Abstract
Aims
Left ventricular diastolic pressure estimation is essential for characterization of heart failure (HF). Patients with normal resting left atrial (LA) pressures (LAP), but steep LAP elevation on exertion, pose a particular diagnostic challenge. Current recommendations on echocardiographic LAP estimation have limited accuracy. Our aim was to investigate whether LA mechanical alterations assessed by LA strain (LA-GS) can contribute to non-invasive LAP diagnostics.
Methods and results
Simultaneous echocardiographic and right heart catheterization (RHC) data at rest and during exercise was analyzed in 164 prospectively enrolled patients, referred for RHC due to HF symptoms. 56% had preserved ejection fraction (pEF). At rest, 97 patients displayed elevated mean pulmonary arterial wedge pressure (PAWPM); further 32 patients had normal resting, but elevated PAWPM during exercise. LA-GS demonstrated a stronger relationship with resting PAWPM (r = − 0.61, p < 0.001) than any of the indices (E/e′, LAVi, TRVmax) incorporated in the currently recommended diagnostic algorithm. The diagnostic ability of LA-GS for detecting elevated resting PAWPM (AUC: 0.80, p < 0.001) outperformed that of the recommended algorithm (AUC: 0.69). Importantly, resting LA-GS performed even better in identifying patients with pathological PAWPM either at rest or during stress (AUC: 0.90, p < 0.001), whereas the diagnostic potential of the current algorithm was modest and limited to pEF patients (AUC = 0.72). Finally, among the non-invasive indices, LA-GS entailed the strongest prognostic value for death or heart transplantation (OR: 2.7; p < 0.05).
Conclusion
LA-GS comprises a robust method for PAWPM assessment at rest. More importantly, it reliably discerns pathological PAWPM rise on exertion despite normal resting pressures.
Electronic supplementary material
The online version of this article (10.1007/s00392-018-1399-8) contains supplementary material, which is available to authorized users.
Keywords: Left atrial strain, Non-invasive, Invasive, Exercise, Diastolic pressures
Introduction
Diagnostic, prognostic and therapeutic reasons confer to the non-invasive estimation of left ventricular (LV) filling pressures fundamental importance when evaluating patients presenting with unexplained dyspnea as well as those with documented heart failure (HF). Despite extensive research and the availability of numerous metrics, the assessment of resting LV diastolic pressures is challenging. Even more puzzling is the non-invasive diagnostics of patients whose resting left atrial (LA) pressure (LAP) is within normal range, but increases abnormally steeply on exertion [1, 2].
Current guidelines recommend the use of a multi-parametric algorithm (ASE/EACVI algorithm) for LAP estimation [3]. However, despite significant improvements in feasibility [4], as compared to previous recommendations, validating studies have demonstrated that the proposed approach entails only moderate diagnostic value for resting LAP [5, 6], which is further restricted for identifying patients with excessive LAP elevation on exertion despite normal resting pressures [2]. Finally, although ventricular pacing is frequent in HF patients, there is ambiguity regarding the proper use of the currently recommended method in this cohort.
LA function has gained recognition as an important focus area in the assessment of LV diastolic function [7–9]. LA reservoir function is influenced both by the LV performance and by the intrinsic LA compliance and plays an important role in disease progression in various clinical states including HF [10–13]. Quantitative LA deformation analysis using speckle tracking has evolved as a highly feasible and reproducible method for evaluating LA function. It has been proven that LA global strain (LA-GS) is associated with mechanical changes and fibrosis even prior to LA geometrical remodeling [8, 14, 15], potentially enabling earlier diagnosis of elevated LAP. Previous studies have shown an inverse relationship between LA-GS and the diastolic pressures [5, 16]. Accordingly, we hypothesized that LA-GS might contribute to improve the non-invasive assessments of elevated LAP, and set out to assess its diagnostic value in that setting. Furthermore, we opted to investigate the applicability of LA-GS in patients on ventricular pacing.
Methods
Study population
All consecutive patients referred right heart catheterization (RHC) at the Karolinska University Hospital for the HF assessment between February 2014 and June 2017 (n = 220) were screened for enrollment. In all cases medical treatment had been titrated and hemodynamic stabilization achieved at the time of examination. No patient presented with acute coronary syndrome or had undergone cardiac surgery for a period of < 1 year prior enrollment. The study conformed to the Declaration of Helsinki, had ethics approval by local ethics committees and all participants provided written informed consent.
Echocardiography
All subjects underwent transthoracic echocardiography using an E9 system (GE Ultrasound, Horten, Norway) equipped with a 2.5 MHz matrix array transducer in keeping with current guidelines. 2D gray-scale images were acquired over 3 heart cycles and analyzed off-line (EchoPAC PC, version 11.0.0.0 GE Ultrasound, Waukesha, Wisconsin) by a single sonographer blinded to clinical and RHC data. LV end-diastolic, end-systolic volume and ejection fraction (EF) were measured using the Simpsons biplane method [17]. For LA volumetric analysis, the ‘method of disk’ method was employed. Myocardial deformation was analyzed by 2-D speckle tracking. LV global longitudinal strain (LV-GLS) was calculated as the average value of 12 segments obtained from the apical 4- and 2-chamber views. LA global strain (LA-GS) was assessed using images obtained in apical 4- and 2-chamber views (frame rate: 60–80 Hz), with attention for optimal visualization of the LA. Acoustic tracking was performed by semi-automated analysis. The endocardial border of the LA was traced manually so that the LA appendage and pulmonary veins were excluded, then an additional epicardial line was automatically generated by the software creating a region of interest (ROI), the shape of which was manually adjusted to precisely draw out the atrial contour and cover the full thickness of atrial myocardium (Fig. 1). Automatic processing was controlled by 1, visual confirmation of correct tracking of the endocardial border throughout the cardiac cycle and 2, by automated self-check function of the software. In case the tracking did not seem appropriate according to the reader or a segment was not approved by the software, repeated manual adjustment of the ROI was performed. If repeated processing did not result in an approved strain curve, the loop was excluded from the analysis (n = 4 cases). Following approval, the software automatically divided the LA endocardium into six segments, and longitudinal strain curves for each segment were generated. Zero point was set at the onset of the QRS complex on the ECG. LA reservoir function was estimated by peak LA longitudinal strain during ventricular systole. LA-GS was calculated by averaging strain measurements from all the segments. In patients in sinus rhythm, measurements from 3, in patients in AF (n = 42) measurements from 5 consecutive beats were averaged. Loops were carefully recorded so that PVCs/PACs were avoided. Reproducibility was tested in 40 randomly selected patients. The early (E) and late (A) mitral flow velocities were recorded using a 5 mm pulsed wave (PW) sample volume. Tricuspid regurgitation peak velocity (TRVmax) was recorded employing continuous wave Doppler. Spectral tissue velocities were recorded in the septal and lateral mitral annulus using a 5 mm PW sample volume and the early myocardial relaxation velocity (e′) was recorded. The E/e′ ratio was calculated from the average of septal and lateral myocardial velocities. At the time of examination 42 patients were in AF.
Fig. 1.
Left atrial strain curves obtained from four- and two-chamber views. The white dotted line indicates the mean strain value over the heart cycle in each view. LA reservoir function was estimated by peak LA longitudinal strain during ventricular systole. Global left atrial strain (LA-GS) was calculated by averaging the peak LA strain values from all 12 segments
Catheterization
Within 1 h following echocardiography, RHC was performed using a 6F Swan-Ganz catheter through the jugular or femoral vein. Mean right atrial pressure, the systolic-, diastolic-, mean pulmonary artery pressure (PAPM) and the mean pulmonary artery wedge pressure (PAWPM) were recorded under fluoroscopy after calibration with the zero-level set at the mid-thoracic line. Pressure tracings were stored (WITT Series III, Witt Biomedical Corp., Melbourne, FL) and analysed offline. PAWPM measurements were averaged from a minimum of 5 heart cycles at spontaneous end-expiration.
Exercise protocol
Following the assessment of resting hemodynamics, patients with normal PAWPM at rest (≤ 15 mmHg) performed supine cycle ergometry. Patients cycled at 60 rpm starting at a 20 W workload and increasing by 10 W increments in 1-min stages to maximum tolerated levels. PAWPM was determined at peak exercise. Prior studies in normal controls have shown that peak PAWPM during supine exercise are < 20–23 mmHg [18, 19]. In our study, PAWPM ≥ 23 mmHg during peak exercise denoted abnormal LAP response.
Biomarkers
NT-proBNP was analyzed by proBNPII (Roche Diagnostics, Bromma, Sweden). Estimated glomerular filtration rate (eGFR) was calculated according to the MDRD study equation: eGFR = 175 × [creatinine] − 1.154 × 106−0.203 × 0.742 [if female] mL/min/1.73; Creatinine in mg/dL, age in years.
Statistical analysis
The IBM SPSS statistics version 23.0 was used. QQ plots tested normality. Continuous variables are expressed as median and interquartile range. Categorical variables were expressed as absolute values and percentage. For comparisons of different groups, the Mann–Whitney test was used. Correlations were tested by the Pearson’s 2-tailed test or Spearman test, as appropriate. All tests were performed at 95% confidence intervals. A p value of < 0.05 was considered statistically significant.
The association of invasive and non-invasive diastolic indices with the combined outcome of death or heart-transplantation (HTX) was tested using a time to event analysis with univariate and multivariable Cox proportional hazards models, adjusting for demographic, clinical and echocardiographic covariates (E/e′, TRVmax, age, hypertension, diabetes, LV-EF, ln[NT-proBNP] and eGFR) and a Kaplan–Meier non-parametric test and compared employing a log-rank test. The proportional hazards assumption was tested for all analyses. Receiver-operating characteristic (ROC) curves were plotted for individual parameters regarding the discrimination of increased PAWPM and to establish the optimal cut-off points.
NT-proBNP data were natural logarithmically transformed. Analysis of intra-observer variability was performed for LA-GS by double measurements in 40 randomly selected patients. Inter-observer variability together with test–retest reliability was tested in 29 individuals, who have undergone two consecutive examinations each, within 20 min, performed by two different examiners and then the two recordings analysed again by two different readers.
Results
Patient characteristics
Demographic data are provided in Table 1. In total 220 patients referred for diagnostic right heart catheterization (RHC) with suspected HF or unexplained dyspnea were prospectively screened. Of the 220 patients catheterized, 11 patients who previously underwent cardiac transplantation with atrial anastomosis technique were excluded. By the results of catheterization, 29 patients turned out to have an underlying disease other than primary left heart myocardial disease (isolated pre-capillary arterial pulmonary hypertension, n = 15; constrictive pericarditis, n = 14), and therefore, were excluded from further analysis. In addition, 3 patients with ARVD, 10 patients with significant valvular disease and 3 patients with inadequate echocardiographic image quality were also excluded from further analysis (Figure S1).
Table 1.
Demographic data stratified according to EF groups
| General characteristics | EF ≥ 50% | EF < 50% | p value |
|---|---|---|---|
| (n = 92) | (n = 72) | ||
| Age years | 73 (67; 79) | 58 (47; 64) | < 0.001 |
| Female | 57 (62%) | 15 (21%) | < 0.001 |
| Medical history and symptoms | |||
| AF | 44 (48%) | 33 (46%) | 0.799 |
| PM/CRT | 8/0 (9%) | 8/16 (33%) | |
| Hypertension | 63 (69%) | 42 (58%) | 0.30 |
| Diabetes mellitus | 17 (19%) | 13 (18%) | 0.84 |
| Hypercholesterolaemia | 22 (24%) | 23 (32%) | 0.197 |
| Ischaemic heart disease | 3 (3%) | 19 (26%) | < 0.001 |
| NYHA I | 12 (13%) | 1 (1%) | |
| NYHA II | 18 (20%) | 9 (13%) | |
| NYHA III | 59 (64%) | 56 (78%) | |
| NYHA IV | 3 (3%) | 6 (8%) | |
| Clinical measurements | |||
| BMI kg/m2 | 27 (23; 30) | 27 (24; 31) | 0.63 |
| Obesity (BMI ≥ 30) | 25 (27%) | 19 (26%) | 0.911 |
| SBP (mm Hg) | 130 (117; 142) | 101 (93; 115) | < 0.001 |
| DBP (mm Hg) | 67 (60; 71) | 62 (55; 70) | 0.04 |
| HR (beats/min) | 70 (60; 80) | 68 (59; 77) | 0.51 |
| Treatment | |||
| ARB or ACE-I | 50 (54) | 64 (89) | < 0.001 |
| Loop diuretic | 63 (69) | 65 (90) | 0.001 |
| Beta blocker | 61 (66) | 68 (94) | < 0.001 |
| MRA | 30 (33%) | 53 (74%) | < 0.001 |
| Calcium channel blocker | 26 (28) | 5 (7) | = 0.001 |
| Laboratory findings | |||
| NT-proBNP (ng/L) | 1250 (365; 2300) | 2580 (1265; 2693) | < 0.001 |
| eGFR (mL/min/1.73 m2) | 65 (46; 88) | 81 (68; 102) | < 0.001 |
| Hemoglobin (mg/L) | 123 (113; 140) | 138 (125; 148) | < 0.001 |
Categorical variables are provided as absolute numbers followed by percentages in brackets; continuous variables or median values followed by 1st and 3rd quartiles in brackets
EF ejection fraction, AF atrial fibrillation or flutter, PM pacemaker, CRT cardiac resynchonization therapy, NYHA New York Heart Association functional class, BMI body mass index, SBP systolic blood pressure, DBP diastolic blood pressure, HR heart rate, ARB angiotensin receptor blocker, ACE-I ACE-inhibitor, MRA mineralocorticoid receptor antagonist, NT-proBNP N-terminal pro-brain natriuretic peptide, eGFR estimated glomerular filtration rate
In effect, recordings of 164 patients were analyzed (age 63 ± 15; 74 female). Median EF was 54% (Q1:25%, Q3:62%), 72 patients (44%) had EF < 50% (HFrEF). At the time of enrollment all patients were symptomatic. Ischemic cardiomyopathy was the cause of HF in 26 cases, idiopathic dilated cardiomyopathy in 53, restrictive cardiomyopathy of various origin in 23 (amyloidosis: 5, sarcoidosis: 1, hypertrophic: 5, other: 12), and viral myocarditis in 1 case, with the rest being of multifactorial origin.
At rest, 97 patients (59%) demonstrated elevated PAWPM (> 15 mmHg). Additionally, 32 patients with normal resting PAWPM displayed abnormal LAP (≥ 23 mmHg) during exercise [preserved EF (pEF), n = 17 (19%); HFrEF, n = 15 (21%)]. In total 129 (79%) patients had elevated LAP either at rest or during exertion. In 8 cases, the exercise testing was not feasible due lower extremity pain (n = 3) or inability to follow instructions (n = 5). Echocardiographic and invasive measurements for pEF and HFrEF are summarized in Table 2.
Table 2.
Cardiac geometric and functional measures in the two groups stratified according to EF
| EF ≥ 50% (n = 92) | EF < 50% (n = 72) | p value | |
|---|---|---|---|
| LV dimensions | |||
| LV EDVi (mL/m2) | 47 (39; 61) (88) | 99 (78; 132) (62) | < 0.001 |
| LV ESVi (mL/m2) | 16 (12; 24) (88) | 75 (46;101) (62) | < 0.001 |
| LVMi (g/m2) | 88 (69; 111) (88) | 139 (103; 164) (71) | < 0.001 |
| LV systolic function | |||
| LV-EF (%) | 60 (57; 65) (92) | 25 (20; 40) (72) | < 0.001 |
| LV-GLS (%) | 18 (14; 20) (91) | 6.8 (4.9; 10) (71) | < 0.001 |
| LV diastolic function | |||
| E/A ratio | 1.3 (0.9; 2.1) (60) | 2.9 (1.7; 3.9) (57) | < 0.001 |
| e′ septal | 6.9 (5.0; 8.0) (92) | 4.5 (3.3; 60) (72) | < 0.001 |
| e′ lateral | 8.1 (6.6; 10.9) (92) | 7.5 (6.0; 10.0) (72) | NS |
| E/e′ | 12.5 (9.5; 18.4) (91) | 15.3 (11.5; 23.7) (72) | 0.015 |
| LA function | |||
| LA ESVi (mL/m2) | 42 (34; 53) (92) | 60 (44; 69) (72) | < 0.001 |
| LA-GS (%) | 12.0 (7.0; 17.9) (90) | 7.9 (5.0; 10.1) (70) | < 0.001 |
| RV parameters | |||
| TAPSE (mm) | 17 (13; 22) (92) | 14 (11; 17) (71) | 0.002 |
| RVSP (mmHg) | 44 (37; 58) (90) | 46 (36; 57) (66) | NS |
| Hemodynamic | |||
| PAWPM (mmHg) | 16 (13; 22) (91) | 19 (14; 25) (72) | 0.023 |
| PAPM (mmHg) | 26 (21; 37) (92) | 29 (22; 37) (72) | NS |
| Cardiac Index (mL/m2) | 2.5 (2.0; 2.9) (92) | 2.0 (1.6; 2.3) (72) | < 0.001 |
Data are provided as median values followed by 1st and 3rd quartiles in brackets. Patient numbers for each measurement are provided in brackets
BMI body mass index, HR heart rate, SBP systolic blood pressure, DBP diastolic blood pressure, LV left ventricle, EDVi end-diastolic volume index, ESVi end-systolic volume index, LVMi LV mass index, EF ejection fraction, LV-GLS LV global longitudinal strain, E/A ratio between the early diastolic inflow velocity (E) to the inflow velocity due to atrial contraction (A), e′ mean, mean value of early myocardial velocity in LV basal septal and lateral wall, E/e′ ratio between the E and the e′, LA left atrium, LA ESVi left atrial end-systolic volume, LA-GS left atrial global longitudinal strain, TAPSE tricuspid annular plane systolic excursion, RVSP right ventricular systolic pressure as assessed by echocardiography, PAWPM pulmonary arterial wedge pressure, PAPM pulmonary arterial mean pressure, NS non-significant (p ≥ 0.05)
At the time of examination, 42 (26%) patients were in atrial fibrillation (AF) and 32 patients (19%) had continuous ventricular pacing (VP) (CRT in 16 cases).
Echocardiographic metrics and PAWP
In the whole cohort, PAWPM showed a significant inverse correlation with LA-GS (r = − 0.54, p < 0.001) and weaker albeit significant relationship with TRVmax, LAVi and E/e′ (r = 0.41, 0.29, 0.28, respectively; p < 0.001 for all). The ASE/EACVI algorithm for diastolic assessment does not apply to patients in AF or those with ventricular pacing. Nonetheless, as LA-GS has not yet been thoroughly investigated in this setting, we decided to study its validity in these specific subgroups. Conceivably, AF might importantly influence LA-GS measurements. Accordingly, separate analysis of the AF group confirmed that neither LA-GS (r = − 0.26, p = 0.092), nor LAVi (r = − 0.116, p = 0.46) or E/e′ (r = 0.21, p = 0.19) were associated with PAWPM. In contrast, in the VP group, PAWPM significantly correlated with LA-GS (r = − 0.54, p = 0.002) and E/e′ (r = 0.41 p = 0.021), but lacked association with either LAVi or TRVmax (r = − 0.14 and 0.2, p > 0.05 in both cases).
Confining the analysis to patients in sinus rhythm (SR) (i.e., where the currently recommended algorithm is applicable), the correlations between PAWPM and LA-GS, LAVi and TRVmax were stronger (r = − 0.66, 0.51 and 0.46 respectively, p < 0.001 for all). However, the E/e′ remained only weakly associated with PAWPM (r = 0.25, p < 0.018). Accordingly, we decided to proceed with all further analysis in the cohort in regular rhythm (RR), i.e., both those in SR and VP and to exclude patients with AF.
In a multivariable analysis including LA-GS, LAVi, TRVmax, E/e′ and LV-GLS, the LA-GS was identified as the strongest predictor of PAWPM with a partial correlation of r = − 0.42 (p < 0.001) in RR patients. The correlation for TRVmax was r = 0.33 (p < 0.001), while the other variables were not associated with PAWPM (p > 0.05). Similarly, in the SR cohort, LA-GS and TRVmax were identified as the only predictors of PAWPM (partial correlations r = − 0.40 and r = 0.33 respectively, p < 0.001), whereas the other variables were not associated with PAWPM (p > 0.05). No correlation between LV-GLS and PAWPM was found in either EF group (p > 0.05).
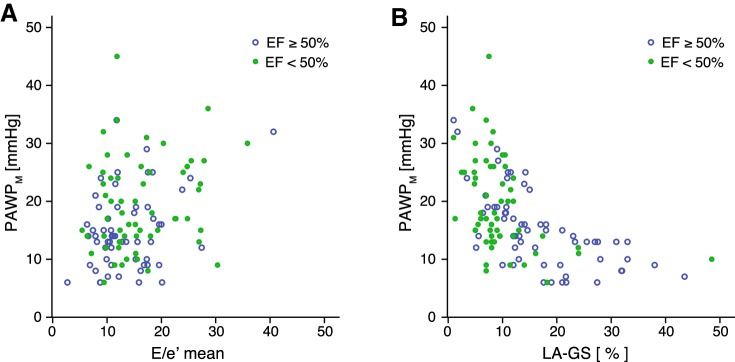
As shown in Table 3a, when dividing our RR cohort based on the EF, compared to the other non-invasive metrics, LA-GS displayed the strongest correlation with PAWPM in both EF groups (r = − 0.61 and − 0.46 in pEF and HFrEF, respectively, p < 0.001 for both) (Fig. 2). Notably, the correlation between LA-GS and PAWPM was strongest in the preserved EF group; further stratification of our cohort into moderately and severely reduced EF confirmed a progressively weaker LA-GS–PAWPM correlation along with lower EF ranges (EF 30–49%: r = − 0.54 p = 0.014; EF < 30%, r = − 0.36 p = 0.03). Echocardiographic and haemodynamic characteristics of these subgroups are provided in Table S1. LAVi and TRVmax were also significantly related to PAWPM (p < 0.05), whereas the correlation of E/e′ with PAWPM was confined to pEF patients (r = 0.32, p = 0.002).
Table 3.
Sensitivity, specificity and area under curve values of various echocardiographic estimates for identifying elevated LAP in patients with preserved or reduced EF (A); at rest and during stress, independent of the EF (B)
| A | EF ≥ 50% | EF < 50% | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| r | p | SP | SN | AUC | p | r | p | SP | SN | AUC | p | ||
| Regular rhythm | (n = 63) | (n = 59) | |||||||||||
| Rest | E/e′ | 0.33 | 0.012 | 67 | 62 | 0.68 | 0.016 | 0.17 | 0.20 | 0.59 | 0.26 | ||
| LAVi | 0.39 | 0.002 | 53 | 96 | 0.79 | < 0.001 | 0.29 | 0.025 | 21 | 97 | 0.66 | 0.041 | |
| TRVmax | 0.55 | < 0.001 | 56 | 71 | 0.68 | 0.019 | 0.37 | 0.006 | 58 | 82 | 0.70 | 0.018 | |
| LA-GS | − 0.64 | < 0.001 | 77 | 93 | 0.87 | < 0.001 | − 0.46 | < 0.001 | 61 | 68 | 0.74 | 0.002 | |
| ASE/EACVI | 44 | 93 | 0.69 | 0.013 | – | – | 0.62 | 0.14 | |||||
| Rest-Cath | 100 | 70 | 0.85 | < 0.001 | 100 | 70 | 0.85 | 0.002 | |||||
| Stress | E/e′ | – | – | 0.56 | 0.46 | – | – | 0.57 | 0.53 | ||||
| LAVi | – | – | 69 | 85 | 0.77 | 0.002 | – | – | – | – | 0.67 | 0.131 | |
| TRVmax | – | – | 0.66 | 0.076 | – | – | 0.71 | 0.121 | |||||
| LA-GS | – | – | 88 | 92 | 0.93 | < 0.001 | – | – | 77 | 96 | 0.85 | 0.003 | |
| AS/EACVI | 56 | 88 | 0.72 | 0.011 | 0.58 | 0.448 | |||||||
| Sinus rhythm | (n = 55) | (n = 35) | |||||||||||
| Rest | E/e′ | 0.35 | 0.014 | 65 | 61 | 0.66 | 0.042 | 0.10 | 0.551 | 0.60 | 0.340 | ||
| LAVi | 0.43 | 0.001 | 61 | 96 | 0.81 | < 0.001 | 0.48 | 0.004 | 31 | 96 | 0.74 | 0.022 | |
| TRVmax | 0.55 | < 0.001 | 21 | 74 | 0.70 | 0.015 | 0.38 | 0.042 | 0.69 | 0.120 | |||
| LA-GS | − 0.66 | < 0.001 | 78 | 86 | 0.90 | < 0.001 | − 0.55 | 0.001 | 59 | 86 | 0.78 | 0.008 | |
| ASE/EACVI | 48 | 91 | 0.70 | 0.013 | 33 | 96 | 0.64 | 0.042 | |||||
| Rest-Cath | 100 | 72 | 0.86 | < 0.001 | 100 | 73 | 0.87 | 0.019 | |||||
| Stress | E/e′ | 0.58 | 0.38 | 0.59 | 0.58 | ||||||||
| LAVi | 69 | 91 | 0.75 | 0.005 | – | – | 0.72 | 0.165 | |||||
| TRVmax | 0.57 | 0.439 | 0.58 | 0.699 | |||||||||
| LA-GS | 88 | 90 | 0.92 | < 0.001 | 100 | 97 | 0.98 | 0.003 | |||||
| ASE/EACVI | 56 | 84 | 0.70 | 0.023 | – | 0.57 | 0.64 | ||||||
| B | Rest | Stress | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| r | p | SP | SN | AUC | p | SP | SN | AUC | p | ||
| Regular rhythm ( n = 122) | |||||||||||
| Rest-Cath | 100 | 70 | 0.85 | < 0.001 | |||||||
| E/e′ | 0.28 | 0.002 | 63 | 57 | 0.65 | 0.005 | 0.57 | 0.307 | |||
| LAVi | 0.40 | < 0.001 | 40 | 97 | 0.75 | < 0.001 | 58 | 91 | 0.75 | < 0.001 | |
| TRVmax | 0.40 | < 0.001 | 61a | 65a | 0.65 | 0.002 | – | – | 0.55 | 0.400 | |
| LA-GS | − 0.61 | < 0.001 | 70 | 80 | 0.80 | < 0.001 | 83 | 89 | 0.90 | < 0.001 | |
| ASE/EACVI | 31 | 94 | 0.66 | 0.003 | 46 | 90 | 0.68 | 0.007 | |||
| Sinus rhythm ( n = 90) | |||||||||||
| Rest-Cath | 100 | 73 | 0.86 | < 0.001 | |||||||
| E/e′ | 0.25 | 0.018 | 66 | 53 | 0.64 | 0.023 | 0.57 | 0.377 | |||
| LAVi | 0.51 | < 0.001 | 52 | 96 | 0.80 | < 0.001 | 65 | 87 | 0.76 | < 0.001 | |
| TRVmax | 0.46 | < 0.001 | 24 | 75 | 0.69 | 0.004 | – | – | 0.50 | 0.95 | |
| LA-GS | − 0.63 | < 0.001 | 64 | 96 | 0.86 | < 0.001 | 84 | 93 | 0.94 | < 0.001 | |
| ASE/EACVI | 38 | 93 | 0.69 | 0.002 | 50 | 89 | 0.68 | 0.014 | |||
Data are provided separately for patients in regular rhythm (patients with atrial fibrillation excluded) and those in sinus rhythm (patients with atrial fibrillation and/or pacemaker rhythm excluded). Patient numbers for each cohort are provided in brackets
r correlation coefficient, AUC area under curve provided by ROC analysis, SP specificity, SN sensitivity, LAVi left atrial volume index, TR-Vmax maximal velocity of the tricuspid regurgitant jet, LA-GS left atrial global strain, followed by the applied cut-off values for pEF and rEF, respectively in brackets, ASE/EACVI the algorithm recommended by the current guidelines, rest-cath resting PAWPM value obtained by invasive measurement, EF ejection fraction
aUsing a cut off value of 2.9 m/s
Fig. 2.
Correlation of invasively measured PAWPM values with left atrial global strain (LA-GS) (a) and E/e′ (b) in patients with regular rhythm with preserved (HFpEF) or reduced (HFrEF) ejection fraction
Correlation between non-invasive markers and NT-proBNP
In patients with RR, NT-proBNP was strongly associated with LA-GS (r = − 0.64, p < 0.001) with significant but weaker correlation with PAWPM, LAVi (r = 0.40 and 0.52, respectively; p < 0.001 for both) and E/e′ (r = 0.25; p = 0.012) but not with TRVmax (p > 0.05). In a multivariable analysis including LA-GS, LAVi, TRVmax, E/e′ and LV-GLS, the LA-GS remained the sole predictor of NT-proBNP with a partial correlation of r = − 0.43 (p < 0.001).
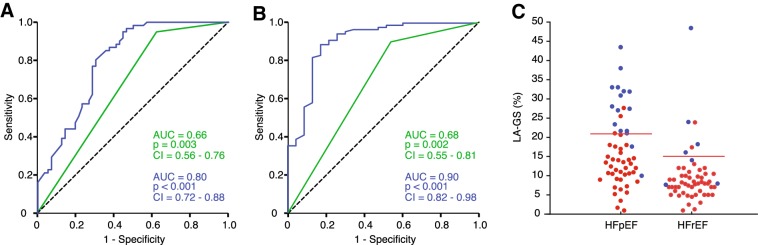
Echocardiographic metrics for elevated LAP at rest and during exercise
As illustrated in Table 3, LAVi and the ASE/EACVI algorithm provided fairly good ability to rule out elevated resting PAWPM. However, their specificity was limited and for the ASE/EACVI algorithm restricted to pEF patients. In contrast, LA-GS yielded a more robust discrimination for resting PAWPM, particularly in the pEF group (LA-GS cut-off: 15%, specificity and sensitivity 83% and 89%, respectively; p < 0.0001). HFrEF patients displayed generally lower LA-GS values, therefore, at an optimal cut-off value of 8% in this cohort, a specificity of 61% and sensitivity of 68% was achieved (p = 0.002) (Fig. 3A).
Fig. 3.
Diagnostic accuracy of LA-GS. ROC curve of LA-GS (blue) and the ASE/EACVI algorithm (green) for identifying elevated PAWPM at rest (a) and at rest and/or during stress (b), independent of the EF. Beeswarm plot showing subjects with normal (blue) or pathological (red) PAWPM values at rest and/or during exercise, dichotomized according to the EF (c). Optimal LA-GS cut-off values for preserved and reduced EF are 21% and 17%, respectively. LA-GS, left atrial global strain; ROC, receiver operating characteristics; PAWPM, mean pulmonary arterial wedge pressure; EF, ejection fraction
Even more diagnostically challenging are those patients displaying resting LAP within the normal range, but an abnormal pressure elevation on exertion. Importantly, we found that taking into account all patients with elevated LAP either at rest or during exercise, the predictive value LA-GS improved further. In patients with pEF, resting LA-GS (cut-off: 21%) displayed a specificity and sensitivity of 88% and 92%, while in HFrEF (cut-off 15%) the corresponding values for identifying pathological LAP at rest or during stress were 67% and 92%, respectively (Fig. 3c). Noticeably, invasive PAWPM measurements at rest had lower sensitivity compared to LA-GS in this diagnostic setting. Finally, the ASE/EACVI algorithm demonstrated limited specificity in pEF patients (specificity: 56%, sensitivity: 88%, AUC = 0.72; p = 0.011) and in fact no significant diagnostic information in the HFrEF group (Fig. 3b).
Recently, a multivariable approach based on echocardiographic (Doppler derived pulmonary artery systolic pressure, E/e′) and clinical (age, BMI, hypertension, atrial fibrillation) parameters for HFpEF diagnosis as assessed by invasive rest and exercise testing [20]. A weighted score based on the above 6 parameters (H2FPEF) provided robust discernment of HFpEF (AUC 0.84). In our cohort, the mean H2FPEF was 5 (3% of the patients had score 0; 5% score 1; 3% score 2; 15% score 3; 16% score 4; 8% score 5; 14% score 6; 23% score 7; 3% score 8 and 9% had score 9). ROC analysis of the predictive ability of the score in the subgroup of patients with EF > 50% was 0.81 (0.71–0.91); p < 0.001. H2FPEF score and the LA-GS demonstrated a significant inverse relationship (r = − 0.51, p < 0.001). The corresponding association between the H2FPEF score and the PAWP at rest was r = 0.44, p < 0.001, whereas there was no significant association with E/e′ (r = 0.12; p > 0.05).
Indices of diastolic function and outcome
The prognostic information provided by non-invasive and invasive metrics of LAP was subsequently evaluated. Using Kaplan–Meier analysis the predictive value of LA-GS (cut-off: < 12%), PAWPM (cut-off: > 15 mmHg) and E/e′ (cut-off: > 14) was investigated (Fig. 4). Over a median follow-up of 561 days (IQR: 270–839) 32 primary outcome events occurred [20 deaths, 12 HTX]. No patients were lost to follow-up. PAWPM > 15 mmHg was related with higher risk for death or HTX [hazard ratio (HR) 2.3; confidence interval (CI) 1.1–4.9, p = 0.022]. Furthermore, LA-GS < 12% was associated with an increased risk for the primary composite endpoint in unadjusted analysis [HR: 2.4, CI 1.1–5.2, p = 0.029] and was the sole independent predictor of outcome when adjusted for E/e′ and TRVmax, using the cut-off values recommended in the ASE/EACVI algorithm [HR: 2.8; CI 1.1–6.1, p = 0.017]. However, when adjusted for age, eGFR, hypertension, diabetes mellitus, LV EF and ln[NT-proBNP], neither the LA-GS nor the PAWPM retained their predictive potential, NT-proBNP remaining the sole significant prognostic index (HR 1.53; p = 0.022) (Table S2).
Fig. 4.
Prognostic value of LA-GS. Kaplan–Meier analysis of the predictive value of E/e′ (a), LA-GS (b) and invasively measured PAWPM (c) on the composite outcome of death and/or HTX. LA-GS, left atrial global strain; PAWPM, mean pulmonary arterial wedge pressure; HTX, heart transplantation
Feasibility and reproducibility
Measurements of LAVi and E/e′ could be performed in all cases whereas the feasibility of LA-GS and TRVmax were 98% and 95%, respectively. In the present study the ASE/EACVI algorithm provided a definite diagnosis in 99% of the cases, with only 1 case remaining indeterminate.
Double measurements for LA-GS in 40 randomly selected patients demonstrated a coefficient of variation of 10% with intra-class correlation coefficient 0.91 (95% CI 0.73–0.96).
Test retest analysis for the LA-GS yielded high reliability with a slightly higher coefficient of variation of 12.8%.
Discussion
In this prospective study we demonstrate that in patients with known or suspected HF, LA-GS provides a feasible and robust diagnostic tool for the identification of elevated LAP either at rest or on exertion, with this single measurement entailing higher diagnostic accuracy as compared to the currently recommended diagnostic algorithm. Furthermore, we show that among the tested non-invasive indices of filling pressures, LA-GS provides the best prognostic value in HF patients.
Recommended algorithm for the assessment of diastolic dysfunction
Given the limited individual accuracy of the established non-invasive metrics, the evaluation of LV filling pressures requires a number of parameters to be taken into account [21], rendering diastolic assessment a laborious task. In 2016 the American Association of Echocardiography (ASE) together with the European Association of Cardiovascular Imaging (EACVI) published a new joint guideline proposing a novel algorithm, based on expert consensus [3], that comprises a simplified thus potentially more feasible approach for echocardiographic LAP estimation. A number of studies have since tested the diagnostic validity of this new algorithm and concluded that it provides an improved yet still moderate sensitivity for elevated LAP [4–6, 21] along with fewer indeterminate cases compared to the previous recommendations [4]. Our findings essentially corroborate these observations as we show that despite good feasibility, the diagnostic potential of the ASE/EACVI algorithm remains modest. More specifically, as compared to previous findings [2, 6] we show that the ASE/EACVI algorithm provided better ability for ruling out elevated LAP, compromised, however, by a poorer specificity, probably due to the higher prevalence of severe HF in our cohort.
LA-strain for the assessment of resting LAP
Normally, the distensible LA accommodates the inflowing volume from the pulmonary veins with only a slight rise in the LAP. However, in HF structural and pro-inflammatory alterations often result in increased LA-wall stiffness, shifting the LA pressure–volume curve upwards with accentuated pressure elevation for the same volume entering the LA [22]. It appears, therefore, pathophysiologically sound to postulate that characterization of LA-wall mechanics might contribute to the diagnostics of diastolic function. Indeed, LA wall deformation as quantified by LA-GS has been shown to correlate well with LV filling pressures in systolic HF [5, 7, 14, 23]. Moreover, Hummel et al. demonstrated that in HFpEF, as compared to established non-invasive metrics, LA-GS exhibited a stronger relationship with PAWPM [5]. In line with these observations we show that in both HFpEF and HFrEF patients, the predictive potential of LA-GS for elevated resting LAP was superior not only to individual established non-invasive markers, but to the ASE/EACVI algorithm as well. Particularly in pEF patients, the fairly high specificity of LA-GS was accompanied by a comparable ability for ruling out elevated resting LAP.
Diagnosis of patients with pathologically elevated resting or exercise-induced LAP
Notwithstanding the evident challenge in regard to non-invasive estimation of resting LAP, the diagnosis of patients presenting with exertional dyspnea comprises an even more perplexing undertaking. This becomes apparent in light of the findings of a recent study in which roughly 40% of HFpEF patients exhibited normal resting LAP, but displayed abnormal pressure elevation during exercise [5]. In our investigation, 20% of the invasively diagnosed HFpEF and HFrEF patients had normal resting, but elevated exercise LAP. Overall, the sensitivity of resting invasive hemodynamics for identifying abnormal diastolic response during exertion was higher yet still moderate (70%) as compared to the aforementioned study [2], a discrepancy that might be ascribed to the higher prevalence of more severe HF in our cohort as indicated by the higher NT-proBNP and LAVi values. Although the ASE/EACVI algorithm was not specifically developed for this purpose, given this being the currently recommended method for the diagnosis of diastolic dysfunction it is plausible to assume that patients with exercise induced pressure elevation and symptoms might score abnormal by this method. Obokata and colleagues were the first to validate the ASE/EACVI algorithm against the gold standard invasive exercise testing, demonstrating a fairly good specificity (80%) limited, however, by poor sensitivity (34%) in HFpEF [2]. Employing similar methodology our results show better sensitivity values and poorer specificity most possibly due to the more advanced HF in our study. Importantly, the ASE/EACVI approach applies to both patients with HFpEF and HFrEF [3]. However, according to the current results, in HFrEF the multi-parametric approach at rest was not predictive for abnormal LAP elevation during exercise.
In contrast, LA-GS had even further increased discriminatory capacity for pathological LAP when both resting- or exercise-induced values were taken into account. In fact, particularly in patients with pEF, resting LA-GS provided superior sensitivity than resting PAWPM implying that LA-GS might be more sensitive in ruling out elevated PAWPM during physical exertion than invasive examination in resting condition. LA-GS has been shown to inversely associate with the degree of LA-wall fibrosis as assessed by delayed-enhancement magnetic resonance imaging [24]. Furthermore, in patients undergoing mitral valve surgery, LA-GS comprised the strongest independent predictor of histologically quantified LA-wall fibrosis [14]. Conceivably, LA-GS might reflect the state of LA compliance, thus allowing identification of elevated LAP at rest but even more predicting abnormal LAP response at states of increased flow conditions such as during exercise.
The physiologic concept of LA-LV volume reciprocity describes the inherent association between the LV and LA function whereby the LV systolic deformation impacts on LA mechanics [7, 22]. Indeed, the current results substantiate this notion showing statistically significant association between LV-GLS and LA-GS (pEF: r = 0.36, p = 0.005; HFrEF: r = 0.38, p < 0.003). Nevertheless, as opposed to LA-GS, no correlation between LV-GLS and PAWPM was found in either HF group (p > 0.05). More importantly, multivariate analysis demonstrated that LA-GS entailed an independent predictive value for LAP, whereas LV-GLS lacked diagnostic potential in that setting. This is not surprising as LA-GS quantifies mechanical events at the LA level associated with PAWPM, as opposed to LV-GLS, which might better reflect LVEDP. Additionally, previous experimental studies have demonstrated differential cellular responses with more pronounced pro-fibrotic changes detected in the LA as compared to the LV wall [25, 26] which advocates for LA-GS entailing a diagnostic value that is independent of the LV-GLS [15].
As the current results reveal, the specificity of LA-GS for resting and/or exercise LAP elevation was higher in patients with pEF which might be ascribed to the disparate degree of LA remodeling with smaller LAVi in pEF (pEF: 42 ± 15 vs. HFrEF: 55 ± 17 mL/m2, p < 0.001). Indeed, the association between LA-GS and PAWPM was lower in patients with severely dilated LA (LAVi > 48 mL/m2) compared to those with mild to moderate LA enlargement (r = 0.69 vs. 0.30, p < 0.001). Although LA-GS is angle independent, extensive geometrical changes in LA might impact on the myocardial tracking. Additionally, the attenuation of wall stress secondary to LA dilatation might affect the reliability of LA-GS in predicting LAP [27].
Outcome
Filling pressures not solely impact on symptoms, but on prognosis as well as previously shown [1]. Employing the currently recommended PAWPM value (> 15 mmHg) demonstrated an increased event rate (death or HTX) in the elevated LAP group. However, when the non-invasive metrics of LAP were tested at the suggested discriminating values, only LA-GS comprised a prognostic value. Following adjustment for demographic and clinical parameters, neither the PAWPM nor LA-GS remained diagnostic. The current findings might reflect inadequate power, but advocate as well for the complexity of the HF as a clinical entity.
Clinical utility
In our study, LA-GS alone provided higher diagnostic accuracy for resting or exercise-induced pathological LAP elevation in HF patients, as compared to the multi-parametric ASE/EACVI algorithm. Thus, routine LA-GS measurements might provide a simple and robust tool in the setting of HF diagnostics and prognostication. Nevertheless, despite LA-GS constituting the best single non-invasive metric, its correlation with invasively measured pressures was still only moderate. Especially in case of reduced LA-GS, there was a considerable overlap between patients with normal and elevated LAP values. This ultimately advocates for the preferential use of various metrics instead of single measurements in the setting of LAP estimation. In addition, future studies are warranted for evaluating the possible incremental values of LA-GS measurements in context of novel HF device therapies, such as the inter-atrial shunt device implantation [28–30].
Limitations
This is a single center study performed on a limited number of patients, still to the best of our knowledge it is the largest of its kind with echocardiographic and parallel resting and stress invasive measurements reported. Referral for RHC constitutes an important selection bias;, therefore, whether LA-GS is a better discriminator of elevated LAP compared to other non-invasive indices in a non-selected population cannot be assessed. The present study did not include a validation cohort, which warrants further studies to validate the established cut-off values as a necessary next step. AF is common in HF. Similarly, to other echocardiographic indices, according to our results LA-GS does not reliably reflect LAP in AF, which hinders the routine applicability of this metric. In contrast, LA-GS remained a reliable marker in patients on VP; however, the sample size of only 32 patients in this subgroup warrants confirmation in larger studies. Importantly, LA-GS measurements are not directly comparable to results obtained by deformation analysis packages from different vendors, thus the current results might not be representative in studies performed with different instrumentation. Finally, our cohort included a large number of highly symptomatic patients with extensive LA remodeling, warranting validation of this approach in less severe cases.
Conclusion
We demonstrate that LA-GS comprises a feasible and fairly accurate tool for the identification of abnormally elevated LAP either at rest or on exertion in patients with known or suspected heart failure. This together with the revealed prognostic value in HF patients advocates for the incremental value of LA-GS in non-invasive HF diagnostics.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Figure S1. Patient selection process. Distribution of patients according to invasive pressure measurement results. RHC, right heart catheterization; HF, heart failure; PH, pulmonary hypertension; ARVC, arrhythmogenic right ventricular cardiomyopathy; PAWPM, mean pulmonary capillary wedge pressure as measured by RHC (PNG 40 KB)
Funding
This project was supported by the János Bolyai Scholarship of the Hungarian Academy of Sciences. LHL reports grants from the Swedish Research Council [Grants 2013-23897-104604-23 and 523-2014-2336], the Swedish Heart Lung Foundation [grants 20120321 and 20150557] and the Stockholm County Council [Grant 20110120].
Compliance with ethical standards
Conflict of interest
The authors declare that they have no competing interests.
References
- 1.Dorfs S, Zeh W, Hochholzer W, Jander N, Kienzle RP, Pieske B, Neumann FJ. Pulmonary capillary wedge pressure during exercise and long-term mortality in patients with suspected heart failure with preserved ejection fraction. Eur Heart J. 2014;35:3103–3112. doi: 10.1093/eurheartj/ehu315. [DOI] [PubMed] [Google Scholar]
- 2.Obokata M, Kane GC, Reddy YN, Olson TP, Melenovsky V, Borlaug BA. Role of diastolic stress testing in the evaluation for heart failure with preserved ejection fraction: a simultaneous invasive-echocardiographic study. Circulation. 2017;135:825–838. doi: 10.1161/CIRCULATIONAHA.116.024822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nagueh SF, Smiseth OA, Appleton CP, Byrd BF, 3rd, Dokainish H, Edvardsen T, Flachskampf FA, Gillebert TC, Klein AL, Lancellotti P, Marino P, Oh JK, Popescu BA, Waggoner AD. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the american society of echocardiography and the european association of cardiovascular imaging. J Am Soc Echocardiogr. 2016;29:277–314. doi: 10.1016/j.echo.2016.01.011. [DOI] [PubMed] [Google Scholar]
- 4.Balaney B, Medvedofsky D, Mediratta A, Singh A, Ciszek B, Kruse E, Shah AP, Addetia K, Lang RM, Mor-Avi V. Invasive validation of the echocardiographic assessment of left ventricular filling pressures using the 2016 diastolic guidelines: head-to-head comparison with the 2009 guidelines. J Am Soc Echocardiogr. 2018;31:79–88. doi: 10.1016/j.echo.2017.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hummel YM, Liu LCY, Lam CSP, Fonseca-Munoz DF, Damman K, Rienstra M, van der Meer P, Rosenkranz S, van Veldhuisen DJ, Voors AA, Hoendermis ES. Echocardiographic estimation of left ventricular and pulmonary pressures in patients with heart failure and preserved ejection fraction: a study utilizing simultaneous echocardiography and invasive measurements. Eur J Heart Fail. 2017;19:1651–1660. doi: 10.1002/ejhf.957. [DOI] [PubMed] [Google Scholar]
- 6.Lancellotti P, Galderisi M, Edvardsen T, Donal E, Goliasch G, Cardim N, Magne J, Laginha S, Hagendorff A, Haland TF, Aaberge L, Martinez C, Rapacciuolo A, Santoro C, Ilardi F, Postolache A, Dulgheru R, Mateescu AD, Beladan CC, Deleanu D, Marchetta S, Auffret V, Schwammenthal E, Habib G, Popescu BA. Echo-doppler estimation of left ventricular filling pressure: results of the multicentre EACVI euro-filling study. Eur Heart J Cardiovasc Imaging. 2017;18:961–968. doi: 10.1093/ehjci/jex067. [DOI] [PubMed] [Google Scholar]
- 7.Santos AB, Roca GQ, Claggett B, Sweitzer NK, Shah SJ, Anand IS, Fang JC, Zile MR, Pitt B, Solomon SD, Shah AM. Prognostic relevance of left atrial dysfunction in heart failure with preserved ejection fraction. Circ Heart Fail. 2016;9:e002763. doi: 10.1161/CIRCHEARTFAILURE.115.002763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pellicori P, Zhang J, Lukaschuk E, Joseph AC, Bourantas CV, Loh H, Bragadeesh T, Clark AL, Cleland JG. Left atrial function measured by cardiac magnetic resonance imaging in patients with heart failure: clinical associations and prognostic value. Eur Heart J. 2015;36:733–742. doi: 10.1093/eurheartj/ehu405. [DOI] [PubMed] [Google Scholar]
- 9.Nappo R, Degiovanni A, Bolzani V, Sartori C, Di Giovine G, Cerini P, Fossaceca R, Kovacs SJ, Marino PN. Quantitative assessment of atrial conduit function: a new index of diastolic dysfunction. Clin Res Cardiol. 2016;105:17–28. doi: 10.1007/s00392-015-0882-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Melenovsky V, Hwang SJ, Redfield MM, Zakeri R, Lin G, Borlaug BA. Left atrial remodeling and function in advanced heart failure with preserved or reduced ejection fraction. Circ Heart Fail. 2015;8:295–303. doi: 10.1161/CIRCHEARTFAILURE.114.001667. [DOI] [PubMed] [Google Scholar]
- 11.Santos AB, Kraigher-Krainer E, Gupta DK, Claggett B, Zile MR, Pieske B, Voors AA, Lefkowitz M, Bransford T, Shi V, Packer M, McMurray JJ, Shah AM, Solomon SD, Investigators P. Impaired left atrial function in heart failure with preserved ejection fraction. Eur J Heart Fail. 2014;16:1096–1103. doi: 10.1002/ejhf.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Altekin RE, Yanikoglu A, Karakas MS, Ozel D, Kucuk M, Yilmaz H, Demir I. Assessment of left atrial dysfunction in obstructive sleep apnea patients with the two dimensional speckle-tracking echocardiography. Clin Res Cardiol. 2012;101:403–413. doi: 10.1007/s00392-011-0404-2. [DOI] [PubMed] [Google Scholar]
- 13.Degiovanni A, Boggio E, Prenna E, Sartori C, De Vecchi F, Marino PN. From the Novara Atrial Fibrillation Study G. Association between left atrial phasic conduit function and early atrial fibrillation recurrence in patients undergoing electrical cardioversion. Clin Res Cardiol. 2018;107:329–337. doi: 10.1007/s00392-017-1188-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cameli M, Lisi M, Righini FM, Massoni A, Natali BM, Focardi M, Tacchini D, Geyer A, Curci V, Di Tommaso C, Lisi G, Maccherini M, Chiavarelli M, Massetti M, Tanganelli P, Mondillo S. Usefulness of atrial deformation analysis to predict left atrial fibrosis and endocardial thickness in patients undergoing mitral valve operations for severe mitral regurgitation secondary to mitral valve prolapse. Am J Cardiol. 2013;111:595–601. doi: 10.1016/j.amjcard.2012.10.049. [DOI] [PubMed] [Google Scholar]
- 15.Nagy AI, Hage C, Merkely B, Donal E, Daubert JC, Linde C, Lund LH, Manouras A. Left atrial rather than left ventricular impaired mechanics are associated with the pro-fibrotic st2 marker and outcomes in heart failure with preserved ejection fraction. J Intern Med. 2018;283:380–391. doi: 10.1111/joim.12723. [DOI] [PubMed] [Google Scholar]
- 16.Wakami K, Ohte N, Asada K, Fukuta H, Goto T, Mukai S, Narita H, Kimura G. Correlation between left ventricular end-diastolic pressure and peak left atrial wall strain during left ventricular systole. J Am Soc Echocardiogr. 2009;22:847–851. doi: 10.1016/j.echo.2009.04.026. [DOI] [PubMed] [Google Scholar]
- 17.Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T, Lancellotti P, Muraru D, Picard MH, Rietzschel ER, Rudski L, Spencer KT, Tsang W, Voigt JU. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the american society of echocardiography and the european association of cardiovascular imaging. Eur Heart J Cardiovasc Imaging. 2015;16:233–270. doi: 10.1093/ehjci/jev014. [DOI] [PubMed] [Google Scholar]
- 18.Yoshida A, Kadota K, Kambara H, Tamaki S, Suzuki Y, Kawai C, Tamaki N, Torizuka K. Left ventricular responses to supine bicycle exercise assessed by radionuclide angiocardiography and a swan-ganz catheter. Jpn Circ J. 1985;49:661–671. doi: 10.1253/jcj.49.661. [DOI] [PubMed] [Google Scholar]
- 19.Thadani U, Parker JO. Hemodynamics at rest and during supine and sitting bicycle exercise in normal subjects. Am J Cardiol. 1978;41:52–59. doi: 10.1016/0002-9149(78)90131-5. [DOI] [PubMed] [Google Scholar]
- 20.Reddy YNV, Carter RE, Obokata M, Redfield MM, Borlaug BA (2018) A simple, evidence-based approach to help guide diagnosis of heart failure with preserved ejection fraction. Circulation [DOI] [PMC free article] [PubMed]
- 21.Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA, Waggoner AD, Flachskampf FA, Pellikka PA, Evangelista A. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. J Am Soc Echocardiogr. 2009;22:107–133. doi: 10.1016/j.echo.2008.11.023. [DOI] [PubMed] [Google Scholar]
- 22.Appleton CP, Kovacs SJ. The role of left atrial function in diastolic heart failure. Circ Cardiovasc Imaging. 2009;2:6–9. doi: 10.1161/CIRCIMAGING.108.845503. [DOI] [PubMed] [Google Scholar]
- 23.Cameli M, Sparla S, Losito M, Righini FM, Menci D, Lisi M, D’Ascenzi F, Focardi M, Favilli R, Pierli C, Fineschi M, Mondillo S. Correlation of left atrial strain and doppler measurements with invasive measurement of left ventricular end-diastolic pressure in patients stratified for different values of ejection fraction. Echocardiography. 2016;33:398–405. doi: 10.1111/echo.13094. [DOI] [PubMed] [Google Scholar]
- 24.Kuppahally SS, Akoum N, Burgon NS, Badger TJ, Kholmovski EG, Vijayakumar S, Rao SN, Blauer J, Fish EN, Dibella EV, Macleod RS, McGann C, Litwin SE, Marrouche NF. Left atrial strain and strain rate in patients with paroxysmal and persistent atrial fibrillation: relationship to left atrial structural remodeling detected by delayed-enhancement mri. Circ Cardiovasc Imaging. 2010;3:231–239. doi: 10.1161/CIRCIMAGING.109.865683. [DOI] [PubMed] [Google Scholar]
- 25.Hanna N, Cardin S, Leung TK, Nattel S. Differences in atrial versus ventricular remodeling in dogs with ventricular tachypacing-induced congestive heart failure. Cardiovasc Res. 2004;63:236–244. doi: 10.1016/j.cardiores.2004.03.026. [DOI] [PubMed] [Google Scholar]
- 26.Sun Y, Ramires FJ, Weber KT. Fibrosis of atria and great vessels in response to angiotensin ii or aldosterone infusion. Cardiovasc Res. 1997;35:138–147. doi: 10.1016/S0008-6363(97)00097-7. [DOI] [PubMed] [Google Scholar]
- 27.Khoo CW, Krishnamoorthy S, Lim HS, Lip GY. Assessment of left atrial volume: a focus on echocardiographic methods and clinical implications. Clin Res Cardiol. 2011;100:97–105. doi: 10.1007/s00392-010-0222-y. [DOI] [PubMed] [Google Scholar]
- 28.Braunauer K, Pieske-Kraigher E, Belyavskiy E, Aravind-Kumar R, Kropf M, Kraft R, Frydas A, Marquez E, Osmanoglou E, Tschope C, Edelmann F, Pieske B, Dungen HD, Morris DA. Early detection of cardiac alterations by left atrial strain in patients with risk for cardiac abnormalities with preserved left ventricular systolic and diastolic function. Int J Cardiovasc Imaging. 2018;34:701–711. doi: 10.1007/s10554-017-1280-2. [DOI] [PubMed] [Google Scholar]
- 29.Bauer A, Khalil M, Ludemann M, Bauer J, Esmaeili A, De-Rosa R, Voelkel NF, Akintuerk H, Schranz D. Creation of a restrictive atrial communication in heart failure with preserved and mid-range ejection fraction: effective palliation of left atrial hypertension and pulmonary congestion. Clin Res Cardiol. 2018;107:845–857. doi: 10.1007/s00392-018-1255-x. [DOI] [PubMed] [Google Scholar]
- 30.Tschope C, Birner C, Bohm M, Bruder O, Frantz S, Luchner A, Maier L, Stork S, Kherad B, Laufs U. Heart failure with preserved ejection fraction: Current management and future strategies: Expert opinion on the behalf of the nucleus of the “heart failure working group” of the german society of cardiology (dkg) Clin Res Cardiol. 2018;107:1–19. doi: 10.1007/s00392-017-1170-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Patient selection process. Distribution of patients according to invasive pressure measurement results. RHC, right heart catheterization; HF, heart failure; PH, pulmonary hypertension; ARVC, arrhythmogenic right ventricular cardiomyopathy; PAWPM, mean pulmonary capillary wedge pressure as measured by RHC (PNG 40 KB)