Abstract
This study was designed to investigate the factors affecting the in-hospital delay of intravenous thrombolysis (IVT) for acute ischemic stroke (AIS).
Two hundred and forty-eight consecutive AIS patients treated with intravenous administration of alteplase in Gansu Provincial Hospital from December 2014 to August 2018 were enrolled retrospectively in this study. According to door-to-needle (DTN) time, the patients were divided into either a delay group (DTN time > 60 minutes; n = 184) or a non-delay group (DTN time ≤60 minutes; n = 64). The baseline data, laboratory tests, onset-to-door (OTD) time, door-to-accepting time (DTA), door-to-imaging time (DTI), and decision-making time in both groups were recorded. Multivariate logistic analysis was performed to analyze the data.
There were significant differences in previous history of cerebral ischemic attack, emergency system admission, education degree of decision makers, annual income, admission National Institutes of Health Stroke Scale (NIHSS), OTD time, DTA time, decision-making time between the 2 groups (all P < .05). Other baseline data and clinical features showed no significant difference between 2 groups (P > .05). Multivariate logistic regression analysis revealed that the risk of in-hospital delay was lower for the higher NIHSS score (OR = 0.775, 95% CI: 0.644-0.933, P = .007), the longer OTD time (OR = 0.963, 95% CI: 0.937-0.991, P = .010), the shorter decision-making time (OR = 1.224, 95% CI: 1.004-1.492, P = .045).
This study suggested that NIHSS score, OTD time and decision-making time are the independent factors affecting the in-hospital delay of IVT for AIS.
Keywords: acute ischemic stroke, alteplase, in-hospital delay, intravenous thrombolysis
1. Introduction
Acute ischemic stroke (AIS) is the most common stroke type, accounting for 80% of the total numbers of stroke and the primary cause of adult disability.[1,2] Intravenous thrombolysis (IVT) is a proven effective therapy for patients suffering from AIS.[3] Studies showed that the time from onset to initiation of therapy is an important factor for good clinical outcome of IVT for AIS patients.[4,5] Recombinant tissue-type plasminogen activator (rt-PA) has a strong thrombolytic effect. Time window (3–4.5 hours) is the only prerequisite for the thrombolysis with intravenous rt-PA.[6,7] The effectiveness of rt-PA treatment decreases as time from onset of AIS to use of rt-PA increases. It is the most effective to use rt-PA within 1.5 hours of onset of AIS and remains effective within 4.5 hours.[8] The American Heart Association (AHA)/American Stroke Association (ASA) guidelines recommend that DTN time should be ≤60 minutes.[9] Nevertheless, the goal of a door-to-IVT time within 60 minutes was achieved in only 40% of patients treated with IVT in America.[10] Chinese National Stroke Registry Study showed that the average door-to-needle (DTN) time of AIS patients was 116 minutes.[11] In China, less than 22% of all AIS patients arrived at hospital within 3 hours of onset of AIS, of which only 1.6% could be treated with IVT.[9] In-hospital delay contributed substantially to the barriers of the availability to IVT, which could even jeopardize the population benefit from extending the therapeutic time window of IVT.[12] The purpose of this study is to determine the factors affecting in-hospital delay and to share our experience to decrease in-hospital delay.
2. Materials and methods
2.1. Participants’ enrollment and groups
Consecutive 248 AIS patients treated with rt-PA in Department of Cerebrovascular Disease Center of Gansu Provincial Hospital from January 2014 to August 2018 were included in this analysis. According to DTN time, they were divided into either a delay group (DTN time > 60 minutes; n = 184) or a non-delay group (DTN time ≤ 60 minutes; n = 64). AIS patients or their family members should complete an in-person interview. The interview contained a detailed questionnaire regarding stroke risk factors and demographics. Emergency system admission, National Institutes of Health Stroke Scale (NIHSS), systolic blood pressure, serum glucose, occlusion site, CT manifestations and typing of responsible vessels, DTN, onset-to-door time (OTD), hospital arrival time, door-to-accepting time (DTA), door-to-imaging time (DTI), decision-making time were collected from the electronic medical record system.
2.2. Standard protocol approvals
This study was approved by the Ethical Committee of Gansu Provincial Hospital. Written informed consents were obtained from all included patients or their family members.
2.3. Performance of IVT
IVT using rt-PA (Boehringer Ingelheim) was performed as method described previously.[13] The doses of rt-PA were 0.5 to 0.9 mg/kg with the maximum dose of less than or equal to 90 mg. The administration rate was that 10% of rt-PA was injected within 1 minute and the remaining 90% was given intravenously within 1 hour. There was no contraindication for thrombolytic therapy. Admission NIHSS scores were evaluated and recorded by specialist senior physicians
2.4. Statistical analysis
All calculations were performed using SPSS 21.0 software, with 2 tailed P < .05 as statistically significant. Pearson chi-squared test was used for categorical variables and a Student's t test or Mann-Whitney U test for continuous variables. Multivariable linear regression analysis was used to identify factors of in-hospital delay.
3. Results
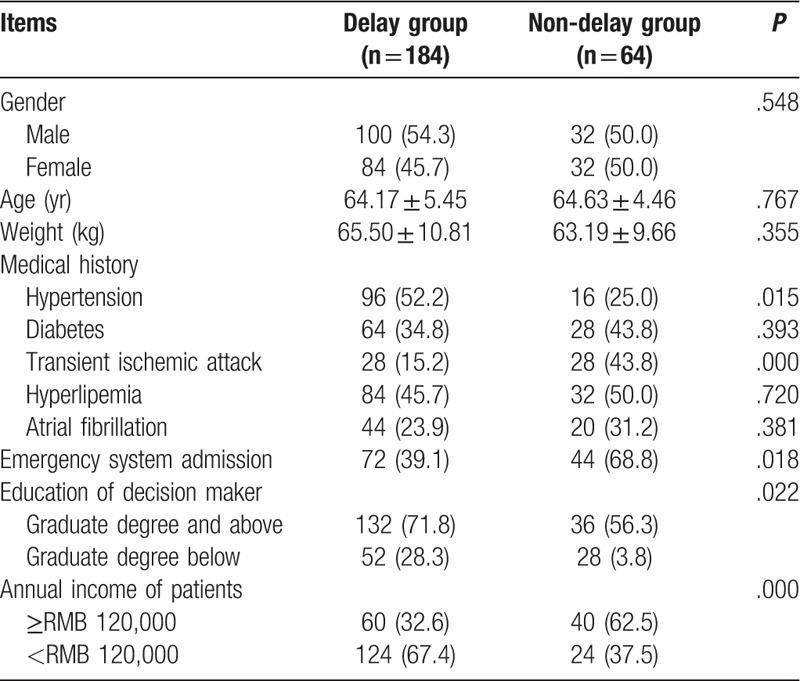
3.1. Comparison of demographic characteristics between 2 groups
As shown in Table 1, there were 184 cases in delay group and 64 cases in non-delay group respectively. The mean ages were 64.17 years in delay group and 64.63 years in non-delay group respectively 54.3% and 50.0% of cases were male patients respectively. There were significant differences in transient ischemic attack, emergency system admission, the education of decision maker, annual income between the 2 groups (all P < .05). Other demographic characteristics such as gender, age and medical history showed no significant differences in 2 groups (P > .05).
Table 1.
Comparison of demographic characteristics between 2 groups.
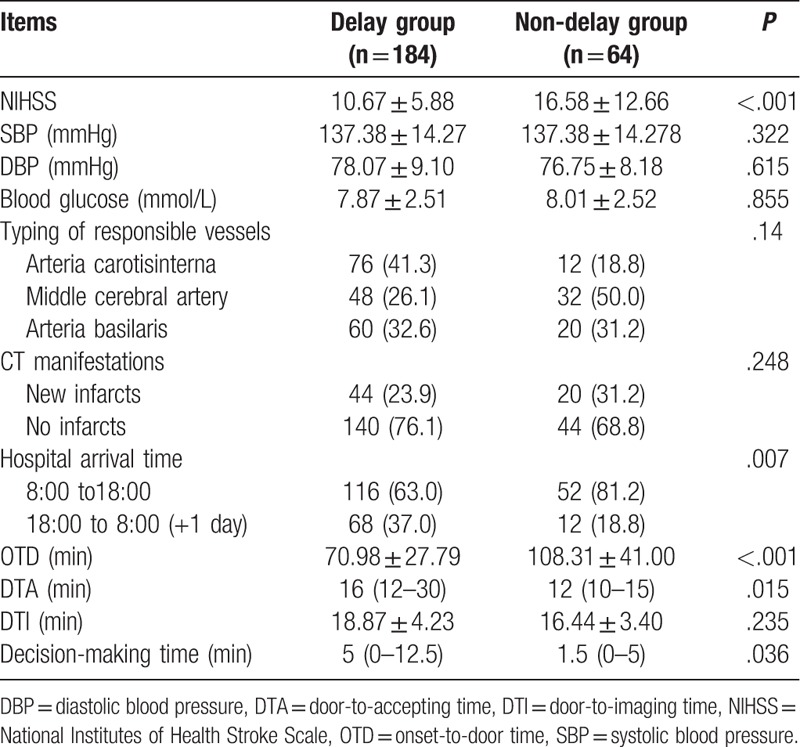
3.2. Comparison of clinical features and time intervals between 2 groups
The results revealed that delay group had lower scores of NIHSS (P < .01) than non-delay group. DTA (P = .01) and decision-making time (P = .03) were significantly longer, but OTD (P < .01) were significantly shorter (Table 2) in delay group than that in non-delay group. Other clinical features such as SBP, DBP, blood glucose, typing of responsible vessels, CT manifestations, hospital arrival time and DTI time showed no significant differences in 2 groups (P > .05).
Table 2.
Comparison of clinical features and time intervals between 2 groups.
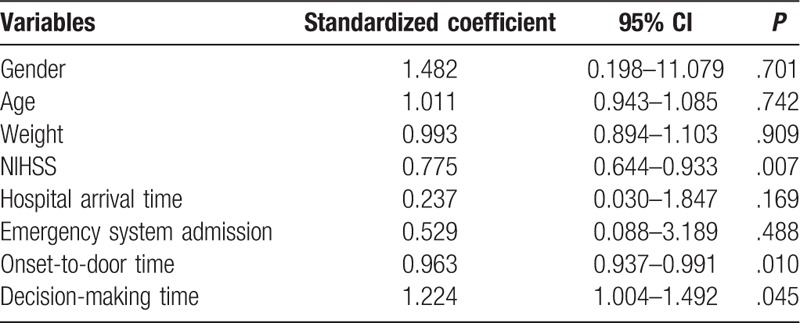
3.3. Multivariate linear regression analysis to identify independent variables that affect in-hospital delay
As shown in Table 3, seven variables (sex, age, weight, NIHSS, hospital arrival time, emergency system admission, OTD time, decision-making time) were included in the multivariate linear regression models, respectively to analyze the risk factors affecting the in-hospital delay. The results revealed that the in-hospital delay was closely related to NIHSS score (OR = 0.775, 95% CI: 0.644-0.933, P = .007), OTD time (OR = 0.963, 95% CI: 0.937-0.991, P = .010) and decision-making time (OR = 1.224, 95% CI: 1.004-1.492, P = .045). These results suggested that NIHSS and OTD and decision-making time were the independent risk factors of in-hospital delay of IVT for AIS patients.
Table 3.
Multivariate linear regression analysis to identify independent variables that affect in-hospital delay.
4. Discussion
At present, the most effective treatment for AIS patients is IVT with rt-PA.[14–16] However, this therapy has the disadvantages of a strict time window, a large number of contraindications and high cost, resulting in not using widely in China. According to the National Stroke Record Database of China, only 1.6% of AIS patients undergo IVT in China. Patients with thrombolytic DTN ≤ 60 minutes are approximately 26.6% to 47.0% all over the world.[9] Prompt administration of rt-PA for AIS patients has been shown to improve patients’ outcomes. To optimize the benefits of IVT, all efforts should be directed towards reducing or even eliminating treatment delays. In the present study, we investigated the factors associated with in-hospital delay in Gansu Provincial Hospital, revealing that NIHSS and OTD and decision-making time were the independent risk factors of in-hospital delay.
NIHSS is a relatively universal and concise stroke assessment scale in the world, mainly evaluating the neurological deficits in the treatment of AIS.[3] The level of NIHSS score can reflect the clinical situation of the patient more intuitively.[17,18] This study shows that patients with higher admission NIHSS scores have a lower risk of in-hospital delays, which might be explained by that fact that severe clinical symptoms easily attracted the family members and emergency medicine specialist and specialist physicians. Namely, the patients who have higher NIHSS score underwent quick inspections after they arrived at hospital and the green channel in hospital for AIS closely connected all stroke units, which reduced hospital transit time and the risk of in-hospital delays. The OTD was independent risk factor of in-hospital delay, which might be attributed to the facts that the longer time of the symptom progression makes the DTN time shorter. Our results are consistent with the reports in other study.[19] The inverse relationship between OTD time and DTN time is known as the ‘3-hour effect’. The DTN time of patients admitted to the hospital at the early time window are longer than that of cases admitted for nearly 3 hours of onset of stroke.[20,21] In our series, the ‘3-hour effect’ significantly interfered with DTA time, which may be associated with the emergency level perceived by clinicians. Clinicians are more concerned about critical patients. Patients with shorter time of symptom progression have more time for IVT and were treated with less urgency. It is well known that the effect of IVT is significantly reduced with the increase in the time from the onset of AIS to the acceptance of IVT. Receiving early IVT suggested the better prognosis of patients. In order to ensure the therapeutic effect, patients within the time window also should receive IVT as soon as possible. For eliminating the 3-hour effect, previous studies proposed some actions including constant review of DTN times by the stroke care team, exchange of feedback among doctors responsible for in-hospital care of acute stroke patients, and better adherence to treatment guidelines.[21]
Decision-making process for IVT could be a factor affecting in-hospital delay. Our study supported that the process of decision-making for IVT contributed to a prominent in-hospital delay. At present, AIS patients should be firstly examined by emergency physician followed by being informed to specialists. Once the definite diagnosis is made, medical professionals should communicate with patients or their family members stating the risk of IVT, letting them to sign the consents which are absolutely necessary. In China, AIS patients or their family members have much more concerns about IVT risks and expensive cost of rt-PA, leading to the longer time to make a decision, subsequently increasing DTN time. The international standard of DTN time is 60 minutes, while the average DTN of Chinese AIS patients are 116 minutes. This difference might be largely due to the longer decision-making time in China. In USA, United Kingdom, and some European countries, IVT for AIS patients is mostly routine and signing a consent form is not necessary.[19] The relationship between doctors and patients in China is complex. Candidates older than 60 years undergoing IVT in China usually have more than 1 son or daughter, making it even harder to designate an appropriate decision-maker. The public education regarding the AIS in China is not as good as that in Western countries, resulting in the facts that the presentation of risk and benefit is often biased by the physicians who are under threat of frequent violence from the patients or their family members. In order to confirm that patients or their family members understand the risks and take all responsibilities of the potential unexpected outcomes, signing a consent form is of absolute necessities. To eliminating the influence, clinical professionals should be trained to have the talking skill; therefore, the DTN time is accordingly reduced.
The in-hospital delay in China is mainly due to the lack of coordination between all stroke units from previous study.[22] In order to reduce the DNT time and increase the rate of thrombolytic therapy, some measures were taken in China and remarkable results were achieved,[23,24] making the delay less serious. For the first time, our study supported that in-hospital delay is mainly due to longer time of physician's assessment of the patient's condition, as well as the poorer communication between physicians and patients.
Our study has several limitations. First, one single-center experience may not depict the full picture of the whole country. Second, we did not divide the degrees of severity of delay situation. Finally, our experience on reducing in-hospital delay might be only successfully applied in specific local conditions (e.g., Lanzhou). However, given to the huge homogeneity in the process of IVT, efforts to reduce in-hospital delay are more likely to work in a similar way.
5. Conclusion
In summary, this study suggested that NIHSS score, OTD time, and decision-making time are the independent factors affecting the in-hospital delay of thrombolysis for AIS.
Author contributions
Conceptualization: Erqing Chai.
Formal analysis: Erqing Chai, Changqing Li.
Investigation: Erqing Chai, Changqing Li, Lei Jiang.
Methodology: Changqing Li, Lei Jiang. Supervision: Erqing Chai.
Supervision: Erqing Chai.
Writing – original draft: Changqing Li.
Writing – review & editing: Erqing Chai
Footnotes
Abbreviations: AIS = acute ischemic stroke, DTA = door-to-accepting time, DTI = door-to-imaging time, DTN = door-to-needle, IVT = intravenous thrombolysis, NIHSS = National Institutes of Health Stroke Scale, OTD = onset-to-door, rt-PA = recombinant tissue-type plasminogen activator.
This study was supported by grant of Lanzhou Talent Innovation and Entrepreneurship (2017-RC-57).
The authors have no conflicts of interest to disclose.
References
- [1].Studnek JR, Bentley M, Crawford JM, et al. An assessment of key health indicators among emergency medical services professionals. Prehosp Emerg Care 2010;14:14–20. [DOI] [PubMed] [Google Scholar]
- [2].Wu C, Wu D, Chen J, et al. Why not intravenous thrombolysis in patients with recurrent stroke within 3 months? Aging Dis 2018;9:309–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Wang R, Zeng J, Chen X, et al. Risk factors of hemorrhagic transformation after intravenous thrombolysis with rt-PA in acute cerebral infarction. QJM 2018. [DOI] [PubMed] [Google Scholar]
- [4].Kim DH, Bae HJ, Han MK, et al. Direct admission to stroke centers reduces treatment delay and improves clinical outcome after intravenous thrombolysis. J Clin Neurosci 2016;27:74–9. [DOI] [PubMed] [Google Scholar]
- [5].Pretnar Oblak J, Sabovic M, Frol S. Intravenous thrombolysis after idarucizumab application in acute stroke patients-a potentially increased sensitivity of thrombi to lysis? J Stroke Cerebrovasc Dis 2019;28:768–73. [DOI] [PubMed] [Google Scholar]
- [6].El Khoury R, Jung R, Nanda A, et al. Overview of key factors in improving access to acute stroke care. Neurology 2012;79:S26–34. [DOI] [PubMed] [Google Scholar]
- [7].Wardlaw JM, Murray V, Berge E, et al. Recombinant tissue plasminogen activator for acute ischaemic stroke: an updated systematic review and meta-analysis. Lancet 2012;379:2364–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Yoo J, Sohn SI, Kim J, et al. Delayed intravenous thrombolysis in patients with minor stroke. Cerebrovasc Dis 2018;46:52–8. [DOI] [PubMed] [Google Scholar]
- [9].Wang Y, Liao X, Zhao X, et al. Using recombinant tissue plasminogen activator to treat acute ischemic stroke in China: analysis of the results from the Chinese National Stroke Registry (CNSR). Stroke 2011;42:1658–64. [DOI] [PubMed] [Google Scholar]
- [10].Mulder MJ, van Oostenbrugge RJ, Dippel DW, et al. Letter by Mulder et al Regarding Article, “2015 AHA/ASA Focused Update of the 2013 Guidelines for the Early Management of Patients With Acute Ischemic Stroke Regarding Endovascular Treatment: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association”. Stroke 2015;46:e235. [DOI] [PubMed] [Google Scholar]
- [11].Liu L, Wang D, Wong KS, et al. Stroke and stroke care in China: huge burden, significant workload, and a national priority. Stroke 2011;42:3651–4. [DOI] [PubMed] [Google Scholar]
- [12].Schwartz A, Money K, Spangehl M, et al. Office-based rapid prototyping in orthopedic surgery: a novel planning technique and review of the literature. Am J Orthop (Belle Mead NJ) 2015;44:19–25. [PubMed] [Google Scholar]
- [13].Khatri P, Yeatts SD, Mazighi M, et al. Time to angiographic reperfusion and clinical outcome after acute ischaemic stroke: an analysis of data from the Interventional Management of Stroke (IMS III) phase 3 trial. Lancet Neurol 2014;13:567–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Broderick JP, Palesch YY, Demchuk AM, et al. Endovascular therapy after intravenous t-PA versus t-PA alone for stroke. N Engl J Med 2013;368:893–903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Emberson J, Lees KR, Lyden P, et al. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet 2014;384:1929–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Zaidat OO, Yoo AJ, Khatri P, et al. Recommendations on angiographic revascularization grading standards for acute ischemic stroke: a consensus statement. Stroke 2013;44:2650–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Garcia Pastor A, Diaz Otero F, Gil Navarro S, et al. Vascular imaging before intravenous thrombolysis: consequences of in-hospital delay in applying two diagnostic procedures. J Neuroimaging 2015;25:397–402. [DOI] [PubMed] [Google Scholar]
- [18].Huang Q, Ma QF, Jia JP, et al. Referral leads to prehospital delay of intravenous thrombolysis for acute ischemic stroke in Beijing. Int J Stroke 2015;10:E80–1. [DOI] [PubMed] [Google Scholar]
- [19].Huang Q, Ma QF, Feng J, et al. Factors associated with in-hospital delay in intravenous thrombolysis for acute ischemic stroke: lessons from China. PLoS One 2015;10:e0143145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Mikulik R, Kadlecova P, Czlonkowska A, et al. Factors influencing in-hospital delay in treatment with intravenous thrombolysis. Stroke 2012;43:1578–83. [DOI] [PubMed] [Google Scholar]
- [21].Xiang QLG, Huang Z. Correlative factors of prehospital and in-hospital delays of arterial thrombolysis in the treatment of patients with acute ischemic stroke. Chin J Disaster Med 2017;5:246–50. [Google Scholar]
- [22].Fonarow GC, Zhao X, Smith EE, et al. Door-to-needle times for tissue plasminogen activator administration and clinical outcomes in acute ischemic stroke before and after a quality improvement initiative. JAMA 2014;311:1632–40. [DOI] [PubMed] [Google Scholar]
- [23].Meretoja A, Strbian D, Mustanoja S, et al. Reducing in-hospital delay to 20 minutes in stroke thrombolysis. Neurology 2012;79:306–13. [DOI] [PubMed] [Google Scholar]
- [24].Thortveit ET, Boe MG, Ljostad U, et al. Organizational changes aiming to reduce iv tPA door-to-needle time. Acta Neurol Scand 2014;130:248–52. [DOI] [PubMed] [Google Scholar]


