Abstract
Background
Specialty palliative care (PC) is underutilized for patients with end-stage liver disease (ESLD). We sought to examine hepatologists’ and gastroenterologists’ attitudes about PC for patients with ESLD.
Methods
We conducted a cross-sectional survey of hepatologists’ and gastroenterologists’ who provide care to patients with ESLD recruited from the American Association for the Study of Liver Diseases membership directory. Using a questionnaire adapted from prior studies, we examined physicians’ attitudes about PC and whether these attitudes varied based on patients’ candidacy for liver transplantation. We identified predictors of physicians’ attitudes about PC using linear regression.
Results
Approximately one-third of eligible physicians (396/1236, 32%) completed the survey. Most (95%) believed that centers providing care to patients with ESLD should have PC services, and 86% trusted PC clinicians to care for their patients. Only a minority reported collaborating frequently with inpatient (32%) or outpatient (11%) PC services. Most believed that when patients hear the term PC, they feel scared (94%) and anxious (87%). Most (83%) believed that patients would think nothing more could be done for their underlying disease if a PC referral was suggested. Physicians who believed that ESLD is a terminal condition (B=1.09, p = 0.006) reported more positive attitudes about PC. Conversely, physicians with negative perceptions of PC for transplant candidates (B = −0.22, SE = 0.05, p < 0.001) reported more negative attitudes toward PC.
Conclusion
Although most hepatologists’ and gastroenterologists’ believe that patients with ESLD should have access to PC, they reported rarely collaborating with PC and had substantial concerns about patients’ perceptions of PC. Interventions are needed to overcome misperceptions of PC and promote collaboration with PC clinicians for patients with ESLD.
Keywords: Supportive care, decompensated cirrhosis, questionnaire, quality of life, liver transplantation
INTRODUCTION
Cirrhosis, the twelfth leading cause of death in the U.S., affects over 600,000 persons and is the seventh leading cause of death for patients aged 25 to 64.1,2 As cirrhosis progresses over time, debilitating symptoms, such as ascites, hepatic encephalopathy, and variceal hemorrhage, can develop. The emergence of these symptoms marks the transition to decompensated cirrhosis, or end-stage liver disease (ESLD), a clinical state marked by substantial morbidity, limited life expectancy, and poor quality of life.3,4
Specialty palliative care (PC), a service focused on the management of physical and psychosocial symptom in patients facing serious illnesses, has been shown to improve quality of life, symptom burden, and mood in patients with cancer and other serious illnesses as well as their caregivers.5–10 Despite evidence supporting the benefit of PC for many chronic conditions, PC remains underutilized for patients with ESLD.11–13 We hypothesize that misperceptions of PC may contribute to the underutilization of specialty PC services by physicians caring for patients ESLD, as has been shown in prior studies of providers caring for patients with cancer and congestive heart failure.14–16 However, we currently have limited empirical data on the perceptions of PC by physicians providing care to patients with ESLD.17,18 Therefore, we need a more comprehensive understanding of hepatologists’ and gastroenterologists’ perceptions of and attitudes about PC for patients with ESLD.
We conducted a cross-sectional study to investigate the attitudes of U.S. hepatologists and gastroenterologists about PC for patients with ESLD. In addition, we examined whether physicians’ attitudes about PC for patients with ESLD varied based on patients’ candidacy for liver transplantation. We hypothesized that physicians would have more negative attitudes about PC for patients with ESLD on the transplant waitlist. We explored potential predictors of physicians’ attitudes about PC and hypothesized that physicians’ demographics and clinical practice characteristics may predict their perceptions of PC.
METHODS
Study Population
Using the American Association for the Study of Liver Diseases membership directory, we identified potentially eligible U.S.-based attending hepatologists and gastroenterologists who provide direct clinical care to adult (age 18 years or older) patients with ESLD. The society maintains a web-based directory for its members that includes email addresses.
Survey Administration
We administered the survey between February and April 2018. We sent participants personalized invitations through email to complete the survey containing individualized links to the web-based survey through Research Electronic Data Capture (REDCap, Vanderbilt University, Nashville, TN), a password protected web-based survey tool. We made a total of four follow-up contacts to non-respondents by sending email reminders in the 2nd, 3rd 4th and 6th weeks. Participants who completed the survey and chose to receive an honorarium received a $20 gift card. Because survey responses were deidentified in this study, the study procedures were deemed exempt from review by the Partners Institutional Review Board.
Survey Instrument
The survey included four screening questions to confirm study eligibility as well as items that were adapted from prior surveys that explored physicians’ collaboration with PC services, attitudes about specialty PC, sense of ownership over addressing PC issues, perceptions of patients’ reactions to PC, and PC referral patterns.19–23 All items included in the survey have been validated and used in prior studies.23–27 We revised and adapted the survey items to ask specifically about the population of patients with ESLD (see Appendix). The survey was designed to measure the following domains: 1) Demographics and clinical practice characteristics (13 items); 2) access to and quality of PC services (2 items); 3) physicians’ perception of ESLD as a terminal condition (1 item); 4) physicians’ attitudes about PC (6 items); 5) physicians’ attitudes about PC for liver transplant candidates (4 items); 6) physicians’ perceptions of patients’ reactions to PC (16 items); 7) physicians’ sense of ownership over addressing PC issues (6 items); and 8) physicians’ attitudes about the timing of PC referrals for patients with ESLD (4 items). Aspects of the survey that explored physicians’ perceptions of barriers to PC referrals will be the focus of a separate publication.
Study investigators (NU, AE) performed cognitive interviews and pilot testing of the survey with eight hepatologists and conducted content analysis to refine the questionnaire and ensure its content validity, readability, and acceptability. We reached thematic saturation with feedback and modified twelve questions based on participants responses, primarily by clarifying ambiguous language. We eliminated five questions due to their repetitive nature.
Statistical Analysis
The primary aims of this study were descriptive, and we generated graphical summaries of participants’ responses to the survey items by using frequencies and percentages for categorical variables and means and standard deviations for continuous variables. Our secondary analysis was aimed at examining predictors of physicians’ attitudes about PC. As has been done in prior studies, we generated a composite score for our primary outcome of interest, physicians’ attitudes about PC based on the six survey items within this domain.14,19 Each of these items was scored on a 4-point Likert scale, and we created a composite score of all six items (with higher scores indicating more positive attitudes about PC; range 4–24). We also generated composite scores corresponding to other survey domains that we defined a priori as potential predictors of physicians’ attitudes about PC14,19: 1) Perception that ESLD is a terminal condition (scored as a yes/no item); 2) extent of collaboration with PC services (higher scores indicating more frequent collaboration with PC services; range 0–6); 3) perceived quality of PC services (higher scores indicating higher perceived quality of PC services; range 0–6); 4) attitudes about PC for liver transplant candidates (higher scores indicating more positive attitudes about PC for liver transplant candidates; range 0–15); 5) perception of patients’ reactions to PC (higher scores indicating more positive perception of patients’ reactions to PC; range 3–21); and 6) sense of ownership over addressing PC issues (higher scores indicating higher sense of ownership; range 2–18).
We used a linear regression model to examine predictors of physicians’ attitudes about PC. We included the following a priori defined predictors in our model: Gender, primary professional role, years of training, prior training in PC, perception of ESLD as a terminal disease, perceived quality of PC services, perception of PC for liver transplant candidates, perception of patients’ reaction to PC, and ownership over PC issues. We considered a p-value of < 0.05 to be statistically significant. We conducted all analyses with STATA version 15.1 (College Station, TX).
RESULTS
Participant Characteristics
In all, 396 of 1236 (32%) eligible physicians completed the survey [Table 1]. The physicians were primarily male (287/396, 73%) and white (250/396, 63%). Most physicians were transplant hepatologists (237/396, 60%), followed by general hepatologists (119/396, 30%) and gastroenterologists (34/296, 9%). The majority (314/396, 79%) practiced in a teaching hospital. Overall, 39% (156/396) had less than 10 years of clinical practice, 22% (88/396) had 10–20 years, and 36% (143/396) had over 20 years in practice. With respect to prior training in PC, none of the 396 responding physicians had formal (≥ 6 months) PC training; over half (205/396, 52%) had no prior training, whereas 46% (183/396) had previously attended a continuing medical education course or participated in a clinical PC rotation. Almost all (366/381, 96%) participants responded that if they had a life-limiting illness, they would use PC. Almost all (364/373, 98%) participants responded that if their loved one had a life-limiting illness, they would use PC. The majority (331/381, 87%) agreed that ESLD is a terminal condition.
Table 1:
Participant Characteristics
| Participant Characteristic (N = 396) | No. (%) |
|---|---|
| Male | 287 (72.5) |
| Hispanic or Latino | 31 (7.8) |
| Race | |
| White | 250 (63.1) |
| Asian | 117 (29.5) |
| Black | 12 (3.0) |
| Native Indian/Native Hawaiian | 3 (0.8) |
| Other | 14 (3.5) |
| Primary role | |
| Transplant hepatologist | 237 (59.8) |
| General hepatologist | 119 (30.1) |
| Gastroenterologist | 34 (8.6) |
| Missing | 6 (1.5) |
| Region | |
| Midwest | 78 (19.7) |
| Northeast | 109 (27.5) |
| South | 114 (28.8) |
| West | 81 (20.5) |
| Missing | 14 (3.5) |
| Years since completing fellowship training | |
| <10 years | 156 (39.4) |
| 10–20 years | 88 (22.2) |
| >20 years | 143 (36.1) |
| Missing | 9 (2.3) |
| Time dedicated to clinical responsibilities | |
| <30% | 36 (9.1) |
| 30 – 60% | 72 (18.2) |
| >60% | 280 (70.7) |
| Missing | 8 (2.0) |
| Primary practice setting | |
| Private practice | 48 (12.1) |
| Community hospital | 18 (4.5) |
| Teaching hospital | 314 (79.3) |
| Other | 10 (2.5) |
| Missing | 6 (1.5) |
| Board certification | |
| Internal medicine | 303 (76.5) |
| Gastroenterology | 358 (90.4) |
| Transplant hepatology | 215 (54.3) |
| Other | 8 (2.0) |
| Prior training in palliative care | |
| No training | 205 (51.8) |
| Attended courses or rotation in palliative care | 183 (46.2) |
| 6 months or more of formal training | 0 (0.0) |
| Missing | 8 (2.0) |
| Provide clinical care as a member of a liver transplant program | |
| Yes | 264 (66.7) |
| No | 126 (31.8) |
| Missing | 6 (1.5) |
| Number of liver transplants performed annually at primary practice center | |
| ≤ 50 | 72 (18.2) |
| 51–99 | 77 (19.4) |
| ≥ 100 | 111 (28.0) |
| Do not know | 1 (0.3) |
| Missing | 135 (34.1) |
Attitudes about timing of PC Referrals for Patients with ESLD
Nearly all (359/365, 98%) physicians indicated that they would use PC services for patients who are not candidates for liver transplantation. Less than half (176/365, 48%) would use PC for patients active on the liver transplant list, and only 36% (130/365) would use PC for newly-diagnosed patients with ESLD.
Collaboration with and Quality of PC services
Almost all respondents had access to inpatient (376/385, 98%) or outpatient (363/385, 94%) PC services. Only a minority of physicians (124/385, 32%) reported that they collaborated often with inpatient PC services. Most physicians rated the quality of their inpatient PC services as “very good” (219/385, 57%) or “good” (136/385, 35%). Few (41/385, 11%) reported that they collaborated often with outpatient PC services, with a substantial minority reporting that they rarely (128/385, 33%) or never (40/385, 10%) had collaborated with outpatient PC services. Most physicians rated the quality of their outpatient PC services as “very good” (154/382, 40%) or “good” (150/382, 39%).
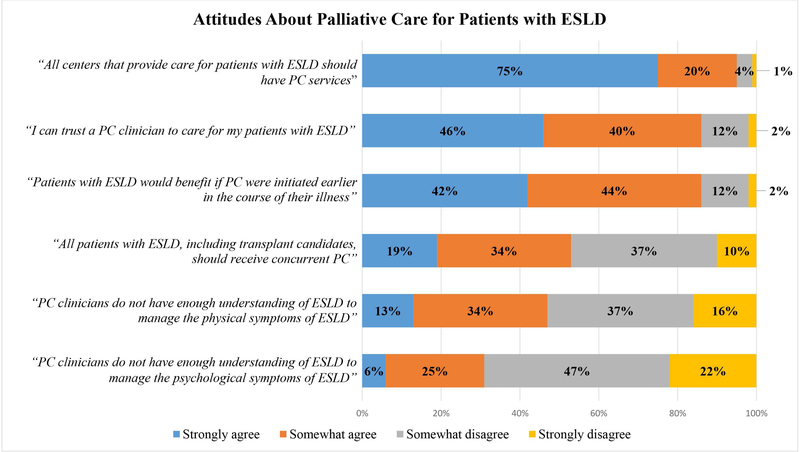
Attitudes About PC for Patients with ESLD
Physicians’ attitudes toward PC for patients with ESLD are depicted in Figure 1. Nearly all (358/378, 95%) participating physicians agreed that all centers providing care for patients with ESLD should have PC services. The majority (326/379, 86%) of respondents thought that patients with ESLD would benefit if PC were provided earlier in the course of their illnesses. Most (326/380, 86%) responded that they can trust a PC clinician participate in the care of their patients with ESLD. Almost half (179/379, 47%) of responding physicians expressed concern that PC clinicians do not have enough understanding of ESLD to manage the physical symptoms of patients with ESLD.
Figure 1:
Physicians’ Attitudes About Palliative Care for Patients with ESLD
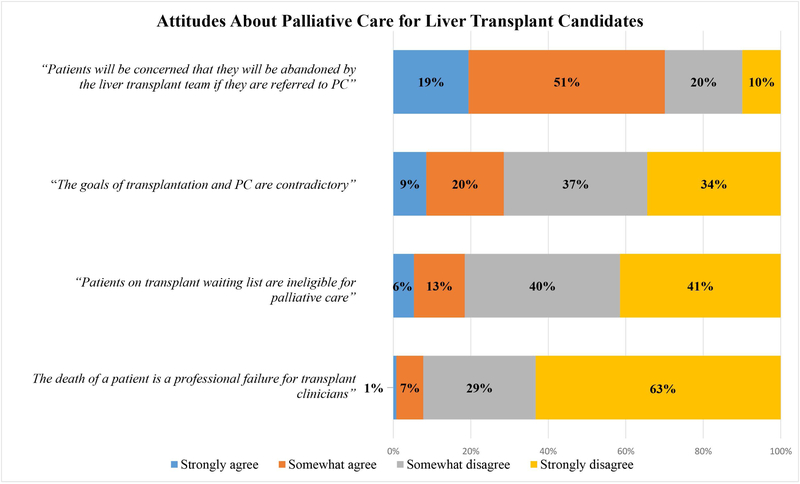
Attitudes About PC for Liver Transplant Candidates
Physicians’ attitudes about PC for liver transplant candidates are depicted in Figure 2. Almost half (178/380, 47%) of physicians disagreed with the statement, “All patient with ESLD, including liver transplant candidates, should receive concurrent PC”. A considerable proportion of physicians (69/374, 18%) indicated that patients on the liver transplant waiting list are ineligible for PC, and 29% (107/375) responded that the goals of transplantation and PC are contradictory. The majority of physicians (263/375, 70%) thought that patients and their caregivers would feel abandoned by the liver transplant team if they were referred for PC.
Figure 2:
Physicians’ Attitudes About Palliative Care for Liver Transplant Candidates
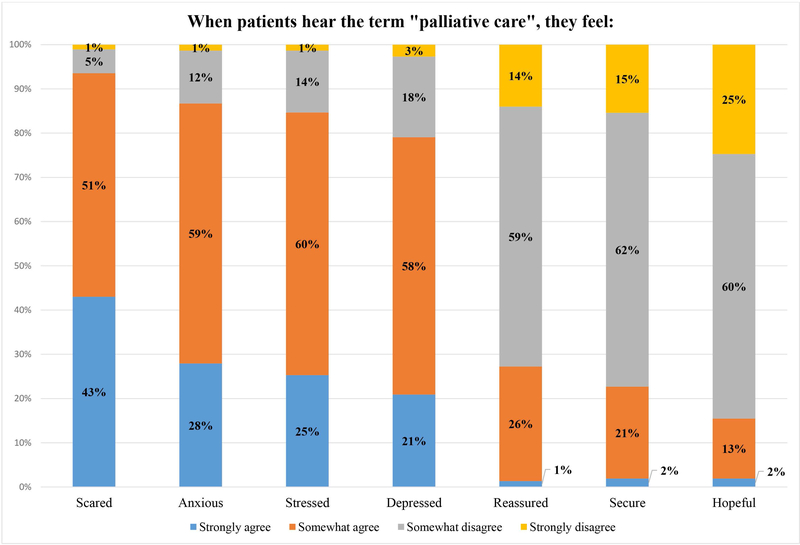
Physicians’ Perceptions of Patients’ Reactions to PC
Most physicians responded that when patients hear the term “palliative care”, they would feel scared (348/372, 94%), anxious (326/371, 87%), and depressed (293/371, 79%); only a minority thought that patients would feel reassured (101/371, 27%) or hopeful (57/368, 15%) [Figure 3]. Most physicians expressed concern that patients referred for PC would think that nothing more could be done for their underlying disease (304/364, 83%) and would worry that the PC team would talk to them about dying (298/364, 79%) [Figure 4]. Only 23% (85/366) of respondents thought that patients would feel more positively about the future if referred for PC.
Figure 3:
Physicians’ Perceptions of Patients’ Reactions to the term “Palliative Care”
Figure 4:
Physicians’ Perceptions of Patients’ Reactions to Palliative Care Referral
Physicians’ Sense of Ownership Over Addressing PC Issues
Nearly all (368/381, 97%) responding physicians indicated that hepatologists should be experts in the management of the physical symptoms of ESLD, and the majority (220/380, 58%) endorsed that hepatologists should be experts in the management of the psychological symptoms [Figure 5]. Most agreed that a hepatologist is the best person to discuss advance care planning with patients with ESLD (319/381, 84%) and should coordinate the care of patients with ESLD at all stages of their disease, including end-of-life care (280/377, 74%). Notably, only 27% (103/381) of physicians felt that a hepatologist is the best person to provide PC to patients with ESLD, with the majority (335/381, 88%) preferring that PC specialists serve in this role.
Figure 5:
Physicians’ Sense of Ownership over Addressing Palliative Care Issues
Predictors of Physicians’ Attitudes About PC
The following predictors were associated with more positive attitudes toward PC: physicians with < 10 years of clinical practice (B = 0.86, SE = 0.32, p = 0.008), those who believe that ESLD is a terminal condition (B = 1.09, SE = 0.40, p = 0.006) and those with a more positive perception of the quality of PC services (B = 0.55, SE = 0.09, p < 0.001) [Table 2]. Conversely, physicians with a higher sense of ownership over PC issues (B = −0.12, SE = 0.05, p = 0.02) and a negative perception of PC for liver transplant candidates (B = −0.22, SE = 0.05, p < 0.001) were more likely to have negative attitudes toward PC.
Table 2:
Predictors of Physicians’ Attitudes About Palliative Care.
| Predictors | Estimate | Standard Error | T-value | P-value |
|---|---|---|---|---|
| Female sex (ref: male) | 0.01 | 0.32 | 0.02 | 0.98 |
| Years of clinical practice (ref: >20 years) | ||||
| <10 years | 0.86 | 0.32 | 2.69 | 0.008 |
| 10–20 years | 0.67 | 0.37 | 1.79 | 0.075 |
| Training in PC (ref: No prior training) | ||||
| Attended courses or rotations in PC | 0.50 | 0.28 | 1.79 | 0.075 |
| Perceived quality of PC services | 0.55 | 0.09 | 6.29 | <0.001 |
| Physicians’ perception that ESLD is a terminal condition | 1.09 | 0.40 | 2.75 | 0.006 |
| Physicians’ sense of ownership over PC issues | −0.12 | 0.05 | −2.37 | 0.02 |
| Physicians’ perception of negative patient reactions to PC | −0.07 | 0.05 | −1.50 | 0.14 |
| Physicians’ negative perception of PC for liver transplant candidates | −0.22 | 0.05 | −4.46 | <0.001 |
Abbreviations: Palliative care (PC), end-stage liver disease (ESLD). The outcome of interest in this predictive model is physicians’ attitudes about PC as measured by a composite score, with higher values indicating more positive attitudes toward PC. A positive coefficient of the estimate indicates a positive attitude about PC. For example, compared with physicians with more than 20 years of clinical practice, those physicians who had less than 10 years of clinical practice had better attitudes about PC (0.86 points higher; p = 0.008). Conversely, a negative coefficient indicates a lower score and a more negative attitude toward PC.
DISCUSSION
In this study, we examined comprehensively the perception of U.S. hepatologists and gastroenterologists about specialty PC for patients with ESLD. Almost all participating physicians responded that patients with ESLD should have access to PC, but only a minority of physicians collaborated frequently with inpatient or outpatient PC services. Although nearly all responding physicians would use PC services for patients with ESLD who were not candidates for liver transplantation, fewer than half would refer their patients who were active on the liver transplant waitlist for PC. Many physicians reported a strong sense of ownership over addressing PC issues for patients with ESLD, such as physical and psychological symptom management as well as advance care planning. Paradoxically, however, the majority of respondents did not believe that hepatologists would be the best providers of PC to patients with ESLD. Although most physicians responded that they could trust PC clinicians to participate in the care for patients with ESLD, many expressed concerns about patients’ reactions to both the term “palliative care” and a referral to PC services. Despite generally positive attitudes toward PC by physicians, our data revealed many potential barriers to specialty PC referrals for patients with ESLD and multiple areas for growth.
Our results show that physicians have different attitudes about PC referrals for patients with ESLD based on their candidacy for liver transplantation. These findings suggest a misperception among physicians that the delivery of PC begins when active therapy ends, which is a noted barrier to PC referral in other transplant populations.14,27 However, in addition to their complex medical needs, patients on the transplant list also have significant psychosocial needs, specifically related to coping and uncertainty while awaiting transplantation, for which PC referrals could provide much-needed support.28,29 Given the specific focus of PC on improving the quality of life for patients at any stage of their disease, contemporary models of PC promote the concurrent delivery of PC in parallel with life-prolonging therapy.30 In a recent study, early integration of specialist PC in the management of patients undergoing hematopoietic stem cell transplantation was shown to improve patient-reported symptom burden and quality of life.31,32 PC has now been embraced as part of the routine medical management of other serious illnesses for which transplantation is curative therapy, such as end-stage renal disease and advanced heart failure.33–35 The findings from our survey underscore the need to increase awareness among hepatologists and gastroenterologists that PC can integrated into the care of patients with ESLD at any stage of their illness trajectory, including those being evaluated for transplantation.
Despite having a strong sense of ownership over core facets of PC, a majority of respondents preferred PC specialists to serve as the primary providers of PC to patients with ESLD. Most physicians agreed that specialists caring for patients with ESLD should be experts in PC issues such as physical and psychological symptom management and advance care planning. However, almost three-quarters of the responding physicians disagreed that a hepatologist is the best person to provide PC to patients with ESLD; instead, respondents had a strong preference for PC specialists to serve in this clinical role. The finding that specialists who manage ESLD feel they should own the PC issues of their patients yet prefer that PC clinicians fulfill this role may reflect current patterns of PC referral by hepatologists, in which PC referrals are underutilized, rarely occur in the outpatient setting, and are delayed until the late stages of ESLD.11,36,37 As such, PC appears to be perceived as end-of-life care that is delivered only to patients who are transitioning to hospice care or comfort measures.11 This misperception represents a missed opportunity for early PC integration, specifically in the ambulatory setting, to improve symptom management and the quality of life and care of patients with ESLD.11,12 A second potential important inference of these findings is that specialists in the management of ESLD want to engage in this care, but have competing time demands that limit their ability to provide comprehensive PC for their patients. Consequently, the PC needs of patients with ESLD are under-addressed – prior studies have shown that only a minority of patients with ESLD receive adequate symptom management or have engaged in timely advance care planning.12,38 These findings suggests three potential areas for growth for physicians providing care to patients with ESLD to integrate PC into their practice: 1) enhancing collaboration with PC specialists in the outpatient setting to support patients with ESLD early in their disease course; 2) developing high-quality interventions studies to improve the state of the science of symptom management in patients with ESLD; and 3) developing educational models to improve communication skills regarding advance care planning discussions.18,39
Most responding physicians expressed concern that patients with ESLD would have negative emotional reactions to a PC referral, which may reveal an important barrier to PC referral for this patient population. The majority of physicians responded that patients with ESLD would associate a PC referral with the end of active, disease-specific therapy, abandonment by their care team, and imminent death, findings that have been corroborated in patient and population-based surveys.40–42 The perception that the term “palliative care” in and of itself triggers distress in patients has been reported previously by clinicians who care for patients with chronic illnesses.15,16,22,23,43 To what extent patients with ESLD have a negative reaction to the term “palliative care” remains unclear and further studies are warranted to specifically assess the perceptions of PC by patients with ESLD.
This study has important limitations. First, with a response rate of 32%, our survey may be subject to nonresponse bias, and given the overrepresentation of physicians primarily practicing at teaching hospitals, our results might not be generalizable to nonacademic settings. However, our response rate is comparable to those reported in other contemporary electronic clinician survey studies.14,19 Second, while the survey items have been validated in prior studies, we adapted these items to apply specifically to patients with ESLD, and this instrument should be validated in future studies of patients with liver disease. Third, our survey did not specifically address patient factors such as hepatic encephalopathy or history of substance use disorder that may also impact physicians’ attitudes about PC use in this population. Fourth, we limited this survey to hepatologists and gastroenterologists who provide clinical care to patients with ESLD. In light of our findings regarding the role of PC for liver transplant candidates, the perceptions of PC by liver transplant surgeons may merit future assessment. Finally, this study focused specifically on physicians’ attitudes about PC; further studies are needed to identify additional barriers to specialty PC referrals for patients with ESLD.
In conclusion, our study demonstrates that although most hepatologists and gastroenterologists believe that patients with ESLD should have access to PC and would trust PC clinicians to deliver care to their patients, these specialists reported rarely collaborating with PC in their own practices and had substantial concerns about how patients perceive PC. Specific interventions are needed to overcome misperceptions in equating PC with end-of-life care and to enhance collaboration with PC services for patients with ESLD.
Supplementary Material
Acknowledgments
Financial Support: NIH DK078772 (RTC)
Abbreviations
- ESLD
end-stage liver disease
- PC
palliative care
Footnotes
Competing Interests: The other authors have no personal or financial disclosures or conflicts of interest to declare related to this research and manuscript
REFERENCES
- 1.Scaglione S, Kliethermes S, Cao G, et al. The Epidemiology of Cirrhosis in the United States: A Population-based Study. J Clin Gastroenterol. 2015;49(8):690–696. [DOI] [PubMed] [Google Scholar]
- 2.Kochanek KD, Murphy SL, Xu J, Tejada-Vera B. Deaths: Final Data for 2014. Natl Vital Stat Rep. 2016;65(4):1–122. [PubMed] [Google Scholar]
- 3.D’Amico G, Garcia-Tsao G, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J Hepatol. 2006;44(1):217–231. [DOI] [PubMed] [Google Scholar]
- 4.Langberg KM, Kapo JM, Taddei TH. Palliative Care in Decompensated Cirrhosis: A Review. Liver Int. 2017. [DOI] [PubMed] [Google Scholar]
- 5.Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med. 2010;363(8):733–742. [DOI] [PubMed] [Google Scholar]
- 6.Bakitas M, Lyons KD, Hegel MT, et al. Effects of a palliative care intervention on clinical outcomes in patients with advanced cancer: the Project ENABLE II randomized controlled trial. JAMA : the journal of the American Medical Association. 2009;302(7):741–749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.WHO | WHO Definition of Palliative Care. WHO; 2012; http://www.who.int/cancer/palliative/definition/en/. Accessed June 30, 2018. [Google Scholar]
- 8.Rogers JG, Patel CB, Mentz RJ, et al. Palliative Care in Heart Failure: The PAL-HF Randomized, Controlled Clinical Trial. J Am Coll Cardiol. 2017;70(3):331–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grubbs V, O’Riordan D, Pantilat S. Characteristics and Outcomes of In-Hospital Palliative Care Consultation among Patients with Renal Disease Versus Other Serious Illnesses. Clin J Am Soc Nephrol. 2017;12(7):1085–1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dionne-Odom JN, Azuero A, Lyons KD, et al. Benefits of Early Versus Delayed Palliative Care to Informal Family Caregivers of Patients With Advanced Cancer: Outcomes From the ENABLE III Randomized Controlled Trial. J Clin Oncol. 2015;33(13):1446–1452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kathpalia P, Smith A, Lai JC. Underutilization of palliative care services in the liver transplant population. World Journal of Transplantation. 2016;6(3):594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Poonja Z, Brisebois A, van Zanten SV, Tandon P, Meeberg G, Karvellas CJ. Patients With Cirrhosis and Denied Liver Transplants Rarely Receive Adequate Palliative Care or Appropriate Management. Clinical Gastroenterology and Hepatology. 2014;12(4):692–698. [DOI] [PubMed] [Google Scholar]
- 13.Patel AA, Walling AM, Ricks-Oddie J, May FP, Saab S, Wenger N. Palliative Care and Health Care Utilization for Patients With End-Stage Liver Disease at the End of Life. Clin Gastroenterol Hepatol. 2017;15(10):1612–1619.e1614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.El-Jawahri A, LeBlanc TW, Burns LJ, et al. What do transplant physicians think about palliative care? A national survey study. Cancer. 2018;124(23):4556–4566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kavalieratos D, Mitchell EM, Carey TS, et al. “Not the ‘grim reaper service’“: an assessment of provider knowledge, attitudes, and perceptions regarding palliative care referral barriers in heart failure. J Am Heart Assoc. 2014;3(1):e000544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.LeBlanc TW, O’Donnell JD, Crowley-Matoka M, et al. Perceptions of palliative care among hematologic malignancy specialists: a mixed-methods study. J Oncol Pract. 2015;11(2):e230–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Beck KR, Pantilat SZ, O’Riordan DL, Peters MG. Use of Palliative Care Consultation for Patients with End-Stage Liver Disease: Survey of Liver Transplant Service Providers. Journal Of Palliative Medicine. 2016;19(8):836–841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Low J, Vickerstaff V, Davis S, et al. Palliative care for cirrhosis: a UK survey of health professionals’ perceptions, current practice and future needs. Frontline Gastroenterol. 2016;7(1):4–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cherny NI, Catane R, European Society of Medical Oncology Taskforce on P, Supportive C. Attitudes of medical oncologists toward palliative care for patients with advanced and incurable cancer: report on a survery by the European Society of Medical Oncology Taskforce on Palliative and Supportive Care. Cancer. 2003;98(11):2502–2510. [DOI] [PubMed] [Google Scholar]
- 20.Milne D, Aranda S, Jefford M, Schofield P. Development and validation of a measurement tool to assess perceptions of palliative care. Psycho-oncology. 2013;22(4):940–946. [DOI] [PubMed] [Google Scholar]
- 21.Nelson JE, Angus DC, Weissfeld LA, et al. End-of-life care for the critically ill: A national intensive care unit survey. Crit Care Med. 2006;34(10):2547–2553. [DOI] [PubMed] [Google Scholar]
- 22.Fadul N, Elsayem A, Palmer JL, et al. Supportive versus palliative care: what’s in a name?: a survey of medical oncologists and midlevel providers at a comprehensive cancer center. Cancer. 2009;115(9):2013–2021. [DOI] [PubMed] [Google Scholar]
- 23.Hui D, Park M, Liu D, Reddy A, Dalal S, Bruera E. Attitudes and Beliefs Toward Supportive and Palliative Care Referral Among Hematologic and Solid Tumor Oncology Specialists. Oncologist. 2015;20(11):1326–1332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Odejide OO, Cronin AM, Condron N, Earle CC, Wolfe J, Abel GA. Timeliness of End-of-Life Discussions for Blood Cancers: A National Survey of Hematologic Oncologists. JAMA Intern Med. 2016;176(2):263–265. [DOI] [PubMed] [Google Scholar]
- 25.Odejide OO, Cronin AM, Condron NB, et al. Barriers to Quality End-of-Life Care for Patients With Blood Cancers. J Clin Oncol. 2016;34(26):3126–3132. [DOI] [PubMed] [Google Scholar]
- 26.Durall A, Zurakowski D, Wolfe J. Barriers to conducting advance care discussions for children with life-threatening conditions. Pediatrics. 2012;129(4):e975–982. [DOI] [PubMed] [Google Scholar]
- 27.Colman RE, Curtis JR, Nelson JE, et al. Barriers to Optimal Palliative Care of Lung Transplant Candidates. Chest. 2013;143(3):736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brown J, Sorrell JH, McClaren J, Creswell JW. Waiting for a liver transplant. Qual Health Res. 2006;16(1):119–136. [DOI] [PubMed] [Google Scholar]
- 29.Martin SC, Stone AM, Scott AM, Brashers DE. Medical, personal, and social forms of uncertainty across the transplantation trajectory. Qual Health Res. 2010;20(2):182–196. [DOI] [PubMed] [Google Scholar]
- 30.About Palliative Care. Palliative Care Definition What is Palliative Care. CAPC. https://www.capc.org/about/palliative-care/. Accessed June 30, 2018. [Google Scholar]
- 31.El-Jawahri A, Traeger L, Greer JA, et al. Effect of Inpatient Palliative Care During Hematopoietic Stem-Cell Transplant on Psychological Distress 6 Months After Transplant: Results of a Randomized Clinical Trial. J Clin Oncol. 2017;35(32):3714–3721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.El-Jawahri A, LeBlanc T, VanDusen H, et al. Effect of Inpatient Palliative Care on Quality of Life 2 Weeks After Hematopoietic Stem Cell Transplantation: A Randomized Clinical Trial. JAMA. 2016;316(20):2094–2103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Davison SN, Levin A, Moss AH, et al. Executive summary of the KDIGO Controversies Conference on Supportive Care in Chronic Kidney Disease: developing a roadmap to improving quality care. Kidney Int. 2015;88(3):447–459. [DOI] [PubMed] [Google Scholar]
- 34.Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;62(16):e147–239. [DOI] [PubMed] [Google Scholar]
- 35.Fang JC, Ewald GA, Allen LA, et al. Advanced (stage D) heart failure: a statement from the Heart Failure Society of America Guidelines Committee. J Card Fail. 2015;21(6):519–534. [DOI] [PubMed] [Google Scholar]
- 36.Kelly SG, Campbell TC, Hillman L, Said A, Lucey MR, Agarwal PD. The Utilization of Palliative Care Services in Patients with Cirrhosis who have been Denied Liver Transplantation: A Single Center Retrospective Review. Ann Hepatol. 2017;16(3):395–401. [DOI] [PubMed] [Google Scholar]
- 37.Rush B, Walley KR, Celi LA, Rajoriya N, Brahmania M. Palliative Care Access for Hospitalized Patients with End Stage Liver Disease Across the United States. Hepatology. 2017. [DOI] [PubMed] [Google Scholar]
- 38.Roth K, Lynn J, Zhong Z, Borum M, Dawson NV. Dying with end stage liver disease with cirrhosis: insights from SUPPORT. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment. J Am Geriatr Soc. 2000;48(5 Suppl):S122–130. [PubMed] [Google Scholar]
- 39.Brisebois A, Ismond KP, Carbonneau M, Kowalczewski J, Tandon P. Advance care planning (ACP) for specialists managing cirrhosis: A focus on patient-centered care. Hepatology. 2018;67(5):2025–2040. [DOI] [PubMed] [Google Scholar]
- 40.Shalev A, Phongtankuel V, Kozlov E, Shen MJ, Adelman RD, Reid MC. Awareness and Misperceptions of Hospice and Palliative Care: A Population-Based Survey Study. Am J Hosp Palliat Care. 2018;35(3):431–439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Davison SN, Jhangri GS, Koffman J. Knowledge of and attitudes towards palliative care and hospice services among patients with advanced chronic kidney disease. BMJ Support Palliat Care. 2016;6(1):66–74. [DOI] [PubMed] [Google Scholar]
- 42.Zimmermann C, Swami N, Krzyzanowska M, et al. Perceptions of palliative care among patients with advanced cancer and their caregivers. CMAJ. 2016;188(10):E217–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rhondali W, Burt S, Wittenberg-Lyles E, Bruera E, Dalal S. Medical oncologists’ perception of palliative care programs and the impact of name change to supportive care on communication with patients during the referral process. A qualitative study. Palliat Support Care. 2013;11(5):397–404. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.