Abstract
Rationale:
The purpose of this study is to introduce the technique of screw view model of navigation (SVMN) for upper cervical pedicle screw (UCPS) insertion. With the assistance of SVMN technology, the difficulty of screw placement manipulation can be diminished and the accuracy of placement can be improved.
Patient concerns:
A 49-year-old man presented with numbness of extremities and limited activity for 2 years.
Diagnoses:
He was diagnosed with old fracture of C1 vertebra and atlantoaxial subluxation.
Interventions:
We used SVMN to assist UCPS insertion and lateral mass screw insertion in this patient.
Outcomes:
A total of 2 pedicle screws and 2 lateral mass screws were inserted, all screws were defined as excellent position according to postoperative computer tomography (CT). The neurological function was intact postoperatively. The operation time was 293 minutes, the total fluoroscopic time was 4.1 minutes and the bleeding volume was 302 ml. There were no complications during the 48 months follow-up period.
Conclusions:
The application of SVMN in UCPS insertion could achieve satisfactory effect of internal fixation for upper cervical spine and avoid neurovascular damage. The utilization of SVMN for UCPS insertion is a safe and efficacious method. Besides, it also increased the patients’ hospital cost, and the surgeon must be quite familiar with the functional state of computer navigation.
Keywords: cervical, navigation, pedicle screw, screw view model
1. Introduction
A wide range of complex spine pathologies, including trauma, tumors, degeneration, or inflammatory diseases, requires instrumentation of the upper cervical spine.[1–7] Options for upper cervical pedicle screw (UCPS) placement include pars, transarticular, translaminar, and pedicle screws.[1] Although each screw has unique clinical indications, the pedicle screws are often the preferred method of instrumentation because of the superior fixation to the translaminar screw.[8]
In the past, screw insertion with freehand for upper cervical spine has obtained acceptable outcomes.[1,9–11] However, because of close proximity to spinal canal and surrounding vessels, misplacement of pedicle screw frequently occurs which can lead to disastrous complications.[12] The malposition rate of pedicle screw is 14% to 23% by freehand,[1,9–11] in which 2.7% to 3.3% patients suffered from vertebral artery injury and even death.[1,13] Computer assist procedures are now being increasingly used for the sake of improving the accuracy of pedicle screw, but there are still 26% to 33% screw malposition rate.[14–16]
To minimize surgical risk, we applied the screw view model of navigation (SVMN) to facilitate UCPS insertion. To our knowledge, the use of this novel technology for intraspinal tumor of the cervical spine has been rarely reported.
2. Ethics
This report was approved by the ethics committee of the Second Hospital of Jilin University, Changchun, China. (2019) Research and Inspection No. (006). The patient provided written informed consent for this report, and his information has been anonymized.
3. Case report
3.1. Patient characteristics
This otherwise healthy male patient presented at 49 years old (Table 1). He presented with numbness of extremities for 2 years and unstable walking for 6 months, in addition, the symptoms of discomfort have deteriorated for a month.
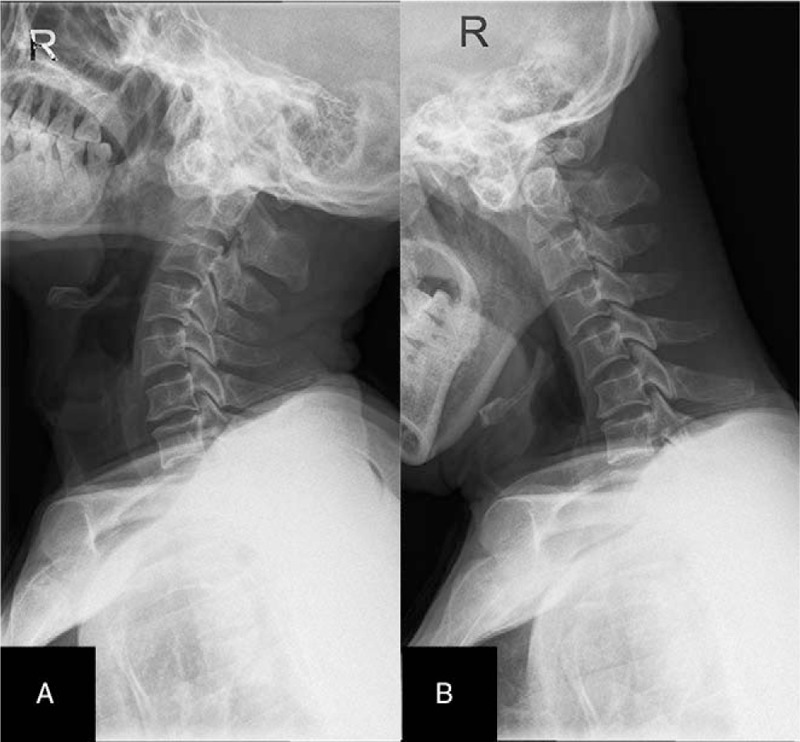
Table 1.
Basic characteristics of patients.
Examination revealed hyposensation of the skin were below the plane of the thoraco-clavicular joint, and the right side is more serious. Bilateral deltoid muscle strength was III grade, bilateral biceps brachii muscle strength was III grade, the muscle strength of bilateral triceps was grade III, and muscular hypertonia of extremities. Bilateral biceps hyperreflexia, hypertrophic triceps tendon reflex, bilateral hyperradial membranous reflex, and hyperactivity of bilateral knee and Achilles tendon reflex. Bilateral Babinski sign and bilateral Hoffman sign were positive, the result of bilateral ankle clonus test was positive. The Lasegue test and Bragard sign were negative.
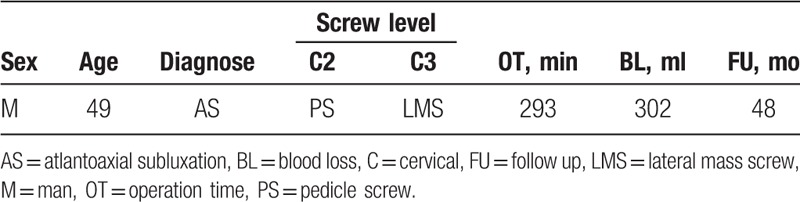
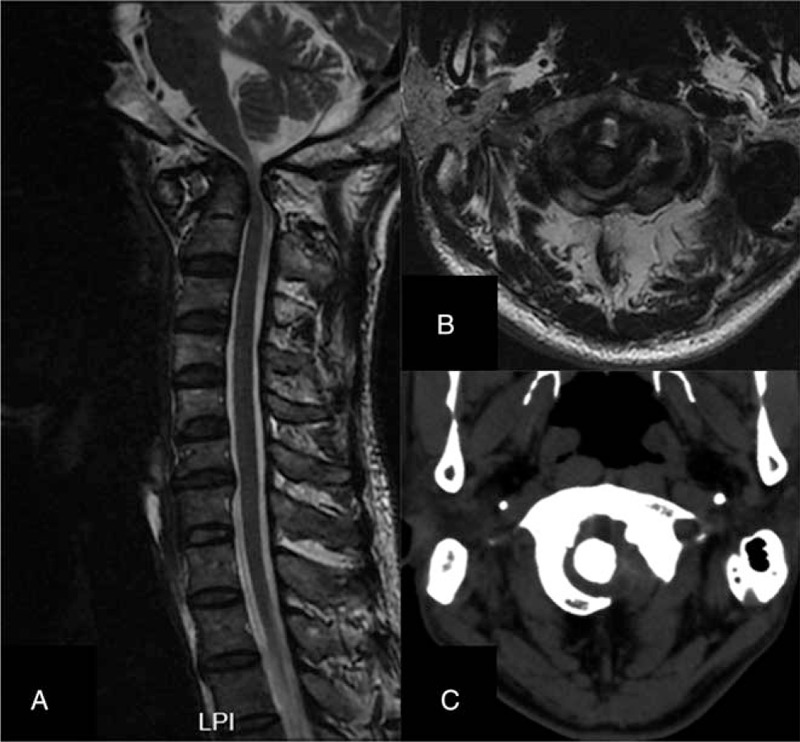
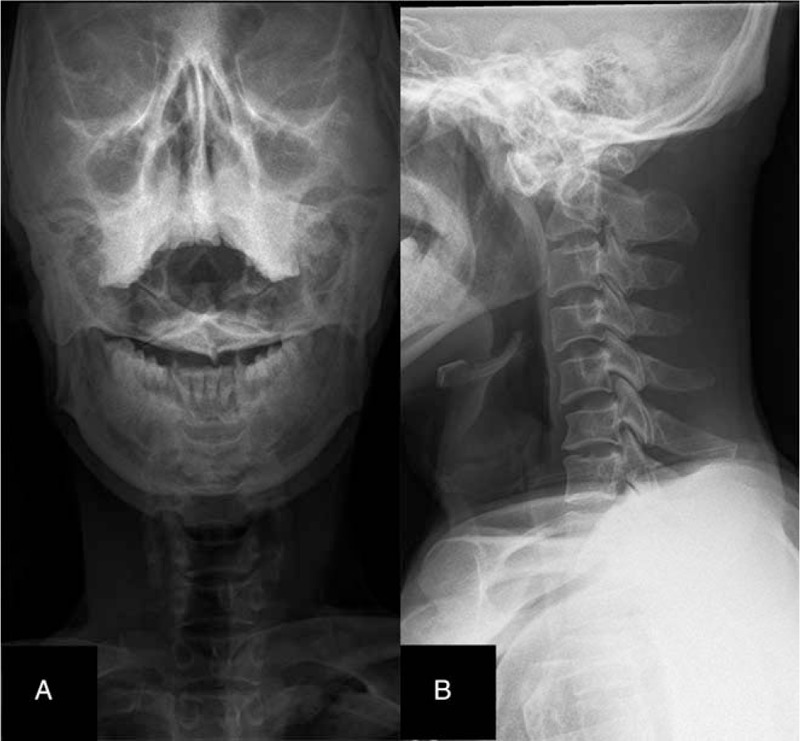
Magnetic resonance imaging demonstrated that the distance between the odontoid process and the left lateral mass was larger than that of the right. The spinal cord at C1 level was significantly compressed and thinned, and the cervical vertebra was hyperosteogeny (Fig. 1A and B). Three dimensional (3D) computed tomography (CT) of cervical spine showed that the distance between odontoid process and lateral atlas was asymmetric, and the left and right side was about 10.6 mm and 5.7 mm, respectively (Fig. 1C). The CT of cervical angiography examination showed that bilateral common carotid artery, bilateral internal carotid artery, bilateral vertebral artery, and basilar artery were clearly developed, and no obvious stenosis and filling defect were found. Cervical vertebrae X-ray film of open mouth position display that the anatomical relationship between odontoid process and lateral mass of atlas was destroyed, and the atlanto-dental-interval (ADI) was abnormal (Fig. 2A). Lateral cervical radiograph showed an increase in ADI (Fig. 2B). Cervical dynamic X-ray showed a significant increase in ADI (Fig. 3A and B). Results of electromyography of extremities showed that the sensory and motor nerve conduction velocity of the lower extremities was normal, and the H reflex of the double tibial nerve was normal, But, the deltoid, the biceps brachii, the triceps brachii expressed as neurogenic damage. The primary diagnosis was old fracture of C1 vertebra and atlantoaxial subluxation.
Figure 1.
Sagittal (A) and axial (B) of cervical spine MRI demonstrated that the spinal cord at C1 level was significantly compressed and thinned. CT of cervical spine (C) showed that the distance between odontoid process and lateral atlas was asymmetric. CT = computer tomography, MRI = magnetic resonance imaging.
Figure 2.
Open mouth position (A) and lateral (B) X-ray film of cervical spine display that the ADI was abnormal. ADI = atlanto-dental-interval.
Figure 3.
Hyperextension (A) and hyperflexion (B) X-ray film of cervical spine showed a significant increase in ADI. ADI = atlanto-dental-interval.
3.2. Surgical technique
Preoperative CT image of cervical spine was scanned and the graphic date was recorded in the disc in Digital Imaging and Communications in Medicine format. The disc could be recognized by computer navigation system, then the diameter, length, and trajectory of the pedicle screw was precise designed at the navigation work station (Fig. 4). The procedure was performed under general anesthesia. The patient was placed in the prone position. The posterior structures of the lesion segments were exposed.
Figure 4.
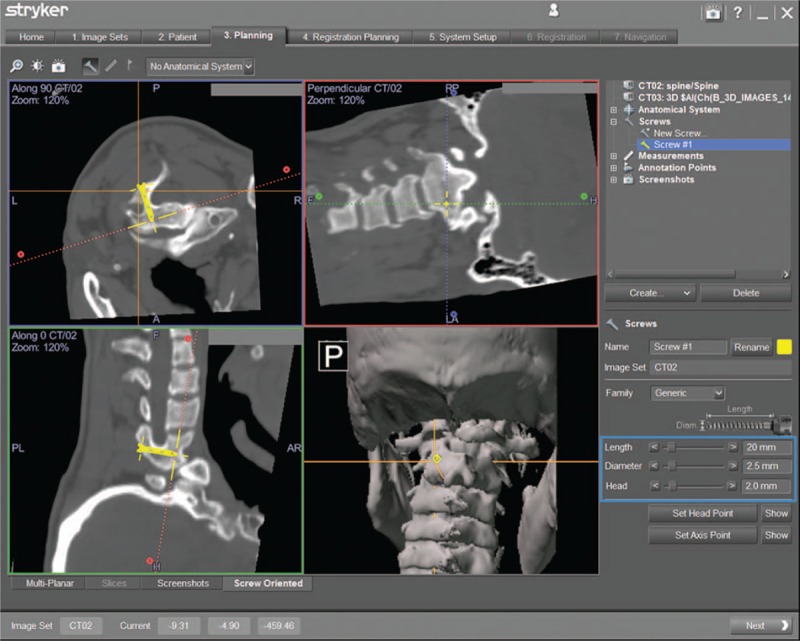
Preoperative designing, including the diameter, length, and trajectory of the pedicle screw, was performed at the navigation work station.
First step, the Navigation System workstation was started, and choose SpineMap 3D 2.0 software (Stryker Navigation, Kalamazoo, MI). Second step, a patient tracker (Stryker Leibinger GmbH & Co, Freiburg, Germany) was fixed on the vertebra spinous process. Third step, the instrument tracker, the patient tracker, and the system's C-arm tracker were activated. Fourth step, after 190° scanning was performed at the center of the segmental lesion, 3D images of the lesion were obtained. Fifth step, the SVMN was selected in the navigation workstation (Fig. 5), the real-time position of the surgical instrument was displayed on a computer monitor while the image of the design screw at the fracture was static. The infrared camera continuously updated the surgical instrument position simultaneously on multiplane, allowing real-time feedback of the designed screws and the location of the surgical instrument as the surgeon moved the instrument. SVMN helped the surgeon determine the optimal entry point and direction of UCPS accurately. The surgical instrument was moved until the direction of the device was completely aligned with the planning screw trajectory. At this point, the right lower corner image was highlighted in green (Fig. 5), and then the screw was placed. Sixth step, radical removal of tumor under electron microscope.[17] Seventh step, postoperative the precision of the pedicle screw was determined by CT scans (Fig. 6A and B). We evaluated the screw position described by Ughwanogho et al.[18] The patient was encouraged to wear a neck and chest brace for functional exercise 1 week postoperatively. Cervical spine X-rays (Fig. 7A and B) and CT were taken at the follow-up visit. The following data were also gathered from the medical records: the operation time, the bleeding volume, and the surgical complications.
Figure 5.
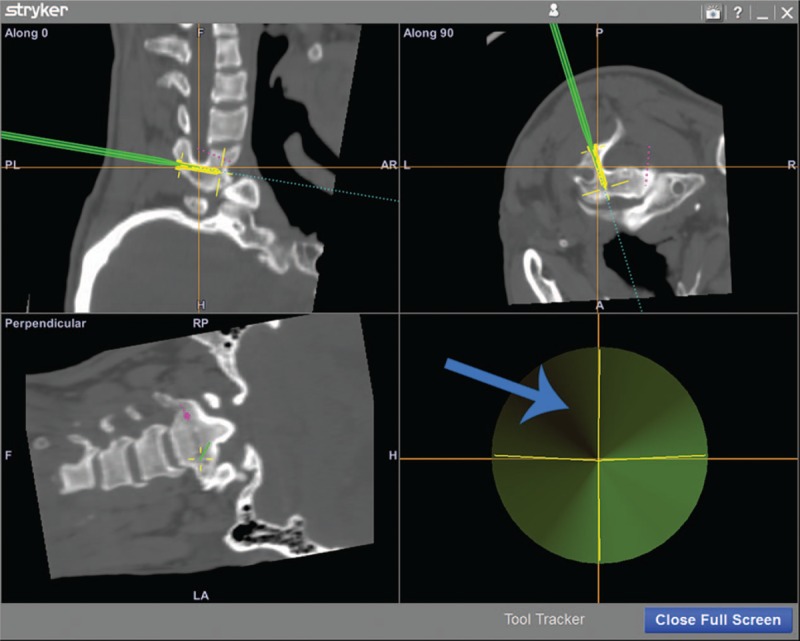
Screw view model of navigation was selected in the navigation workstation (red arrow), and it is the best time to place screw when the right lower corner image was highlighted in green (blue arrow).
Figure 6.
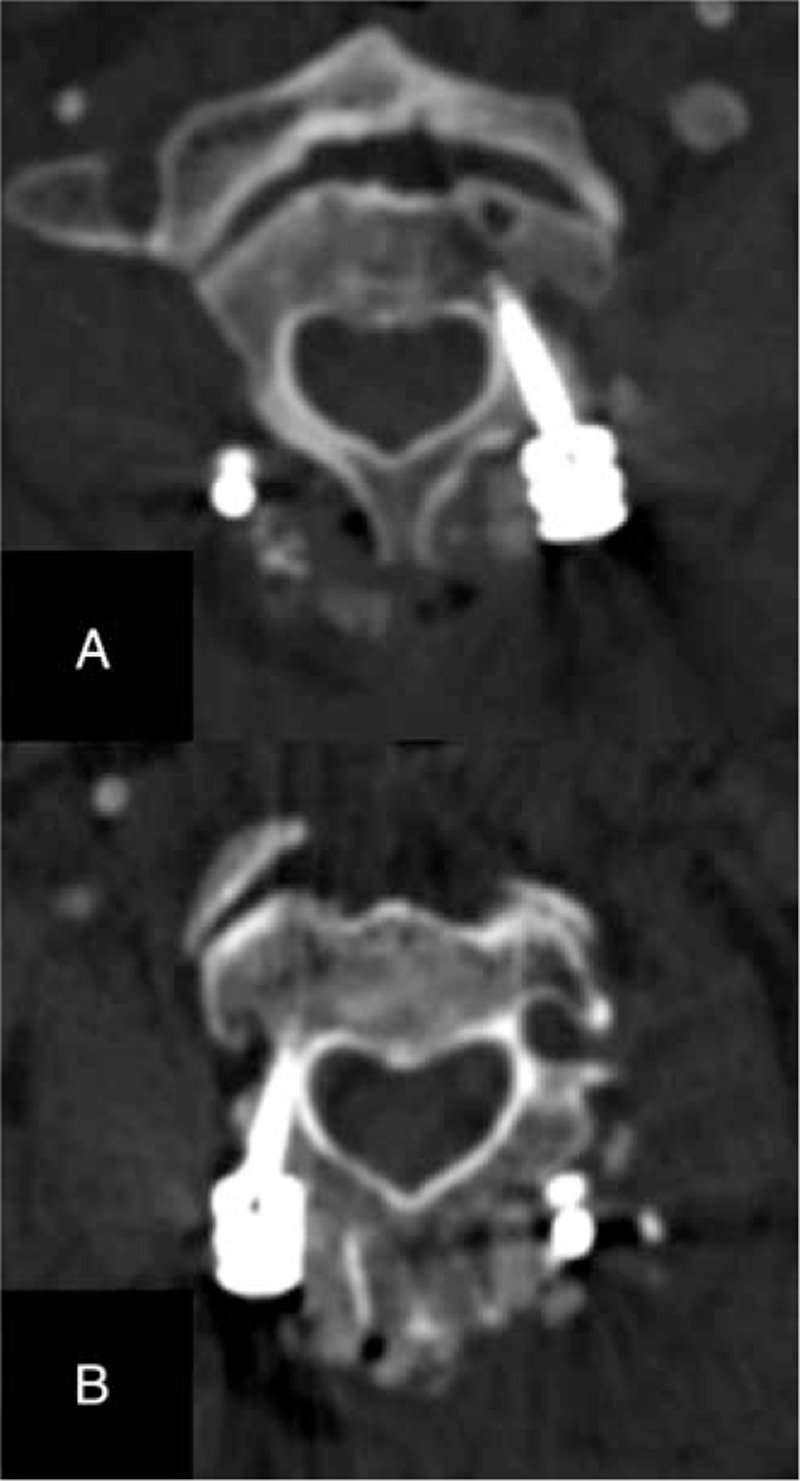
Postoperatively CT scanning showed that the screw position was excellent. CT = computer tomography.
Figure 7.
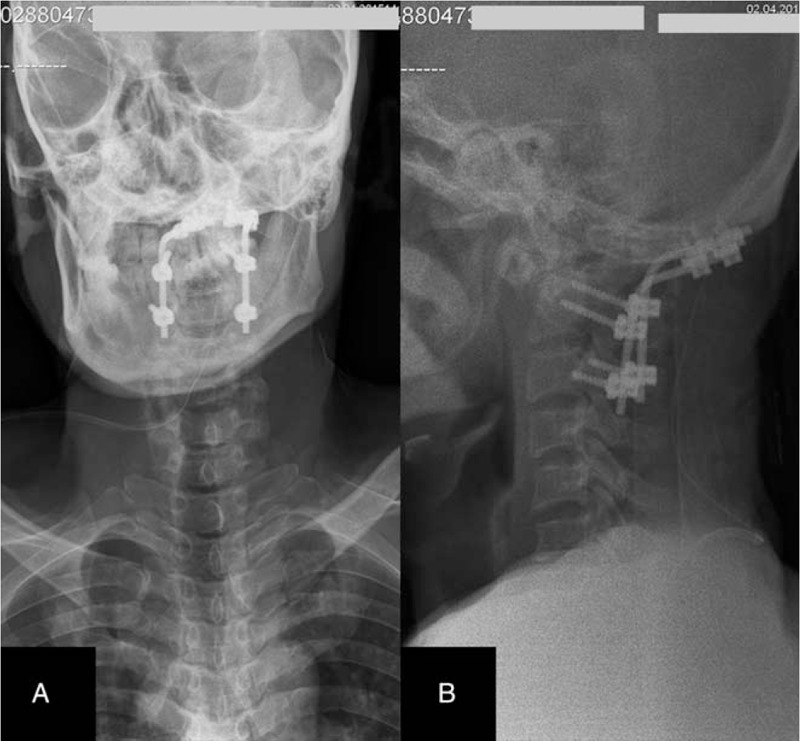
Anteroposterior (A) and lateral (B) x-ray of cervical spine.
A total of 4 pedicle screws were inserted, and the position of all screws were excellent determined by postoperative CT. The neurological function was intact postoperatively. No dysphagia, polypnea, screw loosening, pseudarthrosis formation, or infection was found during the 48 months follow-up period. The operation time was 293 minutes, the total fluoroscopic time was 4.1 minutes and the bleeding volume was 302 ml (Table 1). The patient had minimal postoperative pain easily controlled by oral Loxoprofen Sodium Tablets (Daiichi Sankyo Pharmaceutical Co, Ltd, Shanghai, China).
4. Discussion
Currently, several measures have been adopted to facilitate pedicle screw implantation in spine surgery, involving guiding devices,[19] 2D-guided navigation,[13] 3D-guided navigation,[1,14,15] robot-assisted surgery,[20] and 3D rapid prototyping technique.[21] Due to the complex anatomical structures and narrow osseous channels of vertebrae, the application of these methods still has 9.7% to 16.9% screw malposition rate.[1,13,19–21] To reduce surgical risk, we applied SVMN to facilitate UCPS insertion. In this study, a good therapeutic effect was achieved, and there was no neurovascular damage, less blood loss, and satisfactory stability in 48 months follow up.
Based on our experience, the indications and contraindications of SVMN technology are as follows.
Indications:
-
(1)
cervical fracture or dislocation,
-
(2)
cervical spinal stenosis,
-
(3)
cervical spinal canal tumors,
-
(4)
cervical spine malformation,
-
(5)
continuous ossification of the posterior longitudinal ligament of the cervical spine.
Contraindications:
-
(1)
severe destruction of pedicle screw channel caused by inflammation, tumors, or trauma,
-
(2)
the pedicle screw channel was too narrow that caused by developmental deformities to insert screw.
With regard to screw misplacement. Hlubek et al[1] reported that the misplacement rate of cervical pedicle screws under navigation was as high as 33%. In our study, there was no misplacement of pedicle screws, and there was no neurovascular complication found postoperatively. We attribute the accuracy of pedicle screw placement to SVMN technique. In our opinion, this technology could help surgeon to avoid nerve and vertebral artery compromise, pedicle damage, and can enhance the stability of spine.
The operation time was 293 minutes with SVMN and this outcome was similar to a literature reported by Jing et al.[15] Nevertheless our operation was more complex because we had to perform occipitocervical fusion. This positive outcome was most probably a attributed to full understanding about the spinal anatomical structures via 3D CT preoperatively and quickly identify the entry point, trajectory guided by computer navigation intraoperatively.
With regard to blood loss, there are 2 major factors leading to intraoperative blood loss, including vertebral artery injury[1] and prolonged surgery.[22] Vertebral artery injuries are mostly caused by misplacement of screws intraoperative. The duration of surgery was in association with total bleeding volume intraoperative, and usually blood loss during surgery could be frequently large volume.[22] It is critical for doctors to take effective measures to reduce the amount of bleeding during operation, because allogeneic blood transfusion may cause the infection risks and hemodynamic complications. In this study, we used lateral mass screw fixation in C3, and we believe this not only shortened the operation time and reduced intraoperative blood loss, but also ensured adequate fixation strength. The blood loss was 302 ml without vascular injury by SVMN technology, we attributed this positive result to accuracy screw insertion and much shorter operation time when using SVMN.
Loosening of pedicle screws is a common complication of posterior spinal fusion and fixation operation in spine surgery.[15] Literature reported[15,23,24] that the range of screw loosening from 3.3% to 19.5%. Screw loosening also in association with several complications, including screw breakage, pseudarthrosis, and poor stability of cervical spine. In this study, no pedicle screw loosening was observed during follow up visit. It is our view that screw implantation with SVMN and implanting all screws in 1 attempt avoided multiple drill holes that may lead to screw loosening,[25] and usage of a brace to ensure fusion and maintain stability for 3 months postoperatively contributed to this positive outcome.
Although the perfect results achieved in our study, there are also some limitations as follows, first, it increased the patients’ hospitalization charges, the financial cost was about 5000 Yuan RMB for application of SVMN. Besides, the surgeon needs to be quite familiar with the functional state of navigation, and constantly judge whether the image is drifted in the navigation during the operation, thus to avoid the operation failure of the operation due to the deviation of navigation accuracy.[26] Therefore, reduce operation cost and skillfully using computer navigation should be carried out to assess the effectiveness of SVMN technology for upper cervical screw insertion.
5. Conclusion
This study demonstrates that the SVMN could achieve better therapeutic effect for upper cervical screw insertion. The application of SVMN in upper cervical screw insertion might decrease screw loosening rate, the risk of screw misplacement and with a satisfactory fixation effect. Therefore, the utilization of SVMN for upper cervical screw insertion is a safe and efficacious method. Besides, it also increased the patients’ hospital cost, while we consider this to be insignificant compared with the vast increased safety of SVMN technology.
Acknowledgments
We gratefully acknowledge the cooperation of the doctors and nurses in the operating room.
Author contributions
Conceptualization: Jianwu Zhao, Mingyang Kang, Xin Zhao.
Data curation: Xiwen Zhang.
Methodology: Lili Yang, Rongpeng Dong, Xin Zhao.
Supervision: Jianwu Zhao.
Validation: Yang Qu.
Writing – original draft: Shuang Zheng, Tong Yu.
Writing – review and editing: Jianwu Zhao, Xin Zhao, Tong Yu.
Footnotes
Abbreviations: 3D = three dimensional, ADI = atlanto-dental-interval, C = cervical, SVMN = screw view model of navigation, UCPS = upper cervical pedicle screw.
XZ and TY contributed equally to this work
The authors have no conflicts of interest to disclose.
References
- [1].Hlubek RJ, Bohl MA, Cole TS, et al. Safety and accuracy of freehand versus navigated C2 pars or pedicle screw placement. Spine J 2018;18:1374–81. [DOI] [PubMed] [Google Scholar]
- [2].Guo Q, Wang L, Lu X, et al. Posterior temporary fixation versus nonoperative treatment for Anderson-D’Alonzo type III odontoid fractures: functional computed tomography evaluation of C1-C2 rotation. World Neurosurg 2017;100:675–80. [DOI] [PubMed] [Google Scholar]
- [3].Beytemur O, Baris A, Albay C, et al. Comparison of intramedullary nailing and minimal invasive plate osteosynthesis in the treatment of simple intra-articular fractures of the distal tibia (AO-OTA type 43 C1-C2). Acta Orthop Traumatol Turc 2017;51:12–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Shatsky J, Bellabarba C, Nguyen Q, et al. A retrospective review of fixation of C1 ring fractures – does the transverse atlantal ligament (TAL) really matter? Spine J 2016;16:372–9. [DOI] [PubMed] [Google Scholar]
- [5].Mead LB2nd, Millhouse PW, Krystal J, et al. C1 fractures: a review of diagnoses, management options, and outcomes. Curr Rev Musculoskelet Med 2016;9:255–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Guo Q, Deng Y, Wang J, et al. Comparison of clinical outcomes of posterior C1-C2 temporary fixation without fusion and C1-C2 fusion for fresh odontoid fractures. Neurosurgery 2016;78:77–83. [DOI] [PubMed] [Google Scholar]
- [7].Bednar DA, Almansoori KA. Solitary C1 posterior fixation for unstable isolated atlas fractures: case report and systematic review of the literature. Global Spine J 2016;6:375–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Du JY, Aichmair A, Kueper J, et al. Biomechanical analysis of screw constructs for atlantoaxial fixation in cadavers: a systematic review and meta-analysis. J Neurosurg Spine 2015;22:151–61. [DOI] [PubMed] [Google Scholar]
- [9].Bydon M, Mathios D, Macki M, et al. Accuracy of C2 pedicle screw placement using the anatomic freehand technique. Clin Neurol Neurosurg 2014;125:24–7. [DOI] [PubMed] [Google Scholar]
- [10].Pham MH, Bakhsheshian J, Reid PC, et al. Evaluation of C2 pedicle screw placement via the freehand technique by neurosurgical trainees. J Neurosurg Spine 2018;29:235–40. [DOI] [PubMed] [Google Scholar]
- [11].Punyarat P, Buchowski JM, Klawson BT, et al. Freehand technique for C2 pedicle and pars screw placement: is it safe? Spine J 2018;18:1197–203. [DOI] [PubMed] [Google Scholar]
- [12].Gelalis ID, Paschos NK, Pakos EE, et al. Accuracy of pedicle screw placement: a systematic review of prospective in vivo studies comparing free hand, fluoroscopy guidance and navigation techniques. Eur Spine J 2012;21:247–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Ondra SL, Marzouk S, Ganju A, et al. Safety and efficacy of C2 pedicle screws placed with anatomic and lateral C-arm guidance. Spine (Phila Pa 1976) 2006;31:E263–7. [DOI] [PubMed] [Google Scholar]
- [14].Bredow J, Oppermann J, Kraus B, et al. The accuracy of 3D fluoroscopy-navigated screw insertion in the upper and subaxial cervical spine. Eur Spine J 2015;24:2967–76. [DOI] [PubMed] [Google Scholar]
- [15].Jing L, Sun Z, Zhang P, et al. Accuracy of screw placement and clinical outcomes after O-arm-navigated occipitocervical fusion. World Neurosurg 2018;117:e653–9. [DOI] [PubMed] [Google Scholar]
- [16].Uehara M, Takahashi J, Ikegami S, et al. Screw perforation features in 129 consecutive patients performed computer-guided cervical pedicle screw insertion. Eur Spine J 2014;23:2189–95. [DOI] [PubMed] [Google Scholar]
- [17].Maira G, Amante P, Denaro L, et al. Surgical treatment of cervical intramedullary spinal cord tumors. Neurol Res 2001;23:835–42. [DOI] [PubMed] [Google Scholar]
- [18].Ughwanogho E, Patel NM, Baldwin KD, et al. Computed tomography-guided navigation of thoracic pedicle screws for adolescent idiopathic scoliosis results in more accurate placement and less screw removal. Spine (Phila Pa 1976) 2012;37:E473–8. [DOI] [PubMed] [Google Scholar]
- [19].Yang L, Li H, Tang J, et al. A novel guide device improves the accuracy of pedicle screw placement. Int J Clin Exp Med 2015;8:8634–40. [PMC free article] [PubMed] [Google Scholar]
- [20].Wang JQ, Wang Y, Feng Y, et al. Percutaneous sacroiliac screw placement: a prospective randomized comparison of robot-assisted navigation procedures with a conventional technique. Chin Med J (Engl) 2017;130:2527–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Yang M, Li C, Li Y, et al. Application of 3D rapid prototyping technology in posterior corrective surgery for Lenke 1 adolescent idiopathic scoliosis patients. Medicine (Baltimore) 2015;94:e582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Ialenti MN, Lonner BS, Verma K, et al. Predicting operative blood loss during spinal fusion for adolescent idiopathic scoliosis. J Pediatr Orthop 2013;33:372–6. [DOI] [PubMed] [Google Scholar]
- [23].Ohtori S, Inoue G, Orita S, et al. Comparison of teriparatide and bisphosphonate treatment to reduce pedicle screw loosening after lumbar spinal fusion surgery in postmenopausal women with osteoporosis from a bone quality perspective. Spine (Phila Pa 1976) 2013;38:E487–92. [DOI] [PubMed] [Google Scholar]
- [24].Morr S, Carrer A, Alvarez-Garcia de Quesada LI, et al. Skipped versus consecutive pedicle screw constructs for correction of Lenke 1 curves. Eur Spine J 2015;24:1473–80. [DOI] [PubMed] [Google Scholar]
- [25].Gao H, Luo CF, Hu CF, et al. Minimally invasive fluoro-navigation screw fixation for the treatment of pelvic ring injuries. Surg Innov 2011;18:279–84. [DOI] [PubMed] [Google Scholar]
- [26].Li QJ, Yu T, Liu LH, et al. Combined 3D rapid prototyping and computer navigation facilitate surgical treatment of congenital scoliosis: a case report and description of technique. Medicine (Baltimore) 2018;97:e11701. [DOI] [PMC free article] [PubMed] [Google Scholar]


