Abstract
Background
Suicide and alcohol use disorders (AUD) have high public health and economic costs. We investigate the relationship between religious features that are external to the individual (hereafter, contextual religiosity) and individuals’ risk of AUD and suicidal thoughts.
Methods
Data are from Wave 2 of the National Epidemiological Survey on Alcohol and Related Conditions (analytic N=34,326). Regression analysis assessed whether contextual (i.e., Geographic state) religiosity and membership rates of Catholics and the three major Protestant traditions, are associated with DSM-IV AUD risk in the past 12 months and suicidal thoughts since last interview, controlling for individual and state-level covariates. In a secondary analysis, we test for interactions between individual race/ethnicity and contextual religiosity on the outcomes since prior work suggested differences by race and individual religiosity.
Results
Some contextual religious variables were significantly associated with AUD risk but not suicidal thoughts. Individuals living in a state with higher membership rates of Evangelical Protestant had higher AUD risk (Adjusted Relative Risk [ARR]=1.27, 95%CI=1.08—1.49). Individuals living in states with higher membership rates of Historically Black Protestant had a lower risk of AUD (ARR=0.83, 95% CI=0.72—0.96). The interaction between individual race and contextual-level religious variables on the outcomes were not significant.
Limitations
NESARC is an observational cross-sectional so causality between religiosity and the outcomes cannot be established.
Conclusions
The risk of AUD among individuals varies depending on the religious membership rates among Protestant groups within their geographic state of residence. Contextual religiosity may impact AUD risk above and beyond one’s individual religiosity.
Keywords: alcohol use disorders, contextual, suicide, NESARC, religion
1. Introduction
Suicide and alcohol-use disorders (AUD) are two major public health problems. In 2013 (the latest published estimates available), four percent of adults in the United States (U.S.) contemplated suicide, and 113 completed suicide each day of the year, resulting in a suicide rate of 12.6 per 100,000 person-years (Centers for Disease Control and Prevention, 2015). The medical and productivity-related costs of suicide in a given year are $51 billion (Centers for Disease Control and Prevention, 2015).
Twenty-nine percent of adults in the U.S. will have an alcohol use disorder in their lifetime (Grant et al., 2015), and five percent of years of life lost in the U.S. are attributable to alcohol-related mortality (Shield et al., 2013). The fourth highest lifestyle-related cause of preventable death is mortality from AUD (National Institute on Alcohol Abuse and Alcoholism, 2016). AUD costs $200 million in medical expenditures nationally (Bouchery et al., 2011).
AUD and suicide share several social epidemiological characteristics. For instance, low socioeconomic status and high exposure to environmental and personal stressors are each associated with increased risks of AUD, suicidal thoughts, and completed suicides (Dupéré et al., 2009; Rehkopf & Buka, 2006; Vilhjalmsson et al., 1998; Wilkinson & Marmot, 2003).
Religiosity is associated with both AUD and suicide; however, most of what we know about their associations is based on individual measures of religiosity (e.g., higher frequency of church attendance, spirituality) (Michalak et al., 2007; Rasic et al., 2009). Higher involvement in religious activities is associated with a lower risk of AUD (Borders et al., 2010; Nelson, 2009), suicidal thoughts (Cole-Lewis et al., 2016; Dervic et al., 2004; Toussaint et al., 2015), and suicide attempts (Burshtein et al., 2016; VanderWeele et al., 2016).
However, there remains a gap in the literature about the relationships between religious features that are external to the individual (i.e., contextual religiosity) are protective against AUD and suicide. Contextual explanations for variation in individual health emphasize the opportunity structures, norms, and other socio-cultural factors in the local and physical environment (Macintyre et al., 2002). Examples of contextual effects on individual health, tested using multilevel designs, have drawn upon theories such as neighborhood social disorganization (Sampson & Groves, 1989) and neighborhood social fragmentation (Ivory et al., 2011). Early ecological studies that examined contextual religiosity as explanations for variation in mental health including suicide, have used aggregate scores of variables such as religious service attendance, religious beliefs and practices for contextual religiosity (Neeleman & Lewis, 1999). Ecological studies have found a link between contextual religious factors such as the prevalence of Protestants or Catholics in an area and suicide rates (Pescosolido & Georgianna, 1989; Torgler & Schaltegger, 2014). Some multilevel studies found independent associations between contextual religiosity and an individuals’ risk of suicide (Agerbo et al., 2007; van Tubergen et al., 2005). Although there have been a few studies that investigated a link between religiosity and suicide and AUD risk at the individual level, there is limited research on the associations between contextual religiosity and associations with individual variation in AUD and suicide risk in the U.S.
It is important to understand how contextual religiosity impacts population health in the U.S. because state and local alcohol policies (Naimi et al., 2014) and funding for and investment in substance-use disorders treatment (The Pew Charitable Trusts & MacAurthur Foundation, 2015) correlate strongly with the religious composition of geographic states. Other national policies (e.g., hate crime laws) that shape individual mental health outcomes vary widely across the geographic states (Hatzenbuehler et al., 2009; Kenneth & Calhoun-Brown, 2014). Therefore, if contextual religiosity predicts AUD and suicide risk, then strengthening the religious activities at the contextual (i.e., geographic state level) could be leveraged to reduce individual’s risk of these outcomes in the larger population. Next, these results may guide the direction of future research to concentrate efforts to investigate how contextual religious factors in the environment may buffer other established ecological level risk factors (e.g., social fragmentation) as well as contextual-level religious-specific mechanisms (Joiner et al., 2002) of individual suicide and AUD risk.
We hypothesized that contextual religiosity will be associated with lower individual risk of AUD and suicide ideation independent of individuals’ own religious observance. We hypothesize there to be an independent protective relationship because, at the aggregate level, religious networks may provide greater levels of emotional and instrumental support (beyond the individual level) that can foster social integration and buffer one’s risk of isolation and normlessness, which are risk factors for suicide (van Tubergen, et al., 2005). Another reason is that aggregate-level social support derived through contextual religiosity could protect against AUD and suicide risk factors such as mental health disorders like depression (Braam et al., 1999). Additionally, the moral community hypothesis posits that the impact of individual religious behaviors on health outcomes is most effective when they are reinforced through social norms operating at the contextual level (Stark et al., 1982). This hypothesis implies that contextual level religiosity has substantial impacts on individual health outcomes. Thus within the context of social norms, religious communities are theoretically more likely to espouse prohibitory suicide norms than secular communities (van Tubergen, et al., 2005). For instance, during the temperance movement in the U.S., anti-drinking social norms within religious communities helped influence enforcement of prohibition, which limited the availability of alcohol (Pennock, 2012).
2. Methods
2.1. Sample
The sample for this study consisted of adults from Wave 2 of The National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), conducted between 2004 and 2005. Wave 2 consisted of 34,653 interviews with a response rate of 87 percent from the Wave 1 sample which was collected between 2001 and 2002. NESARC is a population-based survey that assessed health outcomes, behavioral factors, and psychiatric disorders among civilian non-institutionalized adults in the U.S. Further details of the sampling methodology have been previously published (Grant & Dawson, 2006; Grant et al., 2009). Informed consent was obtained from all participants in the study and this study plan was approved by the University Ethics Board (Harvard IRB # 15–0099).
2.2. Measures
2.2.1. Suicide ideation (since last interview)
Suicide ideation or suicidal thought is based on a single question: “During the time since your last interview when your mood was at its lowest/you enjoyed or cared the least about things, did you think about committing suicide?” This question was asked among the sample of individuals who reported a period of two weeks of low mood since the last interview. The response option was yes or no, which we use as the referent group. Along with those who reported no, we include in the referent group all other participants who did not meet criteria for low mood and thus were not asked the question.
2.2.2. Alcohol-use disorders (12 months)
AUD is defined as meeting the diagnostic criteria for alcohol abuse and/or dependence according to the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) (American Psychiatric Association (APA), 2000). The Alcohol Use Disorder and Associated Disabilities Interview Schedule-DSM-IV (AUDADIS-IV) was used in the study and has a high test-retest reliability for AUD (k=0.76 (se=0.05) (Grant et al., 1995; Hasin et al., 1997). The response was yes, meets criteria or no, which we use as the referent group.
2.2.3. Individual-level religious involvement
Individual-level religious service attendance was ascertained with two religious-involvement questions in NESARC, asked in Wave 2 only. One question asked of participants was whether they currently attend religious services at a church, mosque, synagogue, or other religious place (yes or no). The other question was about the frequency of service attendance. Responses ranged from 1 (once a year) to 5 (twice a week or more). Because frequency of service attendance is recorded only among those who attend services, we derived a new variable by adding another category 0 (do not attend), 1 (once a year/a few times a year) (collapsed because of small cell size in once a year), 2 (one to three times a month,), 3 (once a week), and 4 (twice a week or more). Individual-level subjective religiosity/spirituality was ascertained from the question: “how important are religious or spiritual beliefs in your daily life?” Responses ranged from 0 (not at all important) to 3 (very important). The NESARC did not collect data about denominational affiliation.
2.2.4. Contextual religiosity
Contextual-level variables are typically operationalized at the ecological level such as a geographic areal unit or some other group level (Agerbo, et al., 2007; Macintyre, et al., 2002). In this study, we operationalize the contextual level using the geographic unit of American states for reasons described earlier.
We have two sets of contextual religiosity variables that were created from external data sources. The first corresponds to the state-level aggregates of self-reported responses of individuals’ frequency of church attendance and the importance of religion in their lives. The second corresponds to the rates of church membership for the major religious traditions in the U.S. Both sets of contextual religiosity measures reflect the theoretical concept of religiosity and have high correlations with an overall aggregate religiosity index (Blanchard et al., 2008; Borch et al., 2010b; Grant, 2008).
2.2.4.1. Contextual religiosity variable 1: High religiosity
We used survey data that assess public opinions to generate aggregate religious and social measures (Borch, et al., 2010b; Brace et al., 2002). Data were from a Gallup Poll conducted in November 2003; a Gallup Poll from June 2004; a Pew News Interest Poll from July 2005; and the Pew Research Center for the People & The Press Right to Die Poll in November 2005 (archived at the Roper Center for Public Opinion Research Database) (Cornell University, 2016). Adopting one methodological approach from previous research (Stroope & Baker, 2018), we used two items to create one composite variable because of a high correlation between them: (1) the proportion of participants in a state that reported attending “once a week” and “almost every week” based on the question: “how often do you attend church?” and (2) the proportion of participants within each of the included 49 states that responded “very important” to the question: “how important would you say religion is in your own life?” Selecting the upper distributions among those questions is reasonable because the frequency of these questions is often skewed to the upper distribution of positive ratings or responses (Bader & Finke, 2017).
Data were pooled across the four surveys (n=4,009) to improve the precision of state-level prevalence estimates. Polling data are based on random samples of cellphone and landline participants within each state. Prevalence estimates are weighted to adjust for unequal selection probability and non-response, and to match the U.S. population according to gender, age, race, Hispanic ethnicity, education, population density, and phone status (GALLUP, 2015). The samples produced from weighting approximates the adult (18 years and older) civilian population living in private households (Newport & Gallup, 2011).
2.2.4.2. Contextual religiosity variable 2: State-level church membership rates of major religious traditions
The theoretical and empirical grounds for investigating church membership rates have been previously established (Blanchard, et al., 2008). Briefly, church membership (i.e., adherence rate) reflects the demographic dominance or market share of a faith tradition and the cultural content, such as ideologies of that faith tradition, which shape health, mortality, and illness (Blanchard, et al., 2008). We obtained data for Catholics and the three major Protestant subgroups: Evangelical, Mainline, and Historically Black (Pew Forum on Religion and Public Life, 2008). Those data were retrieved from the Religious Congregations and Membership Study (RCMS): 2000 (The Association of Religion Data Archives, nd). Details on RCMS’ methodology have been previously published (Association of Statisticians of American Religious Bodies, 2010; Jones et al., 2002). The adherence rate is defined as the complete count of people affiliated with a congregation (numerator) across all participating congregations in the U.S. (denominator) where congregations can be churches, mosques, temples, or other religious meeting places.
2.2.5. Covariates
We included covariates known to be associated with both religious exposures and the psychiatric outcomes at either the individual- or contextual-level (Borch et al., 2010a; Chatters et al., 1992; Hayward & Krause, 2014; Pan et al., 2013; Smith & Kawachi, 2014; Vilhjálmsson et al., 1998). Individual-level covariates were age; race/ethnicity (non-Hispanic black, non-Hispanic white, Hispanic, other); sex (men, women); marital status (married/cohabitating, widowed, separated or divorced, and never married); nativity (U.S.-born, foreign-born); educational attainment (less than high school, completed high school, college graduate, and graduate education and higher); personal income ($0–$19,999, $20,000–$34,999, $35,000–$69,999, $70,000 and greater); residence in one of the four census regions (Northeast, Midwest, South, West); and residence in a Metropolitan Statistical Area (MSA) (that is a central city, in an MSA that is not a central city, not in an MSA). We considered the following health-related correlates of individual-level religious involvement, AUD, and suicidal thoughts: self-rated general health (excellent, very good, good, fair, poor) and any 12-month mood or anxiety DSM-IV disorders (yes vs. no).
Contextual-level covariates were obtained from the Census 2000 SF1 and SF3 files (Social Explorer, 2015). These included the proportion of black/African American residents in a state, the proportion of persons below the poverty level, the proportion of unemployed persons aged 16 years and over, the proportion of persons aged 25 and over with less than a high school diploma, median household income, proportion of divorced persons aged 15 years and over, and residential instability operationalized as the proportion of persons who lived in a different state in 1995. We standardized all geographic variables to have a mean of zero and a standard deviation of one to reduce collinearity in the models and facilitate a meaningful comparative discussion across predictors.
2.3. Statistical Analyses
Survey-weighted means for continuous variables and percentages for categorical variables described the sample distribution for individual-level religious involvement measures and covariates for adults with AUD and suicidal thoughts separately. Spearman correlation analysis assessed the magnitude of association among the contextual variables. Forty-nine states were included (Hawaii and Alaska were excluded because of a scarcity of data for the outcome or exposure variables).
Prior work suggested that race/ethnicity moderates the association between individual-level religious involvement and suicide ideation (Assari, 2015; Wingate et al., 2005). There is also reason to believe that race/ethnicity will modify the association between individual religiosity and alcohol use (Bohnert et al., 2010; Krause, 2003), although previous work found no significant interactions (Ransome & Gilman, 2016). However, whether individual race/ethnicity moderates the association between contextual religiosity in association with individual’s risk of AUD and suicide ideation is unknown. We therefore conducted exploratory effect modification analyses by including a race/ethnicity * contextual religiosity interaction term in the analyses. The significance of the interaction was tested via the Wald test of contrast that reports an F-statistic and p-value. The interaction between individual race/ethnicity and contextual religiosity variables were not statistically significant at p < 0.10. We therefore fit one multivariate Poisson regression with log link (to obtain the relative risk coefficient), using Generalized Structural Equation Modeling. The model included the individual and contextual religiosity variables along with the covariates at both levels. We conducted the analysis in STATA 14.0 and used the survey ‘svy’ procedures to account for the complex survey design of NESARC so that standard errors would be appropriately calculated (StataCorp, 2015). Adjusted relative risk (ARR) and 95-percent confidence intervals (CI) are reported.
3. Results
The analysis sample included 34,326 persons (99.65 percent) who had non-missing data on all covariates of the total NESARC sample, after removal of Hawaii and Alaska (Table 1). Overall, 3,116 people met criteria for AUD in the past 12 months corresponding to a weighted prevalence of 9.1 percent. There were 1,277 people meeting criteria for suicidal thoughts, corresponding to a prevalence of 3.7 percent. Thirteen percent of persons reporting AUD in the past 12 months attended religious services once a week or more (e.g., 10.60 + 2.76), compared to almost 22 percent of persons who contemplated suicide and 34 percent of persons who did not report AUD or suicidal thoughts. Thirty-seven percent of persons with AUD in the past 12 months rated subjective religiosity/spirituality as very important in contrast to greater than 54 percent of persons who contemplated suicide, and 59 percent for those with no AUD or suicide ideation. A higher prevalence of men reported AUD in the past 12 months, but a higher prevalence of women reported suicidal thoughts since the last interview. The southern region had the highest prevalence of AUD and suicide risk.
Table 1.
Descriptive characteristics of the sample, adults in the National Survey of Alcohol and Related Conditions (NESARC), Wave 2 (N=34,326)*
| DSM-IV Alcohol Use Disorder (12 months) (n=3,116) 09.1% |
DSM-IV Suicide Ideation (since last interview) (n=1,277) 03.7% |
No AUD or Suicide Ideation (n=30,180) 87.9% |
|
|---|---|---|---|
| Religious service attendance, n (%) | |||
| Never | 1998 (65.10) | 724 (59.72) | 12754 (44.09) |
| Once a year/A few times a year | 268 (08.69) | 81 (05.82) | 2407 (07.64) |
| One to three times a month | 401 (12.85) | 171 (15.58) | 4341 (13.94) |
| Once a week | 357 (10.60) | 185 (13.02) | 7182 (23.60) |
| Twice a week or more | 91 (02.76) | 116 (08.86) | 3457 (10.73) |
| Subjective religiosity and spirituality, n (%) | |||
| Not important at all | 234 (08.00) | 100 (08.87) | 1225 (04.52) |
| Not very important | 370 (12.61) | 102 (09.40) | 2095 (07.90) |
| Somewhat important | 1272 (42.55) | 331 (27.45) | 7959 (28.35) |
| Very important | 1238 (36.84) | 742 (54.28) | 18813 (59.23) |
| Race/Ethnicity, n (%) | |||
| Non-Hispanic white | 1997 (74.81) | 776 (73.09) | 17398 (70.74) |
| Non-Hispanic black | 489 (10.17) | 207 (09.96) | 5899 (11.26) |
| Hispanic | 520 (10.31) | 230 (10.56) | 5591 (11.73) |
| Other | 110 (04.71) | 64 (06.38) | 1292 (06.27) |
| Age, n (%) | |||
| 20–34 | 1237 (44.33) | 396 (33.76) | 6428 (23.22) |
| 35–49 | 1183 (35.14) | 456 (34.59) | 9399 (30.62) |
| 50–64 | 561 (16.73) | 333 (24.74) | 7470 (24.87) |
| 65 and older | 135 (03.80) | 92 (06.91) | 6883 (21.29) |
| Sex, n (%) | |||
| Men | 2070 (71.38) | 438 (39.01) | 12050 (45.74) |
| Women | 1046 (28.62) | 839 (60.99) | 18130 (54.26) |
| Marital Status, n (%) | |||
| Married/cohabiting | 1356 (49.59) | 489 (45.14) | 16923 (65.86) |
| Widowed/separated/divorced | 712 (17.27) | 456 (29.72) | 7977 (18.68) |
| Never married | 1048 (33.14) | 332 (25.14) | 5280 (15.46) |
| Nativity, Born outside the US, n (%) | 244 (07.07) | 136 (08.53) | 25225 (85.29) |
| Education, n (%) | |||
| Less than high school | 368 (10.77) | 238 (16.30) | 4904 (14.23) |
| Completed high school | 846 (27.12) | 332 (27.38) | 8256 (27.58) |
| College degree | 1581 (51.75) | 592 (47.42) | 12995 (44.43) |
| Graduate education and higher | 321 (10.37) | 115 (08.90) | 4025 (13.76) |
| Personal income, n (%) | |||
| $0-$19,999 | 805 (25.68) | 677 (51.33) | 10650 (33.84) |
| $20,000-$34,999 | 1034 (33.40) | 365 (30.61) | 9720 (31.55) |
| $35,000-$69,999 | 914 (29.18) | 179 (13.54) | 7048 (24.14) |
| $70,000 and greater | 363 (11.73) | 56 (04.52) | 2762 (10.46) |
| Census region, n (%) | |||
| Northeast | 521 (16.65) | 229 (18.16) | 5308 (17.82) |
| Midwest | 609 (19.14) | 231 (17.73) | 5756 (18.64) |
| South | 1198 (39.92) | 503 (39.13) | 11403 (38.07) |
| West | 788 (24.29) | 314 (24.98) | 7713 (25.47) |
| Metropolitan statistical area (MSA) residence, n (%) | |||
| Is a central city | 999 (31.49) | 449 (34.38) | 10049 (32.78) |
| In an MSA that is not a central city | 1602 (51.55) | 631 (51.12) | 15244 (50.92) |
| Not in an MSA | 515 (19.97) | 197 (14.50) | 4887 (16.30) |
|
Self-rated health, range (1=worse, 5=best) mean (se) |
2.27 (0.01) | 3.06 (0.02) | 2.34 (0.00) |
| 12-month, any mood disorder (yes), n (%) | 582 (18.55) | 930 (73.75) | 2453 (07.56) |
| 12-month, any anxiety disorder (yes), n (%) | 598 (19.33) | 654 (50.74) | 3380 (10.52) |
N based on the multivariable sample with no missing data on the covariates, and excluding respondents from Alaska and Hawaii
Unweighted n and weighted column percent, and for continuous self-rated health, weighted mean and standard error
Results from correlation analysis of the contextual variables are in Table 2. There was a strong positive correlation between the proportion of participants in a state who reported attending church more than once a week and those who rated religion very important in their own lives (rho=0.87, p < 0.05). Given this high correlation, we created a single composite from these two indicators. Within states, Catholic adherence rate was negatively correlated with both a high proportion of church attenders (rho=−0.51, p < 0.05) and the proportion who rated religiosity as very important in their lives (rho=−0.59, p < 0.05). Within states, a high proportion of black/African American residents was positively correlated with a high proportion of Historically Black Protestant membership rates (rho=0.34, p < 0.05).
Table 2.
Correlation matrix of geographic state level variables in the study
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | ||
| 1 | Proportion attending church more than once a week | 1 | ||||||||||||
| 2 | Proportion rating religion is very important in their own life | 0.87* | 1 | |||||||||||
| 3 | Catholic Adherence rate | -0.51* | -0.59* | 1 | ||||||||||
| 4 | Evangelical Protestants Adherence rate | 0.67* | 0.79* | −0.75* | 1 | |||||||||
| 5 | Mainline Protestants Adherence rate | 0.32* | 0.40* | −0.26* | 0.37* | 1 | ||||||||
| 6 | Historically Black Protestant Adherence rate | 0.61* | 0.69* | −0.71* | 0.85* | 0.17* | 1 | |||||||
| 7 | Proportion of black/African American residents | 0.48* | 0.51* | −0.23* | 0.36* | 0.24* | 0.34* | 1 | ||||||
| 8 | Proportion in poverty | 0.27* | 0.34* | −0.086* | 0.32* | −0.31* | 0.41* | 0.28* | 1 | |||||
| 9 | Proportion unemployed | −0.22* | −0.15* | 0.30* | −0.18* | −0.55* | −0.07* | 0.13* | 0.72* | 1 | ||||
| 10 | Proportion with less than high school diploma | 0.32* | 0.38* | −0.15* | 0.40* | −0.24* | 0.51* | 0.42* | 0.90* | 0.60* | 1 | |||
| 11 | Median household income | −0.69* | −0.72* | 0.53* | −0.69* | −0.28* | −0.62* | −0.22* | −0.50* | −0.03* | −0.39* | 1 | ||
| 12 | Proportion divorced | 0.29* | 0.35* | −0.61* | 0.51* | −0.22* | 0.54* | −0.16* | 0.17* | −0.08* | 0.10* | −0.49* | 1 | |
| 13 | Residential instability (proportion residing out of state in 1995) | 0.43* | 0.39* | −0.66* | 0.47* | 0.19* | 0.62* | −0.00 | −0.21* | −0.51* | −0.18* | −0.37* | 0.54* | 1 |
Note. Denotes correlations significant at p < 0.05 level.
N=49 states including Washington, D.C. were included (Alaska and Hawaii excluded).
Results of regression analyses for AUD and suicide ideation risk are shown in Table 3. Living in a state with a high proportion of Evangelical Protestant adherents was associated with higher risk of AUD in the past 12 months. Specifically, for every standard deviation increase in Evangelical Protestant membership rate, an individuals’ risk of AUD increased by 27 percent, ARR=1.27 (95% CI 1.08, 1.49). In contrast, living in a state with a high rate of Historically Black Protestant adherents was associated with a lower risk of AUD in the past 12 months (AOR = 0.83, 95% CI 0.72, 0.96). Or put another way, if we took the inverse of Historically Black Protestant membership rates, for every one standard deviation decrease in their membership rate, an individual’s risk of AUD increased by 20%, ARR=1.20, 95% CI 1.04, 1.38 (result not displayed). Catholic or Mainline Protestant adherence rates were not significantly associated with individuals’ risks of AUD in the past 12 months. Lastly, high contextual religiosity was not associated with AUD risk nor suicide risk since the last interview among individuals.
Table 3.
Multivariate results of contextual-level religious factors in association with DSM-IV alcohol use disorders in the past 12 months and suicide ideation since the past interview, among adults in the NESARC, Wave 2 (N= 34, 326)
| Alcohol Use Disorders | Suicide Ideation | |||
|---|---|---|---|---|
| ARR | [95% CI] | ARR | [95% CI] | |
| Geographic state-level | ||||
| High religiositya | 1.04 | [0.99, 1.09] | 1.03 | [0.97, 1.09] |
| Adherence rate: | ||||
| Catholics | 1.06 | [0.97, 1.15] | 1.05 | [0.93, 1.18] |
| Evangelical Protestant | 1.27** | [1.08, 1.49] | 0.98 | [0.79, 1.23] |
| Mainline Protestant | 1.07 | [0.99, 1.15] | 0.96 | [0.85, 1.08] |
| Historically Black Protestant | 0.83* | [0.72, 0.96] | 0.95 | [0.77, 1.16] |
ARR=Adjusted Relative Risk. CI=Confidence Interval.
Individual-level covariates include continuous age, race/ethnicity, sex, marital status, nativity, education, income, self-rated health, any mood disorder, and any anxiety disorder, residence in one of the four Census regions, and in residence a Metropolitan Statistical Area (MSA).
Geographic state-level covariates include % black in the state, % in poverty, % unemployed, % < high school diploma, median household income, % divorced, and residential instability—% residing out of the state in 1995 in the state. N=49 states including Washington, D.C. were included (Alaska and Hawaii excluded).
p<.001;
p<.01;
p<.05
aHigh religiosity is a composite variable including the sum of the proportion of persons who attend church once a week and almost every day, and the proportion who respond that religion is very important in their own life.
4. Discussion
This study used a national probability sample of participants to investigate the role of contextual religiosity and an individual’s risk of AUD and suicidal thoughts. We did this by examining contextual-level effects (macro) through a range of ecological-level religious factors that reflect the congregational composition of major religious traditions. The theory that underpins congregational composition as predictor is that the larger market share of the specific tradition would have a stronger opportunity to exert religious doctrines and social norms that can impact individual behavior (micro). We also examined contextual factors beyond religious composition that reflect overall religiosity, which included frequency of high religious attendance and religious salience (Stroope & Baker, 2018) (e.g., proportion in a state rating religiosity and spirituality as very important). Those contextual variables were based on validated measures of subjective and objective indicators of religiosity.
We observed an association between contextual religiosity and individuals’ risk of AUD. Our hypothesis that higher contextual religiosity would be associated with lower AUD and suicide risk was observed only for the measure of Historically Black Protestant membership rates. In contrast, individuals residing in states with a higher proportion of Evangelical Protestant membership rates had a higher risk of AUD in the past 12 months. We controlled for a wide range of individual-level factors, including race/ethnicity, individual-level religiosity, residence in Census regions, and ecological variables, including poverty, unemployment, and residential instability.
There is more than one plausible reason for the contextual-level findings that were contrary to our hypotheses. The positive association between Evangelical Protestant membership rates and AUD risk could mean that Evangelical Protestants are drawn to areas and establish ministries in areas with greater needs with respect to mental health. Those areas may also be disadvantaged with respect to the social determinants of mental, physical, and spiritual health. Indeed, part of Evangelical-led outreach ministries includes abuse counseling centers and shelters for the homeless (Chaves & Tsitsos, 2001; McKinney, 1998) while also pursuing their religious mission of winning souls for Christ (Smith, 2000). Another plausible explanation for those findings could be higher prevalence of AUD among individuals in those areas or sampling error.
The protective association between Historically Black Protestant membership rates and a lower risk of AUD among individuals might be explained by the moral community hypothesis. That theology posits that individual behavior is influenced when it is reinforced by the larger religious community (Stark, 1987). Specifically, black/African Americans have the highest levels of religious involvement compared to other racial groups (Taylor et al., 2014), and individual religiosity among them is associated with a lower AUD risk (Ransome & Gilman, 2016). The demographic composition of Historically Black Protestant churches is overwhelmingly black/African American (Pew Forum on Religion and Public Life, 2014; Sahgal et al., 2009) and mostly in the southern region. In this study, AUD prevalence was highest in the southern region. Therefore, we could possibly be observing a reinforcing effect of religious norms at the state-level based on individual-level behavioral influences on AUD risk.
Our findings contribute to an ongoing debate about whether there is a contextual-level protective influence of Historically Black Protestant membership. For instance Harris & Ulmer (2017) conducted an ecological study at the U.S. county level and found that a higher rate of Historically Black Protestant membership was significantly associated with lower rates of crime (e.g., burglary, homicide), and that this relationship was strongest in areas with a higher prevalence of socioeconomic disadvantage. In our study, we show that there appears to be a protective association between Historically Black Protestant membership rates that extends to AUD risk among individuals. The Harris & Ulmer study, however, is different from ours because they conducted an ecological analysis of U.S. counties and examined crime, whereas we examined a macro-micro relationship with psychiatric health outcomes. Contextual religiosity variables were not significantly associated with lower suicide risk in this U.S. sample. Non-significant associations among the contextual religious variables are surprising given that prior work has typically revealed differences in suicide rates between area-level Catholic and Protestant membership composition (Torgler & Schaltegger, 2014).
Our results should be considered in the context of several limitations. DSM-IV AUD is based on a diagnostic measure of multiple items covering the past 12 months. In contrast, suicide ideation is one question within the larger construct of DSM-IV mood disorder and was assessed only among participants who reported having at least 2 weeks of depressed mood or loss of interest since their last interview (approximately 2 to 3 years). The differences in the time of assessment and the recall period between these variables could possibly contribute to the association with one, but not the other outcome. To the extent that suicide ideation occurred outside of the context of depression it would not have been captured in our analysis. Replicating the analysis using measures of suicide ideation irrespective of other symptoms of mood disorders participants is a necessary next step in this research.
Next, because NESARC is an observational cross-sectional study, we cannot assess whether religious involvement is causally associated with the risk of AUD or suicidal thoughts. However, prior evidence demonstrates a temporal ordering between religious involvement as a predictor of future AUD risk (Borders, et al., 2010) and suicide (Stack, 1983; VanderWeele, et al., 2016). Longitudinal studies can examine whether changes in the proportion of church membership rates in an area are correlated with increased or lower risk of AUD or suicidal thoughts. Next, the American state is a large geographic unit and we could not account for potential heterogeneity in state-level religious involvement or denominational composition. NESARC, however, does not have geographic indicators that allow us to link individuals to smaller geographies, such as U.S. counties or Census tracts.
There are important strengths of our study. We investigated the association between contextual religiosity and AUD risk in a large nationally representative population-based sample. The representative nature of NESARC data potentially allows generalizing these findings to the larger U.S. adult population. We used population-based contextual religiosity variables that are theologically validated representations of the individual religious involvement indicators (e.g., church attendance and importance of religiosity in one’s life). For instance, the survey data (e.g., Gallup poll) from which state-level church attendance and subjective religiosity were extracted are nationally representative. Although these data are not necessarily designed to produce state-level prevalence estimates, data are based on a probability design.
Moreover, Gallup Poll data (the world’s oldest and most respected public opinion poll) are frequently used in other non-academic research to inform state-level and national policy, and they have also been used to predict presidential elections (Newport & Gallup, 2011). Developing and validating alternate measures of the contextual-level religious environment are integral parts of future research on this topic. Next, the Religious Congregation and Membership Study, from which church membership rates are calculated, is the largest representative study of religious congregations in the U.S., with more than 149 congregations comprised of approximately 141,371,963 members (Jones, et al., 2002).
We recommend future studies conduct race-specific analyses as well as examine contextual religiosity effects in smaller, less heterogenous areas. If our results are replicated, research could then explore the extent to which information on contextual religiosity could be incorporated into treatment or prevention efforts for AUD.
Figure 1.
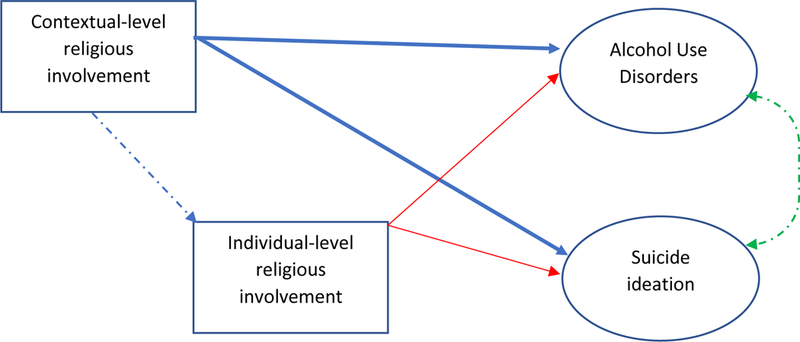
Heuristic diagram showing the model for the analysis. The solid red arrows represent work that has, to some extent, established that direct relationships exist. The solid blue arrows represent work that has not been sufficiently established, and the primary novelty of this study. The dashed blue arrow represents the potential interaction between contextual and individual-level religious involvement on the outcomes but was not tested in this preliminary study. The green dashed arrow illustrates these outcomes, theoretically, will covary at the individual level, yet was not a condition of focus in this study.
Highlights.
Contextual religiosity is independently associated with individual AUD risk
Contextual religiosity is not associated with individual suicidal thoughts
Evangelical Protestants membership rates were associated with higher AUD risk
Historically Black Protestants membership rates were associated with lower AUD risk
Acknowledegements
At the time of this study, Y. Ransome was supported by the Alonzo Smythe Yerby Postdoctoral Fellowship at Harvard T.H. Chan School of Public Health. Dr. Ransome is now an Assistant Professor at Yale School of Public Health. This work was also supported in part by the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development. We thank Dr. Tyler VanderWeele and Alexander Miamen for comments on earlier drafts of this manuscript.
References
- Agerbo E, Sterne JA, & Gunnell DJ (2007). Combining individual and ecological data to determine compositional and contextual socio-economic risk factors for suicide. Soc Sci Med, 64(2), 451–461. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association (APA). (2000). Diagnostic and Statistical Manual of Mental Disorders (4th, Edition, Text Revision ed.). Washington, DC: APA. [Google Scholar]
- Assari S (2015). Ethnic and gender differences in additive effects of socio-economics, psychiatric disorders, and subjective religiosity on suicidal ideation among blacks. Int J Prev Med, 6(1), 53–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Association of Statisticians of American Religious Bodies. (2010). U.S. Religion Census 1952 to 2010. Retrieved from http://www.rcms2010.org/index.php
- Bader CD, & Finke R (2017). Evaluating survey measures using the ARDA’s measurement wizard In Bader CD& Finke R(Eds.), Faithful measures: new methods in the measurement of religion (pp. 140–166). New York, NY: New York University Press. [Google Scholar]
- Blanchard TC, Bartkowski JP, Matthews TL, & Kerley KR (2008). Faith, morality and mortality: the ecological impact of religion on population health. Social Forces, 86(4), 1591–1620. doi: 10.1353/sof.0.0045 [DOI] [Google Scholar]
- Bohnert ASB, Perron BE, Jarman CN, Vaughn MG, Chatters LM, & Taylor RJ (2010). Use of clergy services among individuals seeking treatment for alcohol use problems. Am J Addict, 19(4), 345–351. doi: 10.1111/j.1521-0391.2010.00050.x [DOI] [PubMed] [Google Scholar]
- Borch C, Thye SR, Robinson C, & West MR (2010a). What predicts religious participation and giving? implications for religion in the United States. Sociol Spectr, 31(1), 86–113. doi: 10.1080/02732173.2011.525697 [DOI] [Google Scholar]
- Borch C, Thye SR, Robinson C, & West MR (2010b). What predicts religious participation and giving? implications for religion in the United States. Sociological Spectrum, 31(1), 86–113. [Google Scholar]
- Borders TF, Curran GM, Mattox R, & Booth BM (2010). Religiousness among at-risk drinkers: is it prospectively associated with the development or maintenance of an alcohol-use disorder? J Stud Alcohol Drugs, 71(1), 136–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bouchery EE, Harwood HJ, Sacks JJ, Simon CJ, & Brewer RD (2011). Economic costs of excessive alcohol consumption in the US, 2006. Am J Prev Med, 41(5), 516–524. [DOI] [PubMed] [Google Scholar]
- Braam AW, Beekman ATF, van den Eeden P, Deeg DJH, Knipscheer KPM, & van Tilburg W (1999). Religious climate and geographical distribution of depressive symptoms in older Dutch citizens. J Affect Disord, 54(1–2), 149–159. doi: 10.1016/S0165-0327(98)00172-4 [DOI] [PubMed] [Google Scholar]
- Brace P, Sims-Butler K, Arceneaux K, & Johnson M (2002). Public opinion in the American states: new perspectives using national survey data. Am J Pol Sci, 46(1), 173–189. [Google Scholar]
- Burshtein S, Dohrenwend BP, Levav I, Werbeloff N, Davidson M, & Weiser M (2016). Religiosity as a protective factor against suicidal behaviour. Acta Psychiat Scand, 133(6), 481–488. doi: 10.1111/acps.12555 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2015). Suicide: Facts at a glance. Retrieved from Atlanta, GA: http://www.cdc.gov/violenceprevention/pdf/suicide-datasheet-a.pdf
- Chatters LM, Levin JS, & Taylor RJ (1992). Antecedents and dimensions of religious involvement among older black adults. Journal of Gerontology, 47(6), S269–S278. [DOI] [PubMed] [Google Scholar]
- Chaves M, & Tsitsos W (2001). Congregations and social services: what they do, how they do it, and with whom. Nonprofit and Voluntary Sector Quarterly, 30(4), 660–683. doi: 10.1177/0899764001304003 [DOI] [Google Scholar]
- Cole-Lewis YC, Gipson PY, Opperman KJ, Arango A, & King CA (2016). Protective role of religious involvement against depression and suicidal ideation among youth with interpersonal problems. J Relig Health, 1–17. doi: 10.1007/s10943-016-0194-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornell University. (2016). Roper Center for Public Opinion Research. Retrieved from http://ropercenter.cornell.edu/
- Dervic K, Oquendo MA, Grunebaum MF, Ellis S, Burke AK, & Mann JJ (2004). Religious affiliation and suicide attempt. Am J Psychiatry, 161(12), 2303–2308. [DOI] [PubMed] [Google Scholar]
- Dupéré V, Leventhal T, & Lacourse É (2009). Neighborhood poverty and suicidal thoughts and attempts in late adolescence. Psychol Med, 39(08), 1295–1306. [DOI] [PubMed] [Google Scholar]
- GALLUP. (2015, September 15, 2015). How does the Gallup poll social series work? Methodology. Retrieved from http://www.gallup.com/185477/gallup-poll-social-series-work.aspx?utm_source=METHODOLOGY&utm_medium=topic&utm_campaign=tiles
- Grant BF, & Dawson DA (2006). Introduction to the National Epidemiologic Survey on Alcohol and Related Conditions. Alcohol Health Res World, 29(2), 74–78. [Google Scholar]
- Grant BF, Goldstein RB, Chou SP, Huang B, Stinson FS, Dawson DA, . . . Pickering RP (2009). Sociodemographic and psychopathologic predictors of first incidence of DSM-IV substance use, mood and anxiety disorders: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Mol Psychiatry, 14(11), 1051–1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Goldstein RB, Saha TD, & et al. (2015). Epidemiology of DSM-5 alcohol use disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry, 72(8), 757–766. doi: 10.1001/jamapsychiatry.2015.0584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Harford TC, Dawson DA, Chou PS, & Pickering RP (1995). The alcohol use disorder and associated disabilities interview schedule (AUDADIS): reliability of alcohol and drug modules in a general population sample. Drug Alcohol Depend, 39(1), 37–44. [DOI] [PubMed] [Google Scholar]
- Grant JT (2008). Measuring aggragate religiosity in the United States, 1952–2005. Sociological Spectrum, 28(5), 460–476. doi: 10.1080/02732170802205973 [DOI] [Google Scholar]
- Harris CT, & Ulmer JT (2017). “Mighty like a river”: the Black Protestant church and violence in Black communities. Sociol Q, 58(2), 295–314. [Google Scholar]
- Hasin D, Carpenter KM, McCloud S, Smith M, & Grant BF (1997). The Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS): reliability of alcohol and drug modules in a clinical sample. Drug Alcohol Depend, 44(2–3), 133–141. [DOI] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Keyes KM, & Hasin DS (2009). State-level policies and psychiatric morbidity in lesbian, gay, and bisexual populations. Am J Public Health, 99(12), 2275–2281. doi: 10.2105/ajph.2008.153510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayward RD, & Krause N (2014). The effect of belonging to an alcohol-proscribing religious group on the relationship between moderate alcohol consumption and mortality. Soc Sci Med, 101(0), 1–8. doi: 10.1016/j.socscimed.2013.10.039 [DOI] [PubMed] [Google Scholar]
- Ivory VC, Collings SC, Blakely T, & Dew K (2011). When does neighbourhood matter? Multilevel relationships between neighbourhood social fragmentation and mental health. Soc Sci Med, 72(12), 1993–2002. doi: 10.1016/j.socscimed.2011.04.015 [DOI] [PubMed] [Google Scholar]
- Joiner TE, Perez M, & Walker RL (2002). Playing devil’s advocate: why not conclude that the relation of religiosity to mental health reduces to mundane mediators? Psychological Inquiry, 13(3), 214–216. [Google Scholar]
- Jones DE, Sherri D, Grammich Clifford, Horsch J, Houseal R, Lynn M, . . . Taylor RH (Eds.). (2002). Religious Congregations and Membership Study in the United States 2000. Nashville, TN: Glenmary Research Center. [Google Scholar]
- Kenneth WD, & Calhoun-Brown A (2014). Religion and politics in the United States- seventh edition. Lanham, MD: The Rowman & Littlefield Publishing Group. [Google Scholar]
- Krause N (2003). Race, religion, and abstinence from alcohol in late life. J Aging Health, 15(3), 508–533. doi: 10.1177/0898264303253505 [DOI] [PubMed] [Google Scholar]
- Macintyre S, Ellaway A, & Cummins S (2002). Place effects on health: how can we conceptualise, operationalise and measure them? Soc Sci Med, 55(1), 125–139. [DOI] [PubMed] [Google Scholar]
- McKinney W (1998). Mainline Protestantism 2000. The Annals of the American Academy of Political and Social Science, 558(July), 57–66. [Google Scholar]
- Michalak L, Trocki K, & Bond J (2007). Religion and alcohol in the United States National Alcohol Survey: How important is religion for abstention and drinking? Drug and Alcohol Dependence, 87(2–3), 268–280. doi: 10.1016/j.drugalcdep.2006.07.013 [DOI] [PubMed] [Google Scholar]
- Naimi TS, Blanchette J, Nelson TF, Nguyen T, Oussayef N, Heeren TC, . . . Xuan Z (2014). A new scale of the US alcohol policy environment and its relationship to binge drinking. Am J Prev Med, 46(1), 10–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. (2016, January 2016). Alcohol facts and statistics. Alcohol and your health. Retrieved from http://pubs.niaaa.nih.gov/publications/AlcoholFacts&Stats/AlcoholFacts&Stats.pdf [Google Scholar]
- Neeleman J, & Lewis G (1999). Suicide, religion, and socioeconomic conditions. An ecological study in 26 countries, 1990. J Epidemiol Community Health, 53(4), 204–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson JM (2009). Religion, spirituality, and mental health In Nelson JM (Ed.), Psychology, religion and spirituality (pp. 347–390). New York, NY: Springer Science and Business Media LLC. [Google Scholar]
- Newport F, & Gallup AM (2011). The Gallup Poll: Public Opinion 2010. Lanham, MD: The Rowman & Littlefield Publishing Group, Inc. [Google Scholar]
- Pan Y. j., Stewart R, & Chang C. k. (2013). Socioeconomic disadvantage, mental disorders and risk of 12-month suicide ideation and attempt in the National Comorbidity Survey Replication (NCS-R) in US . Soc Psychiatry Psychiatr Epidemiol, 48(1), 71–79. doi: 10.1007/s00127-012-0591-9 [DOI] [PubMed] [Google Scholar]
- Pennock PE (2012). The number one social problem of our time: American Protestants and temperance politics in the 1950s. J Church State, 54(3), 375–405. doi: 10.1093/jcs/csr086 [DOI] [Google Scholar]
- Pescosolido BA, & Georgianna S (1989). Durkheim, suicide, and religion: toward a network theory of suicide. Am Sociol Rev, 54(1), 33–48. [PubMed] [Google Scholar]
- Pew Forum on Religion and Public Life. (2008). The religious composition of the United States In U.S. religious landscape survey. Washington, DC: Pew Research Center. [Google Scholar]
- Pew Forum on Religion and Public Life. (2014). Religious Landscape Study: racial and ethnic composition. Retrieved from Washington, DC: http://www.webcitation.org/query?url=http%3A%2F%2Fwww.pewforum.org%2Freligious-landscape-study%2Fracial-and-ethnic-composition%2F&date=2017-07-24
- Ransome Y, & Gilman SE (2016). The role of religious involvement in black-white differences in alcohol use disorders. J Stud Alc Drugs, In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasic DT, Belik S-L, Elias B, Katz LY, Enns M, & Sareen J (2009). Spirituality, religion and suicidal behavior in a nationally representative sample. J Affect Disord, 114(1–3), 32–40. doi: 10.1016/j.jad.2008.08.007 [DOI] [PubMed] [Google Scholar]
- Rehkopf DH, & Buka SL (2006). The association between suicide and the socio-economic characteristics of geographical areas: A systematic review. Psychol Med, 36(02), 145–157. doi:doi: 10.1017/S003329170500588X [DOI] [PubMed] [Google Scholar]
- Sahgal N, Smith G, & Center PR (2009). A religious portrait of African Americans. Retrieved from http://www.webcitation.org/query?url=http%3A%2F%2Fwww.pewforum.org%2F2009%2F01%2F30%2Fa-religious-portrait-of-african-americans%2F&date=2018-09-27
- Sampson RJ, & Groves WB (1989). Community structure and crime: esting social-disorganization theory. Am J Sociol, 94(4), 774–802. [Google Scholar]
- Shield KD, Gmel G, Kehoe-Chan T, Dawson DA, Grant BF, & Rehm J (2013). Mortality and potential years of life lost attributable to alcohol consumption by race and sex in the United States in 2005. PLoS One, 8(1), e51923. doi: 10.1371/journal.pone.0051923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith C (2000). Christian America? : what evangelicals really want. Berkeley, CA: University of California Press. [Google Scholar]
- Smith NDL, & Kawachi I (2014). State-level social capital and suicide mortality in the 50 US states. Soc Sci Med, 120, 269–277. [DOI] [PubMed] [Google Scholar]
- Social Explorer. (2015). Census 2000 Social Explorer Tables (SE). Retrieved from http://www.socialexplorer.com/pub/reportdata/HtmlResults.aspx?reportid=R10911132
- Stack S (1983). The effect of the decline in institutionalized religion on suicide, 1954–1978. J Sci Study Relig, 22(3), 239–252. [PubMed] [Google Scholar]
- Stark R (1987). Religion and deviance: A new look In Laufer W & Day JM (Eds.), Crimes, Values, and Religion (pp. 111–120). Norwood, NJ: Ablex Publishing Corporation. [Google Scholar]
- Stark R, Kent L, & Doyle DP (1982). Religion and delinquency: the ecology of a “lost” relationship. J Res Crime Delinq, 19(1), 4–24. doi: 10.1177/002242788201900102 [DOI] [Google Scholar]
- StataCorp. (2015). Stata statistical software: Release 14.0. In. College Station, TX: StataCorp LP. [Google Scholar]
- Stroope S, & Baker JO (2018). Whose moral community? religiosity, secularity, and self-rated health across communal religious contexts. J Health Soc Behav, 59(2), 185–199. [DOI] [PubMed] [Google Scholar]
- Taylor RJ, Chatters LM, & Brown RK (2014). African American religious participation. Rev Relig Res, 56(4), 513–538. doi: 10.1007/s13644-013-0144-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Association of Religion Data Archives. (nd). Religious Congegations and Membership Study, 2000 (Counties File). Retrieved from http://www.thearda.com/Archive/Files/Descriptions/RCMSCY.asp
- The Pew Charitable Trusts, & MacAurthur Foundation. (2015). Mental health and the role of the states. Retrieved from http://www.pewtrusts.org/~/media/assets/2015/06/mentalhealthandroleofstatesreport.pdf
- Torgler B, & Schaltegger C (2014). Suicide and religion: new evidence on the differences between Protestantism and Catholicism. J Sci Study Relig, 53(2), 316–340. [Google Scholar]
- Toussaint L, Wilson CM, Wilson LC, & Williams DR (2015). Religiousness and suicide in a nationally representative sample of Trinidad and Tobago adolescents and young adults. Soc Psychiatry Psychiatr Epidemiol, 50(9), 1441–1450. doi: 10.1007/s00127-015-1045-y [DOI] [PubMed] [Google Scholar]
- van Tubergen F, te Grotenhuis M, & Ultee W (2005). Denomination, religious context, and suicide: neo-Durkheimian multilevel explanations tested with individual and contextual data. Am J Sociol, 111(3), 797–823. [Google Scholar]
- VanderWeele TJ, Li S, Tsai AC, & Kawachi I (2016). Association between religious service attendance and lower suicide rates among US women. JAMA psychiatry, 73(8), 845–851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vilhjalmsson R, Sveinbjarnardottir E, & Kristjansdottir G (1998). Factors associated with suicide ideation in adults. Soc Psychiatry Psychiatr Epidemiol, 33(3), 97–103. [DOI] [PubMed] [Google Scholar]
- Vilhjálmsson R, Sveinbjarnardottir E, & Kristjansdottir G (1998). Factors associated with suicide ideation in adults. Soc Psychiatry Psychiatr Epidemiol, 33(3), 97–103. [DOI] [PubMed] [Google Scholar]
- Wilkinson RG, & Marmot MG (2003). Social determinants of health: The solid facts, 2nd Edition Copenhagen, DK: World Health Organization. [Google Scholar]
- Wingate LR, Bobadilla L, Burns AB, Cukrowicz KC, Hernandez A, Ketterman RL, . . . Sachs-Ericsson N (2005). Suicidality in African American men: the roles of southern residence, religiosity, and social support. Suicide Life Threat Behav, 35(6), 615–629. [DOI] [PubMed] [Google Scholar]


