Abstract
Objectives
To undertake a systematic review of the evidence base for the effectiveness of surgical fixation of lateral compression (LC-1) fragility fractures of the pelvis compared with non-surgical approaches.
Searches
MEDLINE, EMBASE, the Cochrane Central Register of Controlled Trials and two international trials registers were searched up to January 2017 (MEDLINE to February 2019) for studies of internal or external fixation of fragility fractures of the pelvis.
Participants
Patients with lateral compression pelvic fractures, sustained as the result of a low-energy mechanism, defined as a fall from standing height or less.
Interventions
Surgery using either external or internal fixation devices. Conservative non-surgical treatment was the defined comparator.
Outcome measures
Outcomes of interest were patient mobility and function, pain, quality of life, fracture union, mortality, hospital length of stay and complications (additional operative procedures, number and type of adverse events and serious adverse events).
Quality assessment and synthesis
The Joanna Briggs Institute Checklist for Case Series was used to assess the included studies. Results were presented in a narrative synthesis.
Results
Of 3421 records identified, four retrospective case series met the inclusion criteria. Fixation types were not consistent between studies or within studies and most patients had more than one type of pelvic fixation. Where reported, mobility and function improved post-surgery, and a reduction in pain was recorded. Length of hospital stay ranged from 4 days to 54 days for surgical fixation of any type. Reported complications and adverse outcomes included: infections, implant loosening, pneumonia and thrombosis. Use of analgesia was not reported.
Conclusions
There is insufficient evidence to support guidance on the most effective treatment for patients who fail to mobilise after sustaining an LC-1 fragility fracture.
Trial registration number
CRD42017055872.
Keywords: surgery, internal fixation, external fixation, fragility fracture, pelvis, systematic review
Strengths and limitations of this study.
This review systematically examines the available evidence, searching multiple databases, assessing the risk of bias in included studies and using methods to reduce error and bias in study selection, data extraction and assessment of risk of bias.
This is a rapidly evolving area for surgery, with ever increasing incidence, so the searches of electronic databases were supplemented by searches for ongoing trials.
Key health databases were searched and efforts were made to find unpublished studies via trial registers, however we did not have the resources to search more widely and retrieval was restricted to studies published in English.
The review found many narratives on surgery for fragility fractures of the pelvis, but no randomised controlled trials, and only four retrospective case series that met all the inclusion criteria.
Introduction
Fragility fractures of the pelvis (FFP) can result in significant long-term disability,1 have a significant impact on patients and put a strain on healthcare provision. A common fragility fracture pattern in older adults is the lateral compression type-1 (LC-1) pelvic fracture. This typically results from a low-energy fall from standing height and increases in likelihood with age.2–4 LC-1 fractures are projected to have the largest incidence increase (by 56% over 20 years) of all osteoporotic fractures and the associated treatment costs are predicted to rise by 60% between 2005 and 2025.5 6
The effects of LC-1 fractures can be devastating for patients. The pain and associated immobility leads to secondary complications, including respiratory and urinary tract infections, pressure sores and venous thromboembolic events.7 8
Many patients with LC-1 fractures report that they do not return to their pre-injury function and they have reduced independence with activities of daily living.2 4 This can result in the need for intermediate care or residential facilities in addition to anxiety, emotional stress and reduced confidence.9 10 Mortality for FFP at 1 year is 27%,11 which is comparable to hip fractures at 33%.12 Furthermore, hospital stay for FFP has been shown to be similar to hip fractures in the elderly.9 13 The standard treatment for hip fractures (so-called fractured neck of femur) is rapid surgical fixation or joint replacement, within 36 hours of injury, aimed at early weight-bearing and minimising immobility-related complications.14 Paradoxically, despite the similarities in patient cohorts and their vulnerability to pain-induced immobility, the standard of care for elderly LC-1 fragility fractures of the pelvis (LC-1 FFP) is non-operative treatment and to ‘mobilise as pain allows’.15–17 Many patients with stable fractures are able to mobilise within a few days of injury, typically with a walking aid. However, patients with unstable fractures (those that are unable to withstand physiological loads without displacement18) typically have disabling pain with almost all movements, even moving around the bed. This unstable group are at greater risk of the immobility-related complications discussed above.9 11–13 15
There are various classifications of pelvic ring fractures based on the mechanism of injury, ligamentous involvement and anatomical location. For the purpose of this review, LC-1 FFPs were defined by respective anatomical classifications in patients with a low-energy mechanism.
Young and Burgess: an oblique or transverse ramus fracture with or without ipsilateral anterior sacral alar compression fracture (LC-1).19 20
Tile classification: rotationally unstable, vertically stable. Ipsilateral, the rami commonly fractured anteriorly and the posterior complex is crushed (Tile B2).21
AO classification: unilateral, partial disruption of posterior arch, internal rotation (AO 61 - B2.1).22
The Rommens classification is designed specifically to encompass the different fracture patterns seen in fragility fractures of the pelvis. The LC-1 FFP injury corresponds with Rommens type IIb and IIc injuries allowing further stratification of the severity of this injury. This describes an ipsilateral anterior disruption with either a sacral crush fracture (type IIb) or undisplaced sacral alar fracture (type IIc).18
Until recently, surgical fixation options for these fractures were limited. External fixators, a combination of pins, bars and clamps outside of the skin, are cumbersome, poorly tolerated and carry a high risk of pin-site infections and pressure sores.23 24 An alternate surgical option is fixation of the back of the pelvis with sacroiliac screws, a well-established technique in younger patients.4 Augmented screws, transiliac-transsacral screws and sacral bars are additional methods used to stabilise pelvic fractures. However, these procedures require significant technical expertise to implant and, crucially, the screws carry very poor ‘purchase’ in osteoporotic bone,8 leading to ineffective fracture stabilisation.
What works in younger patients with good bone quality is less effective in older patients.25 In 2010 a new technique of anterior subcutaneous internal fixation (INFIX) was developed, combining the principles of internal and external fixation. It involves placing screws in the supra-acetabular corridors and developing a subcutaneous tunnel in which a rod is connected to the screws to stabilise the pelvis.
The use of the INFIX device has been described across younger age groups and pelvic fracture types; alone or in combination with external surgical fixation techniques.26–29 However, the use of INFIX for the management of the FFP population who sustain an LC-1 fracture remains unclear as there has been no systematic review of the evidence.
Given the uncertainty around the management of LC-1 fractures in the elderly and the potential of INFIX to change the management of these injuries, we sought to identify and synthesise the evidence on the effectiveness of surgical fixation in fragility fractures of the pelvis. We included both internal and external surgical fixation, in order to provide a broad overview of the evidence on surgical fixation.
Objective
To undertake a systematic review of the evidence base for the effectiveness of surgical fixation of LC-1 fragility fractures when compared with non-surgical approaches.
Materials and methods
The protocol was prospectively registered in PROSPERO: CRD42017055872. The Centre for Reviews and Dissemination (CRD) guidance for undertaking reviews in healthcare was followed and reporting is in line with Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines.30 31
Patient and public involvement
There was no patient involvement in this systematic review of existing literature.
Data sources
An experienced information specialist undertook searches of MEDLINE (including Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Ovid MEDLINE Daily and Ovid MEDLINE), EMBASE and the Cochrane Central Register of Controlled Trials. ClinicalTrials.gov and the WHO International Clinical Trials Registry Portal were also searched for any information on studies that were in progress. Examples of the search terms included: (‘Ilium’ or ‘Ischium’ or ‘Pubis’ or ‘Pelvic Bones’ or ‘Pelvis’) AND (‘Bone Fractures’ or ‘Osteoporotic Fractures’ or ‘Compression Fractures’ or ‘Fragility Fractures’) AND (‘Fracture fixation’ or ‘Fracture fixation, Internal’ or ‘External fixators’ or ‘Splints’ or ‘Orthopaedic fixation devices’ or ‘Bone plates’ or ‘Bone screws’ or ‘Bone wires’ or ‘Internal fixators’). The full search strategy developed in Ovid MEDLINE is provided in online supplementary file 1. This was adapted for use in the other databases searched. The searches were limited to studies published in the English language from 1980 to date. All searches were initially run on 19 January 2017. As this is an area of rapid development, the search in MEDLINE was updated on 06 July 2017 and again on 19 February 2019.
bmjopen-2018-024737supp001.pdf (224.5KB, pdf)
Study selection
Studies of patients with LC-1 FFP undergoing surgery using either external or internal fixation devices were eligible for inclusion. Conservative non-surgical treatment was the defined comparator. If studies included other types of pelvic fractures, the study was included if the data on LC-1 FFP patients were reported separately and/or if 80% or more of participants had a LC-1 fragility fracture. Studies were excluded if LC-1 fractures were the result of a high-energy mechanism, defined as a fall from greater than standing height or if fractures arose secondary to pathology other than reduced bone density. Randomised controlled trials (RCTs), non-randomised trials and other comparative designs, observational studies (eg, cohort) and case series of 10 or more cases were included. Study designs other than RCTs are at high risk of bias when assessing treatment effectiveness; however, as the review was potentially to inform a future RCT, an inclusive approach was taken. Biomechanical and cadaver studies were excluded.
Titles and abstracts were independently reviewed by two reviewers for potentially relevant studies. Full text articles of potentially relevant studies were obtained and also reviewed independently by two reviewers (AB, HMAI) against the inclusion criteria, with discrepancies resolved by a third reviewer (MN).
Data extraction and quality assessment
Data were extracted by one researcher using a piloted form and checked by a second reviewer with discrepancies resolved by discussion (HMAI, AB). Data extracted were: publication year, study design, number of cases, total sample size, population type, mean age, percentage of male/female patients, fracture details, follow-up period, outcome measures and outcome data, details of the interventions and comparators and complications. Defined outcomes of interest were: patient mobility and function (using standardised outcome measures), pain (visual analogue scale (VAS) scores, analgesic or opiate requirements), quality of life (using standardised patient reported outcome measures (PROMS)), fracture union rate, mortality, hospital length of stay, complications (additional operative procedures, number and type of adverse events and serious adverse events) and radiographical alignment.
Quality assessment using the Joanna Briggs Institute Checklist for Case Series was undertaken by one researcher and checked by a second; disagreements were adjudicated by a third.32
Data synthesis
The aim of the synthesis was to identify gaps in the evidence and identify implications for future research. A narrative and tabular summary of the key study characteristics, study risk of bias and clinical outcomes was undertaken. Where possible, data were reported separately for internal and external fixation. The planned quantitative synthesis as outlined in the protocol was not possible due to the lack of randomised controlled trials.
Results
Study selection
The electronic searches identified 3845 records after deduplication and four records were found through other sources. Following screening of titles and abstracts, 98 full papers were assessed for eligibility, 94 were excluded (see online supplementary file 2) and four studies met the inclusion criteria (figure 1).33–36
Figure 1.
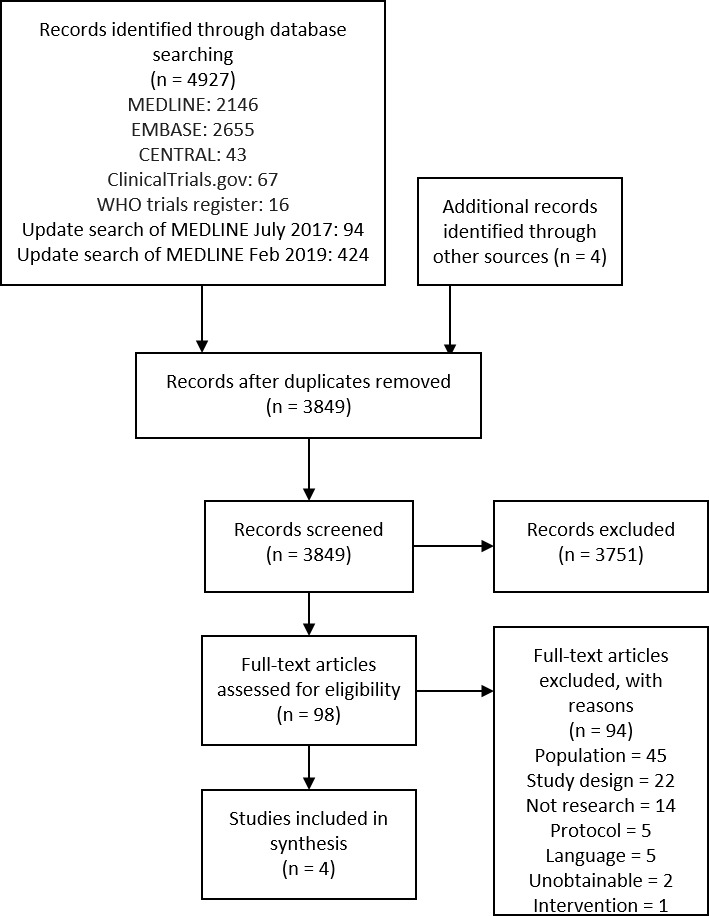
Study flow chart.
bmjopen-2018-024737supp002.pdf (337.9KB, pdf)
We identified two relevant, ongoing trials that are likely to include some patients with LC-1 fractures, though they are not specifically the target population in either trial. One is comparing surgeon choice of surgical technique with non-operative care37 and the other an experimental surgical intervention with conservative care.38 Final data collection for these trials will take place in December 201837 and October 2019.38
Characteristics of included studies
No RCTs comparing the effectiveness of external or internal fixation to non-operative management were identified. All of the included studies were case series: three retrospective34–36 and in the fourth, patients were identified post-operatively with data collected prospectively.33 Sample sizes ranged from 14 to 127 and the total duration of follow-up ranged from the day of removal of external fixator to 31 months. The procedures were undertaken from 2004 onwards to 2014 in Germany (n=3) and Italy (n=1). One study did not report when the procedures were undertaken33 and another reported 7 years after the last patient was included.36 Study characteristics are given in table 1.
Table 1.
Study characteristics
| Author (year) Study site |
Inclusion/exclusion criteria | Patient descriptors | Injuries documented and accounted for | Fracture classification | Cause of fracture and frequencies (eg, fall) | Fixation type | Time to surgery (days) Operation time (minutes) Post-op regime |
Follow-up time points |
| Arduini et al
34
Italy Retrospective case series |
Surgery for fragility fracture of the pelvis. Indications for surgery include: chronic lower limb pain or lower back pain with no other diagnosis following traditional treatment Exclusion Not reported |
Screened
Not reported Sample size 14 Mean age (SD) 69.6 Gender 9F:5M Comorbidities Osteoporosis = 5 taking bisphosphonates |
Concurrent
None reported Previous Undisplaced anterior ring pelvic fracture in the previous 2 years = 4 Other pelvic ring fracture = 2 |
Rommens type II = 3, type III = 9, type IV = 2 |
Low energy = 6 Spontaneous pain = 8 |
SI screws and symphysis plate or pubic rami screw = 8 Trans-sacral bridge plate and SI screws = 3 Lumbar-pelvic fixation and symphysis plate = 3 |
Time to surgery 6 Months Operation time Range 70 to 220 mins Postop Regime Bed rest for 4 to 6 weeks and partially weight-bearing for a further 6 to 8 weeks |
Primary:
6 months Secondary: 1 and 3 months |
| Gänsslen et al
33
Germany Case series: data collected prospectively patients identified from database postoperatively |
Patients ≥65 years with type B injuries stabilised by a supra-acetabular external fixator in a standardised technique were selected from the hospital pelvic database of all patients with pelvic ring and acetabular injuries. Exclusion Not reported |
Screened
Not reported Sample size 25 Mean age (SD) 79.3 (9.9) (range 66 to 99) Gender F23:M2 Comorbidities At least one significant co-morbidity = 19 (76%), most had two including hypertension, chronic heart disease or osteoporosis |
Concurrent
isolated pelvic trauma = 21 distal radius fracture and/or minor head injury = 4 Previous None reported |
AO
B 2.1 = 24 B 3.3 = 1 A 3.3 = 1 |
Low energy = 22 High energy = 3 |
Supra-acetabular external fixation |
Time to surgery Mean (SD) 3.6 (3.3) (range 0 to 13) Operation time Mean (SD) = 19 (7.4) (range 9 to 35) Postop Regime Fully weight-bearing = 14 Partial weight-bearing on the affected sacral side = 4 Partial weight-bearing = 7 |
Primary: postoperative discharge Secondary: removal of external fixator |
| Höch et al
36
Germany Retrospective case series |
Over 65 years, with a lateral compression fracture of the pelvis Exclusion Not reported |
Screened
Not reported Sample size 128 Mean age (SD) Overall 81 (8.3) Non-Operative 82.7 (7.9) Operative 78.3 (7.6) Died before treatment 92 P <0.002 Gender Overall F109:M19 Non-operative F66:M11 Operative F42:M8 Died before treatment F1:M0 Comorbidities Overall ASA 2.7 (SD 0.5) Non-operative ASA 2.8 (SD 0.6) Operative ASA 2.6 (SD 0.5) |
Concurrent
Overall ISS 10.1 (SD 4.6), isolated 89, additional injury ISS <16=31, ISS >16 = 8 Non-operative ISS 10.0 (SD 3.9), isolated 56, additional injury ISS <16 = 15, ISS >16 = 6 Operative ISS 9.4 (SD 2.1), isolated 33, additional injury ISS <16=16, ISS >16 = 1 Died before treatment ISS 48, ISS >16 = 1 Previous Not reported |
AO
B2.1=115 (90%) B3.3=13 (10%) Unilateral pubic rami = 117 (91%) Bilateral = 11 (9%) Complex pelvic fractures = 2 |
Overall
Low energy = 103 High energy = 13 Unknown = 12 Non-Op Low energy = 63 High energy = 7 Unknown = 7 Operative Low energy = 40 High energy = 5 Unknown = 5 Died before treatment High energy = 1 |
Unilateral iliosacral screw fixation = 28 S1 screws x2 = 4 S1+S2 screw = 2 Bilateral iliosacral screws = 14 Additional percutaneously sacroplasty = 13 Triangular fixation = 2 Additional anterior fixation plate = 3 Navigation = 7 |
Time to surgery Mean (SD) 6.4 (4.1) Operation time Not reported Post op Regime Full weight-bearing plus 3 weeks community physio |
Primary: two Years Secondary: 6 weeks, 3, 6 and 12 months included a clinical examination + radiographs |
| Hopf et al
35
Germany Retrospective case series |
Posterior pelvic ring fractures. Over 55 years, low energy trauma. Persistent lower back pain or unacceptable mobility Exclusion Patients under 55 years with a high energy trauma. If pain improved within 6 days and mobility was acceptable |
Screened
‘In the ‘recruitment period’ 87 patients with posterior ring fractures of the pelvis could be treated without surgery’ Sample size 30 Mean age (SD) Mean 78.4, range 56 to 96 Gender 27F:3M Comorbidities Osteoporosis=17 |
Concurrent
Not reported Previous Not reported |
Anterior + posterior = 18 Bilateral posterior = 11 Unilateral posterior = 1 |
Low energy = 30 | IIliosacral screws per side One screw unilateral = 6 Two screws unilateral = 18 Three screws unilateral = 2 Bilateral one screw = 2 patients. Two screws one side, one screw on other side = 2 |
Time to surgery Mean 9.2 (range 1 to 24) Operation time Not reported Postop Regime Mobilised day 1 post op |
Primary: mean 31 months Secondary: none |
ASA, American Society of Anaesthesiologists physical status classification; ISS, injury severity score; SI, sacroiliac.
Fixation types were not consistent between studies or within studies and most patients had more than one type of pelvic fixation. All internal fixations were posterior or a combination of anterior and posterior. Three studies reported effectiveness data on sacroiliac screws,34–36 and one on supra-acetabular external fixation,33 or a combination of these fixations. Höch et al 36 also included patients who had additional sacroplasty (n=13) in combination with the internal fixation techniques.
The average age of participants across the studies ranged from 69.6 to 81 years old and the percentage of female participants ranging from 64% to 92%. Comorbidities were reported within all the studies and included osteoporosis, hypertension, chronic heart disease and physical status. Where reported, between 20% and 57% of participants had osteoporosis.33–35 Two studies included a few patients with high-energy injuries; however, the majority of patients sustained their injuries following low-energy falls.33 36
The fracture classifications used were AO/Tile and Rommens, along with a narrative description of the injury.
Mean time from injury to surgery ranged from 3.6 days33 to 6 months.34 The duration of surgery was reported in two studies: the duration for internal fixation ranged between 70 and 220 min34 and for external fixation was between 9 min and 35 min.33
All four studies allowed most patients to fully or partially weight-bear following surgery. Arduini et al 34 dictated 4 to 6 weeks strict bed rest followed by partial weight-bearing for a further 6 to 8 weeks.34 The patients in this study differ from the other case series in that participants had chronic lower limb or back pain after 6 months of non-operative treatment. These patients were operated on at 6 months for chronic rather than acute pain, making it inappropriate to compare the outcomes and postoperative regime for acute fractures between this and the other studies.
Quality assessment
Höch et al 36 was the only study to include a non-operative group for comparison and a third group of those who died before treatment. This was the highest quality study included and had the largest sample size of 128 patients (50 operative patients, 77 non-operative and one died before treatment and as such was excluded from investigation within the paper), however, the patients were recruited retrospectively (method not defined) and approached at 2 years following injury.36 Patients in this study were selected for surgery if they were not able to mobilise 3 days after injury, after appropriate physical therapy and pain relief. The inclusion criteria or methods for selecting patients for inclusion were not clear in two studies33 34 and it is uncertain in three studies whether there was complete and/or consecutive inclusion of eligible patients in the case series (table 2).33–35
Table 2.
Quality assessment
| Question | Arduini et al 34 | Gänsslen et al 33 | Höch et al 36 | Hopf et al 35 |
| 1. Were there clear criteria for inclusion in the case series? | Unclear | Unclear | Yes | Yes |
| 2. Was the condition measured in a standard, reliable way for all participants included in the case series? | Yes | Yes | Yes | Yes |
| 3. Were valid methods used for identification of the condition for all participants included in the case series? | Unclear | Yes | Unclear | Unclear |
| 4. Did the case series have consecutive inclusion of participants? | Unclear | Yes | Yes | Unclear |
| 5. Did the case series have complete inclusion of participants? | Unclear | Unclear | Yes | Unclear |
| 6. Was there clear reporting of the demographics of the participants in the study? | Yes | Yes | Yes | Yes |
| 7. Was there clear reporting of clinical information of the participants? | Yes | Yes | Yes | Yes |
| 8. Were the outcomes or follow-up results of cases clearly reported? | Yes | Yes | Yes | Yes |
| 9. Was there clear reporting of the presenting site(s)/clinic(s) demographic information? | Yes | Yes | Yes | Yes |
| 10. Was statistical analysis appropriate? | Yes | Unclear | Yes | Yes |
The inclusion criteria varied across the studies; three had age-related criteria; over 6533 36 and over 55 years35; and one had criteria relating to type of fixation.33 The injuries were identified in a standard way using radiographs and CT in all four studies.
Exclusion criteria and details of the number and characteristics of patients screened to identify eligible participants were poorly reported or not reported at all.
Clinical outcomes
The outcomes extracted from the studies were mobility and function, pain, fracture union, hospital length of stay, quality of life, additional procedures and complications (table 3).
Table 3.
Outcomes: measures used and main findings
| Study ID | Patient mobility and function | Pain | Fracture union | Hospital length of stay | Additional operative procedures (for complication or as part of routine treatment) received: number of patients | Complications: AE and SAE Details of event: number of patients (overall/per group) |
| Arduini et al 34 | Mobility description Independent = 11 One crutch = 2 Two crutches = 1 |
Not measured | % healed at 6 months 100% |
Mean 5.8 days | One intra-pelvic iliac screw removed but no vascular, neurological or internal organ lesion was seen: 1 | No neurological palsy or vascular lesions were observed and no patients needed ICU. No major complications |
| Gänsslen et al 33 | Not stated, but degree of weight-bearing reported Pre-op: FWB = 24 Frame = 1 At discharge: FWB = 14 (56%) Crutches with PWB on affected side = 4 PWB = 7 At ExFix removal: Return to pre-injury mobility = 88% PWB = 3 |
VAS Preoperative: 7.7±1.4 (4 to 10) Postoperative: 2.3±1.7 (p<0.0001) Reduction pre to postop: 5.3±2 (2 to 9) At fixator removal: 0.6 (0 to 5) (p<0.0003) Reduction postop and at implant removal: 1.8±2.1. Pain free: 21 (84%) Mild pain (VAS 1 to 2): 3 Worse pain(VAS 5): 1 No change/1 point change: 10 Remaining patients showed improvement: 3.1 points |
Not measured | Total LOS 11±5.2 days (4 to 24 days) Postop LOS 7±5.4 (1 to 18 days) |
ExFix removed after an average 4±1.6 weeks (3 to 8 weeks): 25 56% were removed after 3 weeks |
Pin-infections treated with antibiotics: 2 No cases of postoperative nerve lesions or pin perforations seen |
| Höch et al 36 | Not measured | VAS Non-operative: 3.1 (SD 2.3) Failed non-operative: 2.3 (SD 2.8) Operative: 2.6 SD (2.8) p>0.5 |
Not measured | Non-Operative 9.2 (SD 6.2) days Operative group 18.1 (SD 10.0 days) (p<0.001) |
Mal-positioning of iliosacral screw with neurological complaints: 3 (6%) Wound infection with salvaging of the osteosynthesis: 1 (2%) |
Non-Op 6 (8%)
Severe complications: 2 Pneumonia: 2 Thrombosis: 2 Mesenteric infarction: 1 ARDS: 1 Surgery 9 (18%) Severe complications: 1 Pneumonia: 1 Thrombosis: 1 Diarrhoea: 1 Blood transfusions: 2 Implant loosening: 1 Delayed union: 1 Delayed surgery sub-group: 2 (14%) complications recorded |
| Hopf et al 35 | Not measured | VAS 0 to 10 preop, second day postoperative, pain at discharge Admission = 6.8 second day mean = 3.6 p<0.001 Discharge mean = 1.8 p<0.001 long-term pain = 6 in two patients |
Not measured | Mean=23.7 days, range 8 to 54 days | Complications: 3 Intra-op blood loss: 1 Nerve irritation/screw malposition: 1 Gluteal haematoma: 2 |
Three patients Pneumonia: 2 UTI: 2 |
AE, adverse event; ARDS, acute respiratory distress syndrome; ExFix, external fixator; FWB, full weight-bearing; ICU, intensive care unit; LFCN, lateral femoral cutaneous nerve; LOS, length of stay; PWB, partial weight-bearing; SAE, serious adverse event; UTI, urinary tract infection; VAS, visual analogue scale.
Quality of life
Only one study used PROMS, the EuroQol–5 domains (EQ-5D) and Short Form (SF)-12, to assess quality of life.36 Höch et al 36 (n=127), the only study with a non-operative arm for comparison, reported no statistically significant difference in quality of life, as measured via the EQ-5D, between the surgical fixation (mean 74.6, SD 15.5), surgical fixation after failed non-operative management (mean 76.3, SD 14.4) and non-operative management (mean 75.1, SD 13.4) groups (p>0.3). The analysis of the SF-12 questionnaire for physical and mental scores also showed no statistically significant difference between groups (p>0.2), but summary scores for the groups were not presented.
Mobility and function
Postoperative mobility was reported in two case series. This was assessed by the ability to stand and walk without crutches at 6 month follow-up34; and proportion mobilised with or without aids, and under full or partial weight-bearing at the time of external fixation removal, which was on average 4 weeks post operation.33 The reporting of mobilisation is not standardised between the two studies, making comparisons difficult. In Arduini et al,34 at 6 month follow-up, 11 (78%) patients were asymptomatic with restored ability to stand and walk without crutches and two patients were able to walk with one crutch. A patient with a history of previous acetabular fracture walked with two crutches and was still waiting for a total hip arthroplasty. In the Gänsslen et al,33 at the time of discharge, 14 patients (56%) were mobilised under full weight-bearing. Four patients (16%) were mobilised with crutches with partial weight-bearing on the affected sacral injury side. The remaining patients were mobilised partial weight-bearing (n=7). At the time of external fixation removal, 88% of patients had the same mobility as before the accident. Only three were still mobilised partial weight-bearing.
Postoperatively, 88% of those who received external fixation33 returned to their premorbid function.
Pain
Two studies reported a pain outcome. In one pain, measured by a 11 point VAS, significantly reduced following posterior internal fixation (mean pain score: on admission 6.8 and day 2 postoperative 3.6; p<0.001)35 and supra-acetabular external fixation (mean score (SD): preoperative 7.7 (1.4) and postoperative 2.3 (1.7); p<0.0001).33 Following removal of the external fixator, 84% of patients were pain free, 12% had mild residual pain and 4% had worse pain.33 In a second study there was no statistically significant difference in pain 2 years after discharge between the non-operative (mean 3.1, SD 2.3), failed non-operative (mean 2.3, SD 2.8) and operative (mean 2.6, SD 2.8) groups (p>0.5) based on an 11 point VAS.36
Length of hospital stay
All four studies reported length of hospital stay: ranging from 4 days33 to 54 days35 for surgical fixation of any type. Gänsslen et al reported that seven (28%) patients were discharged to a geriatric rehabilitation centre and one (4%) transferred to a different hospital. The mean length of hospital stay in Höch et al was statistically significantly (p<0.001) longer in the surgical fixation group (mean 18.1 days, SD 10.0) than in the non-operative group (mean 9.2 days, SD 6.2).36 Indications for surgery were not fully reported, making it difficult to distinguish why one patient had a primary surgical intervention and another did not. Over all the studies, of the 119 patients who received surgery, 14 patients had already undergone a period of conservative treatment before delayed surgery (6 months post injury), which may partly account for the increased length of stay for operative patients.
Complications
All studies reported on whether patients experienced complications: the percentage of participants who suffered from complications ranged from no major complications (0%) to 14% across studies. Reported complications and adverse outcomes included: infections,33 implant loosening,36 pneumonia35 36 and thrombosis36 (table 3). Höch et al observed no statistically significant difference in the number of complications between the combination of screw and plate fixations and non-operative groups (18% vs 8%, p=0.8).
In the study by Gänsslen et al, removal of the external fixation was performed after an average of 4 weeks requiring a second procedure (SD 1.6, range 3 to 8).33 There were two (8%) pin site infections in this series.
Posterior fixations also required further procedures; three patients (6%) had sacroiliac (SI) screws removed due to malposition and neurological complications in one study.36 Another study had one patient (7%) with an intra-pelvic iliac screw removed with no residual complaint.34 Other infrequent surgical complications with posterior fixation included two gluteal haematomas, one wound infection and one intra-operative bleed.35
Gänsslen et al was the only study to report radiographic alignment; postoperatively reduction was near anatomic with an average residual sacral displacement of 0.3 mm (0 to 1 mm) and anterior displacement of 1.4 mm (0 to 12 mm).
Mortality
Mortality was reported in one study36: during hospital stay three patients died due to respiratory insufficiency (two following from pneumonia and one from a pulmonary embolism) in the non-operative group; and one patient died of a pulmonary embolism and one of a suspected myocardial infarction in the operative group. By 2 year follow-up, 30% (n=38) of the patients had died; 41% in the non-operative group, 21% in the failed non-operative group and 18% of the operative group.36
Discussion
This systematic review searched for evidence on the effectiveness of surgical fixation compared with non-operative management in the treatment of LC-1 FFP with no age restriction. No robust evidence from RCTs was identified. The evidence-base was restricted to four case series, three of which were retrospective. Poor reporting of the inclusion criteria, how patients were selected and the completeness of inclusion of potential patients raise concerns of study results being affected by selection bias. The limitations of this study design in providing robust evidence of effectiveness is well recognised.39
The focus of this review was on surgical fixation. Surgical interventions used in the included studies were unilateral and bilateral percutaneous iliac screws, with or without plating or supra-acetabular external fixation. One study included adjunctive sacroplasty. The effectiveness of sacroplasty is yet to be established with contradictory results in the literature, however it is thought that the injection of cement into the fracture site can hinder fracture healing.18 Therefore, studies of sacroplasty as the primary technique were excluded from this review.
The four included studies reported on pain pre and postoperatively using visual analogue scores. The majority of patients recorded reduced levels of pain postoperatively. The other commonly reported outcome measure was length of hospital stay, which ranged from 4 days to 54 days. In one study the mean length of hospital stay was statistically significantly longer in the surgical fixation group than in the non-operative group. The proportion of patients across the four studies who had complications ranged from 0% to 14%. In the absence of details of the severity of the reported complications it is difficult to draw inferences. In addition, the level of experience of the surgeons and their familiarity with the techniques used in the studies were not reported.
Not all the studies reported on all the outcomes of interest in this review. Only one study assessed quality of life. Pelvic fractures are painful injuries and can significantly affect patients’ mobility and their ability to carry out activities of daily living independently.10 Immobility from prolonged bed rest can lead to potentially serious complications. Hence the role of surgery in improving mobility and quality of life in this frail, at risk population needs to be better defined. Although three studies reported return to pre-injury walking status or independent mobility, none of the studies used a standardised measure, so varied in how they reported patient mobility, ability to perform pre-injury walking status or ability to stand and walk without crutches. The time point for assessment also varied, ranging from an average of 4 weeks to 7.2 months after surgery. This makes the ability to compare the results limited and suggests there is a need for standardisation of a mobility measurement. In 2014, a survey of 111 surgeons from the Orthopaedic Trauma Association in the USA showed a large discrepancy in practice decisions and operative agreement of LC-1 pelvic fractures.40 Future studies should use standardised PROMS to assess important outcomes such as quality of life and ability of patients to undertake activities of daily living.
It is clear that there is also a need for consistency in the language and terminology used for describing low impact fractures of the pelvis.18–22 The existence and use of a number of different classification systems is concerning in terms of understanding decision making processes and the sharing of good practice.
The strength of this systematic review is in the rigorous methods used, including searching of multiple databases, duplicate study selection and checking of data extraction and quality assessment as well as protocol registration prior to commencing the review. Although key health databases were searched and efforts were made to search for unpublished studies via trial registers, we did not have the resources to search more widely and retrieval was limited to English language studies. We set out to include internal and external surgical fixation as two separate interventions due to differences in the technique which may lead to differences in effectiveness and complications. The included studies were mostly of internal fixation and reported the methods of surgical fixation as a single group but the impact of specific methods of internal fixation (in the form of SI screws or plates/screws) cannot be determined from the four case series analysed.
The lack of robust evidence makes it inappropriate to draw any definitive conclusions about effectiveness of internal or external surgical fixation compared with non-surgical management of LC-1 fragility fractures. It is clear from this review that the disparity in management between hip fractures (treated with early surgery) and LC-1 FFP (treated non-operatively) is primarily due the fact that, to date, there has been no effective surgical solution for the latter group, despite them being at very high risk of immobility-related illness. None of the studies examined here provided evidence supporting surgical fixation of FFP; indeed, there is a suggestion that internal fixation might paradoxically contribute to an increased length of hospital stay. The included studies all used traditional pelvic implants (iliosacral screws and external fixators) that may be less suitable for LC-1 FFP populations. Other studies suggest that iliosacral screws anchored in very soft, deficient bone have poor purchase and become loose and ineffective very quickly.25 External fixators are poorly tolerated and are prone to pin-site infections.28
However, it is clear from the epidemiological data that LC-1 fractures in the elderly are catastrophically disabling for many patients, who either do not survive or never return to their pre-injury baseline function.7 8 The surgical approach taken to hip fractures is therefore conceptually appealing, provided an effective technique can be identified to provide pain-relieving stability to the pelvis and allow patients to mobilise rapidly.
The introduction of the INFIX technique in 2010 means there is now a device which has the potential to effectively stabilise LC-1 fractures in older adults. The intervention is already in everyday use in specialist pelvic fracture units for the younger population, meaning that pelvic surgeons have experience of the technique.
There is a potential that the enthusiasm of surgeons using INFIX in the younger population may apply the same principles to the older population (as with hip fractures), so the surgery could potentially become the new ‘standard of care’ for these patients. However, although there are a number of papers reporting on the use of INFIX, we were unable to identify any studies that met our inclusion criteria.29 41 42 More robust evidence in the form of high-quality RCTs is needed to support surgical intervention and the use of devices such as INFIX in the elderly population with fragility fractures of the pelvis. Although a multicentre RCT within this patient group would be challenging, it would help avoid a situation where patients either do not receive surgical fixation because of lack of evidence, or where they are exposed to a treatment that might be neither beneficial nor cost effective.
Conclusion
There is currently insufficient robust evidence to support guidance on the most effective treatment for elderly patients who fail to mobilise after sustaining an LC-1 fragility fracture. Given the growing interest of specialist pelvic surgeons in the use of surgical interventions in this population, there is an urgent need for more robust evidence of effectiveness.
Supplementary Material
Footnotes
Contributors: AB: protocol development, search strategy, study selection, critical appraisal, analysis, writing, approval of final submission. HMAI: protocol development, search strategy, study selection, critical appraisal, analysis, writing, critique of drafts, approval of final submission. MN: protocol development, search strategy, study selection, critical appraisal, analysis, writing, critique of drafts, approval of final submission. EC: protocol development, analysis, writing, critique of drafts, approval of final submission. MH: search strategy, literature searches, writing search methods for protocol and final report, approval of final submission. JK: concept for review, protocol development, search strategy, study selection, analysis, writing, critique of drafts, approval of final submission. IK: protocol development, search strategy, study selection, writing, critique of drafts, approval of final submission. CH: protocol development, search strategy, study selection, writing, critique of drafts, approval of final submission. PB: concept for review, protocol development, search strategy, analysis, writing, critique of drafts, approval of final submission. CM: concept for review, protocol development, search strategy, analysis, writing of paper, critique of draft papers, approval of final submission.
Funding: CM receives funding from the British Orthopaedic Association; HI’s Fellowship at the University of York is funded by Orthopaedic Research UK (ORUK).
Competing interests: HMAI, MN, EC, MH, IK, CH declare they have no conflicts of interest. Since starting this review, AB, JK, PB and CM have received funding for a trial of surgical fixation compared to non-surgical treatment in a LC1 FFP population.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: The data extraction tables and quality assessment tables are available from the corresponding author upon reasonable request.
Patient consent for publication: Not required.
References
- 1. National Osteoporosis Society. Effective secondary prevention of fragility fractures: clinical standards for fracture liaison services. Bath: National Osteoporosis Society, 2015. [Google Scholar]
- 2. Andrich S, Haastert B, Neuhaus E, et al. Epidemiology of pelvic fractures in Germany: considerably high incidence rates among older people. PLoS One 2015;10:e0139078 10.1371/journal.pone.0139078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hill RMF, Robinson CM, Keating JF. Fractures of the pubic rami. J Bone Joint Surg Br 2001;83-B:1141–4. 10.1302/0301-620X.83B8.0831141 [DOI] [PubMed] [Google Scholar]
- 4. Studer P, Suhm N, Zappe B, et al. Pubic rami fractures in the elderly–a neglected injury? Swiss Med Wkly 2013;143:w13859 10.4414/smw.2013.13859 [DOI] [PubMed] [Google Scholar]
- 5. Burge R, Dawson-Hughes B, Solomon DH, et al. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res 2007;22:465–75. 10.1359/jbmr.061113 [DOI] [PubMed] [Google Scholar]
- 6. Aprato A, Joeris A, Tosto F, et al. Direct and indirect costs of surgically treated pelvic fractures. Arch Orthop Trauma Surg 2016;136:325–30. 10.1007/s00402-015-2373-9 [DOI] [PubMed] [Google Scholar]
- 7. Greenleaf JE, Kozlowski S. Physiological consequences of reduced physical activity during bed rest. Exerc Sport Sci Rev 1982;10:84–119. 10.1249/00003677-198201000-00004 [DOI] [PubMed] [Google Scholar]
- 8. Soles GL, Ferguson TA. Fragility fractures of the pelvis. Curr Rev Musculoskelet Med 2012;5:222–8. 10.1007/s12178-012-9128-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lefaivre KA, Slobogean GP, Ngai JT, et al. What outcomes are important for patients after pelvic trauma? Subjective responses and psychometric analysis of three published pelvic-specific outcome instruments. J Orthop Trauma 2014;28:23–7. 10.1097/BOT.0b013e3182945fe9 [DOI] [PubMed] [Google Scholar]
- 10. Taillandier J, Langue F, Alemanni M, et al. Mortality and functional outcomes of pelvic insufficiency fractures in older patients. Joint Bone Spine 2003;70:287–9. 10.1016/S1297-319X(03)00015-0 [DOI] [PubMed] [Google Scholar]
- 11. Morris RO, Sonibare A, Green DJ, et al. Closed pelvic fractures: characteristics and outcomes in older patients admitted to medical and geriatric wards. Postgrad Med J 2000;76:646–50. 10.1136/pmj.76.900.646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Keene GS, Parker MJ, Pryor GA. Mortality and morbidity after hip fractures. BMJ 1993;307:1248–50. 10.1136/bmj.307.6914.1248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Marrinan S, Pearce MS, Jiang XY, et al. Admission for osteoporotic pelvic fractures and predictors of length of hospital stay, mortality and loss of independence. Age Ageing 2015;44:258–61. 10.1093/ageing/afu123 [DOI] [PubMed] [Google Scholar]
- 14. National Institute for Health and Care Excellence (NICE). Hip fracture: management. NICE guideline [CG124]. London: NICE, 2017. [PubMed] [Google Scholar]
- 15. National Institute for Health and Care Excellence (NICE). Fractures (complex): assessment and management. NICE guideline [NG37]. London: NICE, 2016. [PubMed] [Google Scholar]
- 16. Krappinger D, Struve P, Schmid R, et al. Fractures of the pubic rami: a retrospective review of 534 cases. Arch Orthop Trauma Surg 2009;129:1685–90. 10.1007/s00402-009-0942-5 [DOI] [PubMed] [Google Scholar]
- 17. Scheyerer MJ, Osterhoff G, Wehrle S, et al. Detection of posterior pelvic injuries in fractures of the pubic rami. Injury 2012;43:1326–9. 10.1016/j.injury.2012.05.016 [DOI] [PubMed] [Google Scholar]
- 18. Rommens PM, Hofmann A. Comprehensive classification of fragility fractures of the pelvic ring: Recommendations for surgical treatment. Injury 2013;44:1733–44. 10.1016/j.injury.2013.06.023 [DOI] [PubMed] [Google Scholar]
- 19. Young JW, Burgess AR, Brumback RJ, et al. Lateral compression fractures of the pelvis: the importance of plain radiographs in the diagnosis and surgical management. Skeletal Radiol 1986;15:103–9. 10.1007/BF00350202 [DOI] [PubMed] [Google Scholar]
- 20. Burgess AR, Eastridge BJ, Young JW, et al. Pelvic ring disruptions: effective classification system and treatment protocols. J Trauma 1990;30:848–56. [PubMed] [Google Scholar]
- 21. Tile M. Pelvic ring fractures: should they be fixed? J Bone Joint Surg Br 1988;70:1–12. 10.1302/0301-620X.70B1.3276697 [DOI] [PubMed] [Google Scholar]
- 22. Marsh JL, Slongo TF, Agel J, et al. Fracture and dislocation classification compendium - 2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma 2007;21:S1–133. [DOI] [PubMed] [Google Scholar]
- 23. McDonald C, Firoozabadi R, Routt ML, et al. Complications Associated With Pelvic External Fixation. Orthopedics 2017;40:e959–e963. 10.3928/01477447-20170918-02 [DOI] [PubMed] [Google Scholar]
- 24. Rommens PM, Wagner D, Hofmann A. Minimal Invasive Surgical Treatment of Fragility Fractures of the Pelvis. Chirurgia, 2017;112:524–37. Bucharest, Romania: 1990. [DOI] [PubMed] [Google Scholar]
- 25. Wagner D, Kamer L, Rommens PM. Bone mass distribution in the sacrum : Rommens PM, Hofmann A, Fragility fractures of the pelvis. Cham: Springer International Publishing, 2017:35–42. [Google Scholar]
- 26. Hesse D, Kandmir U, Solberg B, et al. Femoral nerve palsy after pelvic fracture treated with INFIX: a case series. J Orthop Trauma 2015;29:138–43. 10.1097/BOT.0000000000000193 [DOI] [PubMed] [Google Scholar]
- 27. Hoskins W, Bucknill A, Wong J, et al. A prospective case series for a minimally invasive internal fixation device for anterior pelvic ring fractures. J Orthop Surg Res 2016;11:135 10.1186/s13018-016-0468-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Vaidya R, Colen R, Vigdorchik J, et al. Treatment of unstable pelvic ring injuries with an internal anterior fixator and posterior fixation: initial clinical series. J Orthop Trauma 2012;26:1–8. 10.1097/BOT.0b013e318233b8a7 [DOI] [PubMed] [Google Scholar]
- 29. Vaidya R, Nasr K, Feria-Arias E, et al. INFIX/EXFIX: Massive open pelvic injuries and review of the literature. Case Rep Orthop 2016;2016:1–7. 10.1155/2016/9468285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Centre for Reviews and Dissemination. Systematic reviews. CRD’s guidance for undertaking reviews in healthcare. York: CRD, University of York, 2009. [Google Scholar]
- 31. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 2010;8:336–41. 10.1016/j.ijsu.2010.02.007 [DOI] [PubMed] [Google Scholar]
- 32. The Joanna Briggs Institute. Joanna Briggs Institute Reviewer’s Manual: 2016 edition. Australia: The Joanna Briggs Institute, 2016. [Google Scholar]
- 33. Gänsslen A, Hildebrand F, Kretek C. Supraacetabular external fixation for pain control in geriatric type B pelvic injuries. Acta Chir Orthop Traumatol Cech 2013;80:101–5. [PubMed] [Google Scholar]
- 34. Arduini M, Saturnino L, Piperno A, et al. Fragility fractures of the pelvis: treatment and preliminary results. Aging Clin Exp Res 2015;27:61–7. 10.1007/s40520-015-0430-4 [DOI] [PubMed] [Google Scholar]
- 35. Hopf JC, Krieglstein CF, Müller LP, et al. Percutaneous iliosacral screw fixation after osteoporotic posterior ring fractures of the pelvis reduces pain significantly in elderly patients. Injury 2015;46:1631–6. 10.1016/j.injury.2015.04.036 [DOI] [PubMed] [Google Scholar]
- 36. Höch A, Özkurtul O, Pieroh P, et al. Outcome and 2-year survival rate in elderly patients with lateral compression fractures of the pelvis. Geriatr Orthop Surg Rehabil 2017;8:3–9. 10.1177/2151458516681142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. O’Toole R. Pelvis RCT: impact of surgery on pain in lateral compression type pelvic fractures. ClinicalTrials.gov, Last verified: March 2017 Available: https://ClinicalTrials.gov/show/NCT02625766 [Accessed Mar 2017].
- 38. Jakob M. Treatment of pelvic ring fractures in the elderly. ClinicalTrials.gov, Last verified: April 2017 Available: https://ClinicalTrials.gov/show/NCT02590783 [Accessed Apr 2017].
- 39. Guyatt GH, Oxman AD, Vist G, et al. GRADE guidelines: 4. Rating the quality of evidence–study limitations (risk of bias). J Clin Epidemiol 2011;64:407–15. 10.1016/j.jclinepi.2010.07.017 [DOI] [PubMed] [Google Scholar]
- 40. Beckmann JT, Presson AP, Curtis SH, et al. Operative agreement on lateral compression-1 pelvis fractures. a survey of 111 OTA members. J Orthop Trauma 2014;28:681–5. 10.1097/BOT.0000000000000133 [DOI] [PubMed] [Google Scholar]
- 41. Fang C, Alabdulrahman H, Pape HC. Complications after percutaneous internal fixator for anterior pelvic ring injuries. Int Orthop 2017;41:1785–90. 10.1007/s00264-017-3415-4 [DOI] [PubMed] [Google Scholar]
- 42. Vaidya R, Martin AJ, Roth M, et al. INFIX versus plating for pelvic fractures with disruption of the symphysis pubis. Int Orthop 2017;41:1671–8. 10.1007/s00264-016-3387-9 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2018-024737supp001.pdf (224.5KB, pdf)
bmjopen-2018-024737supp002.pdf (337.9KB, pdf)


