous participation in a clinical trial. These characteristics were parent reported and not verified with clinical information.
Uncertainty
Maternal uncertainty was measured using a revised version of the Parental Uncertainty of Children’s Health scale (PUCHs), a scale previously used in two studies of caregivers of children with undiagnosed conditions (Cronbach alpha were 0.79 and 0.90).25,26 The PUCHs measures four domains of perceived parental uncertainty: medical management, reproductive, social, and existential. It was designed to measure the level of perceived uncertainty in each domain and weight each by its importance. Participants were asked to rank their level of uncertainty about 13 statements on a 5-point scale ranging from −2 (strongly disagree) to 2 (strongly agree) followed by a ranking of the level of importance to resolve the uncertainty, on a 5-point scale ranging from 1 (unimportant) to 5 (most important) for each of the same 13 statements. A final score was calculated for each domain and in total by multiplying the perceived uncertainty levels by their importance and then dividing by the sum of the importance values. Scores range from −2 to 2 with higher scores indicating higher weighed uncertainty. The Cronbach alpha for the PUCHs in this study was 0.76, demonstrating internal reliability.
Hope
We adopted Dufault and Martocchio’s state-dependent operationalization of hope based on our prior experience with this population, and using that operationalization we created the Parent Hope Scale (PHS) to assess situational, disorder-specific hope (Supplemental Figure 1).18 Items were informed by the literature and findings from previous interview studies of parents of children with DBMD.3,16,27–29 The items were piloted with ten mothers of children with DBMD; based on their input, we made changes to clarify the meaning of several items and to better define the prompts.
The resulting PHS is a 14-item tool to assess how often in the past 4 weeks participants found hope for the future based on: routine experience (2 items), a sense of personal expertise (2 items), the present situation (2 items), optimistic future orientation (2 items), the promise of uncertainty (2 items), and their resources (4 items).
Items are shown in Supplemental Figure 1 and use a 1–5 rating scale anchored by “Never” to “Always.” Since the PHS was a novel scale, prior to using the measure data in other analyses, the items were subjected to an exploratory principle component analysis (PCA) followed by calculation of Cronbach alpha to measure internal reliability using SPSS Version 24.
Spirituality
The Daily Spiritual Experience Scale (DSES) is a 16-item measure of spiritual experience selected for its ability to measure ordinary spiritual experience and designed to be relevant to all spiritual beliefs.30 The first 15 items are measured on a 6-point scale anchored by “many times a day” to “never or almost never.” Item 16 is measured on a 4-point scale anchored by “Not Close at All” to “As Close as Possible.” Scores are then summed and totals range from 16 to 94, with higher scores indicating less spiritual experience. The Cronbach alpha was 0.97.30
Coping Efficacy
The Coping Self-Efficacy Scale (CSES) was used to measure coping efficacy, defined as perceived ability to cope effectively with a stressor.31 It is a 26-item measure that uses a 0–10 scale anchored by “cannot do at all” and “certain can do.” The total score is a sum of the items with higher scores indicating greater coping efficacy. The Cronbach alpha was 0.96.31
Data Analysis
Statistical analysis was conducted using SPSS Version 24. Most of the demographic variables with multiple response categories or continuous responses were dichotomized after performing preliminary descriptive analyses. These included: annual income (<$99,999 vs. > $100,000), marital status (not married/long-term relationship vs. married/long-term relationship), level of education (completed college or more vs. some college or less), race (Caucasian vs. not), employment (not employed vs. full time/part time employed), number of children with DBMD (1 vs. >1), and the child’s DBMD diagnosis (DMD vs. BMD/intermediate phenotype). The following variables were categorical: total number of children (1 vs. 2 vs. 3 vs. >3), oldest affected child’s age at diagnosis (prenatal vs. 0–3 years vs. 4–7 years vs. 8–11 years vs. 12 years or older), and oldest affected child’s functional status (ambulatory vs. transition to the use of a power wheelchair full-time vs full-time users of power wheelchairs). Key predictor variables (uncertainty, hope, spirituality, and coping efficacy) remained continuous variables in the analysis.
Bivariate relationships were analyzed among the key predictor variables (hope, uncertainty, coping efficacy, spirituality) and potential confounding variables (other child and mother characteristics and demographic variables) using Pearson’s and Spearman’s correlations. All independent variables with a significant bivariate relationship with uncertainty or coping efficacy at the p<0.05 level were included in the multivariate regression. A backwards elimination strategy was used to remove one variable at a time, starting with the highest p-value, until only those with a p-value of <0.05 remain. A change in estimate strategy was used to assess the impact of confounding variables. Each potential confounder was added to the model individually and if the Beta for any key predictor variables in the model changed by more than 10%, the confounder was included in the final model.
Results
Participants
Two hundred twenty-eight eligible mothers completed surveys. Twenty-six participants were eliminated due to incomplete or unanswered questions. As such, the final sample size for data analysis was 202 participants.
Demographics of Participants and Participants’ Children
Table 1 displays the sociodemographic of the participants and participants’ oldest affected child. The mean age of the mothers was 44.8 years. Participants were primarily married or in a long-term relationship (85.2%), Caucasian (91.6%), non-Hispanic (92.6%), and have a median household income of $50,000-$99,999. A majority of the participants had only one child affected (93.1%) and had child(ren) with DMD (84.2%). The mean age of the oldest affected child was 14.0 (± 7.2), with the mean age of 16.2 for children with a BMD diagnosis, 13.6 for children with a DMD diagnosis, and 17.0 for children with an intermediate phenotype. In regards to functional status, 38.6% of the oldest affected children were ambulatory, 20.8% were transitioning to full-time power wheelchair use, and 40.6% were full-time users of power wheelchairs.
Table 1.
Demographics and sample characteristics (n=202)
| Variable | Group | n | % |
|---|---|---|---|
| Race (check all that apply) | Caucasian | 185 | 91.58 |
| Asian American/Pacific Islander | 5 | 2.48 | |
| African American | 2 | 0.99 | |
| Native American | 0 | 0 | |
| Other | 14 | 6.93 | |
| Ethnicity | Not Hispanic or Latino | 187 | 92.57 |
| Hispanic or Latino | 14 | 6.93 | |
| Not disclosed | 1 | 0.50 | |
| Current Marital Status | Single/Never Married | 4 | 1.98 |
| Married or long-term committed relationship | 172 | 85.15 | |
| Divorced or Separated | 23 | 11.39 | |
| Widowed | 3 | 1.48 | |
| Highest Level of Education | Grade school or middle school | 0 | 0 |
| High School/GED | 11 | 5.45 | |
| Some College/Technical School | 45 | 22.28 | |
| Completed College | 94 | 46.53 | |
| Post-Baccalaureate Degree | 52 | 25.74 | |
| Annual Income | Under $50,000 | 29 | 14.36 |
| $50,000 - $99,999 | 83 | 41.09 | |
| $100,000 - $149,999 | 39 | 19.31 | |
| $150,000 - $199,999 | 29 | 14.36 | |
| Greater than $200,000 | 18 | 8.91 | |
| Not disclosed | 4 | 1.98 | |
| Employment Level of Mother | All of my time is spent caring for my family | 65 | 32.18 |
| Part-time job or school | 97 | 48.02 | |
| Full-time job or school | 40 | 19.80 | |
| Diagnosis of Child with DBMD | Duchenne | 170 | 84.62 |
| Becker | 23 | 10.86 | |
| Intermediate Phenotype | 9 | 4.52 | |
| Age at Diagnosis of Oldest child with DBMD | Prenatally | 2 | 0.99 |
| 0-3 years | 79 | 39.11 | |
| 4-7 years | 97 | 48.02 | |
| 8-12 years | 21 | 10.40 | |
| >12 years | 3 | 1.49 | |
| Functional Status of Oldest Child with DBMD | Presymptomatic | 14 | 6.93 |
| Early-ambulatory | 64 | 31.68 | |
| Late-ambulatory | 33 | 16.34 | |
| Early non-ambulatory | 9 | 4.46 | |
| Non-ambulatory I | 45 | 22.28 | |
| Non-ambulatory II | 29 | 14.36 | |
| Non-ambulatory III | 8 | 3.96 | |
| Current Age of Oldest Child with DMBD | ≤4 | 7 | 3.47 |
| 5-9 | 54 | 26.73 | |
| 10-14 | 60 | 29.70 | |
| 15-18 | 30 | 14.85 | |
| 19-22 | 25 | 12.38 | |
| ≥23 | 26 | 12.87 |
Analysis of the Parent Hope Scale (PHS)
The Kaiser-Meyer-Olkin value was .89 and Bartlett’s test of sphericity reached statistical significance, supporting the factorability of the items. Principal components analysis revealed the presence of four components with eigenvalues exceeding 1. An inspection of the screeplot revealed a clear break after the first component, and a single component solution was supported by results of the varimax and oblimin rotations. Thus we forced and retained a one component solution that explained 44.3% of the variance; item loadings are shown in Table 2. To determine internal reliability of the 14 items we conducted a reliability analysis, resulting in a Cronbach alpha 0.90. Additionally, the distribution of responses and median for each item of the PHS are shown in Supplemental Table 1.
Table 2.
Factor loadings and communalities based on a principle components analysis for the 14 items of the Parent Hope Scale (PHS) (n=202)
| Stem | Item | Component 1 | Communalities |
|---|---|---|---|
| In the past 4 weeks, how often have you found hope in… | The day-to-day life with your child | 0.677 | 0.459 |
| Parenting your child | 0.660 | 0.436 | |
| Begin able to care for your child | 0.726 | 0.526 | |
| Understanding your child | 0.511 | 0.261 | |
| Research being done today | 0.763 | 0.582 | |
| Aspects of your child’s clinical care | 0.637 | 0.406 | |
| Imagining your child’s bright future | 0.706 | 0.498 | |
| Your confidence about your child’s future | 0.626 | 0.391 | |
| The uncertain potential of your child | 0.778 | 0.605 | |
| Your child’s long-term health could be better than expected | 0.655 | 0.429 | |
| In the past 4 weeks, how often have you found hope through… | Your relationships with others | 0.633 | 0.401 |
| Your determination | 0.699 | 0.489 | |
| Your faith or spirituality | 0.627 | 0.393 | |
| Your use of the resources available to you | 0.572 | 0.327 | |
Descriptive Results and Bivariate Analysis
The means, standard deviations, and response ranges of the primary variables are presented in Table 3. Response distributions for each scale are in supplemental figures 2–5. Pearson’s and Spearman’s correlations were used to perform bivariate analysis to determine the strength and significance of predicted relationships among key variables and demographics (Table 4). Greater perceived uncertainty was significantly correlated with lower coping efficacy, lower hope, less spirituality, and having children with less ability to ambulate. Lower coping efficacy was significantly correlated with greater perceived uncertainty, less spirituality, and less hope. Lower perceptions of hope were significantly correlated with lower coping efficacy, greater uncertainty, and less spirituality.
Table 3.
Means and range of key variables (n=202)
| Variable | Scale range | Mean ± SD | Response Range |
|---|---|---|---|
| Uncertainty | (−2 – 2) |
−0.72 ± 0.78 | (−2 – 1.48) |
| Coping Efficacy | (0 – 260) | 168.97 ± 45.59 | (44 – 260) |
| Hope | (1 – 5) | 3.71 ± 0.62 | (1.8 – 5) |
| Spirituality | (16 – 94) | 48.73 ± 19.92 | (16 – 93) |
Table 4.
Bivariate associations between key variables (n=202)
| Variable | Coping Efficacy | Uncertainty | Hope | Spirituality | Functional status |
|---|---|---|---|---|---|
| Coping Efficacy | 1.000 | — | — | — | — |
| Uncertainty | −0.436** | 1.000 | — | — | — |
| Hope | 0.546* | −0.292* | 1.000 | — | — |
| Spirituality | −0.469* | 0.247* | −0.518* | 1.000 | — |
| Functional status | 0.067 | −0.271* | 0.030 | −0.031 | 1.000 |
p<0.001
Multivariate Regression Analyses
Uncertainty
A multilinear regression was performed to assess predictors of uncertainty. The final model including mothers’ age, hope, and child’s functional status revealed that older mothers’ age (p=0.001), greater hope (p<0.001), and having children with less ability to ambulate (p=0.042) were associated with lower perceived uncertainty (Table 5). These three variables accounted for 20.0% of the variance in perceptions of uncertainty.
Table 5.
Multilinear regressions between key variables (n=202)
| Variable | R2 | Unstandardized Coefficients |
t | P-value | |
|---|---|---|---|---|---|
| Beta | Std. Error | ||||
| Uncertainty | 0.200 | ||||
| Hope | −0.410 | 0.424 | −5.07 | <0.001 | |
| Functional status | −0.128 | 0.081 | −2.05 | 0.042 | |
| Maternal age | −0.021 | 0.006 | −3.36 | 0.001 | |
| Coping Efficacy | 0.416 | ||||
| Hope | 25.682 | 4.724 | 5.44 | <0.001 | |
| Uncertainty | −16.376 | 3.357 | −4.88 | <0.001 | |
| Spirituality | −0.499 | 0.146 | −3.41 | 0.001 | |
Coping Efficacy
A multilinear regression was performed to examine predictors of coping efficacy. The final model included hope, uncertainty, and spirituality and revealed that mothers with less hope (p<0.001), higher perceptions of uncertainty (p<0.001), and less spirituality (p=0.001) were less confident in their ability to cope with their child’s DBMD (Table 5). These three variables together accounted for 41.6% of the variance in coping efficacy.
Discussion
Hope has been reported to affect appraisals of uncertainty and adaptation to a condition.15 In this study we developed a novel state-based hope scale to better understand the relationships among uncertainty, hope, spirituality, and coping efficacy in mothers of children with DBMD.
In our exploratory analysis, the Parent Hope Scale (PHS) items fit a one-component solution and exhibited high internal reliability. Additionally, the PHS demonstrated evidence of convergent validity in that hope was positively correlated with coping efficacy and negatively correlated with uncertainty, which is consistent with published evidence.8,19,21–23,25 We assessed if the PHS was measuring a distinct concept based on the potential for conceptual overlap between hope and constructs including spirituality, faith, optimism, and wishful thinking.32–34 Hope, spirituality, and uncertainty all independently predicted coping efficacy through multivariate regression, providing evidence that the PHS measured a distinct concept from these related variables. Further research on the PHS in larger datasets and replication are needed.
Additionally, uncertainty and hope are both independent predictors of coping efficacy. This finding supports the possibility that hope can both offer a way to manage uncertainty, as well as the value of hope in supporting confidence in coping with a child’s life-shortening condition. Since we assessed hope as a disease-specific state and not a personality trait, we expect hope to be dynamic and influenced by circumstance, support, and coping strategies. Although more research is needed to better understand the factors influencing hope, it may be possible for healthcare providers such as genetic counselors to bolster hope in low-hope individuals using interventions such as strength-based counseling strategies.35 This research also suggests that even if hope is not easily fostered, guiding mothers with low hope towards uncertainty management and reappraisal strategies may facilitate their adaptation.
This study also revealed other predictors of maternal perceptions of uncertainty related to the nature of their children’s condition. Independently, child’s functional status and maternal age predicted maternal perceptions of uncertainty, whereas mothers of children with less ability to ambulate perceived less uncertainty and younger mothers reported more uncertainty. Mishel’s Uncertainty Theory asserts that uncertainty surrounding an illness typically decreases with age for most chronic or stable conditions;13 our data suggests that this trend is also true for this progressive condition. This finding could be due to several factors. First, it is possible that mothers of children with more progressed symptoms simply have less to be uncertain about. A second possibility is that as their child’s condition progresses, mothers have had more time to process the diagnosis and associated uncertainties and may therefore be appraising the uncertainty differently, resulting in lower perceptions of uncertainty. Additionally, it is possible that the period immediately following diagnosis is filled with greater anxiety, fear, and uncertainty, but over time, the negative psychological emotions and uncertainty subside due to learning more about DBMD, finding a trustworthy medical team, and meeting other DBMD families.
Our data suggests that techniques aimed at reducing or reframing perceptions of uncertainty may increase coping efficacy. Although it may be difficult to mitigate uncertainty, efforts to help mothers manage uncertainty may be more effective if tailored towards specific uncertainties that are more salient to them. For example, because younger mothers with ambulatory children report more uncertainty, offering extra support and education to families with a newly diagnosed child may help alleviate some of the initial uncertainty of the condition.
Future research including longitudinal studies is needed to further assess the relationship between hope, spirituality, uncertainty, and coping efficacy, as well as causality in these relationships. Exploring these concepts in other populations of mothers and other types of conditions could provide further understanding of these relationships, and ultimately inform the development of interventions to bolster hope and reframe uncertainty to hopefully support the adaptation process.
Limitations
Due to the cross-sectional nature of this study, assessments can only be made about how the variables are associated with one another, rather than the direction of the relationships. This study was also limited by the potential for recruitment bias. Although the representativeness of the study sample was increased by the diversity of recruitment sources, participation bias may have been generated due to the opt-in design of the study.
Conclusions
The concepts of hope and uncertainty are inherently related, and this study suggests that hope plays a role in shaping uncertainty appraisals and facilitating coping efficacy. Additionally, reduced uncertainty is also associated with increased coping efficacy. Therefore, both promoting the reduction of uncertainty and providing hope-bolstering interventions that offer a productive way of managing uncertainty may enhance coping efficacy and ultimately support adaptation.
Data Sharing
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Supplementary Material
Acknowledgements
This study was funded by the Intramural Research Program of the National Human Genome Research Institute.
Footnotes
Conflicts of Interest
Megan Bell reports no conflict of interest. Barbara B. Biesecker reports no conflict of interest.
Joann Bodurtha reports no conflict of interest. Holly L. Peay reports no conflict of interest.
References
- 1.Passamano L, Taglia A, Palladino A, et al. Improvement of survival in Duchenne Muscular Dystrophy: retrospective analysis of 835 patients. Acta Myol myopathies cardiomyopathies Off J Mediterr Soc Myol. 2012;31(2):121–125. http://www.ncbi.nlm.nih.gov/pubmed/23097603. [PMC free article] [PubMed] [Google Scholar]
- 2.Saito T, Kawai M, Kimura E, et al. Study of Duchenne muscular dystrophy long-term survivors aged 40 years and older living in specialized institutions in Japan. Neuromuscul Disord. 2017;27(2):107–114. doi: 10.1016/j.nmd.2016.11.012 [DOI] [PubMed] [Google Scholar]
- 3.Samson A, Tomiak E, Dimillo J, et al. The lived experience of hope among parents of a child with Duchenne muscular dystrophy: perceiving the human being beyond the illness. Chronic Illn. 2009;5(2):103–114. doi: 10.1177/1742395309104343 [DOI] [PubMed] [Google Scholar]
- 4.Koocher GP. Terminal care and survivorship in pediatric chronic illness. Clin Psychol Rev. 1984;4(5):571–583. doi: 10.1016/0272-7358(84)90045-X [DOI] [Google Scholar]
- 5.Han PKJ, Klein WMP, Arora NK. Varieties of uncertainty in health care: a conceptual taxonomy. Med Decis Making. 2011;31(6):828–838. doi: 10.1177/0272989X10393976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rosenthal ET, Biesecker LG, Biesecker BB. Parental attitudes toward a diagnosis in children with unidentified multiple congenital anomaly syndromes. Am J Med Genet. 2001;103(2):106–114. doi: 10.1002/ajmg.1527 [DOI] [PubMed] [Google Scholar]
- 7.Lipinski SE, Lipinski MJ, Biesecker LG, Biesecker BB. Uncertainty and perceived personal control among parents of children with rare chromosome conditions: The role of genetic counseling. Am J Med Genet Part C Semin Med Genet. 2006;142C(4):232–240. doi: 10.1002/ajmg.c.30107 [DOI] [PubMed] [Google Scholar]
- 8.Truitt M, Biesecker B, Capone G, Bailey T, Erby L. The role of hope in adaptation to uncertainty: the experience of caregivers of children with Down syndrome. Patient Educ Couns. 2012;87(2):233–238. doi: 10.1016/j.pec.2011.08.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stewart JL, Mishel MH. Uncertainty in childhood illness: a synthesis of the parent and child literature. Sch Inq Nurs Pract. 2000;14(4):299–319; discussion 321–6. http://www.ncbi.nlm.nih.gov/pubmed/11372189. [PubMed] [Google Scholar]
- 10.Bally JMG, Smith NR, Holtslander L, et al. A Metasynthesis: Uncovering What Is Known About the Experiences of Families With Children Who Have Life-limiting and Life-threatening Illnesses. J Pediatr Nurs. 2018;38:88–98. doi: 10.1016/j.pedn.2017.11.004 [DOI] [PubMed] [Google Scholar]
- 11.De Graves S, Aranda S. Living with hope and fear--the uncertainty of childhood cancer after relapse. Cancer Nurs. 2008;31(4):292–301. doi: 10.1097/01.NCC.0000305745.41582.73 [DOI] [PubMed] [Google Scholar]
- 12.Hinton D, Kirk S. Living with uncertainty and hope: A qualitative study exploring parents’ experiences of living with childhood multiple sclerosis. Chronic Illn. 2017;13(2):88–99. doi: 10.1177/1742395316664959 [DOI] [PubMed] [Google Scholar]
- 13.Mishel MH. Uncertainty in illness. Image J Nurs Sch. 1988;20(4):225–232. http://www.ncbi.nlm.nih.gov/pubmed/3203947. [DOI] [PubMed] [Google Scholar]
- 14.Mishel MH. Reconceptualization of the uncertainty in illness theory. Image J Nurs Sch. 1990;22(4):256–262. http://www.ncbi.nlm.nih.gov/pubmed/2292449. [DOI] [PubMed] [Google Scholar]
- 15.Fitzgerald Miller J Hope: a construct central to nursing. Nurs Forum. 2007;42(1):12–19. doi: 10.1111/j.1744-6198.2007.00061.x [DOI] [PubMed] [Google Scholar]
- 16.Duggleby W, Holtslander L, Kylma J, Duncan V, Hammond C, Williams A. Metasynthesis of the hope experience of family caregivers of persons with chronic illness. Qual Health Res. 2010;20(2):148–158. doi: 10.1177/1049732309358329 [DOI] [PubMed] [Google Scholar]
- 17.Farran CJ, Wilken C, Popovich JM. Clinical assessment of hope. Issues Ment Health Nurs. 1992;13(2):129–138. http://www.ncbi.nlm.nih.gov/pubmed/1577591. [DOI] [PubMed] [Google Scholar]
- 18.Dufault K, Martocchio BC. Symposium on compassionate care and the dying experience. Hope: its spheres and dimensions. Nurs Clin North Am. 1985;20(2):379–391. http://www.ncbi.nlm.nih.gov/pubmed/3846980. [PubMed] [Google Scholar]
- 19.Herth KA. The relationship between level of hope and level of coping response and other variables in patients with cancer. Oncol Nurs Forum. 1989;16(1):67–72. http://www.ncbi.nlm.nih.gov/pubmed/2911529. [PubMed] [Google Scholar]
- 20.Bruhn JG. Therapeutic value of hope. South Med J. 1984;77(2):215–219. http://www.ncbi.nlm.nih.gov/pubmed/6701591. [DOI] [PubMed] [Google Scholar]
- 21.Felder BE. Hope and coping in patients with cancer diagnoses. Cancer Nurs. 2004;27(4):320–324. http://www.ncbi.nlm.nih.gov/pubmed/15292728. [DOI] [PubMed] [Google Scholar]
- 22.Zhang J, Gao W, Wang P, Wu Z. Relationships among hope, coping style and social support for breast cancer patients. Chin Med J (Engl). 2010;123(17):2331–2335. http://www.ncbi.nlm.nih.gov/pubmed/21034544. [PubMed] [Google Scholar]
- 23.Wonghongkul T, Moore SM, Musil C, Schneider S, Deimling G. The influence of uncertainty in illness, stress appraisal, and hope on coping in survivors of breast cancer. Cancer Nurs. 2000;23(6):422–429. http://www.ncbi.nlm.nih.gov/pubmed/11128121. [DOI] [PubMed] [Google Scholar]
- 24.Barrera M, Granek L, Shaheed J, et al. The tenacity and tenuousness of hope: parental experiences of hope when their child has a poor cancer prognosis. Cancer Nurs. 2013;36(5):408–416. doi: 10.1097/NCC.0b013e318291ba7d [DOI] [PubMed] [Google Scholar]
- 25.Yanes T, Humphreys L, McInerney-Leo A, Biesecker B. Factors Associated with Parental Adaptation to Children with an Undiagnosed Medical Condition. J Genet Couns. 2017;26(4):829–840. doi: 10.1007/s10897-016-0060-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Macnamara EF, Han PK, Lipinski S, Biesecker BB. The Role of Uncertainty in Coping Efficacy: The Experience of Parents of Children with Undiagnosed Medical Conditions. [ScM thesis]. Baltimore, MD: Johns Hopkins University; 2014. [Google Scholar]
- 27.Holtslander LF, Duggleby WD. The hope experience of older bereaved women who cared for a spouse with terminal cancer. Qual Health Res. 2009;19(3):388–400. doi: 10.1177/1049732308329682 [DOI] [PubMed] [Google Scholar]
- 28.Bland R, Darlington Y. The nature and sources of hope: perspectives of family caregivers of people with serious mental illness. Perspect Psychiatr Care. 38(2):61–68. http://www.ncbi.nlm.nih.gov/pubmed/12132632. [DOI] [PubMed] [Google Scholar]
- 29.Holtslander LF, Duggleby W, Williams AM, Wright KE. The experience of hope for informal caregivers of palliative patients. J Palliat Care. 2005;21(4):285–291. http://www.ncbi.nlm.nih.gov/pubmed/16483098. [PubMed] [Google Scholar]
- 30.Underwood LG, Teresi JA. The daily spiritual experience scale: development, theoretical description, reliability, exploratory factor analysis, and preliminary construct validity using health-related data. Ann Behav Med. 2002;24(1):22–33. doi: 10.1207/S15324796ABM2401_04 [DOI] [PubMed] [Google Scholar]
- 31.Chesney MA, Neilands TB, Chambers DB, Taylor JM, Folkman S. A validity and reliability study of the coping self-efficacy scale. Br J Health Psychol. 2006;11(Pt 3):421–437. doi: 10.1348/135910705X53155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bruininks P, Malle BF. Distinguishing Hope from Optimism and Related Affective States. Motiv Emot. 2005;29(4):324–352. doi: 10.1007/s11031-006-9010-4 [DOI] [Google Scholar]
- 33.Bryant FB, Cvengros JA. Distinguishing Hope and Optimism: Two Sides of a Coin, or Two Separate Coins? J Soc Clin Psychol. 2004;23(2):273–302. doi: 10.1521/jscp.23.2.273.31018 [DOI] [Google Scholar]
- 34.Magaletta PR, Oliver JM. The hope construct, will, and ways: Their relations with self-efficacy, optimism, and general well-being. J Clin Psychol. 1999;55(5):539–551. doi:10.1002/(SICI)1097–4679(199905)55:5<539::AID-JCLP2>3.0.CO;2-G [DOI] [PubMed] [Google Scholar]
- 35.Padesky CA, Mooney KA. Strengths-based cognitive-behavioural therapy: a four-step model to build resilience. Clin Psychol Psychother. 2012;19(4):283–290. doi: 10.1002/cpp.1795 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


