Abstract
Purpose
Overweight and obese adolescents are at risk for low health-related quality of life (HRQOL). We examined the role of individual- and environmental-level variables on the relationship between body mass index (BMI kg/m2) and HRQOL in adolescents.
Methods
Linear regressions were performed to conduct mediation and moderation analyses on the relationship between BMI and HRQOL in overweight and obese adolescents (N = 205). HRQOL was measured by the Pediatric Quality of Life Inventory. Hypothesized mediators included depression, measured by the Center for Epidemiologic Studies Depression Scale; body image, measured by the gender-specific body dissatisfaction subscale of the Eating Disorder Inventory; and self-esteem, measured by the Rosenberg Self-Esteem Scale. Mediation was assessed using Baron and Kenny’s approach and Sobel’s test of indirect effects. Anglo-acculturation, measured by the Short Acculturation Scale for Hispanics-Youth, and environmental perception, measured by parent-proxy report of the Neighborhood Environment Walkability Scale, were hypothesized moderators.
Results
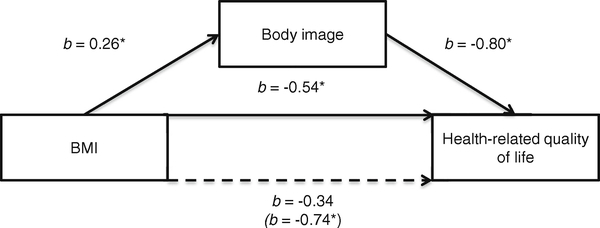
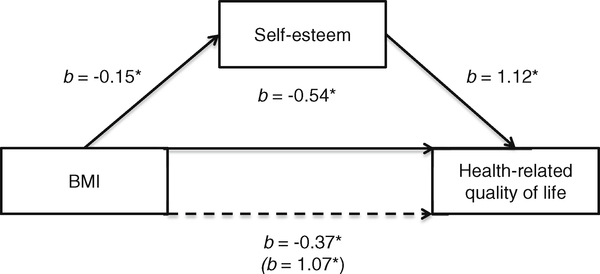
Body image mediated the relationship between BMI and HRQOL (b = −0.34, SE = 0.17, adj R2 = 0.19, p = .051), and self-esteem was a partial mediator (b = −0.37, SE = 0.17, adj R2 = 0.24, p = .027). Sobel’s test confirmed these results (p < .05). No significant moderation effects were found.
Conclusions
The finding that individual-level factors, such as body image and self-esteem, influence the relationship between BMI and HRQOL while environmental factors, such as neighborhood environment and acculturation, do not extends previous research. The finding that body image and self-esteem partially mediate this relationship presents new areas to investigate in interventions that address BMI in youth.
Keywords: Overweight, Obesity, Adolescent, Self-esteem, Body image, Depression
Introduction
Adolescent overweight and obesity continues to affect US youth, with approximately one-third of adolescents aged 12–19 overweight or obese in 2009–2010 [1]. Moreover, the prevalence is higher among Mexican American adolescents (43.4 %) compared to white non-Hispanic adolescents (30 %), which suggests racial disparities [1]. Research has shown that health-related quality of life (HRQOL) in obese adolescents is significantly lower than their normal-weight cohorts [2–6]. A meta-analysis of Body Mass Index (BMI) and HRQOL in children and adolescents also supports these findings as it showed that both physical and psychosocial dimensions of HRQOL are lower for obese children and adolescents [7].
The Centers for Disease Control and Prevention define HRQOL as a multidimensional concept focusing on how a person’s health affects his or her physical, mental, social, and emotional functioning [8]. Recent calls in public health have emphasized the need to focus on improving HRQOL among all individuals. In the Healthy People 2020 report, the importance of QOL measures was acknowledged by making HRQOL one of the four foundation health measures used to indicate progress toward achieving the overarching goals [9]. Similarly, the National Institute of Health’s strategic plan for obesity research includes QOL as an important outcome for intervention research [10].
The social ecological model posits that an individual’s health is influenced by proximal and distal factors including individual, interpersonal, community, and societal levels [11]. To understand the relationship between HRQOL and childhood obesity, it may be important to examine multiple levels of influence to work toward developing more comprehensive models.
Research with adults has examined how individual-level factors such as depression, self-esteem, self-efficacy, coping style, body image, sense of coherence, and emotional well-being are related to obesity and HRQOL [12–14]. As adolescents transition from childhood to adulthood, they are at particular risk for depression, declining body imagine, and low self-esteem, so it is important to examine HRQOL in the context of obesity and obesity interventions in this population [15–17]. Previous research with children and adolescents has found that depression and lower self-esteem are negatively related to HRQOL [18, 19]. Body image dissatisfaction also has been correlated with low QOL scores, and there is a negative association with overweight and obesity and body image [20, 21]. Overall, these psychosocial factors may play an important role in adolescent HRQOL. Furthermore, not only do Hispanic adolescents have higher rates of overweight and obesity, but also they report higher levels of depression [22], poorer body image [23], and lower self-esteem [24] than non-Hispanic whites and Asians. This suggests that it may be important to examine how and whether these psychosocial variables influence the relationship between BMI and HRQOL among Hispanic youth.
Environmental-level variables examined in past obesity research have been diverse and included the neighborhood, home, and school [25]. The present study, however, specifically focuses on the neighborhood environment and walkability, aspects of the built environment. Past research has found components of the built environment associated with obesity [26]. In particular, walkability, which includes quantifying the safety and desirability of walking routes within a neighborhood [27], has been related to higher levels of physical activity and a lower risk of being overweight or obese [28].
The built environment also is associated with HRQOL. The Danish National Institute of Public Health found people who lived farther from green space reported lower HRQOL scores than people who lived closer to green spaces [29]. Another study found parents who reported living in neighborhoods rated as safe and having access to parks and other recreational opportunities had children who reported higher HRQOL [30].
The relationship between the built environment, obesity, and QOL is exacerbated in disadvantaged populations. Individuals from lower SES neighborhoods reported poorer health, suggesting that these individuals endured more uncontrollable environmental stressors such as crowding, noise, crime, and threats to personal safety [31]. Furthermore, one possible explanation for why disadvantaged populations have high rates of obesity is that they tend to live in areas lacking aspects of health-promoting built environments (e.g., access to grocery stores and exercise facilities) [32].
Culture is also an important type of environmental factor. Previous research on HRQOL scores among Hispanic and white non-Hispanic children suggests acculturation may have a stronger negative effect on HRQOL scores than ethnicity [33]. Acculturation also is associated with obesity in Hispanic populations [34, 35]. In fact, previous cross-sectional research has found that acculturation was the strongest correlate of obesity, even stronger than physical activity and diet [34]. However, more work is needed to assess how acculturation interacts with other potential contributors of obesity and HRQOL in a Hispanic population.
The present study assessed the relationship of BMI and HRQOL within a predominantly Hispanic overweight and obese adolescent population. Psychosocial factors were tested as mediators, and acculturation and environmental factors were tested as moderators. It was hypothesized that: (1) BMI and HRQOL will be negatively associated; (2) psychosocial variables (i.e., depression, body image, and self-esteem) may be a mechanism driving the relationship between BMI and HRQOL; and (3) built environment factors and acculturation may affect the strength of the relationship between BMI and HRQOL.
Methods
Participants
Baseline data were merged from 2 intervention trials that aimed to reduce weight in overweight or obese adolescents by intervening in physical activity and nutrition behaviors (merged sample N = 205). The Primary Care Management of Adolescent Obesity (PACE-PC) study was a 12-month randomized controlled trial that aimed to reduce BMI in obese adolescents using a computer-supported intervention initiated in primary healthcare settings (N = 106) (under review, Norman et al., 2013). The Intervention for Youth at Risk for Diabetes (PACE-iDP) study was a 12-month randomized controlled trial that aimed to reduce BMI in overweight or obese adolescents at risk for type 2 diabetes through technology-based modalities (i.e., Web sites, text-messaging) (N = 99) [36]. Participants in both studies included one adolescent and one parent or guardian. Consent from both individuals was obtained. Ethical approval for both studies was obtained from participating healthcare organizations and University of California, San Diego, human subjects review board.
PACE-PC participants and recruitment
Obese (BMI > 95 percentile for age and gender) adolescents aged 11–13 were recruited through their primary care providers between February 2008 and November 2009. Three sites within the Children’s Primary Care Medical Group in Chula Vista, California, agreed to participate in the study. Participants were primarily recruited at the recommendation of their pediatricians during routine visits. Study information also was distributed through flyers placed in office waiting rooms and through physician-generated letters mailed to patients’ homes. In addition to meeting criteria for obesity, it was required that participants were literate in English, planned to be a San Diego County resident for the next year, had a parent or guardian willing to participate, were willing to return to the physician office for counseling sessions, and were able to attend measurement visits. Parents were eligible if they were literate in English or Spanish. Adolescents were excluded if they did not have reliable transportation, were taking or had previously taken (within 6 months of study inititaion) weight-altering medications, were unable to do moderate-to-vigorous physical activity, weighed more than 77.7 kg, were living in foster care, were receiving special needs education, was a previous participant in our weight loss studies, was currently enrolled in a weight loss program, or had been diagnosed with obesity-related disorders requiring immediate weight loss management or diseases of the liver, pancreas, or small intestine affecting absorption or processing of nutrients.
Upon completion of an initial phone screening for eligibility with the adolescent and parent, a 2-week screening program was conducted. During the 2-week run-in program, the adolescent-parent dyads were asked to perform some of the activities that would be required of them if they were enrolled in the intervention trial (independent of randomization assignment). These tasks included: (1) attending a measurement visit; (2) scheduling and completing a phone call with a study staff member; (3) locating a food item at home, reading the food label, and describing the nutrition content; (4) tracking basic food intake and physical activity in a written diary over 4 days; and (5) scheduling and attending a follow-up appointment. Following successful completion of the program, eligible participants and their parents were invited to a baseline measurement visit.
PACE-iDP participants and recruitment
Eighteen pediatric practices in San Diego, California, were recruited to participate as the primary provider sites for recruitment into the study, twelve of which served economically and ethnically diverse adolescent patient populations. Providers were asked to identify potential at-risk patients aged 12–16 due for their annual visit or who had an existing appointment for a physical examination or well-visit. Study information was also distributed via local media, and fliers were posted in waiting rooms. The recruitment period was between February 2006 and March 2008.
Eligible adolescents were ages 12–16 and at “high-risk” for diabetes. High risk was defined by the American Diabetes Association expert consensus panel [37] as overweight (BMI > 85th percentile for age and sex, weight for height > 85th percentile, or weight > 120 % ideal for height) plus two of the following risk factors: family history of type 2 diabetes in a first- or second-degree relative, race/ethnicity, or signs of insulin resistance. Other inclusion criteria for both the participant and parent included access to the Internet, a functioning telephone, literacy in English (for adolescent) or English or Spanish (for the parent), and willingness to participate in online activities and attend monthly group sessions. Patients were excluded if they had a diagnosis of diabetes, were pregnant, were planning to leave San Diego during the study, or had a medical condition that would prevent them from participating in the intervention.
Measures
Demographics were collected by self-report. Categorical information was based on categories predefined by investigators. The following information was collected: age, gender (male, female), education (≤high school, high school degree, trade/technical/some college, or college graduate/graduate degree), income (<$24,999, $25,000–$49,999, $50,000–$100,000, or prefer not to state/did not state), and race/ethnicity (Hispanic, White non-Hispanic, African American, other, or prefer not to state/did not state).
BMI was calculated as kg/m2. Height was measured without shoes using a stadiometer, and weight was measured using a calibrated digital scale. Measurement staff took the average of the 2 readings for both height and weight. BMI was correlated highly with BMI percentile and BMI z-scores (Spearman correlation for both measures = 0.86, p < .001). Therefore, BMI was used in this analysis because it is more interpretable.
HRQOL was measured using the 23-item Pediatric Quality of Life Inventory [38]. It measures the previous month’s physical, emotional, social, and school functioning aspects of HRQOL. Respondents were asked rate their response to each item using a 5-point scale ranging from “never” to “almost always”. Items were reverse scored and linearly transformed to a 0–100 scale. Item scores were summed to obtain a total summary score, with higher scores indicating better HRQOL. This measure has been shown to be valid and reliable, with a high Cronbach’s alpha (α = 0.91) [38]. In the current sample, Cronbach’s alpha was α = 0.89.
Depression was measured using the 10-item Center for Epidemiologic Studies Depression Scale short form, a questionnaire that assesses depressive symptoms in the general population [39]. For each item, respondents are asked to rate the frequency of their reactions within the last week using a 4-point Likert scale ranging from “rarely” to “all of the time”. Positively worded items were reverse-coded, each item was weighted, and item weighted scores were summed. Scores range from 0–30. Scores between 0–11 indicate “minimal” depressive symptoms, 12–20 indicate “somewhat elevated” depressive symptoms, and 21–30 indicate “very elevated” depressive symptoms [40]. In youth, this measure has shown acceptable a Cronbach’s alpha value (α = 0.85) and discriminative and construct validity [39, 40]. In the current sample, Cronbach’s alpha was α = 0.71.
Body image was measured using the 9-item gender-specific body dissatisfaction subscale of the Eating Disorder Inventory [41, 42]. Respondents were asked to rate the frequency of time spent thinking about various parts of their body on a 5-point Likert scale ranging from “always” to “never”. This questionnaire included 6 gender-specific items and 3 gender-neutral items. Responses to each item were weighted and summed. Scores range from 0–27, with lower scores indicating high levels of body dissatisfaction. The scale demonstrated sensitivity to treatment in addition to acceptable Cronbach’s alpha and 1-week test–retest for Female Concerns (α = 0.90, r = 0.87) and Male Concerns (α = 0.75, r = 0.82) was acceptable [42]. The Eating Disorder Inventory has been determined to be reliable for use with children as young as age 8 [42]. In the current sample, Cronbach’s alpha for girls was α = 0.82, and for boys it was α = 0.68.
Self-esteem was measured via the 10-item Rosenberg Self-Esteem Scale [43]. Responses were rated on a 4-point Likert scale ranging from “strongly disagree” to “strongly agree”. Negatively worded items were reversed scored, and items were summed. Scores range from 0–40, with higher scores indicating higher self-esteem. This scale is the most widely used measure of global self-esteem and has been determined to be reliable and valid among youth samples, including showing good internal consistency (α = 0.81) [44]. In the current sample, Cronbach’s alpha was α = 0.81.
Environmental variables were measured using the Neighborhood Environment Walkability Scale, a questionnaire that assesses perceptions of the environment [47]. The current study used 56 items from 7 subscales (i.e., land use mix-diversity, land use mix-access, street connectivity, infrastructure and safety for walking/cycling, neighborhood esthetics, pedestrian/automobile traffic safety, and crime safety). Land use mix-diversity was based on a 1 (1–5 min-walk) to 5 (≥30 min-walk) scale and assessed walking proximity from home to various types of stores and facilities. Responses were averaged, and scores ranged from 1–5, with higher scores indicating closer proximity. Responses for the other subscales were rated on a 4-point Likert scale ranging from “strongly disagree” to “strongly agree”. Responses were averaged, and scores ranged from 1–4, with higher scores indicating more favorable environmental surroundings. This measure demonstrated acceptable test-retest (R = 0.63–0.80) and validity [47]. In the current sample, Cronbach’s alpha values were as follows: land use mix-diversity (α = 0.94), land use mix-access (α = 0.66), street connectivity (α = 0.43), infrastructure and safety for walking/cycling (α = 0.56), neighborhood esthetics (α = 0.84), pedestrian/automobile traffic safety (α = 0.34), and crime safety (α = 0.80).
Acculturation was measured using 4 “language-use” items from a modified version of Short Acculturation Scale for Hispanics-Youth [45] as these were the only 4 items assessed in both PACE-PC and PACE-IDP. The following 4 items were used: (1) “In general, what language(s) do you read and speak?”, (2) “In what language(s) do you usually speak at home?”, (3) “In what language(s) do you usually think?”, and (4) “What language(s) do you usually speak with your friends?” Responses were rated on a 5-point Likert scale and were as follows: (1) only Spanish, (2) more Spanish than English, (3) both equally, (4) more English than Spanish, and (5) only English. Responses were averaged, and scores ranged from 1–4, with higher scores reflecting more Anglo-acculturation. An average of 2.99 is recommended to differentiate less acculturated respondents from more acculturated respondents. Reliability and validity for the 4 language-use items have not been determined. However, the modified version of the SASH-Y used in this study has demonstrated strong internal consistency (α = 0.89), test–retest reliability (70.8 % agreement), and criterion validity by parent report (90.3 % agreement) [46]. In the current sample, Cronbach’s alpha was α = 0.87.
Statistical analysis
Linear regressions were performed to conduct mediation and moderation analyses on the relationship between BMI and HRQOL using a merged sample of adolescents from the PACE-PC and PACEiDP studies. SAS version 9.0 was used to conduct statistical analyses. Mediation was assessed using Baron and Kenny’s 4-step approach [48]. For each hypothesized mediator, 4 regressions were conducted that assessed relationships between BMI and HRQOL. The hypothesized mediators were depression, body image, and self-esteem. Sobel’s test was used to assess indirect effects of the mediation models [49]. The hypothesized moderators were acculturation and environmental variables.
We chose the mediators and moderators based on the conceptual relationship between these variables [50]. Depression, body image, and self-esteem were hypothesized mediators because they are conceptualized as in the “causal path” from BMI to HRQOL. That is, it was hypothesized that BMI works through depression to affect HRQOL. Moderators are conceptualized as factors that can change the magnitude and direction of a relationship and are not in the causal path. For example, the presence or absence of particular environmental conditions was hypothesized to influence the relationship between BMI and HRQOL differentially. Although these analyses were conducted with a cross-section of data, we specified the hypothesized mediator or moderator relationship based on these conceptual relationships.
Correlations and ANOVAs were conducted with the HRQOL variable to determine appropriate covariates to include in multivariate models. T tests and chi-square tests were performed to assess if there were significant differences between demographic variables before merging the 2 samples (p < .05). Variables significantly related to the outcome measure at p < .10 level were included. Variables were assessed for co-linearity, and variables correlated >.50 were excluded.
Linear regression models were used to examine the mediating and moderating effects (significant at p < .05). Non-normal dependent variables were transformed. If the covariate was significantly related to the dependent variable or changed the parameter estimate(s) by >10 %, it was retained in the model. Total effects and indirect effects were calculated.
Results
Descriptive statistics
Tables 1 and 2 display descriptive statistics for demographics and individual and environmental variables. Most participants were female, Hispanic, and had a household income of <$25,000. Mean age for the merged sample was 13. Participants’ parents had approximately equal levels of education. There were no significant differences between data from the PACE-PC and PACE-iDP samples, with the exception of the following: age was higher in the iDP sample (mean = 13.8, SD = 1.57) versus the PC sample (mean = 12.1, SD = 0.94) (t = 9.78, SE = 0.15, p < .001), BMI was higher in the iDP sample (mean = 33.9, SD = 4.9) versus the PC sample (mean = 29.3, SD = 3.9) (t = 7.44, SE = 0.49, p < .001), and 93 % of the PC sample had a household income level of <$25,000 versus 38 % in the iDP sample (χ2 = 0.34, p < .0001). Based on cutoff scores from published literature [40, 45], on average, participants did not display depressive symptoms and were Anglo-acculturated. Participants also had high HRQOL (mean 77.8, range 38.0–100.0), high self-esteem (mean 31.1, range 16.0–40.0), and low body image (mean 8.83, range 0.0–26.0).
Table 1.
Demographic characteristics of the PACE-PC and PACE-iDP adolescents (N = 205)
| Characteristics | Merged samplea |
|---|---|
| Age at study entry in years, mean (SD) | 12.9 (1.54) |
| BMI (kg/m2), mean (SD) | 31.6 (5.0) |
| BMI percent over mean, mean (SD) | 67.9 (23.93) |
| Female, N (%) | 118 (57.6) |
| Race/ethnicity, N (%) | |
| Hispanic | 159 (77.6) |
| White non-Hispanic | 15(7.3) |
| African American | 15 (7.3) |
| Other | 7 (3.4) |
| Prefer not to state/did not state | 9 (4.4) |
| Parent income, N (%) | |
| < $24,999 | 131 (63.9) |
| $25,000–$49,999 | 34 (16.6) |
| $50,000–$100,000 | 25 (12.2) |
| Prefer not to state/did not state | 15 (7.3) |
| Parent education, N (%) | |
| ≤ High school | 45 (22.0) |
| High school degree | 37 (18.0) |
| Trade/technical/some college | 69 (33.7) |
| College graduate/graduate degree | 53 (25.9) |
Percentages are rounded, and therefore, some categories may not equal 100 %
Table 2.
Descriptive statistics of the individual- and environmental-level variables of the PACE-PC and PACE-iDP adolescents in a merged sample
| Variables | N | Mean | SD | Median | Min | Max |
|---|---|---|---|---|---|---|
| Psychosocial | ||||||
| HRQOL | 205 | 77.82 | 12.86 | 79.35 | 38.00 | 100.00 |
| Physical functioning subscale | 204 | 80.53 | 14.46 | 81.25 | 21.90 | 100.00 |
| Emotional functioning subscale | 204 | 72.11 | 17.91 | 75.00 | 15.00 | 100.00 |
| Social functioning subscale | 205 | 80.71 | 18.25 | 85.00 | 10.00 | 100.00 |
| School functioning subscale | 205 | 76.04 | 16.53 | 75.00 | 15.00 | 100.00 |
| Depression | 205 | 6.23 | 4.04 | 5.00 | 0.00 | 20.00 |
| Body image | 205 | 8.83 | 5.86 | 8.00 | 0.00 | 26.00 |
| Self-esteem | 205 | 31.11 | 4.87 | 31.00 | 16.00 | 40.00 |
| Environmental | ||||||
| Land use mixed diversity | 201 | 2.67 | 0.90 | 3.00 | 1.00 | 5.00 |
| Land use mixed accessibility | 201 | 3.03 | 0.78 | 2.56 | 1.00 | 4.00 |
| Street connectivity | 201 | 2.88 | 0.84 | 3.00 | 1.00 | 4.00 |
| Safety for walking/biking | 201 | 2.83 | 0.64 | 3.00 | 1.00 | 4.00 |
| Esthetics | 198 | 2.72 | 0.81 | 2.75 | 1.00 | 4.00 |
| Traffic | 198 | 2.60 | 0.59 | 2.67 | 1.00 | 4.00 |
| Crime | 198 | 1.86 | 0.85 | 1.67 | 1.00 | 4.00 |
| Acculturation | 203 | 3.11 | 0.79 | 2.57 | 1.25 | 4.00 |
HRQOL health-related quality of life
Mediation analyses
Bivariate analyses revealed HRQOL was significantly related to female gender (r = −0.16, p < .05), parent’s education (ρ = 0.14, p < .05), and race/ethnicity (F(4, 200) = 3.64, p < .05). Only race/ethnicity was significantly related to HRQOL in the first multivariate model (Table 3). Therefore, we adjusted for this variable in the other multivariate models as well.
Table 3.
Final linear regression model for the cross-sectional analysis of the relationship between body mass index (BMI) and health-related quality of life (HRQOL) in the PACE-PC and PACE-iDP adolescents merged sample (N = 205)
| HRQOL on BMI | Betaa (SE) | Adj R2 | SS error | DF error | p value |
|---|---|---|---|---|---|
| BMI (kg/m2) | −0.54**(0.18) | 0.08 | 30105.00 | 199 | .004 |
| Covariates | |||||
| Race/ethnicity | |||||
| Hispanic | 11.82** (4.22) | .006 | |||
| White non-Hispanic | 16.68** (5.19) | .002 | |||
| African American | 9.57 (5.33) | .074 | |||
| Other race | 17.43** (6.20) | .005 |
Prefer not to state/did not state (reference)
SE standard error, Adj adjusted, SS sum of squares, DF degrees of freedom
p < .05
p < .01
Unstandardized parameter estimate
As our linear regression results suggested, BMI was significantly related to HRQOL. We proceeded to test the mediator variables. In the first mediation analysis, BMI to HRQOL (b = −0.54, SE = 0.18, adj R2 = 0.08, p = .004) and depression to HRQOL (b = −1.63, SE = 0.19, adj R2 = 0.31, p < .0001) were significant. However, because BMI to depression was not significant (b = 0.80, SE = 0.06, adj R2 = 0.02, p = .175), we did not perform the fourth mediation step.
Figure 1 depicts the mediation model from BMI to HRQOL, BMI to body image (b = 0.26, SE = 0.08, adj R2 = 0.04, p = .002), body image to HRQOL (b = −0.80, SE = 0.14, adj R2 = 0.18, p < .0001), and BMI to HRQOL (b = −0.34, SE = 0.17, adj R2 = 0.19, p = .051), controlling for body image (b = −0.74, SE = 0.14, p < .0001). This figure illustrates complete mediation, as the relationship between BMI and HRQOL was no longer significant after controlling for body image. Sobel’s test confirmed these results (t = −2.82, SE = 0.07, p = .005). The total effect equaled −0.75, and the indirect effect equaled −0.21, indicating the indirect path explained 28.0 % of the total effect.
Fig. 1.
Regression models of the relationship among BMI, body image, and health-related quality of life in adolescents that support complete mediation. Unstandardized beta values for BMI are presented (*p < .05). Solid lines represent direct paths, and dotted lines represent the mediated path. The beta value in parentheses is the parameter estimate for the relationship between body image and health-related quality of life when controlling for BMI
Figure 2 depicts the mediation model from BMI to HRQOL, BMI to self-esteem (b = −0.15, SE = 0.07, adj R2 = 0.02, p = .032), self-esteem to HRQOL (b = 1.12, SE = 0.16, adj R2 = 0.23, p < .0001), and BMI to HRQOL (b = −0.37, SE = 0.17, adj R2 = 0.24, p = .027), controlling for self-esteem (b = 1.07, SE = 0.16, p < .0001). This figure portrays partial mediation, as the relationship between BMI and HRQOL remained significant after controlling for self-esteem. Sobel’s test confirmed these results (t = −2.05, SE = 0.08, p = .040). The total effect equaled −0.71, and the indirect effect equaled −0.17, indicating the indirect path explained 23.9 % of the total effect.
Fig. 2.
Regression models of the relationship among BMI, self-esteem, and health-related quality of life in adolescents that support partial mediation. Unstandardized beta values for BMI are presented (*p < .05). Solid lines represent direct paths, and dotted lines represent the mediated path. The beta value in parentheses is the parameter estimate for the relationship between self-esteem and quality of life when controlling for BMI
Moderation analyses
In the moderation analyses, gender was controlled for as this variable was either significantly related to HRQOL or affected parameter estimates by >10 %. None of the variables in these models displayed multicollinearity. Acculturation (b = −0.11, SE = 0.23, adj R2 = 0.05, p = .63), land use mixed diversity (b = 0.02, SE = 0.21, adj R2 = 0.05, p = .92), land use mixed accessibility (b = 0.42, SE = 0.21, adj R2 = 0.11, p = .05), street connectively (b = −0.19, SE = 0.23, adj R2 = 0.05, p = .40), safety for walking/biking (b = −0.40, SE = 0.27, adj R2 = 0.09, p = .15), aesthetics (b = −0.13, SE = 0.21, adj R2 = 0.06, p = .52), traffic (b = −0.36, SE = 0.28, adj R2 = 0.07, p = .20), and crime (b = −0.19 SE = 0.21, adj R2 = 0.06, p = .35) were not significantly related to HRQOL.
Discussion
As hypothesized, there was an inverse association between BMI and HRQOL. Body image and self-esteem partially mediated the relationship between BMI and HRQOL. Depression was not found to be a mediator. Acculturation and environmental variables were not found to be moderators. Study findings indicate that psychosocial variables, such as body image and self-esteem, influence the relationship between BMI and HRQOL in adolescents, while environmental variables do not. To our knowledge, this is the first study to explore the mediation and moderation of individual- and environmental-level influences on the relationship between BMI and HRQOL in adolescents.
The result that body image was associated with BMI and HRQOL and mediates the relationship between BMI and HRQOL is consistent with previous research [20, 21, 51, 52]. One study in obese and normal-weight children, using a measure that separated assessment of psychosocial and physical aspects of QOL, found that body image was a mediator in the relationship between BMI and psychosocial QO [51]. However, the study did not find BMI to be associated with physical QOL. The present study begins to build a case for the mediating relationship between BMI and HRQOL, extending the mediation to include both physical and psychosocial aspects of HRQOL. More research is needed to confirm this relationship and determine whether it may be an important intervention target in improving HRQOL for overweight or obese adolescents.
The association of self-esteem with BMI and HRQOL is consistent with previous research [53, 54]. Additionally, self-esteem as a partial mediator of the relationship between BMI and HRQOL is also consistent with the literature. Previous research indicates that in obese adolescents low self-esteem was associated with lower QOL scores, while also finding self-esteem was a partial mediator of the relationship between weight-related teasing and QOL [54]. Although weight-related teasing is probably not universally experienced by adolescents with a high BMI and may result in additional psychosocial trauma, the mediating relationship found in this previous study hints at the findings of the present study in which self-esteem partially mediates the relationship between BMI and HRQOL.
The finding that depression was associated with HRQOL is congruent with the literature [4]. Similar to previous research [55, 56], the current study did not find a significant relationship between BMI and depression. Prior studies have found that self-perception of weight had a stronger association with depression than actual weight status [55]. Previous findings coupled with results from this study suggest that obesity is not a predictor of depression, but indicate that depression is an important factor associated with HRQOL.
Prior research has identified relationships between environmental factors and BMI and HRQOL separately but has not explored moderation of this relationship by environmental factors [29, 30]. Thus, the finding that the relationship between BMI and HRQOL was not moderated by environmental variables provides new insight and suggests that environmental factors may not influence the relationship between BMI and HRQOL. However, because the present study conceptualized environment as the neighborhood environment and walkability, there may be additional aspects of the environment (i.e., food environment) that, if included, may have moderated the relationship between BMI and HRQOL.
Past research has found acculturation influences HRQOL but has not explored the influence of acculturation on the relationship between BMI and HRQOL [33]. The finding that acculturation did not moderate the relationship between BMI and HRQOL provides new information about this relationship. However, this sample also was negatively skewed and included more highly acculturated adolescents, which may have biased the results. Future studies should strive for a diverse sample with equal amounts of low- and high-acculturated adolescents to examine the relationship acculturation has on BMI and HRQOL. Additionally, because the present study conceptualized acculturation as language use, there may be additional aspects of acculturation (i.e., time in resident country) that, if included, may have moderated the relationship between BMI and HRQOL.
Several study limitations should be noted. The study aimed to examine the influences of different levels of the SEM model on the relationship between BMI and HRQOL. However, the measure of environment was limited to the neighborhood environment and walkability. A more comprehensive measure of the environment may have found a moderating relationship between HRQOL and BMI. Additionally, interpersonal variables, such as social support [57] and school/social functioning [58], were not available for both samples and therefore were not included in the analyses. The sample was limited to predominantly Hispanic youth in San Diego County, which may not be indicative of Hispanic youth in other regions. Additionally, only treatment-seeking youth participated in the studies, which do not include overweight and obese youth who may not have health insurance or are healthier overall. Results within nontreatment-seeking obese youth may be different. Moreover, only youth living in urban areas of San Diego, California, were sampled. Prior research indicates children reported higher HRQOL if they lived in urban areas [30]. A final limitation of the study was that it consisted of only overweight and obese youth and did not include normal-weight youth.
Strengths of the study relate primarily to its novelty in examining both individual and environmental mediators and moderators of the relationship between body weight and HRQOL. Confirmation of the influence of individual-level factors such as self-esteem and body image on the relationship between BMI and HRQOL, with simultaneous findings that environmental factors may not influence this relationship, is important. Additionally, because the present study consisted primarily of Hispanic adolescents, these findings advance our understanding of the influences on HRQOL for this underserved group. Finally, because the present analyses found that body image and self-esteem partially mediated the relationship between BMI and HRQOL in this population, these psychological characteristics could be potential targets for interventions that address obesity in this population.
More research needs to be conducted in this area. Future research should include investigating mediators and moderators of BMI and HRQOL in a large diverse sample. Additionally, researchers can investigate the mediating and moderating effects of the variables used in these analyses using the subdimensions of the HRQOL measure. Finally, researchers also may want to consider the use of an obesity-specific HRQOL measure in future research [59, 60].
Results from the current analyses suggest that body image and self-esteem may be important intervention targets to improve HRQOL among overweight and obese adolescents. This provides avenues, beyond targeting physical weight loss, for improving the life experiences of adolescents. In Hispanic youth, in particular, ethnic identity may play an important role in influencing body image and self-esteem. Interventions targeting Hispanic youth need to consider cultural factors involved with self-esteem and body image such as cultural understandings of beauty and a healthy weight. Future interventions and policies should focus not only on decreasing body weight to improve the HRQOL of adolescents but also on addressing individual factors such as body image and self-esteem in a careful and culturally sensitive manner.
Acknowledgments
PACE-PC was supported by a grant from the National Cancer Institute (Bethesda, Maryland), R01 CA121300 (Clinical Trial Registration Number: #NCT00415974). PACE-iDP was supported by a grant from National Institute of Diabetes and Digestive and Kidney Diseases (Bethesda, Maryland), 5 R18 DK064321 (Clinical Trial Registration Number: #NCT00412165). We also gratefully acknowledge support from the physicians and clinic staff at Children’s Primary Care Medical Group (South Bay Locations), Rady Children’s Hospital of San Diego, Pediatric Endocrinology Department, Rady Children’s Physician Management Services, and Kaiser Permanente Pediatrics Department.
Abbreviations
- BMI
Body mass index
- HRQOL
Health-related quality of life
- PACE-PC
Primary Care Management of Adolescent Obesity study
- PACE-iDP
Intervention for Youth at Risk for Diabetes study
Contributor Information
Julia K. Kolodziejczyk, Department of Family and Preventive Medicine, University of California, San Diego, 9500 Gilman Drive, Dept 0811, La Jolla, CA 92093-0811, USA Center for Wireless and Population Health Systems, Qualcomm Institute/Calit2, University of California, San Diego, La Jolla, CA 92093, USA; Graduate School of Public Health, San Diego State University, San Diego, CA 92182, USA.
Kyle Gutzmer, Department of Family and Preventive Medicine, University of California, San Diego, 9500 Gilman Drive, Dept 0811, La Jolla, CA 92093-0811, USA; Graduate School of Public Health, San Diego State University, San Diego, CA 92182, USA.
Shana M. Wright, Graduate School of Public Health, San Diego State University, San Diego, CA 92182, USA
Elva M. Arredondo, Graduate School of Public Health, San Diego State University, San Diego, CA 92182, USA
Linda Hill, Department of Family and Preventive Medicine, University of California, San Diego, 9500 Gilman Drive, Dept 0811, La Jolla, CA 92093-0811, USA; Center for Wireless and Population Health Systems, Qualcomm Institute/Calit2, University of California, San Diego, La Jolla, CA 92093, USA; Graduate School of Public Health, San Diego State University, San Diego, CA 92182, USA.
Kevin Patrick, Center for Wireless and Population Health Systems, Qualcomm Institute/Calit2, University of California, San Diego, La Jolla, CA 92093, USA; Department of Family and Preventive Medicine, University of California, San Diego, 9500 Gilman Drive, Dept 0811, La Jolla, CA 92093-0811, USA.
Jeannie S. Huang, Department of Family and Preventive Medicine, University of California, San Diego, 9500 Gilman Drive, Dept 0811, La Jolla, CA 92093-0811, USA Center for Wireless and Population Health Systems, Qualcomm Institute/Calit2, University of California, San Diego, La Jolla, CA 92093, USA; Rady Children’s Hospital, San Diego, CA 92123, USA; Department of Pediatrics, University of California, San Diego, La Jolla, CA 92123, USA.
Michael Gottschalk, Rady Children’s Hospital, San Diego, CA 92123, USA; Department of Pediatrics, University of California, San Diego, La Jolla, CA 92123, USA.
Gregory J. Norman, Department of Family and Preventive Medicine, University of California, San Diego, 9500 Gilman Drive, Dept 0811, La Jolla, CA 92093-0811, USA Center for Wireless and Population Health Systems, Qualcomm Institute/Calit2, University of California, San Diego, La Jolla, CA 92093, USA.
References
- 1.Ogden CL, Carroll MD, Kit BK, & Flegal KM (2012). Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA, 307, 483–490. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schwimmer JB, Burwinkle TM, & Varni JW (2003). Health-related quality of life in severely obese children and adolescents. JAMA, 289, 1813–1819. [DOI] [PubMed] [Google Scholar]
- 3.Pinhas-Hamel O, Singer S, Fradkin A, Modan D, & Reichman B (2006). Health-related quality of life among children and adolescents: Associations with obesity. International Journal of Obesity, 30, 267–272. [DOI] [PubMed] [Google Scholar]
- 4.Zeller MH, & Modi AC (2006). Predictors of health-related quality of life in obese youth. Obesity, 14, 122–130. [DOI] [PubMed] [Google Scholar]
- 5.Griffiths LJ, Parsons TJ, & Hill AJ (2010). Self-esteem and quality of life in obese children and adolescents: A systematic review. International Journal of Pediatric Obesity, 5, 282–304. doi: 10.3109/17477160903473697. [DOI] [PubMed] [Google Scholar]
- 6.Tsiros MD, Olds T, Buckley JD, et al. (2009). Health-related quality of life in obese children and adolescents. International Journal of Obesity, 33, 387–400. doi: 10.1038/ijo.2009.42. [DOI] [PubMed] [Google Scholar]
- 7.Ul-Haq Z, Mackay DF, Fenwick E, & Pell JP (2013). Meta-analysis of the association between body mass index and health-related quality of life among children and adolescents, assessed using the Pediatric Quality of Life Inventory Index. Journal of Pediatrics, 162(280–286), e1. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention (2011). Health related quality of life (HRQOL).
- 9.Healthy People 2020—Improving the Health of Americans. http://healthypeople.gov/2020/. Accessed 7 Aug 2012.
- 10.Anon. NIH Obesity Research Task Force, US Department of Health and Human Services, National Institutes of Health (2011) Strategic plan for obesity research. Bethesda, MD. [Google Scholar]
- 11.Anon. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control (2011) The social ecological model: A framework for prevention.
- 12.Lerdal A, Andenxs R, Bjørnsborg E, et al. (2011). Personal factors associated with health-related quality of life in persons with morbid obesity on treatment waiting lists in Norway. Quality of Life Research, 20, 1187–1196. doi: 10.1007/s11136-011-9865-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Palmeira AL, Markland DA, Silva MN, et al. (2009). Reciprocal effects among changes in weight, body image, and other psychological factors during behavioral obesity treatment: A mediation analysis. International Journal of Behavioral Nutrition and Physical Activity, 6, 9. doi: 10.1186/1479-5868-6-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wright F, Boyle S, Baxter K, et al. (2013). Understanding the relationship between weight loss, emotional well-being and health-related quality of life in patients attending a specialist obesity weight management service. J Health Psychol, 18, 574–586. doi: 10.1177/1359105312451865. [DOI] [PubMed] [Google Scholar]
- 15.Anon. National Institute of Mental Health; Science Writing, Press & Dissemination Branch (2012) Depression in children and adolescents. Bethesda, MD. [Google Scholar]
- 16.Richman G, Hope T, & Mihalas S (2010). Assessment and treatment of self-esteem in adolescents with ADHD In Guindon MH (Ed.), Self-esteem across lifespan (pp. 111–121). New York, NY: Routledge. [Google Scholar]
- 17.Smith AJ (2010). Body image, eating disorders, and self-esteem problems during adolescence In Guindon MH (Ed.), Self-esteem cross lifespan (pp. 125–142). New York, NY: Routledge. [Google Scholar]
- 18.Kim HS, Park J, Ma Y, & Ham OK (2013). Factors influencing health-related quality of life of overweight and obese children in South Korea. The Journal of School Nursing, 29, 361–369. doi: 10.1177/1059840513475363. [DOI] [PubMed] [Google Scholar]
- 19.Gaspar T, Ribeiro JP, de Matos MG, et al. (2012). Health-related quality of life in children and adolescents: Subjective well being. The Spanish journal of Psychology, 15, 177–186. [DOI] [PubMed] [Google Scholar]
- 20.Saloumi C, & Plourde H (2010). Differences in psychological correlates of excess weight between adolescents and young adults in Canada. Psychology, Health and Medicine, 15, 314–325. doi: 10.1080/13548501003668711. [DOI] [PubMed] [Google Scholar]
- 21.Vallance JK, Latner JD, & Gleaves DH (2011). The relationship between eating disorder psychopathology and health-related quality of life within a community sample. Quality of Life Research, 20, 675–682. doi: 10.1007/s11136-010-9799-x. [DOI] [PubMed] [Google Scholar]
- 22.Mikolajczyk RT, Bredehorst M, Khelaifat N, et al. (2007). Correlates of depressive symptoms among Latino and Non-Latino White adolescents: findings from the 2003 California Health Interview Survey. BMC Public Health, 7, 21. doi: 10.1186/1471-2458-7-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xie B, Unger JB, Gallaher P, et al. (2010). Overweight, body image, and depression in Asian and Hispanic adolescents. American Journal of Health Behavior, 34, 476–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McClure AC, Tanski SE, Kingsbury J, et al. (2010). Characteristics associated with low self-esteem among US adolescents. Academic Pediatric, 10(238–44), e2. doi: 10.1016/j.acap.2010.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Katzmarzyk PT, Barreira TV, Broyles ST, et al. (2013). The International Study of Childhood Obesity, Lifestyle and the Environment (ISCOLE): Design and methods. BMC Public Health, 13, 900. doi: 10.1186/1471-2458-13-900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Papas MA, Alberg AJ, Ewing R, et al. (2007). The built environment and obesity. Epidemiologic Reviews, 29, 129–143. doi: 10.1093/epirev/mxm009. [DOI] [PubMed] [Google Scholar]
- 27.U.S. Department of Health and Human Services, Office of the Surgeon General (2011) Childhood obesity prevention: Community checklist. Washington, DC. [Google Scholar]
- 28.Sallis JF, Saelens BE, Frank LD, et al. (2009). Neigh-borhood built environment and income: examining multiple health outcomes. Social Science and Medicine, 68, 1285–1293. doi: 10.1016/j.socscimed.2009.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stigsdotter UK, Ekholm O, Schipperijn J, Toftager M, Kamper-Jorgensen F, & Randrup TB (2010). Health promoting outdoor environments: Associations between green space, and health, health-related quality of life and stress based on Danish national representative survey. Scandinavian Journal of Public Health, 38, 411–417. doi: 10.117/1403494810367468. [DOI] [PubMed] [Google Scholar]
- 30.Wu XY, Ohinmaa A, & Veugelers PJ (2010). Sociodemographic and neighborhood determinants of health-related quality of life among grade-five students in Canada. Quality of Life Research, 19, 969–976. doi: 10.007/s11136-010-9663-z. [DOI] [PubMed] [Google Scholar]
- 31.Feldman PJ, & Steptoe A (2004). How neighborhoods and physical functioning are related: the roles of neighborhood socioeconomic status, perceived neighborhood strain, and individual health risk factors. Annals of Behavioral Medicine, 27, 91–99. doi: 10.1207/s15324796abm2702_3. [DOI] [PubMed] [Google Scholar]
- 32.Lovasi GS, Hutson MA, Guerra M, & Neckerman KM (2009). Built environments and obesity in disadvantaged populations. Epidemiologic Reviews, 31, 7–20. doi: 10.1093/epirev/mxp005. [DOI] [PubMed] [Google Scholar]
- 33.Arif AA, & Rohrer JE (2006). The relationship between obesity, hyperglycemia symptoms, and health-related quality of life among Hispanic and non-Hispanic white children and adolescents. BMC Family Practice,. doi: 10.1186/1471-2296-7-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hubert HB, Snider J, & Winkleby MA (2005). Health status, health behaviors, and acculturation factors associated with overweight and obesity in Latinos from a community and agricultural labor camp survey. Preventive Medicine (Baltim), 40, 642–651. doi: 10.1016/j.ypmed.2004.09.001. [DOI] [PubMed] [Google Scholar]
- 35.Pérez-Escamilla R (2011). Acculturation, nutrition, and health disparities in Latinos. American Journal of Clinical Nutrition, 93, 1163S–1167S. doi: 10.3945/ajcn.110.003467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Patrick K, Norman GJ, Davila EP, et al. (2013). Outcomes of a 12-month technology-based intervention to promote weight loss in adolescents at risk for type 2 diabetes. Journal of Diabetes Science and Technology, 7, 759–770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.American Diabetes Association. (2000). Type 2 diabetes in children and adolescents. Diabetes Care, 23, 381–389. [DOI] [PubMed] [Google Scholar]
- 38.Varni J, Seid M, & Kurtin P (2001). PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Medical Care, 39, 800–812. [DOI] [PubMed] [Google Scholar]
- 39.Radloff LS (1977). The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- 40.Poulin AC, Hand D, & Boudreau B (2005). Validity of a 12-item version of the CES-D used in the National Longitudinal Study of Children and Youth. Chronic Diseases in Canada, 26, 65–72. [PubMed] [Google Scholar]
- 41.Garner DM, Olmstead MP, & Polivy J (1983). Development and validation of a multidimensional eating disorder inventory for anorexia nervosa and bulimia. International Journal of Eating Disorders, 2, 15–34. [Google Scholar]
- 42.Zabinski MF, Calfas KJ, Gehrman CA, et al. (2001). Effects of a physical activity intervention on body image in university seniors: Project GRAD. Annals of Behavioral Medicine, 23, 247–252. doi: 10.1207/S15324796ABM2304_3. [DOI] [PubMed] [Google Scholar]
- 43.Rosenberg M (1965). Society and the adolescent self-image. Princeton, NJ: Princeton University Press. [Google Scholar]
- 44.Robins RW, Hendin HM, & Trzesniewski KH (2001). Measuring global self-esteem: Construct validation of a single-item measure and the Rosenberg Self-Esteem Scale. Personality and Social Psychology Bulletin, 27, 151–161. doi: 10.1177/0146167201272002. [DOI] [Google Scholar]
- 45.Barona A, & Miller JA (1994). Short Acculturation Scale for Hispanic Youth (SASH-Y): A preliminary report. Hispanic Journal of Behavioral Sciences, 16, 155–162. doi: 10.1177/07399863940162005. [DOI] [Google Scholar]
- 46.Serrano E, & Anderson J (2003). Assessment of a refined Short Acculturation Scale for Latino preteens in rural Colorado. Hispanic Journal of Behavioral Sciences, 25, 240–253. doi: 10.1177/0739986303025002006. [DOI] [Google Scholar]
- 47.Saelens BE, Sallis JF, Black JB, & Chen D (2003). Neighborhood-based differences in physical activity: An environment scale evaluation. American Journal of Public Health 9, 93, 1552–1558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Baron RM, & Kenny DA (1986). The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Personality and Social Psychology Bulletin, 51, 1173–1182. [DOI] [PubMed] [Google Scholar]
- 49.Sobel M (1986). Some new results on indirect effects and their standard errors in covariance structure models. Sociological Methodology, 16, 159–186. [Google Scholar]
- 50.Kraemer HC (2001). How do risk factors work together? Mediators, moderators, and independent, overlapping, and proxy risk factors. American Journal of Psychiatry, 158, 848–856. doi: 10.1176/appi.ajp.158.6.848. [DOI] [PubMed] [Google Scholar]
- 51.Wallander JL, Taylor WC, Grunbaum JA, Franklin FA, Harrison GG, Kelder SH, Schuster MA (2009) Weight status, quality of life, and self-concept in African American, Hispanic, and white fifth-grade children. Obesity 17, 1363–1368. [DOI] [PubMed] [Google Scholar]
- 52.Xanthopoulos MS, Borradaile KE, Hayes S, et al. (2011). The impact of weight, sex, and race/ethnicity on body dissatisfaction among urban children. Body Image, 8, 385–389. doi: 10.1016/j.bodyim.2011.04.011. [DOI] [PubMed] [Google Scholar]
- 53.Cohen M, Mansoor D, Langut H, & Lorber A (2007). Quality of life, depressed mood and self-esteem in adolescents with heart disease. Psychosomatic Medicine, 69, 313–318. doi: 10.1097/PSY.0b013e3180051542c. [DOI] [PubMed] [Google Scholar]
- 54.Stern M, Mazzeo SE, Gerke CK, Porter JS, Bean MK, & Laver JH (2007). Gender, ethnicity, psychosocial factors, and quality of life among severely overweight, treatment-seeking adolescents. Journal of Pediatric Psychology, 32, 90–94. doi: 10.1093/jpepsy/jsl013. [DOI] [PubMed] [Google Scholar]
- 55.Ali MM, Fang H, & Rizzo JA (2010). Body weight, self-perception and mental health outcomes among adolescents. The Journal of Mental Health Policy and Economics, 13, 53–63. [PubMed] [Google Scholar]
- 56.Goodman E, & Must A (2011). Depressive symptoms in severely obese compared with normal weight adolescents: Results from a community based longitudinal study. Journal of Adolescent Health, 49, 64–69. doi: 10.1016/j.jadohealth.2010.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Herzer M, Zeller MH, Rausch JR, & Modi AC (2011). Perceived social support and its association with obesity-specific health-related quality of life. Journal of Developmental and Behavioral Pediatrics, 32, 188–195. doi: 10.1097/DBP.0b013e318208f576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Swallen KC, Reither EN, Haas SA, & Meier AM (2005). Overweight, obesity, and health-related quality of life among adolescents: The National Longitudinal Study of Adolescent Health. Pediatrics, 115, 340–347. doi: 10.1542/peds.2004-0678. [DOI] [PubMed] [Google Scholar]
- 59.Zeller MH, & Modi AC (2009). Development and initial validation of an obesity-specific quality-of-life measure for children: Sizing me up. Obesity, 17, 1171–1177. doi: 10.1038/oby.2009.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kolotkin RL, Zeller M, Modi AC, et al. (2006). Assessing weight-related quality of life in adolescents. Obesity, 14, 448–457. doi: 10.1038/oby.2006.59. [DOI] [PMC free article] [PubMed] [Google Scholar]