Abstract
Introduction
Nintedanib slows disease progression in patients with idiopathic pulmonary fibrosis (IPF) by reducing the rate of decline in forced vital capacity, with an adverse event profile that is manageable for most patients. We used data from six clinical trials to characterise the safety and tolerability profile of nintedanib and to investigate its effects on survival.
Methods
Data from patients treated with ≥1 dose of nintedanib 150 mg two times per day or placebo in the 52-week TOMORROW trial and/or its open-label extension; the two 52-week INPULSIS trials and/or their open-label extension, INPULSIS-ON; and a Phase IIIb trial with a placebo-controlled period of ≥6 months followed by open-label nintedanib were pooled. All adverse events, irrespective of causality, were included in descriptive analyses. Parametric survival distributions were fit to pooled Kaplan-Meier survival data from the trials and extrapolated to estimate long-term survival.
Results
There were 1126 patients in the pooled nintedanib group and 565 patients in the pooled placebo group. The mean duration of nintedanib treatment was 28 months. No new safety signals were observed. Incidence rates of bleeding, liver enzyme elevations and cardiovascular events were consistent with those observed in the INPULSIS trials. Diarrhoea was reported at a lower event rate in the pooled nintedanib group than in nintedanib-treated patients in the INPULSIS trials (76.5 vs 112.6 events per 100 patient exposure-years) and infrequently led to permanent treatment discontinuation (3.6 events per 100 patient exposure-years). Based on the Weibull distribution, mean (95% CI) survival was estimated as 11.6 (9.6, 14.1) years in nintedanib-treated patients and 3.7 (2.5, 5.4) years in placebo-treated patients.
Conclusions
Based on pooled data from six clinical trials, the adverse event profile of nintedanib was manageable for most patients. Exploratory analyses based on extrapolation of survival data suggest that nintedanib extends life expectancy in patients with IPF.
Keywords: interstitial fibrosis
Key messages.
Is nintedanib therapy well tolerated in patients with idiopathic pulmonary fibrosis (IPF) and does it improve survival?
Data from 1126 patients with IPF participating in prospective clinical trials showed that the adverse event profile of nintedanib was manageable for most patients; extrapolation of survival data suggested that nintedanib extends life expectancy.
This is the largest data set on nintedanib to be published to date and the first analyses to estimate life expectancy in patients with IPF treated with nintedanib based on extrapolation of survival data from clinical trials.
Introduction
Idiopathic pulmonary fibrosis (IPF) is an interstitial lung disease associated with progressive loss of lung function, worsening dyspnoea and substantial impairment in quality of life.1 2 IPF has a variable clinical course but a poor prognosis. In patients not receiving antifibrotic therapies, median survival following diagnosis of IPF is approximately 3–5 years.3–6
Nintedanib, an intracellular inhibitor of tyrosine kinases, is an approved treatment for IPF. The efficacy, safety and tolerability of nintedanib 150 mg two times per day in patients with IPF and mild or moderate impairment in lung function have been assessed in several international clinical trials: the Phase II TOMORROW trial7 and its open-label extension8; the two replicate Phase III INPULSIS trials9 and their open-label extension INPULSIS-ON10; and an exploratory Phase IIIb trial.11 The results of these trials demonstrated that nintedanib reduces disease progression by slowing the rate of decline in forced vital capacity (FVC), with a side effect profile characterised mainly by gastrointestinal adverse events. Although no individual trial of nintedanib in patients with IPF has been powered to show a reduction in mortality versus placebo, an analysis of pooled data from the TOMORROW and INPULSIS trials suggested that nintedanib was associated with a 30% reduction in the risk of mortality compared with placebo over 52 weeks of treatment (HR 0.70 [95% CI 0.46 to 1.08]; p=0.095).12
We used data from the six international Phase II/III trials of nintedanib conducted in patients with IPF and mild or moderate impairment in lung function7–11 to extend the characterisation of the safety and tolerability profile of nintedanib and to investigate its effects on survival in patients with IPF.
Methods
Study design
The TOMORROW trial (NCT00514683) began with a 52-week period in which patients with IPF, FVC≥50% predicted and diffusing capacity of the lung for carbon monoxide (DLco) 30%–79% predicted were randomised to receive placebo or one of four doses of nintedanib (50 mg once daily, 50 mg two times per day, 100 mg two times per day, 150 mg two times per day).7 Patients who completed 52 weeks’ treatment in this period (period 1) continued treatment in a blinded phase (period 2), until the last patient had completed 52 weeks’ treatment in period 1. This was followed by an open-label extension period in which all patients received nintedanib (NCT01170065).8 In each of the INPULSIS trials (NCT01335464 and NCT01335477), patients with IPF, FVC≥50% predicted and DLco 30%–79% predicted were randomised 3:2 to receive nintedanib 150 mg two times per day or placebo for 52 weeks.9 Patients who completed the 52-week treatment period and a follow-up visit 4 weeks later were eligible to receive open-label nintedanib in INPULSIS-ON (NCT01619085).10 In the Phase IIIb trial (NCT01979952), patients with IPF, FVC≥50% predicted and DLco 30%–79% predicted were originally randomised to receive nintedanib 150 mg two times per day or placebo double-blind for 12 months, but this was amended to a placebo-controlled period of 6 months following regulatory approval of nintedanib in some participating countries. The double-blind period was ≥6 months for some patients due to the variable time required to implement the protocol amendment.11 In all these trials, dose reductions from 150 to 100 mg two times per day and treatment interruptions were allowed to manage adverse events. No dose re-escalations were permitted in the TOMORROW trial, but dose could be increased from 100 to 150 mg two times per day in the open-label extension of the TOMORROW trial, and in the other trials described above. In all these trials, specific recommendations were provided to the investigators for the management of adverse events of diarrhoea and hepatic enzyme elevations. Patients at an increased risk of bleeding (ie, with a genetic predisposition to bleeding, or requiring fibrinolysis, full-dose therapeutic anticoagulation, or high-dose antiplatelet therapy) were not eligible to participate in these trials. Patients with a recent history of thrombotic events, including stroke and transient ischaemic attacks (previous year), myocardial infarction (MI; previous 6 months) and unstable angina (previous month), were excluded from the randomised placebo-controlled trials. Patients who developed new major thromboembolic events after completion of the INPULSIS trials were excluded from INPULSIS-ON.
For the purposes of this analysis, patients treated with ≥1 dose of nintedanib 150 mg two times per day in the trials described above were pooled to form a pooled nintedanib group. Patients who were randomised to placebo or nintedanib 50 mg once a day, 50 mg two times per day, or 100 mg two times per day in the double-blind phase of the TOMORROW trial were not included in the pooled nintedanib population, even if they received a dose of nintedanib 150 mg two times per day in the open-label extension. Patients who switched from blinded placebo to open-label nintedanib in INPULSIS-ON and the Phase IIIb trial were analysed as part of the pooled nintedanib population from their first dose of nintedanib. Patients treated with ≥1 dose of placebo in the TOMORROW, INPULSIS and Phase IIIb trials were pooled to form a pooled placebo group.
Patient and public involvement
Patients were not involved in the design, recruitment to or conduct of the studies included in this analysis.
Safety and tolerability
All adverse events reported by investigators, irrespective of causality, were included in this analysis. Adverse events were coded according to preferred terms in the Medical Dictionary for Regulatory Activities (MedDRA) version 19.1. Safety data from INPULSIS-ON and the Phase IIIb trial were based on a snapshot conducted on 15 April 2017. The other trials had been completed by this date, but the MedDRA coding was updated to obtain consistent coding within the pooled population. Based on the mechanism of action of nintedanib, bleeding, major adverse cardiovascular events (MACE), MI and hepatic enzyme elevations were considered of particular interest. Bleeding was based on the standardised MedDRA query (SMQ) ‘haemorrhage terms (excluding laboratory terms)’. MACE were based on fatal adverse events in the MedDRA system organ classes ‘cardiac disorders’ and ‘vascular disorders’; fatal and non-fatal events in the subordinate SMQ ‘myocardial infarction’; stroke based on selected preferred terms from the subordinate SMQs ‘haemorrhagic cerebrovascular conditions’ and ‘ischaemic cerebrovascular conditions’; and the MedDRA preferred terms ‘sudden death’, ‘cardiac death’ and ‘sudden cardiac death’. MI was based on the subordinate SMQ ‘myocardial infarction (narrow definition)’. Hepatic enzyme elevations were based on a list of MedDRA preferred terms.
Event rates per 100 patient exposure-years were calculated based on adverse events with onset after the first dose and up to 28 days (or 14 days in the TOMORROW trial) after the last dose of study drug. Analyses were descriptive.
Survival
Survival data from INPULSIS-ON and the Phase IIIb trial were based on a snapshot conducted on 15 April 2017. The other trials had been completed by this date. Weibull13 and exponential14 parametric survival distributions were fit to pooled Kaplan-Meier survival data for patients treated with nintedanib 150 mg two times per day and placebo and extrapolated to estimate life expectancy over the long term. The extent to which these statistical models fit the data was estimated using Akaike’s information criterion. The estimated survival of patients treated with nintedanib and placebo was calculated from the area under the curve. Survival time was estimated from randomisation in the double-blind placebo-controlled trials and from the first intake of nintedanib if started in the open-label trials.
Results
Patients
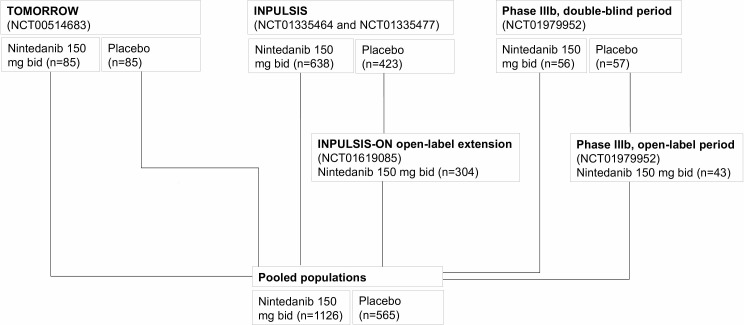
A total of 1126 patients treated with nintedanib 150 mg two times per day and 565 patients treated with placebo comprised the pooled populations (figure 1). Baseline characteristics were generally similar between the nintedanib and placebo groups (table 1). In the pooled nintedanib population, the majority of patients were male (78.3%) and white (61.7%); at baseline, mean (SD) age was 66.9 (8.1) years, FVC was 78.7 (18.4)% predicted and DLco was 48.2 (13.5)% predicted.
Figure 1.
Patients treated with nintedanib 150 mg two times per day and placebo who comprised the pooled populations.
Table 1.
Baseline characteristics
| Pooled population treated with nintedanib (n=1126) | Pooled population treated with placebo (n=565) |
INPULSIS trials | ||
| Nintedanib (n=638) | Placebo (n=423) | |||
| Age, years, mean (SD) | 66.9 (8.1) | 66.6 (8.2) | 66.6 (8.1) | 67.0 (7.9) |
| Male, n (%) | 882 (78.3) | 434 (76.8) | 507 (79.5) | 334 (79.0) |
| Race, n (%) | ||||
| White | 695 (61.7) | 367 (65.0) | 360 (56.4) | 248 (58.6) |
| Asian | 316 (28.1) | 151 (26.7) | 194 (30.4) | 128 (30.3) |
| Black | 2 (0.2) | 0 (0.0) | 2 (0.3) | 0 (0.0) |
| Missing* | 113 (10.0) | 47 (8.3) | 82 (12.9) | 47 (11.1) |
| Body mass index, kg/m2, mean (SD) | 27.9 (4.6) | 27.9 (4.6) | 28.1 (4.6) | 27.6 (4.6) |
| Smoking history, n (%) | ||||
| Former smoker | 768 (68.2) | 374 (66.2) | 435 (68.2) | 283 (66.9) |
| Never smoker | 313 (27.8) | 167 (29.6) | 174 (27.3) | 122 (28.8) |
| Current smoker | 45 (4.0) | 24 (4.2) | 29 (4.5) | 18 (4.3) |
| FVC, % predicted, mean (SD) | 78.7 (18.4) | 79.5 (18.3) | 79.7 (17.6) | 79.3 (18.2) |
| FEV1/FVC, %, mean (SD) | 81.6 (6.4) | 81.7 (5.9) | 81.7 (5.8) | 81.7 (6.0) |
| DLco, % predicted, mean (SD) | 48.2 (13.5)† | 47.7 (13.5) | 47.4 (13.5) | 47.0 (13.4) |
*In France, regulation did not permit the collection of data on race.
†n=821 (DLco was not collected at the start of the open-label extensions of TOMORROW and INPULSIS-ON).
DLco, diffusing capacity of the lung for carbon monoxide; FEV1, forced expiratory volume in 1 s; FVC, forced vital capacity.
Exposure
The mean (SD) exposure to nintedanib in the pooled population was 27.7 (20.5) months (online supplementary table S1). The median exposure to nintedanib was 22.5 months and the maximum was 93.1 months. Exposure to nintedanib in the individual trials is summarised in the online supplementary table S2. In total, 458 (40.7%) patients in the pooled nintedanib population had ≥1 dose reduction from 150 to 100 mg two times per day. Median exposures to nintedanib 150 and 100 mg two times per day were 14.2 and 8.3 months, respectively.
bmjresp-2018-000397supp001.pdf (149.1KB, pdf)
Mean (SD) exposure to placebo in the pooled population was 10.4 (3.1) months. The median exposure to placebo was 11.9 months and the maximum was 13.1 months.
Adverse events
Diarrhoea was the most frequent adverse event in patients treated with nintedanib. In the pooled nintedanib population, the event rate of diarrhoea was 76.5 events per 100 patient exposure-years, which was lower than that reported in nintedanib-treated patients in the INPULSIS trials (112.6 events per 100 patient exposure-years) but higher than that in the pooled placebo population (25.6 events per 100 patient exposure-years) (table 2). The event rate of hepatic enzyme elevation was 12.1 events per 100 patient exposure-years in the pooled nintedanib population compared with 3.4 events per 100 patient exposure-years in placebo-treated patients in the INPULSIS trials (table 3). The event rate of bleeding was 9.3 events per 100 patient exposure-years in the pooled nintedanib population compared with 10.2 events per 100 patient exposure-years in placebo-treated patients in the INPULSIS trials (table 3). The most common bleeding events in the pooled nintedanib population were epistaxis (3.1 events per 100 patient exposure-years) and haemoptysis (1.3 events per 100 patient exposure-years). The event rates for MACE and MI in the pooled nintedanib population were 3.7 and 1.1 events per 100 patient exposure-years, compared with 2.7 and 0.5 events per 100 patient exposure-years, respectively, in placebo-treated patients in the INPULSIS trials (table 3).
Table 2.
Adverse events reported in the pooled population treated with nintedanib and in nintedanib-treated and placebo-treated patients in the INPULSIS trials
| Pooled population treated with nintedanib (n=1126) | INPULSIS | |||||
| Nintedanib (n=638) | Placebo (n=423) | |||||
| Events, n | Event rate (per 100 patient exposure-years) |
Events, n | Event rate (per 100 patient exposure-years) |
Events, n | Event rate (per 100 patient exposure-years) |
|
| Diarrhoea | 2084 | 76.5 | 671 | 112.6 | 106 | 25.6 |
| Nausea | 489 | 18.0 | 208 | 34.9 | 29 | 7.0 |
| Nasopharyngitis | 410 | 15.1 | 117 | 19.6 | 91 | 22.0 |
| Bronchitis | 395 | 14.5 | 92 | 15.5 | 62 | 15.0 |
| Cough | 359 | 13.2 | 96 | 16.1 | 67 | 16.2 |
| Progression of IPF* | 350 | 12.9 | 70 | 11.8 | 73 | 17.7 |
| Vomiting | 304 | 11.2 | 102 | 17.1 | 11 | 2.7 |
| Upper respiratory tract infection | 274 | 10.1 | 72 | 12.1 | 55 | 13.3 |
| Dyspnoea | 253 | 9.3 | 50 | 8.4 | 51 | 12.3 |
| Weight decreased | 230 | 8.4 | 64 | 10.7 | 15 | 3.6 |
| Decreased appetite | 225 | 8.3 | 75 | 12.6 | 26 | 6.3 |
| Abdominal pain | 168 | 6.2 | 68 | 11.4 | 10 | 2.4 |
| Lower respiratory tract infection | 164 | 6.0 | 47 | 7.9 | 22 | 5.3 |
| Respiratory tract infection | 160 | 5.9 | 33 | 5.5 | 28 | 6.8 |
| Pneumonia | 159 | 5.8 | 40 | 6.7 | 31 | 7.5 |
| Fatigue | 153 | 5.6 | 44 | 7.4 | 35 | 8.5 |
Adverse events with event rate >5 per 100 patient exposure-years in the pooled population are shown.
*Corresponds to MedDRA preferred term ‘IPF’, which included disease worsening and acute exacerbations.
IPF, idiopathic pulmonary fibrosis; MedDRA, Medical Dictionary for Regulatory Activities.
Table 3.
Adverse events of particular interest in the pooled population treated with nintedanib and in the INPULSIS trials
| Pooled population treated with nintedanib (n=1126) | INPULSIS | |||||
| Nintedanib (n=638) | Placebo (n=423) | |||||
| Events, n |
Event rate (per 100 patient exposure-years) |
Events, n |
Event rate (per 100 patient exposure-years) |
Events, n |
Event rate (per 100 patient exposure-years) |
|
| Hepatic enzyme elevation | 330 | 12.1 | 132 | 22.2 | 14 | 3.4 |
| Bleeding | 253 | 9.3 | 94 | 15.8 | 42 | 10.2 |
| MACE | 101 | 3.7 | 26 | 4.4 | 11 | 2.7 |
| Myocardial infarction | 30 | 1.1 | 11 | 1.8 | 2 | 0.5 |
MACE, major adverse cardiovascular events.
The event rates of adverse events that led to permanent dose reduction or permanent treatment discontinuation in the pooled nintedanib population were generally lower than those reported in nintedanib-treated patients in the INPULSIS trials (online supplementary tables S3 and S4). In the pooled nintedanib population, the event rate of adverse events that led to permanent dose reduction was 12.8 events per 100 patient exposure-years. Diarrhoea was the most frequent adverse event that led to permanent dose reduction of nintedanib (at a rate of 7.4 events per 100 patient exposure-years). The event rate of adverse events that led to permanent discontinuation of nintedanib was 23.8 events per 100 patient exposure-years. The event rate of diarrhoea that led to permanent discontinuation of nintedanib was 3.6 events per 100 patient exposure-years.
The event rate of serious adverse events in the pooled nintedanib population was 64.6 events per 100 patient exposure-years (online supplementary table S5). Progression of IPF, which included disease worsening and acute exacerbations, was the most frequent serious adverse event reported in the pooled nintedanib population. This was reported at a lower rate than in placebo-treated patients in the INPULSIS trials (8.4 vs 11.4 events per 100 patient exposure-years).
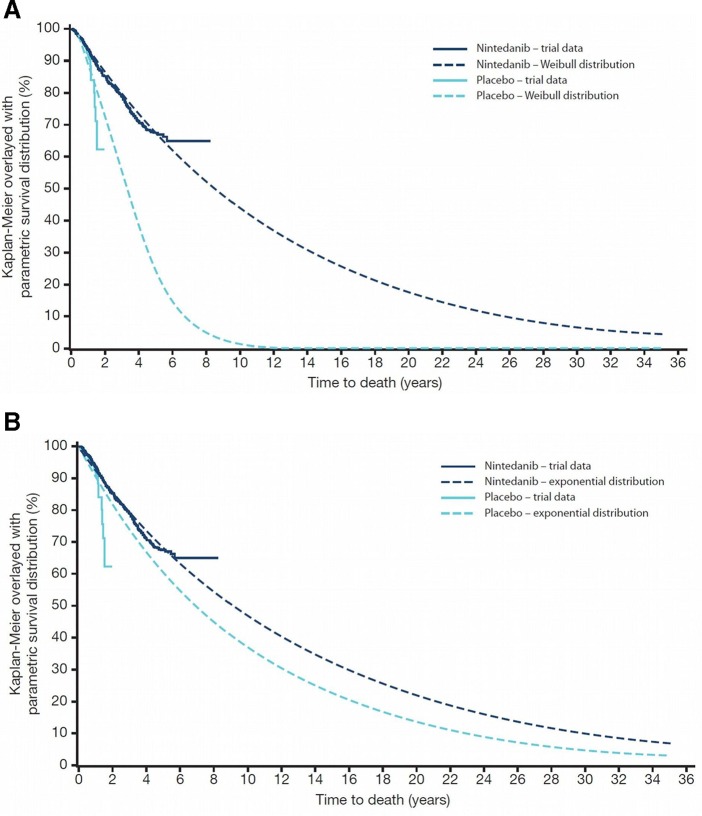
Survival
The numbers of deaths in the individual trials are shown in the online supplementary tables S6 and S7. Based on the Weibull distribution, mean (95% CI) survival was estimated as 11.6 (9.6, 14.1) years in nintedanib-treated patients and 3.7 (2.5, 5.4) years in placebo-treated patients (figure 2A). Median survival was estimated as 8.5 years and 3.3 years in these groups, respectively. Based on the exponential distribution, mean (95% CI) survival was estimated as 13.1 (11.6, 14.9) years in nintedanib-treated patients and 10.1 (7.8, 13.0) years in placebo-treated patients (figure 2B). Median survival was estimated as 9.1 years and 7.0 years in these groups, respectively. Model fit based on Akaike’s information criterion was superior (lower) for the Weibull model compared with the exponential model in placebo-treated patients (428 vs 440) but not in nintedanib-treated patients (1593 for both models).
Figure 2.
Estimated time to death using (A) the Weibull distribution and (B) exponential distribution.
Discussion
We conducted a comprehensive analysis of the safety and tolerability of nintedanib using pooled data from six clinical trials conducted in patients with IPF and mild or moderate impairment in lung function. Based on data from 1126 patients followed up for a mean of 28 months and a maximum of 93 months, nintedanib had a safety and tolerability profile that was manageable for most patients, with adverse events that were mainly gastrointestinal in nature. As expected, the most frequently reported adverse event was diarrhoea, which was reported at an event rate of 76.5 events per 100 patient exposure-years but led to permanent treatment discontinuation at a much lower rate (3.6 events per 100 patient exposure-years). Diarrhoea is a well-known side effect of tyrosine kinase inhibitors but the precise mechanism/s that cause it are unclear.15 It is recommended that patients who experience diarrhoea while taking nintedanib should ensure adequate hydration and take antidiarrheal medicine (eg, loperamide) straight away.16 17 If diarrhoea persists, dose adjustment is recommended, and indeed in our analysis, diarrhoea was the most common reason for permanent dose reduction of nintedanib. Dose adjustment is also recommended to treat nausea and vomiting.16 Importantly, data from the INPULSIS trials showed that the rate of decline in FVC was similar in patients treated with nintedanib irrespective of whether they had dose reductions and/or treatment interruptions to manage adverse events.18
Elevations in hepatic enzymes (alanine aminotransferase and aspartate aminotransferase) and bilirubin occur in a small proportion of patients treated with nintedanib and cases of drug-induced liver injury have been reported.16 It is recommended that hepatic enzymes be monitored prior to the initiation of nintedanib, at regular intervals during the first 3 months of treatment, and periodically thereafter.16 In the pooled nintedanib population, hepatic enzyme elevations (based on a list of MedDRA preferred terms) occurred at a rate of 12.1 events per 100 patient exposure-years, compared with 3.4 events per 100 patient exposure-years in placebo-treated patients in the INPULSIS trials. None of the nintedanib-treated patients with hepatic enzyme elevations developed liver failure and there were no liver-related deaths.
Like other inhibitors of the vascular endothelial growth factor receptor19 nintedanib has been associated with an increased risk of bleeding.20 The event rate of bleeding observed in the pooled population of nintedanib-treated patients was no higher than that observed in placebo-treated patients in the INPULSIS trials (9.3 vs 10.2 events per 100 patient exposure-years, respectively). The lower event rate of bleeding in the pooled nintedanib population compared with nintedanib-treated patients in the INPULSIS trials suggests that the risk of bleeding events does not increase with more prolonged treatment. However, it should be noted that patients at known risk of bleeding, including those treated with full-dose anticoagulants or high-dose antiplatelet therapy, were excluded from these trials. It is recommended that nintedanib be used in patients with known risk of bleeding only if the anticipated benefit outweighs the potential risk.16
Event rates of MACE and MI in the pooled nintedanib population were low and consistent with those observed in nintedanib-treated patients in the INPULSIS trials.9 In postmarketing surveillance data collected in the USA in the year following the launch of nintedanib as a treatment for IPF, the incidence rates of MACE and MI were lower than those in nintedanib-treated patients in the INPULSIS trials21; further, the incidence of MI was lower than that observed in an analysis of insurance claims data from 9286 US patients with IPF.22 These data are reassuring with regard to the cardiovascular safety profile of nintedanib.
Modelling and extrapolation of survival data from the clinical trials included in this pooled analysis suggest that nintedanib extends life expectancy in patients with IPF. Median survival based on the better fitting statistical model (Weibull) was extended by approximately 5 years in patients treated with nintedanib compared with placebo. Clearly such extrapolations have limitations and should be interpreted with caution, but these data add to the growing body of evidence suggesting that antifibrotic therapies are associated with improved survival in patients with IPF.6 12 23–26
Strengths of these analyses include the use of a large and well-characterised cohort of patients participating in prospectively designed clinical trials and a maximum treatment duration of over 7 years. Limitations include the exclusion of patients who had severe impairment in lung function, had certain comorbidities, or who were using full-dose anticoagulants from these trials, and selection bias in the patients who entered the open-label extension trials, in that these patients were likely to have milder disease and to be better able to tolerate nintedanib than those who discontinued during the parent trial.
In conclusion, in 1126 patients with IPF treated with nintedanib for a mean duration of 28 months, adverse events were manageable for most patients. The adverse event profile of nintedanib in the pooled population was consistent with that observed in the INPULSIS trials, with no new safety signals observed. Exploratory analyses based on extrapolation of survival data suggested that patients with IPF who are treated with nintedanib have longer life expectancy than those who do not receive treatment.
Acknowledgments
Medical writing assistance, supported financially by Boehringer Ingelheim, was provided by Julie Fleming and Wendy Morris of FleishmanHillard Fishburn, London, UK, during the preparation of this manuscript. The authors received no direct compensation for the development of the manuscript, were fully responsible for all content and editorial decisions, were involved at all stages of manuscript development and have approved the final version. Boehringer Ingelheim was given the opportunity to review the manuscript for medical and scientific accuracy as well as intellectual property considerations.
Footnotes
Contributors: All authors were involved in planning the analyses, in the interpretation of data and in drafting the manuscript.
Funding: The trials that provided data for these analyses were funded by Boehringer Ingelheim.
Competing interests: LLa has served on advisory boards for Genentech, Global Blood Therapeutics, Boehringer Ingelheim, Veracyte, Theravance, Magnolia Therapeutics, Galapagos and Bellerophon; has provided disease state education for Genentech and Boehringer Ingelheim; has served as a principal investigator in clinical trials in IPF and other ILDs for Genentech, Global Blood Therapeutics, Celgene, FibroGen, Stromedix, Veracyte, Afferent, Merck, Bellerophon, Novartis, Galapagos, Galecto, the National Institutes of Health and Boehringer Ingelheim. BC has received grants from Apellis and MedImmune; grants and personal fees from Boehringer Ingelheim and Roche; and personal fees from AstraZeneca and Sanofi. PH has served on advisory boards for Actelion, AstraZeneca, Boehringer Ingelheim, GlaxoSmithKline, Teva and Trudell; served as a principal investigator in clinical trials in IPF for Boehringer Ingelheim and Prometic; and provided disease state education in IPF/ILDs for Boehringer Ingelheim and Roche. YI has served on advisory boards for Boehringer Ingelheim and reports lecture and advisory fees from Boehringer Ingelheim, Shionogi & Co, Ltd, Takeda, Nobel Pharma, Novartis, Serendex, Bayer, Chugai and Daiichi Sankyo. LR has served on advisory boards for Anthera, Asahi-Kasei, AstraZeneca, Bayer, Boehringer Ingelheim, Biogen Idec, FibroGen, GlaxoSmithKline, ImmuneWorks, InterMune, MedImmune, PatientsLikeMe, Promedior, Roche, Sanofi-Aventis, Takeda and UCB; received grants from InterMune, the Italian Ministry of Health, the National Drug Agency (Italy), the National Research Council (Italy) and Roche; and received speaker fees from Boehringer Ingelheim, Cipla, InterMune and Roche. DW, LLo, MQ and SS are employees of Boehringer Ingelheim.
Patient consent for publication: Not required.
Ethics approval: All clinical trial protocols were approved by an independent ethics committee or institutional review board at every participating institution.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Data are available uponon request. A request can be submitted via https://trials.boehringer-ingelheim.com/trial_results/clinical_submission_documents.html.
References
- 1. Raghu G, Remy-Jardin M, Myers JL, et al. Diagnosis of idiopathic pulmonary fibrosis. An official ATS/ERS/JRS/ALAT clinical practice guideline. Am J Respir Crit Care Med 2018;198:e44–68. 10.1164/rccm.201807-1255ST [DOI] [PubMed] [Google Scholar]
- 2. Kreuter M, Swigris J, Pittrow D, et al. Health related quality of life in patients with idiopathic pulmonary fibrosis in clinical practice: insights-IPF registry. Respir Res 2017;18 10.1186/s12931-017-0621-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Fernández Pérez ER, Daniels CE, Schroeder DR, et al. Incidence, prevalence, and clinical course of idiopathic pulmonary fibrosis: a population-based study. Chest 2010;137:129–37. 10.1378/chest.09-1002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Nathan SD, Shlobin OA, Weir N, et al. Long-term course and prognosis of idiopathic pulmonary fibrosis in the new millennium. Chest 2011;140:221–9. 10.1378/chest.10-2572 [DOI] [PubMed] [Google Scholar]
- 5. Raghu G, Chen S-Y, Yeh W-S, et al. Idiopathic pulmonary fibrosis in US Medicare beneficiaries aged 65 years and older: incidence, prevalence, and survival, 2001-11. Lancet Respir Med 2014;2:566–72. 10.1016/S2213-2600(14)70101-8 [DOI] [PubMed] [Google Scholar]
- 6. Guenther A, Krauss E, Tello S, et al. The European IPF registry (eurIPFreg): baseline characteristics and survival of patients with idiopathic pulmonary fibrosis. Respir Res 2018;19 10.1186/s12931-018-0845-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Richeldi L, Costabel U, Selman M, et al. Efficacy of a tyrosine kinase inhibitor in idiopathic pulmonary fibrosis. N Engl J Med 2011;365:1079–87. 10.1056/NEJMoa1103690 [DOI] [PubMed] [Google Scholar]
- 8. Richeldi L, Kreuter M, Selman M, et al. Long-term treatment of patients with idiopathic pulmonary fibrosis with nintedanib: results from the tomorrow trial and its open-label extension. Thorax 2018;73:581–3. 10.1136/thoraxjnl-2016-209701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Richeldi L, du Bois RM, Raghu G, et al. Efficacy and safety of nintedanib in idiopathic pulmonary fibrosis. N Engl J Med 2014;370:2071–82. 10.1056/NEJMoa1402584 [DOI] [PubMed] [Google Scholar]
- 10. Crestani B, Huggins JT, Kaye M, et al. Long-term safety and tolerability of nintedanib in patients with idiopathic pulmonary fibrosis: results from the open-label extension study, INPULSIS-ON. Lancet Respir Med 2019;7:60–8. 10.1016/S2213-2600(18)30339-4 [DOI] [PubMed] [Google Scholar]
- 11. Lancaster L, Ilowite J, Trampisch M, et al. Effect of nintedanib on disease progression: results from a phase IIIB trial in patients with idiopathic pulmonary fibrosis. Nashville, TN, USA: Poster presented at the Pulmonary Fibrosis Foundation, 2017. [Google Scholar]
- 12. Richeldi L, Cottin V, du Bois RM, et al. Nintedanib in patients with idiopathic pulmonary fibrosis: Combined evidence from the TOMORROW and INPULSIS(®) trials. Respir Med 2016;113:74–9. 10.1016/j.rmed.2016.02.001 [DOI] [PubMed] [Google Scholar]
- 13. Collett D. Modelling survival data in medical research. London: Chapman and Hall, 1994. [Google Scholar]
- 14. Beck JR, Kassirer JP, Pauker SG. A convenient approximation of life expectancy (the "DEALE"). I. Validation of the method. Am J Med 1982;73:883–8. [DOI] [PubMed] [Google Scholar]
- 15. Bowen JM. Mechanisms of TKi-induced diarrhea in cancer patients. Curr Opin Support Palliat Care 2013;7:162–7. 10.1097/SPC.0b013e32835ec861 [DOI] [PubMed] [Google Scholar]
- 16. Boehringer Ingelheim Pharmaceuticals, Inc OFEV® (nintedanib) prescribing information, 2018. Available: http://bidocs.boehringer-ingelheim.com/BIWebAccess/ViewServlet.ser?docBase=renetnt&folderPath=/Prescribing+Information/PIs/Ofev/ofev.pdf [Accessed 30 Nov 2018].
- 17. Bendstrup E, Wuyts W, Alfaro T, et al. Nintedanib in idiopathic pulmonary fibrosis: practical management recommendations for potential adverse events. Respiration 2019;97:173–84. 10.1159/000495046 [DOI] [PubMed] [Google Scholar]
- 18. Maher TM, Inoue Y, Case AH, et al. Effect of dose reductions and/or interruptions on the efficacy of nintedanib in patients with idiopathic pulmonary fibrosis (IPF): Subgroup analysis of the INPULSIS trials. Washington, DC, USA: Poster presented at the American Thoracic Society International Conference, 2017. [Google Scholar]
- 19. Chen HX, Cleck JN. Adverse effects of anticancer agents that target the VEGF pathway. Nat Rev Clin Oncol 2009;6:465–77. 10.1038/nrclinonc.2009.94 [DOI] [PubMed] [Google Scholar]
- 20. Corte T, Bonella F, Crestani B, et al. Safety, tolerability and appropriate use of nintedanib in idiopathic pulmonary fibrosis. Respir Res 2015;16 10.1186/s12931-015-0276-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Noth I, Oelberg D, Kaul M, et al. Safety and tolerability of nintedanib in patients with idiopathic pulmonary fibrosis in the USA. Eur Respir J 2018;52. doi: 10.1183/13993003.02106-2017. [Epub ahead of print: 27 Jul 2018]. [DOI] [PubMed] [Google Scholar]
- 22. Collard HR, Ward AJ, Lanes S, et al. Burden of illness in idiopathic pulmonary fibrosis. J Med Econ 2012;15:829–35. 10.3111/13696998.2012.680553 [DOI] [PubMed] [Google Scholar]
- 23. Fisher M, Nathan SD, Hill C, et al. Predicting life expectancy for pirfenidone in idiopathic pulmonary fibrosis. J Manag Care Spec Pharm 2017;23(3-b Suppl):S17–S24. 10.18553/jmcp.2017.23.3-b.s17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. HE J, Glaspole I, Grainge C, et al. Baseline characteristics of idiopathic pulmonary fibrosis: analysis from the Australian idiopathic pulmonary fibrosis registry. Eur Respir J 2017;49. [DOI] [PubMed] [Google Scholar]
- 25. Rinciog C, Watkins M, Chang S, et al. A cost-effectiveness analysis of nintedanib in idiopathic pulmonary fibrosis in the UK. Pharmacoeconomics 2017;35:479–91. 10.1007/s40273-016-0480-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Vašáková M. Real world idiopathic pulmonary fibrosis in the Empire registry. Poster presented at the European Respiratory Society International Congress, 2018. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjresp-2018-000397supp001.pdf (149.1KB, pdf)