Abstract
Purpose
Mild traumatic brain injury (TBI) is common but accurate diagnosis and its clinical consequences have been a problem. Maxillofacial trauma does have an association with TBI. Neuron-specific enolase (NSE) has been developed to evaluate neuronal damage. The objective of this study was to investigate the accuracy of NSE serum levels to detect mild brain injury of patients with sustained maxillofacial fractures during motor vehicle accidents.
Methods
Blood samples were drawn from 40 healthy people (control group) and 48 trauma patients who has sustained isolated maxillofacial fractures and mild brain injury in motor vehicle accidents. Brain injuries were graded by Glasgow Coma Scale. In the trauma group, correlations between the NSE serum value and different facial fracture sites were also assessed.
Results
The NSE serum level (mean ± SD, ng/ml) in the 48 patients with maxillofacial fractures and mild TBI was 13.12 ± 9.68, significantly higher than that measured in the healthy control group (7.72 ± 1.82, p < 0.001). The mean NSE serum level (ng/ml) in the lower part of the facial skeleton (15.44 with SD 15.34) was higher than that in the upper facial part (12.42 with SD 7.68); and the mean NSE level (ng/ml) in the middle-and lower part (11.97 with SD 5.63) was higher than in the middle part (7.88 with SD 2.64).
Conclusion
An increase in NSE serum levels can be observed in patients sustained maxillofacial fractures and mild brain injury.
Keywords: Neuron-specific enolase, Serum, Maxillofacial fractures, Mild brain injuries
Introduction
Mild traumatic brain injury (TBI) is common. Its accurate diagnosis and clinical consequences remain a problem. Mild TBI causes transient neurophysiologic brain dysfunction, sometimes with structural axonal and neuronal damage. Clinically mild TBI presents late phase post-traumatic symptoms such as headache, dizziness, imbalance, fatigue, sleep disruption, and impaired cognition. These symptoms resolve for several days even weeks and they are largely related to brain trauma and concomitant injuries. The late phase post-traumatic symptoms exist in minority of patients, consisting of somatic, emotional, and cognitive symptoms. Effective management at early phase may prevent or limit the later phase symptoms, which should includes education about symptoms and expectations for recovery, as well as recommendations for activity modifications.1
In a recent retrospective study, Salentijn et al.2 found that maxillofacial trauma does have an association with TBI. In comparison to the overall maxillofacial trauma population, their results demonstrate that frontal sinus fractures are more commonly diagnosed to accompany brain injury and the location of impact is potentially considered to be the cause. Despite substantial progress in post-traumatic neuro-monitoring, it remains difficult to quantify the exact extent of brain injuries sustained during such fractures. To date the Glasgow Coma Scale (GCS) is still considered to be the gold standard in assessing the consciousness level of TBI patients after trauma (Teasdale and Jennett 1974).3 However the GCS scale lacks of specificity to assess the exact magnitude of brain injuries sustained during the trauma. Even with the current used scale like the Marshall CT classification, such injuries still remain difficult to assess.4
Despite numerous studies on maxillofacial trauma combined with TBI have been carried out,5, 6, 7, 8, 9 the information on undetected mild brain injuries in maxillofacial trauma patients after vehicle accidents is rare. Knowing the consequences of untreated mild brain injury is very important to detect TBI in early stage.
In recent years, several new biomarkers have been developed to evaluate neuronal injuries and have ever since become increasingly important supplements to the GCS. Neuron-specific enolase (NSE) is one of such protein-based enzyme found primarily within neurons and is commonly used to assess the grade of neuronal damage after trauma.10, 11, 12, 13, 14 Increased concentration of NSE can be measured in the cerebrospinal fluid and peripheral blood after neuronal damage and thus provides a quick and reliable laboratory indicator for the degrees of brain cell damage sustained after trauma.15
The present pilot study aims to investigate the NSE serum levels in patients that sustained maxillofacial fractures during motor vehicle accidents. Furthermore we also assessed the differences of NSE serum values at different maxillofacial fracture sites, hopefully to investigate prospectively the accuracy of NSE in detecting mild brain injuries in patients with maxillofacial trauma.
Methods
Ethical approval was granted by the Health Research Ethics Committee at the Faculty of Medicine University of Padjadjaran/Dr. Hasan Sadikin General Hospital Bandung, Indonesia.
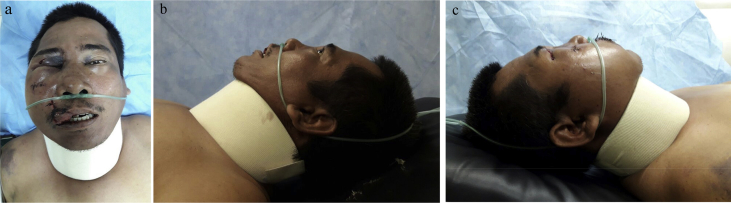
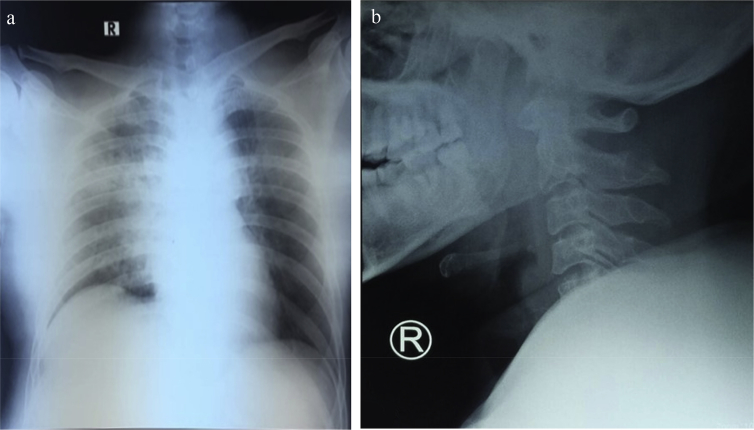
Patients presented with isolated maxillofacial injuries during motor vehicle accidents (Fig. 1), structural imaging normal (Fig. 2), loss of consciousness for 0–30 min, alteration of consciousness/mental state up to 24 h, and post-traumatic amnesia for 0–1 day were investigated. Only patients with a mild brain injury (GCS score 13–15) were included in this study. Patients with multiple traumas with Abbreviated Injury Score (AIS) ≥ 3 in other body region were excluded from the study.
Fig. 1.
Clinical view of a patient who presented with isolated maxillofacial injuries in a motor vehicle accident. (A) frontal view; (B, C) lateral view.
Fig. 2.
Structural images of a patient in the trauma group. (A) Chest X-ray: no sign of fracture of the costae or scapulae clavicle and no sign of cardiomegaly. (B) Cervical X-ray; within normal limit.
A total of 62 patients with maxillofacial injuries were surgically treated in the three months study period. However eleven patients had to be excluded from the study due to the incomplete medical data. Two patients were excluded due to pulmonary disease and one patient was excluded because he decided to leave the hospital before completing his treatment. In the end the trauma group consisted of 48 adult patients who had sustained isolated maxillofacial fractures during motor vehicle accidents in the Bandung area. Prognosis of all patients was good. The control group employed 40 healthy adults with no history of facial trauma who underwent routine medical checkup at the Dr. Hasan Sadikin Hospital in Bandung.
The fracture locations were divided into three parts: upper, middle and lower part. The upper part of facial skeleton is comprised of the frontal bone; the middle part comprised of the midfacial bone, the maxilla, the nasoethmoid, and the lateral midfacial bone-zygoma, and the lower part comprised of the mandible.
Blood samples were withdrawn from trauma patients and healthy controls by peripheral vein puncture. All NSE measurements were performed with an electrochemiluminescence immunoassay (ECLIA), using a sandwich technique in duplicate, with NSE kits (Roche, Mannheim, Germany) and the Elecsys 2010 analyzer (Roche Diagnostics, Mannheim, Germany). Since the half-life of NSE in the serum is approximately 48 h,16 all trauma and healthy patients in this study underwent NSE screening within 24 h.
In the trauma group, the time from injury to blood drawn was 30 h in one patient, 28 h in another, and <24 h for the rest. Furthermore it must be noted that NSE values vary from hour to hour after trauma and subsequently reflect the status of axonal injury.17
The statistical analysis was performed using SPSS (IBM). The Mann-Whitney test was used to assess the NSE serum levels of all maxillofacial fracture patients and the results were subsequently compared to those of the healthy group. Furthermore the Kruskal-Wallis test was used to calculate the mean increase in NSE serum levels in correlation to the location of maxillofacial fractures. Finally the Spearman's ranked correlation was used to calculate the correlation between the increased serum NSE levels and location of maxillofacial fractures in adult patients with mild head injury. A p value less than 0.05 was considered to be statistically significant.
Results
Of the trauma group, which consisted of 48 traumaxillofacial fracture patients with mild brain injury, the mean age was 27.56 (range 19–65) years; whereas the mean age was 37.12 (range 19–65) years for healthy subjects. The gender distribution was 41 males/7 females in trauma group and 24 males/16 females in healthy group.
The mean NSE serum level (ng/ml) in the trauma group was 13.12 ± 9.68 (SD) which proved to be significantly higher than the healthy control group, i.e. 7.72 ± 1.82 (SD) (p < 0.001, Table 1).
Table 1.
NSE serum levels in the trauma patients and healthy controls.
| Group | NSE Results (ng/mL) |
Range | p value | |
|---|---|---|---|---|
| Mean | SD | |||
| Trauma group (n = 48) | 13.12 | 9.68 | 3.19–54.51 | <0.001 |
| Healthy group (n = 40) | 7.72 | 1.82 | 4.27–10.70 | |
The mean NSE serum value recorded in the male patients differed from that in the female patients, however the result was not significant (p > 0.05) (Table 2).
Table 2.
Serum NSE levels in patients with facial injury divided into gender and fracture site.
| Variables | NSE Results (ng/mL) |
Significance | p value | |
|---|---|---|---|---|
| Mean | SD | |||
| Gender | ZMW = 0.174 | 0.183a | ||
| Male (n = 41) | 11.13 | 9.40 | ||
| Female (n = 7) | 17.57 | 10.77 | ||
| Fractures site | X2KW = 9.518 | 0.049b | ||
| Upper (n = 17) | 12.42 | 7.68 | ||
| Middle (n = 22) | 7.88 | 2.64 | ||
| Lower (n = 9) | 15.44 | 15.34 | ||
ZMW = Mann-Whitney test.
X2KW = Kruskall-Wallis test.
Table 3 demonstrates that the mean NSE values in patients with a lower part facial fracture and patients with a combination of fractures in all three facial parts were significantly higher than that recorded in patients with only upper facial fractures (Kruskall-Wallis) (p < 0.05).
Table 3.
The correlation between NSE serum level and the fracture location.
| Facial fracture location | rs | p value |
|---|---|---|
| Upper (n = 17) | 0.25 | 0.091 |
| Middle (n = 22) | 0.05 | 0.726 |
| Lower (n = 9) | 0.23 | 0.121 |
| Total | 0.33 | 0.020 |
rs Spearman ranked correlation coefficient.
Note: Upper: the frontal bone; Middle: the midfacial bone, the maxilla, the nasoethmoid, and the lateral midfacial bone-zygoma;Lower: the mandible.
As shown in Table 3, the result of Spearman ranked correlation test demonstrates a significant correlation between NSE and location of facial fractures (upper, middle and lower facial skeleton) (p = 0.02).
Discussion
Maxillofacial fractures are mainly caused by motor vehicle accidents and can be accompanied with TBI.5, 6, 7, 8, 9 Mild brain injuries have severe future consequences when not detected at the early stage. Until now information related to undetected mild brain injuries is rare. In this pilot study we aimed to investigate the accuracy of NSE in detecting mild brain injuries. The NSE levels of patients with maxillofacial fractures accompanied with mild brain injuries were compared to those of normal persons. The findings indicate that patients having sustained facial fractures have higher NSE values than healthy controls. Furthermore the results showed no gender differences in serum NSE levels in adult facial fracture patients. These results are comparable to those reported by Hayes et al.10 and Wu et al.12 which suggest that serum NSE levels are not gender bases.
Furthermore the NSE levels differed significantly depending on the location of facial fractures. The lowest NSE level was recorded in the midfacial part, implying that the midfacial bony structures absorb traumatic forces better than other bony structures and subsequently protect the neurocranium from heavy trauma.18 The midface anatomy is unique in its scaffold-like structure and offers vertical supporting structures, i.e., nasomaxillar, zigomaticomaxillar, and pterigomaxilar buttresses; and horizontal supporting structures, i.e., lateral antrum, medial nasal wall, and zygomatic arc.19
The aforementioned differences in sight-specific NSE values can be due to biomechanical differences in the bony structures of the upper facial area when compared to the midface region. The upper facial bones often lack of sufficient amount of cancellous bone, therefore the scaffold-like structure of the midface responds with a minimum deformation to a load increase induced by a trauma. This lack of deformation subsequently leads to higher forces induced on the skull and increases the risk of head injury as previously reported by Lee et al.18 and by Salentijn et al.2
Interestingly all patients who had sustained blows to their lower jaws in our study had higher NSE values. These results agree with a study held by Keenan et al.20 indicating that facial fractures are markers to a high risk of brain injury. However these results are contradictive to the same study mentioned earlier by Lee et al.18 who reported that patients who had sustained injuries in the lower facial part (mandible) had less risk for sustaining a head injury. One explanation for the higher NSE values in the patients who sustained fractures in the lower jaw could be due to the direct energy transmission into the skull base and brain. The impact acted to the lower jaw forces are transmitted through the condyles into the disks and directly into the temporal bone, hence skull base causing a possible increase in the NSE serum values. Interestingly in clinical settings, mandible fractures are often classified as being less problematic than midface traumas. A recent study by Salentijn et al.2 reported that fractures of the midface and upper third part of the skull are more prone to cause brain injury than mandibular fractures. The results of the present study are not in good agreement with the aforementioned clinical studies by Salentijn et al.2
In several recent articles, authors state that NSE is released into the blood by hemolysis, which may be a serious source of error in some cases.21 Furthermore, increases in NSE levels have been observed in multiple types of trauma with and without TBI, limiting its ability to properly discriminate the magnitude of brain injury.21 As our pilot study is limited in NSE level in maxillofacial fracture patients without mild brain injury, further research using a more comparable control group should be conducted to decisively sum up a conclusion on this issue. In addition, the number of cases involved in this study is limited, thus should be enhanced in subsequent research.
In conclusion, despite the shortcomings of the present pilot study, it can be carefully concluded that an increase in NSE serum levels is able to be observed in patients who have sustained maxillofacial fractures and mild brain injury. Further, our findings suggest that maxillofacial fracture patients may sustain mild brain injuries which can remain undiagnosed in clinical settings. However to draw firm conclusion on the accuracy of NSE measurement in discriminating between patients with maxillofacial trauma accompanied with mild brain injury and patients with maxillofacial injury without brain injury, a prospective study consisting of these two group of patients is mandatory.
Competing interests
The authors declare that they have no competing interests.
Funding
Nil.
Ethical statement
This study was approved by the Health Research Ethics Committee at the Faculty of Medicine University of Padjadjaran/Dr. Hasan Sadikin General Hospital Bandung, Indonesia. Informed consent was obtained from all individual participants included in the study.
Footnotes
Peer review under responsibility of Chinese Medical Association.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.cjtee.2018.12.004.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Katz D.I., Cohen S.I., Alexander M.P. Mild traumatic brain injury. Handb Clin Neurol. 2015;127:131–156. doi: 10.1016/B978-0-444-52892-6.00009-X. https://doi: 10.1016/B978-0-444-52892-6.00009-X [DOI] [PubMed] [Google Scholar]
- 2.Salentijn E.G., Peerdeman S.M., Boffano P. A ten-year analysis of the traumatic maxillofacial and brain injury patient in Amsterdam: incidence and aetiology. J Cranio-Maxillo-Fac Surg. 2014;426:705–710. doi: 10.1016/j.jcms.2013.12.008. https://doi: 10.1016/j.jcms.2013.12.008 [DOI] [PubMed] [Google Scholar]
- 3.Teasdale G., Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2:81–84. doi: 10.1016/S0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- 4.Kobeissy F.H., Ottens A.K., Zhang Z. Novel differential neuroproteomics analysis of traumatic brain injury in rats. Mol Cell Proteomics. 2006;5:1887–1898. doi: 10.1074/mcp.M600157-MCP200. https://doi [DOI] [PubMed] [Google Scholar]
- 5.Gassner R., Tuli T., Hachl O. Cranio-maxillofacial trauma: a 10 year review of 9543 cases with 21067 injuries. J Cranio-Maxillo-Fac Surg. 2003;31:51–61. doi: 10.1016/s1010-5182(02)00168-3. [DOI] [PubMed] [Google Scholar]
- 6.Thoren H., Snall J., Salo J. Occurrence and types of associated injuries in patients with fractures of the facial bones. J Oral Maxillofac Surg. 2010;68:805–810. doi: 10.1016/j.joms.2009.09.057. https://doi:10.1016/j.joms.2009.09.057 [DOI] [PubMed] [Google Scholar]
- 7.Shankar A.N., Shankar V.N., Hegde N. The pattern of the maxillofacial fractures – A multicenter retrospective study. J Cranio-Maxillo-Fac Surg. 2011;40:467–469. doi: 10.1016/j.jcms.2011.11.004. https://doi:10.1016/j.jcms.2011.11.004 [DOI] [PubMed] [Google Scholar]
- 8.Allareddy V., Allareddy V., Nalliah R.P. Epidemiology of facial fracture injuries. J Oral Maxillofac Surg. 2011;69:2613–2618. doi: 10.1016/j.joms.2011.02.057. https://doi:10.1016/j.joms.2011.02.057 [DOI] [PubMed] [Google Scholar]
- 9.Rajandram R.K., Syed O.S.N., Rashdi M.F. Maxillofacial injuries and traumatic brain injury – a pilot study. Dent Traumatol. 2014;30:128–132. doi: 10.1111/edt.12052. https://doi:10.1111/edt.12052 [DOI] [PubMed] [Google Scholar]
- 10.Hayes RL, Wang KKW, Tortella FC, et al. Biochemical markers of brain injury: applications to combat casualty care. https://www.researchgate.net/publication/235021461_Biochemical_Markers_of_Brain_Injury_Applications_to_Combat_Casualty_Care.
- 11.Pineda J.A., Wang K.K.W., Hayes R. Biomarkers of proteolytic damage following traumatic brain injury. Brain Pathol. 2004;14:202–209. doi: 10.1111/j.1750-3639.2004.tb00054.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wu Y.C., Zhao Y.B., Lu C.Z. Correlation between serum level of neuron-specific enolase and long-term functional outcome after acute cerebral infarction: prospective study. Hong Kong Med J. 2004;10:251–254. [PubMed] [Google Scholar]
- 13.Wang K.K., Ottens A.K., Liu M.C. Proteomic identification of biomarkers of traumatic brain injury. Expert Rev Proteomics. 2005;2:603–614. doi: 10.1586/14789450.2.4.603. https://doi:10.1586/14789450.2.4.603 [DOI] [PubMed] [Google Scholar]
- 14.Laterza O.F., Modur V.R., Crimmins D.L. Identification of novel brain biomarkers. Clin Chem. 2006;52:1713–1721. doi: 10.1373/clinchem.2006.070912. https://doi:10.1373/clinchem.2006.070912 [DOI] [PubMed] [Google Scholar]
- 15.Ergun R., Bostanci U., Akdemir G. Prognostic value of serum neuron-specific enolase after head injury. Neural Res. 1998;20:418–420. doi: 10.1080/01616412.1998.11740541. [DOI] [PubMed] [Google Scholar]
- 16.Wunderlich M.T., Ebert A.D., Kratz T. Early neurobehavioral outcome after stroke is related to release of neurobiochemical markers of brain damage. Stroke. 1999;30:1190–1195. doi: 10.1161/01.str.30.6.1190. [DOI] [PubMed] [Google Scholar]
- 17.Bazarian J.J., Merchant-Borna K. Tau, s-100 calcium-binding protein B, and neuron-specific enolase as biomarkers of concussion. JAMA Neurol. 2014;71:925–926. doi: 10.1001/jamaneurol.2014.1082. https://doi:10.1001/jamaneurol.2014.1082 [DOI] [PubMed] [Google Scholar]
- 18.Lee K.F., Wagner L.K., Lee Y.E. The impact-absorbing effect of facial fractures in closed-head injuries. J Neurosurg. 1987;66:542–547. doi: 10.3171/jns.1987.66.4.0542. https://doi:10.3171/jns.1987.66.4.0542 [DOI] [PubMed] [Google Scholar]
- 19.Plaisier B.R., Punjabi A.P., Super D.M. The relationship between facial fractures and death from neurologic injury. J Oral Maxillofac Surg. 2000;58:708–712. doi: 10.1053/joms.2000.7250. https://doi:10.1053/joms.2000.7250 [DOI] [PubMed] [Google Scholar]
- 20.Keenan H.T., Brundage S.I., Thompson D.C. Does the face protect the brain? A case-control study of traumatic brain injury and facial fractures. Arch Surg. 1999;134:14–17. doi: 10.1001/archsurg.134.1.14. [DOI] [PubMed] [Google Scholar]
- 21.Yokobori S., Hosein K., Burks S. Biomarkers for the clinical differential diagnosis in traumatic brain injury; a systematic review. CNS Neurosci Ther. 2013;19:556–565. doi: 10.1111/cns.12127. https://doi:10.1111/cns.12127 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.