Abstract
We present our seven-year experience of using moderate deep inspiration breath-hold (mDIBH) with an active breathing control (ABC) device for patients with early-stage breast cancer and dosimetric comparison to evaluate the benefit of mDIBH on the heart, lung, and liver.
We retrospectively reviewed all patients with newly diagnosed breast cancer and having clinical stage Tis, I, or II disease treated between November 2010 and October 2017. Among the 369 patients included in this study, 107 patients were treated with mDIBH and 262 patients were treated with free breathing (FB). Dosimetric analysis was performed to compare dose distribution in the heart, lung, and liver between the two treatment groups. The chi-square test was used to compare the distribution of stage and tumor site between the two groups. The independent samples t-test was used to compare the remaining parameters between the two groups.
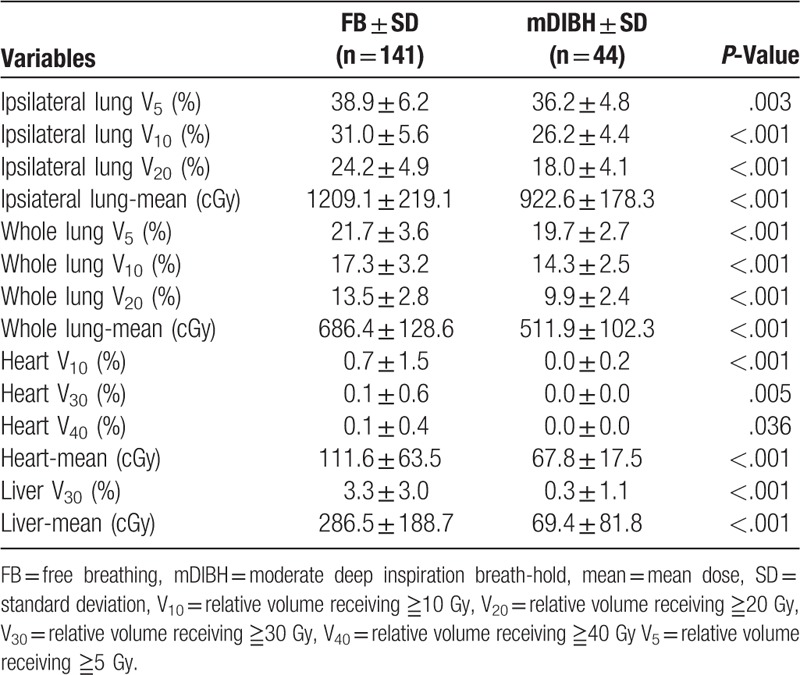
For all 369 patients, there was a significantly lower ipsilateral lung V5 (relative volume receiving ≧5 Gy), ipsilateral lung V10, ipsilateral lung V20, mean ipsilateral lung dose, whole lung V5, whole lung V10, whole lung V20, mean whole lung dose, heart V10, heart V30, heart V40, and mean heart dose in the mDIBH group. For 184 patients with a left-sided breast tumor, significantly lower ipsilateral lung V5, ipsilateral lung V10, ipsilateral lung V20, mean ipsilateral lung dose, whole lung V10, whole lung V20, mean whole lung dose, heart V10, heart V30, heart V40, and mean heart dose were observed in the mDIBH group. For 185 patients with a right-sided breast tumor, significantly lower ipsilateral lung V5, ipsilateral lung V10, ipsilateral lung V20, mean ipsilateral lung dose, whole lung V5, whole lung V10, whole lung V20, mean whole lung dose, heart V10, heart V30, heart V40, mean heart dose, liver V30, and mean liver dose were observed in the mDIBH group.
For early-stage breast cancer patients, mDIBH reduces not only the heart dose but also the lung and liver doses. The routine integration of mDIBH using an ABC device may decrease radiation-induced toxicity in the heart, lung, and liver.
Keywords: active breathing control, early stage breast cancer, moderate deep inspiration breath-hold
1. Introduction
Breast-conserving therapy has become the major treatment modality for early-stage breast cancer, of which radiotherapy is an important component. Several studies have demonstrated a lower risk of recurrence by the administration of adjuvant radiotherapy.[1,2] Whole breast radiation reduces the risk of local recurrence and has shown to have a beneficial effect on survival.[3,4] For patients with breast irradiation, a significant reduction in the heart and lung doses using deep inspiration breath-hold with active breathing control (ABC) has been established.[5–13] However, the breath hold technique has not been routinely implemented in many breast cancer treatment centers because of concerns about the increase in the required resources and workload. We present our experience over a period of 7 years of using moderate deep inspiration breath-hold (mDIBH) using an ABC device for patients with early-stage breast cancer. Patients with early-stage breast cancer were retrospectively reviewed in order to compare the radiation doses to the heart, lung, and liver.
2. Materials and methods
2.1. Patient selection
In our previous experience, the quality of the verification images of patients with advanced-stage breast cancer before treatment with mDIBH was not very good. Electronic portal imaging device (EPID) was placed in the exit megavoltage beam to produce the image. The images were captured and displayed on a video screen. These images could be compared with the simulation films to determine the placement differences. This was our verification technique used in both locally advanced disease and the early disease. The image quality of megavoltage port images is poorer than the quality for companion kV-equivalent digitally reconstructed radiographs because of poor subject contrast caused by the dominance of the Compton effect. The treatment field included partial clavicle and humerus in locally advanced disease. The quality of lateral verification image was worse in locally advanced disease than in the early disease due to interference of clavicle and humerus. Therefore, we favored using mDIBH for patients with early-stage breast cancer due to more confidence in verification. However, due to the limited resources, not all early-stage patients received mDIBH. We recommended mDIBH technique to all left-sided breast cancer patients. But some left-sided breast cancer patient did not receive mDIBH technique due to some reasons, including limited workload of our institution, patient's insurance coverage, and patient's preference. Some left-sided breast cancer patients failed to receive mDIBH technique due to hearing impairment. The mDIBH technique was also performed for right-sided breast cancer patients if they were eager to have more precise treatment. We retrospectively reviewed all newly diagnosed breast cancer patients diagnosed with clinical stage Tis, I, or II disease and who were treated with radiotherapy between November 2010 and October 2017. The study was approved by the Ethics Committee of Chi-Mei Medical Center, and was carried out in accordance with the Helsinki declaration and its later amendments or comparable ethical standards. All persons gave their informed consent before their inclusion in the study. We reviewed the records and plans of the 369 patients included in this study to obtain demographic data, staging, planning target volume for evaluation (PTVeval) V95% (relative volume receiving ≧95% of prescribed dose), clinical target volume for evaluation (CTVeval) V95%, volume of the normal organs, and relative dose-volume histograms (DVHs). Of the 369 patients, 107 patients were treated with mDIBH and 262 patients were treated with free breathing (FB). Subsequently, we compared the dose difference between the two groups in order to understand the benefit of mDIBH.
2.2. mDIBH technique
Patients had to demonstrate a comprehension of the rationale of this treatment so that an optimal level of compliance could be attained. They underwent a training session with the ABC apparatus to determine the breath-hold threshold level and breath-hold time. They were then immobilized on a homemade T-board supporting the thorax, the shoulders, and the elbows, with both arms raised above the head and connected to the ABC device. The ABC device is commercially available from the Elekta Oncology Systems. It consists of a digital spirometer to record the patients’ real-time breathing traces and a balloon valve that is triggered to automatically inflate when the patients inspire to their preset mDIBH level. This allows for a predictable and consistent level of chest wall expansion with each mDIBH. A nose clip is used to prevent leakage and to allow for an accurate measurement of the inspiratory volume. Their maximal inspiratory capacity was recorded using the ABC spirometry software. A comfortable level of breath-hold was then determined, which would be used throughout the treatment course. This level was generally set at approximately 75% maximal inspiratory capacity and was termed mDIBH. Patients who could comfortably maintain this level of breath-hold for 15 to 25 s were deemed suitable for this treatment. Patients underwent a planning CT scan in mDIBH while being connected to the ABC device. In the treatment room, all patients followed our radiotherapist's audio orders to take a deep breath and to suspend their breathing motion. Verification images were obtained before treatment. The patient was irradiated when the ABC monitor showed that a breath-hold was in progress. ABC was not used for the tumor bed boost. It took us additional 30 min to perform every patient's breathing training before simulation. It also took us additional 10 min to perform every treatment with mDIBH technique. An additional radiotherapist was required to control the ABC device. During 25 fractions of treatment, we needed additional 280 min and additional 25 radiotherapists to treat one patient. Obviously the mDIBH technique increased our workload. Therefore, before the routine integration of mDIBH using an ABC device, a careful estimation of the available resources was essential.
2.3. Treatment planning
The delineation of CTV in all 369 patients was based on the consensus of Radiation Therapy Oncology Group (RTOG). The PTV was 2 cm on the anterior and lateral side and 0.7 cm on the other side. PTV was used for field design of conventional tangential-field plan. We used PTVeval (PTV for evaluation) to evaluate target coverage. We tried to keep contralateral breast lower than 3 Gy and skin dose lower than 70% of prescribed dose as possible as we could. The prescribed dose was 50 Gy in 25 fractions to the whole breast and 10 to 16 Gy in a 5- to 8-fraction boost to the tumor bed. Hybrid intensity-modulated radiotherapy (IMRT) was performed for the treatment planning, and an electron beam in the energy range of 6 to 9 MeV was prescribed to the 90% isodose curve for the tumor bed boost. The hybrid IMRT plans were generated using Pinnacle treatment planning system. The hybrid IMRT consisted of a conventional tangential-field plan and a tangential-field IMRT plan. The two plans were hybrid using different weightings of 80% and 20%, respectively. The contribution of the low weighting tangential-field IMRT plan was to increase the dose homogeneity of the hybrid IMRT plan. The maximum number of segments was set to 20 and the minimum segment MUs was set to 4 to effectively perform the tangential-field IMRT plan.
2.4. Statistical analysis
All planning and dosimetric evaluations were performed on the Pinnacle treatment planning system (Phillips Healthcare, Andover, MA). The calculated DVH was compared between the FB and mDIBH groups. The chi-square test was used to compare the distribution of stage and tumor site between the two groups. The independent samples t-test was used to compare the remaining parameters between the two groups. Analysis was performed using SPSS v.22.
3. Results
Three hundred and sixty-nine female patients with early-stage breast cancer were treated in our institution between November 2010 and October 2017. Of these patients, 107 patients were treated with mDIBH, and 262 patients were treated without mDIBH. All patients received partial mastectomy followed by whole breast irradiation of 50 Gy and an additional 10 to 16 Gy to the tumor bed. In the mDIBH group, the average threshold was 1.2 L and the average duration of breath hold was 19.5 s. There was significant difference in the distribution of stage, tumor site, and age between the FB and mDIBH groups (Table 1). There was a significant difference in the ipsilateral lung volume, whole lung volume, and liver volume between the FB and mDIBH groups, but no difference in the PTVeval V95%, CTVeval V95%, and the volume of CTV and heart (Table 2). All 369 patients presented with a significantly lower ipsilateral lung V5, ipsilateral lung V10, ipsilateral lung V20, mean ipsilateral lung dose, whole lung V5, whole lung V10, whole lung V20, mean whole lung dose, heart V10, heart V30, heart V40, and mean heart dose in the mDIBH group (Table 3). For 184 patients with a left-sided breast tumor, significantly lower ipsilateral lung V5, ipsilateral lung V10, ipsilateral lung V20, mean ipsilateral lung dose, whole lung V10, whole lung V20, mean whole lung dose, heart V10, heart V30, heart V40, and mean heart dose were observed in the mDIBH group (Table 4). For 185 patients with a right-sided breast tumor, significantly lower ipsilateral lung V5, ipsilateral lung V10, ipsilateral lung V20, mean ipsilateral lung dose, whole lung V5, whole lung V10, whole lung V20, mean whole lung dose, heart V10, heart V30, heart V40, mean heart dose, liver V30, and mean liver dose were observed in the mDIBH group (Table 5).
Table 1.
Distribution of stage, site, and age.
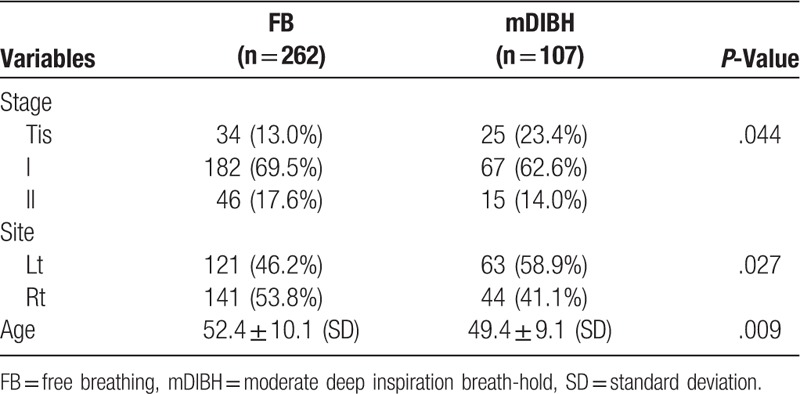
Table 2.
Comparison of volume and coverage.
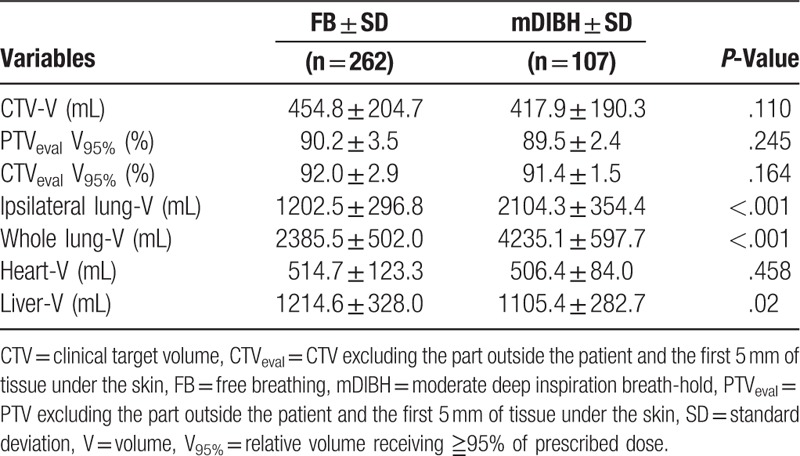
Table 3.
Dosimetric comparison of all patients.
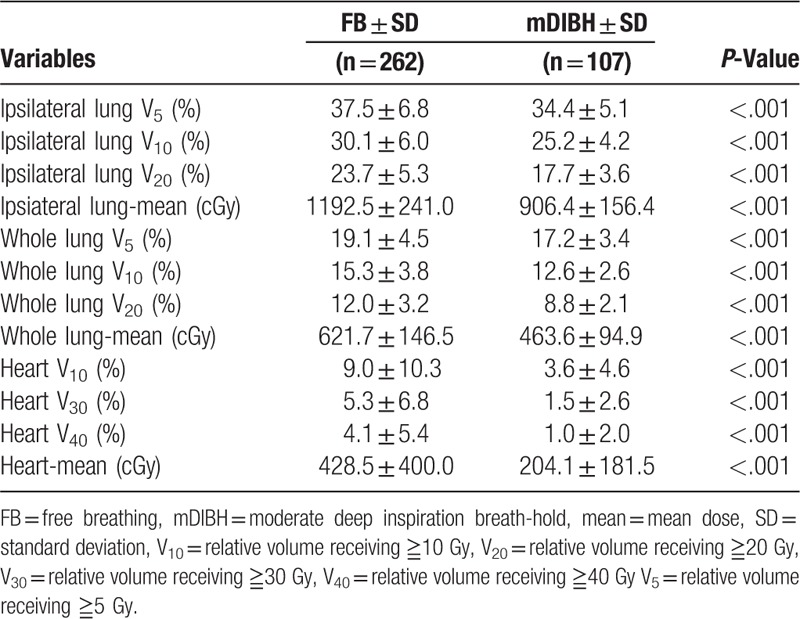
Table 4.
Dosimetric comparison of patients with left side breast tumor.
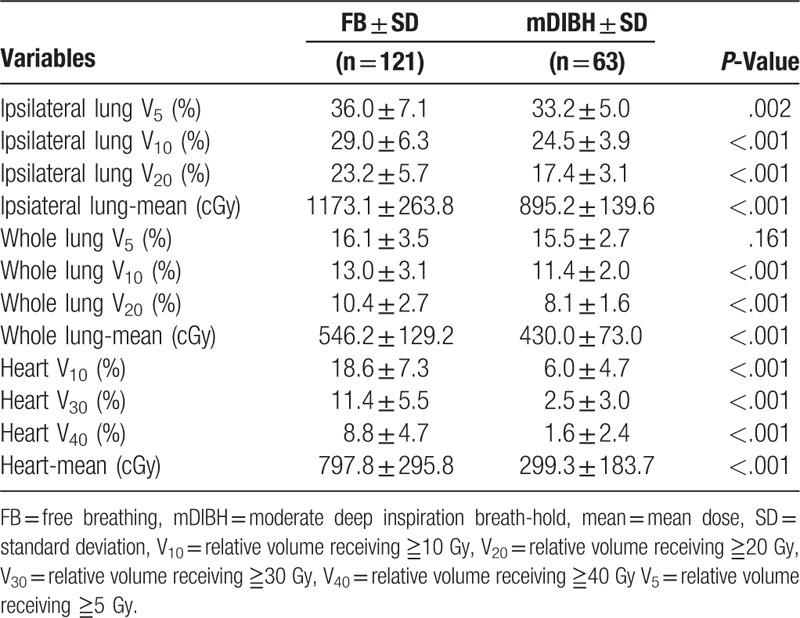
Table 5.
Dosimetric comparison of patients with right side breast tumor.
4. Discussion
A recent analysis of 42,000 women treated in 78 randomized trials using radiotherapy for breast cancer showed small but significant reductions in breast cancer mortality within the first 10 years after treatment, primarily because of excess mortality due to heart disease and lung cancer.[4] It has long been speculated that one of the primary factors responsible for the detrimental effect of radiotherapy on survival was cardiac toxicity related to radiotherapy exposure.[10] An additional concern is that most breast cancer patients are now also receiving systemic cardiotoxic therapy. Therefore, the radiation dose to the heart should be as low as possible. Vincent et al[14] reported that a reduction in the percentage of the heart receiving 30 Gy can be achieved in patients with left-sided breast cancer using an ABC device. In our study, the use of mDIBH in left-sided breast cancer patients could reduce the heart V30 by 78.1%, the heart V40 by 81.8%, and the mean heart dose by 62.5%, when compared with free-breathing techniques. These observations were also consistent with those from previous studies that used deep inspiration breath-hold strategies.[8,11,12,15–20]
We also showed that the mDIBH technique significantly decreased the dose to the whole lung and the ipsilateral lung. This seems counterintuitive, as there would be more lung volume within the tangential beam when the heart moves out of the treatment field during mDIBH. However, Zurl et al[21] reported that the use of deep inspiration breath-hold technique in breast cancer patients can reduce the mean lung dose by 15% and the lung V20 by 17%, when compared with FB techniques. These results were comparable with the reductions seen in our present study. In our study, the use of mDIBH in all breast cancer patients reduced the ipsilateral lung V10 by 16.3%, the ipsilateral lung V20 by 25.3%, and the mean ipsilateral lung dose by 24.0%. Additionally, a similar result was obtained with the total lung dose. It is believed that the deep inspiration breath-hold technique reduces the ipsilateral or total lung dose through inflation, so that very little tissue remains in the irradiated region.
Several studies have reported that the mDIBH technique using the ABC device for left-sided breast cancer radiotherapy can displace the heart from the breast radiation field, thus significantly reducing the dose to the heart and the coronary artery.[22–24] Our study showed that mDIBH can significantly reduce the mean heart dose, even for right-sided breast cancer patients, although the clinical benefit is not well understood.
Conway et al[9] reported that the use of deep inspiration breath-hold technique in breast cancer patients can reduce liver volume receiving 50% of the prescribed dose. In our study, the mDIBH group showed significantly lower liver V30 and mean liver dose.
To our knowledge, this was the first study to retrospectively compare the dosimetric parameters between the FB and mDIBH groups in all early-stage breast cancer patients of a single institution. Following analysis, the two groups were observed to be different in their distribution of stage, tumor site, and age. The mDIBH group showed higher ratio of Tis stage, left side, and younger age. Moreover, there was no difference in the CTV volume and heart volume; the difference observed was in the lung volume as a result of lung expansion.
Our study was a retrospective study that had some limitations. First, different radiation oncologists delineated the tumor contours and some personal variation would exist. Second, the patients received mDIBH based on their personal choice or the oncologist's advice, thereby leading to possible selection bias. Third, we only investigated early-stage breast cancer patients; hence, the effect of mDIBH on advanced-stage breast cancer patients is unknown.
5. Conclusions
For early-stage breast cancer patients, the mDIBH technique not only reduces the heart dose but also reduces the lung and liver doses. Right-sided breast cancer patients can also acquire benefit by using the mDIBH technique. The routine integration of mDIBH using an ABC device may decrease toxicity in the heart, lung, and liver. However, this technique will increase the workload to provide breathing training, higher treatment time, and the requirement of an additional radiotherapist to control the ABC device. Therefore, before the routine integration of mDIBH using an ABC device, a careful estimation of the available resources is essential. Also, long-term follow-up is needed to determine the clinical outcomes associated with decreased radiation doses to the heart, lung, and liver.
Author contributions
Conceptualization: Chia-Hui Lin.
Data curation: Chia-Hui Lin.
Formal analysis: Chung-Han Ho.
Investigation: Chia-Hui Lin.
Methodology: Chung-Han Ho.
Resources: Chia-Hui Lin.
Software: Chung-Han Ho.
Supervision: Li-Ching Lin.
Validation: Jenny Que.
Writing – original draft: Chia-Hui Lin.
Writing – review & editing: Chia-Hui Lin.
Footnotes
Abbreviations: ABC = active breathing control, CTV = clinical target volume, DVHs = dose-volume histograms, FB = free breathing, mDIBH = moderate deep inspiration breath-hold, PTV = planning target volume, RTOG = Radiation Therapy Oncology Group, Vnumber = relative volume receiving ≧ number Gy.
The authors report no conflicts of interest.
References
- [1].Fisher B, Anderson S, Bryant J, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med 2002;347:1233–41. [DOI] [PubMed] [Google Scholar]
- [2].van Dongen JA, Voogd AC, Fentiman IS, et al. Long-term results of a randomized trial comparing breast-conserving therapy with mastectomy: European Organization for Research and Treatment of Cancer 10801 trial. J Natl Cancer Inst 2000;92:1143–50. [DOI] [PubMed] [Google Scholar]
- [3].Darby S, McGale P, et al. Early Breast Cancer Trialists’ Collaborative Group (EBCTCG). Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10,801 women in 17 randomised trials. Lancet 2011;378:1707–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Clarke M, Collins R, Darby S, et al. Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials. Lancet 2005;366:2087–106. [DOI] [PubMed] [Google Scholar]
- [5].Dumane VA, Saksornchai K, Zhou Y, et al. Reduction in low-dose to normal tissue with the addition of deep inspiration breath hold (DIBH) to volumetric modulated arc therapy (VMAT) in breast cancer patients with implant reconstruction receiving regional nodal irradiation. Radiat Oncol 2018;13:187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Walston S, Quick AM, Kuhn K, et al. Dosimetric considerations in respiratory-gated deep inspiration breath-hold for left breast irradiation. Technol Cancer Res Treat 2017;16:22–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].van Haaren P, Claassen-Janssen F, van de Sande I, et al. Heart position variability during voluntary moderate deep inspiration breath-hold radiotherapy for breast cancer determined by repeat CBCT scans. Phys Med 2017;40:88–94. [DOI] [PubMed] [Google Scholar]
- [8].Mohamad O, Shiao J, Zhao B, et al. Deep inspiration breathhold for left-sided breast cancer patients with unfavorable cardiac anatomy requiring internal mammary nodal irradiation. Pract Radiat Oncol 2017;7:e361–7. [DOI] [PubMed] [Google Scholar]
- [9].Conway JL, Conroy L, Harper L, et al. Deep inspiration breath-hold produces a clinically meaningful reduction in ipsilateral lung dose during locoregional radiation therapy for some women with right-sided breast cancer. Pract Radiat Oncol 2017;7:147–53. [DOI] [PubMed] [Google Scholar]
- [10].Boero IJ, Paravati AJ, Triplett DP, et al. Modern radiation therapy and cardiac outcomes in breast cancer. Int J Radiat Oncol Biol Phys 2016;94:700–8. [DOI] [PubMed] [Google Scholar]
- [11].Eldredge-Hindy H, Lockamy V, Crawford A, et al. Active Breathing Coordinator reduces radiation dose to the heart and preserves local control in patients with left breast cancer: report of a prospective trial. Pract Radiat Oncol 2015;5:4–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Chi F, Wu S, Zhou J, et al. Dosimetric comparison of moderate deep inspiration breath-hold and free-breathing intensity-modulated radiotherapy for left-sided breast cancer. Cancer Radiother 2015;19:180–6. [DOI] [PubMed] [Google Scholar]
- [13].Remouchamps VM, Vicini FA, Sharpe MB, et al. Significant reductions in heart and lung doses using deep inspiration breath hold with active breathing control and intensity-modulated radiation therapy for patients treated with locoregional breast irradiation. Int J Radiat Oncol Biol Phys 2003;55:392–406. [DOI] [PubMed] [Google Scholar]
- [14].Remouchamps VM, Letts N, Vicini FA, et al. Initial clinical experience with moderate deep-inspiration breath hold using an active breathing control device in the treatment of patients with left-sided breast cancer using external beam radiation therapy. Int J Radiat Oncol Biol Phys 2003;56:704–15. [DOI] [PubMed] [Google Scholar]
- [15].Comsa D, Barnett E, Le K, et al. Introduction of moderate deep inspiration breath hold for radiation therapy of left breast: Initial experience of a regional cancer center. Pract Radiat Oncol 2014;4:298–305. [DOI] [PubMed] [Google Scholar]
- [16].Swanson T, Grills IS, Ye H, et al. Six-year experience routinely using moderate deep inspiration breath-hold for the reduction of cardiac dose in left-sided breast irradiation for patients with early-stage or locally advanced breast cancer. Am J Clin Oncol 2013;36:24–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Nissen HD, Appelt AL. Improved heart, lung and target dose with deep inspiration breath hold in a large clinical series of breast cancer patients. Radiother Oncol 2013;106:28–32. [DOI] [PubMed] [Google Scholar]
- [18].Korreman SS, Pedersen AN, Josipović M, et al. Cardiac and pulmonary complication probabilities for breast cancer patients after routine end-inspiration gated radiotherapy. Radiother Oncol 2006;80:257–62. [DOI] [PubMed] [Google Scholar]
- [19].Korreman SS, Pedersen AN, Aarup LR, et al. Reduction of cardiac and pulmonary complication probabilities after breathing adapted radiotherapy for breast cancer. Int J Radiat Oncol Biol Phys 2006;65:1375–80. [DOI] [PubMed] [Google Scholar]
- [20].Pedersen AN, Korreman S, Nyström H, et al. Breathing adapted radiotherapy of breast cancer: reduction of cardiac and pulmonary doses using voluntary inspiration breath-hold. Radiother Oncol 2004;72:53–60. [DOI] [PubMed] [Google Scholar]
- [21].Zurl B, Stranzl H, Winkler P, et al. Quantitative assessment of irradiated lung volume and lung mass in breast cancer patients treated with tangential fields in combination with Deep Inspiration Breath Hold (DIBH). Strahlenther Onkol 2010;186:157–62. [DOI] [PubMed] [Google Scholar]
- [22].Moran JM, Ben-David MA, Marsh RB, et al. Accelerated partial breast irradiation: what is dosimetric effect of advanced technology approaches? Int J Radiat Oncol Biol Phys 2009;75:294–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Krauss DJ, Kestin LL, Raff G, et al. MRI-based volumetric assessment of cardiac anatomy and dose reduction via active breathing control during irradiation for left-sided breast cancer. Int J Radiat Oncol Biol Phys 2005;61:1243–50. [DOI] [PubMed] [Google Scholar]
- [24].Sixel KE, Aznar MC, Ung YC. Deep inspiration breath hold to reduce irradiated heart volume in breast cancer patients. Int J Radiat Oncol Biol Phys 2001;49:199–204. [DOI] [PubMed] [Google Scholar]


