Abstract
Objective To evaluate the classification proposed by David Dejour to describe trochlear dysplasia of the knee through inter- and intraobserver reproducibility measurements.
Methods Ten patients with trochlear dysplasia were studied. Three physicians, members of the Sociedade Brasileira de Cirurgia do Joelho (Brazilian Society of Knee Surgery), were invited to evaluate the images. Intra- and interobserver analyses were performed at one-week intervals. Reproducibility was evaluated in four scenarios: using only radiography; using radiography and tomography; using radiography and consulting the classification; and using radiography and tomography, consulting the classification.
Results The intraobserver evaluation presented discordant results. In the interobserver analysis, the degree of agreement was low for the analyses that used only radiography and excellent for those in which both radiography and tomography were used.
Conclusion The Dejour classification presented a low intra- and interobserver reproducibility when only the profile radiography was used. It was demonstrated that the use of the radiography alone for classification may generate lack of uniformity even among experienced observers. However, when radiography and tomography were combined, reproducibility improved.
Keywords: femoropatellar joint, joint instability, reproducibility
Introduction
The patella, known as the largest sesamoid bone in the human body, is critical to the biomechanics of the knee joint. It increases the mechanical power of the extensor apparatus and protects the knee joint. 1
Patellofemoral syndrome is a term used to describe a condition in which the patellar course between the femoral condyles is inappropriate. This improper slip causes anterior knee pain and it may lead to degenerative changes or dislocation/instability of the patellofemoral joint. 2
Patellofemoral instability is a frequent condition, and it is associated with predisposing factors in most patients. The most important factors include femoral trochlea dysplasia and patellar height. 3
Patellar instability is more common among young women between 10 and 17 years-old. The dislocation rate after the first episode varies from 15 to 44%, following conservative treatment, and it is higher in patients who had more than one instability episode. 4
Trochlear dysplasia is characterized by abnormal trochlear morphology and a “shallow” groove. It is not clear whether trochlear dysplasia is a cause or a consequence of the instability. Thus, congenital alterations could lead to dysplastic trochlea, which would be less deep, favoring instability; alternatively, muscle changes would result in an abnormal patellar course, which would reduce patellofemoral pressure and generate an inadequate stimulus to trochlea anatomy development, rendering it flatter and dysplastic; lastly, trochlear dysplasia might result from a combination of these factors. 3 5
Imaging techniques show many signs, allowing the identification of large and small anatomical abnormalities and helping the establishment of treatment plan. 6 7 8 9 Lateral radiographic images are critical in trochlear dysplasia evaluation and classification and in high patella quantification. Axial views allow the measurement of intercondylar line angles and congruence. 10 Computed tomography (CT) scans allow the definition of distance between the tibial tuberosity and trochlear groove (TT-TG), slope value and rotational characteristics, in addition of evaluating trochlear dysplasia. 11 Magnetic resonance imaging (MRI) is valuable in acute dislocations and may show a rupture of the medial patellofemoral ligament, as well as osteochondral lesions and bone contusions. 12
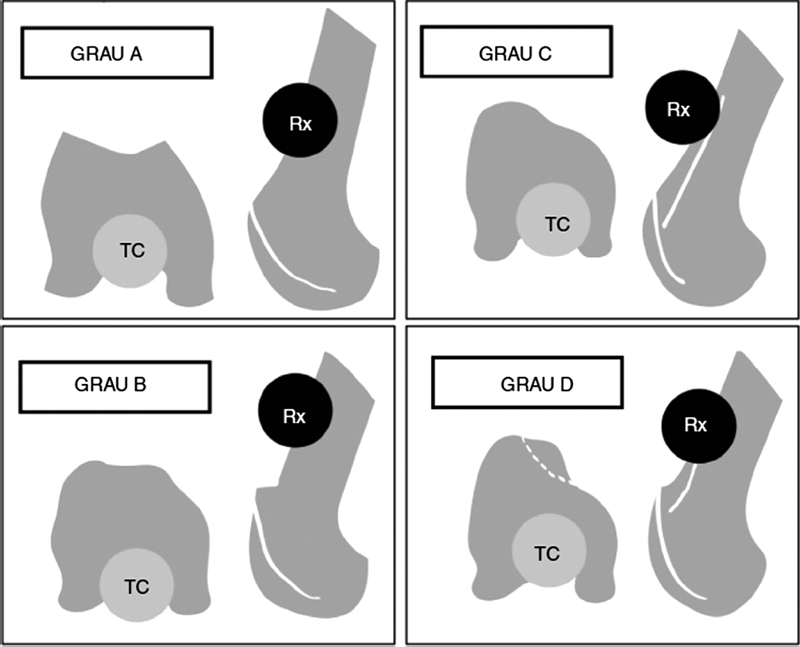
Trochlear dysplasia was well evaluated and graded by Dejour using images. 13 Assisted by radiography and CT scans, Dejour 14 classified dysplasia in types A, B, C and D 15 ( Fig. 1 ).
Fig. 1.
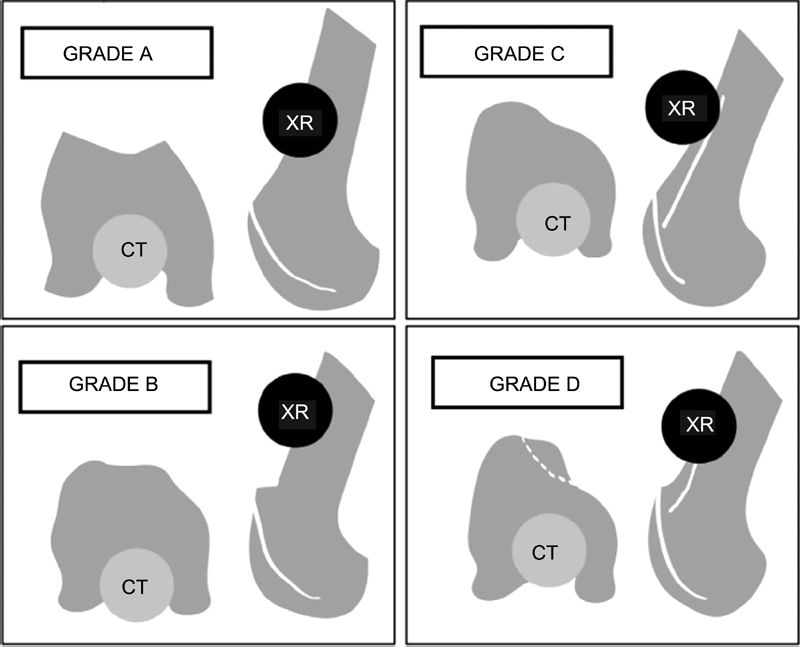
Dejour classification of trochlear dysplasia 14 (radiography and computed tomography scan). Abbreviations: CT, computed tomography; XR, X-ray.
As already mentioned, the Dejour classification is important for the treatment of the patient with trochlear dysplasia. However, a feature that must be present in any classification is its reproducibility. 16 As such, classification should be simple, easy to memorize and assist in the choice of treatment, guide the prognosis and facilitate communication between health care professionals. 16
Thus, the main objective of the present study is to evaluate, through interobserver and intraobserver reproducibility measurements, the classification proposed by David Dejour 14 to describe knee trochlear dysplasia.
Material and Methods
The study was approved by the Ethics Committee under number CAAE 67648217.3.0000.5049. All participants agreed and signed the informed consent form delivered before the start of the study. No financial incentive was offered for the patients to participate and volunteers could refuse participation in the study or withdraw their consent at any time, without the need of justifying their decision.
Ten subjects diagnosed with patellofemoral instability were randomly selected at the outpatient facility, with no gender or age restriction. All patients underwent radiographic examinations to monitor their conditions. No additional imaging was requested in this study, which used only images already available.
We asked the patients for a copy of their most recent imaging tests: a lateral radiograph and a cross-sectional CT scan of the affected knee, recorded on digital media, such as CD-ROM.
Exclusion criteria included individuals who reported previous surgery of the knee in question and who did not have radiological images prior to this procedure. No participant was excluded due to these criteria.
Three observers, all members of the Sociedade Brasileira de Cirurgia do Joelho (Brazilian Society of Knee Surgery), were invited to analyze the images. Scanned images were delivered on CD-ROM (copied after patient authorization) to the observers. To minimize bias, due to interpretation difficulty or possible forgetfulness, the classification and its variants are described in Fig. 1 . Radiographic analyzes were performed blindly and briefly preceded by a classification review ( Fig. 1 ). The three examiners, separately and without contact with each other, evaluated the images of the 10 subjects. First, they classified them (as Dejour A, B, C or D) using only with the lateral radiography (Analysis 1) and, then, using both the CT scan and the radiography (Analysis 2).
After one week, the same images were randomized and examined by the same evaluators. First, they classified them (as Dejour A, B, C or D) using only the lateral radiography (Analysis 3) and, then, using both the CT scan and the radiography (Analysis 4).
Shortly after this second evaluation, the same observers again classified the lateral radiography and then the CT scan, but this time they could consult the classification during analysis (Analysis 5 and 6).
The inter- and intraobserver variations of the tabulated data were analyzed by SPSS (Statistical Package for the Social Sciences), v23, SPSS, Inc. Comparisons with p -values up to 0.05, with a confidence interval of 95%, were considered significant. Agreement analysis among evaluators used the Kendall coefficient (W) ( Table 1 ). They were categorized in an ordinal scale with the Dejour classification, in which A = 1 / B = 2 / C = 3 / 4 = D.
Table 1. Kendall W degree of concordance among evaluators, from poor to excellent.
| Kendall W | Interpretation |
|---|---|
| < 0.4 | Poor |
| 0.400–0.599 | Regular |
| 0.600–0.800 | Good |
| > 0.8 | Excellent |
Results
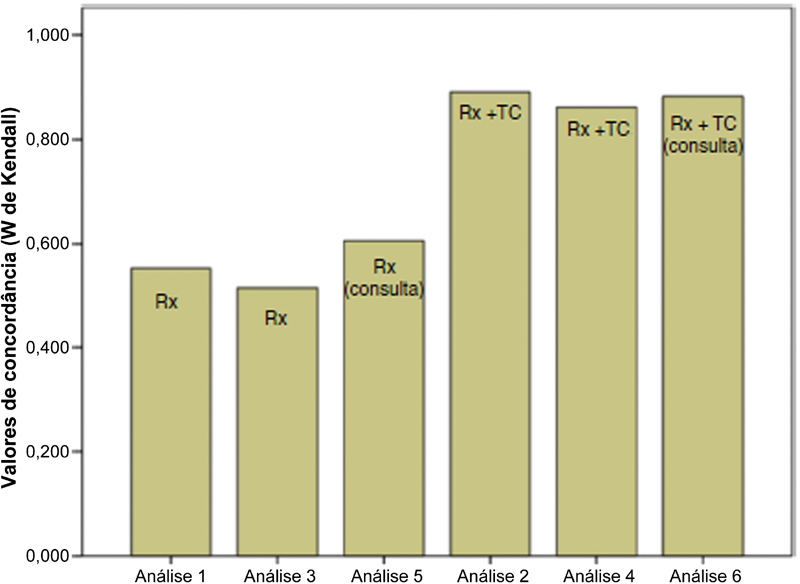
The interobserver variation was calculated from six situations: Analysis 1: evaluation of the classification only with a radiography; Analysis 2: evaluation with radiography and CT scan; Analysis 3: reevaluation after one week, only with a radiography; Analysis 4: reevaluation after one week, with radiography and CT scan; Analysis 5: evaluation with radiography and consulting the classification; Analysis 6: evaluation with radiography and CT scan and consulting the classification ( Table 2 and Fig. 2 ).
Table 2. Interobserver variation at the six proposed situations.
| Situation | Kendall W | Chi-square | df | Asymptotic significance ( p ) |
|---|---|---|---|---|
| Analysis 1 (XR) | 0.553 | 14.931 | 9 | 0.093 |
| Analysis 2 (XR + CT) | 0.891 | 24.058 | 9 | 0.004 |
| Analysis 3 (XR) | 0.515 | 13.903 | 9 | 0.126 |
| Analysis 4 (XR + CT) | 0.861 | 23.238 | 9 | 0.006 |
| Analysis 5 (XR + visit) | 0.606 | 16.354 | 9 | 0.060 |
| Analysis 6 (XR + CT + visit) | 0.883 | 23.840 | 9 | 0.005 |
Abbreviations: CT, computed tomography; df, degrees of freedom; XR X-ray.
Fig. 2.
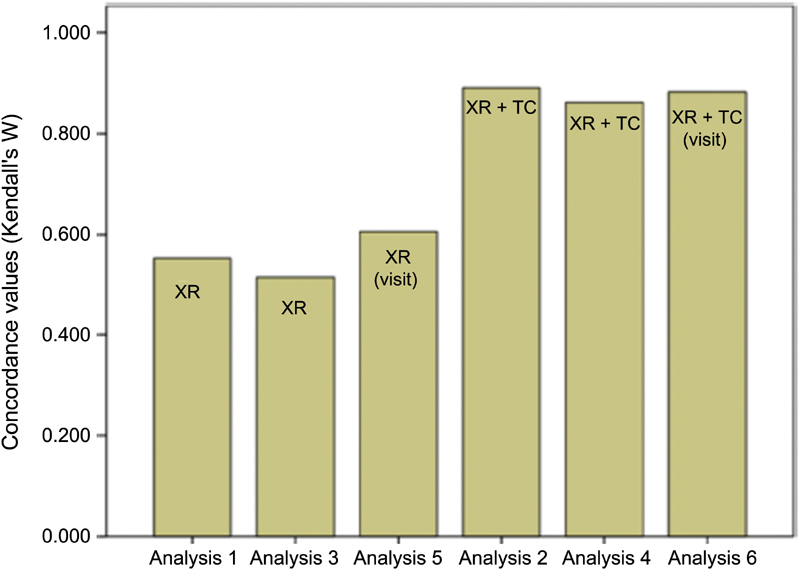
Interobserver variation at the six proposed situations. Abbreviations: CT, computed tomography; XR, X-ray.
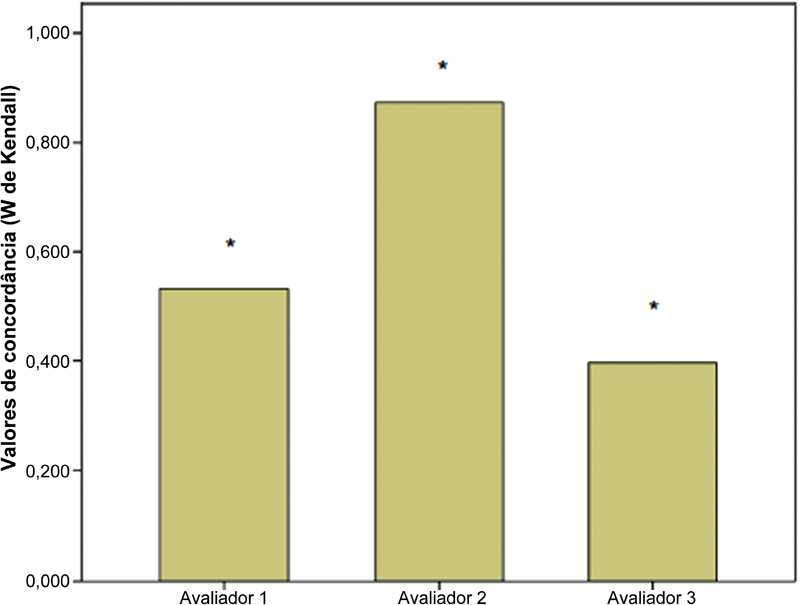
The intraobserver variation was expressed in Kendall concordance values between the three evaluators for each type of evaluation (Table 3 and Fig. 3 ).
Table 3. Intraobserver variation.
| Kendall W | Chi-square | df | Asymptotic significance ( p ) | |
|---|---|---|---|---|
| Evaluator 1 | 0.532 | 28.716 | 9 | 0.001 |
| Evaluator 2 | 0.873 | 47.143 | 9 | 0.000 |
| Evaluator 3 | 0.397 | 21.422 | 9 | 0.011 |
Abbreviations: df, degrees of freedom.
Fig. 3.
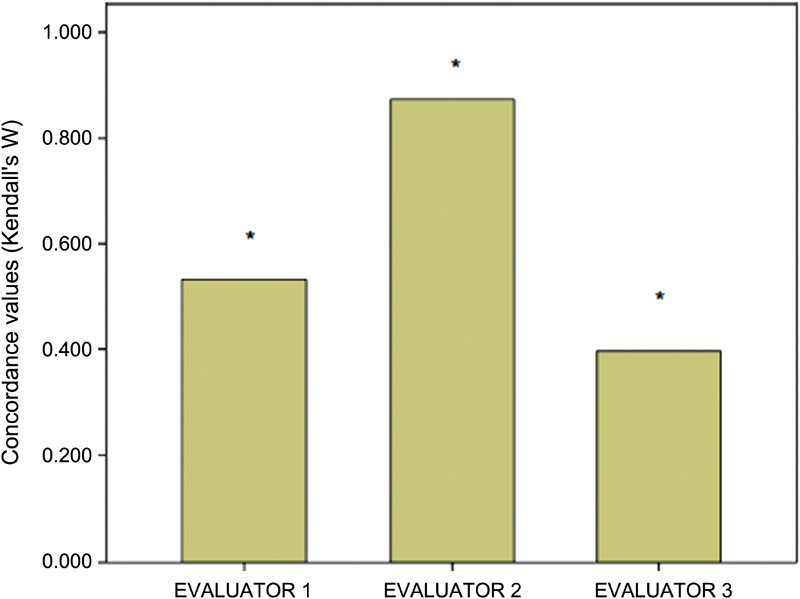
Intraobserver variation ( * p < 0.05).
Discussion
The classification of diseases is a common practice, especially in orthopedics and traumatology. A good classification system is intended to be simple, reproducible and capable of grouping different stages of an injury into homogeneous subgroups to allow comparisons and the development of therapeutic and prognostic algorithms. 16 The problem with classifications, however, is the occasional case that does not fit the description. Thus, over time, some classifications have been replaced by others, more complete. 17
The stability of the patellofemoral joint is critical to the proper functioning of the extensor knee mechanism and joint as a whole. 18 However, it has a low degree of congruence, as established by the balance of the bone architecture and soft tissues restrictions. Anatomical changes are not uncommon, and instability may occur as a result of mechanical imbalance. The clinical instability scenario, however, has a spectrum of manifestations. Thus, it is important to differentiate patients who have symptoms, but not anatomical abnormalities, from those with subdislocation and/or dislocation. 19
According to Dejour et al, 6 four main anatomical factors result in instability 6 20 :
Patellar face dysplasia or Trochlear dysplasia: the shape of the patellar face is abnormal and the bone restraint to patellar deviation is lost; 6 20
Excessive distance between tibial tuberosity and the trochlear groove (TT-TG): a condition associated with poor alignment of the extensor mechanism, resulting in a valgus vector acting on the patella; 6 20
Patellar slope: due to the insufficiency of the medial restraints, patellar dysplasia also plays an important role as a causative agent; 6 20
High patella: A condition in which the patella, due to the advancement of flexion, is unstable in the femoral patellar due to the altered lever arm. 6 20
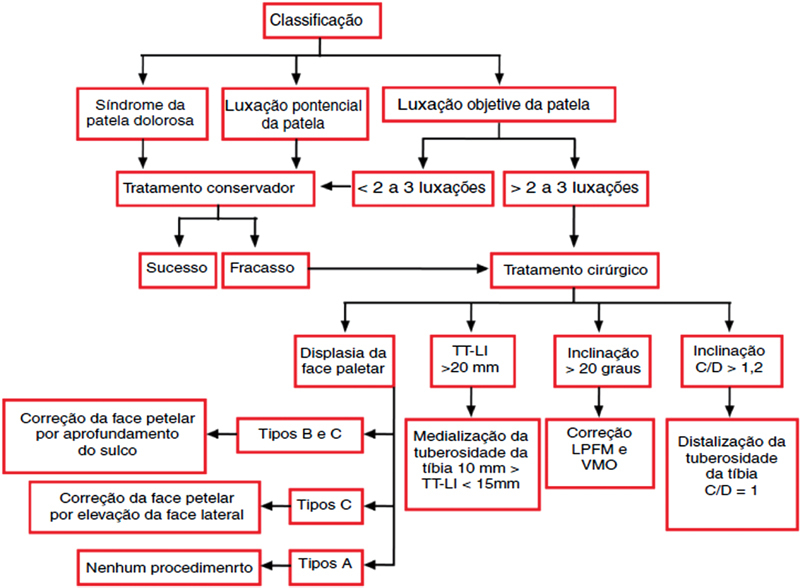
Treatment may be conservative or surgical, following a flowchart in which several factors are considered ( Fig. 4 ). 18
Fig. 4.
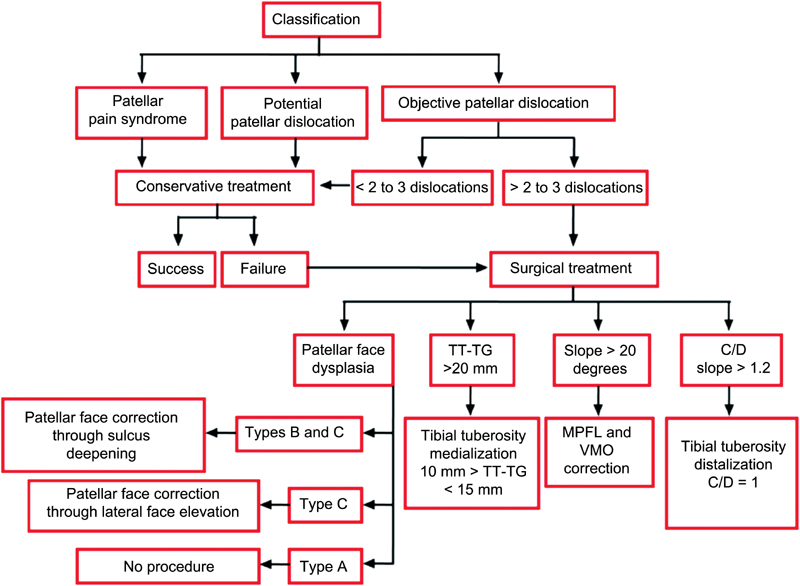
Flow chart for patellofemoral instability treatment. 18 Abbreviations: TT-TG; tibial tuberosity and trochlear groove; MPFL, medial patellofemoral ligament; VMO, vastus medialis obliquus.
The main factors include: number of dislocations; conservative treatment failure; increased TT-TG distance; increased patellar slope; high patella; and trochlear dysplasia (quantified by the Dejour classification and discussed in our study). 18 20
As such, for many authors, the current classification is a therapeutic guide. Therefore, it is critical that the classification presents good reproducibility.
Lippacher et al 21 compared the reproducibility of the classification in 50 radiographs and 50 magnetic resonance imaging (MRI) scans and concluded that the Dejour classification is valid for dysplasia, being particularly useful in the differentiation between low (A) and high degree (B-D) lesions.
Rémy et al 22 evaluated the reproducibility of the classification only with lateral radiographs and concluded that it had low intra- and interobserver agreement.
A study by Nelitz et al 23 highlights the limited value of the classification, since it is useful only to differentiate high and low dysplasia degrees.
In the present study, we performed an analysis in four scenarios, using only a lateral radiography; a radiography and a CT scan; a radiography and the classification; and a radiography, a CT scan and the classification.
Figures and Table 2 show that, even consulting the classification during analysis, the interobserver variation using only a lateral radiography has a Kendall W that is not too high. However, analyses using radiography and CT scans had a Kendall W coefficient greater than 0.8, which expresses excellent agreement.
At the intraobserver evaluation, according to Table 1 , agreement was excellent for the first evaluator, regular for the second evaluator and poor for the third evaluator ( Table 3 and Fig. 3 ).
Conclusion
The Dejour classification generated a low intraobserver and interobserver reproducibility when only the lateral radiography was used.
It has been shown that the use only of radiographies for the classification can generate lack of uniformity even among experienced observers.
However, the use of radiography and CT scans improved reproducibility.
Conflitos de interesse Os autores declaram não haver conflitos de interesse.
Trabalho desenvolvido no Departamento de Ortopedia e Traumatologia, Centro Universitário Christus (Unichristus), Fortaleza, CE, Brasil. Originalmente publicado por Elsevier Ltda.
Work developed at the Department of Orthopedics and Traumatology of Centro Universitário Christus (Unichristus), Fortaleza, CE, Brazil.
References
- 1.Ribeiro M M, Nogueira F, Sardinha J, Jones J H. Critérios imagiológicos da instabilidade femoro-patelar por ressonância magnética. Rev Port Ortop Traumatol. 2012;20(04):425–435. [Google Scholar]
- 2.Ferrari D, Kuriki H U, Silva C R, Alves N, Mícolis de Azevedo F. Diagnostic accuracy of the electromyography parameters associated with anterior knee pain in the diagnosis of patellofemoral pain syndrome. Arch Phys Med Rehabil. 2014;95(08):1521–1526. doi: 10.1016/j.apmr.2014.03.028. [DOI] [PubMed] [Google Scholar]
- 3.Rebouças Moreira T A, Demange M K, Gobbi R G, Mustacchi Z, Pécora J R, Passarelli Tírico L E et al. Trochlear dysplasia and patellar instability in patients with Down syndrome. Rev Bras Ortop. 2015;50(02):159–163. doi: 10.1016/j.rboe.2015.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fithian D C, Paxton E W, Stone M L, Silva P, Davis D K, Elias D A et al. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med. 2004;32(05):1114–1121. doi: 10.1177/0363546503260788. [DOI] [PubMed] [Google Scholar]
- 5.Bollier M, Fulkerson J P. The role of trochlear dysplasia in patellofemoral instability. J Am Acad Orthop Surg. 2011;19(01):8–16. doi: 10.5435/00124635-201101000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2(01):19–26. doi: 10.1007/BF01552649. [DOI] [PubMed] [Google Scholar]
- 7.Steiner T M, Torga-Spak R, Teitge R A. Medial patellofemoral ligament reconstruction in patients with lateral patellar instability and trochlear dysplasia. Am J Sports Med. 2006;34(08):1254–1261. doi: 10.1177/0363546505285584. [DOI] [PubMed] [Google Scholar]
- 8.White B J, Sherman O H. Patellofemoral instability. Bull NYU Hosp Jt Dis. 2009;67(01):22–29. [PubMed] [Google Scholar]
- 9.Fulkerson J P. Diagnosis and treatment of patients with patellofemoral pain. Am J Sports Med. 2002;30(03):447–456. doi: 10.1177/03635465020300032501. [DOI] [PubMed] [Google Scholar]
- 10.Schöttle P B, Schmeling A, Rosenstiel N, Weiler A. Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35(05):801–804. doi: 10.1177/0363546506296415. [DOI] [PubMed] [Google Scholar]
- 11.Gigante A, Pasquinelli F M, Paladini P, Ulisse S, Greco F. The effects of patellar taping on patellofemoral incongruence. A computed tomography study. Am J Sports Med. 2001;29(01):88–92. doi: 10.1177/03635465010290011901. [DOI] [PubMed] [Google Scholar]
- 12.Carrillon Y, Abidi H, Dejour D, Fantino O, Moyen B, Tran-Minh V A. Patellar instability: assessment on MR images by measuring the lateral trochlear inclination-initial experience. Radiology. 2000;216(02):582–585. doi: 10.1148/radiology.216.2.r00au07582. [DOI] [PubMed] [Google Scholar]
- 13.Dejour H, Walch G. 1987. La pathologie femoro-patellaire. [PubMed] [Google Scholar]
- 14.Dejour D, Reynaud P, Lecoultre B.Douleurs et instabilité rotulienne, Essai de classification Med Hyg (Geneve) 199856(2217):1466–1471. [Google Scholar]
- 15.Burmann R C, Locks R, Pozzi J F, Konkewicz E R, Souza M P. Avaliac¸ão dos fatores predisponentes nas instabilidades femoropatelares. Acta Ortop Bras. 2011;19(01):37–40. [Google Scholar]
- 16.Albuquerque R P, Giordano V, Sturm L, Azevedo Júnior V, Leão A, Amaral N P. Análise da reprodutibilidade de três classificações para a osteoartrose do joelho. Rev Bras Ortop. 2008;43(08):329–335. [Google Scholar]
- 17.Gonc¸ alves FB, Rocha FA, Albuquerque RP, Mozella AP, Crespo B, Cobra H. Avaliac¸ão da reprodutibilidade das diferentes descric¸ ões da classificac¸ão de Kellgren e Lawrence para osteoartrite do joelho. Rev Bras Ortop. 2016;51(06):687–689. doi: 10.1016/j.rboe.2016.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Scott W N. Philadelphia: Churchill Livingstone; 2011. Insall & Scott surgery of the knee. [Google Scholar]
- 19.Azar F M, Canale S T, Beaty J H. Philadelphia: Elsevier Health Sciences; 2013. Campbell's operative orthopaedics. [Google Scholar]
- 20.Scott W N. Philadelphia: Elsevier Health Sciences; 2017. Insall & Scott Surgery of the Knee. [Google Scholar]
- 21.Lippacher S, Dejour D, Elsharkawi M, Dornacher D, Ring C, Dreyhaupt J et al. Observer agreement on the Dejour trochlear dysplasia classification: a comparison of true lateral radiographs and axial magnetic resonance images. Am J Sports Med. 2012;40(04):837–843. doi: 10.1177/0363546511433028. [DOI] [PubMed] [Google Scholar]
- 22.Rémy F, Chantelot C, Fontaine C, Demondion X, Migaud H, Gougeon F. Inter- and intraobserver reproducibility in radiographic diagnosis and classification of femoral trochlear dysplasia. Surg Radiol Anat. 1998;20(04):285–289. doi: 10.1007/BF01628492. [DOI] [PubMed] [Google Scholar]
- 23.Nelitz M, Lippacher S, Reichel H, Dornacher D. Evaluation of trochlear dysplasia using MRI: correlation between the classification system of Dejour and objective parameters of trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc. 2014;22(01):120–127. doi: 10.1007/s00167-012-2321-y. [DOI] [PubMed] [Google Scholar]