Abstract
Introduction:
An isolated injury to the tibial division is rare among compressive sciatic neuropathy. To date, isolated injury to the tibial division of the sciatic nerve after self-massage of the gluteal muscle has not been reported. Here, we report a case of compressive sciatic neuropathy diagnosed after self-massage of the gluteal muscle using magnetic resonance image (MRI) and ultrasound images and its associated therapeutic process.
Patient concerns:
A 50-year-old woman presented right lower extremity pain for the past 7 days.
Diagnosis:
Electrophysiological findings were consistent with right tibial neuropathy proximal to the branch to hamstring muscles. However, T2-weighted MRI showed high signal intensity and swelling in the right sciatic nerves from the superior gemellus level to the quadratus femoris level. After considering both radiologic and electrophysiological findings, the patient was diagnosed with an isolated injury to the tibial division of the right sciatic nerve.
Interventions:
The patient agreed to an ultrasound-guided perineural steroid injection upon receiving detailed explanation of the procedure.
Outcomes:
After the injection, there was significant improvement in pain.
Conclusion:
Therefore, in making a diagnosis of sciatic neuropathy, it may be important to find the lesion via MRI than relying solely on the patient's history or electrophysiologic study.
Keywords: massage, massage ball, magnetic resonance image, sciatic neuropathy, steroid, ultrasound
1. Introduction
Sciatic neuropathy is usually caused by an external compression of the nerve, or by stretching around the hip during surgical procedure.[1] Less common causes include vasculitis and injuries from injection, gunshot, or knife.[1] Compressive sciatic neuropathy can be a result of various conditions, including mass lesion, trauma, gluteal hematoma, or compartment syndrome.[2,3]
In sciatic neuropathy, clinical findings are often more consistent with injury to the peroneal division rather than to the tibial division; the latter sometimes mimic a common fibular neuropathy at the knee.[4] Because the peroneal division has fewer and larger fascicles with less supportive tissue compared with the tibial division, it is thought to be more vulnerable to compressive injury.[4] Moreover, the peroneal division is more taut, and it is secured at the sciatic notch and fibular neck, resulting in greater risk for stretch injury. However, except for focal injury, such as knife stab, or space occupying lesions, such as tumor, injury to the tibial division of the sciatic nerve is rare. To date, there has not been any report of an isolated injury to the tibial division of the sciatic nerve after self-massage of the gluteal muscle using a massage ball. Here, we report a case of compressive sciatic neuropathy diagnosed after self-massage of the gluteal muscle using magnetic resonance image (MRI) and ultrasound images and its associated therapeutic process. This case report was approved by the institutional review board of Daegu Fatima Hospital (DFE19ORIO049). Informed written consent was obtained from the patient for publication of this case report and accompanying images.
2. Case report
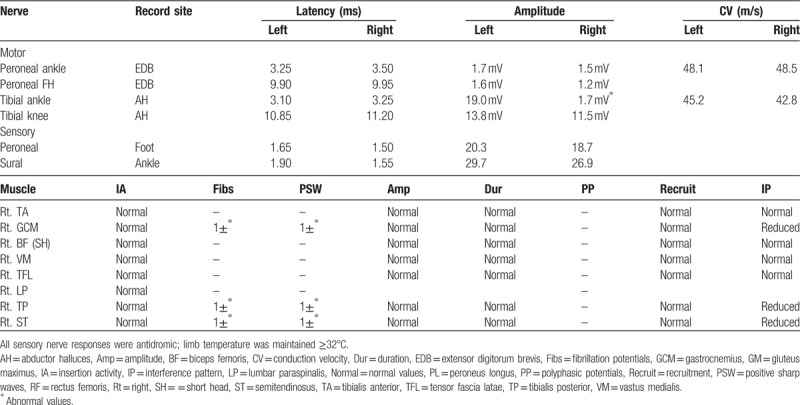
A 50-year-old woman presented right lower extremity pain for the past 7 days. The patient had repeated history of pain in the back and right gluteal area, which had improved after L5 transforaminal epidural steroid injection (TFESI) at a local medical center (LMC). Three days before admission at our institution, pain had developed again, for which she received L5 TFESI at the LMC; with no sign of improvement in pain, she was referred to our clinic for further evaluation. The patient complained of radiating pain to the right lower extremity. The physical examination at our clinic revealed focal tenderness at the right gluteal muscle, right where the sciatic nerve passes. The patient had no previous history of trauma, except self-massage of the right gluteal muscle using a massage ball (Fig. 1). There was no weakness of the right lower extremity; sensory impairment and dysesthesia were checked in the medial area of the calf muscle and the right sole area. At 8 days after pain development, we performed an electrophysiologic study. In the nerve conduction study, there was no abnormality of the motor and sensory nerves on the both lower extremities. However, needle electromyography (EMG) revealed active denervation with reduced interference pattern in the tibial-innervated muscles, not in the peroneal-innervated muscles. Moreover, no abnormalities were observed in the quadriceps, adductor longus, iliopsoas, and paraspinal muscles. The electrophysiological findings were consistent with right tibial neuropathy, proximal to the branch supplies hamstring muscles (Table 1). To rule out space-occupying lesions and to define the site of tibial nerve injury, we performed MRI of the lumbar spine and pelvis. Although there was no difference in the protruded L4/5 intervertebral disc with previous MRI, the axial T2-weighted MRI of the pelvis showed high signal intensity and swelling of the right sciatic nerves, from the superior gemellus level to the quadratus femoris level (Fig. 1). After considering both radiologic and electrophysiologic findings, we concluded that patient‘s right lower extremity pain was due to right sciatic neuropathy (mainly tibial component) at the gluteal area.
Figure 1.
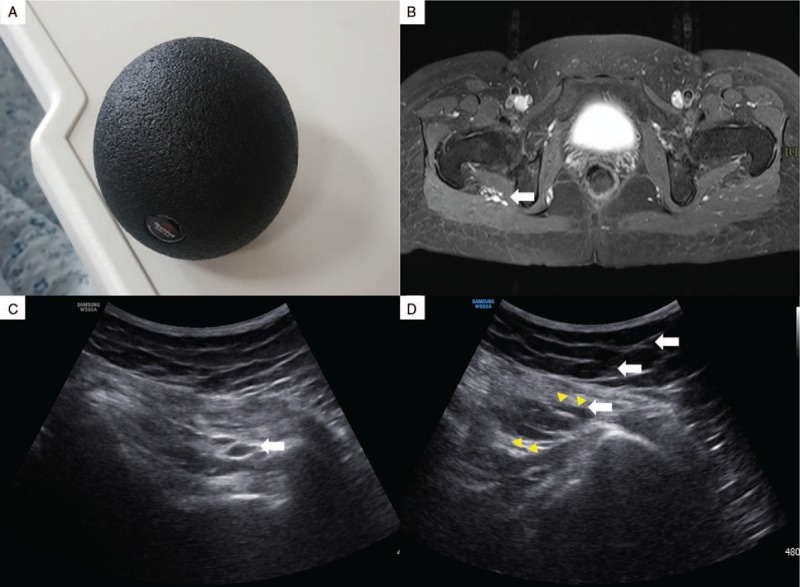
(A) Massage ball used for self-massage, (B) axial T2-weighted MRI of the pelvis showing high signal intensity and swelling of the right sciatic nerves (arrow), from the superior gemellus level to the quadratus femoris level, (C) ultrasound image of the right sciatic nerve (arrow), and (D) ultrasound image of the right sciatic nerve after ultrasound-guided perineural steroid injection. Needle pathway (arrow) and the injected fluid (arrow head) were seen around the sciatic nerve. MRI = magnetic resonance image.
Table 1.
The results of the electrophysiologic study.
The patient was initially prescribed pregabalin 300 mg for pain control. Although right lower extremity pain improved from 9 to 7 on numeric rating scale (NRS) score, there was no significant improvement with respect to her symptoms. The patient agreed to an ultrasound-guided perineural steroid injection, upon receiving detailed explanation of the disease and treatment procedure. During the ultrasound-guided injection, the patient was placed in a prone position. Following aseptic preparation of the puncture site, a 2 to 5 MHz curved ultrasound probe (Samsung Medison, Hongchun, Korea) was placed in a sterile plastic bag with ultrasound gel, and the probe was positioned transversely, lateral to the ischial tuberosity. Using the in-plane approach, a 23G long needle was pointed slightly to the medial side from the lateral side of the probe, which was then advanced toward the target using ultrasound guidance.[5] Then, a total of 10 mL of a mixture of 20 mg of triamcinolone (Dongkwang Pharm, Seoul, Korea) and 0.5% lidocaine was slowly injected (Fig. 1). Two days after the ultrasound-guided perineural steroid injection, the patient started to show significant pain improvement, going from an NRS score of 7 to 3. She was discharged on the third day after steroid injection. Thereafter, 2 additional ultrasound-guided perineural steroid injections were performed at 2-week intervals. Two months after the first visit, the patient's pain was well controlled at a NRS score of 3 to 4.
3. Discussion
The sciatic nerve is comprised of the medial and lateral division enclosed in a common sheath, with no exchange between the fascicles.[1] The medial division is the tibial nerve, and the lateral division is the peroneal nerve.[1] Generally, the sciatic nerve is divided into the common peroneal and tibial nerves at about 11 cm above the popliteal fossa crease. The sciatic nerve leaves the pelvis via the sciatic notch, passing underneath—in most cases—the piriformis muscle, which is covered by the gluteus maximus. In some individuals, the nerve occasionally passes through the piriformis muscle, or less commonly, above the piriformis muscle. In the thigh, the tibial nerve innervates all the hamstring muscles (semimembranosus, semitendinosus, and long head of biceps femoris), except the short head of the biceps femoris; the latter is innervated by the peroneal nerve. It has long been observed that partial sciatic nerve injuries usually affect the lateral division (common peroneal nerve) more severely than the medial division (tibial nerve). In this case report, however, a patient suffered an injury to the tibial division of the sciatic nerve after self-massage of the gluteal muscle using a massage ball. Unlike other sciatic neuropathies, this seems to be a selective, focal injury to the tibial division caused by a compression from the massage ball, rather than by stretching.
The treatment of sciatic neuropathy is generally medication specific to the pain, such as tricyclics, anticonvulsants, and topical analgesia.[3] In some cases, a simple combination of anti-inflammatory medication and mild exercise may also be prescribed. However, treatment of sciatic neuropathy solely with medication often leads to unsatisfactory outcome. In such cases, ultrasound-guided perineural steroid injection should be considered like other compressive neuropathies.[6,7] Perineural corticosteroid injection has been widely acknowledged for its excellent analgesic effects in compressive neuropathy.[7] Our case demonstrated unsatisfactory pain improvement with medication, but significant pain improvement after ultrasound-guided perineural steroid injection.
The patient received right L5 TFESI without any specific work-up (such as electrophysiologic study or pelvis MRI) due to radiating pain and repeated history of right L5 radiculopathy. Although the patient did not complain of any other symptoms, except radiating pain, there were tenderness and positive Tinel's sign at the gluteal muscle on physical examination. However, the electrophysiologic study showed a right tibial neuropathy proximal to the hamstring muscles. However, through MRI, we discovered that the patient's symptoms were caused by injury to the tibial division of the sciatic nerve. Therefore, it may be important to find a lesion via MRI when planning for treatment than rely solely on patient history and EMG test result.
Author contributions
Conceptualization: Byung Joo Lee.
Data curation: Hyunseok Moon.
Supervision: Sungwon Park.
Writing – original draft: Ju Young Cho, Donghwi Park.
Writing – review & editing: Donghwi Park.
Footnotes
Abbreviations: AH = abductor halluces, Amp = amplitude, BF = biceps femoris, CV = conduction velocity, Dur = duration, EDB = extensor digitorum brevis, EMG = electromyography, Fibs = fibrillation potentials, GCM = gastrocnemius, GM = gluteus maximus, IA = insertion activity, IP = interference pattern, LMC = local medical center, LP = lumbar paraspinalis, MRI = magnetic resonance image, Normal = normal values, NRS = numeric rating scale, PL = peroneus longus, PP = polyphasic potentials, Recruit = recruitment, PSW = positive sharp waves, RF = rectus femoris, Rt = right, SH = = short head, ST = semitendinosus, TAvtibialis anterior, TFESI = transforaminal epidural steroid injection, TFL = tensor fascia latae, TP = tibialis posterior, VM = vastus medialis.
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT, and Future Planning (NRF—2017R1D1A1B03033127).
No commercial party having a direct financial interest in the results of the research supporting this article has or will confer a benefit upon the authors or upon any organization with which the authors are associated.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Ropper AH, Zafonte RD. Sciatica. N Engl J Med 2015;372:1240–8. [DOI] [PubMed] [Google Scholar]
- [2].Plewnia C, Wallace C, Zochodne D. Traumatic sciatic neuropathy: a novel cause, local experience, and a review of the literature. J Trauma 1999;47:986–91. [DOI] [PubMed] [Google Scholar]
- [3].Ko JU, Seo H, Lee GJ, Park D. Bilateral sciatic neuropathy with severe rhabdomyolysis following venlafaxine overdose: a case report. Medicine 2018;97:e12220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Katirji B, Wilbourn AJ. High sciatic lesion mimicking peroneal neuropathy at the fibular head. J Neurol Sci 1994;121:172–5. [DOI] [PubMed] [Google Scholar]
- [5].Park D. Ultrasound-guided S1 transforaminal epidural injection using the in-plane approach and color doppler imaging. Am J Phys Med Rehabil 2018;97:e14–6. [DOI] [PubMed] [Google Scholar]
- [6].Park D. Ultrasonography of the transverse movement and deformation of the median nerve and its relationships with electrophysiological severity in the early stages of carpal tunnel syndrome. PM R 2017;9:1085–94. [DOI] [PubMed] [Google Scholar]
- [7].Wang JC, Chiou HJ, Lu JH, et al. Ultrasound-guided perineural steroid injection to treat intractable pain due to sciatic nerve injury. Can J Anaesth 2013;60:902–6. [DOI] [PubMed] [Google Scholar]


