Abstract
Background:
To compare the clinical efficacy between Orthopilot navigation system and conventional manual surgery in total hip arthroplasty (THA).
Methods:
Electronic databases were searched to identify randomized controlled trials (RCTs) investigating Orthopilot navigation system versus conventional manual in patients undergoing THA. Outcome measurements include anteversion angle, inclination angle, preoperative leg length discrepancy, postoperative leg length discrepancy and femoral offset. Statistical software Stata 12.0 was used for data-analysis.
Results:
A total of 5 studies were finally included in this meta-analysis. The results showed that the conventional manual group have a less anteversion angle than that in Orthopilot navigation system group (weighted mean difference (WMD) = 4.67, 95% confidence interval (CI) = 3.53, 5.82, P = .000). And pooled analysis showed that the inclination angle in Orthopilot navigation group was less than that in conventional manual group (WMD = −4.19, 95% CI = −8.00, −0.37, P = .031). There was no significant difference between the preoperative leg length discrepancy and postoperative leg length discrepancy (P > .05). Orthopilot navigation system compared with conventional manual procedure was associated with decreased of femoral offset by 2.76 (WMD = −2.76, 95%CI = −3.90, −1.62, P = .000).
Conclusion:
Both Orthopilot navigation system and conventional THA result in significant improvements in patient function with similar overall complication rates and have their own edges in cup position.
Keywords: conventional, meta-analysis, orthopilot navigation, total hip arthroplasty
1. Introduction
Total hip arthroplasty (THA) is one of the most effective and frequent performed operations worldwide to relieve pain and restore function to the hip joint osteoarthritis.[1,2] Every year, more than 1 million people worldwide undergo THA for severe hip osteoarthritis (OA) with intractable or permanent pain and dysfunctions, and this number is expected to double within the next 20 years.[3] THA completely changed the treatment method of previous hip disease with arthritis in the 1960s and achieved excellent long-term efficacy.[4] The scholars have devoted themselves to prolonging the service life of artificial joints by accurately positioning the prosthesis, reducing wear, and reducing the fretting of the prosthesis in THA.[5,6]
In recent years, with the breakthrough of computer and artificial intelligence technology, imageless navigation system has become an important application in clinic,[7] and used successfully in total knee arthroplasty, unicompartmental knee arthroplasty, THA, and shoulder arthroplasty, etc.[8] Imageless navigation system is used to detect the anatomic data, mechanical axis of the limbs or position of the joint intraoperatively through a 3-dimensional optical positioning device and without the preoperative or intraoperative images of patients (computed tomography (CT), magnetic resonance imaging (MRI), C-arm fluoroscopy, and X-ray image).[9] In January 1997, Saragaglia et al first introduced the Orthopilot imageless navigation system into total knee arthroplasty.[10] Imageless navigation uses optical sensors as 3D position sensors to track the target bones and surgical tools or implants. In cup placement, the imageless navigation system measures the anteversion and inclination angles relative to the anterior pelvic plane. Since then, a large number of clinical trials have showed that navigation operation of such systems improves precision and accuracy over conventional manual surgery.[11,12] However, it remains controversial on the choice of imageless navigation or traditional operation in THA.[13]
This study aimed to systematically compare the clinical efficacy between the 2 methods through meta-analysis so as to give some theoretical guidance for clinical practice.
2. Methods
The current meta-analysis was performed according to the recommendations of the Cochrane Handbook for Systematic Reviews of Interventions and was reported in compliance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement guidelines. This is a meta-analysis; no ethics approval and consent to participate exist.
2.1. Search strategy
Following the recommendations of the Cochrane collaborations, the retrieval was performed in the online databases include Embase, Pubmed, Web of Science from inception to September 2018. Manually search the magazine catalog and references, and strive to find gray literature, such as unpublished academic papers and chapters in monographs. Searching all pertinent papers without restricting the language and translating if necessary. Keywords both for Chinese and English search were: total hip arthroplasty, THA, imageless, navigation, conventional, manual, and freehand. Search strategy was: total hip arthroplasty OR THA AND imageless OR navigat∗ AND conventional OR manual OR freehand.
2.2. Inclusion criteria
Inclusion criteria for the study were
-
1.
Adults with severe hip disease (Osteoarthritis, developmental dysplasia of the hip (DDH), adult avascular necrosis (AVN), rheumatoid arthritis (RA), Paget's disease etc.);
-
2.
controlled trials, prospective studies, retrospective studies, and cohort studies;
-
3.
all patients underwent for THA;
-
4.
study compared clinical efficacy of Orthopilot navigation system and conventional manual approaches.
2.3. Exclusion criteria
The exclusion criteria were:
-
1.
duplicates publications;
-
2.
letters, comments, editorials, case reports, proceedings, personal communications, or reviews;
-
3.
cadaveric study;
-
4.
study objective or intervention measures failed to meet the inclusion criteria;
-
5.
the original documents of experimental design being not precise;
-
6.
studied with incomplete data.
2.4. Data extraction and quality assessment
Data in included trials were extracted by 2 independent investigators (Jianguo Jia and Qun Zhao). Disagreement between the 2 reviewers was settled by discussion and consulting to a third reviewer. The extracted information included:
-
1.
the basic characteristics of the included studies, including the titles, authors, journals, volume, publication date;
-
2.
research methodological characteristics: random, control, blindness, etc.;
-
3.
research object characteristics: The general condition of patients, such as gender, age, race, etc., and the baseline situation of patients, disease course, severity, etc.;
-
4.
sample size, Intervention methods, follow-up time, outcome measurements.
The risk-of-bias assessment tool outlined in Cochrane Handbook was used to assess the methodological quality of controlled clinical trials (CCTs). Six domains are evaluated:
-
1.
random sequence generation;
-
2.
allocation concealment;
-
3.
blinding of patients and personal;
-
4.
blinding of outcome assessment;
-
5.
incomplete outcome data;
-
6.
and selective reporting risk.
Relevant data were recorded in this analysis, including: first author's name, published year, sample size of Orthopilot navigation system and conventional manual approaches for THA etc.
2.5. Outcome measures
Outcome measurements include 5 main aspects:
-
1.
anteversion angle,
-
2.
inclination angle,
-
3.
preoperative leg length discrepancy,
-
4.
postoperative leg length discrepancy,
-
5.
femoral offset.
2.6. Statistical analysis
All data analyses were conducted by using the Stata 12.0 software. Dichotomous outcomes were expressed in terms of risk ratio (RR) and the weighted mean difference (WMD) or the weighted mean difference (WMD) was used for continuous outcomes, both with 95% confidence intervals (CI).[14] Heterogeneity was tested using both the chi-square test and I2 test. A fixed-effects model was chosen when there was no statistical evidence of heterogeneity (I2 < 50%) and random-effects model was adopted if significant heterogeneity was found (I2 ≥ 50%).[15] If the heterogeneity was found, we checked the study population, treatment, outcome and methodologies to determine the source of heterogeneity. If it could not be quantitatively synthesized or the event rate was too low to be measured, we used qualitative evaluation.[16] By eliminating some of the studies for sensitivity analysis and making funnel plots to assess the bias. The difference was statistically significant when P < .05.
3. Results
3.1. Search results
A total of 115 articles were retrieved based on the search strategy through online database searching and manual searching. After removing the duplication, a total of 59 studies were included for overview. By reading the titles and abstracts, 54 articles that are not related to the purpose of the study were excluded. Finally, 5 studies[17–21] involving 719 patients were included. The literature screening process and the results shown in Figure 1. Basic characteristics of included literature presented in Table 1.
Figure 1.
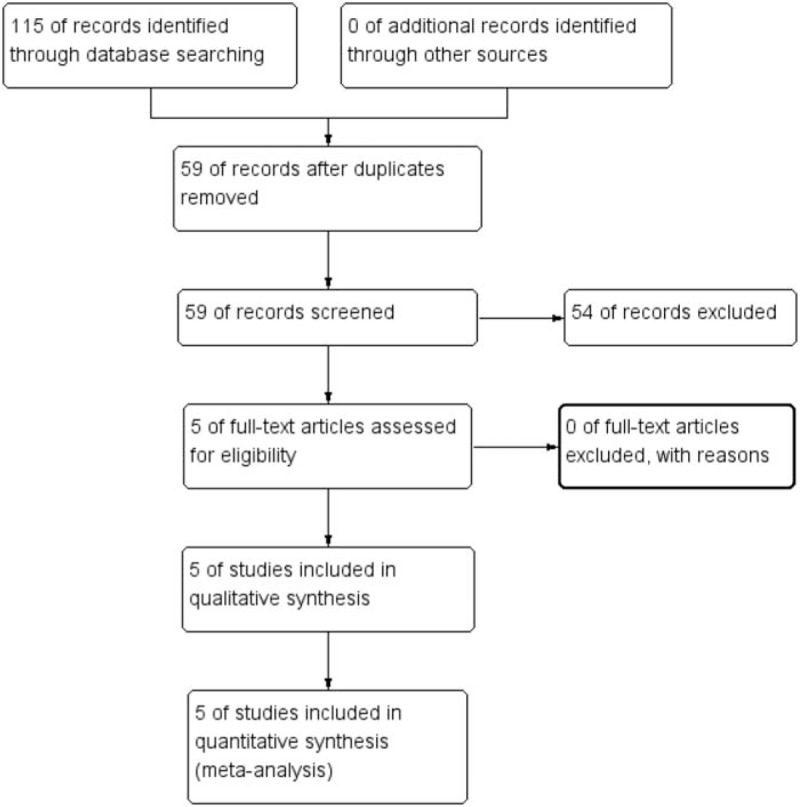
The flow diagram of study selection.
Table 1.
General characteristic of the included studies.

Figure 2 and Figure 3 shows the risk of bias summary and risk of bias graph respectively. Only 1 study did not describe the random sequence generation and classified as unclear risk of bias. Allocation concealment was low risk of bias in 2 studies, the rest studies were classified as unclear risk of bias.
Figure 2.
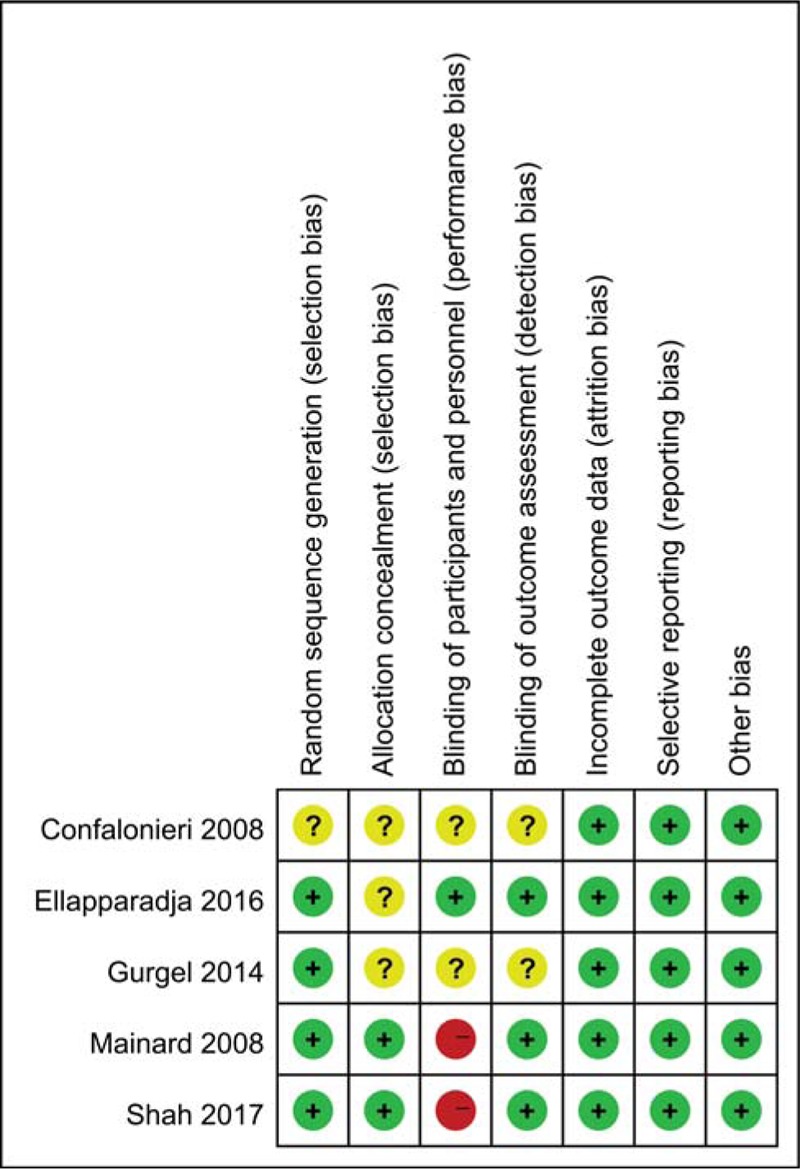
Risk of bias summary for included studies. +, no bias; –, bias; ?, bias unknown.
Figure 3.
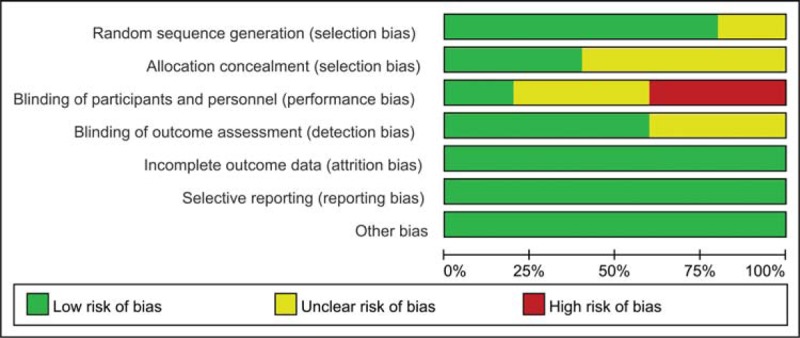
Risk of bias graph: review authors’ judgments about each risk of bias item presented as percentages across all included studies.
3.2. Anteversion angle
Three studies involving 468 patients compared the anteversion angle between the Orthopilot navigation system and conventional manual procedure. Fixed effect model was employed in meta-analysis with the absence of heterogeneity (I2 = 0.0%, P = .715) among the 3 studies. The results showed that the conventional manual group have a less anteversion angle than that in Orthopilot navigation system group (WMD = 4.67, 95%CI = 3.53, 5.82, P = .000, Fig. 4).
Figure 4.
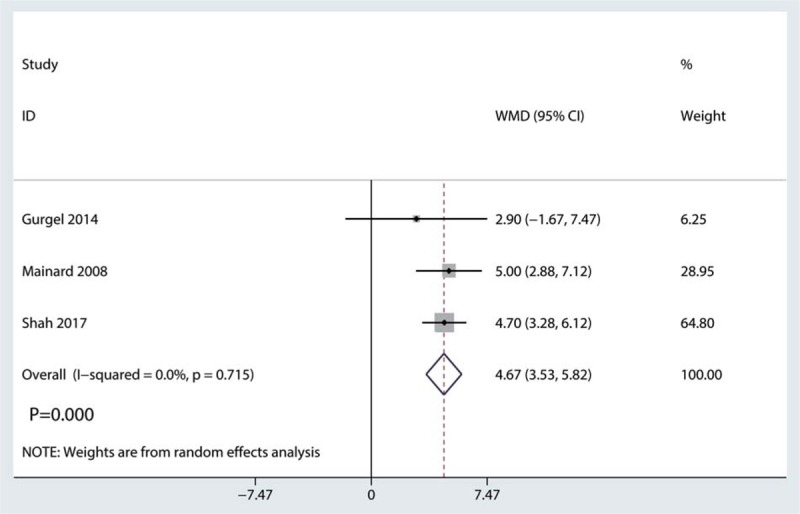
Forest plot for comparing Orthopilot navigation system and conventional manual procedure in terms of anteversion angle.
3.3. Inclination angle
Three studies included have compared inclination angle between Orthopilot navigation system and conventional manual procedure. Random effect model was employed in meta-analysis because the heterogeneity between the studies was significant (I2 = 91%). The meta-analysis showed that the inclination angle in Orthopilot navigation group was less than that in conventional manual group (WMD = −4.19, 95%CI = −8.00, −0.37, P = .031, Fig. 5).
Figure 5.

Forest plot for comparing Orthopilot navigation system and conventional manual procedure in terms of inclination angle.
3.4. Complications
We compared preoperative leg length discrepancy, result was shown in Figure 6. There was no significant difference between the preoperative leg discrepancy (WMD = −1.09, 95%CI = −5.01, 2.82, P = .584).
Figure 6.
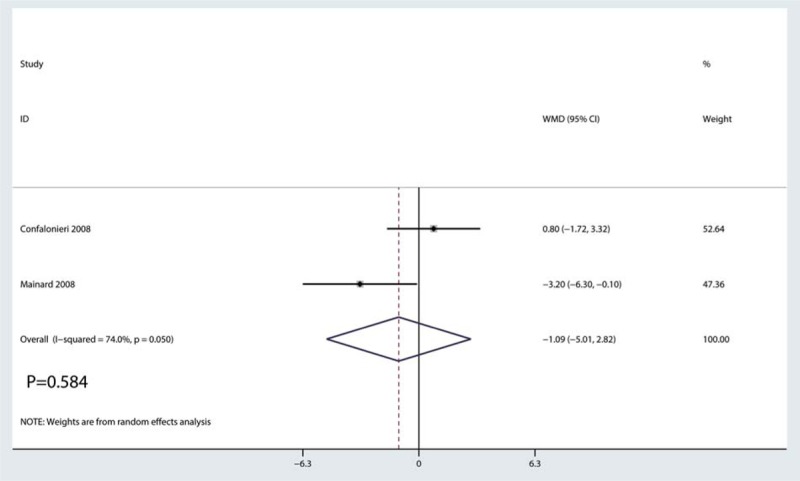
Forest plot for comparing Orthopilot navigation system and conventional manual procedure in terms of preoperative leg length discrepancy.
We then compared postoperative leg length discrepancy between Orthopilot navigation system and conventional manual procedure. Results shown that there was no significant difference between Orthopilot navigation system and conventional manual procedure in terms of the postoperative leg length discrepancy (WMD = −1.36, 95% CI = −4.36, 1.63, P = .372, Fig. 7).
Figure 7.
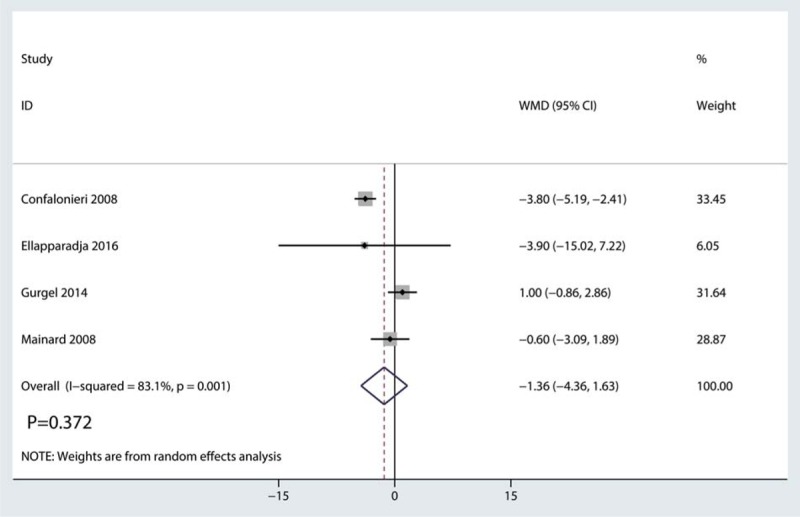
Forest plot for comparing Orthopilot navigation system and conventional manual procedure in terms of potoperative leg length discrepancy.
Two trials involving 386 participants reported femoral offset. Orthopilot navigation system compared with conventional manual procedure was associated with decreased of femoral offset by 2.76 (WMD = −2.76, 95%CI = −3.90, −1.62, P = .000, Fig. 8).
Figure 8.
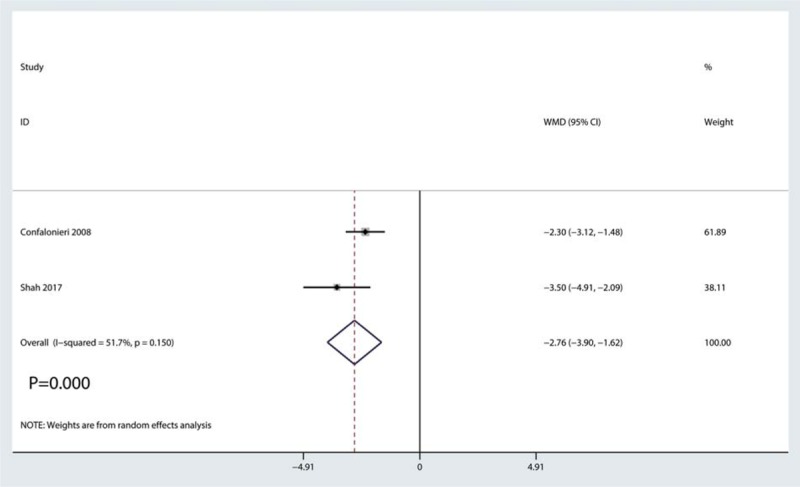
Forest plot for comparing Orthopilot navigation system and conventional manual procedure in terms of femoral offset.
4. Discussion
Total hip arthroplasty (THA) is a relatively mature and widely used in orthopaedic surgery.[22,23] The key to the long-term success rate of THA is the accurate placement of the prosthesis.[24] Inaccurate placement of the prosthesis will lead to false femoral head and acetabulum impact and limited mobility.[25] Accurate mounting of the prosthesis requires the surgeon to accurately position the patient's pelvic and femoral locations.[26] In traditional surgery, preoperative imaging, and template measurements assist in the intraoperative placement of the prosthesis.[27] However, due to the large number of factors affecting preoperative imaging, and the unstable position of the intraoperative patient, the position of pelvis and femur changes,[28] causing deviations between the intraoperative and preoperative results, which ultimately affect the placement of the prosthesis.[29]
The core of imageless navigation technology is to use computer technology to accurately correlate the preoperative image data with the anatomy of the intraoperative patient, track the surgical instruments in real time by detecting markers and display them in a virtual scene, and transmit the information to the surgeon in real time. A number of clinical studies have shown that imageless navigation can improve the accuracy of prosthesis placement, thereby reducing the occurrence of complications such as postoperative dislocation, compared with traditional THA surgery.
Imageless navigation (Orthopilot system) can obtain 3-dimensional image data and simulate the degree of hip movement before surgery, which facilitates to the preparation of planning; it can track and guide the operation during surgery, and it can also assess the placement of the prosthesis. However, due to the high cost of computer navigation equipment, complex application of the system, and navigation takes time, there continues to be controversial for THA under navigation. We selected 3 outcomes including anteversion, Inclination, complication and strive to fully compare the efficacy between the 2 procedures. By comparison, statistically significant differences on femoral offset, overall complications, anteversion and inclination between 2 groups were found. The results indicating that using Orthopilot navigation system can achieve less complication of femoral offset and better inclination compared with conventional THA, but conventional manual method showed its edge on anteversion.
This systematic review included 5 trials, and the methodological quality evaluation results were all middle quality. But a slight risk of bias remained in some studies, which may be related to that the patients should be informed which surgical method can be chose and medical ethical problems are involved. Incomplete outcome data, insufficient cases number of trials, and the various level between clinical surgeons may also lead to low methodological quality evaluation results and affect reliability of meta-analysis results. In the same outcome measurements system, we include into the maximum of 5 articles least of 2, therefore, the heterogeneity between groups will increase. Therefore, the above conclusions still need to further verify depends on the emergence of more randomized controlled trials with higher quality and larger sample sizes in the future.
5. Conclusion
This meta-analysis demonstrates that acetabular implant positioning can be significantly improved by the use of Orthopilot navigation system. However, studies with larger sample sizes and long-term results are needed in the future.
Author contributions
Data curation: Jianguo Jia, Hao Chen, Zhengshuai Jin.
Formal analysis: Zhengshuai Jin.
Investigation: Pei Lu, Jinlian Liu.
Methodology: Chaoqun Liu.
Project administration: Chaoqun Liu, Jinlian Liu.
Resources: Qun Zhao, Jinlian Liu, Sheng Chen.
Software: Qun Zhao.
Supervision: Guiyong Fan.
Validation: Guiyong Fan, Sheng Chen.
Writing – review & editing: Jianguo Jia, Pei Lu.
Footnotes
Abbreviations: AVN = adult avascular necrosis, CCTs = controlled clinical trials, CI = confidence interval, CT = computed tomography, DDH = developmental dysplasia of the hip, MRI = magnetic resonance imaging, OA = osteoarthritis, RA = rheumatoid arthritis, RCTs = randomized controlled trials, RR = risk ratio, THA = total hip arthroplasty, WMD = weighted mean difference.
The authors have no funding and conflicts of interests to disclose.
Supporting data is available.
References
- [1].Wang Z, Hou JZ, Wu CH, et al. A systematic review and meta-analysis of direct anterior approach versus posterior approach in total hip arthroplasty. J Orthop Surg Res 2018;13:229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Shi J, Liang G, Huang R. Effects of bisphosphonates in preventing periprosthetic bone loss following total hip arthroplasty: a systematic review and meta-analysis. J Orthop Surg Res 2018;13:225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Learmonth ID, Young C, Rorabeck C. The operation of the century: total hip replacement. Lancet 2007;370:1508–19. [DOI] [PubMed] [Google Scholar]
- [4].Zhu XT, Chen L, Lin JH. Selective COX-2 inhibitor versus non-selective COX-2 inhibitor for the prevention of heterotopic ossification after total hip arthroplasty: a meta-analysis. Medicine (Baltimore) 2018;97:e11649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Girard J, Lavigne M, Vendittoli PA, et al. Biomechanical reconstruction of the hip: a randomised study comparing total hip resurfacing and total hip arthroplasty. J Bone Joint Surg Br 2006;88:721–6. [DOI] [PubMed] [Google Scholar]
- [6].Saucedo JM, Marecek GS, Wanke TR, et al. Understanding readmission after primary total hip and knee arthroplasty: who's at risk? J Arthroplasty 2014;29:256–60. [DOI] [PubMed] [Google Scholar]
- [7].Chang JD, Kim IS, Prabhakar S, et al. Revision total hip arthroplasty using imageless navigation with the concept of combined anteversion. J Arthroplasty 2017;32:1576–80. [DOI] [PubMed] [Google Scholar]
- [8].Zagra L. Advances in hip arthroplasty surgery: what is justified? EFORT Open Rev 2017;2:171–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Wassilew GI, Perka C, Janz V, et al. Use of an ultrasound-based navigation system for an accurate acetabular positioning in total hip arthroplasty: a prospective, randomized, controlled study. J Arthroplasty 2012;27:687–94. [DOI] [PubMed] [Google Scholar]
- [10].Parratte S, Argenson JN, Flecher X, et al. Computer-assisted surgery for acetabular cup positioning in total hip arthroplasty: comparative prospective randomized study. Rev Chir Orthop Reparatrice Appar Mot 2007;93:238–46. [DOI] [PubMed] [Google Scholar]
- [11].Brown ML, Reed JD, Drinkwater CJ. Imageless computer-assisted versus conventional total hip arthroplasty: one surgeon's initial experience. J Arthroplasty 2014;29:1015–20. [DOI] [PubMed] [Google Scholar]
- [12].Rebal BA, Babatunde OM, Lee JH, et al. Imageless computer navigation in total knee arthroplasty provides superior short term functional outcomes: a meta-analysis. J Arthroplasty 2014;29:938–44. [DOI] [PubMed] [Google Scholar]
- [13].Renkawitz T, Weber M, Springorum HR, et al. Impingement-free range of movement, acetabular component cover and early clinical results comparing ‘femur-first’ navigation and ‘conventional’ minimally invasive total hip arthroplasty: a randomised controlled trial. Bone Joint J 2015;97-b:890–8. [DOI] [PubMed] [Google Scholar]
- [14].Chen IJ, Chang KV, Wu WT, et al. Ultrasound parameters other than the direct measurement of ulnar nerve size for diagnosing cubital tunnel syndrome: a systemic review and meta-analysis. Arch Phys Med Rehabil 2018;[Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- [15].Chang KV, Chen JD, Wu WT, et al. Association between loss of skeletal muscle mass and mortality and tumor recurrence in hepatocellular carcinoma: a systematic review and meta-analysis. Liver Cancer 2018;7:90–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Chang KV, Wu WT, Han DS, et al. Ulnar nerve cross-sectional area for the diagnosis of cubital tunnel syndrome: a meta-analysis of ultrasonographic measurements. Arch Phys Med Rehabil 2018;99:743–57. [DOI] [PubMed] [Google Scholar]
- [17].Confalonieri N, Manzotti A, Montironi F, et al. Leg length discrepancy, dislocation rate, and offset in total hip replacement using a short modular stem: navigation vs conventional freehand. Orthopedics 2008;31Suppl 1:35541. [PubMed] [Google Scholar]
- [18].Ellapparadja P, Mahajan V, Atiya S, et al. Leg length discrepancy in computer navigated total hip arthroplasty - how accurate are we? Hip Int 2016;26:438–43. [DOI] [PubMed] [Google Scholar]
- [19].Gurgel H, Croci AT, Cabrita HA, et al. Acetabular component positioning in total hip arthroplasty with and without a computer-assisted system: a prospective, randomized and controlled study. J Arthroplasty 2014;29:167–71. [DOI] [PubMed] [Google Scholar]
- [20].Mainard D. Navigated and nonnavigated total hip arthroplasty: results of two consecutive series using a cementless straight hip stem. Orthopedics 2008;31.Suppl 1:35528. [PubMed] [Google Scholar]
- [21].Shah SM, Deep K, Siramanakul C, et al. Computer navigation helps reduce the incidence of noise after ceramic-on-ceramic total hip arthroplasty. J Arthroplasty 2017;32:2783–7. [DOI] [PubMed] [Google Scholar]
- [22].Fillingham YA, Ramkumar DB, Jevsevar DS, et al. The safety of tranexamic acid in total joint arthroplasty: a direct meta-analysis. J Arthroplasty 2018;33:3070–82. [DOI] [PubMed] [Google Scholar]
- [23].Sun Y, Jiang C, Li Q. A systematic review and meta-analysis comparing combined intravenous and topical tranexamic acid with intravenous administration alone in THA 2017;12:e0186174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Migliorini F, Biagini M, Rath B, et al. Total hip arthroplasty: minimally invasive surgery or not? Meta-analysis of clinical trials. Int Orthop 2018;[Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- [25].Renkawitz T, Tingart M, Grifka J, et al. Computer-assisted total hip arthroplasty: coding the next generation of navigation systems for orthopedic surgery. Expert Rev Med Devices 2009;6:507–14. [DOI] [PubMed] [Google Scholar]
- [26].Fukunishi S, Nishio S, Fujihara Y, et al. Accuracy of combined anteversion in image-free navigated total hip arthroplasty: stem-first or cup-first technique? Int Orthop 2016;40:9–13. [DOI] [PubMed] [Google Scholar]
- [27].Hoorntje A, Janssen KY, Bolder SBT, et al. The effect of total hip arthroplasty on sports and work participation: a systematic review and meta-analysis. Sports Med 2018;48:1695–726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Nganga M, Bramwell D, Monaghan J, et al. Evaluation of the multi-attribute prioritisation tool for total joint replacement. J Orthop 2018;15:242–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].York PJ, McGee AW, Jr, Dean CS, et al. The relationship of pelvic incidence to post-operative total hip arthroplasty dislocation in patients with lumbar fusion. Int Orthop 2018;42:2301–6. [DOI] [PubMed] [Google Scholar]


