Abstract
C-reactive protein (CRP) is a biomarker for cardiovascular events and also has been studied as a biomarker for cognitive decline. By the year 2050 the Hispanic population in the United States will reach 106 million, and 65% of those will be of Mexican heritage. The purpose of this study was to evaluate the association between CRP levels and cognitive functioning in a sample of Mexican American older adults. A cross-sectional analysis of data from 328 cognitive normal, Mexican American participants from the community-based Health and Aging Brain Among Latino Elders (HABLE) study were performed. Statistical methods included t-test, chi square, multiple linear regression, and logistic regression modeling. Cognitive performance was measured by the Mini Mental State Examination (MMSE), Logical Memory I and II, Digit Span, FAS, and Animal Naming tests. Age, years of education, gender, diagnostic of hypertension, diabetes, and dyslipidemia were entered in the model as covariates. High CRP levels significantly predicted FAS scores (B = −0.135, P = .01), even after adjusting for covariates. Education (B = 0.30, P < .05), and diagnosis of hypertension (B = −0.12, P = .02) were also independent predictors of FAS scores. Participants with higher CRP levels had greater adjusted odds of poorer performance in the FAS test (OR = 1.75, 95% CI = 1.13–2.72, P = .01) when compared to participants with lower CRP levels. This was also true for participants with hypertension (OR = 2.20, 95% CI = 1.34–3.60, P < .05). Higher CRP levels were not associated with MMSE, logical memory, digit span, and animal naming scores. In conclusion, our study showed a clear association between CRP levels and verbal fluency and executive function in a cognitively normal community-dwelling population of Mexican-Americans.
Keywords: C- reactive protein, cognitive functioning, cognitive impairment, executive function, Mexican-American
1. Introduction
C-Reactive Protein (CRP), one of the acute phase inflammatory proteins synthetized in the hepatocytes, has been associated with depression,[1,2] lung,[3] colorectal,[4] and breast cancer,[5] along with other pathologies. CRP is considered an independent risk for future cardiovascular events. The Physicians Health Study (PHS) found that high plasma concentrations of CRP were associated with increased risk of stroke, myocardial infarction, and peripheral vascular disease.[6] Many population-based studies have investigated the association between CRP levels and cognitive function. In 2015, Yang et al, in an extensive systematic review and meta-analysis reported a weak association between CRP levels and global cognitive decline and stated that the association of CRP with specific cognitive domains is not strongly supported.[7] Gorelick has found that the inflammatory pathway of cognitive impairment is corroborated by epidemiological studies and clinical trials while acknowledging that the mechanism involved in vascular cognitive impairment can be explained by a coexistence of different conditions and overlap of risk factors.[8] Many studies support the idea that inflammation is involved in the development of neurodegenerative disorders through mechanisms like activation of microglia, increased levels of proinflammatory cytokines, activation of the complement cascade,[9] and disruption of the blood–brain barrier.[10] According to the US Census Bureau, by the year 2050 the Hispanic population will reach 106 million, and 65% of this population will be of Mexican heritage.[11] The last CDC racial and ethnic estimate of Alzheimer's disease and related dementias in adults 65 years and older projected that by the year 2060 over 3 million Hispanics will have Alzheimer's disease and related dementias.[12] Research has shown that black and Mexican women and children have higher CRP levels than their white counterparts.[13] Additionally, higher levels of acculturation have been associated with increased CRP levels in Hispanics.[14] The present study aims to evaluate the relationship of CRP levels to cognition in a sample of cognitively normal, older Mexican-Americans. We theorized that higher levels of circulating serum CRP would be associated with poorer performance on neuropsychological tests.
2. Methods
2.1. Study design and setting
Data from 329 participants from the Health and Aging Brain Study among Latino Elders (HABLE) were evaluated in a cross-sectional design investigation. In this study, we used a dataset from 2012 to 2015. Participants selected for the final analysis were Mexican-American, over 50 years of age, diagnosed as cognitive normal during a consensus review according to published criteria (clinical dementia rating scale sum of boxes score of 0, and performance on cognitive testing within 1 standard deviation of education and age adjusted norms).[15]
The HABLE study is an ongoing longitudinal study that has been conducted since 2012 at the University of North Texas Health Science Center. The HABLE study uses a community-based participatory research approach and recruitment methodology and has been described in detail elsewhere.[16] In brief, each participant undergoes a comprehensive interview, medical history, neuropsychological testing, and fasting blood draw for clinical labs panel and inflammatory biomarkers. The HABLE study is conducted under the approval of the University of North Texas Health Science Center IRB Board, 2012-083.
2.2. Study population
Between May 2012 and June 2015, a total of 771 participants were admitted to the study. Five hundred fifty nine participants were Mexican-American, and from those, 415 were diagnosed as cognitively normal. Eighty-six participants were excluded from the analysis because of missing CRP levels results. The final sample for analysis consisted of 329 cognitively normal, Mexican-American participants, including 62 male and 267 female, with ages ranging from 50 to 85 years, with available CRP level results and neuropsycological tests scores.
2.3. Predicting variable
Log transformed serum CRP values were used as predictors of performance on neuropsychological tests. CRP was measured in a thawed sample of frozen serum from a fasting blood draw performed during the interview. Blood samples were collected on a 10 mL serum-separating vacutainer tubes. Samples were then allowed to clot at room temperature 30 to 60 min in a vertical position before centrifugation at 2000 rpm for 10 min. Hamilton Robotics Easyblood robot combined with a customized Lab Information Management system (LIMS) was used to process the blood. 250 μL of serum blood samples were aliquoted into 0.5 mL tubes and serum blood samples were stored at −80°C. Serum levels of CRP were measured with sandwich ELISA and electrochemiluminescence with kits from Meso Scale Discovery in a Multiplexing Imager reader.
2.4. Cognitive function
Global cognition functioning was measured with the Mini-Mental State Examination (MMSE). The MMSE is widely used in clinical and research settings, it tests 5 areas of cognitive function and has a maximum score of 30. Scores lower than 24, adjusted by age and education level, may be indicative of cognitive impairment.[17] Logical Memory I and II, from the Wechsler Memory Scale III, were used to assess verbal memory and learning capacity. After a short story is orally presented, the participant is asked to recall as many details as possible (immediate recall). Approximately 20 to 30 min later, a free recall of the story is evaluated (delayed recall).[18] The Wechsler Memory Scale III Digit Span which includes both forward and backward tasks was used as a measure of attention. A sequence of digits is verbally administered at the rate of 1 s. If a series is completed successfully, the number of digits increased. The task ends when the participant makes an error in two trials in a row.[19] Verbal fluency and executive function were evaluated with the FAS test. The FAS, a verbal fluency test, is also considered a measure of executive functions including organization, initiation, and maintenance of effort,[20] and has been used as such in many studies.[21–23] Participants are asked to produce as many words as they can than begin with the letters F, A, and S, with the instruction of not using proper nouns. Sixty seconds are given for each letter, and the overall score is the sum of all the correct words produced. Neuropsychological testing is completed in English or Spanish depending on the participant's preference.
2.5. Covariates
Relevant demographic information, including age, gender, educational level, and medical history was obtained during the interview. Diabetes, hypertension, and dyslipidemia diagnosis was ascertain during consensus review based on participants self-report of medical diagnosis, and/or use of medications (insulin, oral hypoglycemic agents, blood pressure lowering drugs, and cholesterol lowering drugs). In participants with no medical diagnosis and no medication use, standardized procedures based on the American Medical Association guidelines were used for diagnosis (hypertension: average blood pressure >140/90, diabetes: HbA1C >6.4, and dyslipidemia: total cholesterol >200 mg/dL, triglycerides >150 mg/dL).
2.6. Statistical analyses
Due to non-normality, CRP levels were log transformed. Data were analyzed via t-tests for continuous variables, and x2 for categorical variables. For logistic regression, the variables were categorized as follows: CRP levels below or above the 7.9 median (low CRP = 0, high CRP = 1), diagnosis of hypertension (absent = 0, present = 1), diagnosis of diabetes (absent = 0, present = 1), diagnosis of dyslipidemia (absent = 0, present = 1). Test scores were categorized as low and high, depending on if they were below or above the respective median (low = 0, high = 1). Age was categorized as under 65 and over 65 (age under 65 = 0, age over 65 = 1), and education level was categorized as low and high with a cut off value of 12 years of education (low education = 0, high education = 1). First, a linear regression model was used to examine the utility of CRP levels in predicting neuropsychological tests scores, and odds ratios were calculated with logistic regression to predict the odds of having lower test scores when the independent variable were present. We adjusted for age, gender, educational level, and diagnosis of hypertension, diabetes, and dyslipidemia. Cognitive tests scores used for analysis were scale scores stratified by education and age that were generated for Texas-based Mexican-Americans.[24] Significant differences were indicated when the 2-sided P values were less than .05. The data were analyzed by SPSS version 22 for Windows (SPSS Inc., Chicago, IL).
3. Results
3.1. Demographics
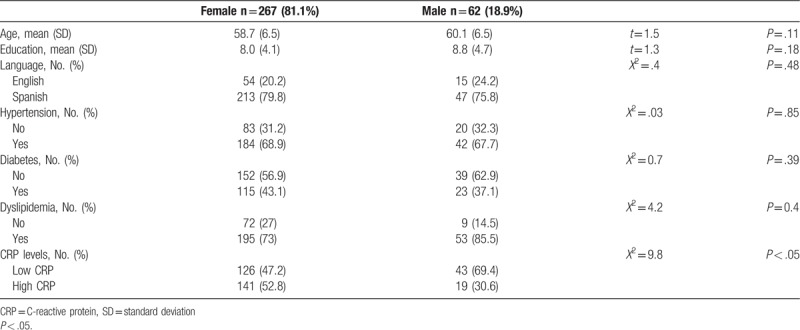
The study population was composed of 329 participants. Table 1 presents the characteristics of the sample. The study sample was primarily female (81.1%) with a mean age of 58.7 for females and 60.1 for males. Eighty percent of the sample was tested in Spanish, and no significant differences were found in years of education between genders (8 for females vs 8.8 for males). More females had higher CRP levels (52.8%) than males (19 out of 62). While no significant gender differences were found in the prevalence of hypertension and diabetes, more males have a diagnosis of dyslipidemia (53 out of 62) than females (73%).
Table 1.
Demographics.
3.2. Relationship of CRP levels and covariates to neuropsychological test scores
Results showed a significant regression equation in participants with high CRP levels only for FAS (F (1–327) = 4.59, P = .03). CRP levels significantly predicted FAS scores (B = −0.135, P = .01). When the covariates were entered in the linear regression analysis, years of education (F (2,325) = 19.16, P < .05), and diagnosis of hypertension (F (2,325) = 4.59, P = .01) regression equations were significant. Age, diagnosis of diabetes and dyslipidemia were not related with FAS scores. Education (B = .30, P < .05), and diagnosis of hypertension (B = −0.12, P = .02) significantly predicted FAS scores.
3.3. Logistic regression analysis of the independent risk factors for test performance
Logistic regression was performed to evaluate the effect of independent risk factors in predicting neuropsychological test scores. We found that subjects with high CRP levels were 1.7 times more likely to score lower in FAS (OR = 1.75, 95% CI = 1.13–2.72, P = .01). High CRP levels did not significantly predict MMSE, logical memory I and II, digit span, and animal naming test scores. When covariates were entered in the model, diagnosis of hypertension and education also predicted FAS scores. Subjects with hypertension were 2.2 times more likely to score lower in FAS (OR = 2.20, 95% CI = 1.34–3.60, P < .05), while subjects with lower levels of education are less likely to have higher scores in FAS (B = 0.43, 95% CI = 0.25–0.71, P < .05).
4. Discussion
This study analyzed the relationship of systemic levels of CRP to measures of global cognition (MMSE), verbal memory (Logical memory I and II), attention (Digit span), verbal fluency and executive function (FAS and animal naming) in a Mexican-American population.
Prior studies that evaluated the association between CRP levels and cognitive function showed contradictory results. Studies were mostly done on non-Hispanic White populations, and only a few studies used a Mexican-Americans cohort[25,26] A few longitudinal[27,28] and cross-sectional studies[29,30] reported that higher CRP levels were associated with elevated risk of cognitive decline. Other studies demonstrated a minor association,[31] while studies with subjects with dementia excluded showed no significant association.[32,33] Discrepancies in the results may be explained by the different cohort characteristics and the variety of neuropsychological tests used. In the present study, we found a relationship between higher CRP levels and FAS measures, but no relationship was found for any of the other cognitive measures. These findings were attenuated but still significant when controlling for hypertension, gender, and education. The diagnoses of diabetes mellitus and dyslipidemia had no effect on the results.
Inflammatory processes have been related to the development of ischemic events associated with atherosclerosis.[34] The relationship between small vessels disease, measured as white matter hyperintensities in MRI scans, with inflammation it is not fully understood, but demyelination, loss of oligodendrocytes, and axonal damage have been suggested as the explanation.[35] Small vessel disease in specific regions of the brain like the frontal cortex can explain the dysfunction in executive functioning.[36] The present study shown that even in cognitively normal individuals, high CRP levels are related to poorer performance in a test of executive functioning, independently of other vascular risk factors like hypertension.
Several limitations are seen in the study. First, the cross-sectional design makes it difficult to interpret data in relation to causation. Longitudinal follow up of this cohort will permit us to analyze if CRP can predict future cognitive impairment. The majority of the sample was females, and since the only Hispanic group involved were Mexican Americans, it would be difficult to generalize the results to other Latino groups and males. CRP levels were only measured once so it is difficult to evaluate the exposure over time. Lastly, the impact of other potential cofounders, related to inflammation and cognition, like depression,[37] obesity,[38] APOE e4 allele,[39] and other chronic inflammatory disorders (e.g., lupus, rheumatoid arthritis) were not analyzed. The present study has a number of strengths that support the value of the findings. First, the sample was community based rather than a clinic-based sample and likely is a better reflection of the CRP levels in the general population. Secondly, our sample was very well characterized as cognitively normal allowing the investigation of the effect of CRP in individuals not yet showing overt cognitive impairment. Additionally, the neuropsychological tests used in this study had been normed on a Mexican-American population[22] and as such are better indicators of actual levels of functioning than the standard norms.
In conclusion, our study demonstrated a clear association between CRP levels and a measure of verbal fluency and executive function in a cognitively normal community-dwelling population of Mexican Americans. This suggests that the early effects of CRP may be on frontal lobe processes. Further studies with a larger sample size, and longitudinal analysis of our population will explain further the relationship between CRP concentrations and cognitive functioning.
Acknowledgments
Research reported in this publication was supported by the National Institute on Aging of the National Institutes of Health under Award Numbers R01AG054073. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. LAJ is also supported by award AARG-16-442652 from the Alzheimer's Association. The research team also thanks the local Fort Worth community and participants of the Health & Aging Brain Study.
Author contributions
Conceptualization: Raul Vintimilla, James Hall, Leigh Johnson, Sid O’Bryant.
Formal analysis: Raul Vintimilla, James Hall.
Funding acquisition: Sid O’Bryant.
Investigation: Raul Vintimilla, James Hall, Leigh Johnson, Sid O’Bryant.
Methodology: Raul Vintimilla, James Hall, Leigh Johnson, Sid O’Bryant.
Project administration: Sid O’Bryant.
Resources: Sid O’Bryant.
Writing – original draft: Raul Vintimilla.
Writing – review & editing: James Hall, Leigh Johnson, Sid O’Bryant.
Footnotes
Abbreviations: 95% CI = 95% confidence interval, CRP = C-reactive protein, HABLE = Health and Aging Brain among Latino Elders, MMSE = mini mental state examination, OR = odds ratio, PHS = Physicians Health Study.
Conflicts of interest: The authors have no conflicts of interest to declare.
References
- [1].Kop WJ, Gottdiener JS, Tangen CM, et al. Inflammation and coagulation factors in persons >65 years of age with symptoms of depression but without evidence of myocardial ischemia. Am J Cardiol 2002;89:419–24. [DOI] [PubMed] [Google Scholar]
- [2].Penninx BW, Kritchevsky SB, Yaffe K, et al. Inflammatory markers and depressed mood in older persons: results from the Health, Aging and Body Composition study. Biol Psychiatry 2003;54:566–72. [DOI] [PubMed] [Google Scholar]
- [3].Siemes C, Visser L, Jan-Willen W, et al. C-reactive protein levels, variation in the C-reactive protein gene, and cancer risk: the Rotterdam Study. J Clin Oncol 2006;24:5216–22. [DOI] [PubMed] [Google Scholar]
- [4].Gunter MJ, Stolzenberg-Solomon R, Cross AJ, et al. A Prospective Study of serum C-reactive protein and colorectal cancer risk in men. Cancer Res 2006;66:2483–7. [DOI] [PubMed] [Google Scholar]
- [5].Guo L, Liu S, Zhang S, et al. C-reactive protein and risk of breast cancer: a systematic review and meta-analysis. Sci Rep 2015;5:10508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Ridker PM, Cushman M, Stampfer MJ, et al. Inflammation, aspirin, and the risk of cardiovascular disease in apparently healthy men. N Engl J Med 1997;336:973–9. [DOI] [PubMed] [Google Scholar]
- [7].Yang J, Fan C, Pan L, et al. C-reactive protein plays a marginal role in cognitive decline: a systematic review and meta-analysis. Int J Psychiatry 2015;30:156–65. [DOI] [PubMed] [Google Scholar]
- [8].Gorelick PB. Role of inflammation in cognitive impairment: results of observational epidemiological studies and clinical trials. Ann N Y Acad Sci 2017;1207:155–62. [DOI] [PubMed] [Google Scholar]
- [9].Russo I, Barlatti S, Bosetti F. Effects of neuroinflammation on the regenerative capacity of brain stem cells. J Neurochem 2011;116:947–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Kuhlmann RW, Librizzi D, Clshen T, et al. Mechanisms of C-reactive protein-induced blood-brain barrier disruption. Stroke 2009;40:1458–66. [DOI] [PubMed] [Google Scholar]
- [11].www.census.gov Accessed May 10, 108. [Google Scholar]
- [12].Maththews KA, Xu W, Gaglioti AH, et al. Racial and ethnic estimates of Alzheimer's disease and related dementias in the United States (2015–2060) in adults aged ≥65 years. Alzheimers Dement 2018;1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Albert MA, Ridker PM. C-reactive protein as a risk predictor do race/ethnicity and gender make a difference? Circulation 2006;114:e67–74. [DOI] [PubMed] [Google Scholar]
- [14].Daviglus LM, Pirzada A, Talavera GA. Cardiovascular disease risk factors in the Hispanic/Latino population: lessons from the Hispanic Community Health Study/Study of Latinos. Prog Cardiovas Dis 2014;3:230–6. [DOI] [PubMed] [Google Scholar]
- [15].Ivnik R, Malec JF, Smith GE, et al. Mayo's Older Americans normative studies: WAIS-R norms for age 56 to 97. Clin Neuropsychologist 1992;6:1–30. [Google Scholar]
- [16].Johnson LA, Gamboa A, Vintimilla R, et al. Comorbid depression and diabetes as a risk for mild cognitive impairment and Alzheimer's disease in elderly Mexican Americans. J Alzheimers Dis 2015;129–36. [DOI] [PubMed] [Google Scholar]
- [17].Pezzotti P, Scalmanal S, Mastromattei A, et al. The accuracy of the MMSE in detecting cognitive impairment when administered by general practitioners: a prospective observational study. BMC Fam Pract 2008;9:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Chapman RK, Bing-Canar H, Alosco ML, et al. Mini Mental State Examination and Logical Memory scores for entry into Alzheimer's disease trials. Alzheimers Res Ther 2016;8:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Woods DL, Kishiyama M, Yund EW, et al. Improving digit span assessment of short-term verbal memory. J Clin Exp Neuropsychol 2011;33:101–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Barry D, Bates ME, Labouvie E. FAS and CFL forms of verbal fluency differ in difficulty: a meta-analytic study. Appl Neuropsychol 2008;15:97–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Morelly LN, Cachioni M, Lopes A, et al. Verbal fluency in elderly with and without hypertension and diabetes from the FIBRA study in Emelino Matarazzo. Dement Neuropsychol 2017;11:413–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Weakley A, Schmitter-Edgecombe M, Anderson J. Analysis of verbal fluency ability in Amnestic and Non-Amnestic Mild Cognitive Impairment. Archi Clin Neuropsychol 2013;28:721–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Fitz Patrick S, Gilbert SJ, Serpell LE. Systematic review: are overweight and obese individuals impaired on behavioral tasks of executive functioning? Neuropsychol Rev 2013;23:138–56. [DOI] [PubMed] [Google Scholar]
- [24].O’Bryant SE, Edwards M, Johnson L, et al. Texas Mexican American adult normative studies: normative data for commonly used clinical neuropsychological measures for English- and Spanish-speakers. Dev Neuropsychol 2018;43:1–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Noble JM, Manly JJ, Schupf N, et al. Association of C-reactive protein to cognitive impairment. Arch Neurol 2010;67:87–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].O’Bryant SE, Johson L, Edwards M, et al. The link between C-reactive protein and Alzheimer's disease among Mexican Americans. J Alzheimers Dis 2013;34:701–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Laurin D, Curve JD, Masaki KH, et al. Midlife C-reactive protein and risk of cognitive decline: a 31-year follow up. Neurobiol Aging 2009;30:1724–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Gimeno D, Marmot MG, Singh-Manoux A. Inflammatory markers and cognitive function in middle-aged adults: the Whitehall II study. Pscychoneuroendocrinology 2008;33:1322–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Watanabe Y, Kitamura K, Nakamura K, et al. Elevated C-reactive protein is associated with cognitive decline in outpatients of a general hospital: the Project in Sado for Total Health (PROST). Dement Geriatr Cogn Disor Extra 2016;6:10–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Roberts RO, Geda YE, Knopman DS, et al. Association of C-reactive protein with mild cognitive impairment. Alzheimers Dement 2009;5:398–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Schram MT, Euser SM, de Craen AJ, et al. Systemic markers of inflammation and cognitive decline in old age. J Am Geriatr Soc 2007;55:708–16. [DOI] [PubMed] [Google Scholar]
- [32].Alley DE, Crimmins EM, Karlamangla A, et al. Inflammation and rate of cognitive change in high-functioning older adults. J Gerontol A Biol Sci Med Sci 2008;63:50–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Weuve J, Ridker PM, Cook NR, et al. Epidemiology 2006;17:183–9. [DOI] [PubMed] [Google Scholar]
- [34].van Dijk EJ, Prins ND, Veermer SE, et al. C-reactive protein and small–vessel disease. The Rotterdam Scan Study. Circulation 2005;112:900–5. [DOI] [PubMed] [Google Scholar]
- [35].Shi Y, Wardlaw, Joanna Update on cerebral small vessel disease: a dynamic whole-brain disease. Stroke Vasc Neurol 2016;1:e000035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Kurz AF. What is vascular dementia? Int J Clin Pract Suppl 2001;120:5–8. [PubMed] [Google Scholar]
- [37].Gimeno D, Kivimaki M, Brunner EJ, et al. Associations of C-reactive protein and interleukin-6 with cognitive symptoms of depression: 12 year follow-up of the Whitehall II study. Pscychol Med 2009;39:413–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Yaffe K, Kanaya A, Lindquist MS, et al. The metabolic syndrome, inflammation, and risk of cognitive decline. JAMA 2004;292:2237–42. [DOI] [PubMed] [Google Scholar]
- [39].Hann MN, Aiello AE, West NA, et al. C-reactive protein and rate of dementia in carriers and non carriers of Apolipoprotein APOE4 genotype. Neurobil Aging 2008;29:1774–82. [DOI] [PMC free article] [PubMed] [Google Scholar]


