Abstract
Objective To describe the surgical technique of distal closing-wedge femoral osteotomy and a cases series submitted to this technique.
Methods A total of 26 patients submitted to medial closing-wedge distal femoral osteotomy from 2002 to 2013 were evaluated. All of the patients had their medical files and imaging exams reviewed to evaluate the degree of correction and their current state.
Results Out of the 26 patients, 12 were male and 14 were female. Their mean age was 47.15 years old. In all of the cases, a neutral alignment related to the anatomical axis was achieved. Most of the patients presented bone healing at 6 weeks. There were no cases of bleeding during the surgery. One patient presented with delayed bone healing. One patient complained of plaque-related discomfort, requiring the removal of the device. One patient had a superficial infection, but no osteotomy revision was needed. There were no cases of deep venous thrombosis or of pulmonary thromboembolism. To date, there has been no conversion to total knee replacement.
Conclusion Treatment with medial closing-wedge distal femoral osteotomy sustained the proposed correction in patients with up to 15 years of follow-up.
Keywords: osteotomy, femur, knee, osteoarthritis, genu valgum
Introduction
Osteoarthritis (OA) is a degenerative joint disease observed in the general population. The knee is the main peripheral joint affected, resulting in progressive functional loss, joint pain, and stiffness. It is estimated that ∼ 10% of the population > 50 years old will be affected by this condition. 1
The surgical osteotomy technique for long bones on the lower limbs (the femur and the tibia) aims to change the alignment of the affected limb, slowing down the evolutionary process of OA. As a result, it improves pain and limb function, and it can postpone knee replacement procedures, such as knee arthroplasty, for up to 10 years. 2
Distal femoral osteotomy is a well-accepted procedure for the treatment of unicompartmental OA in the early stages of valgus knee. Chahla et al report that the best outcomes are obtained when osteotomies are performed in patients < 55 years old. 1 3 4 5
Femoral osteotomy may be performed as lateral opening-wedge or medial closing-wedge. On average, the deformity must be corrected to obtain a neutral anatomical alignment. However, there is no evidence in the literature about the superiority of the medial closing-wedge technique over the lateral opening-wedge. 4 6
The present study aims to describe the surgical technique and a case series submitted to femoral osteotomy with medial closing-wedge in a referral service, and to evaluate the current characteristics resulting from this procedure in up to 15 years of follow-up.
Materials and Methods
The present study was evaluated and approved by the Ethics and Research Committee of this institution under the number CAAE 01609812.9.0000.5505.
A total of 26 patients who underwent a distal femoral osteotomy with medial closing-wedge from 2002 to 2013 were evaluated. One of the patients was submitted to bilateral osteotomy, with a total of 27 operated knees.
Medical files and imaging results from all of the patients were reviewed to collect data regarding gender, age at surgery, laterality, deformity, and intraoperative complications. Next, the patients were clinically analyzed with their imaging results to characterize their current status: treatment failure, required conversion to total knee arthroplasty, and other complications.
Surgical Technique
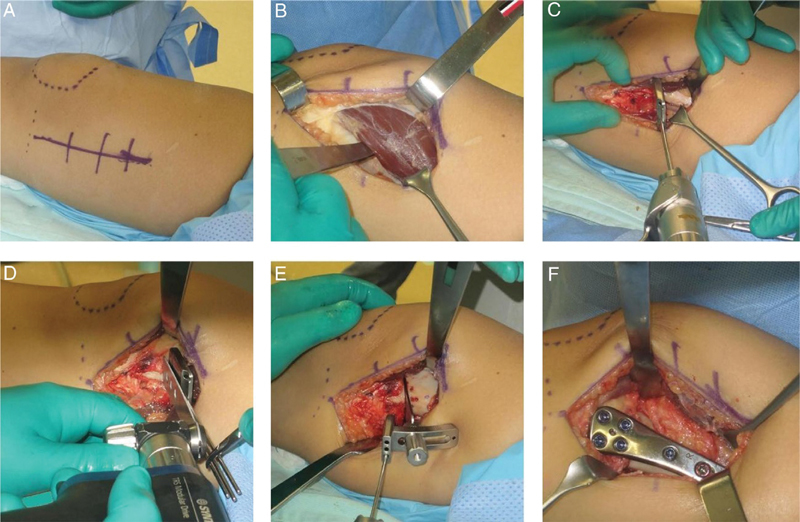
With the patient positioned in the supine position on a radiolucent table, the articular surface was identified by palpation and radioscopy. An incision of ∼ 10 cm was performed, extending proximally from the medial knee joint line. Next, the vastus medialis was bluntly dissected to expose the condyle and the medial femoral cortex. Thus, no neurovascular structure was exposed or put at risk during the surgical access, and the bone surface required for osteotomy was safely approached. The diaphyseal midline was marked with an electrocautery and a Codman pen to avoid angular deviation during the stabilization of the plaque. With a guide plate, parallel pins were positioned to aid the wedge cut. Then, the proximal part of the osteotomy was performed. The wedge guidewire was positioned with the angular cut predefined for each case, and ∼ 75% of the wedge was sectioned and removed; this was considered a partial procedure. The osteotomy was checked with radioscopy and stabilized with an angled blade plaque at 90° in older cases or locked with proximal and distal screws in the most recent ones ( Fig. 1 ).
Fig. 1.
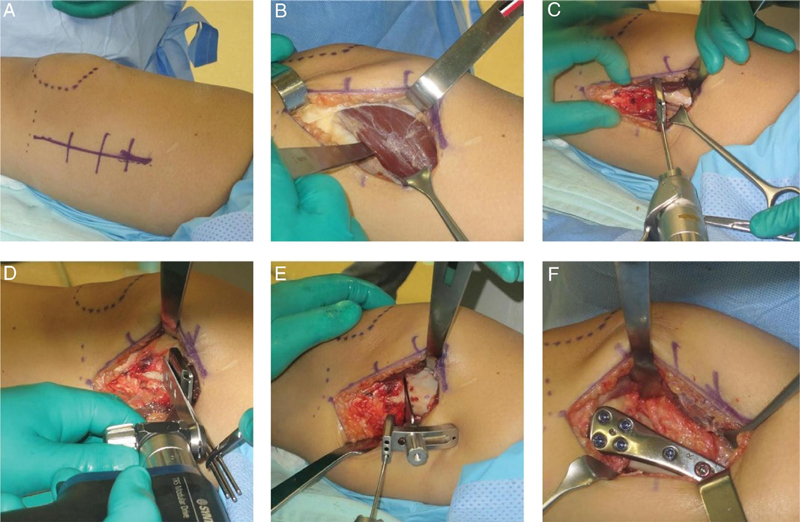
A, joint line marking, patella and surgical access; B, subvastus retractor placement; C, parallel pins with guide plate placement; D, proximal part of the osteotomy; E, placement of pins on the wedge cutting guide to complete the osteotomy; F, plate placed after osteotomy.
Results
Out of the 26 patients, 12 were male and 14 were female. Their mean age was 47.15 years old (ranging from 25 to 61 years old). Regarding the side, 13 patients underwent left femur osteotomies, 12 underwent right femur osteotomies, and 1 patient underwent a bilateral osteotomy, totaling 27 distal femoral osteotomies.
The valgus deformity ranged from 13° to 18° before the surgery. After the osteotomy, all of the cases achieved a neutral anatomical alignment, with the valgus angle ranging from 0° to 1°.
There was no significant bleeding during the surgery. Neurovascular injuries due to surgical access were not reported.
In most patients, osteotomy bone healing occurred at 6 weeks (ranging from 6 to 16 weeks). Consolidation was defined according to the serial radiographic follow-up.
A female patient presented with delayed consolidation and with a fracture after falling from her own height. The lesion was submitted to medial and lateral stabilization for bone consolidation.
One patient presented with persistent discomfort on the plaque despite conservative treatment. After 1 year, we decided to remove the synthesis material. This surgical procedure lead to pain relief.
One patient had a superficial infection treated with cleansing and antibiotics, with no need for the removal of the plaque and of the screws.
There were no cases of deep venous thrombosis or of pulmonary thromboembolism. There was no conversion to total knee arthroplasty in a follow-up of at least 5 years.
Discussion
Femoral varization osteotomy is a surgical technique usually used to correct deformities in the knee valgus. This procedure can be performed in selected patients with lateral knee compartment overload to reduce the increased pressure between the lateral femoral condyle and the lateral tibial plateau. In 27 osteotomies, the mean age was 47.15 years old, ranging from 25 to 61 years old. The youngest osteotomy patient (25 years old) was a soccer player who had a previous lateral meniscectomy and evolved with rapid osteoarthritis progression, probably due to high sports demand. 5 6 In the systematic review with 248 knees from Chahla et al, 4 the mean age of the patients was 48.9 years old.
Although OA is more prevalent in females, 6 the literature is inconclusive as to the gender in which the procedure is most frequently performed. 6 7 In our study, 12 osteotomy patients were male, whereas 14 were female.
The main discussion about femoral distal varization osteotomy continues to be which technique should be applied: medial closing-wedge or lateral opening-wedge. The latter technique is more popular. This is probably because most surgeons consider it easier and safer due to their familiarity with the surgical access. 4 8 Medial closing-wedge osteotomies seemed to have more complications, but a great deal of this information came from older studies, in which surgeons used clamping methods rather than additional plates and screws. 9 We believe that the medial closing-wedge technique allows a more anatomical correction with a shorter consolidation time. In addition, it eliminates the need for bone grafting and earlier loading on the operated limb. The neurovascular risk, commonly described as the main cause of the lack of popularity of this technique, is low when the surgical approach is properly made. In our series, there was no case of complication or of neurovascular involvement. 4 8 Visser et al, 8 in a cadaver study, corroborate this data and discuss about the safety of the medial approach for plaque placement. These authors also point out that vastus medialis damage and the risk of neurovascular lesions are marginal, even with the minimally invasive technique.
In most patients, bone healing was achieved 6 weeks after the surgery. On average, studies cite that bone healing occurs in between 6 and 8 weeks. Only one patient presented with delayed consolidation. This patient was a long-time smoker and chose not to stop smoking during the postoperative period, which corroborates the increased risk of delayed bone healing. 4 10 11
In addition, plaque-related discomfort is a complication reported in the literature. 4 One of our patients presented this complication. A probable reason for that was his low body weight and the fact that the muscular mass of the vastus medial would not properly cover the plaque, generating this discomfort. 3 4 Forkel et al, in a follow-up of 23 patients submitted to femoral medial closing-wedge osteotomy, reported 16 individuals with plaque-related discomfort We have decided to remove the synthesis material after the adequate time. The removal of the plaque resulted in the improvement of the symptoms. 12 13
Finally, surgical infection is an event that, despite preoperative, intraoperative, and postoperative measures, may occur in some cases. One patient from the present study had a superficial infection which was treated with antibiotic therapy and surgical cleaning. There was no need for synthesis material review. 4 9 10 11 12
Whenever required, pharmacological and nonpharmacological measures were used to avoid the most serious events reported in the literature, that is, deep vein thrombosis and pulmonary embolism. However, none of our patients had any of these complications. 2 4
Wylie et al, 10 in another systematic review, showed that the 10-year survival rate after medial closing-wedge osteotomies was of 82%. Chahla et al 4 showed that the mean survival rate ranged from 64 to 89.9% in the same 10-year follow-up period. In a follow-up of up to 15 years, this same study showed a much lower survival rate, from 45 to 78.9%. In our follow-up of up to 15 years, conversion to knee arthroplasty was not necessary until now. 4 10
Conclusion
Distal femoral medial closing-wedge osteotomy is a procedure that sustains the proposed correction in patients with up to 15 years of follow-up with very few complications resulting from the surgery.
Conflitos de interesse Os autores declaram não haver conflitos de interesse.
Trabalho desenvolvido no Centro de Traumatologia do Esporte, Departamento de Ortopedia e Traumatologia, Escola Paulista de Medicina, Universidade Federal de São Paulo, São Paulo, SP, Brasil. Publicado originalmente por Elsevier Ltda.
Work developed at the Centro de Traumatologia do Esporte, Departamento de Ortopedia e Traumatologia, Escola Paulista de Medicina, Universidade Federal de São Paulo, São Paulo, SP, Brazil.
References
- 1.Hussain S M, Neilly D W, Baliga S, Patil S, Meek R. Knee osteoarthritis: a review of management options. Scott Med J. 2016;61(01):7–16. doi: 10.1177/0036933015619588. [DOI] [PubMed] [Google Scholar]
- 2.Brouwer R W, Raaij van T M, Bierma-Zeinstra S M, Verhagen A P, Jakma T S, Verhaar J A. Osteotomy for treating knee osteoarthritis. Cochrane Database Syst Rev. 2007;(03):CD004019. doi: 10.1002/14651858.CD004019.pub3. [DOI] [PubMed] [Google Scholar]
- 3.Haviv B, Bronak S, Thein R, Thein R. The results of corrective osteotomy for valgus arthritic knees. Knee Surg Sports Traumatol Arthrosc. 2013;21(01):49–56. doi: 10.1007/s00167-012-2180-6. [DOI] [PubMed] [Google Scholar]
- 4.Chahla J, Mitchell J J, Liechti D J, Moatshe G, Menge T J, Dean C S et al. Opening- and closing-wedge distal femoral osteotomy: a systematic review of outcomes for isolated lateral compartment osteoarthritis. Orthop J Sports Med. 2016;4(06):2.325967116649901E15. doi: 10.1177/2325967116649901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hoorntje A, Witjes S, Kuijer P PFM, Koenraadt K LM, van Geenen R CI, Daams J G et al. High rates of return to sports activities and work after osteotomies around the knee: a systematic review and meta-analysis. Sports Med. 2017;47(11):2219–2244. doi: 10.1007/s40279-017-0726-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Leone J M, Hansse A D. Rio de Janeiro: Elsevier; 2014. Osteotomia ao redor do joelho: perspectiva americana. In: Scott NW, ed. Insall & Scott cirurgia do joelho. 5 a. ed; pp. 2070–2105. [Google Scholar]
- 7.Murphy G A. Philadelphia: Elsevier; 2017. Total ankle arthroplasty; pp. 508–534. [Google Scholar]
- 8.Visser J, Brinkman J M, Bleys R L, Castelein R M, van Heerwaarden R J. The safety and feasibility of a less invasive distal femur closing wedge osteotomy technique: a cadaveric dissection study of the medial aspect of the distal femur. Knee Surg Sports Traumatol Arthrosc. 2013;21(01):220–227. doi: 10.1007/s00167-012-2133-0. [DOI] [PubMed] [Google Scholar]
- 9.Gardiner A, Richmond J C. Periarticular osteotomies for degenerative joint disease of the knee. Sports Med Arthrosc Rev. 2013;21(01):38–46. doi: 10.1097/JSA.0b013e31826d2f5d. [DOI] [PubMed] [Google Scholar]
- 10.Wylie J D, Jones D L, Hartley M K et al. Distal femoral osteotomy for the valgus knee: medial closing wedge versus lateral opening wedge: a systematic review. Arthroscopy. 2016;32(10):2141–2147. doi: 10.1016/j.arthro.2016.04.010. [DOI] [PubMed] [Google Scholar]
- 11.Lobenhoffer P, Kley K, Freiling D, van Heerwaarden R. [Medial closed wedge osteotomy of the distal femur in biplanar technique and a specific plate fixator] Oper Orthop Traumatol. 2017;29(04):306–309. doi: 10.1007/s00064-017-0493-9. [DOI] [PubMed] [Google Scholar]
- 12.Shantz J S, Marcucio R, Kim H T, Miclau T, Court-Brown C M, Heckman J D, Mcqueen M M, Ricci W M, Tornetta P.Bone and cartilage healingIn:, eds.Rockwood and Green's fractures in adults Philadelphia: Wolters Kluwer; 2015109–125. [Google Scholar]
- 13.Forkel P, Achtnich A, Metzlaff S, Zantop T, Petersen W. Midterm results following medial closed wedge distal femoral osteotomy stabilized with a locking internal fixation device. Knee Surg Sports Traumatol Arthrosc. 2015;23(07):2061–2067. doi: 10.1007/s00167-014-2953-1. [DOI] [PubMed] [Google Scholar]