Abstract
Background:
An adductor canal block (ACB) provides recognized analgesia following total knee arthroplasty (TKA). This meta-analysis compared the single-injection ACB (SACB) with the continuous-injection ACB (CACB).
Method:
Relevant studies were searched from PubMed (1996–October 2018), Embase (1980–October 2018), and Cochrane Library (CENTRAL, October 2018). Four randomized controlled trials (RCTs), which compared SACB with CACB, were included in our meta-analysis.
Results:
Four RCTs met the inclusion criteria. Our pooled data indicated that the SACB group had similar efficacy compared with the CACB group in terms of morphine consumption (P = .19), time to first opioid request (P = .32), range of motion (P = .97), and visual analogue scale (VAS) scores at 24 hours at rest (P = .12) and movement (P = .24), without increasing the risk of complications (P = .97) and length of stay (P = .54).
Conclusion:
The SACB technique provides similar analgesia in the 24 hours following TKA compared with CACB, while the CACB method was better over 48 hours.
Keywords: adductor canal block, continuous, meta-analysis, single shot, total knee arthroplasty
1. Introduction
Total knee arthroplasty (TKA) is a common surgical procedure for a painful arthritic knee. It has been reported that the number of TKA procedures will reach 3.48 million by 2030.[1,2] However, TKA is followed by moderate to severe pain during the postoperative period.[3] Adequate pain relief following TKA can promote early rehabilitation. Patient-controlled analgesia (PCA) and epidural analgesia are the conventional analgesia methods,[4–7] and the femoral nerve block (FNB) is recognized as the gold standard for pain relief following TKA.[8,9] On the contrary, FNB adds the risk of reducing quadriceps muscle strength, thus compromising postoperative rehabilitation.[10]
The adductor canal block (ACB), one kind of peripheral nerve block (PNB), is increasingly being used.[11–13] Several published studies have demonstrated the superiority of the ACB in analgesic effect as compared to FNB.[14,15] There is a growing consensus that the ACB should be recommended as the analgesic choice for patients undergoing TKA.[16,17] However, there is no consensus as to which is better between the single-shot adductor canal and the continuous adductor canal blockade.
Thus, we performed the first meta-analysis to compare the efficacy of the continuous ACB (CACB) and the single-shot ACB (SACB).
2. Method and materials
Our meta-analysis was conducted by the Cochrane Handbook for systematic review of interventions (Review Manager 5.3). The study was approved by the ethics committee of Xiaoshan Traditional Chinese Medical Hospital.
2.1. Search strategy
We systematically searched PubMed (1996–October 2018), Embase (1980–October 2018), and the Cochrane Library (CENTRAL, October 2018). We also searched related references and Google Scholar. Only randomized controlled trials (RCTs) were included in our meta-analysis. “Total knee arthroplasty,” “Total knee replacement,” “ACB,” “Adductor canal block” were the key words used with Boolean operators “AND” or “OR.” The search results are shown in Fig. 1.
Figure 1.
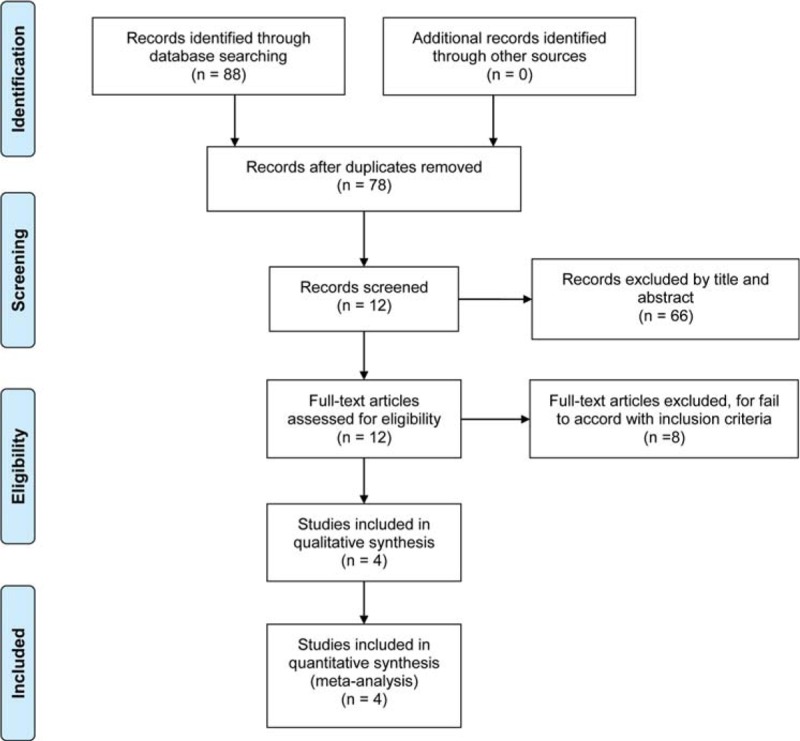
The search results and selection procedure.
2.2. Inclusion criteria
RCTs were included in our meta-analysis if they met the following PICOS (patients, intervention, comparator, outcome, study design) criteria:
-
(1)
Patients: patients had received TKA for the first time.
-
(2)
Intervention: Patients received a single-shot ACB for TKA.
-
(3)
Comparator: Patients received a continuous ACB for TKA.
-
(4)
Outcomes: morphine consumption, VAS score at rest and movement, time to first opioid request, range of motion (ROM), complications, and LOS.
-
(5)
Study design: RCTs.
2.3. Data extraction and bias risk assessment
Two reviewers independently collected available data from studies, and any disagreement between the 2 reviewers was judged by a third reviewer. Basic characteristics include patients’ age, gender, body mass index (BMI), and reference type. The morphine consumption and VAS score were primary outcomes in our meta-analysis. All opioids were converted to equivalent morphine consumption dosage according to the standard formula.[18] The VAS score consists of 11 pain levels with 0 being no pain and 10 representing the worst pain. Secondary outcomes consisted of time to first opioid request, ROM, complications, and length of stay (LOS). We emailed corresponding authors to obtain any incomplete data. We chose the Cochrane Handbook for systematic review of interventions (Review Manager 5.3) to evaluate the risk bias of the included studies.
2.4. Statistical analysis
We used Review Manager 5.3 software (Cochrane Collaboration, Copenhagen: The Nordic Cochrane Centre) for our meta-analysis. For continuous data, the mean difference (MD) with 95% confidence interval (95% CI) was applied to weigh the effect interval. For noncontinuous data, the risk ratio (RR) and risk differences (RDs) with 95% CIs were used to figure the effect interval. P and I2 were used to assess the statistical heterogeneity among the included studies. When I2 < 50% and P > .1, we applied a fixed-effects model; otherwise, a random-effect model was applied.
3. Results
3.1. Search results
According to our search strategy, a total of 88 studies were found. Ten studies were excluded by Endnote software, and 66 studies were removed after reading the title and abstract. Of the original 88, 4 RCTs[19–22] were included in our meta-analysis. The basic characteristics and interventions are summarized in Tables 1 and 2.
Table 1.
The characteristics of included studies.
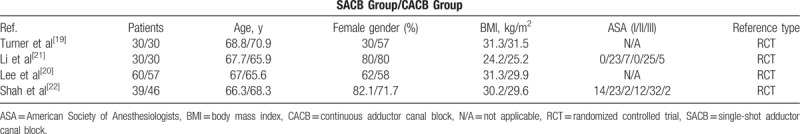
Table 2.
Characteristics of included studies showing general intervention information.
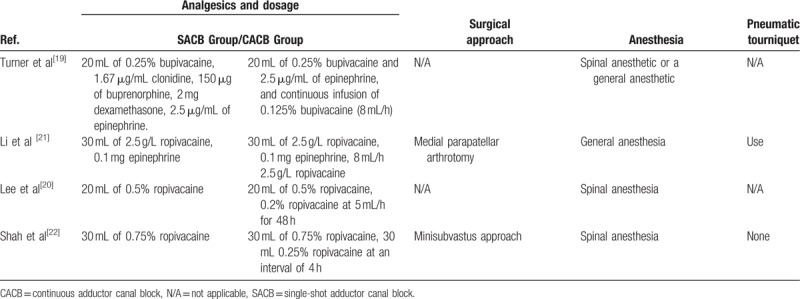
3.2. Risk of bias of assessment
The risk of bias of assessment of RCTs is presented in Figs. 2 and 3. Among the 4 RCTs, 2 studies[20,22] were recorded using computer-generated randomization or a web-based randomization service. Two RCTs reported allocation concealment via sealed envelopes or other methods.[19,21] A double-blind method was applied by Turner et al.[19] The publication bias was assessed using a funnel plot diagram (Fig. 4).
Figure 2.
The risk of bias summary: review authors’ judgment of each risk of bias items for each included studies.
Figure 3.
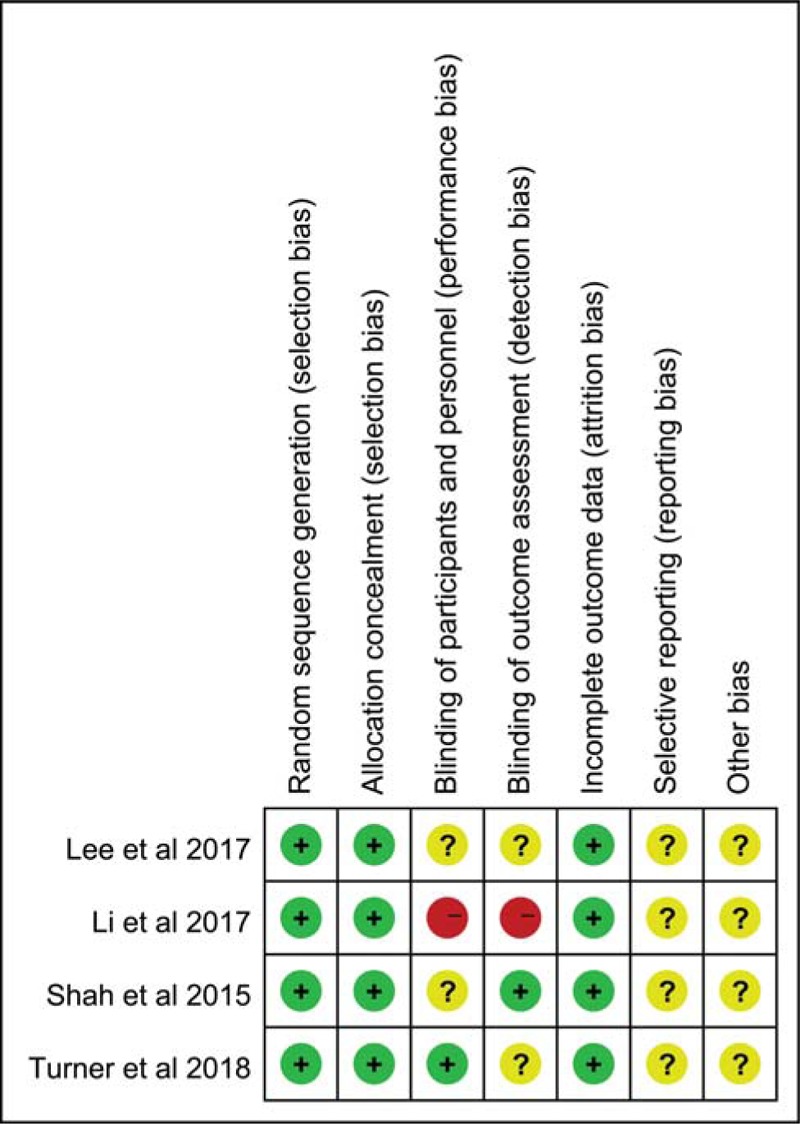
The risk of bias graph of the included studies.
Figure 4.
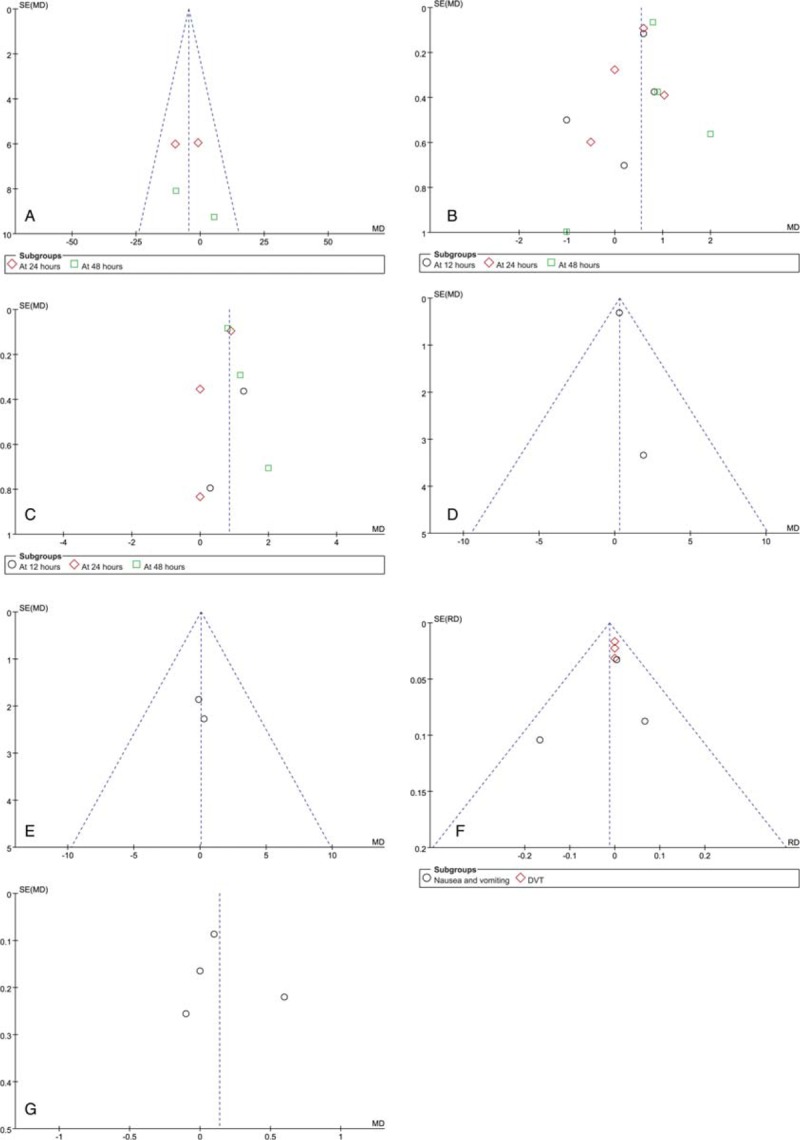
(A) A funnel plot of morphine consumption (mg); (B) A funnel plot of VAS at rest; (C) A funnel plot of VAS at movement; (D) A funnel plot of time to first opioid request (hours); (E) A funnel plot of range of motion; (F) A funnel plot of Complications; (G) A funnel plot of LOS.
3.3. Results of meta-analysis
3.3.1. Morphine consumption
Two studies, including 176 patients, reported morphine consumption for postoperative day 1, and no significant differences were found between the 2 groups (MD = −5.25; 95% CI, −13.53 to 3.02; P = .21, Fig. 5). A similar finding was found for postoperative day 2 (MD = −3.04; 95% CI, −14.98 to 8.90; P = .62, Fig. 5). Due to no significant heterogeneity in morphine consumption for day 1 (x2 = 1.09; df = 1; P = .30; I2 = 8%, Fig. 5) or day 2 (x2 = 1.47; df = 1; P = .23; I2 = 32%, Fig. 5), a fixed-effects model was applied.
Figure 5.
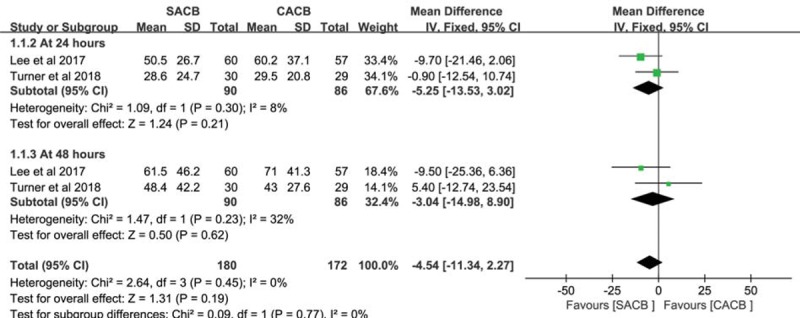
A forest plot diagram showing the equivalent morphine consumption (mg).
3.3.2. VAS score at rest
Four studies consisting of 321 patients reported VAS scores at rest at postoperative 12 hours, and no significant differences were found between the 2 groups (MD = 0.25; 95% CI, −0.44 to 0.95; P = .47, Fig. 6). Data from 4 studies, including 321 patients, compared the VAS scores at rest at postoperative 24 hours. No significant differences were found between the 2 groups (MD = 0.39; 95% CI, −0.10 to 0.88; P = .12, Fig. 6). The VAS scores at rest at postoperative 48 hours were reported in 4 studies containing 321 patients. The SACB group had higher scores than the CACB group (MD = 0.90; 95% CI, 0.28–1.53; P < .05, Fig. 6). Due to significant heterogeneity in VAS scores at rest at postoperative 12 hours (x2 = 10.60; df = 3; P < .05; I2 = 72%, Fig. 6), a random-effects model was applied.
Figure 6.
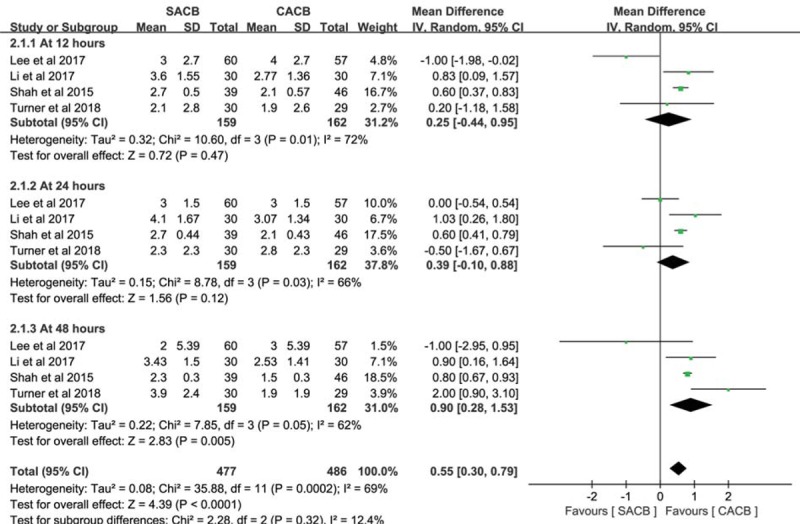
A forest plot diagram showing the VAS at rest.
3.3.3. VAS score at movement
Two studies reported VAS scores at movement at postoperative 12 hours, and the SACB group had higher scores than the CACB group (MD = 1.04; 95% CI, 0.24–1.85; P < .05, Fig. 7). A similar finding was found at postoperative 48 hours (MD = 1.03; 95% CI, 0.57–1.49; P = .62, Fig. 7). Three studies consisting of 204 patients reported the VAS scores in movement at postoperative 24 hours, while we were unable to find any significant differences between the 2 groups (MD = 0.45; 95% CI, −0.30 to 1.20; P = .24, Fig. 7). We used a random-effects model because of the significant heterogeneity in VAS scores in movement at postoperative 24 hours (x2 = 7.04; df = 2; P = .03; I2 = 72%, Fig. 7) and 48 hours (x2 = 4.20; df = 2; P = .12; I2 = 52%, Fig. 7).
Figure 7.
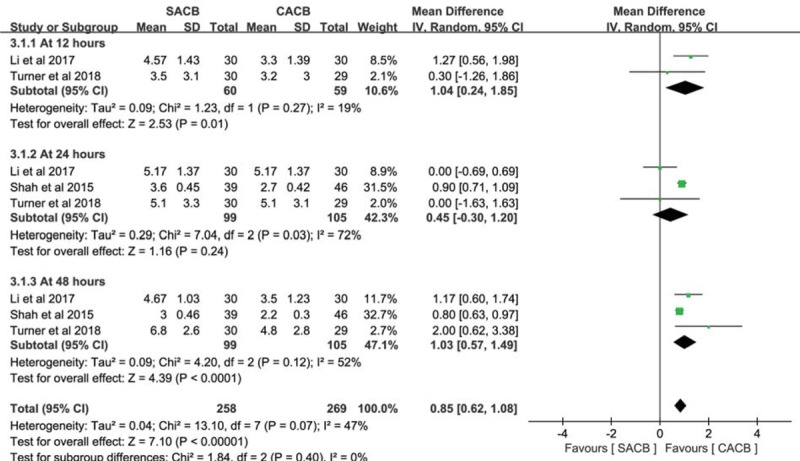
A forest plot diagram showing the VAS at movement.
3.3.4. Time to first opioid request (hours)
Two studies consisting of 176 patients reported the time to first opioid request (hours), and no significant differences were found between the 2 groups (MD = 0.31; 95% CI, −0.30 to 0.93; P = .32, Fig. 8). We used a fixed-effects model, as no significant heterogeneity was found between the SACB and CACB groups (x2 = 0.23; df = 1; P = .63; I2 = 0%, Fig. 8).
Figure 8.
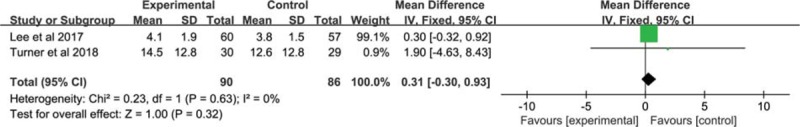
A forest plot diagram showing the time to first opioid request (h).
3.3.5. Range of motion
ROM was reported in 2 studies consisting of 145 patients. No significant differences were found between the SACB and CACB groups (MD = 0.06; 95% CI, −2.76 to 2.88; P = .97, Fig. 9). We used a fixed-effects model because no significant heterogeneity was found (x2 = 0.02; df = 1; P = .89; I2 = 0%, Fig. 9).
Figure 9.
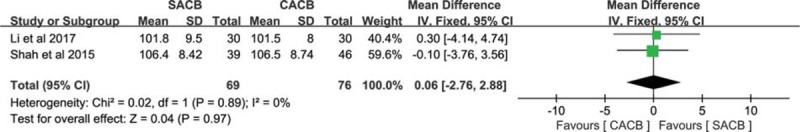
A forest plot diagram showing the range of motion.
3.3.6. Complications
Three studies reported postoperative nausea and vomiting (PONV) in the SACB and CACB groups, and no significant differences were found between the 2 groups (RD = −0.03; 95% CI, −0.11 to 0.05; P = .51, Fig. 10). Data from 3 studies consisting of 262 patients reported the incidence of deep venous thrombosis (DVT). No significant differences were found between the 2 groups (RD = 0; 95% CI, −0.03 to 0.03; P = 1, Fig. 10). We used a fixed-effects model because no significant heterogeneity was found in PONV (x2 = 3.85; df = 2; P = .15; I2 = 48%, Fig. 10) and DVT (x2 = 0; df = 2; P = 1; I2 = 0%, Fig. 10).
Figure 10.
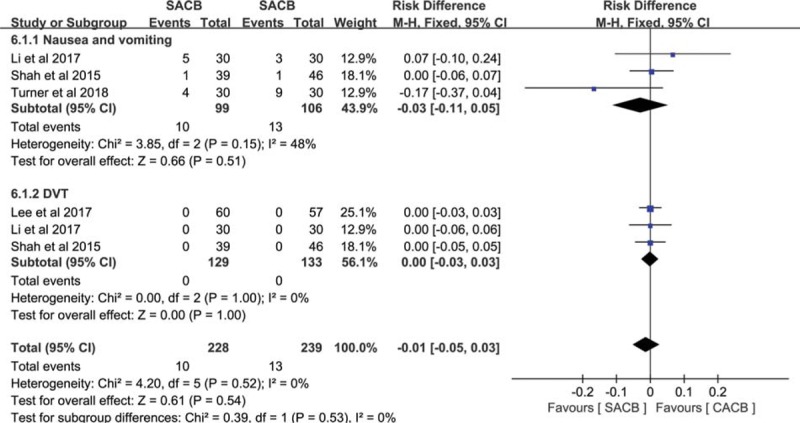
A forest plot diagram showing the complications.
3.3.7. LOS
Then, LOS was reported in 4 studies with a total of 321 patients. Our pooled data indicated that the SACB group had similar LOS compared with the CACB group (MD = 0.12; 95% CI, −0.02 to 0.25; P = .09, Fig. 11). We used a random-effects model for heterogeneity between the included studies (x2 = 6.09; df = 3; P = .11; I2 = 51%, Fig. 11).
Figure 11.
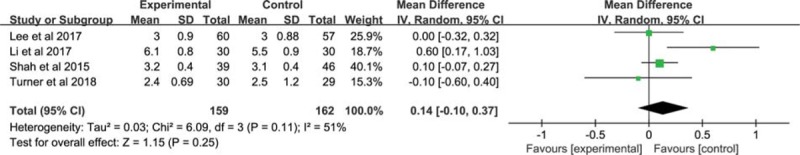
A forest plot diagram showing the LOS. Credit: All figures can be printed by the Medicine.
4. Discussion
This study, to the best of our knowledge, is the first meta-analysis comparing the SACB and CACB methods. The results of our meta-analysis demonstrated that the SACB technique provides similar analgesia in the 24 hours following TKA when compared with the ACB, while the CACB was better over 48 hours.
Appropriate pain management following TKA can lower postoperative pain and promote early rehabilitation.[23,24] Postoperative analgesia is usually managed by a PNB and a FNB. The FNB is recognized as the gold standard for pain relief following TKA. Alternatives to the FNB include epidural analgesia, periarticular infiltration analgesia, and an ACB.[24,25] In our previous study,[7] we found that local infiltration analgesia has similar analgesic properties to the FNB. Recently published studies[19,20] have reported that the ACB has equivalent analgesia efficacy as compared with the FNB method. However, it is not clear which method is better between the SACB and the CACB.
Morphine consumption was the primary outcome in our meta-analysis. Morphine consumption is one of most important indexes to estimate the efficacy of analgesia methods. Shah et al[22] found that compared with the SACB method, the CACB has better efficacy in terms of pain control, but was similar for early functional recovery. Some other recently published studies have different opinions. An RCT conducted by Lee et al[20] found that at 24 and 48 hours, the SACB was equal to the CACB for opioid consumption. Turner et al[19] also reported that there were no significant differences found between the SACB and the CACB groups related to opioid consumption at either 36 or 48 hours. Our meta-analysis results also indicated that the SACB had similar morphine consumption when compared with the CACB group within 48 hours postoperative. Thus, we draw a conclusion that the SACB group had the same morphine consumption as the CACB group.
In this meta-analysis, we used a VAS score to weigh the analgesia effect. We found that the SACB group was equal to the CACB group within 24 hours. Turner et al[19] also reported that numerical rating scale (NRS) pain score comparisons were not statistically different between the 2 groups with 42 hours postoperative (rest, P = .01; movement, P = .25) and 48 hours (rest, P = .001; movement, P = .04). Similar findings were reported by Shah et al.[22]
ROM was used to measure early mobilization. It is well-known that early mobilization can facilitate functional recovery and reduce postoperative complications and length of hospital stay. Shah et al[22] used a large hospital database to assess the data of ROM among both the SACB and CACB groups. The results of the RCT demonstrated that the ROM at discharge and length of hospital stay displayed almost identical results with no statistical significance (106.5 vs 106.4, 3.08 vs 3.20, P > .05, respectively). Li et al[21] also reported that there was no statistical significance toward ROM between the SACB and CACB groups at discharge (101.8 ± 9.5 vs 101.5 ± 8, P > .05, respectively). Taking these findings together, the SACB achieved similar effects for ROM and LOS when compared with the CACB in patients undergoing TKA. With regard to time to first opioid request, Turner et al[19] found that in the SACB group versus the CACB group, time to first analgesic administration was 869 versus 754.5 minutes, P = .57. Similar findings were reported by Lee et al.[20] Postoperative PONV was a common complication in TKA. Our meta-analysis failed to find any significant differences between the SACB and CACB groups. Similar findings were reported by Li et al[21] and Turner et al.[19] Lee et al[20] reported that no occurrences of catheter site infections were found in their study. Shah et al[22] also reported that none of the patients in either group showed any other side effects or treatment-related complications. Therefore, the SACB method was found to be a suitable method for pain relief for patients undergoing TKA.
Our systematic review and meta-analysis has several limitations. First, only 4 RCTs were included in our meta-analysis. Pooled data would be more accurate and reliable if more RCTs had been included. Second, we evaluated only the VAS score within 48 hours after TKA. Therefore, a long-term follow-up study would be more persuasive. Third, outcomes such as quadriceps muscle strength and total duration of analgesia failed to be analyzed due to insufficient data. Finally, the PRISMA guidelines and Cochrane Handbook[26] were used in our meta-analysis to ensure the quality of our meta-analysis.
5. Conclusion
Overall, our meta-analysis results demonstrated that compared with the CACB method, the SACB may be more preferable, particularly for hospitals without experienced anesthesiologists and resources to perform the continuous infusions.
Author contributions
Conceptualization: Jian-hong Zhou.
Data curation: Bo-ya Zhang, Ren_fu Quan.
Formal analysis: Bo-ya Zhang.
Investigation: Bo-ya Zhang, Hong Xu.
Methodology: Yu-jie Sun.
Resources: Yu-jie Sun.
Software: Hong Xu, Yu-jie Sun.
Supervision: Yu-jie Sun.
Validation: Jian-hong Zhou.
Visualization: Jian-hong Zhou.
Writing – original draft: Jian-hong Zhou.
Writing – review & editing: Lu-kai Zhang, Ren_fu Quan, Jian-hong Zhou.
Footnotes
Abbreviations: BMI = body mass index, CACB = continuous-injection adductor canal block, CIs = confidence intervals, DVT = deep vein thrombosis, LOS = length of hospital stay, MD = mean difference, OR = odds ratio, PE = pulmonary embolism, PONV = postoperative nausea and vomiting, PRISMA = Preferred Reporting Items for Systematic Review and Meta-analyses, RCT = randomized controlled trial, RD = risk difference, ROM = range of motion, RR = relative risk, SACB = single-injection adductor canal block, TKA = total knee arthroplasty, VAS = visual analogue scale.
L-kZ and B-yZ contributed equally to this work.
The authors report no conflicts of interest.
References
- [1].Cram P, Lu X, Kates SL, et al. Total knee arthroplasty volume, utilization, and outcomes among Medicare beneficiaries, 1991–2010. JAMA 2012;308:1227–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Kurtz S, Ong K, Lau E, et al. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 2007;89:780–5. [DOI] [PubMed] [Google Scholar]
- [3].Puolakka PA, Rorarius MG, Roviola M, et al. Persistent pain following knee arthroplasty. Eur J Anaesthesiol 2010;27:455–60. [DOI] [PubMed] [Google Scholar]
- [4].Gomez-Cardero P, Rodriguez-Merchan EC. Postoperative analgesia in TKA: ropivacaine continuous intraarticular infusion. Clin Orthop Relat Res 2010;468:1242–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Kazak Bengisun Z, Aysu Salviz E, Darcin K, et al. Intraarticular levobupivacaine or bupivacaine administration decreases pain scores and provides a better recovery after total knee arthroplasty. J Anesth 2010;24:694–9. [DOI] [PubMed] [Google Scholar]
- [6].Safa B, Gollish J, Haslam L, et al. Comparing the effects of single shot sciatic nerve block versus posterior capsule local anesthetic infiltration on analgesia and functional outcome after total knee arthroplasty: a prospective, randomized, double-blinded, controlled trial. J Arthroplasty 2014;29:1149–53. [DOI] [PubMed] [Google Scholar]
- [7].Zhang LK, Ma JX, Kuang MJ, et al. Comparison of periarticular local infiltration analgesia with femoral nerve block for total knee arthroplasty: a meta-analysis of randomized controlled trials. J Arthroplasty 2018;33:1972–8. e1974. [DOI] [PubMed] [Google Scholar]
- [8].Basques BA, Tetreault MW, Della Valle CJ. Same-day discharge compared with inpatient hospitalization following hip and knee arthroplasty. J Bone Joint Surg Am 2017;99:1969–77. [DOI] [PubMed] [Google Scholar]
- [9].Salinas FV, Liu SS, Mulroy MF. The effect of single-injection femoral nerve block versus continuous femoral nerve block after total knee arthroplasty on hospital length of stay and long-term functional recovery within an established clinical pathway. Anesth Analg 2006;102:1234–9. [DOI] [PubMed] [Google Scholar]
- [10].Elkassabany NM, Antosh S, Ahmed M, et al. The risk of falls after total knee arthroplasty with the use of a femoral nerve block versus an adductor canal block: a double-blinded randomized controlled study. Anesth Analg 2016;122:1696–703. [DOI] [PubMed] [Google Scholar]
- [11].Grevstad U, Mathiesen O, Valentiner LS, et al. Effect of adductor canal block versus femoral nerve block on quadriceps strength, mobilization, and pain after total knee arthroplasty: a randomized, blinded study. Reg Anesth Pain Med 2015;40:3–10. [DOI] [PubMed] [Google Scholar]
- [12].Mariano ER, Perlas A. Adductor canal block for total knee arthroplasty: the perfect recipe or just one ingredient? Anesthesiology 2014;120:530–2. [DOI] [PubMed] [Google Scholar]
- [13].Memtsoudis SG, Yoo D, Stundner O, et al. Subsartorial adductor canal vs femoral nerve block for analgesia after total knee replacement. Int Orthop 2015;39:673–80. [DOI] [PubMed] [Google Scholar]
- [14].Jaeger P, Zaric D, Fomsgaard JS, et al. Adductor canal block versus femoral nerve block for analgesia after total knee arthroplasty: a randomized, double-blind study. Reg Anesth Pain Med 2013;38:526–32. [DOI] [PubMed] [Google Scholar]
- [15].Zhao XQ, Jiang N, Yuan FF, et al. The comparison of adductor canal block with femoral nerve block following total knee arthroplasty: a systematic review with meta-analysis. J Anesth 2016;30:745–54. [DOI] [PubMed] [Google Scholar]
- [16].Andersen LO, Gaarn-Larsen L, Kristensen BB, et al. Subacute pain and function after fast-track hip and knee arthroplasty. Anaesthesia 2009;64:508–13. [DOI] [PubMed] [Google Scholar]
- [17].Webb CA, Mariano ER. Best multimodal analgesic protocol for total knee arthroplasty. Pain Manag 2015;5:185–96. [DOI] [PubMed] [Google Scholar]
- [18].Chaumeron A, Audy D, Drolet P, et al. Periarticular injection in knee arthroplasty improves quadriceps function. Clin Orthop Relat Res 2013;471:2284–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Turner JD, Dobson SW, Henshaw DS, et al. Single-injection adductor canal block with multiple adjuvants provides equivalent analgesia when compared with continuous adductor canal blockade for primary total knee arthroplasty: a double-blinded, randomized, controlled, equivalency trial. J Arthroplasty 2018;33:3160–6.e1. [DOI] [PubMed] [Google Scholar]
- [20].Lee S, Rooban N, Vaghadia H, et al. A randomized non-inferiority trial of adductor canal block for analgesia after total knee arthroplasty: single injection versus catheter technique. J Arthroplasty 2018;33:1045–51. [DOI] [PubMed] [Google Scholar]
- [21].Li C, Xu H, Shen B, et al. [Effect of continuous and single shot adductor canal blocks for postoperative analgesia and early rehabilitation after total knee arthroplasty]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2017;31:1049–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Shah NA, Jain NP, Panchal KA. Adductor canal blockade following total knee arthroplasty-continuous or single shot technique? Role in postoperative analgesia, ambulation ability and early functional recovery: a randomized controlled trial. J Arthroplasty 2015;30:1476–81. [DOI] [PubMed] [Google Scholar]
- [23].Parvataneni HK, Shah VP, Howard H, et al. Controlling pain after total hip and knee arthroplasty using a multimodal protocol with local periarticular injections: a prospective randomized study. J Arthroplasty 2007;226 suppl 2:33–8. [DOI] [PubMed] [Google Scholar]
- [24].Duellman TJ, Gaffigan C, Milbrandt JC, et al. Multi-modal, pre-emptive analgesia decreases the length of hospital stay following total joint arthroplasty. Orthopedics 2009;32:167. [PubMed] [Google Scholar]
- [25].Kerr DR, Kohan L. Local infiltration analgesia: a technique for the control of acute postoperative pain following knee and hip surgery: a case study of 325 patients. Acta Orthop 2008;79:174–83. [DOI] [PubMed] [Google Scholar]
- [26].Green S. Cochrane Handbook for Systematic Reviews of Interventions: Cochrane Book Series. Naunyn-Schmiedebergs Archiv für experimentelle Pathologie und Pharmakologie. 2011;5(2):S38. [Google Scholar]


