Abstract
Background
Common bile duct (CBD) stones are extracted with a basket or balloon during ERCP with sphincterotomy. However, some stones are difficult to extract by conventional means. Cholangioscopy with lithotripsy is a modality to treat these difficult stones. We describe the clinical efficacy of single-operator per oral cholangioscopy (SOPOC) for difficult stones and discuss cost savings by avoiding surgical intervention.
Methods
Retrospective chart review was performed for all patients referred for difficult CBD stones. Clinical success was defined as clearing the duct of all stones. The cost of cholangioscopy (in $CDN) was calculated by adding all costs associated with the procedure(s), surgery, hospital stay or treatment of adverse events. This cost was compared with the projected cost of surgical bile duct exploration.
Results
A total of 51 patients (35 female) with a mean age of 66 years underwent 58 SOPOC procedures. Median procedure time was 67 minutes (95% CI, 61.5–73.5). The CBD was successfully cleared in 47 of 51 patients (93%). Minor adverse events were seen in seven patients (14%). The actual average per procedure cost was $4555±$2647. This compares with a projected cost of $7766 and $6175 for open and laparoscopic bile duct exploration, with a cost-per-case saving of $3210 and $1619, respectively.
Conclusion
SOPOC with lithotripsy is highly effective and safe for the treatment of difficult common bile duct stones. In addition, significant cost savings may be realized by avoiding surgical bile duct exploration.
Keywords: Cholangioscopy, Cost-comparison, Lithotripsy, Stones
INTRODUCTION
Common bile duct (CBD) stones occur in approximately 10%–15% of patients with cholelithiasis (1). Conventional treatment for CBD stones currently entails endoscopic retrograde cholangiopancreatography (ERCP) with sphincterotomy and extraction of stones with a balloon catheter or basket (2). The most cost-effective management of these stones in patients undergoing cholecystectomy appears to be peri-operative ERCP (3). However, in 10%–15% of patients with CBD stones, the stones are not amenable to conventional ERCP, including additional intervention such as balloon sphincteroplasty and mechanical basket lithotripsy (4–8). Such ‘difficult’ CBD stones are large, multiple-stacked and faceted (square-shaped) and include those that are impacted in the CBD, or located proximal to a stricture (Figure 1). With failed conventional ERCP, the accepted choice of treatment for these stones would be open CBD exploration (OCBDE) or laparoscopic CBD exploration (LCBDE). Furthermore, patients with prior cholecystectomy who present with CBD stones would need to undergo surgery exclusively for the CBDE. Per oral cholangioscopy (POC) and electrohydraulic lithotripsy (EHL) provide an alternative treatment for such patients to avoid surgical management of these difficult CBD stones pre- or post-cholecystectomy (9–11). To date, no studies have assessed the cost-efficacy associated with treatment of difficult CBD stones with POC. Herein, we evaluate the clinical impact of single-operator POC (SOPOC) on the treatment of difficult CBD stones, as well as assess the cost of SOPOC compared with surgical bile duct exploration.
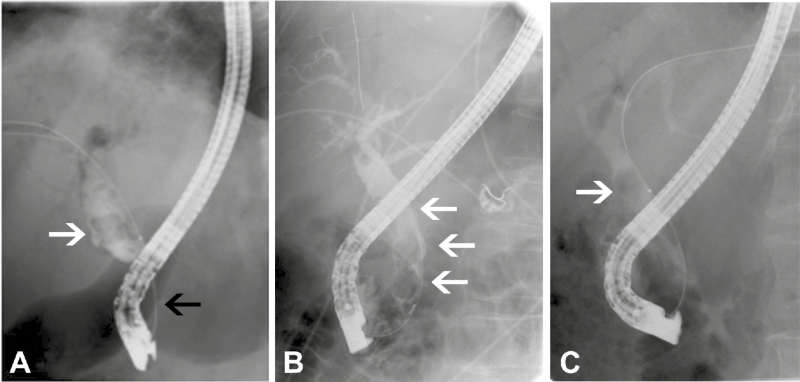
Figure 1.
‘Difficult’ common bile duct (CBD) stones. A, single, large, faceted stone (white arrow) proximal to a CBD stricture (black arrow). B, multiple, stacked stones (arrows). C, stone impacted in CBD (arrow).
METHODS
We performed a retrospective chart review of SOPOC procedures done at the University of Alberta Hospital (UAH) referred for difficult CBD stones for which conventional ERCP was unsuccessful. The goal of treatment was to clear the CBD of the indicated stone(s).
All patients referred for SOPOC had at least one previous ERCP, during which conventional methods to extract the stone(s) failed. Most of these cases were referred by high-volume endoscopists performing >75 ERCPs/year. Whenever possible, cases (procedure note and fluoroscopy images) were reviewed before performing SOPOC. If the stone(s) fit the definition of a ‘difficult’ stone, as per our criteria, and if conventional methods of stone extraction (including mechanical basket lithotripsy and dilation-assisted stone extraction) had been employed previously and failed, then we chose to proceed directly to SOPOC. All SOPOC procedures, done as outpatient day procedures, were planned electively and scheduled with general anesthesia (GA). However, if GA was unavailable, endoscopist-administered conscious sedation was performed.
SOPOC procedures were initially performed with the original SpyGlass Legacy single-operator direct visualization system (Boston Scientific Corporation, Marlborough, MA, USA). However, a switch was made to the newer Digital SpyGlass (DS) system (Boston Scientific Corporation, Marlborough, MA, USA) when it became commercially available.
Procedure
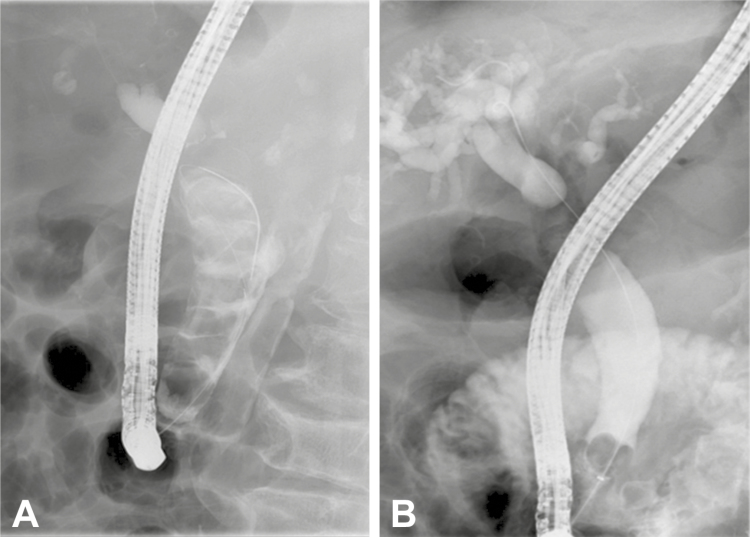
After the removal of a previously placed biliary stent, cannulation of the CBD with the SOPOC probe was performed with or without the use of a guidewire. Our protocol is for initiating direct cholangioscopy without injecting radiographic contrast, as we believe that the density of the contrast dye may impede optimal cholangioscopic visualization. This was particularly true for the Legacy system, but with the enhanced and improved visualization with the DS system, this is less of a concern. Our preferred solution for irrigation in the CBD is 0.9% normal saline, as it also aids in conducting the electrical impulse required for EHL. Once the stone was visualized, EHL was performed using the Autolith EHL generator and a 1.9 French (Fr) EHL probe (Nortech, Northgate Technologies, Elgin, IL, USA). An initial power setting of 50 watts and a frequency of five pulses per second were used, but depending upon the impact on the stone, these parameters were changed during the procedure. The number of EHL applications was purely at the discretion of the endoscopist based on visual fissuring and fragmentation of the stone. When the stone was optimally fragmented, the SOPOC system was removed, and then conventional means of stone extraction by standard ERCP were used to clear the CBD of all fragments. A stent was only replaced if duct clearance could not be guaranteed and a repeat procedure was being contemplated. Repeat ERCP with or without cholangioscopy was performed as necessary and at the discretion of the endoscopist. Clinical success was defined as complete clearance of the CBD (Figure 2) as evidenced by cholangiography done during the index procedure or on any subsequent procedure done to extract any remaining fragments.
Figure 2.
ERCP images of the common bile duct before (A) and after (B) extraction of multiple stacked stones with complete clearance of CBD.
The average cost per case of extracting a difficult CBD stone (or stones) was calculated by adding the cumulative costs of all ERCPs conducted following the initial failed ERCP. This included the index SOPOC and any subsequent ERCPs with or without cholangioscopy until the CBD was clear. These include the cost of the SOPOC (Legacy or DS), the EHL probes, and the cost of equipment based on actual usage of extraction/assisting devices (snare, guidewire, balloon extraction catheter, balloon dilator, extraction basket, rat-tooth forceps, stent retriever, etc.). Anesthesia or sedation and reimbursement of all personnel involved in the procedure, including the gastroenterologist, nursing staff, technical staff and anesthesiologist—if present—were also added to the total cost (Table 1). Costs associated with any adverse event, subsequent surgery or hospital stay arising from the procedure were also included in this cost analysis. The upfront capital cost to purchase the SOPOC system was not included in the cost analysis. Similarly, we did not include capital cost for the purchase of surgical instruments.
Table 1.
Cost, in $CDN, of ERCP (with SpyGlass+EHL)
| Diagnostic imaging component | |
| Radiology tech time, benefits, and clerical costs | 55.56 |
| Radiographic film (digital) and contrast | 81.84 |
| Fluoroscopy equipment service package (per case) ($25,000 per year/800 ERCPs) | 31.25 |
| Radiologist reimbursement fee | 29.03 |
| Gastroenterology Component | |
| Nursing salary and benefits (RN for procedure room and LPN for recovery room) | |
| RN | 60.25 |
| LPN | 39.94 |
| Medications (unit price) | |
| Midazolam (per mg) | 1.25 |
| Fentanyl (per 100 μg) | 0.44 |
| Diazemuls (per 5 mg) | 1.15 |
| Medical and surgical supplies (including gloves, IV tubing, O2 tubing etc.), scope disinfection and laundry | 80.00 |
| Endoscopy equipment service package (service contract with vendor per ERCP) | 12.00 |
| SpyGlass cost/case (Legacy and DS) | |
| Legacy ($950+$375) | 1325.00 |
| DS (based on purchase of a pack of 10 probes) | 1695.00 |
| EHL probe (single use) | 395.00 |
| SpyBite forceps | 595.00 |
| Sphincterotome | 275.00 |
| Balloon extraction catheter | 140.00 |
| Locking device | 90.00 |
| Snare | 11.00 |
| Extraction basket | 270.00 |
| Balloon dilator | 150.00 |
| Guide wire | 100.00 |
| Stent—Plastic | 145.00 |
| Stent—Metal | 1300.00 |
| Soehendra stent retriever | 199.00 |
| Rat-tooth forceps | 171.00 |
| Gastroenterologist reimbursement fees | |
| ERCP | 262.18 |
| Cholangioscopy | 164.85 |
| Electrohydraulic lithotripsy | 113.99 |
| Stone extraction | 57.00 |
| Anesthesia Component | |
| Anesthesia machine service package | 27.00 |
| Anesthesia cost/case for GA (cost of gases, tubing, ECG leads etc.) | 100.00 |
| Anesthesia tech time and benefits ($50/hr) | 50.00 |
| Anesthesiologist reimbursement ($18.10 per 5 min) | 217.20 |
| Inpatient component | |
| Cost of medical ward/day | 973.00 |
The average actual cost of SOPOC was compared with the calculated costs of surgical alternatives, such as OCBDE and LCBDE. This projected surgical cost included reimbursement of the surgeon, anesthesiologist, nursing and technical staff, and the cost related to the postoperative length of stay (LOS) in hospital (Table 2). The average LOS was extracted from expert opinion from our local surgeons and from published data from the provincial Alberta Health Services (AHS) database. For the purposes of this study, the accepted LOS was two days for LCBDE and four days for OCBDE. Published literature, however, has LOS data (average LOS for LCBDE 4.2 days and for OCBDE 12.6 days) that does not reflect the current pattern of practice at our hospital (12). We chose not to include the additional cost of a cholecystectomy (for those patients that had concomitant cholelithiasis), as our intent is simply to compare the costs associated with therapeutic intervention for difficult CBD stones. All costs were calculated based on the current Alberta Health Services reimbursement schedule.
Table 2.
Cost, in $CDN, of CBD exploration ($CDN)
| Diagnostic imaging component (For intra-operative cholangiogram) |
OCBDE | LCBDE |
| Radiology tech time, benefits, and clerical costs | 55.56 | 55.56 |
| Radiographic film (digital) and contrast | 81.84 | 81.84 |
| Fluoroscopy equipment service package (per case) | 31.25 | 31.25 |
| Radiologist reimbursement fee | 29.03 | 29.03 |
| Surgery Component | ||
| Nursing salary and benefits (2–3 nurses for the procedure including recovery room) | 836.00 | 762.00 |
| Medical and surgical supplies (including surgical kit, gloves, IV tubing, O2 tubing etc.), sterilization and laundry | 620.00 | 1280.00 |
| Biliary Fogarty catheters (3–5 Fr) | 39.24 | 39.24 |
| Specimen collection bag | 180.00 | 180.00 |
| Guide wire | 42.00 | 42.00 |
| 8 mm balloon dilator | 140.00 | 140.00 |
| Choledochoscope cost per case (with light source/monitor etc., service contact with vendor) | 12.00 | 12.00 |
| Loop ligatures | 6.41 | 6.41 |
| T-tube | 15.00 | 15.00 |
| Surgeon reimbursement fee | 1024.28 | 1024.28 |
| Hospital LOS | 4 days | 2 days |
| Anesthesia Component | ||
| Anesthesia machine service package | 27.00 | 27.00 |
| Anesthesia cost/case for GA (cost of gases, tubing, ECG leads etc.) | 100.00 | 100.00 |
| Anesthesia tech time and benefits ($50/hr) | 91.66 | 75.00 |
| Anesthesiologist reimbursement ($18.10 per 5 min) | 398.20 | 325.80 |
| Inpatient component | ||
| Cost of ICU/day | 3296.00 | 3296.00 |
| Cost of surgical ward/day | 1044.00 | 1044.00 |
STATISTICS
Descriptive statistics were used for continuous variables using mean or median, as appropriate, along with their corresponding 95% confidence intervals.
RESULTS
Patient Characteristics
Between April 2011 and June 2015, 51 patients were referred to the UAH for SOPOC for difficult CBD stones (Table 3). There were 35 females (69%), and the mean age was 66 years (range 30–88 years). Referrals were from received from other tertiary care hospitals in adjacent provinces (3 of 51 patients, 6%), local and regional community hospitals (13 of 51 patients, 25%) and from other endoscopists at our own hospital (35 of 51 patients, 69%). Difficult CBD stones (Figure 1) were defined as those that were single-large (26 of 51), multiple-large and stacked (15 of 51), faceted (one of 51), impacted (seven of 51) or located proximal to a stricture in the CBD (eight of 51). There was overlap of categories in seven patients.
Table 3.
Patient characteristics
| Patients (n) | 51 |
| Age in years, mean (range) | 66 (30–88) |
| Gender (F) | 35 |
| Indication for SOPOC/EHL (n) | |
| Single large stone | 26 |
| Multiple stacked stones | 15 |
| Faceted stone | 1 |
| Impacted stone | 7 |
| Stone proximal to stricture | 8 |
| Prior cholecystectomy (n) | 27 |
| Prior ERCPs (n) | 108 |
| SOPOCs (n) | 58 |
| SOPOC procedure time (minutes), median (95% CI) (range) | 67 (61.5, 73.5) (24–124) |
| Adverse events secondary to SOPOC/EHL | 87 |
| Spontaneously-resolving EHL-induced CBD trauma | 4 |
| GE junction tear (plastic stent-induced) | 1 |
| Wire-induced CD stump leak | 1 |
| Post-ERCP pancreatitis | 1 |
| Subsequent procedures | |
| ERCP | 14 |
| Cholecystectomy | 2 |
| OCBDE | 1 |
| LC-OC+CBDE | 1 |
GE, gastro-esophageal; CD, cystic duct; LC-OC, laparoscopic cholecystectomy converted to open cholecystectomy.
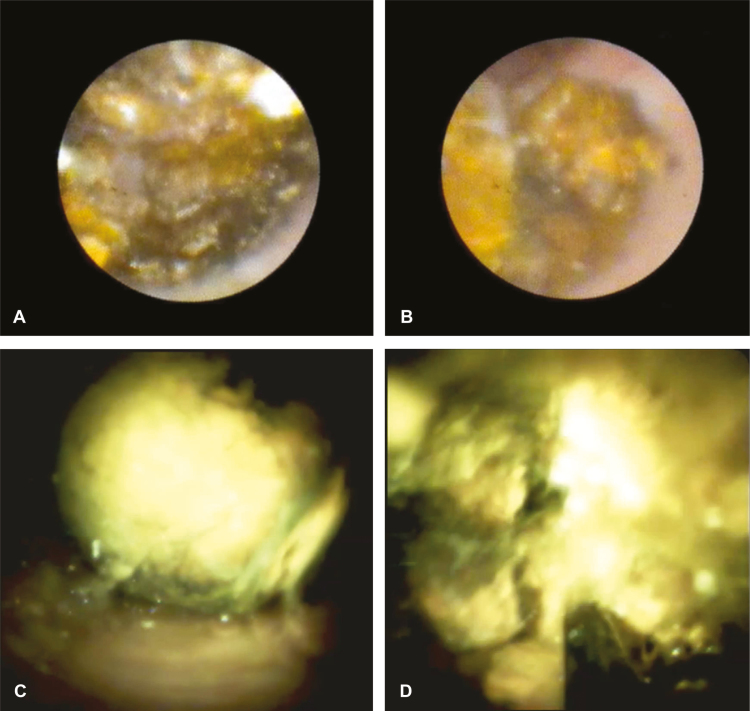
A total of 58 ERCPs with SOPOC were performed in these 51 patients by a single endoscopist (GS). All ERCPs were performed using the Olympus TJ180 side-viewing duodenoscope (Olympus America, Melville, NY USA). Of these 58 SOPOC procedures, 49 were performed with the original SpyGlass Legacy system and nine with the SpyGlass Digital system that was acquired in April 2015 (Figure 3). The median time per procedure was 67 ± 6.5 minutes (95% confidence interval, 61.5–73.5), calculated from 56 of the 58 procedures for which procedure time was noted. The range of time for the whole cohort was 24–124 minutes. The total time per procedure includes not only the time spent on SOPOC and EHL but also the time spent on extracting the stone fragments. Forty-eight of these procedures were done under general anesthesia (with an attendant anesthesiologist), and 10 were done with topical xylocaine anesthesia and conscious sedation using midazolam and fentanyl (administered and monitored by the nurse and endoscopist).
Figure 3.
SpyGlass Legacy images (A and B) and SpyGlass DS images (C and D) before and after fragmentation of stone.
Twenty-seven patients previously underwent cholecystectomy (Table 3). Two had a cholecystectomy after a successful removal of CBD stones by SOPOC, one underwent cholecystectomy with CBDE after a failed SOPOC, and one had an open CBDE after a failed SOPOC. One patient with a prior cholecystectomy also had undergone a failed CBDE prior to referral for SOPOC.
A total of 108 ERCPs were performed before referral for SOPOC. Twenty-three patients had one ERCP, 19 patients had two ERCPs, four patients had three ERCPs, one patient had 4, one patient had 6, while one patient had 25 ERCPs (for routine plastic stent replacement every three months over the previous five years) before SOPOC. This last patient was found to have a 4 cm CBD stone that was not amenable to endoscopic extraction, and she was deemed not to be a surgical candidate by her local surgeon. One patient was referred directly for SOPOC without a prior ERCP.
Clinical Success
All patients referred for SOPOC underwent cholangioscopy prior to cholangiography. Of the 58 SOPOC procedures, EHL was performed in 52 procedures by utilizing 53 probes (one patient required a second EHL probe after the first one had burnt out, presumably because of prolonged use). Successful fragmentation of stone(s) and extraction with duct clearance were possible in 50 of 52 procedures where EHL was used (overall therapeutic efficacy of EHL: 96%) for difficult CBD stones. The actual number of pulses fired was not calculated, and the duration of EHL was purely based on the discretion of the endoscopist based on visual evidence of fracturing and fragmentation. EHL was not used in six procedures: in two patients, there were no stones visible in the CBD on cholangioscopy, and cholangiography revealed a clear duct as well; in another two patients, the CBD stones were above a stricture and not of a size for which EHL was necessary (the strictures were deemed to be the more clinically relevant and significant pathology); in the remaining two patients, stones were deemed to be of a size small enough that they were extracted without the need for EHL.
On an intention-to-treat basis (i.e., with the intent of referral for SOPOC being clearance of the duct), SOPOC was successful in clearing the CBD in 47 of 51 patients (overall efficacy 93%). The presence of a CBD stricture precluded stone extraction in two patients (one with primary sclerosing cholangitis and one with a benign stone-induced stricture), and the stones were of a size that did not warrant EHL. One patient had a large stone impacted at the cystic duct confluence with the CBD and could not be fragmented by EHL. This patient underwent OCBDE and was found to have Mirizzi’s syndrome and required repair of the cholecyst-choledochal fistula. Another patient had a 4–5 cm stone concretion around a metal stent placed five years previously for a benign CBD stricture. EHL was unsuccessful, and a second, longer metal stent was placed for drainage.
In eight patients, an additional 14 ERCPs were performed after SOPOC. Two of these patients had a total of seven ERCPs, but the indication for these subsequent procedures was a CBD stricture rather than the stone. Therefore, the cost of these extra procedures was not factored into the overall cost of SOPOC. In the remaining six patients, seven ERCPs were required to clear the CBD of remnant fragments of stone. The cost associated with these procedures was included in the overall cost of SOPOC.
Adverse Events
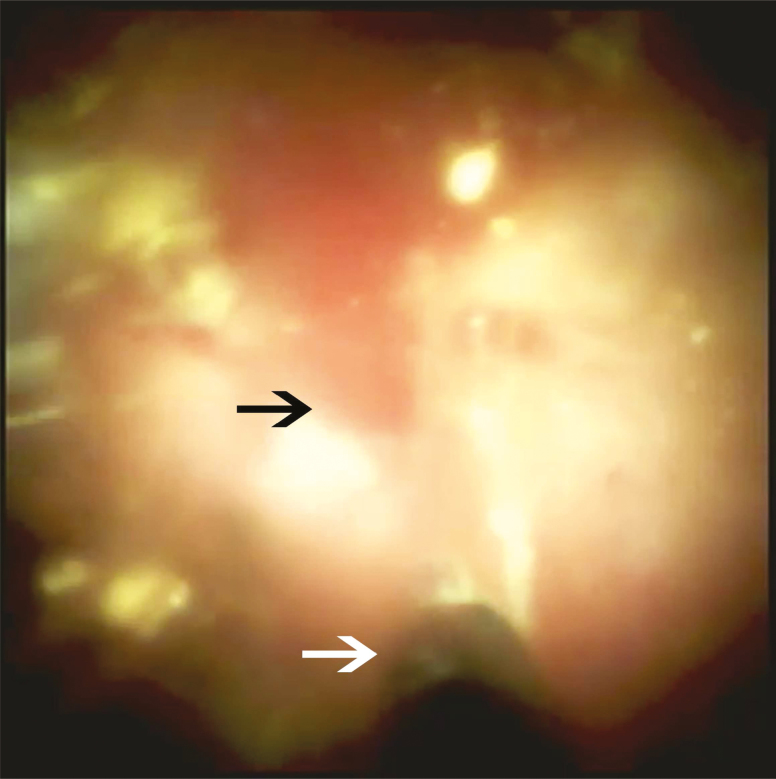
A total of seven patients (14%) suffered minor adverse events from SOPOC. Four patients suffered mild bleeding from the CBD as a result of contact trauma from EHL (Figure 4). All of these were self-resolving, as observed during direct cholangioscopy, and did not require any further intervention. One patient was noticed to have a tear at the gastroesophageal junction. We feel this occurred as a result of snare extraction of an 11.5 Fr stent. After the ERCP was completed, this tear was repaired with eight clips placed with a gastroscope, and the patient did well. One patient with stone fragments in the cystic duct stump with a prior cholecystectomy incurred a cystic duct stump leak caused by the guidewire used for the stone extraction. A plastic stent was inserted during the Spyglass ERCP and was removed in a subsequent ERCP. One patient developed acute post-ERCP pancreatitis despite a previous sphincterotomy, and this resulted in a four-day hospital stay.
Figure 4.
Mild trauma (black arrow) to the common bile duct from electrohydraulic lithotripsy probe (white arrow).
Cost Comparison
The average cost of SOPOC was $4555±$2647 (range $2538–$14,923). We calculated the cost of OCBDE and LCBDE to be $7766 and $6175, respectively. The cost saved per patient by performing SOPOC compared with OCBDE and LCBDE was $3211 and $1620, respectively. The rate of adverse events for CBDE as extracted from published data is 3.2%. The total treatment cost of the most common surgical adverse events was calculated to be $4977 for a bile leak, $5216 for an intra-abdominal hemorrhage, and $3701 for an intra-abdominal abscess. These costs have not been added to the cost of OCBDE and LCBDE listed above.
DISCUSSION
Difficult CBD stones can present technical challenges to attempts at removal during ERCP. These stones are large (single or multiple and stacked), faceted (square-shaped), impacted or situated proximal to a stricture, and thus not amenable to conventional modalities of treatment such as balloon extraction or engagement within a retrieval basket. Additional interventions such as mechanical lithotripsy and balloon sphincteroplasty may also not be helpful because of size, shape or impaction of the stone(s).
The options for removal of such difficult CBD stones are extra-corporeal shock-wave lithotripsy (ESWL), cholangioscopy with intra-ductal lithotripsy (with EHL or laser) and CBDE. In a comparative study, POC with laser lithotripsy was found to be more effective and safer than ESWL for fragmentation of CBD stones (97% versus 73%, respectively) (13). Furthermore, ESWL requires subsequent ERCP for removal of fragmented stones. POC using mother-baby cholangioscopy with EHL reported stone clearance in 90% of patients (14). The authors recommend the use of POC as the first line treatment for difficult stones before using other modalities. However, because of the fragility of the baby endoscope, mother-baby cholangioscopy has fallen out of favour amongst most biliary endoscopists.
With the introduction of the SOPOC system, there has been renewed interest in the diagnostic and therapeutic abilities within the CBD. The original SpyGlass Legacy system has recently been upgraded to the Digital SpyGlass system with significant improvements, such as enhanced optical resolution, wider field of view and better operator handling. Using the SOPOC system in our referral institution, we achieved a technical success rate of 96%, with fragmentation of difficult CBD stones with EHL and a duct clearance rate of 93% on an intention-to-treat basis. These results are in keeping with a recent meta-analysis of 31 studies showing a technical success rate of 91% and stone clearance in 88% (15). However, there have been no studies comparing the cost of cholangioscopy with conventional alternatives such as surgical bile duct exploration.
Adverse events seen in our study were higher than that reported with CBDE (14% versus 3.2%), but they were all minor and self-resolving, except one patient requiring a four-day hospitalization for mild post-ERCP pancreatitis. Adverse events associated with surgery (e.g., bile leak, intra-abdominal hemorrhage, or intra-abdominal abscess) are more severe and have a greater impact on patient quality of life and longer hospital LOS, which further adds to health care resource utilization.
In the Canadian health care system, the upfront capital cost of investing in a SOPOC system, such as the SpyGlass system, is a significant deterrent to the acquisition of such technology. However, our study shows that even in the small subset of patients with difficult CBD stones who pose a significant medical challenge, the procedure is very effective and has an excellent safety profile. We believe this justifies the adoption of SOPOC in a limited number of specialized centers so that the technology is available for direct patient care. In addition, the significant cost savings realized by avoiding alternative methods of intervention—especially surgery (LCBDE and OCBDE—show that the technology is cost effective.
Our study analyzed the actual costs of SOPOC for difficult CBD stones compared with the alternative of surgical intervention. Most of the studies comparing endoscopic with surgical management of CBD stones address the issue in the context of cholecystectomy. A recent Cochrane review suggested the superiority of OCBDE over ERCP in managing CBD stones based on data from early endoscopic studies (2). They found no differences in the clinical efficacy or outcomes comparing LCBDE and pre- or post-cholecystectomy ERCP. However, they do not address the specific question of difficult CBD stones but instead deal with the issue of CBD stones when a cholecystectomy also needs to be done. In our cohort of 51 patients, 27 patients (53%) already had a previous cholecystectomy and would have had to undergo another surgical procedure in the event of failure of endoscopic treatment of these difficult CBD stones.
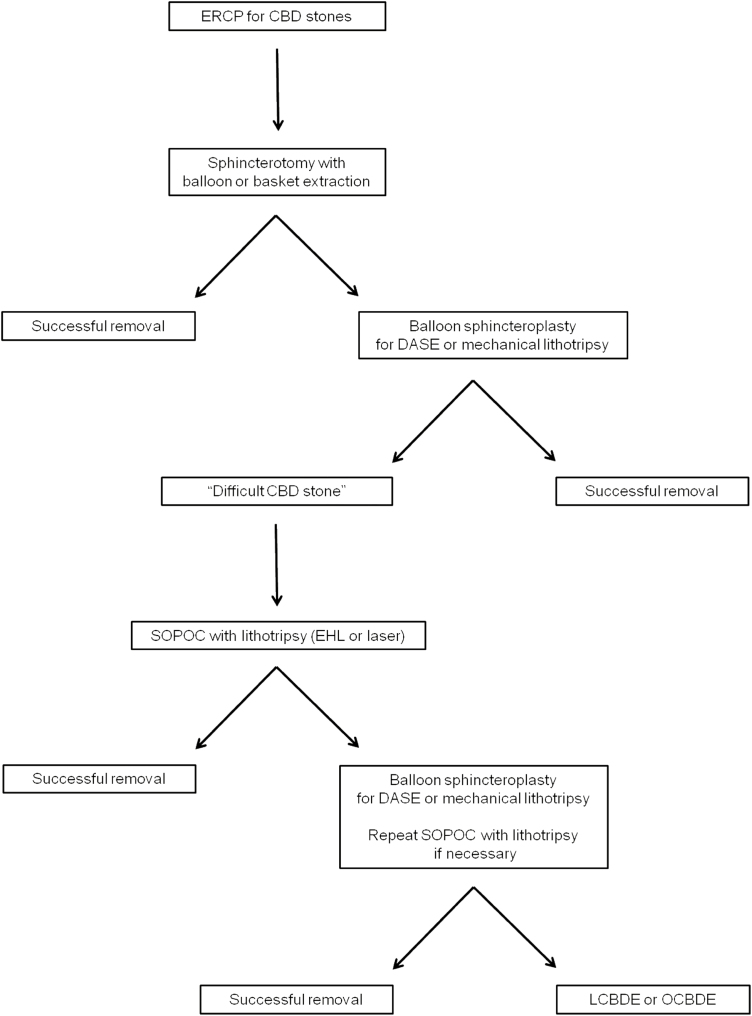
It is also important to note that our patient cohort had previously undergone an average of more than two ERCP procedures before being referred for SOPOC for difficult stones. We believe that further cost savings can be realized with the appropriate and timely identification of difficult CBD stones. Based on our experience, we propose an algorithmic approach to the management of these difficult CBD stones (Figure 5). Patients with CBD stones should undergo routine ERCP with conventional methods of stone removal such as sphincterotomy followed by balloon or basket extraction. If unsuccessful, advanced interventions such as mechanical lithotripsy and balloon sphincteroplasty should be performed during the index ERCP. If the endoscopist is not comfortable with these techniques, the patient should be referred to a tertiary care facility. Failure of these advanced interventions defines difficult CBD stones and the patient should be referred for SOPOC for further management. Streamlining and minimizing unnecessary procedures can realize further healthcare resource savings.
Figure 5.
Proposed algorithm for management of common bile duct (CBD) stones. ERCP, Endoscopic retrograde cholangiopancreatography; CBD, Common bile duct; DASE, Dilation-assisted stone extraction; SOPOC, Single-operator per oral cholangioscopy; EHL, electrohydraulic lithotripsy; LCBDE, laparoscopic common bile duct exploration; OCBDE, open common bile duct exploration.
We recognize that anesthesia services are not readily available at many centres. GA definitely allowed for a very comfortable procedure, not only for the patient but for the endoscopist as well, because these procedures can be fairly lengthy and laborious. Also, since a significant amount of saline is required for irrigation, and because some of this fluid can sequester in the fundus of the stomach with patients being in the left lateral position, endotracheal intubation ensured airway protection. Because the average procedure time for our cohort was slightly over an hour, GA was felt to be more beneficial than conscious sedation, especially in the extremely time-consuming cases. Other than the ease of performing procedures under GA, we do not feel that GA had any impact on the high rate of success. Procedures can be performed equally effectively provided patients are well sedated with conscious sedation. However, if this is not possible, we highly recommend repeating the procedure with GA.
There are several limitations of our study. First, this is a single-centre, single-operator experience that brings into question the generalizability of the results. However, the authors believe that similar results are achievable when procedures are done in a high-volume facility. Furthermore, most of the cases described were performed with the original SpyGlass Legacy system. The new Digital SpyGlass platform is significantly improved and makes it easier to achieve operator performance. Secondly, this is a retrospective observational study and does not address the comparison of efficacy and costs in a randomized, prospective manner. Moreover, because this is a comparison of actual costs of SOPOC versus calculated estimates of CBDE, we may have underestimated the true cost of surgical intervention, which may be greater due to adverse events not mentioned in this report and the associated increase in hospital LOS. So, in reality, the true difference in cost between SOPOC and CBDE may actually be greater than we have described.
In summary, SOPOC with EHL, done on an outpatient basis, is a highly effective treatment modality for difficult CBD stones and offers a less invasive approach compared with conventional surgical management by CBDE. Our study demonstrates that the cost-per-case savings compared with surgical management offsets the upfront capital cost and ongoing operational costs required for SOPOC and EHL. We recommend that SOPOC with EHL be adopted as the standard of care for treatment of difficult CBD stones after failure of conventional ERCP before CBDE.
ACKNOWLEDGMENTS
The authors wish to acknowledge the assistance of Ralph Ennis-Davis (Endoscopy Unit Manager, University of Alberta Hospital) and Dr. Michael Murphy, Dr. Barry Finegan (Department of Anesthesiology, University of Alberta Hospital) and Dr. Ronald Brisebois (Department of Surgery, University of Alberta Hospital) for their assistance in providing data information for this manuscript. Ethics approval was obtained from the Ethics Review Board of the University of Alberta (Study # Pro00057683). Author contributions: JS and GS acquired, analyzed and interpreted data. JS wrote the manuscript. JS, SVVZ and GS revised the manuscript and gave final approval.
Glossary
Abbreviations
- CBD
common bile duct
- ERCP
endoscopic retrograde cholangiopancreatography
- $CDN
Canadian dollars
- OCBDE
open CBD exploration
- LCBDE
laparoscopic CBD exploration
- POC
per oral cholangioscopy
- EHL
electrohydraulic lithotripsy
- SOPOC
single-operator per oral cholangioscopy
- UAH
University of Alberta Hospital
- GA
general anesthesia
- DS
Digital SpyGlass
- Fr
French
- LOS
Length of stay
- AHS
Alberta Health Services
- ESWL
Extra-corporeal shock-wave lithotripsy
This study has been presented in abstract form as a poster presentation at the Canadian Digestive Disease Week, February 26–29, 2016, Montreal, Quebec, Canada and at the Digestive Disease Week, May 21–24, 2016, San Diego, California, USA.
Conflicts of Interest
Dr. Gurpal Sandha is a consultant and member of the biliary medical advisory board for Boston Scientific Corporation and has received honoraria for speaking and proctoring. Jaskiran Sandha and Dr. Sander Veldhuyzen van Zanten have no conflicts of interest relevant to this study.
References
- 1. Soltan HM, Kow L, Toouli J. A simple scoring system for predicting bile duct stones in patients with cholelithiasis. J Gastrointest Surg. 2001;5(4):434–7. [DOI] [PubMed] [Google Scholar]
- 2. Dasari BV, Tan CJ, Gurusamy KS, et al. Surgical versus endoscopic treatment of bile duct stones. Cochrane Database Syst Rev 2013;12:CD003327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Brown LM, Rogers SJ, Cello JP, et al. Cost-effective treatment of patients with symptomatic cholelithiasis and possible common bile duct stones. J Am Coll Surg 2011;212(6):1049–60.e1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Binmoeller KF, Schafer TW. Endoscopic management of bile duct stones. J Clin Gastroenterol 2001;32(2):106–18. [DOI] [PubMed] [Google Scholar]
- 5. McHenry L, Lehman G. Difficult bile duct stones. Curr Treat Options Gastroenterol 2006;9(2):123–32. [DOI] [PubMed] [Google Scholar]
- 6. Neuhaus H. Endoscopic and percutaneous treatment of difficult bile duct stones. Endoscopy 2003;35(8):S31–4. [DOI] [PubMed] [Google Scholar]
- 7. van der Velden JJ, Berger MY, Bonjer HJ, et al. Percutaneous treatment of bile duct stones in patients treated unsuccessfully with endoscopic retrograde procedures. Gastrointest Endosc 2000;51(4 Pt 1):418–22. [DOI] [PubMed] [Google Scholar]
- 8. Yasuda I, Itoi T. Recent advances in endoscopic management of difficult bile duct stones. Dig Endosc 2013;25(4):376–85. [DOI] [PubMed] [Google Scholar]
- 9. Trikudanathan G, Arain MA, Attam R, et al. Advances in the endoscopic management of common bile duct stones. Nat Rev Gastroenterol Hepatol 2014;11(9):535–44. [DOI] [PubMed] [Google Scholar]
- 10. Alameel T, Bain V, Sandha G. Clinical application of a single-operator direct visualization system improves the diagnostic and therapeutic yield of endoscopic retrograde cholangiopancreatography. Can J Gastroenterol 2013;27(1):15–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Chen YK, Parsi MA, Binmoeller KF, et al. Single-operator cholangioscopy in patients requiring evaluation of bile duct disease or therapy of biliary stones (with videos). Gastrointest Endosc 2011;74(4):805–14. [DOI] [PubMed] [Google Scholar]
- 12. Grubnik VV, Tkachenko AI, Ilyashenko VV, et al. Laparoscopic common bile duct exploration versus open surgery: Comparative prospective randomized trial. Surg Endosc 2012;26(8):2165–71. [DOI] [PubMed] [Google Scholar]
- 13. Neuhaus H, Zillinger C, Born P, et al. Randomized study of intracorporeal laser lithotripsy versus extracorporeal shock-wave lithotripsy for difficult bile duct stones. Gastrointest Endosc 1998;47(5):327–34. [DOI] [PubMed] [Google Scholar]
- 14. Arya N, Nelles SE, Haber GB, et al. Electrohydraulic lithotripsy in 111 patients: A safe and effective therapy for difficult bile duct stones. Am J Gastroenterol 2004;99(12):2330–4. [DOI] [PubMed] [Google Scholar]
- 15. Korrapati P, Ciolino J, Wani S, et al. The efficacy of peroral cholangioscopy for difficult bile duct stones and indeterminate strictures: A systematic review and meta-analysis. Endosc Int Open 2016;4(3):E263–75. [DOI] [PMC free article] [PubMed] [Google Scholar]