Abstract
Introduction:
Pulmonary sarcomatoid carcinomas (PSCs) are rare tumors within the sarcomatoid carcinoma group. Giant cell carcinoma of the lung (GCCL) is a rare type of PSCs that consists entirely of highly pleomorphic tumor giant cells; the prognosis is poor.
Patient concerns:
A patient presented with a single cyst and was diagnosed with GCCL. The patient was a 59-year-old male who was admitted to the hospital with a cough. A chest computerized tomography (CT) scan showed a single, thin-walled cyst containing air in the left upper lobe of the lung. Bronchoscopy revealed chronic bronchitis. The initial diagnosis was pulmonary infection and the patient was treated with antibiotics. The cyst wall increased in thickness, and the cyst eventually formed a cavity.
Diagnosis:
Surgery was performed, and a diagnosis of GCCL was established. The stage was pT1bN1M0 (equal to stage IIB).
Interventions:
The patient underwent video-assisted thoracoscopic surgery and 4 cycles of adjuvant chemotherapy consisting of cisplatin and docetaxel. After 9 months, the patient occurred mediastinal lymph node metastasis, and received radiotherapy (60Gy/30F).
Outcomes:
His prognosis was good without progression (complete response) based on serial CT scans over 9 months of follow-up evaluations, then the patient occurred mediastinal lymph node metastasis. The patient lived during 30 months of follow-up, after which he was lost to follow-up.
Conclusion:
A solitary pulmonary parenchymal cystic lesion usually suggests an infectious disease or congenital abnormality; however, a cystic lesion is occasionally encountered in GCCL.
Keywords: giant cell carcinoma of the lung, imaging, isolated cyst, pulmonary sarcomatoid carcinoma
1. Introduction
Pulmonary sarcomatoid carcinomas (PSCs) are rare tumors within the sarcomatoid carcinoma group. PSCs, containing sarcomatous and/or sarcomatoid elements, are a heterogeneous group of non-small cell lung carcinomas based on their phenotypic characteristics and poor prognosis, and account for 0.5% to 0.52% of non-small cell lung cancers (NSCLCs).[1,2] Giant cell carcinoma of the lung (GCCL) is a rare PSCs subtype that consists entirely of highly pleomorphic tumor giant cells. The prognosis of GCCLs is poor.[3–5] GCCLs represent 0.11% of all NSCLCs.[5]
GCCLs predominantly affect males and smokers.[5] Patients with GCCLs have no specific signs or symptoms; the common complications of GCCLs include a cough, hemoptysis, chest pain, weight loss, dyspnea, and general malaise.[6,7] GCCLs can occur in any lobe of the lung, but are commonly found in the upper (52.7%) and lower lobes (21.7%).[5] The 5-year overall survival (OS) for patients with GCCLs is significantly less than that for patients with non-GCCL NSCLCs, probably because GCCL patients present with multiple adverse features, including a higher grade, larger tumor size, more advanced stage, and a tendency toward metastasis.[1,2,5]
Herein, we report a male patient with a single cyst containing air in the left upper lobe of the lung that developed into a cavity over a short time and was ultimately diagnosed as a GCCL. The development of the cyst into a cavity over a short time led us to investigate the mechanism underlying the development of GCCLs and may help us to understand the role of epithelial–mesenchymal transition (EMT) in GCCLs.
2. Case report
A 59-year-old male complained of a cough and scant bloody mucous sputum for 2 weeks. A chest computerized tomography (CT) scan showed a solitary, thin-walled cyst containing air in the left upper lobe of the lung (Fig. 1A). The patient did not have a history of a chronic cough, fever, chest pain, or shortness of breath. He was previously employed as a laborer in a burglar-proof-door factory. He had a history of smoking (40 pack-years). A chest CT scan at a local hospital in January 2014 revealed a small fibrotic lesion in the right upper lobe of the lung (Fig. 1B). The chest examination was significant for crackles in the left upper lung. The remainder of the physical examination was unremarkable. The markers of infection, including the erythrocyte sedimentation rate, C-reaction protein, and procalcitonin, were normal. The (1–3)-β-D-glucan and galactomannan tests were negative. Further examination by electronic bronchoscopy showed changes consistent with chronic bronchial inflammation. No tuberculosis bacilli or fungus were noted in the bronchial alveolar lavage fluid. We initially diagnosed the patient with a pulmonary cyst and bacterial infection, for which he was prescribed antibiotics and symptomatic treatment for 13 days, but there was no clinical improvement.
Figure 1.
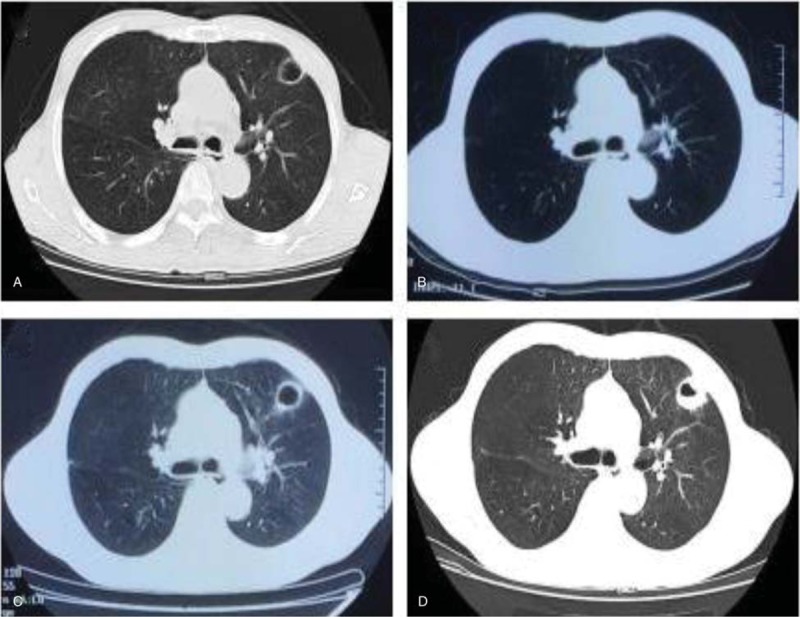
The chest CT scan of the patient upon admission (A), 6 months ago (B), 2 weeks later (C), and 23 days later (D). (A) A single thin-walled cyst containing air in the left upper lobe; (B) normal image presentation in the left upper lobe; (C) thicker wall of the cyst in the left upper lobe than before; (D) a cavity containing air in the same location.
Two weeks later, a repeat chest CT scan showed that the wall of the cyst contained air in the left upper lobe and had become thicker (Fig. 1C). The borders of the lesion were clear. Because of the rapid progression of the lesion and the variation, we considered a diagnosis of lung mycosis and adjusted the antibiotic regimen and continued symptomatic treatment for 9 days. Another chest CT scan was obtained that showed a cavity containing air in the same location, which was not conducive to a percutaneous lung biopsy (Fig. 1D). Because it was difficult to establish a diagnosis, the patient underwent video-assisted thoracoscopic surgery. Hematoxylin–eosin-staining was performed, and the examination showed anaplastic, giant tumor cells. The tumor cells were uni or multinucleated, discohesive, with leukocyte emperipolesis, bizarre and hyperchromatic nuclei, and prominent nucleoli (Fig. 2 A). The immunohistochemical results showed CK(P) (Focal+) (Fig. 2B), vimentin (Fig. 2C), CK7 (Focal+) (Fig. 2D), Ki67 (20–30%+), epithelial membrane antigen (Focal+), P63 (Focal+), lymphocytotoxic antibody (−), CK5/6 (−), and thyroid transcription factor-1 (−). The histopathologic and immunohistochemical results revealed a diagnosis of giant cell carcinoma (a PSC subtype) and the stage was pT1bN1M0 (equal to stage IIB). The patient then underwent 4 cycles of adjuvant chemotherapy consisting cisplatin (DDP [30 mg/m2/day]) on days 1 to 3 and docetaxel (DDP [75 mg/m2/day]) on day 1. The only adverse effect was grade 3 hypoleukemia (Common Terminology Criteria for Adverse Events v5.0). His prognosis was good and there was no progression (complete response) based on serial CT scans over 9 months of follow-up evaluations, then the patient occurred mediastinal lymph node metastasis, and received radiotherapy (60Gy/30F). The patient lived during 30 months of follow-up, after which he was lost to follow-up.
Figure 2.
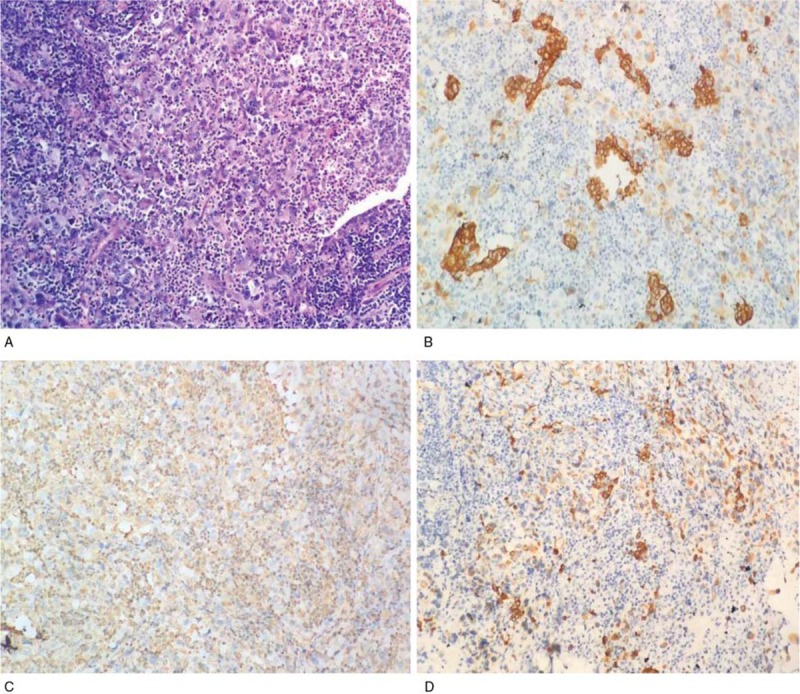
Histopathological and immunohistochemical specimens from the patient. (A) Hematoxylin and eosin (H&E) [original magnification, 400×] staining of the specimens demonstrated anaplastic, giant tumor cells which were uni or multinucleated, discohesive, showing leukocyte emperipolesis, bizarre and hyperchromatic nuclei, and prominent nucleoli; (B) immunohistochemical staining for CKP; (C) immunohistochemical staining for vimentin; (D) immunohistochemical staining for CK7 (B–D original magnification, 200×[all images from the same tissue core]).
3. Discussion
PSCs are a group of 5 rare subtypes of poorly differentiated NSCLCs that contain sarcoma-like elements histologically, including pleomorphic carcinomas, spindle cell carcinomas, giant cell carcinomas, carcinosarcomas, and pulmonary blastomas.[1,2] As a common subtype of PSCs, GCCLs account for 0.11% of all NSCLCs.[5] GCCLs are more prevalent in males (63%) and smokers.[5] Patients with GCCLs present with non-specific symptomatology, including a cough, hemoptysis, chest pain, weight loss, dyspnea, general malaise, or may be asymptomatic as in other NSCLC patients.[6–8]
GCCLs can occur in any lobe of the lung. GCCLs are frequently located in the upper lobes (52.7%), lower lobes (21.7%), middle lobe (4.9%), main bronchus (4.3%), and as an overlapping lesion (1.1%).[5] In our case, the lesion was located in the left upper lobe.
GCCLs do not have specific radiologic characteristics. The hallmark of GCCL imaging often shows intrapulmonary masses with predominant involvement of the upper lobes of the lungs.[5,7–10] In this case, the patient presented with newborn parenchymal focal cyst in the left upper lobe. Cysts are described as thin-walled (<4 mm) air-containing spaces, while cavities are air-containing lesions with thick walls (≥5 mm).[11] Cystic lung lesions can present with a large variety of different pathologic forms. Initially, we diagnosed the patient with lung infection. Indeed, misdiagnosis of PSCs in patients presenting with a cavity or pneumothorax have been reported before surgery.[12–14] We report, for the first time, a case of primary giant cell carcinoma presenting as a single cyst containing air on CT scan and a cavity during stage progression. A cyst is a circumscribed space surrounded by epithelial cells or a fibrous wall[11]; the evolving process may support epithelial-to-mesenchymal conversion based on radiological evaluation. Considering EMT plays a crucial role in PSCs,[15] the complex and dynamic networks orchestrating EMT should be investigated further and targeting the EMT pathways may be a promising therapy.
The 5-year OS of patients with GCCLs is significantly less than that of patients with non-GCC NSCLCs (16% and 19%, respectively), and the median OS is 6.0 months, compared to 14.0 months.[5] For limited-stage GCCLs, in accordance with other NSCLC subtypes, surgical resection is an effective treatment and provides adequate local control[5]; however, many patients lose the chance to undergo surgery because 60.3% of patients already have metastasis at the time of diagnosis.[5] In our patient, although the size of the tumor was small, hilar and interlobar lymph node metastases had occurred. Adjuvant cisplatin-based doublet chemotherapy in patients with NSCLC is the standard of care in patients with stages IIA, IIB, and IIIA after complete tumor resection.[16] In our patient, adjuvant chemotherapy consisted of cisplatin and docetaxel. Unfortunately, previous studies had suggested that GCCL is not sensitive to chemotherapy.[17]
Epidermal growth factor receptor-tyrosine kinase inhibitors are standard first-line therapy for advanced lung adenocarcinoma patients with EGFR mutations.[18] Weng et al[5] reported that 4 out of 10 GCCL patients harbor EGFR mutations and 1 patient received and benefited from EGFR-targeted treatment, which indicated that GCCL patients with EGFR mutations may benefit from EGFR-targeted treatment. Recent studies have demonstrated that programmed death-ligand 1 (PD-L1) expression is more frequent in PSCs than in NSCLCs.[19,20] In 1 series, 75% (27/36) of PSCs were PD-L1 positive, and 16 positive patients gave ≥50% PD-L1 expression.[21] GCCL patients with PD-L1 expression may benefit from pembrolizumab treatment. Nakayama et al[9] reported that GCCL patients who received pembrolizumab treatment had rapid regression of primary lung nodules, with the progression-free period maintained for at least 4 treatment cycles.[9] Based on those findings, immunotherapy targeting PD-1/PD-L1 may be an option for GCCL patients with PD-L1-positive expression.
In conclusion, the current case of GCCL presented with an isolated cyst that evolved to a cavity on CT scan follow-up. The current case highlights that we should pay attention to newborn single lung cysts and carry out a pathologic biopsy to ensure the diagnosis.
Author contributions
Conceptualization: Hui You.
Formal analysis: Yuquan Liu, Dan Li.
Funding acquisition: Yijun Tang.
Investigation: Meifang Wang, Xin Qian.
Methodology: Yijun Tang.
Project administration: Meifang Wang.
Resources: Yijun Tang.
Supervision: Yuquan Liu.
Validation: Na Wei, Yijun Tang.
Footnotes
Abbreviations: CRP = C-reaction protein, CT = computerized tomography, EMT = epithelial–mesenchymal transition, ESR = erythrocyte sedimentation rate, GCCL = giant cell carcinoma of the lung, NSCLC = non-small cell lung cancer, PSC = pulmonary sarcomatoid carcinomas.
M.W. wrote the manuscript; Y.L., X.Q., D.L., H.Y., N.W., and Y.T. were involved in the work.
The Ethics Committee of Shiyan Taihe Hospital approved the study (ethical number: 2019KS006). Informed written consent was obtained from the patient for publication of this case report and accompanying images.
This work was supported by National Natural Science Foundation of China (project code: 81270092) and Educational Commission of Hubei Province of China (project code: D20152104).
The authors have no conflicts of interest to disclose.
References
- [1].Steuer CE, Behera M, Liu Y, et al. Pulmonary sarcomatoid carcinoma: an analysis of the National Cancer Data Base. Clin Lung Cancer 2017;18:286–92. [DOI] [PubMed] [Google Scholar]
- [2].Rahouma M, Kamel M, Narula N, et al. Pulmonary sarcomatoid carcinoma: an analysis of a rare cancer from the surveillance, epidemiology, and end results database. Eur J Cardiothorac Surg 2018;53:828–34. [DOI] [PubMed] [Google Scholar]
- [3].Attanoos RL, Papagiannis A, Suttinont P, et al. Pulmonary giant cell carcinoma: pathological entity or morphological phenotype? Histopathology 1998;32:225–31. [DOI] [PubMed] [Google Scholar]
- [4].Laforga JB. Giant cell carcinoma of the lung. Report of a case with cytohistologic and clinical correlation. Acta Cytol 1999;43:263–7. [DOI] [PubMed] [Google Scholar]
- [5].Weng SS, Cao Y, Tang XJ, et al. Epidemiological features of lung giant cell carcinoma and therapy for patients with EGFR mutations based on case reports and the surveillance, epidemiology, and end results (SEER) database. Oncotarget 2017;8:25323–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Herman DL, Bullock WK, Waken JK. Giant cell adenocarcinoma of the lung. Cancer 1966;19:1337–46. [DOI] [PubMed] [Google Scholar]
- [7].Weissferdt A, Moran CA. Primary giant cell carcinomas of the lung: a clinicopathological and immunohistochemical analysis of seven cases. Histopathology 2016;68:680–5. [DOI] [PubMed] [Google Scholar]
- [8].Li X, Zhang Z, Liu J, et al. Molecular features of giant-cell carcinoma of the lung: a case report and literature review. Onco Targets Ther 2018;11:751–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Nakayama S, Sasaki M, Morinaga S, et al. Nonsmall cell lung carcinoma with giant cell features expressing programmed death-ligand 1: a report of a patient successfully treated with pembrolizumab. Case Rep Oncol Med 2018;2018:5863015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Habib S, Leifer LE, Azam M, et al. Giant cell carcinoma of the lung successfully treated with surgical resection and adjuvant vinorelbine and cisplatin. Respir Med Case Rep 2018;25:300–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Ryu JH, Swensen SJ. Cystic and cavitary lung diseases: focal and diffuse. Mayo Clin Proc 2003;78:744–52. [DOI] [PubMed] [Google Scholar]
- [12].Ciarallo A, Makis W, Novales-Diaz JA, et al. Sarcomatoid carcinoma (carcinosarcoma) of the lung mimics malignant pleural mesothelioma on 18F-FDG PET/CT: a report of 2 cases. Clin Nucl Med 2012;37:416–9. [DOI] [PubMed] [Google Scholar]
- [13].Zhang Y, Li B, Shi H, et al. Sarcomatoid carcinoma of the lung mimics aspergilloma on (1)(8)F-FDG PET/CT. Hell J Nucl Med 2015;18:268–70. [DOI] [PubMed] [Google Scholar]
- [14].Zhou XM, Li P, Zhao L, et al. Lung carcinosarcoma masked by tracheobronchial aspergillosis. Intern Med 2015;54:1905–7. [DOI] [PubMed] [Google Scholar]
- [15].Thomas VT, Hinson S, Konduri K. Epithelial-mesenchymal transition in pulmonary carcinosarcoma: case report and literature review. Ther Adv Med Oncol 2012;4:31–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Kolek V, Losse S, Kultan J, et al. Real life adjuvant chemotherapy uptake and survival in patients with non-small cell lung cancer after complete resection. Curr Med Res Opin 2018;34:1687–94. [DOI] [PubMed] [Google Scholar]
- [17].Giroux Leprieur E, Antoine M, Vieira T, et al. Clinical and molecular features in patients with advanced non-small-cell lung carcinoma refractory to first-line platinum-based chemotherapy. Lung Cancer 2013;79:167–72. [DOI] [PubMed] [Google Scholar]
- [18].Travis WD, Brambilla E, Noguchi M, et al. International association for the study of lung cancer/American Thoracic Society/European Respiratory Society international multidisciplinary classification of lung adenocarcinoma. J Thorac Oncol 2011;6:244–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Velcheti V, Rimm DL, Schalper KA. Sarcomatoid lung carcinomas show high levels of programmed death ligand-1 (PD-L1). J Thorac Oncol 2013;8:803–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Vieira T, Antoine M, Hamard C, et al. Sarcomatoid lung carcinomas show high levels of programmed death ligand-1 (PD-L1) and strong immune-cell infiltration by TCD3 cells and macrophages. Lung Cancer 2016;98:51–8. [DOI] [PubMed] [Google Scholar]
- [21].Yvorel V, Patoir A, Casteillo F, et al. PD-L1 expression in pleomorphic, spindle cell and giant cell carcinoma of the lung is related to TTF-1, p40 expression and might indicate a worse prognosis. PLoS One 2017;12:e0180346. [DOI] [PMC free article] [PubMed] [Google Scholar]


