Supplemental Digital Content is available in the text
Keywords: acupuncture, Bell's palsy, meta-analysis, randomized controlled trial, systematic review
Abstract
Background:
Bell's palsy or idiopathic facial paralysis is an acute facial paralysis caused by the inflammation of facial nerve. Several previous studies showed that acupuncture was beneficial in the treatment of facial paralysis. However, its effectiveness is still controversial compared with drug therapy. Therefore, this systematic review and meta-analysis was performed to assess the efficacy of acupuncture for Bell's palsy.
Methods:
This is a systematic review and meta-analysis of clinical studies among patients with Bell's palsy. We did a systematic literature search in PubMed, Embase, and the Cochrane Register of Controlled Trials to identify studies comparing the efficacy of acupuncture and drug treatment in treating facial paralysis. The search was last updated on July 2018.
Results:
The study included 11 randomized controlled trials with an overall sample of 1258 individuals. Acupuncture treatment was associated with an increased cure rate [relative risk (RR) = 1.77, 95% confidence interval (CI): 1.41–2.21], with significant heterogeneity in the pooled results (I2 = 67%, P = .0008). There was a significant difference in total effective rate in acupuncture and drug treatment for Bell's palsy (RR = 1.18,95% CI: 1.07–1.31), with substantial heterogeneity (I2 = 90%, P < .00001).
Conclusion:
Although there was not enough evidence to prove its safety, acupuncture seems to be an effective therapy for Bell's palsy. Results of the present meta-analysis showed that acupuncture was associated with increased cure rate and total effective rate of the treatment of Bell's palsy in comparison with drugs. However, the results should be interpreted cautiously, because of the poor quality and heterogeneity of the included studies. In the future, more and more high quality randomized controlled trials (RCT) are needed to prove the safety and effectiveness of acupuncture.
1. Introduction
Bell's palsy, also known as acute idiopathic facial paralysis, is an acute peripheral facial neuropathy which is the most common cause of lower motor neuron facial palsy.[1] The common clinical features of Bell's palsy include sudden onset, unilateral, weakness of the facial nerve, auricular pain, headache, hyperacusis, dysgeusia, dry eye, and epiphora.[2,3] Sometimes, it is accompanied by a subjective change in taste sensation, facial sensation and over activity.[4] However, some patients recovered with insignificant sequelae, and may had permanent diminished facial function, contracture or synkinesis.[5] The incidence of Bell's palsy is about 11 to 40 per 100,000 adults each year,[6] and 1 in 60 people may have a fatal risk.[7] According to the data of the United States (US), there were more than 60,000 people that developed Bell's palsy in the US each year.[8] Therefore, the treatment of this disease has received widespread attention around the world.
Because of the unclear etiology of Bell's palsy, there were a variety of treatment options. The treatments usually include antiviral drugs,[9] Vitamin B drugs,[10]corticosteroids,[11] surgery,[12] physiotherapy, acupuncture treatment and others. In the treatment of facial paralysis, some neurotrophic and neurorestorative drugs are often used. Vitamin B was beneficial for the recovery of peripheral nerve function and can be used orally.[13] Corticosteroids have long been used in Bell's palsy due to their potent anti-inflammatory effects and have proven to be an effective treatment. Previous studies showed that there were evidences of the presence of the herpes simplex virus in some cases of Bell's palsy.[14,15] Thus, antiviral agents were applied in some patients with Bell's palsy. As optional treatments for Bell's palsy, surgical decompression of facial nerve or physical therapy has been suggested in several studies,[16] but some studies found that surgical therapy was not effective.[17]
In China, acupuncture, as one of the oldest traditional therapies, has been used to treat various diseases including facial palsy for many years. Meanwhile, acupuncture has been recognized as one of the main therapies for complementary and alternative medicine (CAM) in the United States.[18] Acupuncture is a practical and low-cost intervention that works well for many diseases with few side effects. In recent years, there were several Cochrane systematic review for the treatment of facial paralysis in which acupuncture interventions had been reported.[19,20] These studies investigated that there was insufficient evidence to prove that acupuncture had a positive effect on the treatment of facial paralysis.
As acupuncture is receiving extensive attention, investigating its efficacy and potential modifiers are necessary to better understand and apply this traditional Chinese medical treatment. Nowadays, more and more doctors in Asia choose to use acupuncture to treat facial paralysis. However, the effects of acupuncture and drugs on the treatment of facial paralysis are still controversial. Therefore, we conducted a systematic Review and meta-analysis of randomized controlled trials (RCTs) to investigate whether Bell's palsy patients would benefit from acupuncture treatment comparing with drug therapy.
2. Materials and methods
2.1. Search strategy
This meta-analysis was performed in adherence to PRISMA statement.[21] A comprehensive literature search with no language restriction was conducted using PubMed, Embase, the Cochrane Register of Controlled Trials. We did not search gray literature, such as conference abstracts and unpublished reports. During the search process, the full-texts of some articles were limited as the problem of copyright in PubMed, and Embase, the Cochrane Register of Controlled Trials. Then we tried to find these full-texts by searching them in China National Knowledge Infrastructure (CNKI), Wanfang Database and the websites of related journals by using the information of PMID, DOI and others. The searching process was independently performed by two investigators (Rongchao Zhang and Tao Wu). We searched terms related to Bell's palsy, acupuncture, and terms related to randomized controlled trials. The detailed search strategy is showed in the Appendix 1: (Search Strategy and detailed records.)
2.2. Study selection
Inclusion criteria of studies:
-
1.
study design: randomized controlled trials;
-
2.
population: patients with Bell's palsy (Facial paralysis or idiopathic facial paralysis or herpetic facial paralysis);
-
3.
intervention: the intervention was acupuncture therapy, the acupuncture therapy refers to needling or needling combined with moxibustion;
-
4.
Comparison: oral medication or topical injection without other therapy.
Exclusion criteria of studies:
-
1.
not RCTs;
-
2.
trials testing other forms of acupuncture, such as laser acupuncture or electric acupuncture;
-
3.
studies of comparison of 2 different forms of acupuncture methods;
-
4.
the intervention group of studies combined more than 2 therapies, such as acupuncture plus medication.
2.3. Data extraction and outcome measures
The data extraction process was applied blindly. Two investigators (Rongchao Zhang and Tao Wu) independently extracted the following information from each study: first author, publication year, country, ethnicity, mean age, number of cases and controls, treatment methods for each group. The primary outcome was cure rate, and the secondary outcome was total effective rate. The efficacy criteria for facial paralysis treatment were determined with reference to the House-Brackmann judging and grading system of facial nerve function.[22] There are 4 levels of the efficacy: cured, markedly effective, effective, and ineffective. The percentage of cured was called cure rate, and the percentage of markedly effective or effective were called total effective rate.
2.4. Assessment of bias risks and methodological quality of included studies
The following aspects of included studies were assessed by 2 authors (Rongchao Zhang and Tao Wu), respectively: random sequence generation; allocation concealment; blinding of participants and personnel; blinding of outcome assessment; incomplete outcome data; selective reporting; other bias. A grade of ‘high’, ‘low’, or ‘unclear’ was given for each item. The risk of bias was assessed using the modified tool for “risk of bias” from the Cochrane Handbook for Systematic Reviews of Interventions.[23] Any disagreement was resolved by discussion with a third investigator (Ruihui Wang).
2.5. Statistical analysis
Relative risks (RR) with 95% confidence intervals (CI) were evaluated for outcomes. We firstly used the fixed model to pool the effect sizes of the primary and secondary outcomes, and the results showed that the homogeneity among the pooled studies was poor (the I2 statistic = 67%, Cochrane Q test P = .0008 and the I2 statistic = 90%, Cochrane Q test P < .00001, respectively). Then the random effect model was used to pool RRs. Publication bias was assessed using funnel plots and we did not analyze Egger test or Begg test, since there are only 11 included studies. Heterogeneity across studies was assessed using the Q statistic and I2 statistic. We defined that the statistical heterogeneity was set at the I2 statistic >50% and/or Cochrane Q test P < .10. It was performed by excluding any single study to test the robustness of the pooled results. Subgroup analyses were performed by intervention methods (acupuncture vs acupuncture combine with moxibustion), different methods of medicine (western medicine vs Chinese and western medicine), published year (before 2005 vs after 2005), sample sizes (≥90 vs < 90). P value < .05 were considered statistically significant. The sensitivity analysis was analyzed using Stata 14.0 (Stata Corporation, College Station, TX), and the rest of available data were analyzed using RevMan 5.3 (The Nordic Cochrane Centre, Copenhagen, Denmark)
2.6. Ethics statement
This study is a systematic review and meta-analysis, which was a secondary data processing of previously published studies. All contents were not related to human and animal experiments, so no ethical approval was required.
3. Results
3.1. Study selection and characteristics
Detailed steps of the literature search and study selection are summarized in Fig. 1. We identified 323 relative articles: 68 articles in PubMed, 53 articles in Embase, and 202 articles in cochrane database. Of the 323 inferences, 178 repeated studies were excluded by reading titles and abstracts. Finally, only the full texts of 46 articles were obtained for further review. Then 20 articles were excluded: 13 were not RCTs, 4 meta-analyses and 3 reviews. Among the left 26 articles, 15 studies with mixed interventions did not meet our inclusion criteria and were excluded: in 3 articles,[24–26] the control group combined with non-drug therapy; in 6 articles, non-acupuncture therapy was used in the observation group; in 2 studies,[27,28] the intervention of the observation group was acupuncture plus electroacupuncture; 1 study,[29] used light irradiation therapy device; 2 studies[29,30] used cupping therapy; and the acupuncture group of 1 study[31] used drug therapy. Four studies[32–35] compared the effectiveness of different types of acupuncture therapy. The efficacy evaluation of 1 article[36] is not clear, and 1 article.[37] was repeated with the previous study. Therefore, of the 46 full-text publications obtained, only 11 RCTs[38–48] met our inclusion criteria.
Figure 1.

Flowchart of study search.
Characteristics of the 11 included RCTs were shown in Table 1. All the included studies were based on patients with newly developed facial paralysis, excluding patients with intractable paralysis. The newly developed facial paralysis was defined as the time during which facial paralysis occurs within one month. The observation time points of each study were between 1 to 1.5 months, and the cure rate and total effective rate of the experimental group and the control group were evaluated at the same time. All the included studies were performed in China and published from 1996 to 2015. Nine studies were written in Chinese and 2 in English.[40–45] A total of 1258 participants were enrolled in this meta-analysis with sample sizes ranging from 28 to 284. The patients were randomly assigned to intervention group (acupuncture group) or control group (drug group), with their age ranging from 8 to 78 years old. In the intervention group, acupuncture treatment only included manual acupuncture or manual acupuncture combined with moxibustion, while the control group only included drugs (oral or injection). In the intervention group, 3[40,41,47] of the 11 articles used acupuncture combined with moxibustion, and the rest 8 studies used traditional acupuncture. All the included RCTs used drug therapy as control. Only 1 RCT referred to adverse effects and/or complications during acupuncture therapy.[40] The rest of studies did not report the side effects and/or complications of patients.
Table 1.
Characteristics of 11 eligible RCTs.

3.2. Methodologies bias of selected studies
Details of the quality of included studies were shown in Fig. 2.
Figure 2.
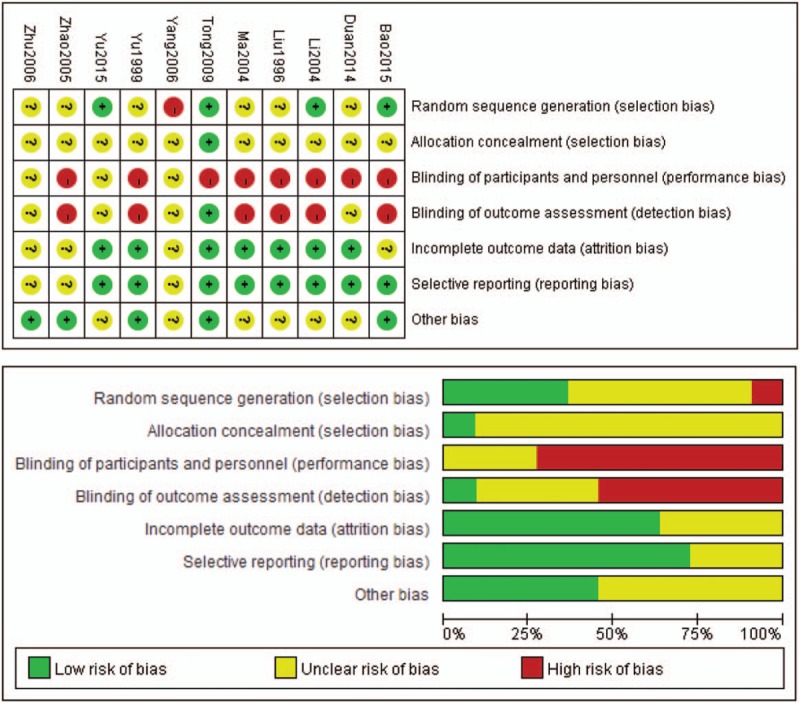
Risk of bias summary: review authors’ judgments about each risk of bias item for each included study.
Randomization was performed in all studies, but only 4 studies reported the details of random sequence generation.[40,45,47,48] Only 1 study[45] reported the information of allocation concealment, and none of the other studies mentioned it. Some included studies were assessed as having high risks cause because they did not describe the blinding process. One study reported that the outcome assessment was blinded.[45] Incomplete outcome data were reported in 7 trails, and 8 trails conducted selective reporting with a low risk of bias. Five trials reported other kinds of bias.[39,42,43,45,48] In general, the overall risk of bias in included studies is pretty high.
3.3. Primary and secondary outcomes
All the selected 11 studies were used to calculate the pooled estimate for assessing the cure rate and total effective rate.
In summary, 379 individuals were cured in the acupuncture group (n = 646) and 199 individuals were cured in the drug group (n = 612). The total cure rates for the acupuncture and drug groups were 59.7% and 32.5%, respectively. Acupuncture treatment was associated with an increased cure rate (RR = 1.77, 95% CI: 1.41–2.21, Fig. 3), with significant heterogeneity in the pooled results (I2 = 67%, P = .0008).
Figure 3.

Meta-analysis on acupuncture for cured rate on Bell's palsy.
There were 626 individuals in the acupuncture group were evaluated as effective in treatment among 646 patients and 508 individuals in the control group were evaluated as effective among 612 patients. The total effective rates in the acupuncture and drug groups were 96.9% and 83.0%, respectively. Acupuncture therapy was associated with an increased total effective rate (RR = 1.18, 95% CI: 1.07–1.31, Fig. 4), with significant heterogeneity in the pooled results (I2 = 90%, P < .00001).
Figure 4.
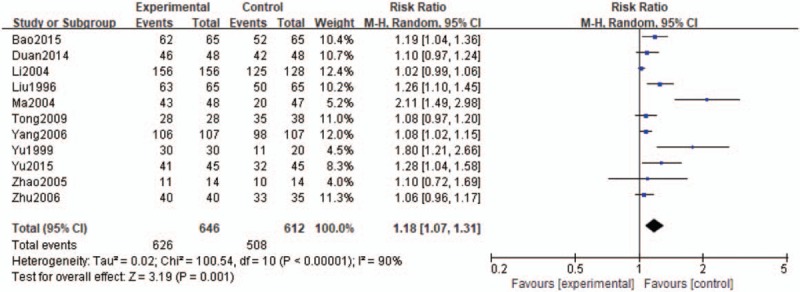
Meta-analysis on acupuncture for total effective rate of Bell's palsy.
3.4. Publication bias, subgroup analyses and sensitivity analysis
We conducted funnel plots for the primary and secondary outcomes to assess the potential publication bias of the included studies. In regards to the cure rate, we initially found that funnel plot yielded no extreme publication bias (Fig. 5). And for the outcome of total effective rate, there was also no obvious publication bias can be observed based on the funnel plot (Fig. 6).
Figure 5.

The funnel plot of the cure rate.
Figure 6.
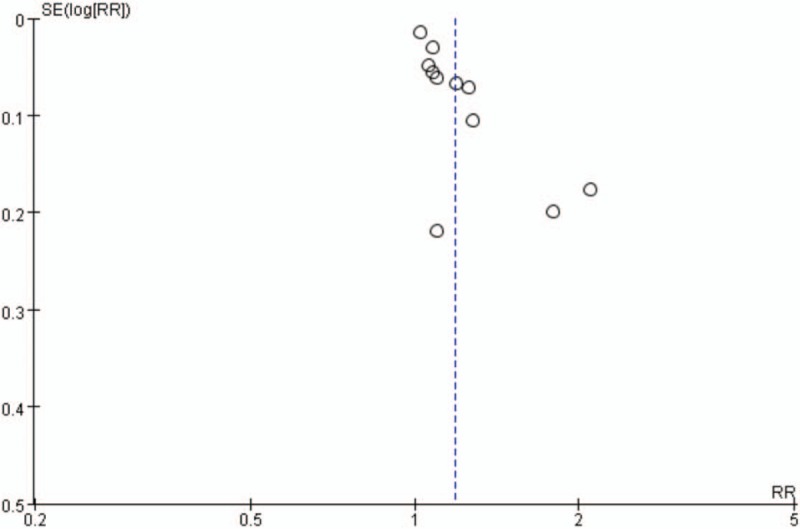
The funnel plot of the total effective rate.
Subgroup analyses based on intervention methods, different methods of medicine, published year and sample sizes showed similar results across all the analyses (Table 2 and Appendix 2)
Table 2.
Subgroup analysis.

Sensitivity analysis was conducted to evaluate the stability of the results. In sensitivity analysis, excluding any single study at each turn did not lead to a remarkable change in the overall RR and 95% CI of cured rate and total effective rate, indicating that the pooled results were stable. (Figs. 7 and 8)
Figure 7.

Sensitivity analysis on acupuncture for cured rate of Bell's palsy.
Figure 8.

Sensitivity analysis on acupuncture for total effective rate of Bell's palsy.
4. Discussion
In this systematic review and meta-analysis, 323 RCTs were found by searching PubMed, Embase and Cochrane Central Register of Controlled, and finally 11 RCTs were included with 1258 patients. The observation group used traditional Chinese acupuncture therapy (acupuncture or acupuncture plus moxibustion), and the control group used drug therapy (oral or injection). Through this study, more evidence can be provided to explore whether acupuncture is beneficial to Bell's palsy and whether it is more effective than drug therapy. The interventions included in the previous studies were complicated, such as acupuncture combined with drug therapy as an intervention group and drug therapy alone as a control group. The studies included in this meta-analysis was acupuncture as an intervention group, and drug treatment as a control group, which is a more direct and accurate comparison of the effects of acupuncture treatment and drug treatment for Bell's facial paralysis.
The results showed that patients in the acupuncture group may associated with increased cure rates and total effective rate (RR = 1.77, 95% CI: 1.41–2.21; RR = 1.18, 95% CI: 1.07–1.31) compared with the drug group. All the RCTs included in this meta-analysis indicate that acupuncture was an effectively treatment for Bell's facial paralysis (peripheral facial paralysis). Bell's palsy is a self-limiting disease, and some patients can recover spontaneously without treatment. Therefore, researches related to the treatment of Bell's palsy may be uncommon. As one of the most classic therapy of traditional Chinese medicine, acupuncture is pretty popular in Asian countries such as China and South Korea, but not common in Europe and the America.
Significant heterogeneity was observed in studies comparing acupuncture and drug efficacy. Experimental design, methodological deficiencies and operator skill differences may be the main causes of heterogeneity. Meanwhile, the various sample size between studies is also a source of heterogeneity. There are some methodological flaws in the included studies. First, in the part of allocation concealment, some studies have not been concealed or not described. Second, some studies did not perform the blinding of participants and personnel, which may cause performance bias. Analysis of the risk of bias indicated that the high-risk bias of the included studies was mainly due to the fact that the study process was not blinded or unreported, and assessment of the results were not blinded or unreported. In further studies, the conditions of the experimental group and the control group should be strictly controlled, and blind grouping and treatment should be strictly applied. Meanwhile, future researches should expand the sample size to obtain more objective and accurate results.
There were several meta-analyses about the acupuncture treatment for patients with Bell's palsy. Zhou et al[49] searched for relevant literature before 2009 and included 6 RCTs, including 537 Bell's palsy participants. However, due to the poor quality of the included studies, reliable conclusions cannot be drawn about the efficacy of traditional acupuncture and other treatments. Kim et al[50] searched for relevant literature before June 2010. A total of 8 RCTs were included in their study. The Cochrane bias risk tool was used to assess the quality of these trials. Due to the low quality of the trials, no definitive conclusions were reached. Li et al[51] searched for literature before 2015 and included 14 RCTs, including 1541 Bell palsy patients. Since the data included in the study were incomplete, no complication rate was assessed. They investigated that acupuncture seems to be an effective treatment for Bell's palsy, but due to the poor quality and great heterogeneity of the included studies, there is insufficient evidence to support the efficacy and safety of acupuncture. Zhang et al[52] searched for literature before July 2016 and included 20 RCTs, including 2508 Bell palsy patients. Their results show that due to limited methodological quality and potential biases of studies, it was not possible to conclude that acupuncture was effective against facial paralysis.
Although acupuncture therapy shows benefits, the efficacy may be influenced by factors such as patient's compliance and doctor's experience. Because the use of acupuncture is a complex technical process, differences in the depth and strength of the needles penetrated by different operators may also affect the effectiveness of acupuncture treatment, which increases the difficulty of assessing the consistency of each trial. However, acupuncture therapists can achieve constant standards through regular training and practice. Insufficient information about the side effects or complications of acupuncture treatment means that we cannot further evaluate other meaningful clinical indicators. Therefore, we need more high-quality and large sample randomized controlled studies to explore the effects and side effects of acupuncture treatment.
This study has several limitations. First, the sample size of included studies were small, which may lead to limited generalizability. Second, the experimental design of several studies was not good enough, such as randomization, allocation concealment, and blinding were not performed strictly. Third, information of the side effects and complications of acupuncture were not presented in the trails. This means that there was not enough evidence to prove the safety of acupuncture treatment, so potential risks need to be considered when giving treatment advice.
5. Conclusion
Despite the poor quality of the included studies, our meta-analysis further confirmed the results of previous researches. Despite the high risk of bias and heterogeneity, acupuncture seems to be superior to drug therapy in the treatment of Bell's palsy including cure rate and total effective rate, which may be an effective method of treating Bell's palsy. When treating patients with facial paralysis, Acupuncture can be seen as one of the effective and operational treatment options. However, due to the existence of methodological flaws and potential bias risk in the included studies, more high-quality and large-sample RCTs are needed. Therefore, please carefully refer to the research conclusions of this meta-analysis.
Author contributions
Conceived and designed the experiments: Rongchao Zhang, Ruihui Wang.
Performed the experiments: Rongchao Zhang, Tao Wu, Dong Wang
Analyzed the data: Rongchao Zhang, Tao Wu, Dong Wang
Contributed reagents/materials/analysis tools: Rongchao Zhang, Ruihui Wang.
Wrote the paper: Rongchao Zhang.
Revised the manuscript: Rongchao Zhang, Ruihui Wang.
Data curation: Rongchao Zhang, Tao Wu.
Formal analysis: Rongchao Zhang, Tao Wu.
Funding acquisition: Tao Wu.
Investigation: Rongchao Zhang, Tao Wu.
Methodology: Rongchao Zhang, Ruihui Wang.
Project administration: Rongchao Zhang, Tao Wu.
Resources: Ruihui Wang, Qi Liu.
Software: Tao Wu, Dong Wang, Qi Liu.
Supervision: Dong Wang.
Visualization: Dong Wang.
Writing – original draft: Rongchao Zhang.
Writing – review & editing: Rongchao Zhang.
Supplementary Material
Footnotes
Abbreviations: CAM = complementary and alternative medicine, CI = confidence interval, RCTs = randomized controlled trials, RR = relative risk, US = the United States.
We are very grateful for the financial support provided by Ruihui Wang and Dong Wang. The funding came from National Natural Science Foundation of China (Project No. 81674088 and No. 81704186) and the Shaanxi Natural Science Foundation Youth Project (No. 2018JQ8070 and No. 2017JQ8020). Scientific Project of Shaanxi Provincial Department of Education (18JK0219).
The authors have no conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
References
- [1].Gilden DH. Clinical practice. Bell's Palsy. N Engl J Med 2004;351:1323–31. [DOI] [PubMed] [Google Scholar]
- [2].Peitersen E. Natural history of Bell's palsy. Acta Otolaryngol Suppl 1992;492:122–4. [DOI] [PubMed] [Google Scholar]
- [3].Peitersen E. The natural history of Bell's palsy. Am J Otol 1982;4:107–11. [PubMed] [Google Scholar]
- [4].Eviston TJ, Croxson GR, Kennedy PG, et al. Bell's palsy: aetiology, clinical features and multidisciplinary care. J Neurol Neurosurg Psychiatry 2015;86:1356–61. [DOI] [PubMed] [Google Scholar]
- [5].Shannon S, Meadow S, Horowitz SH. Clinical inquiries. Are drug therapies effective in treating Bell's palsy? J Fam Pract 2003;52:156159. [PubMed] [Google Scholar]
- [6].Hauser WA, Karnes WE, Annis J, et al. Incidence and prognosis of Bell's palsy in the population of Rochester, Minnesota. Mayo Clin Proc 1971;46:258–64. [PubMed] [Google Scholar]
- [7].Cave JA. Recent developments in Bell's palsy: Does a more recent single research paper trump a systematic review? BMJ 2004;329:1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Morris AM, Deeks SL, Hill MD, et al. Annualized incidence and spectrum of illness from an outbreak investigation of Bell's palsy. Neuroepidemiology 2002;21:255–61. [DOI] [PubMed] [Google Scholar]
- [9].Gagyor I, Madhok VB, Daly F, et al. WITHDRAWN: Antiviral treatment for Bell's palsy (idiopathic facial paralysis). Cochrane Database Syst Rev 2015;7:2015;Cd001869. [DOI] [PubMed] [Google Scholar]
- [10].Weiju H. Progress in the diagnosis and treatment of Bell's facial paralysis. Chin J Clinicians (Electronic Edition) 2009;9:1435–44. [Google Scholar]
- [11].Madhok VB, Gagyor I, Daly F, et al. Corticosteroids for Bell's palsy (idiopathic facial paralysis). Cochrane Database Syst Rev 2016;7:Cd001942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].McAllister K, Walker D, Donnan PT, et al. Surgical interventions for the early management of Bell's palsy. Cochrane Database Syst Rev 2013;10:Cd007468. [DOI] [PubMed] [Google Scholar]
- [13].Altun I, Kurutaş EB. Vitamin B complex and vitamin B12 levels after peripheral nerve injury. Neural Regen Res 2016;11:842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Theil D, Arbusow V, Derfuss T, et al. Prevalence of HSV-1 LAT in human trigeminal, geniculate, and vestibular ganglia and its implication for cranial nerve syndromes. Brain Pathol 2001;11:408–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Stjernquist-Desatnik A, Skoog E, Aurelius E. Detection of herpes simplex and varicella-zoster viruses in patients with Bell's palsy by the polymerase chain reaction technique. Ann Otol Rhinol Laryngol 2006;115:306–11. [DOI] [PubMed] [Google Scholar]
- [16].Sun DQ, Andresen NS, Gantz BJ. Surgical management of acute facial palsy. Otolaryngol Clin North Am 2018;51:1077–92. [DOI] [PubMed] [Google Scholar]
- [17].Adour KK. Decompression for Bell's palsy: why I don’t do it. Eur Arch Otorhinolaryngol 2002;259:40–7. [DOI] [PubMed] [Google Scholar]
- [18].Fan AY. Obamacare” covers fifty-four million Americans for acupuncture as Essential Healthcare Benefit. J Integr Med 2014;12:390–3. [DOI] [PubMed] [Google Scholar]
- [19].Li P, Qiu T, Qin C. Efficacy of acupuncture for Bell's Palsy: a systematic review and meta-analysis of randomized controlled trials. PLoS One 2015;10:e0121880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Chen N, Zhou M, He L, et al. Acupuncture for Bell's palsy. Cochrane Database Syst Rev 2010;8:2010;Cd002914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Knobloch K, Yoon U, Vogt PM. Preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement and publication bias. J Craniomaxillofac Surg 2011;39:91–2. [DOI] [PubMed] [Google Scholar]
- [22].Coulson SE, Croxson GR, Adams RD, et al. Reliability of the “Sydney,” “Sunnybrook,” and “House Brackmann” facial grading systems to assess voluntary movement and synkinesis after facial nerve paralysis. Otolaryngol Head Neck Surg 2005;132:543–9. [DOI] [PubMed] [Google Scholar]
- [23].Higgins JP, Altman DG, Gotzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Xu KS, Huang MW, Wang QM. Observation on therapeutic effect of aponeurotic system penetration needling on peripheral facial paralysis. Zhongguo Zhen Jiu 2006;26:169–71. [PubMed] [Google Scholar]
- [25].Qu Y. Clinical observation on acupuncture by stages combined with exercise therapy for treatment of Bell palsy at acute stage. Zhongguo Zhen Jiu 2005;25:545–7. [PubMed] [Google Scholar]
- [26].Yang JS, Li XG, Li YM. Comparative observation on clinical efficacy of acupuncture and chinese herbal medicine in treating peripheral facial paralysis. J Clin Acupunct Moxibust 2002;7–8. [Google Scholar]
- [27].Yuan B. Clinical observation on 30 cases of facial paralysis treated by Acupuncture and moxibustion. Chin Med Cosmetol 2015;No.:134–5. [Google Scholar]
- [28].Xiang QY, Fu LP. Clinical observation on the treatment of peripheral facial paralysis by balancing yin and yang acupuncture 2015;8:32–3. [Google Scholar]
- [29].Zhang XZ. The relationship between different therapies and the prognosis of acute idiopathic facial paralysis. Chin J Acupunct Moxibust 2005;5:320–1. [Google Scholar]
- [30].Wen XX, Shen CR, Yin YY. Study of electric acupuncture and cupping jar on facial paralysis. Mod J Integr TradChin West Med 2003;12:15881679. [Google Scholar]
- [31].Fan Q. Electroacupuncture plus flash tank combined with traditional Chinese medicine for the treatment of refractory facial paralysis in 15 cases. Fujian J TCM 2004;35:14–5. [Google Scholar]
- [32].Wang LZ. Clinical observation of acupuncture combined with acute idiopathic facial paralysis. J Sichuan Tradit Chin Med 2007;11:109–10. [Google Scholar]
- [33].Xing W, Liu H. Clinical observation on acupuncture treatment of persistent facial paralysis. Tradit Chin Med 1997;17:18–20. [PubMed] [Google Scholar]
- [34].Zhen Z, Ruan YD, Ning XJ, et al. Clinical Observations on the Treatment of Peripheral Facial Paralysis with Acupuncture Plus Needle Knife (in Chinese). Shanghai J Acupunct Moxibust 2004;23:21–2. [Google Scholar]
- [35].Zhou GL, Jin JZ, Xin TX, et al. Clinical observation of 30 cases of neuritis Integrative face quadruple therapy. Guangming J Chin Med [Guang Ming Zhong Yi] 2015;30:1496–7. [Google Scholar]
- [36].Xuan LH, Wang LL. The study of facial nerve neuritis and facial muscle function recovery by acupuncture at Shen Dao. Chin Med Sci Technol 2007;1:6–7. [Google Scholar]
- [37].Liang F, Li Y, Yu S, et al. A multicentral randomized control study on clinical acupuncture treatment of Bell's palsy. J Tradit Chin Med 2006;26:3–7. [PubMed] [Google Scholar]
- [38].Liu M. Observation of the efficacy of shallow-multi needle and drug therapy for facial paralysis of 130 cases. Clin Acupunct Moxibust (Chinese) 1996;56. [Google Scholar]
- [39].Yu Y. Analysis of acupuncture for peripheral facial palsy. Shanghai J Acupunct Moxibust 1999;26. [Google Scholar]
- [40].Li Y, Liang FR, Yu SG, et al. Efficacy of acupuncture and moxibustion in treating Bell's palsy: a multicenter randomized controlled trial in China. Chin Med J 2004;117:1502–6. [PubMed] [Google Scholar]
- [41].Ma Z. Clinical observations on acupuncture and noxibustion treatment of HIV positive peripheral facial paralysis. Shanghai J Acupunct Moxibust 2004;18:19–20. [Google Scholar]
- [42].Zhao Y, He L, Zhang QH. Effectiveness of three different treatments for peripheral facial paralysis. Chin J Clin Rehab 2005;32:41–3. [Google Scholar]
- [43].Zhu LJ. Observations on the efficacy of combined acupuncture and medication for treating the acute stage of peripheral facial paralysis. Shanghai Acupunct Moxibust (Chinese) 2006;25:17. [Google Scholar]
- [44].Yang CD, BJ, Song ZZ, JC Observations on the efficacy of combined acupuncture and medication for treating in 320 cases of facial paralysis. Sci Tech Info Gansu (Chinese) 2006;35:240. [Google Scholar]
- [45].Tong FM, Chow SK, Chan PYB, et al. A prospective randomised controlled study on efficacies of acupuncture and steroid in treatment of idiopathic peripheral facial paralysis. Acupunct Med 2009;27:169–73. [DOI] [PubMed] [Google Scholar]
- [46].Duan DC. Therapeutic effect of acupuncture on peripheral facial paralysis. Chin J Clinical Rational Drug Use 2014;8:138–9. [Google Scholar]
- [47].Yu LR. Acupuncture treatment of peripheral facial paralysis and its safety study. Linchuangyushijian 2015;13:50–1. [Google Scholar]
- [48].Bao JY. Clinical analysis of acupuncture treatment of 65 patients with facial paralysis. Int Med Health Newslett 2015;6:840–2. [Google Scholar]
- [49].Zhou M, He L, Zhou D, et al. Acupuncture for Bell's palsy. J Altern Complement Med 2009;15:759–64. [DOI] [PubMed] [Google Scholar]
- [50].Kim JI, Lee MS, Choi TY, et al. Acupuncture for Bell's palsy: a systematic review and meta-analysis. Chin J Integr Med 2012;18:48–55. [DOI] [PubMed] [Google Scholar]
- [51].Li P, Qiu T, Qin C. Efficacy of acupuncture for Bell's palsy: a systematic review and meta-analysis of randomized controlled trials. PloS One 2015;10:e0121880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Zhang XW, Wang FM, Yu SS, et al. The effect of acupuncture on Bell's palsy: an overall and cumulative meta-analysis of randomized controlled trials[J]. Int J Clin Exp Med 2018;11:3309–10. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


