Sir,
An 18-year-old male patient diagnosed with Crouzon syndrome (CS) was posted for subcranial osteotomy and distracter application. On examination patient had a short neck, short nose with depressed bridge, short philthrum, high arched palate, receded upper alveolar ridge and proptosis of eyeball with telecanthus. Mouth opening was 2.5 cm with restricted neck movements. Modified Mallampati grade 4, thyromental distance of 5 cm and sterno-mental distance of 8 cm was noted. Distance between the cricoid cartilage and sternal notch was just 1.5 cm and no tracheal rings could be palpated above the sternal notch.
An ultrasonography (USG) examination of the airway was done with the patient supine and neck extended, using a high-frequency linear probe (6-13 MHz). It revealed enlarged false cords suggestive of periglottic oedema [Figure 1a]. The vocal chords showed normal movement [Figure 1c]. No tracheal rings could be appreciated above the sternum and the cricoid cartilage was just above it. Lateral view X-ray of the neck was suggestive of fusion of C3-C4 and C5-C6 vertebrae. X-ray and USG findings were further corroborated with 3D reconstructed computed tomography (CT) images [Figure 2].
Figure 1.
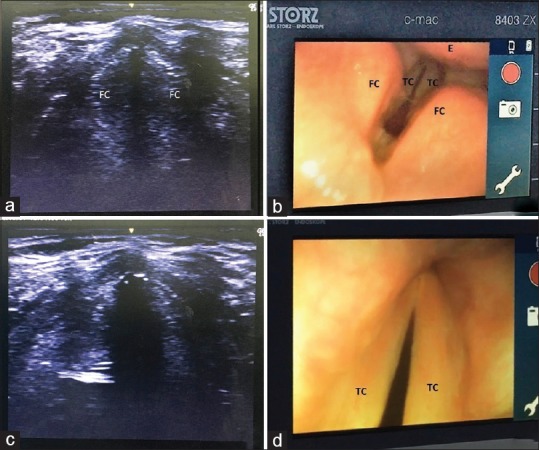
FC: False chords, TC: True chords, E: Epiglottis. (a) Ultrasound image of enlarged false chords. (b) Fibreoptic view of enlarged false chords. (c) Ultrasound image at the level of vocal chords (Inspiration). (d) Fibreoptic view of vocal chords (Expiration)
Figure 2.
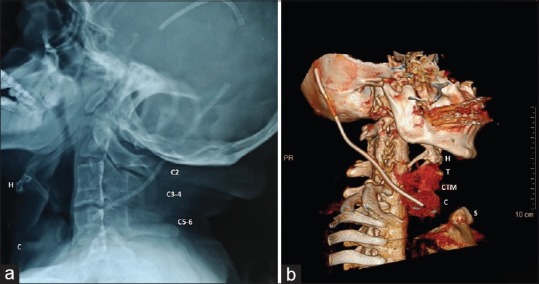
H: Hyoid, T: Thyroid notch, C: Cricoid, CTM: Crico-thyroid membraine, S: Sternal notch, C2-C6: Cervical vertebrae. (a) X-ray neck lateral view. (b) 3D reconstructed CT of neck and larynx
The patient was prepared for an awake fibreoptic intubation as the primary plan for securing the airway. Conventional tracheostomy was ruled out due to short neck and inaccessible trachea after discussion with the otorhinolaryngology team. Elective surgical cricothyroidotomy was thus decided to be the secondary airway management plan which could be used even in case of sudden loss of airway. The cricothyroid membrane (CTM) was pre-marked using USG. Use of laryngeal mask airway was also kept for emergency maintenance of oxygenation and ventilation.
Following premedication and topicalisation of the airway along with airway nerve blocks (USG-guided superior laryngeal nerve block and trans-tracheal block), a fibreoptic scope railroaded with a 7-mm ID flexometallic endotracheal tube (ET) was inserted orally with the help of a bite block. The endoscopic view revealed enlarged and swollen false cords and epiglottis beneath which the true chords were barely visible [Figure 1b and d]. After securing the airway, general anaesthesia was induced. Rest of the intra-operative and post-operative period was uneventful.
CS is a rare genetic condition which causes craniofacial abnormalities and poses specific anaesthetic challenges mainly related to the airway.[1] Point-of-care ultrasound (POCUS) is an emerging tool for a wide variety of anaesthetic uses including airway assessment.[2,3] The current difficult airway guidelines describe numerous options of airway management[4] including secondary airway options following failure of the primary plan. In the present case, the options were restricted and awake fibreoptic intubation was the safest and most feasible option. USG examination revealed abnormal swelling around the glottis which was later confirmed on the endoscopic view. Thus we had reserved the use of LMA only as a rescue technique in case of emergency or airway compromise due to blood/secretions causing laryngospasm requiring deepening the plane of anaesthesia or loss of patient cooperation requiring induction of anaesthesia, with the purpose to maintain ventilation and oxygenation. This in other scenarios would have been a possible secondary option to facilitate awake intubation through an intubating LMA or to guide the fibreoptic scope.[5] Harde et al. in a case report reported difficulty in LMA insertion and ventilation in an adult patient of CS for orthopaedic surgery due to abnormal airway anatomy.[6] Conventional tracheostomy was also not a viable option due to lack of tracheal access above the sternum due to fused cervical vertebrae and extremely short neck, although front of neck access would have been relatively easier due to a lower cricoid cartilage and well-appreciated CTM. This along with the use of LMA was reserved for use in an emergent scenario.
In cases of syndromic airway difficulties, use of advanced radiological adjuncts and bedside techniques such as POCUS can further enhance our assessment of the airway: not just to decide the safest technique but to also rule out unsafe options.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
Dr. Madhubari Vathulya, Department of Burns and Plastic surgery, Departments of Oral and Maxillo-facial surgery, Otorhinolaryngology and Radio-diagnosis, All India Institute of Medical Sciences, Rishikesh, India.
REFERENCES
- 1.Nargozian C. The airway in patients with craniofacial abnormalities. Paediatr Anaesth. 2004;14:53–9. doi: 10.1046/j.1460-9592.2003.01200.x. [DOI] [PubMed] [Google Scholar]
- 2.Kundra P, Mishra SK, Ramesh A. Ultrasound of the airway. Indian J Anaesth. 2011;55:456–62. doi: 10.4103/0019-5049.89868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reddy PB, Punetha P, Chalam KS. Ultrasonography - a viable tool for airway assessment. Indian J Anaesth. 2016;60:807–13. doi: 10.4103/0019-5049.193660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Apfelbaum JL, Hagberg CA, Caplan RA, Blitt CD, Connis RT, Nickinovich DG, et al. Practice guidelines for management of the difficult airway: An updated report by the American Society of Anaesthesiologists Task Force on management of the difficult airway. Anaesthesiology. 2013;118:251–70. doi: 10.1097/ALN.0b013e31827773b2. [DOI] [PubMed] [Google Scholar]
- 5.Kim YH, Kim JH. Tracheal intubation in a patent with Crouzon's syndrome using LMA-Fastrach [TM] with the cook airway exchange catheter. Anaesth Intensive Care. 2009;37:145–6. [PubMed] [Google Scholar]
- 6.Harde M, Suryavanshi V, Chhatrapati S, Vaidyanathan M, Bhadade R. Crouzon syndrome: An anaesthetic challenge. Ain-Shams J Anaesthesiol. 2015;8:683–5. [Google Scholar]


