Abstract
Background and Aims:
Perioperative fasting guidelines have been published and updated to standardise practices. Hence, Indian Society of Anaesthesiologists decided to conduct a survey to assess the fasting practices and the food habits across India, which would be subsequently used for developing preoperative fasting guidelines for the Indian population. We detail and discuss herewith the content validity of the questionnaire developed for the survey.
Methods:
Thirty-six questions related to perioperative fasting practices were framed based on the collected evidence and relevance to regional diet and concerns. Subsequently, an information sheet was prepared and sent to 10 experts to grade each question. The responses were tabulated, and item-wise content validity index (I-CVI), scale-wise content validity index (S-CVI) and modified kappa statistic were calculated in Microsoft Excel™ sheet.
Results:
Seven of the 10 experts completed the assessment and grading as per the instructions provided and submitted a completed proforma. S-CVI for relevance, simplicity, clarity and ambiguity was 0.72, 0.86, 0.72 and 0.72, respectively. S-CVI/average or average congruency percentagewas 0.95, 0.97, 0.95 and 0.95 for relevance, simplicity, clarity and ambiguity, respectively. Question 2 received an I-CVI of 0.71 in terms of clarity and question 23 received an I-CVI of 0.71. They were modified as persuggestions of the experts.
Conclusion:
We conclude that our questionnaire designed to ascertain the preoperative fasting practices for a surveymet the content validity criteria both by qualitative and quantitative analyses.
Key words: Fasting, perioperative, questionnaire, survey, validity
INTRODUCTION
Perioperative fasting guidelines have been published and updated in continued attempts to standardise the practices in the surgical population. The guidelines provided by professional associations such as American Society of Anesthesiologists (ASA) and European Society of Anaesthesiologists (ESA) classify food items into solids, clear liquids, breast milk and non-human milk and advise duration of fasting for different subsets of patients based on evidence.[1,2] In India, in the absence of specific guidelines suited for local practice, the guidelines provided by ASA or ESA and others are followed. Hence, Indian Society of Anaesthesiologists decided to assess the fasting practices and the food habits across India, which would be subsequently used for developing preoperative fasting guidelines for the Indian population. We describe the content validity of the questionnaire developed.[3]
The process of development of a validated toolinvolves mainly two steps.[4] The first step involves extensive literature review and development of the questionnaire and the second step involves validation of the questionnaire based on expert opinion. Content validation is an essential step in instrument development as it signifies the extent to which a measurement reflects a specific intended domain of content.[5]
Quantification of the content validity is required and can be done using methods such as content validity index and multirater agreement tests.[5] In this article, we report the development and subsequent validation of a questionnaire to elicit the present perioperative fasting practices across institutions in various parts of India. We used the content validity index and modified kappa statistic (MKS) using the probability of chance agreement as described by Polit et al. to estimate the content validity of the questionnaire developed.[3,6]
METHODS
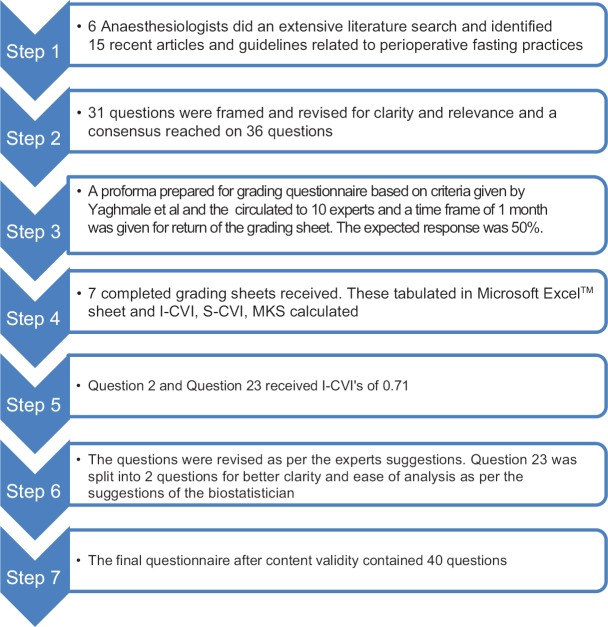
The content questions related to perioperative fasting practices were framed after an extensive literature search by six independent anaesthesiologists, from data bases that included PubMed, Google Scholar, EMBASE, Cochrane Library and guidelines framed by other societies all over the world; the collected information was collated. The search words and phrases used were 'NPO guidelines', 'NBM guidelines', 'fasting guidelines', 'preoperative fasting practices' and 'peri-operative fasting practices'. The bibliographic references were searched manually as well. Fifteen articles including recent review articles and latest guidelines by various societies were identified. Guidelines published after 2010 and recent review articles published after 2015 were taken into account. After collation, 31 questions were framed which underwent intensive scrutiny for clarity and relevance. Grammatical and spelling errors were ironed out. The questionnaire was expanded to 36 questions eliciting information on the perioperative fasting practices based on the collected evidence and with relevance to regional diet and concerns [Figure 1 and Appendix 1 is available online]. Subsequently, an information sheet was prepared for an expert group to grade each question based on relevance, simplicity, clarity and ambiguity of the framed question on a 4-point scale [Appendix 2 is available online]. This scale was adopted from a scale devised by Yaghmale[7] and subsequently used by Emmanueland Clow.[8] The questionnaire and the information sheet for grading the content were sent by e-mail to 10 experts with an experience of at least 10 years in the field of anaesthesiology and hailing from different regions.
Figure 1.
The procedure followed for content validity of the questionnaire
A time frame of 1 month was provided to the experts to assess and grade the questionnaire. The target was receipt of response from at least 50% of the experts at the end of the month. The results were compiled and tabulated (grading of 3 or 4 was labelled as x and any grading of 1 or 2 as 0) in Microsoft Excel™ sheet. The item-wise content validity index (I-CVI) was calculated for each question from the questionnaire using the method described by Polit et al.[3,6] The scale-wise content validity index (S-CVI) and S-CVI/average or average congruency percentage (ACP) were also calculated based on the methods described by Polit et al.[3,6] Probability of chance agreement on relevance (Pc) was calculated using the formula Pc = [N!/{A!(N − A)!}] ×0.5N, where N = number of experts and A = number of experts in agreement on relevance. MKS was calculated using the following formula for each of the questions:
K = I-CVI − Pc/1 − Pc
If the I-CVI was less than 0.78, the group reached a consensus on whether to change the question as per the suggestion. Each item was also evaluated based on the evaluation parameters suggested by Cichetti and Fleiss.[9,10] The values obtained for I-CVI for relevance, simplicity, clarity and ambiguity were tabulated along with the calculated MKS and the evaluation of each item.
RESULTS
Seven of the 10 experts completed the assessment and grading as per the instructions provided and submitted a completed proforma. S-CVI for relevance, simplicity, clarity and ambiguity was 0.72 [Table 1], 0.86 [Table 2], 0.72 [Table 3] and 0.72 [Table 4] respectively. ACPs were calculated as 0.95 [Table 1], 0.97 [Table 2], 0.95 [Table 3] and 0.95 [Table 4] for relevance, simplicity, clarity and ambiguity respectively.
Table 1.
Content validity of relevance
| Question No. | I-CVI | Probability of chance agreement | Modified kappa statistic | Interpretation |
|---|---|---|---|---|
| 1 | 1 | 0.008 | 1.0 | Excellent |
| 2 | 1 | 0.008 | 1.0 | Excellent |
| 3 | 1 | 0.008 | 1.0 | Excellent |
| 4 | 1 | 0.008 | 1.0 | Excellent |
| 5 | 0.85 | 0.055 | 0.8 | Excellent |
| 6 | 1 | 0.008 | 1.0 | Excellent |
| 7 | 1 | 0.008 | 1.0 | Excellent |
| 8 | 1 | 0.008 | 1.0 | Excellent |
| 9 | 1 | 0.008 | 1.0 | Excellent |
| 10 | 1 | 0.008 | 1.0 | Excellent |
| 11 | 0.85 | 0.055 | 0.8 | Excellent |
| 12 | 1 | 0.008 | 1.0 | Excellent |
| 13 | 0.85 | 0.055 | 0.8 | Excellent |
| 14 | 0.85 | 0.055 | 0.8 | Excellent |
| 15 | 1 | 0.008 | 1.0 | Excellent |
| 16 | 1 | 0.008 | 1.0 | Excellent |
| 17 | 0.85 | 0.055 | 0.8 | Excellent |
| 18 | 1 | 0.008 | 1.0 | Excellent |
| 19 | 1 | 0.008 | 1.0 | Excellent |
| 20 | 1 | 0.008 | 1.0 | Excellent |
| 21 | 1 | 0.008 | 1.0 | Excellent |
| 22 | 1 | 0.008 | 1.0 | Excellent |
| 23 | 1 | 0.008 | 1.0 | Excellent |
| 24 | 1 | 0.008 | 1.0 | Excellent |
| 25 | 0.85 | 0.055 | 0.8 | Excellent |
| 26 | 0.71 | 0.164 | 0.7 | Good |
| 27 | 0.85 | 0.055 | 0.8 | Excellent |
| 28 | 1 | 0.008 | 1.0 | Excellent |
| 29 | 0.85 | 0.055 | 0.8 | Excellent |
| 30 | 0.85 | 0.055 | 0.8 | Excellent |
| 31 | 1 | 0.008 | 1.0 | Excellent |
| 32 | 1 | 0.008 | 1.0 | Excellent |
| 33 | 1 | 0.008 | 1.0 | Excellent |
| 34 | 1 | 0.008 | 1.0 | Excellent |
| 35 | 1 | 0.008 | 1.0 | Excellent |
| 36 | 1 | 0.008 | 1.0 | Excellent |
Mean I-CVI - 0.95, S-CVI - 0.72, S-CVI/Average=0.95
Table 2.
Content validity of simplicity
| Question No. | I-CVI | Probability of chance agreement | Modified kappa statistic | Interpretation |
|---|---|---|---|---|
| 1 | 1 | 0.008 | 1.0 | Excellent |
| 2 | 1 | 0.008 | 1.0 | Excellent |
| 3 | 1 | 0.008 | 1.0 | Excellent |
| 4 | 1 | 0.008 | 1.0 | Excellent |
| 5 | 1 | 0.008 | 1.0 | Excellent |
| 6 | 0.85 | 0.055 | 0.8 | Excellent |
| 7 | 1 | 0.008 | 1.0 | Excellent |
| 8 | 1 | 0.008 | 1.0 | Excellent |
| 9 | 1 | 0.008 | 1.0 | Excellent |
| 10 | 1 | 0.008 | 1.0 | Excellent |
| 11 | 1 | 0.008 | 1.0 | Excellent |
| 12 | 1 | 0.008 | 1.0 | Excellent |
| 13 | 1 | 0.008 | 1.0 | Excellent |
| 14 | 1 | 0.008 | 1.0 | Excellent |
| 15 | 1 | 0.008 | 1.0 | Excellent |
| 16 | 1 | 0.008 | 1.0 | Excellent |
| 17 | 1 | 0.008 | 1.0 | Excellent |
| 18 | 1 | 0.008 | 1.0 | Excellent |
| 19 | 1 | 0.008 | 1.0 | Excellent |
| 20 | 1 | 0.008 | 1.0 | Excellent |
| 21 | 1 | 0.008 | 1.0 | Excellent |
| 22 | 1 | 0.008 | 1.0 | Excellent |
| 23 | 0.85 | 0.055 | 0.8 | Excellent |
| 24 | 0.85 | 0.055 | 0.8 | Excellent |
| 25 | 1 | 0.008 | 1.0 | Excellent |
| 26 | 1 | 0.008 | 1.0 | Excellent |
| 27 | 0.85 | 0.055 | 0.8 | Excellent |
| 28 | 1 | 0.008 | 1.0 | Excellent |
| 29 | 1 | 0.008 | 1.0 | Excellent |
| 30 | 0.85 | 0.055 | 0.8 | Excellent |
| 31 | 1 | 0.008 | 1.0 | Excellent |
| 32 | 1 | 0.008 | 1.0 | Excellent |
| 33 | 1 | 0.008 | 1.0 | Excellent |
| 34 | 1 | 0.008 | 1.0 | Excellent |
| 35 | 1 | 0.008 | 1.0 | Excellent |
| 36 | 1 | 0.008 | 1.0 | Excellent |
I-CVI mean=0.9, S-CVI=0.86, S-CVI/Average=0.97
Table 3.
Content validity of clarity
| Question No. | I-CVI | Probability of chance agreement | Modified kappa statistic | Interpretation |
|---|---|---|---|---|
| 1 | 0.85 | 0.055 | 0.8 | Excellent |
| 2 | 0.72 | 0.164 | 0.7 | Good |
| 3 | 1 | 0.008 | 1.0 | Excellent |
| 4 | 1 | 0.008 | 1.0 | Excellent |
| 5 | 1 | 0.008 | 1.0 | Excellent |
| 6 | 1 | 0.008 | 1.0 | Excellent |
| 7 | 1 | 0.008 | 1.0 | Excellent |
| 8 | 1 | 0.008 | 1.0 | Excellent |
| 9 | 0.85 | 0.055 | 0.8 | Excellent |
| 10 | 1 | 0.008 | 1.0 | Excellent |
| 11 | 1 | 0.008 | 1.0 | Excellent |
| 12 | 1 | 0.008 | 1.0 | Excellent |
| 13 | 0.85 | 0.055 | 0.8 | Excellent |
| 14 | 1 | 0.008 | 1.0 | Excellent |
| 15 | 0.85 | 0.055 | 0.8 | Excellent |
| 16 | 1 | 0.008 | 1.0 | Excellent |
| 17 | 1 | 0.008 | 1.0 | Excellent |
| 18 | 1 | 0.008 | 1.0 | Excellent |
| 19 | 1 | 0.008 | 1.0 | Excellent |
| 20 | 1 | 0.008 | 1.0 | Excellent |
| 21 | 1 | 0.008 | 1.0 | Excellent |
| 22 | 1 | 0.008 | 1.0 | Excellent |
| 23 | 0.85 | 0.055 | 0.8 | Excellent |
| 24 | 0.85 | 0.055 | 0.8 | Excellent |
| 25 | 1 | 0.008 | 1.0 | Excellent |
| 26 | 1 | 0.008 | 1.0 | Excellent |
| 27 | 0.85 | 0.055 | 0.8 | Excellent |
| 28 | 1 | 0.008 | 1.0 | Excellent |
| 29 | 1 | 0.008 | 1.0 | Excellent |
| 30 | 0.85 | 0.055 | 0.8 | Excellent |
| 31 | 1 | 0.008 | 1.0 | Excellent |
| 32 | 0.85 | 0.055 | 0.8 | Excellent |
| 33 | 1 | 0.008 | 1.0 | Excellent |
| 34 | 1 | 0.008 | 1.0 | Excellent |
| 35 | 1 | 0.008 | 1.0 | Excellent |
| 36 | 1 | 0.008 | 1.0 | Excellent |
Mean I-CVI=0.95, S-CVI=0.72, S-CVI/Average=0.95
Table 4.
Content validity of ambiguity
| Question No. | I-CVI | Probability of chance agreement | Modified kappa statistic | Interpretation |
|---|---|---|---|---|
| 1 | 1.00 | 0.008 | 1.0 | Excellent |
| 2 | 1.00 | 0.008 | 1.0 | Excellent |
| 3 | 1.00 | 0.008 | 1.0 | Excellent |
| 4 | 1.00 | 0.008 | 1.0 | Excellent |
| 5 | 0.85 | 0.055 | 0.8 | Excellent |
| 6 | 1.00 | 0.008 | 1.0 | Excellent |
| 7 | 1.00 | 0.008 | 1.0 | Excellent |
| 8 | 1.00 | 0.008 | 1.0 | Excellent |
| 9 | 1.00 | 0.008 | 1.0 | Excellent |
| 10 | 1.00 | 0.008 | 1.0 | Excellent |
| 11 | 0.85 | 0.055 | 0.8 | Excellent |
| 12 | 1.00 | 0.008 | 1.0 | Excellent |
| 13 | 0.85 | 0.055 | 0.8 | Excellent |
| 14 | 0.85 | 0.055 | 0.8 | Excellent |
| 15 | 1.00 | 0.008 | 1.0 | Excellent |
| 16 | 1.00 | 0.008 | 1.0 | Excellent |
| 17 | 0.85 | 0.055 | 0.8 | Excellent |
| 18 | 1.00 | 0.008 | 1.0 | Excellent |
| 19 | 1.00 | 0.008 | 1.0 | Excellent |
| 20 | 1.00 | 0.008 | 1.0 | Excellent |
| 21 | 1.00 | 0.008 | 1.0 | Excellent |
| 22 | 1.00 | 0.008 | 1.0 | Excellent |
| 23 | 0.71 | 0.164 | 0.7 | Good |
| 24 | 1.00 | 0.008 | 1.0 | Excellent |
| 25 | 0.85 | 0.055 | 0.8 | Excellent |
| 26 | 1.00 | 0.008 | 1.0 | Excellent |
| 27 | 0.85 | 0.055 | 0.8 | Excellent |
| 28 | 1.00 | 0.008 | 1.0 | Excellent |
| 29 | 0.85 | 0.055 | 0.8 | Excellent |
| 30 | 0.85 | 0.055 | 0.8 | Excellent |
| 31 | 1.00 | 0.008 | 1.0 | Excellent |
| 32 | 1.00 | 0.008 | 1.0 | Excellent |
| 33 | 1.00 | 0.008 | 1.0 | Excellent |
| 34 | 1.00 | 0.008 | 1.0 | Excellent |
| 35 | 1.00 | 0.008 | 1.0 | Excellent |
| 36 | 1.00 | 0.008 | 1.0 | Excellent |
Mean I-CVI=0.95, S-CVI=0.72, S-CVI/Average=0.95
In terms of relevance [Table 1], 26 of the 36 questions were graded as 'relevant but need minor revision'or'very relevant' by all the experts (I-CVI-1, K-1). Nine questions were thought to be 'relevant but need minor revision' or 'very relevant' by six of the seven experts and one question was graded as 'relevant but need minor revision' or 'very relevant' by five experts out of seven (I-CVI 0.71, K 0.7).
Thirty-five questions received a grading of 'simple but need minor revision' or 'very simple' by all the seven experts (I-CVI = 1; K = 1), and five questions received a grading of 'simple but need minor revision' or 'very simple' by six of the seven experts (I-CVI = 0.85, K = 0.8) [Table 2].
Twenty-six of the 36 questions were graded as 'clear but need minor revision' or 'very clear' by the seven experts (I-CVI = 1, K = 1). Six of the seven experts graded nine questions as 'clear but need minor revision' or 'very clear' (1-CVI = 0.85, K = 0.8) and five of the seven experts graded one question as 'clear but need minor revision' or 'very clear' (I-CVI = 0.71, K = 0.7) [Table 3].
Twenty-six of the 36 questions were graded as 'no doubt but need minor revision' or 'meaning is clear' by all the seven experts (I-CVI = 1, K = 1). Six of the seven experts graded eight questions as 'no doubt but need minor revision' or 'meaning is clear' for nine questions (I-CVI = 0.85, K = 0.8), and six of the seven experts graded one question 'no doubt but need minor revision' or 'meaning is clear' (I-CVI = 0.71, K = 0.7) [Table 4]. Experts who graded questions as 1, 2 and 3 did give suggestions on how to revise the questions. Question 2 received an I-CVI of 0.71 in terms of clarity; the answers were modified as per the instructions of the experts to convey better clarity on the method of answer entry. The experts had advised to mention common kinds of food consumed specific to regions with examples. The examples on how to answer the question were included in the question in brackets. The experts had also suggested to add the term large/heavy meal instead of the term heavy meal. This was also complied with [Appendix 3 is available online].
Question 23 too received an I-CVI of 0.71 in terms of ambiguity and the experts had suggested that data needed to be collected for both elective and emergency surgeries. The questionnaire was initially modified to include both elective and emergency surgeries as shown in Appendix 3 is available online.
DISCUSSION
Content validity of an instrument is defined as the extent to which an instrument adequately samples the research domain of interest when attempting to measure aphenomena. It can be measured in two main steps: (a) identifying the domain through literature search and (b) developing the instrument items identified with domain of content which involves the quantification of content validity.[11] There are various methods of estimating the content validity of an instrument. They are mainly consistency estimates, consensus estimates and measurement estimates.[3,6] While estimating content validity researchers are usually guided by ease of computation, ease of understanding and communication, adjustment for chance agreement and focus on consensus agreement rather than consistency.
We chose content validity index and MKS as suggested by Polit et al.[3,6] in estimating the content validity of our scale. We used the criteria provided by Yaghmale[7] in measuring content validity. It included a 4-point scale in assessing four parameters for each question designed [Appendix 2 is available online].
According to Lynn,[12] an I-CVI of 0.78 and an S-CVI/Average of 0.90 are acceptable when more than six experts have graded the tool. Wynd et al.[11] quote theevaluation of magnitude of kappa coefficients by parameters given by Landis and Koch,[13] Cichetti,[10] and Fleiss.[11] We in our estimation used the parameters given by Cichetti and Fleiss as they had provided for four grades in comparison to those provided by Landis and Koch. They grade the kappastatistic as <0.40 = poor, 0.40–0.59 = fair, 0.60–0.74 = good and 0.75–1.00 = excellent.
In our estimation, of the 36 questions, 34 questions were quantitatively valid. One question had an I-CVI of 0.71 for ambiguity and a kappa statistic of 0.7 (good). One question had an I-CVI of 0.71 for clarity and a kappa statistic of 0.7. We considered that any I-CVI of >0.78 as acceptable and any item with an I-CVI <0.78 meant the item needed to be eliminated or rectified.
Considering these criteria, we accepted the suggestionsof the experts related to twoquestions (2 and 23) after assessing the suggestions and coming to a consensus among the experts. In question 2, the answers were modified to convey better clarity. The experts had advised to mention common kinds of food, which was duly attended to. Question 23was also modified as per the suggestions provided by the experts as mentioned above. A consultation was sought with the biostatistician regarding restructuring the questions without modifying the content to ease the analysis. As per those suggestions, the questionnaire was further modified. The final questionnaire constituted 40 questions. Question numbers 23 and 26 were split into two questions each to collect the data for emergency and elective cases separately, and questions which elicited the data on therapy and were related to questions 23 and 26were again duplicated to collect data specifically for emergency and elective cases. This resulted in the increase in the number of questions from 36 to 40.
CONCLUSION
We conclude that our questionnaire designed to ascertain the preoperative fasting practices met the content validity criteria both by qualitative and quantitative analyses. The two questions which did not meet the criteria were modified as per the suggestions given by the experts.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
APPENDIX 1- QUESTIONNAIRE FOR THE SURVEY
‘A National Survey of Perioperative Fasting Practices in India’
-
Please provide the following details
- Name of the Institution:
- State:
-
In your geographic area/hospital (common ones, can be more than one)
- Name food items are considered as Heavy Meal?:
- Name food items are considered as Light Meal?:
- Name liquids are considered as Clear liquids?:
-
Is your hospital a ________ (can select more than one)
- Multispeciality Hospital
- Single Speciality Hospital
- Government Institution
- Private Institution
- Teaching Institution
- Non Teaching Institution
-
Types of surgical population frequent in your institution
- Adult
- Paediatric
- Geriatric
- Pregnant
-
What are the common techniques of anaesthesia performed in the Institution? (Multiple Choices allowed)
- General Anaesthesia
- Regional Anaesthesia
- Local Anaesthesia
- Procedural Sedation
- Monitored Anaesthesia Care
-
What surgical specialities the institution caters to? (can select more than one)
- General Surgery
- Orthopaedics
- Ophthalmology
- Otorhinolaryngology
- Neurosurgery
- Surgical Gastroenterology/Oncology
- Plastic Surgery/Dental
- Obstetrics and Gynaecology
- Paediatric
- Bariatric
- Others (specify)
-
Approximate estimate of the total number of cases performed every month (give numbers)
- Elective
- Emergency
-
How many elective cases (percent of total elective) receive ‘NBM from MIDNIGHT’ (solids onwards) orders overall?
- <25
- 25-50
- 50-75
- >75
- 100
-
How many elective cases (percent of total) overall receive NBM instructions as per ASA guidelines (solids onwards)?
- <25
- 25-50
- 50-75
- >75
- 100
-
What percentage of elective fasting patients receives intravenous hydration during fasting period?
- <25
- 25-50
- 50-75
- >75
- 100
-
What is NBM duration advised as per Institutional/Centre’s NBM protocol? (each item open, Please enter in the format described For e.g., 8,6,4,2 etc)
- Paediatric: Solids-Breast milk- Liquids- Clear Fluids (Enter in given box as _,_,_,_ in Hours)
- Adult: Solids- Liquids-Clear Fluids (Enter in given box as _,_,_,_ in Hours)
- Geriatric: Solids- Liquids-Clear Fluids (Enter in given box as _,_,_,_ in Hours)
- Obese: Solids- Liquids-Clear Fluids/(Enter in given box as _,_,_,_ in Hours)
- Diabetic: Solids- Liquids-Clear Fluids (Enter in given box as _,_,_,_ in Hours)
- Gestational DM: Solids- Liquids-Clear Fluids (Enter in given box as _,_,_,_ in Hours)
- Renal failure: Solids- Liquids-Clear Fluids (Enter in given box as _,_,_,_ in Hours)
- Term Pregnancy: Solids- Liquids-Clear Fluids (Enter in given box as _,_,_,_ in Hours)
-
Are you are actively promoting preoperative clear fluids intake?
- No
- Yes, Plain Water advised
- Yes, sugar/glucose water advised
- Yes, Coconut Water/Electrolyte/ORS advised
- Yes, Maltodextrin advised
- Yes, Clear Tea advised
- Yes, Black Coffee advised
- Yes, Fruit Juice without pulp advised
-
Do you have the services of a dietician in your hospital?
- Yes
- No
-
Do you advice the type of diet during preoperative period as per fasting protocol?
- Yes
- No
-
Is the same NBM protocol used for patients receiving GA/RA, also used for Sedation/MAC procedures?
- Yes
- No
-
Is it a practice to estimate the gastric volume routinely preoperatively?
- Yes:
- Only in at risk cases:
- No:
-
If yes to Q. No. 16, What method do you use?
- Ultrasound
- Aspiration with Ryle’s tube and estimation.
- Other (please specify)
-
Have you encountered any of the below when prolonged fasting (>6 hrs) was advocated in any of the patient groups?
- Hypoglycaemia
- Ketosis
- Hypotension on induction
- Other (please specify)
-
If fasting protocols are not adhered to (lesser duration of fasting than advocated by ASA protocols or institutional protocols), FOR SOLIDS, what will be your response?
- Taken up at a later time of the day
- The case is postponed to another day
- Taken up with aspiration risk consent
- Taken up with RSI
- Insert a Ryle’s tube, aspirate the contents and continue
- Assess the gastric content with endoscope and decide
- Assess the gastric contents with ultrasound and decide
- Proceed if case to be done under regional anesthesia
- Advice drugs which increase the gastric motility and take up the case
- Others (please specify)
-
If fasting protocols are not adhered to (lesser duration of fasting than advocated by ASA protocols or institutional protocols) FOR CLEAR LIQUIDS what will be your response
- Taken up at a later time of the day
- The case is postponed to another day
- Taken up with aspiration risk consent
- Taken up with RSI
- Insert a Ryle’s tube, aspirate the contents and continue
- Assess the gastric content with endoscope and decide
- Assess the gastric contents with ultrasound and decide
- Proceed if case to be done under regional anesthesia
- Advice drugs which increase the gastric motility and take up the case
- Others (please specify)
-
Anti aspiration prophylaxis is followed in your institution/centre for
- All cases
- At risk cases only
-
What anti aspiration prophylaxis measures are administered?
- H2 receptor antagonist (Ranitidine)
- Prokinetics (metoclopramide)
- Proton Pump Inhibitor (pantaprazole and similar)
- Ryle’s tube and aspiration
- 0. 3 M chilled sodium citrate
- 5. HT3 receptor antagonist (Ondansetron and similar)
- Others (please specify)
-
Have you encountered cases of regurgitation/aspiration/pneumonitis in your hospital in the past 10 years, overall? (can select more than one WITH NUMBERS)
- Yes, regurgitationatIntubation: _ (nos)
- Yes, regurgitation/aspiration at Intubation: _(nos)
- Yes, regurgitation/aspiration/pneumonitisat/after Intubation: _(nos)
- Yes, regurgitationatExtubation: _(nos)
- Yes, regurgitation/aspiration atExtubation: _(nos)
- Yes, regurgitation/aspiration/pneumonitisat/after Extubation: _(nos)
- None
-
In continuation of Q.23, what was the outcome? (mention as number of cases for each section, if applicable)
- Required oxygen supplementation and Survived: _
- Required non invasive ventilation and Survived: _
- Required mechanical ventilation and Survived: _
- Death after mechanical ventilation: _
-
How many Diabetic patients, overall, are provided anaesthesia services every month? (Enter numbers)
- Elective Surgeries -
- Emergency Surgeries -
-
How many cases of regurgitation/aspiration/pneumonitis have been encountered in Diabetic Patients in the past 10 years?
- Elective surgeries (regurgitation):_ (nos)
- Elective surgeries
- (regurgitation -aspiration):_ (nos)
- Elective surgeries
- (regurgitation -aspiration -pneumonitislater):_ (nos)
- Emergency Surgeries
- (regurgitation):_ (nos)
- Emergency Surgeries
- (regurgitation -aspiration):_ (nos)
- Emergency Surgeries
- (regurgitation -aspiration -pneumonitis later):_ (nos)
- Nil
-
In continuation of Q.26, what was the outcome? (mention as number of cases for each section, if applicable)
- Required oxygen supplementation and Survived: _
- Required non invasive ventilation and Survived: _
- Required mechanical ventilation and Survived: _
- Death after mechanical ventilation: _
-
How many pregnant diabetics received anaesthesia every month? (Enter Numbers)
- Elective Surgeries -
- Emergency Surgeries -
-
How many cases of regurgitation/aspiration have been encountered in Diabetic pregnant mothers in the past 10 years?
- Elective surgeries (regurgitation):_ (nos)
- Elective surgeries (regurgitation -aspiration):_ (nos)
- Elective surgeries (regurgitation -aspiration -pneumonitislater):_ (nos)
- Emergency Surgeries (regurgitation):_ (nos)
- Emergency Surgeries (regurgitation -aspiration):_ (nos)
- Emergency Surgeries (regurgitation -aspiration -pneumonitis later):_ (nos)
- Nil
-
In continuation of Q.29, what was the outcome? (mention as number of cases for each section, if applicable)
- Required oxygen supplementation and Survived: _
- Required non invasive ventilation and Survived: _
- Required mechanical ventilation and Survived: _
- Death after mechanical ventilation: _
-
Whose role is to advice nil by mouth protocol?
- Surgeon:
- Ward nurse:
- Anaesthesiologist:
- Combination of these:
-
NBM instructions for elective cases are started as per (provide percentage of patients)
- ASA protocol:
- NBM from midnight:
- Other:
-
How do you advice? (can select more than one)
- Orally, during PAC/PAE
- Written in Pre anaesthetic instructions
- Written in Patient information sheet
- Written in the patient consent form
-
Whose role is to advice return to Oral intake postoperatively?
- Surgeon:
- Ward nurse:
- Anaesthesiologist:
- Combination of these:
-
When do you allow the patient to resume feeds postoperatively, in ROUTINE* cases? (Enter numbers in hours) (*Without medical or surgical contraindications for early oral intake)
- Clear Liquids: _hrs
- Solids: _hrs
-
Please enter the average number of surgeries/procedures performed per month
- Paediatric
- Obstetric
- Day Care
- Bariatric
APPENDIX 2
Please grade each question as per the below given criteria in the tables given. Relevance
1 = not relevant
2 = item needs some revision
3 = relevant but needs minor revision
4 = very relevant
Clarity
1 = not clear
2 = item needs some revision
3 = clear but needs minor revision
4 = very clear
Simplicity
1 = not simple
2 = item needs some revision
3 = simple but needs minor revision
4 = very simple
Ambiguity
1 = doubtful
2 = needs revision
3 = no doubt but needs minor revision
4 = meaning is clear
*(If the grading for the particular question is 2 or 3, please provide the suggestion on how to change the question or choices)
APPENDIX 3
A National Survey of Perioperative Fasting Practices in India
* 1. Please provide the following details
Name of the Institution: 
State: 
How old is your Institution? 
* 2. In your geographic area/ hospital, mention the food items you consider as (Enter common ones, can be more than one. For Eg. Chapathi 2, Jowar Roti 5, Rava Idli 3, Regular idli 2 etc.)
Light Meal (Mention food item and number below which it is considered as light meal) 
Heavy Meal (List items not mentioned as Light meal) 
Clear liquids 
* 3. Is your hospital a ________ (can select more than one)
◻ Multispeciality Hospital
◻ Single Speciality Hospital
◻ Government Institution
◻ Private Institution
◻ Teaching Institution
◻ Non Teaching Institution
* 4. Types of surgical population frequent in your institution (Can select more than one)
◻ Adult
◻ Paediatric
◻ Geriatric
◻ Pregnant
◻ Other (please specify)

* 5. What are the common techniques of anaesthesia performed in the Institution? (Can select more than one)
◻ General Anaesthesia (GA)
◻ Regional Anaesthesia (RA)
◻ Local Anaesthesia (LA)
◻ Procedural Sedation
◻ Monitored Anaesthesia Care (MAC)
* 6. What surgical specialities the institution caters to? (can select more than one)
◻ General Surgery
◻ Orthopaedics
◻ Ophthalmology
◻ Otorhinolaryngology
◻ Neurosurgery
◻ Surgical Gastroenterology/Oncology
◻ Plastic Surgery/Dental
◻ Obstetrics & Gynaecology
◻ Paediatric
◻ Bariatric
◻ Other (please specify)

* 7. Approximate estimate of the total number of cases performed every month (give numbers)
Elective 
Emergency 
* 8. How many elective cases (percent of total elective) receive ‘Nil By Mouth (NBM) or Nil Per Oral (NPO) from MIDNIGHT’ (solids onwards) orders overall?
◯ < 25
◯ 25-50
◯ 50-75
◯ > 75
◯ 100
* 9. How many elective cases (percent of total) receive NBM/NPO instructions as per American Society of Anaesthesiologists(ASA) guidelines (solids onwards)?
◯ < 25
◯ 25-50
◯ 50-75
◯ > 75
◯ 100
* 10. What percentage of elective fasting patients receives intravenous hydration during fasting period?
◯ < 25
◯ 25-50
◯ 50-75
◯ > 75
◯ 100
* 11. What is NBM/NPO duration advised as per Institutional/ Centre’s protocol?(each item open, Please enter as number of hours from 0-24, 0 if allowed until shifting the patient inside the theatre)
Paediatric: Solids 
Paediatric - Breast Milk 
Paediatric-Liquids 
Paediatric- Clear liquids 
Adult- Solids 
Adult- Liquids 
Adult- Clear Liquids 
Geriatric: Solids 
Geriatric- Liquids 
Geriatric- Clear liquids 
Obese- Solids 
Obese-Liquids 
Obese-Clear liquids 
Diabetic- Solids 
Diabetic-Liquids 
Diabetic- Clear Liquids 
Gestational DM- Solids 
Gestational DM-Liquids 
Gestational DM-Clear liquids 
Renal failure- Solids 
Renal failure-Liquids 
Renal Failure- Clear liquids 
Term Pregnancy-Solids 
Term Pregnancy- Liquids 
Term Pregnancy- Clear Liquids 
* 12. Are you actively promoting preoperative clear fluids intake?
◯ No
◯ Yes, Plain Water advised
◯ Yes, sugar/glucose water advised
◯ Yes, Coconut Water /Electrolyte / Oral Rehydration Solution advised
◯ Yes, Maltodextrin advised
◯ Yes, Clear Tea advised
◯ Yes, Black Coffee advised
◯ Yes, Fruit Juice without pulp advised
* 13. Do you have the services of a dietician in your hospital?
◯ Yes
◯ No
* 14. Do you advice the type of diet during preoperative period as per fasting protocol?
◯ Yes
◯ No
* 15. Is the same NBM/NPO protocol used for patients receiving GA/RA, also used for Sedation/ MAC procedures?
◯ Yes
◯ No
* 16. Is it a practice to estimate the gastric volume routinely preoperatively?
◯ Yes
◯ Only in at risk cases
◯ No
17. What method of gastric volume estimation do you use?
◯ Ultrasound
◯ Aspiration with Ryle’s tube and estimation.
◯ Other (please specify)

* 18. Have you encountered any of the below when prolonged fasting (> 6 hrs) was advocated in any of the patient groups?
◻ Hypoglycaemia
◻ Ketosis
◻ Hypotension on induction
◻ Other (please specify)

* 19. If fasting protocols are not adhered to (lesser duration of fasting than advocated by ASA protocols or institutional protocols), FOR SOLIDS, what will be your response?
◯ Taken up at a later time of the day
◯ The case is postponed to another day
◯ Taken up with aspiration risk consent
◯ Taken up with Rapid Sequence Induction (RSI)
◯ Insert a Ryle’s tube, aspirate the contents and continue
◯ Assess the gastric content with endoscope & decide
◯ Assess the gastric contents with ultrasound & decide
◯ Proceed if case to be done under regional anesthesia
◯ Advice drugs which increase the gastric motility and take up the case
◯ Other (please specify)

* 20. If NBM/NPO protocols are not adhered to (lesser duration of fasting than advocated by ASA protocols or institutional protocols), FOR NONCLEAR LIQUIDS, what will be your response?
◯ Taken up at a later time of the day
◯ The case is postponed to another day
◯ Taken up with aspiration risk consent
◯ Taken up with Rapid Sequence Induction (RSI)
◯ Insert a Ryle’s tube, aspirate the contents and continue
◯ Assess the gastric content with endoscope & decide
◯ Assess the gastric contents with ultrasound & decide
◯ Proceed if case to be done under regional anesthesia
◯ Advice drugs which increase the gastric motility and take up the case
◯ Other (please specify)

* 21. If fasting protocols are not adhered to (lesser duration of fasting than advocated by ASA protocols or institutional protocols) FOR CLEAR LIQUIDS what will be your response
◯ Taken up at a later time of the day
◯ The case is postponed to another day
◯ Taken up with aspiration risk consent
◯ Taken up with RSI
◯ Insert a Ryle’s tube, aspirate the contents and continue
◯ Assess the gastric content with endoscope & decide
◯ Assess the gastric contents with ultrasound & decide
◯ Proceed if case to be done under regional anesthesia
◯ Advice drugs which increase the gastric motility and take up the case
◯ Other (please specify)

* 22. Anti aspiration prophylaxis is followed in your institution / centre for
◯ All cases
◯ At risk cases only (like pregnant patient, emergency surgery etc)
◯ Only for emergency surgeries
◯ Not followed at all
* 23. What anti aspiration prophylaxis measures are administered?
◻ H2 receptor antagonist (Ranitidine)
◻ Prokinetics (metoclopramide)
◻ Proton Pump Inhibitor (pantaprazole and similar)
◻ Ryle’s tube and aspiration
◻ 0.3 M chilled sodium citrate
◻ 5 HT3 receptor antagonist (Ondansetron and similar)
◻ Other (please specify)

* 24. Have you encountered cases of regurgitation / aspiration / pneumonitis in your hospital in the past 20 years in ELECTIVE surgeries? (PLEASE Mention numbers, if not applicable mention 0)
Yes, regurgitation at Intubation : _ (nos) 
Yes, regurgitation and aspiration at Intubation : _(nos) 
Yes, regurgitation / aspiration leading to pneumonitis at/after Intubation : _(nos) 
Yes, regurgitation at Extubation : _(nos) 
Yes, regurgitation and aspiration at Extubation : _(nos) 
Yes, regurgitation / aspiration leading to pneumonitis at/after Extubation : _(nos) 
* 25. In continuation of Q.24, what was the outcome in elective? (mention as number of cases for each section, if not applicable enter 0)
Required oxygen supplementation & Survived:_ 
Required non invasive ventilation & Survived:_ 
Required mechanical ventilation & Survived:_ 
Death after mechanical ventilation:_ 
* 26. Have you encountered cases of regurgitation / aspiration / pneumonitis in your hospital in the past 20 years in EMERGENCY surgeries? (Please mention as numbers in all boxes, if not applicable mention 0)
Yes, regurgitation at Intubation : _ (nos) 
Yes, regurgitation & aspiration at Intubation : _(nos) 
Yes, regurgitation / aspiration leading to pneumonitis at/after Intubation : _(nos) 
Yes, regurgitation at Extubation : _(nos) 
Yes, regurgitation and aspiration at Extubation : _(nos) 
Yes, regurgitation / aspiration leading to pneumonitis at/after Extubation : _(nos) 
* 27. In continuation of Q.26, what was the outcome in emergency surgeries? (mention as number of cases for each section, if not applicable enter 0 in the box)
Required oxygen supplementation & Survived:_ 
Required non invasive ventilation & Survived:_ 
Required mechanical ventilation & Survived:_ 
Death after mechanical ventilation:_ 
* 28. Whose role is to advice nil * by mouth protocol?
◯ Surgeon:
◯ Ward nurse:
◯ Anaesthesiologist:
◯ Combination of these:
* 29. How do you advice? (can select more than one)
◻ Orally, during Pre Anaesthetic Checkup/Preanaesthetic Evaluation
◻ Written in Pre anaesthetic instructions
◻ Written in Patient information sheet
◻ Written in the patient consent form
* 30. Whose role is to advice return to Oral intake * postoperatively?
◯ Surgeon:
◯ Ward nurse:
◯ Anaesthesiologist:
◯ Combination of these:
* 31. When do you allow the patient to resume feeds postoperatively, in ROUTINE* cases? (Enter numbers in hours) (*Without medical or surgical contraindications for early oral intake)
Clear Liquids:_ hrs 
Solids:_ hrs 
* 32. How many Diabetic patients, overall, are provided anaesthesia services every month? (Enter numbers)
Elective Surgeries - 
Emergency Surgeries - 
* 33. How many cases of regurgitation / aspiration / pneumonitis have been encountered in Diabetic Patients in the past 20 years? (Please enter numbers, where not applicable enter 0)
Elective surgeries (regurgitation):_ (nos) 
Elective surgeries (regurgitation and aspiration) :_ (nos) 
Elective surgeries (regurgitation -aspiration leading to pneumonitis later) :_ (nos) 
Emergency Surgeries (regurgitation):_ (nos) 
Emergency Surgeries (regurgitation and aspiration) :_ (nos) 
Emergency Surgeries (regurgitation -aspiration leading to pneumonitis later) :_ (nos) 
* 34. In continuation of Q.33, what was the outcome in diabetics coming fo relective surgeries? (mention as number of cases for each section, if not applicable enter 0 in the box)
Required oxygen supplementation & Survived:_ 
Required non invasive ventilation & Survived:_ 
Required mechanical ventilation & Survived:_ 
Death after mechanical ventilation:_ 
* 35. In continuation of Q.33, what was the outcome in diabetics coming for EMERGENCY surgeries? (mention as number of cases for each section, if applicable otherwise enter 0 in each box)
Required oxygen supplementation & Survived:_ 
Required non invasive ventilation & Survived:_ 
Required mechanical ventilation & Survived:_ 
Death after mechanical ventilation:_ 
* 36. How many pregnant diabetics received anaesthesia every month? (Enter Numbers)
Elective Surgeries - 
Emergency Surgeries - 
* 37. How many cases of regurgitation / aspiration have been encountered in Diabetic pregnant women in the past 20 years? (Please enter numbers, if not applicable enter 0)
Elective surgeries (regurgitation):_ (nos) 
Elective surgeries (regurgitation and aspiration) :_ (nos) 
Elective surgeries (regurgitation -aspiration leading to pneumonitis later) :_ (nos) 
Emergency Surgeries (regurgitation):_ (nos) 
Emergency Surgeries (regurgitation and aspiration) :_ (nos) 
Emergency Surgeries (regurgitation -aspiration leading to pneumonitis later) :_ (nos) 
* 38. In continuation of Q.37, what was the outcome in diabetic pregnant women coming fo relective surgeries? (mention as number of cases for each section, if not applicable enter 0 in the box )
Required oxygen supplementation & Survived:_ 
Required non invasive ventilation & Survived:_ 
Required mechanical ventilation & Survived:_ 
Death after mechanical ventilation:_ 
* 39. In continuation of Q.37, what was the outcome in diabetic pregnant women coming for emergency surgeries? (mention as number of cases for each section, if not applicable enter 0 in the box )
Required oxygen supplementation & Survived:_ 
Required non invasive ventilation & Survived:_ 
Required mechanical ventilation & Survived:_ 
Death after mechanical ventilation:_ 
* 40. Please enter the average number of surgeries / procedures performed per month(Please enter numbers)
Paediatric 
Obstetric 
Day Care 
Bariatric 
REFERENCES
- 1.American Society of Anesthesiologists Committee. Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: Application to healthy patients undergoing elective procedures: An updated report by the American Society of Anesthesiologists Committee on Standards and Practice Parameters. Anesthesiology. 2011;114:495–511. doi: 10.1097/ALN.0b013e3181fcbfd9. [DOI] [PubMed] [Google Scholar]
- 2.Smith I, Kranke P, Murat I, Smith A, O'Sullivan G, Søreide E, et al. , Perioperative fasting in adults and children: guidelines from the European Society of Anaesthesiology. Eur J Anaesthesiol. 2011;28:556–69. doi: 10.1097/EJA.0b013e3283495ba1. [DOI] [PubMed] [Google Scholar]
- 3.Polit DF, Beck CT. The Content Validity Index: Are You Sure You Know What's Being Reported? Critique and Recommendations. Res Nurs Health. 2006;29:489–97. doi: 10.1002/nur.20147. [DOI] [PubMed] [Google Scholar]
- 4.Peacock JL, Peacock PJ. Oxford Handbook of Medical Statistics. NewYork: Oxford Universityy Press; 2011. p. 92. [Google Scholar]
- 5.Larsson H, Tegern M, Monnier A, Skoglund J, Helander J, Persson E, et al. Content validity index and intra- and inter-rater reliability of a new muscle/endurance test battery for Swedish soliders. PLoS One. 2015;10:e0132185. doi: 10.1371/journal.pone.0132185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Polit DF, Beck CT, Owen SV. Is the CVI an acceptable indicator of content validity? Appraisal and recommendations. Res Nurs Health. 2005;30:459–67. doi: 10.1002/nur.20199. [DOI] [PubMed] [Google Scholar]
- 7.Yaghmale F. Content Validity and its estimation. Journal of Medical Education Spring. 2003;3:25–27. [Google Scholar]
- 8.Emmanuel A, Clow SE. A questionnaire for assessing breastfeeding intentions and practices in Nigeria: Validity, reliability and translation. BMC Pregnancy Childbirth. 2017;17:174. doi: 10.1186/s12884-017-1366-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cichetti DV. On a model for assessing the security of infantile attachment: Issues of observer reliability and validity. BehavBrain Sci. 1984;7:149–50. [Google Scholar]
- 10.Fleiss J. Measuring nominal sale agreement among many raters. Psycholo Bull. 1971;76:378–82. [Google Scholar]
- 11.Wynd CA, Schmidt B, Schaefer MA. Two Quantitative approaches of measuring content validity. West J Nurs Res. 2003;25:508–18. doi: 10.1177/0193945903252998. [DOI] [PubMed] [Google Scholar]
- 12.Lynn MR. Determination and quantification of content validity. Nurs Res. 1986;33:382–5. [PubMed] [Google Scholar]
- 13.Landis J, Koch JJ. The measurement of observer agreement for categorical data. Biometrics. 1977;33:1159–74. [PubMed] [Google Scholar]