INTRODUCTION
Transverse abdominis plane block (TAP) blocks have gained widespread use with the availability of ultrasound. TAP catheters, whether placed surgically or ultrasound guided, are very useful in providing prolonged post-operative analgesia for any type of abdominal surgery incisions. Apart from prolonged analgesia, TAP catheters appear to provide good conditions for mobilising post-operative patients without any motor block or hypotension. Local anaesthetic toxicity with TAP block has been reported mainly in parturient for post-operative analgesia after caesarean section and other surgery.[1,2,3,4] While inserting catheters, there is a possibility that the catheter can inadvertently enter the epigastric vessels. However, the incidence of this is not known. We would like to report a case on inadvertent local anaesthetic bolus of TAP block into the vessel, relevant vessel anatomy, sono anatomy and possible techniques used to minimise it.
CASE REPORT
A 54-year-old male had mesenteric panniculitis, diverticulitis and hiatus hernia; there were no other co-morbidities. The indication for laparotomy was recurrent panniculitis of small bowel mesentery with abdominal pain. He underwent laparotomy with midline incision resulting in a number of nodes biopsied for analysis. For post-operative analgesia, he consented for post procedure bilateral lower subcostal TAP block described by Hebbard.[5] This was performed with the ultrasound probe placed just beneath and parallel to the costal margin. The needle was then introduced in plane of the ultrasound beam, and a bolus dose of 0.5% ropivacaine 20 ml on each side was administered followed by the catheters. In recovery, he required 260 mcg of fentanyl. Post-operatively in the ward, he was ordered 8 hourly bolus by the registrar on call. Around midnight when the bolus dose of 20 ml of 0.2% ropivacaine was due to be given, on initial aspiration there was no blood after 5 ml of bolus, on second aspiration blood was noticed and remaining dose was terminated. The patient was monitored for haemodynamic and CNS symptoms assessment. There were no untoward effects. The catheter was pulled back to 2 cm and on further aspiration there was no blood and the catheter was secured. A test dose of 3 ml of 2% adrenalized lignocaine was bolused with no change in heart rate and subsequent doses continued. His pain scores were 1/10 and 4/10 on the second post-operative day. As he didn't require much rescue analgesia (Fentanyl 580 mcg), the catheters were removed. We advised the surgical team on the events. They advised that they had experienced abdominal wall haematoma after performing surgically placed pre-peritoneal catheter, with most likely needle puncturing the branch of superior epigastric vessels.
The superior epigastric artery emerges around the sixth or seventh costal cartilage and is a section of the internal thoracic artery. While moving across the diaphragm in the space between the costal, as well as the sternal parts of the muscle, it declines to the anterior abdominal wall. The superior epigastric artery by entering the gap between the costal and xiphoid slips at the start of the diaphragm and goes inside the rectus and also enters deep to the rectus abdominis and transverse abdominis [Figure 1]. Figure 1 shows the sono anatomy of the branch of the epigastric vessel near the transverse abdominis plane. At the same time, a section of external iliac artery, the inferior epigastric artery, by coming in front of the arcuate line, moves in the sheath. These arteries circulate the rectus muscle and also anastomose along with each other inside the sheath.
Figure 1.
Showing the superimposed images of the vessel anatomy, subcostal probe placement 6 cm from midline and sono anatomy of subcostal transversus abdominis plane with epigastric vessel
DISCUSSION
The TAP block is a regional technique used for providing post-operative analgesia (or potentially, surgical anaesthesia) for a range of clinical procedures. This study reported a reduction in opioid consumption and improvement in post-operative pain relief.[5] Although TAP block is safe, its toxicity from accidental intravascular injection is a very rare event with unknown prevalence. We can however co-relate the occurrence of the surgically placed laparoscopy trocars and injury to the epigastric vessels, which is 0.2%-2%[6] There is a safe zone to avoid epigastric vessels injury for any anterior abdominal wall procedure[6] [Figure 2]. Saber et al. described at the level midway between the xiphoid and the umbilicus, the average distance of the epigastric vessel was 5.50 cm on the right and 5.36 cm on the left.[6] Subcostal TAP blocks are commonly placed near this area [Figure 1]. Avoiding this area and utilising colour Doppler on ultrasound may identify vessels and may reduce injury.
Figure 2.
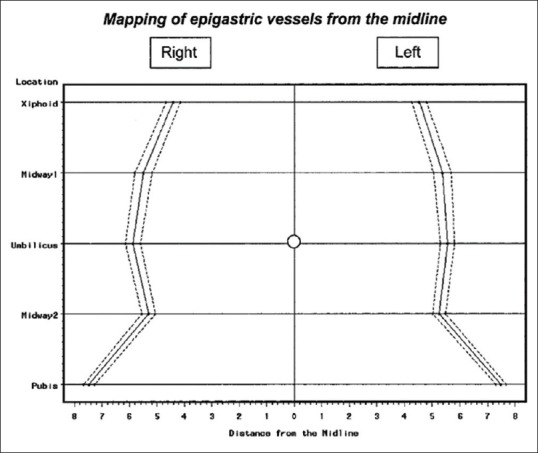
Showing the mapping of the epigastric vessels (permission from Prof A Saber)
There are few cases reported of potentially neurotoxic plasma ropivacaine concentrations in patients receiving TAP blocks after gynaecological laparotomy and caesarean section.[7,8] But it is relatively safe.[9] We had provided intermittent bolus for the advantage of providing the patient with minimal attachments to improve mobility. Spreading the LA through the plane is likely more extensive when it is distended by a bolus, potentially offering more complete coverage. However, we have encountered inadvertent intravenous injection and possible systemic toxicity.
To avoid this situation, there are a few safety precautions. One is to maintain a safe zone to avoid injections and catheters in and around the epigastric vessels.[6] Epigastric vessels (superior and inferior) are usually located in the area between 4 and 8 cm from the midline on the anterior abdominal wall, staying away from this area may reduce the risk. Every intermittent dose administration needs aspiration before injection followed by neuro-haemodynamic observations for 30 minutes. Otherwise, the competent use of continuous ultrasound visualisation during injection also decreases the risk of inadvertent intravascular or intramuscular injection but this is not full proof. Following the ASRA guidelines, safety precautions may reduce the toxicity situations.[10] It involves using lower concentrations of local anaesthetics, dosing on lean body weight, adjunctive epinephrine, and observation for at least 30-45 minutes after the block.
CONCLUSION
Ultrasound guided TAP block is a safe post-operative analgesic technique, but rarely inadvertent intravascular catheter insertion or bolus may be prevented by colour imaging for vessels, intermittent aspiration and small boluses at a time.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Department of anaesthesia and colorectal surgery. The Queen Elizabeth hospital. Woodville.SA. Australia
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Carey A. Safe dose of local anaesthetic for transversus abdominis plane block. Anaesthesia. 2011;66:1048–60. doi: 10.1111/j.1365-2044.2011.06901.x. [DOI] [PubMed] [Google Scholar]
- 2.Ishida T, Tanaka S, Sakamoto A, Hirabayashi T, Kawamata M. Plasma ropivacaine concentration after TAP block in a patient with cardiac and renal failure. Local Reg Anesth. 2018;11:57–60. doi: 10.2147/LRA.S173877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Naidu RK, Richebe P. Probable local anesthetic systemic toxicity in a postpartum patient with acute fatty liver of pregnancy after a transversus abdominis plane block. A A Case Rep. 2013;1:72–4. doi: 10.1097/ACC.0b013e3182973a2f. [DOI] [PubMed] [Google Scholar]
- 4.Weiss E, Jolly C, Dumoulin JL, Meftah RB, Blanié P, Laloë PA, et al. Convulsions in 2 patients after bilateral ultrasound-guided transversus abdominis plane blocks for cesarean analgesia. Reg Anesth Pain Med. 2014;39:248–51. doi: 10.1097/AAP.0000000000000088. [DOI] [PubMed] [Google Scholar]
- 5.Hebbard P. Subcostal transversus abdominis plane block under ultrasound guidance. Anesth Analg. 2008;106:674–5. doi: 10.1213/ane.0b013e318161a88f. [DOI] [PubMed] [Google Scholar]
- 6.Saber AA, Meslemani AM, Davis R, Pimentel R. Safety zones for anterior abdominal wall entry during laparoscopy a CT scan mapping of epigastric vessels. Ann Surg. 2004;239:182–5. doi: 10.1097/01.sla.0000109151.53296.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Torup H, Mitchell AU, Breindahl T, Hansen EG, Rosenberg J, Moller AM. Potentially toxic concentrations in blood of total ropivacaine after bilateral transversus abdominis plane blocks; a pharmacokinetic study. Eur J Anaesthesiol. 2012;29:235–8. doi: 10.1097/EJA.0b013e328350b0d5. [DOI] [PubMed] [Google Scholar]
- 8.Griffiths JD, Barron FA, Grant S, Bjorksten AR, Hebbard P, Royse CF. Plasma ropivacaine concentrations after ultrasound-guided transversus abdominis plane block. Br J Anaesth. 2010;105:853–6. doi: 10.1093/bja/aeq255. [DOI] [PubMed] [Google Scholar]
- 9.Rahiri J, Tuhoe J, Svirskis D, Lightfoot NJ, Lirk PB, Hill AG. Systematic review of the systemic concentrations of local anaesthetic after transversus abdominis plane block and rectus sheath block. Br J Anaesth. 2017;118:517–26. doi: 10.1093/bja/aex005. [DOI] [PubMed] [Google Scholar]
- 10.Neal JM, Barrington MJ, Fettiplace MR, Gitman M, Memtsoudis SG, Mörwald EE, et al. The third American society of regional anesthesia and pain medicine practice advisory on local anesthetic systemic toxicity: Executive summary 2017. Reg Anesth Pain Med. 2018;43:113–23. doi: 10.1097/AAP.0000000000000720. [DOI] [PubMed] [Google Scholar]



