Abstract
The NLRP3 inflammasome is a multimeric protein complex that cleaves caspase-1 and the pro-inflammatory cytokines interleukin 1 beta (IL-1β) and IL-18. Dysregulated NLRP3 inflammasome signalling is linked to several chronic inflammatory and autoimmune conditions; thus, understanding the activation mechanisms of the NLRP3 inflammasome is essential. Studies over the past few years have implicated vital roles for distinct intracellular organelles in both the localisation and assembly of the NLRP3 inflammasome. However, conflicting reports exist. Prior to its activation, NLRP3 has been shown to be resident in the endoplasmic reticulum (ER) and cytosol, although, upon activation, the NLRP3 inflammasome has been shown to assemble in the cytosol, mitochondria, and mitochondria-associated ER membranes by different reports. Finally, very recent work has suggested that NLRP3 may be localised on or adjacent to the Golgi apparatus and that release of mediators from this organelle may contribute to inflammasome assembly. Therefore, NLRP3 may be strategically placed on or in close proximity to these subcellular compartments to both sense danger signals originating from these organelles and use the compartment as a scaffold to assemble the complex. Understanding where and when NLRP3 inflammasome assembly occurs may help identify potential targets for treatment of NLRP3-related disorders.
Keywords: NLRP3, caspase-1, mitochondria, endoplasmic reticulum, Golgi, inflammasome, IL-1β, IL-18, cholesterol, SREBP2
Introduction
Inflammasomes are multimeric protein complexes composed of typically a Nod-like receptor (NLR) or absent in myeloma 2 (AIM2), the adaptor molecule apoptosis-associated speck-like protein containing a CARD (ASC), and the effector protease caspase-1. Upon activation, the receptor dimerises and recruits ASC via pyrin domain interactions and ASC subsequently interacts with caspase-1 via their respective CARD domains. Caspase-1 undergoes autoproteolytic cleavage to produce an active fragment which is able to cleave the precursor forms of cytokines interleukin 1 beta (IL-1β) and IL-18, leading to pro-inflammatory responses 1– 5. In addition to cleaving the above cytokines, caspase-1 cleaves gasdermin-D (GSDMD) to produce an active N-terminal fragment which subsequently inserts into the plasma membrane and assembles a pore, resulting in an inflammatory cell death termed pyroptosis 6– 8.
Of all the NLR inflammasomes characterised to date, the NLRP3 inflammasome has been the most extensively studied, largely due to its role in several infectious and inflammatory disorders 9– 14. Activation of the NLRP3 inflammasome is unique in that it requires two signals to assemble. The first signal involves ligation of typically a Toll-like receptor (TLR), initiating activation of the transcription factor nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) and upregulation of pro-IL-1β and NLRP3. This initial step is often referred to as the “priming” signal. The second signal (also known as the activating signal) is induced by a wide variety of substances, including exogenous and endogenous compounds such as ATP, silica, cholesterol crystals, and alum, as well as a variety of bacterial, viral and fungal pathogens or their toxins (or both). How such a wide variety of structurally and chemically diverse entities are all able to activate the NLRP3 inflammasome has been at the forefront of inflammasome biology for the last decade. It is commonly accepted that all of these ligands do not bind NLRP3 directly and instead converge on a cellular pathway which subsequently activates NLRP3 15. Mechanisms proposed for NLRP3 activation include K + efflux, mitochondrial dysfunction, production of reactive oxygen species (ROS), lysosomal rupture, and Ca 2+ mobilisation. Although some of these mechanisms are involved in response to many NLRP3 activators, absolute requirement of any specific mechanism with all activating signals is still to be demonstrated, thereby precluding a consensus on the central NLRP3 inflammasome-activating mechanism. A common theme among many of the proposed mechanisms is the sensing of molecules released as a result of cellular/organelle stress and dysfunction 16– 18. Additionally, emerging evidence has now suggested key homeostatic functions for endoplasmic reticulum (ER) and Golgi in NLRP3 activation 18– 22. Here, we review recent literature focusing on the roles that mitochondria, ER, and Golgi play in the localisation, assembly, and activation of the NLRP3 inflammasome. Though less studied, the requirement of these organelles in activation of other inflammasomes, when relevant, is also discussed. A critical role for lysosomes has been recognised in response to particulate ligands; however, we have not included a separate section on this organelle as it has been discussed in detail in several published reviews 23– 25.
Cellular localisation of NLRP3 and ASC
Studies conducted almost a decade ago suggested NLRP3 inflammasome localisation on mitochondria and mitochondria-associated ER membranes (MAMs) 26. Detailed biochemical studies demonstrated that, under resting conditions, the majority of NLRP3 is located in the ER and cytosol of THP-1 cells overexpressing NLRP3. However, upon activation with NLRP3 activators monosodium urate (MSU) or nigericin, NLRP3 relocated to the perinuclear space and associated with both mitochondrial and ER markers and therefore is thought to be located on MAMs, composed of both ER and mitochondrial outer membrane fragments 26. A small fraction of NLRP3 was also found in the cytosol upon activation. Similarly, Yang et al. have demonstrated that the activated NLRP3 inflammasome is located on the mitochondria 27. Conversely, Wang et al. showed that the NLRP3 inflammasome shows no association with mitochondrial markers and was located solely in the cytosol of mouse macrophages exposed to lipopolysaccharide (LPS) and ATP 28. However, the location of NLRP3 may be cell-specific, as nuclear localisation was reported in CD4 + Th2 cells, whereas cytoplasmic location was observed in CD4 + Th1 cells following differentiation 29. In this case, nuclear NLRP3 transcriptionally regulated Th2 differentiation of CD4 + T cells but did not participate in inflammasome formation per se 29.
The recruitment of NLRP3 to MAMs may be dependent on mitochondrial cardiolipin or the presence of mitochondrial antiviral signalling (MAVS), an outer mitochondrial membrane protein involved in retinoic acid–inducible gene I (RIG-I)-mediated interferon (IFN) responses 30– 32. Additionally, the translocation of NLRP3 to mitochondria may rely on the presence of a short sequence in the N-terminal domain of human NLRP3 30; although murine NLRP3 differs in this minimal N-terminal sequence, it too was found to be associated with mitochondria upon activation 32. Other studies found a role for microtubules in the transport of NLRP3 to mitochondria and this was aided by microtubule-affinity regulating kinase 4 (MARK4), which helped position NLRP3 to mitochondria for effective “speck” formation and optimal inflammasome activity ( Figure 1). mCherry-tagged NLRP3 was shown to move along microtubules towards mitochondria in nigericin-activated THP-1 cells, a response that was diminished in MARK4 knock-down cells 33. In agreement, inhibition of tubulin polymerisation by either colchicine or nocodazole diminished NLRP3 inflammasome activation 33, 34. The localisation of NLRP3 on or in close vicinity to mitochondria offers an obvious advantage to the cell as any disturbance in cellular homeostasis leading to mitochondrial dysfunction would result in efficient sensing and activation of NLRP3. Studies on the localisation of ASC within the cell are somewhat contradictory; Misawa et al. demonstrated the localisation in the mitochondria, cytosol, and nucleus under resting conditions in primary bone marrow–derived macrophages (BMDMs) 34. Once an activating signal is sensed, a dynein-dependent mechanism transports ASC on the mitochondria in close proximity to NLRP3 on the ER 34. This transport was shown to be independent of K + efflux and mitochondrial ROS (mtROS). Additionally, other reports have shown ASC to reside exclusively in the cytosol and in the nucleus under resting conditions and to associate with mitochondria upon NLRP3 inflammasome activation 26, 35. Whether the nature of the upstream stimuli calibrates the localisation of the NLRP3 inflammasome to distinct subcellular compartments is still unclear, as is the localisation of other inflammasome-forming receptors.
Figure 1. Mitochondria and ER in activation of the NLRP3 inflammasome.
A proportion of NLRP3 has been shown to reside in the ER prior to activation and translocate to the mitochondria or mitochondria-associated membranes during activation. The translocation of NLRP3 to the mitochondria has been shown to be dependent on microtubule rearrangement and microtubule kinase MARK4. Activation of the NLRP3 inflammasome requires two signals. The first signal, referred to as NLRP3 “priming”, requires activation of NF-κB (for example, through TLR stimulation) and the upregulation of NLRP3 and IL-1β. The second activating signal has been shown to be mediated via several mechanisms. TLR priming induced upregulation of mtDNA via CMPK2, and the upregulation of mtROS has been shown to activate the NLRP3 at the mitochondria. mtDNA may also be able to activate the AIM2 inflammasome. ER stress has also been implicated in NLRP3 inflammasome activation, and ER stress–induced activation of the UPR response pathway, including UPR sensors IRE1α and PERK, is required for NLRP3 inflammasome activation. Following activation, the NLRP3 inflammasome leads to the activation of caspase-1 and subsequent cleavage of IL-1β and IL-18. AIM2, absent in myeloma 2; ASC, apoptosis-associated speck-like protein containing a CARD; CMPK2, cytidine/uridine monophosphate kinase 2; ER, endoplasmic reticulum; IL-1β, interleukin-1 beta; IL-18, interleukin-18; IRE1α, inositol-requiring protein 1 alpha; MARK4, microtubule-affinity regulating kinase 4; mtDNA, mitochondrial DNA; mtROS, mitochondrial reactive oxygen species; NF-κB, nuclear factor kappa-light-chain-enhancer of activated B cells; PERK, protein kinase R-like endoplasmic reticulum kinase; TLR, Toll-like receptor; UPR, unfolded protein response.
Mitochondria
Mitochondrial dysfunction leads to NLRP3 inflammasome activation
Positioning of NLRP3 following activation on MAMs/mitochondria is thought to enable immediate recognition of mitochondrial damage, which has been proposed as a central event downstream of various NLRP3-activating stimuli. These damage signals include mtROS, mitochondrial DNA (mtDNA) and cardiolipin ( Figure 1) 26, 36, 37.
Cellular ROS was initially shown to activate the NLRP3 inflammasome in an NAPDH-dependent manner; however, further studies showed that ROS generated by the mitochondria is sufficient to lead to NLRP3 activation 26, 38, 39. Specific inhibition of mtROS significantly diminishes NLRP3 inflammasome activation 40. Yu et al. demonstrated that mitochondrial damage following NLRP3 inflammasome activation occurs in a caspase-1–dependent manner, resulting in the release of mtROS 41. Caspase-1 was demonstrated to amplify this response by inhibiting mitophagy, the process of removal of damaged mitochondria, which then contributed to pyroptosis induction 41. Conversely, ROS production has been shown to be dispensable for NLRP3 inflammasome activation, and the significance of K + efflux has been highlighted 42, thereby suggesting these as independent NLRP3 activation mechanisms. How increases in mtROS production activate NLRP3 is still unclear, although TXNIP has been implicated by various studies 43– 45. TXNIP is a negative regulator of the antioxidant thioredoxin (TRX) and is thought to dissociate from TRX in the presence of ROS, allowing TXNIP to bind to NLRP3. In agreement, NLRP3 inflammasome activation is impaired in TXNIP -/- mice 46. The precise mechanism remains unresolved. Furthermore, mutations in mtDNA-encoded cytochrome b gene in patients with fibromyalgia are associated with mitochondrial dysfunction and increased ROS production, leading to enhanced caspase-1 cleavage, and IL-1β and IL-18 secretion in fibroblasts and serum respectively 47. Increases in ROS have previously been implicated in other inflammatory disorders 48, 49.
In addition to mtROS, the release of mtDNA—in particular, oxidised mtDNA—in response to mitochondrial dysfunction activates the NLRP3 inflammasome 36, 50, 51. NLRP3 inflammasome priming via TLRs has been shown to induce mtROS production and, more recently, the production of mtDNA 52, 53. The latter is dependent on MyD88/TRIF- and IRF-1-mediated upregulation of mitochondrial deoxyribonucleotide kinase, CMPK2, an enzyme with rate-limiting activity in mtDNA synthesis 53. The newly synthesised mtDNA (made during priming) was found to be necessary to generate oxidised mtDNA fragments when cells were subsequently exposed to an NLRP3-activating signal ( Figure 1) 53. Of note, oxidised DNA from any cellular source can activate the NLRP3 inflammasome. In fact, mtDNA contributes to inflammation in diseases such as atherosclerosis and inflammatory kidney disorders, and the inhibition of its release by exposure to agents that maintain mitochondrial integrity prevents NLRP3 inflammasome activation 54– 59. Contrary to the above, TLR-dependent priming also restricts inflammasome activation through efficient removal of damaged mitochondria. TLR-activated NF-κB pathway induces prolonged accumulation of the autophagic receptor p62/SQSTM1, which targets damaged mitochondria for clearance by mitophagy 60, thereby preventing NLRP3 over-activation 61. Whether inhibition of mtDNA release or maintenance of mitochondrial integrity (or both) will translate into novel therapeutics for disorders in which NLRP3 inflammasome is dysregulated is yet to be seen.
A small number of studies have implicated mtDNA in the activation of other inflammasome complexes. Mitochondrial damage by Pseudomonas aeruginosa leads to the release of ROS and mtDNA; the latter was shown to bind and activate the NLRC4 inflammasome. In agreement, abolition of mtDNA by DNase I treatment resulted in reduced caspase-1 activation and IL-1β secretion following P. aeruginosa infection 62. However, caspase-1 activation was not completely abolished by DNase I in Nlrc4 −/− macrophages, suggesting roles for other inflammasomes, and the authors attributed this to AIM2 inflammasome activation. Although NLRP3 is not thought to be involved during P. aeruginosa infection, a role for NLRP3 was not experimentally ruled out 62, 63. Dang et al. also demonstrated that mtDNA, released as a result of loss of mitochondrial integrity by elevated cellular cholesterol levels, can activate the AIM2 inflammasome in macrophages lacking cholesterol-25-hydroxylase. In wild-type cells, production of 25-hydroxycholesterol (25-HC) by cholesterol-25-hydroxylase repressed cholesterol biosynthesis, thereby maintaining mitochondrial integrity 64. However, only a small redundant role for NLRP3 was found in the above study, although mtDNA is known to activate this inflammasome 36. As the AIM2 inflammasome can recognise both foreign and self-DNA, it is likely that it can also recognise mtDNA; however, further studies are required to confirm these findings. Whether mtDNA has the ability to directly activate multiple inflammasomes 65 or whether upstream stimuli direct differential activation of NLRP3 and AIM2 inflammasomes requires further clarification.
NLRP3 is recruited to and binds mitochondrial cardiolipin
Cardiolipin, a phospholipid localised to the inner mitochondrial membrane (IMM), has also been linked to NLRP3 inflammasome activation. Upon NLRP3 activation or in the presence of stimuli that destabilise mitochondria, cardiolipin redistributes to the outer leaflet of the mitochondrial membrane (OMM), where NLRP3 anchors through its leucine-rich repeat (LRR) domain 37, 66 ( Figure 1). Depletion of cardiolipin or abrogation of cardiolipin synthesis by culturing cells in the presence of palmitate (C16:0), a saturated long-chain fatty acid, blunted inflammasome activation in J774A.1 macrophages 37. Similarly, small interfering RNA (siRNA) knock-down of cardiolipin synthase reduced NLRP3 activation 37. Corroborating these findings, activation of the NLRP3 inflammasome, by HIV reverse transcriptase inhibitor abacavir, was abrogated following inhibition of cardiolipin synthase-1 37. Furthermore, cardiolipin-dependent NLRP3 inflammasome activation by the antibiotic linezolid, which induces mitochondrial toxicity, was ROS-independent 37. Thus, mitochondrial dysfunction, which induces ROS under certain conditions, and not ROS itself, may be responsible for NLRP3 inflammasome activation. Additionally, recent work from the group established that NLRP3 is recruited to the mitochondria at the priming stage and binds to cardiolipin on the OMM 67. Interestingly, the movement of cardiolipin to the OMM was found to be dependent on ROS produced during the NLRP3 priming step. Surprisingly, caspase-1 also binds cardiolipin at the mitochondria, while ASC was recruited only following NLRP3 activation 67. The binding of both caspase-1 and NLRP3 to mitochondrial cardiolipin validates mitochondria as a scaffold for inflammasome activation, thereby amplifying its activation by bringing molecules together ( Figure 1). In line with this, other immune signalling pathways initiated at the mitochondria, including the MAVS complex, occur in a similar manner 68. Additionally, these studies identify a role for priming beyond the upregulation of NLRP3 and pro-IL-1β.
Endoplasmic reticulum
Endoplasmic reticulum stress triggers caspase-1 activation
NLRP3 has been shown to reside in the ER prior to its activation, and ER dysfunction has been reported to trigger inflammasome activation ( Figure 1). The ER is a membrane-bound organelle that is critical for protein folding, assembly and modification in addition to being the site for lipid synthesis and Ca 2+ homeostasis. Cellular stress leading to accumulation of misfolded or unfolded proteins induces an unfolded protein response (UPR) aimed at restoring ER homeostasis by regulating levels of transcription, translation, and protein folding 69. The UPR response activates several stress sensors located in the ER, including inositol-requiring protein 1 alpha (IRE1α), protein kinase R-like endoplasmic reticulum kinase (PERK), and activating transcription factor 6 (ATF6). These sensors subsequently regulate downstream cytosolic effectors and signalling pathways, including proteasomal degradation, autophagy, and antioxidant defence mechanisms. Prolonged ER stress induces an inflammatory response and cell damage, thereby triggering NLRP3 inflammasome activation 18, 70– 73. An initial study suggested that ER stress activated the NLRP3 inflammasome via a UPR-independent pathway, as short hairpin RNA (shRNA) knock-down of either Ire1α or Perk or macrophages obtained from Atf6α −/− mice released comparable IL-1β following NLRP3 activation 74. However, the authors also noted that not all NLRP3 activators induced ER stress, indicating that this may be just one mechanism by which the NLRP3 inflammasome is activated. In agreement, Bronner et al. found that ER stress and IRE1α were not induced in mouse BMDMs with the canonical NLRP3 activator ATP, although they were induced during Brucella abortus infection 18. During B. abortus infection, IRE1α-initiated mtROS production recruited NLRP3 to mitochondria. Mechanistically, IRE1α activated TXNIP and caspase-2, leading to truncation and activation of the mitochondrial protein Bid, which resulted in mitochondrial damage and release of mitochondrial damage-associated molecular patterns (DAMPs) that promoted NLRP3 activation 18. Surprisingly, NLRP3 was required to activate caspase-2/Bid upstream of mitochondrial damage, suggesting a role for NLRP3 in initiating mitochondrial damage by a feed-forward loop. IRE1α and its activation of TXNIP have been implicated in NLRP3 inflammasome activation in other studies 19, 75– 78. Similarly, inhibition of the ER stress sensor PERK was shown to reduce caspase-1 activation and IL-1β secretion in J744.1 macrophages, although how PERK inhibition decreases NLRP3 activation was not determined 79. Targeting IRE1α to dampen ER stress–induced NLRP3 inflammasome activation has shown benefits in a wide variety of inflammatory conditions 75, 76, 80– 85. These studies again suggest mitochondrial damage as the downstream mechanism by which ER stress initiates NLRP3 inflammasome formation. Additionally, this work may indicate that the ER is the site where NLRP3 activation is initiated before the inflammasome is assembled in the cytosol or at the mitochondria/MAMs.
In addition to being implicated in the activation of the NLRP3 inflammasome, ER stress is thought to play a role in the activation of the NLRP1 inflammasome. NLRP1 expression in HeLa cells is upregulated upon induction of ER stress by tunicamycin and thapsigargin, which inhibit the N-linked glycosylation of proteins and sarcoplasmic/endoplasmic reticulum Ca 2+-ATPase (SERCA) respectively. Upregulation of Nlrp1 involved IRE1α and PERK, and siRNA knock-down of either Ire1α or Perk abrogated increase in NLRP1 expression 86. Consistent with this, studies have shown a link between ER stress and NLRP1 upregulation in leukaemia and cardiovascular injury models 87, 88. Thus, as suggested by studies discussed below, ER seems to be a key subcellular site to regulate inflammasome activation.
Endoplasmic reticulum calcium homeostasis in inflammasome activation
The ER is also the site at which Ca 2+ homeostasis occurs, and Ca 2+ mobilisation has been implicated in NLRP3 inflammasome activation. Blockade of the ER-resident calcium channel IP3R led to reduced NLRP3 inflammasome activation in mouse macrophages 89, 90. Other studies have challenged these claims, showing no role for Ca 2+ and indicating that K + efflux is more important 42, 91. It can be expected that, as with other mechanisms of NLRP3 activation, Ca 2+ mobilisation from the ER activates the NLRP3 inflammasomes only under specific conditions. Similarly, it is possible that Ca 2+ mobilisation precedes ER stress or is a consequence of ER dysfunction and therefore happens to occur alongside ER stress–induced NLRP3 activation.
Endoplasmic reticulum cholesterol levels regulate NLRP3 activation
The ER not only is involved in lipid synthesis but also is the site at which cholesterol levels within the cell are sensed and regulated. Cellular cholesterol homeostasis is achieved by maintaining an equilibrium between de novo synthesis at the ER, exogenous cholesterol uptake in the form of low-density lipoprotein (LDL), and cholesterol efflux programs. LDL is endocytosed by LDL receptor and subsequently trafficked through the endosomal system to other subcellular compartments, including the ER, plasma membrane, and Golgi. Blockade of cholesterol efflux from the lysosome was recently demonstrated to inhibit NLRP3 inflammasome activation in mouse macrophages, an effect attributed to decreased cholesterol within the ER 21. Similarly, inhibition of cholesterol biosynthesis in the ER by exposing cells grown in lipoprotein-deficient media to statins dampened NLRP3 inflammasome activation 21. Additionally, the ER-localised cholesterol-sensing transcription factor sterol regulatory element-binding protein 2 (SREBP2) has been implicated in NLRP3 inflammasome activation 92. The cholesterol metabolite, 25-HC, has also been shown to activate the NLRP3 inflammasome by induction of K + efflux, mtROS production, and activation of the cholesterol transcriptional regulator liver X receptors (LXRs) 93. Thus, either cholesterol may be involved in directly influencing inflammasome complex formation or ER cholesterol content may support NLRP3 in achieving the necessary conformation. Regardless, these studies emphasise a critical role for ER in inflammasome activation.
The Golgi complex
NLRP3 translocation near the Golgi is required for inflammasome activation
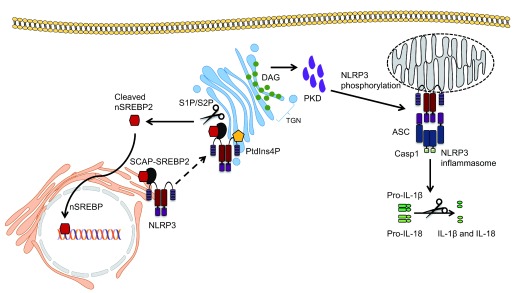
Although roles for mitochondria and ER have been suggested by many labs in the last decade, a few recent studies have also implicated Golgi in inflammasome activation. The Golgi apparatus is important for the modification and transport of proteins and lipids within the cell. Zhang et al. first implicated the Golgi in NLRP3 inflammasome activation. Following treatment with NLRP3 activators, the levels of diacyl glycerol (DAG) at the Golgi increased and this coincided with the localisation of NLRP3 on MAMs adjacent to the Golgi 20. Disruption of Golgi integrity with brefeldin A reduced caspase-1 activation, IL-1β secretion and ASC speck formation following NLRP3 inflammasome activation, a result which was corroborated in a subsequent study 94. This effect was attributed to protein kinase D (PKD), a DAG effector, which phosphorylated NLRP3 at a conserved residue (Ser293) in its NBD domain, allowing its release from MAMs to form an inflammasome complex within the cytosol ( Figure 2). Of note, PKD phosphorylated after NLRP3 self-oligomerised and PKD inactivation both retained self-oligomerised NLRP3 at MAMs and reduced NLRP3 inflammasome activation. Interestingly, PKD inhibition in cells from patients with cryopyrin-associated periodic syndrome (who exhibit spontaneous NLRP3 oligomerisation) also showed reduced NLRP3 activation 20. This added to previous studies that indicate that post-translational modifications can both positively and negatively affect NLRP3 activation 95, 96. Furthermore, this study highlights cross-talk between Golgi and MAMs during NLRP3 inflammasome activation by means of DAG accumulation. In support of this, a recent study demonstrated recruitment of NLRP3 to the trans-Golgi network (TGN) through ionic bonding between NLRP3 and phosphatidylinositol-4-phosphate (PtdIns4P) in the membrane of the Golgi ( Figure 2) 22. The authors found that the TGN dispersed and formed vesicles in the perinuclear space that co-localised with overexpressed NLRP3 following inflammasome activation in HeLa cells. Similar results were shown in primary BMDMs lacking ASC; therefore, whether the full assembly of the inflammasome complex occurs at the TGN was not addressed. However, in that study, in contrast to previous studies, NLRP3 was not found to be associated with mitochondria, and instead the TGN, rather than the mitochondria, provided the scaffold for NLRP3 inflammasome activation 22. Furthermore, translocation of NLRP3 from the ER to the Golgi, this time requiring SREBP and SREBP cleavage-activating protein (SCAP), has also been reported in primary mouse macrophages 92. When cholesterol levels within the cell are low, the SCAP-SREBP2 complex translocates from the ER to the Golgi, where SREBP2 is cleaved into its active form by site-1 protease (S1P) and site-2 protease (S2P), and translocates to the nucleus to transcribe genes involved in cholesterol biosynthesis and uptake 97. The latter study demonstrated that NLRP3 partially co-localises with SCAP-SREBP2 and translocates to the Golgi, and that inhibition of SCAP-SREBP2 translocation abrogated NLRP3 inflammasome activation ( Figure 2). Subcellular fractionation studies showed NLRP3 in the Golgi as well as in the mitochondrial fraction with SCAP. This correlates with findings from Zhang et al., who suggested that NLRP3 activation occurs in close proximity to both the Golgi and the mitochondria 20. Whether multiple mechanisms can independently initiate NLRP3 recruitment to the Golgi requires further work and so does the role of NLRP3 phosphorylation in inflammasome activation.
Figure 2. Emerging role of the Golgi apparatus in NLRP3 inflammasome activation.
NLRP3 localised at the endoplasmic reticulum has been shown to translocate to the Golgi via binding to the SCAP-SREBP2 complex, which regulates cholesterol homeostasis. SREBP2 is cleaved at the Golgi by S1P and S2P to yield the active nuclear form of SREBP2, which then translocates to the nucleus and upregulates genes involved in cholesterol synthesis. NLRP3 has also been shown to be recruited to the TGN through ionic bonds formed with PtdIns4P. The Golgi then acts as a scaffold for NLRP3 assembly. Finally, DAG accumulation at the Golgi recruits and activates PKD, which is required for NLRP3 phosphorylation at the mitochondria, leading to its release and activation at mitochondrial-associated membranes. ASC, apoptosis-associated speck-like protein containing a CARD; DAG, diacylglycerol; IL-1β, interleukin-1 beta; IL-18, interleukin-18; PKD, protein kinase D; PtdIns4p, phosphatidylinositol-4-phosphate; S1P, site-1 protease; S2P, site-2 protease; SREBP2, sterol regulatory element-binding protein 2; TGN, trans-Golgi network.
Concluding remarks
The intracellular milieu of the cell is vital for maintenance of cell function as well as the many cellular processes. Damage to organelles, caused by either endogenous agents or invading pathogens, has been demonstrated to activate NLRP3 inflammasome, leading to pro-inflammatory cytokine release and cell death via pyroptosis. Although a consensus has yet to be reached as to the precise location of the resting NLRP3 and the inflammasome complex, several studies have indicated that NLRP3 translocates to the mitochondria or MAMs following activation ( Table 1). The mitochondria are integral to providing the cell with its source of energy; therefore, it is conceivable that any insult to this compartment is sufficient to be perceived as a danger signal. NLRP3 localisation on or in proximity to mitochondria upon activation supports the notion that it is competently positioned to sense danger signals originating from this organelle. This is backed by the numerous studies demonstrating an association between loss of mitochondrial integrity and NLRP3 inflammasome activation. The direct roles of other subcellular compartments in inflammasome assembly remain to be established, although studies have shown vital roles for ER stress signalling and ER cholesterol content in NLRP3 inflammasome activation. Unravelling the input of distinct organelles in NLRP3 inflammasome assembly will provide crucial insights into how cells sense and coordinate the activation of the NLRP3 inflammasome. This new understanding would enable the development of therapeutics that calibrate NLRP3 activation to maintain cellular homeostasis.
Table 1. Localisation of NLRP3 before and after NLRP3 inflammasome activation.
| Cells and method employed | Resting NLRP3 | Activated NLRP3/NLRP3
inflammasome |
Reference | |
|---|---|---|---|---|
| 1. | THP-1 cells overexpressing FLAG-tagged NLRP3
and ASC Subcellular fractionation and confocal and electron microscopy |
ER and cytosol | MAMs | Zhou et al. 26 (2011) |
| 2. | Peritoneal macrophages from C57BL/6 mice
Immunofluorescence microscopy |
- | Cytosol | Wang et al. 28 (2013) |
| 3. | HEK-293T overexpressing NLRP3 – Confocal
microscopy Wild-type and Asc −/− immortalised BMDMs – Subcellular fractionation |
Cytosol | Mitochondria | Subramanian et al. 30 (2013) |
| 4. | BMDMs – Immunofluorescence microscopy | ER | Mitochondria/ER
(microtubules bring ASC on mitochondria and NLRP3 on ER together) |
Misawa et al. 34 (2013) |
| 5. | BMDMs – Subcellular fractionation and
immunofluorescence microscopy |
- | Mitochondria | Yang et al. 27 (2015) |
| 6. | BMDMs and THP-1 cells – Confocal microscopy | Cytosol | MAMs → cytosol | Zhang et al. 20 (2017) |
| 7. | HeLa cells overexpressing NLRP3 – Subcellular
fractionation and fluorescence microscopy Asc −/− BMDMs – Immunofluorescence microscopy |
Cytosol and
trans-
Golgi network |
Trans-Golgi network | Chen and Chen 22 (2018) |
ASC, apoptosis-associated speck-like protein containing a CARD; BMDM, bone marrow–derived macrophage; ER, endoplasmic reticulum; MAM, mitochondria-associated endoplasmic reticulum membrane.
Acknowledgements
We apologise to the numerous investigators whose work could not be cited due to space limitations.
Editorial Note on the Review Process
F1000 Faculty Reviews are commissioned from members of the prestigious F1000 Faculty and are edited as a service to readers. In order to make these reviews as comprehensive and accessible as possible, the referees provide input before publication and only the final, revised version is published. The referees who approved the final version are listed with their names and affiliations but without their reports on earlier versions (any comments will already have been addressed in the published version).
The referees who approved this article are:
Masafumi Takahashi, Division of Inflammation Research, Center for Molecular Medicine, Jichi Medical University, Tochigi, Japan
Je-Wook Yu, Department of Microbiology and Immunology, Yonsei University College of Medicine, Seoul, South Korea
Rongbin Zhou, Institute of Immunology, School of Life Science, University of Science and Technology of China, Hefei, China
Funding Statement
Research in the laboratory of PA is supported by funds from the Wellcome Trust (108248/Z/15/Z), the Medical Research Council (MR/S00968X/1), and core funds from Imperial College London.
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
[version 1; peer review: 3 approved]
References
- 1. Broz P, Dixit VM: Inflammasomes: mechanism of assembly, regulation and signalling. Nat Rev Immunol. 2016;16(7):407–20. 10.1038/nri.2016.58 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 2. Man SM, Kanneganti TD: Regulation of inflammasome activation. Immunol Rev. 2015;265(1):6–21. 10.1111/imr.12296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mathur A, Hayward JA, Man SM: Molecular mechanisms of inflammasome signaling. J Leukoc Biol. 2018;103(2):233–257. 10.1189/jlb.3MR0617-250R [DOI] [PubMed] [Google Scholar]
- 4. Sharma D, Kanneganti TD: The cell biology of inflammasomes: Mechanisms of inflammasome activation and regulation. J Cell Biol. 2016;213(6):617–29. 10.1083/jcb.201602089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Groslambert M, Py BF: Spotlight on the NLRP3 inflammasome pathway. J Inflamm Res. 2018;11:359–74. 10.2147/JIR.S141220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Liu X, Zhang Z, Ruan J, et al. : Inflammasome-activated gasdermin D causes pyroptosis by forming membrane pores. Nature. 2016;535(7610):153–8. 10.1038/nature18629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Shi J, Zhao Y, Wang K, et al. : Cleavage of GSDMD by inflammatory caspases determines pyroptotic cell death. Nature. 2015;526(7575):660–5. 10.1038/nature15514 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 8. Kayagaki N, Stowe IB, Lee BL, et al. : Caspase-11 cleaves gasdermin D for non-canonical inflammasome signalling. Nature. 2015;526(7575):666–71. 10.1038/nature15541 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 9. Mangan MSJ, Olhava EJ, Roush WR, et al. : Targeting the NLRP3 inflammasome in inflammatory diseases. Nat Rev Drug Discov. 2018;17(8):588–606. 10.1038/nrd.2018.97 [DOI] [PubMed] [Google Scholar]
- 10. Hamilton C, Tan L, Miethke T, et al. : Immunity to uropathogens: the emerging roles of inflammasomes. Nat Rev Urol. 2017;14(5):284–95. 10.1038/nrurol.2017.25 [DOI] [PubMed] [Google Scholar]
- 11. Lupfer C, Anand PK: Integrating Inflammasome Signaling in Sexually Transmitted Infections. Trends Immunol. 2016;37(10):703–14. 10.1016/j.it.2016.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lupfer CR, Anand PK, Liu Z, et al. : Reactive oxygen species regulate caspase-11 expression and activation of the non-canonical NLRP3 inflammasome during enteric pathogen infection. PLoS Pathog. 2014;10(9):e1004410. 10.1371/journal.ppat.1004410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gurung P, Malireddi RK, Anand PK, et al. : Toll or interleukin-1 receptor (TIR) domain-containing adaptor inducing interferon-β (TRIF)-mediated caspase-11 protease production integrates Toll-like receptor 4 (TLR4) protein- and Nlrp3 inflammasome-mediated host defense against enteropathogens. J Biol Chem. 2012;287(41):34474–83. 10.1074/jbc.M112.401406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lukens JR, Kanneganti TD: Beyond canonical inflammasomes: emerging pathways in IL-1-mediated autoinflammatory disease. Semin Immunopathol. 2014;36(5):595–609. 10.1007/s00281-014-0434-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Anand PK, Malireddi RK, Kanneganti TD: Role of the nlrp3 inflammasome in microbial infection. Front Microbiol. 2011;2:12. 10.3389/fmicb.2011.00012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Próchnicki T, Latz E: Inflammasomes on the Crossroads of Innate Immune Recognition and Metabolic Control. Cell Metab. 2017;26(1):71–93. 10.1016/j.cmet.2017.06.018 [DOI] [PubMed] [Google Scholar]
- 17. Gurung P, Lukens JR, Kanneganti TD: Mitochondria: diversity in the regulation of the NLRP3 inflammasome. Trends Mol Med. 2015;21(3):193–201. 10.1016/j.molmed.2014.11.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bronner DN, Abuaita BH, Chen X, et al. : Endoplasmic Reticulum Stress Activates the Inflammasome via NLRP3- and Caspase-2-Driven Mitochondrial Damage. Immunity. 2015;43(3):451–62. 10.1016/j.immuni.2015.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lerner AG, Upton JP, Praveen PV, et al. : IRE1α induces thioredoxin-interacting protein to activate the NLRP3 inflammasome and promote programmed cell death under irremediable ER stress. Cell Metab. 2012;16(2):250–64. 10.1016/j.cmet.2012.07.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Zhang Z, Meszaros G, He WT, et al. : Protein kinase D at the Golgi controls NLRP3 inflammasome activation. J Exp Med. 2017;214(9):2671–93. 10.1084/jem.20162040 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 21. de La Roche M, Hamilton C, Mortensen R, et al. : Trafficking of cholesterol to the ER is required for NLRP3 inflammasome activation. J Cell Biol. 2018;217(10):3560–76. 10.1083/jcb.201709057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Chen J, Chen ZJ: PtdIns4P on dispersed trans-Golgi network mediates NLRP3 inflammasome activation. Nature. 2018;564(7734):71–6. 10.1038/s41586-018-0761-3 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 23. Campden RI, Zhang Y: The role of lysosomal cysteine cathepsins in NLRP3 inflammasome activation. Arch Biochem Biophys. 2019; pii: S0003-9861(18)30811-7. 10.1016/j.abb.2019.02.015 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 24. Hornung V, Latz E: Critical functions of priming and lysosomal damage for NLRP3 activation. Eur J Immunol. 2010;40(3):620–3. 10.1002/eji.200940185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. He Y, Hara H, Núñez G: Mechanism and Regulation of NLRP3 Inflammasome Activation. Trends Biochem Sci. 2016;41(12):1012–21. 10.1016/j.tibs.2016.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Zhou R, Yazdi AS, Menu P, et al. : A role for mitochondria in NLRP3 inflammasome activation. Nature. 2011;469(7329):221–5. 10.1038/nature09663 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 27. Yang CS, Kim JJ, Kim TS, et al. : Small heterodimer partner interacts with NLRP3 and negatively regulates activation of the NLRP3 inflammasome. Nat Commun. 2015;6:6115. 10.1038/ncomms7115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Wang Y, Yang C, Mao K, et al. : Cellular localization of NLRP3 inflammasome. Protein Cell. 2013;4(6):425–31. 10.1007/s13238-013-2113-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Bruchard M, Rebé C, Derangère V, et al. : The receptor NLRP3 is a transcriptional regulator of T H2 differentiation. Nat Immunol. 2015;16(8):859–70. 10.1038/ni.3202 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 30. Subramanian N, Natarajan K, Clatworthy MR, et al. : The adaptor MAVS promotes NLRP3 mitochondrial localization and inflammasome activation. Cell. 2013;153(2):348–61. 10.1016/j.cell.2013.02.054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Seth RB, Sun L, Ea CK, et al. : Identification and characterization of MAVS, a mitochondrial antiviral signaling protein that activates NF-kappaB and IRF 3. Cell. 2005;122(5):669–82. 10.1016/j.cell.2005.08.012 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 32. Park S, Juliana C, Hong S, et al. : The mitochondrial antiviral protein MAVS associates with NLRP3 and regulates its inflammasome activity. J Immunol. 2013;191(8):4358–66. 10.4049/jimmunol.1301170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Li X, Thome S, Ma X, et al. : MARK4 regulates NLRP3 positioning and inflammasome activation through a microtubule-dependent mechanism. Nat Commun. 2017;8:15986. 10.1038/ncomms15986 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 34. Misawa T, Takahama M, Kozaki T, et al. : Microtubule-driven spatial arrangement of mitochondria promotes activation of the NLRP3 inflammasome. Nat Immunol. 2013;14(5):454–60. 10.1038/ni.2550 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 35. Sagulenko V, Thygesen SJ, Sester DP, et al. : AIM2 and NLRP3 inflammasomes activate both apoptotic and pyroptotic death pathways via ASC. Cell Death Differ. 2013;20(9):1149–60. 10.1038/cdd.2013.37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Shimada K, Crother TR, Karlin J, et al. : Oxidized mitochondrial DNA activates the NLRP3 inflammasome during apoptosis. Immunity. 2012;36(3):401–14. 10.1016/j.immuni.2012.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 37. Iyer SS, He Q, Janczy JR, et al. : Mitochondrial cardiolipin is required for Nlrp3 inflammasome activation. Immunity. 2013;39(2):311–23. 10.1016/j.immuni.2013.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Cruz CM, Rinna A, Forman HJ, et al. : ATP activates a reactive oxygen species-dependent oxidative stress response and secretion of proinflammatory cytokines in macrophages. J. Biol. Chem. 2007;282(5):2871–9. 10.1074/jbc.m608083200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Dostert C, Pétrilli V, Van Bruggen R, et al. : Innate immune activation through Nalp3 inflammasome sensing of asbestos and silica. Science. 2008;320(5876):674–7. 10.1126/science.1156995 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 40. Wu J, Yan Z, Schwartz DE, et al. : Activation of NLRP3 inflammasome in alveolar macrophages contributes to mechanical stretch-induced lung inflammation and injury. J Immunol. 2013;190(7):3590–9. 10.4049/jimmunol.1200860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Yu J, Nagasu H, Murakami T, et al. : Inflammasome activation leads to Caspase-1-dependent mitochondrial damage and block of mitophagy. Proc Natl Acad Sci U S A. 2014;111(43):15514–9. 10.1073/pnas.1414859111 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 42. Muñoz-Planillo R, Kuffa P, Martínez-Colón G, et al. : K + efflux is the common trigger of NLRP3 inflammasome activation by bacterial toxins and particulate matter. Immunity. 2013;38(6):1142–53. 10.1016/j.immuni.2013.05.016 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 43. Mohamed IN, Hafez SS, Fairaq A, et al. : Thioredoxin-interacting protein is required for endothelial NLRP3 inflammasome activation and cell death in a rat model of high-fat diet. Diabetologia. 2014;57(2):413–23. 10.1007/s00125-013-3101-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. El-Azab MF, Baldowski BRB, Mysona BA, et al. : Deletion of thioredoxin-interacting protein preserves retinal neuronal function by preventing inflammation and vascular injury. Br J Pharmacol. 2014;171(5):1299–313. 10.1111/bph.12535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Chen W, Zhao M, Zhao S, et al. : Activation of the TXNIP/NLRP3 inflammasome pathway contributes to inflammation in diabetic retinopathy: a novel inhibitory effect of minocycline. Inflamm Res. 2017;66(2):157–66. 10.1007/s00011-016-1002-6 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 46. Zhou R, Tardivel A, Thorens B, et al. : Thioredoxin-interacting protein links oxidative stress to inflammasome activation. Nat Immunol. 2010;11(2):136–40. 10.1038/ni.1831 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 47. Cordero MD, Alcocer-Gómez E, Marín-Aguilar F, et al. : Mutation in cytochrome b gene of mitochondrial DNA in a family with fibromyalgia is associated with NLRP3-inflammasome activation. J Med Genet. 2016;53(2):113–22. 10.1136/jmedgenet-2015-103392 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 48. Tassi S, Carta S, Delfino L, et al. : Altered redox state of monocytes from cryopyrin-associated periodic syndromes causes accelerated IL-1beta secretion. Proc Natl Acad Sci U S A. 2010;107(21):9789–94. 10.1073/pnas.1000779107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Bulua AC, Simon A, Maddipati R, et al. : Mitochondrial reactive oxygen species promote production of proinflammatory cytokines and are elevated in TNFR1-associated periodic syndrome (TRAPS). J Exp Med. 2011;208(3):519–33. 10.1084/jem.20102049 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 50. Nakahira K, Haspel JA, Rathinam VA, et al. : Autophagy proteins regulate innate immune responses by inhibiting the release of mitochondrial DNA mediated by the NALP3 inflammasome. Nat Immunol. 2011;12(3):222–30. 10.1038/ni.1980 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 51. Coll RC, Holley CL, Schroder K: Mitochondrial DNA synthesis fuels NLRP3 inflammasome. Cell Res. 2018;28(11):1046–7. 10.1038/s41422-018-0093-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. West AP, Brodsky IE, Rahner C, et al. : TLR signalling augments macrophage bactericidal activity through mitochondrial ROS. Nature. 2011;472(7344):476–80. 10.1038/nature09973 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 53. Zhong Z, Liang S, Sanchez-Lopez E, et al. : New mitochondrial DNA synthesis enables NLRP3 inflammasome activation. Nature. 2018;560(7717):198–203. 10.1038/s41586-018-0372-z [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 54. Carlos D, Costa FR, Pereira CA, et al. : Mitochondrial DNA Activates the NLRP3 Inflammasome and Predisposes to Type 1 Diabetes in Murine Model. Front Immunol. 2017;8:164. 10.3389/fimmu.2017.00164 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 55. Szeto HH, Liu S, Soong Y, et al. : Mitochondria Protection after Acute Ischemia Prevents Prolonged Upregulation of IL-1 β and IL-18 and Arrests CKD. J Am Soc Nephrol. 2017;28(5):1437–49. 10.1681/asn.2016070761 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 56. Tumurkhuu G, Shimada K, Dagvadorj J, et al. : Ogg1-Dependent DNA Repair Regulates NLRP3 Inflammasome and Prevents Atherosclerosis. Circ Res. 2016;119(6):e76–90. 10.1161/CIRCRESAHA.116.308362 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 57. Lu B, Kwan K, Levine YA, et al. : α7 nicotinic acetylcholine receptor signaling inhibits inflammasome activation by preventing mitochondrial DNA release. Mol Med. 2014;20:350–8. 10.2119/molmed.2013.00117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Liu X, Zhou W, Zhang X, et al. : Dimethyl fumarate ameliorates dextran sulfate sodium-induced murine experimental colitis by activating Nrf2 and suppressing NLRP3 inflammasome activation. Biochem Pharmacol. 2016;112:37–49. 10.1016/j.bcp.2016.05.002 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 59. Yao X, Carlson D, Sun Y, et al. : Mitochondrial ROS Induces Cardiac Inflammation via a Pathway through mtDNA Damage in a Pneumonia-Related Sepsis Model. PLoS One. 2015;10(10):e0139416. 10.1371/journal.pone.0139416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Lupfer C, Thomas PG, Anand PK, et al. : Receptor interacting protein kinase 2-mediated mitophagy regulates inflammasome activation during virus infection. Nat Immunol. 2013;14(5):480–8. 10.1038/ni.2563 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 61. Zhong Z, Umemura A, Sanchez-Lopez E, et al. : NF-κB Restricts Inflammasome Activation via Elimination of Damaged Mitochondria. Cell. 2016;164(5):896–910. 10.1016/j.cell.2015.12.057 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 62. Jabir MS, Hopkins L, Ritchie ND, et al. : Mitochondrial damage contributes to Pseudomonas aeruginosa activation of the inflammasome and is downregulated by autophagy. Autophagy. 2014;11(1):166–82. 10.4161/15548627.2014.981915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Sutterwala FS, Mijares LA, Li L, et al. : Immune recognition of Pseudomonas aeruginosa mediated by the IPAF/NLRC4 inflammasome. J Exp Med. 2007;204(13):3235–45. 10.1084/jem.20071239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Dang EV, McDonald JG, Russell DW, et al. : Oxysterol Restraint of Cholesterol Synthesis Prevents AIM2 Inflammasome Activation. Cell. 2017;171(5):1057–1071.e11. 10.1016/j.cell.2017.09.029 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 65. Lupfer CR, Rippee-Brooks MD, Anand PK: Common Differences: The Ability of Inflammasomes to Distinguish Between Self and Pathogen Nucleic Acids During Infection. Int Rev Cell Mol Biol. 2019;344:139–72. 10.1016/bs.ircmb.2018.10.001 [DOI] [PubMed] [Google Scholar]
- 66. Shi CS, Kehrl JH: Cytochrome c Negatively Regulates NLRP3 Inflammasomes. PLoS One. 2016;11(12):e0167636. 10.1371/journal.pone.0167636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Elliott EI, Miller AN, Banoth B, et al. : Cutting Edge: Mitochondrial Assembly of the NLRP3 Inflammasome Complex Is Initiated at Priming. J Immunol. 2018;200(9):3047–52. 10.4049/jimmunol.1701723 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 68. Mills EL, Kelly B, O'Neill LAJ: Mitochondria are the powerhouses of immunity. Nat Immunol. 2017;18(5):488–98. 10.1038/ni.3704 [DOI] [PubMed] [Google Scholar]
- 69. Bravo R, Parra V, Gatica D, et al. : Endoplasmic reticulum and the unfolded protein response: dynamics and metabolic integration. Int Rev Cell Mol Biol. 2013;301:215–90. 10.1016/B978-0-12-407704-1.00005-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Sano R, Reed JC: ER stress-induced cell death mechanisms. Biochim Biophys Acta. 2013;1833(12):3460–70. 10.1016/j.bbamcr.2013.06.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Chaudhari N, Talwar P, Parimisetty A, et al. : A molecular web: endoplasmic reticulum stress, inflammation, and oxidative stress. Front Cell Neurosci. 2014;8:213. 10.3389/fncel.2014.00213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Shenderov K, Riteau N, Yip R, et al. : Cutting edge: Endoplasmic reticulum stress licenses macrophages to produce mature IL-1β in response to TLR4 stimulation through a caspase-8- and TRIF-dependent pathway. J Immunol. 2014;192(5):2029–33. 10.4049/jimmunol.1302549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Kim S, Joe Y, Jeong SO, et al. : Endoplasmic reticulum stress is sufficient for the induction of IL-1β production via activation of the NF-κB and inflammasome pathways. Innate Immun. 2014;20(8):799–815. 10.1177/1753425913508593 [DOI] [PubMed] [Google Scholar]
- 74. Menu P, Mayor A, Zhou R, et al. : ER stress activates the NLRP3 inflammasome via an UPR-independent pathway. Cell Death Dis. 2012;3:e261. 10.1038/cddis.2011.132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Chen D, Dixon BJ, Doycheva DM, et al. : IRE1α inhibition decreased TXNIP/NLRP3 inflammasome activation through miR-17-5p after neonatal hypoxic-ischemic brain injury in rats. J Neuroinflammation. 2018;15(1):32. 10.1186/s12974-018-1077-9 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 76. Tufanli O, Telkoparan Akillilar P, Acosta-Alvear D, et al. : Targeting IRE1 with small molecules counteracts progression of atherosclerosis. Proc Natl Acad Sci U S A. 2017;114(8):E1395–E1404. 10.1073/pnas.1621188114 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 77. Oslowski CM, Hara T, O'Sullivan-Murphy B, et al. : Thioredoxin-interacting protein mediates ER stress-induced β cell death through initiation of the inflammasome. Cell Metab. 2012;16(2):265–73. 10.1016/j.cmet.2012.07.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Robblee MM, Kim CC, Porter Abate J, et al. : Saturated Fatty Acids Engage an IRE1α-Dependent Pathway to Activate the NLRP3 Inflammasome in Myeloid Cells. Cell Rep. 2016;14(11):2611–23. 10.1016/j.celrep.2016.02.053 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 79. Ando T, Komatsu T, Naiki Y, et al. : GSK2656157, a PERK inhibitor, reduced LPS-induced IL-1β production through inhibiting Caspase 1 activation in macrophage-like J774.1 cells. Immunopharmacol Immunotoxicol. 2016;38(4):298–302. 10.1080/08923973.2016.1192191 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 80. Han CY, Rho HS, Kim A, et al. : FXR Inhibits Endoplasmic Reticulum Stress-Induced NLRP3 Inflammasome in Hepatocytes and Ameliorates Liver Injury. Cell Rep. 2018;24(11):2985–99. 10.1016/j.celrep.2018.07.068 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 81. Guo M, Wang X, Zhao Y, et al. : Ketogenic Diet Improves Brain Ischemic Tolerance and Inhibits NLRP3 Inflammasome Activation by Preventing Drp1-Mediated Mitochondrial Fission and Endoplasmic Reticulum Stress. Front Mol Neurosci. 2018;11:86. 10.3389/fnmol.2018.00086 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 82. Lebeaupin C, Vallée D, Rousseau D, et al. : Bax inhibitor-1 protects from nonalcoholic steatohepatitis by limiting inositol-requiring enzyme 1 alpha signaling in mice. Hepatology. 2018;68(2):515–32. 10.1002/hep.29847 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 83. Hu X, Li D, Wang J, et al. : Melatonin inhibits endoplasmic reticulum stress-associated TXNIP/NLRP3 inflammasome activation in lipopolysaccharide-induced endometritis in mice. Int Immunopharmacol. 2018;64:101–9. 10.1016/j.intimp.2018.08.028 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 84. Li A, Zhang S, Li J, et al. : Metformin and resveratrol inhibit Drp1-mediated mitochondrial fission and prevent ER stress-associated NLRP3 inflammasome activation in the adipose tissue of diabetic mice. Mol Cell Endocrinol. 2016;434:36–47. 10.1016/j.mce.2016.06.008 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 85. Lebeaupin C, Proics E, de Bieville CH, et al. : ER stress induces NLRP3 inflammasome activation and hepatocyte death. Cell Death Dis. 2015;6:e1879. 10.1038/cddis.2015.248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. D'Osualdo A, Anania VG, Yu K, et al. : Transcription Factor ATF4 Induces NLRP1 Inflammasome Expression during Endoplasmic Reticulum Stress. PLoS One. 2015;10(6):e0130635. 10.1371/journal.pone.0130635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Xu Z, Wang H, Wei S, et al. : Inhibition of ER stress-related IRE1α/CREB/NLRP1 pathway promotes the apoptosis of human chronic myelogenous leukemia cell. Mol Immunol. 2018;101:377–85. 10.1016/j.molimm.2018.07.002 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 88. Cao L, Chen Y, Zhang Z, et al. : Endoplasmic Reticulum Stress-Induced NLRP1 Inflammasome Activation Contributes to Myocardial Ischemia/Reperfusion Injury. Shock. 2019;51(4):511–8. 10.1097/SHK.0000000000001175 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 89. Murakami T, Ockinger J, Yu J, et al. : Critical role for calcium mobilization in activation of the NLRP3 inflammasome. Proc Natl Acad Sci U S A. 2012;109(28):11282–7. 10.1073/pnas.1117765109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Lee GS, Subramanian N, Kim AI, et al. : The calcium-sensing receptor regulates the NLRP3 inflammasome through Ca 2+ and cAMP. Nature. 2012;492(7427):123–7. 10.1038/nature11588 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 91. Katsnelson MA, Rucker LG, Russo HM, et al. : K + efflux agonists induce NLRP3 inflammasome activation independently of Ca 2+ signaling. J Immunol. 2015;194(8):3937–52. 10.4049/jimmunol.1402658 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 92. Guo C, Chi Z, Jiang D, et al. : Cholesterol Homeostatic Regulator SCAP-SREBP2 Integrates NLRP3 Inflammasome Activation and Cholesterol Biosynthetic Signaling in Macrophages. Immunity. 2018;49(5):842–856.e7. 10.1016/j.immuni.2018.08.021 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 93. Jang J, Park S, Jin Hur H, et al. : 25-hydroxycholesterol contributes to cerebral inflammation of X-linked adrenoleukodystrophy through activation of the NLRP3 inflammasome. Nat Commun. 2016;7:13129. 10.1038/ncomms13129 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 94. Hong S, Hwang I, Gim E, et al. : Brefeldin A-sensitive ER-Golgi vesicle trafficking contributes to NLRP3-dependent caspase-1 activation. FASEB J. 2019;33(3):4547–58. 10.1096/fj.201801585R [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 95. Stutz A, Kolbe CC, Stahl R, et al. : NLRP3 inflammasome assembly is regulated by phosphorylation of the pyrin domain. J Exp Med. 2017;214(6):1725–36. 10.1084/jem.20160933 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 96. Spalinger MR, Kasper S, Gottier C, et al. : NLRP3 tyrosine phosphorylation is controlled by protein tyrosine phosphatase PTPN22. J Clin Invest. 2016;126(5):1783–800. 10.1172/JCI83669 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 97. Brown MS, Goldstein JL: Cholesterol feedback: from Schoenheimer's bottle to Scap's MELADL. J Lipid Res. 2009;50 Suppl:S15–27. 10.1194/jlr.R800054-JLR200 [DOI] [PMC free article] [PubMed] [Google Scholar]