Highlights
-
•
Magnetic therapy as a novel alternative treatment is suitable for managing LBP. Its advantage over the standard pharmacological intervention is due to fewer side effects.
-
•
Previous studies reflect that there is still a gap in selecting the optimum parameters of pulsed electromagnetic field for treating acute and chronic nonspecific LBP. Many studies used high intensity and frequency of the PEMF, while others applied low parameters of the PEMF. While this study used 50 Hz frequency, with low intensity of 20 Gauss.
-
•
The dose of with 50 Hz and 20 Gauss seems to be useful.
Keywords: Non-specific low back pain, Pulsed electromagnetic field, Conventional physical therapy program
Abstract
Background
Further research on pulsed electromagnetic field (PEMF) effects on the different conditions of low back pain was warranted due to lack of studies in this area.
Objectives
To investigate the effects of pulsed electromagnetic field therapy with 50 Hz frequency, with low intensity of 20 Gauss compared to conventional non-invasive treatment modalities in patients with chronic non-specific low back pain.
Methods
Design – A prospective, randomized, patient-blinded, controlled trial. Setting – The study was conducted at Outpatient Physiotherapy Clinic in Cairo, Egypt. The study was conducted between May 2015 and September 2016. Participants – Fifty participants with non-specific low back pain enrolled into experimental and control groups. Interventions – The experimental group received the Conventional physical therapy Protocol as well as magnetic field, while the control group received the same Conventional physical therapy and sham electromagnetic field. Both groups received 12 sessions over 4 weeks’ period. Outcome measures – Primary outcome measures was pain intensity while the secondary outcome measures were disability and lumbar range of motion – ROM. There were no adverse events occurred during the study.
Results
Fifty participants with non-specific low back pain (control group n = 25; experimental group n = 25) were randomized. There were significant between-group differences in pain scores (mean difference – MD 1.52; 95%CI −0.34 to 3.35), function disability (MD 8.14; 95%CI 6.5 to 9.96), Range of Motion (ROM) of lumbar flexion (MD −1.27; 95%CI −1.09 to −1.45), ROM of lumbar extension (MD −1.1; 95%CI −0.97 to −1.23), ROM of lumbar right side bending (MD 8.2; 95%CI 6.56 to 9.84) and ROM of lumbar left side bending (MD 10.4; 95%CI 8.81 to 11.99) in favour of the experimental group.
Conclusion
Adding pulsed electromagnetic field to Conventional physical therapy Protocol yields superior clinical improvement in pain, functional disability, and lumbar ROM in patients with non-specific low back pain than Conventional physical therapy alone.
Introduction
Non-specific low back pain is considered as a public health problem globally.1 A study speculated that the lifetime prevalence of low back pain reaches 62% in adults. While, the mean point prevalence among the adults was 32%.1, 2 The lifetime of low back pain among Egyptian patients in a family center reached 48%, which indicates that low back pain is a prevalent symptom that deserves more attention.3
Low back pain is not only recognized as a significant medical disease problem, but also regarded as a major cause for work absences in industrialized societies.4 Both results in substantial costs for national economics and health care systems because of long lasting and cost intensive treatment options especially in chronic cases. These treatments in chronic cases include non-invasive as well as invasive or minimally invasive modalities, which are associated with high risks of adverse effects and increased morbidity.4 The risk/benefit ratio in pharmacotherapy for low back pain conditions often does not have strength enough to persist with the drug usage. Moreover, the risk of pharmacological addition, potential side-effects, and adverse events, as well as long-term toxicity may weaken the potential benefit of the pharmacotherapy approach.5 Despite the variety of treatments available, no modality or therapeutic approach stood out as a definitive solution.6
Thus, there is still a demand for new approaches, less invasive and unlikely to provide side effects.7 In this sense, the pulsed electromagnetic fields (PEMF) therapy can play an important role in pain relief since it is a drug-free, non-thermal, with low risk that works to enhance cellular activity healing and repair.6 Therefore, it could be an option to the non-steroidal anti-inflammatory drugs (NSAIDs) medication, avoiding several potential side-effects from chronic NSAIDs usage.6 Along with this line, many reviews have been performed to assess the PEMF effectiveness in several conditions. In this sense, PEMF therapy seems to be able to reduce the pain intensity and improve function in individuals suffering from low back pain. However, when added to a standard therapy, PEMF did not add any beneficial effect.7 Li et al.8 concluded that the PEMF showed moderate or no benefits in knee osteoarthritis. The PEMF showed beneficial tendency on the bone growth stimulation in acute fractures and efficient in relieving pain and enhancing bone formation in osteoporosis.9
Further research is needed to warranty the clinical effect of PEMF in patients with low back pain.7 So, the aim of this study was to investigate the additional effects of pulsed electromagnetic field therapy combined with conventional non-invasive treatment modalities in patients with chronic non-specific low back pain compared to conventional treatment alone.
Methods
Study design
The study was designed as a prospective, randomized, patient-blinded, placebo controlled trial. Ethical approval was obtained from the institutional review board at Faculty of physical therapy, Cairo University before study commencement [No.: P.T.REC/012/00422]. The study was followed the Guidelines of Declaration of Helsinki on the conduct of human research. The study was conducted between May 2015 and September 2016. This trial was prospectively registered at Pan African Clinical Trials Registry (PACTR): PACTR201805003393380 (https://pactr.samrc.ac.za/TrialDisplay.aspx?TrialID=3393)
Participants
A convenient sample of sixty patients was recruited from Out Clinic of Faculty of Physical Therapy, Cairo University. They were enrolled and assessed for their eligibility to participate in the study. To be included in the study, the participants were diagnosed clinically with chronic non-specific low back pain by a neurologist. The participants’ ages ranged from 20 to 40 years, had low back pain with a minimum duration of 3 months, with a Visual analogue scale (VAS) Pain score of at least 4 points (out of 10). The patients were excluded if they were pregnant or lactating women, had history of previous back surgery, radicular pain, current lower extremity symptoms, cardiopulmonary disease with decreased activity tolerance, open wound in the treated area, cauda equina symptoms or the known presence of tumor, or previous any participation in a clinical trial or physical therapy treatment within the past 30 days.6, 10, 11
Randomization
Informed consent was obtained from each participant after explaining the nature, purpose, and benefits of the study, informing them of their right to refuse or withdraw at any time, and about the confidentiality of any obtained information. Anonymity was assured through coding of all data. They were randomly allocated into experimental and control treatment group by a blinded and an independent research assistant who opened sealed, opaque envelopes that contained a computer generated randomization card. No subjects dropped out of the study after randomization.
Interventions
Participants were randomly assigned into; experimental group received active electromagnetic field (PEMF) and Conventional physical therapy Protocol. The control group received both sham electromagnetic field and Conventional physical therapy Protocol for 12 sessions over a four-week period. The Conventional physical therapy program for both groups included: TENS therapy for the low back (15 min 3 days/week), with a frequency of 100 Hz and fixed pulse12; ultrasound for 5 minutes, 1 Hz, continuous mode of application 1.5 w/cm2.13 The exercise programs were individually designed based on the patient examination and the clinical findings. The programs consisted strengthening, stretching exercises for the abdominal, back, pelvic, and lower limb muscles, suited to the clinical findings, 3 sessions per week every other day for 1 month.14, 15 The experimental group received (PEMF) in addition to the conventional protocol were treated with an ASA magnetic field device (Automatic PMT Quattro pro) with frequency of 50 Hz. The patient was exposed to low intensity 20 Gauss of (PEMF) from prone lying position for 20 min/session.16 The control group received the conventional physical therapy treatment and sham electromagnetic field. The sham device did not produce a radiofrequency electromagnetic field and was identical to the active device. The energy from the active device did not make any sensation, thus it could not be notable from the placebo device. All interventions were applied with an expert physical therapist, who has 10 years of experience in orthopedic physical therapy field.
Outcome measures
The primary outcome measure was pain intensity assessed by a 10-point visual analogue rating scale, with zero indicating no pain while 10 representing the worst pain.4 The secondary outcomes were (1) the Oswestry Disability Index (ODI), and (2) spinal range of motion. The ODI is a valid tool for measuring the functional disability of LBP across five domains. 0% indicating no disability and 100%, representing a patient that is completely disabled.6 Each item is scored on a 0–5 scale, and the maximum score is 50.17 Both pain intensity and disability are considered as core outcomes for clinical trials in the field of back pain.18, 19 The valid Arabic form was completed by each patient.20 Spinal range of motion was measured by the modified Schober test. A mark 5 cm below and another one 10 cm above the lumbosacral junction.21 The range of motion (ROM) is the difference between 15 cm and the length measured at the end of the motion.11 Firstly, for measuring lumbar flexion, the examiner instructed the patient to bend forward into full lumbar flexion, then the distance between the skin marks was measured. Then the examiner instructed the patient to bend backward as much as he can and the distance between skin marks was measured as lumbar extension. For measuring Lateral flexion, the distance from the tip of the index finger to the floor at maximal comfortable lateral flexion was measured.22
Sample size and statistical analysis
To avoid a type II error, a preliminary power analysis [power (1 − α error P) = 0.85, α = 0.05, effect size = 0.87, with a two-tailed for a comparison of 2 independent groups] determined a sample size of 25 for each group in this study. This effect size was calculated according after a pilot study of 12 participants (6 in each group) considering the pain intensity as a primary outcome. All statistical measures were performed using the Statistical Package for Social Science (SPSS) program version 20 for windows. Prior to final analysis, data were screened for normality assumption, and presence of outliers. Descriptive analysis using histograms with the normal distribution curve showed that the data were normally distributed and did not violate the parametric assumption for the pain, function, and lumbar flexion, extension, right, and left side bending. Additionally, testing for the homogeneity of covariance using Box's test revealed that there was no significant difference with p values of >0.05. Normality test of data using the Shapiro–Wilk test was used, that reflect the data was normally distributed for the pain, function, and lumbar flexion, extension, right, and left side bending. All these findings allowed the researchers to conduct parametric analysis. Therefore, a 2 × 2 mixed design MANOVA was used to compare the tested variables of interest at different tested groups and measuring periods. The alpha level was set at 0.05 (Table 1).
Table 1.
Demographic characteristics of patients in both groups, presented as mean (SD).a
| Variables | Control group | Study group |
|---|---|---|
| Age (year) | 37.27 ± 2.52 | 36.73 ± 2.52 |
| Weight (kg) | 72.73 ± 8.66 | 77.4 ± 10.23 |
| Height (cm) | 164.27 ± 8.71 | 162.2 ± 9.73 |
| Duration of illness (month) | 7.53 ± 3.27 | 8.0 ± 2.93 |
Significant level is set at alpha level <0.05.
Results
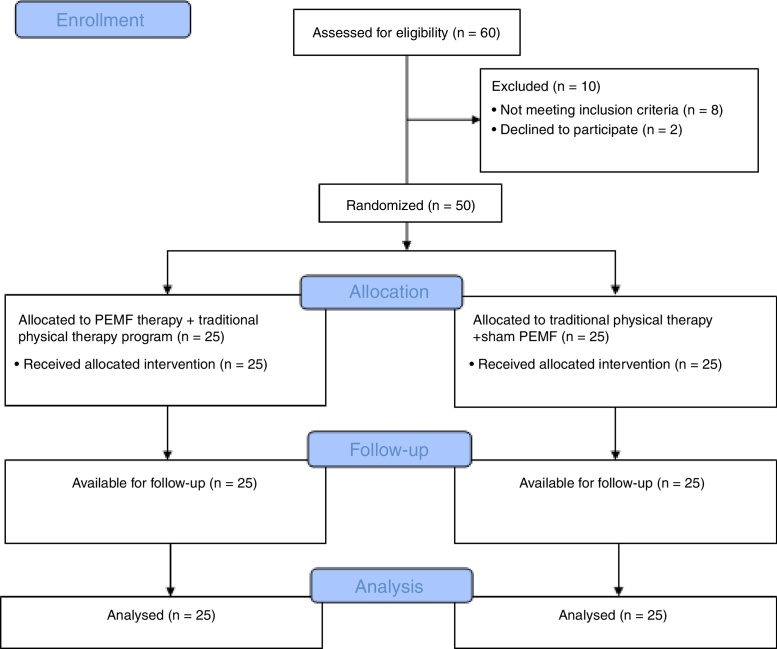
A total of 60 patients with chronic non-specific low back pain were eligible for inclusion, and 50 were randomized to study intervention (Fig. 1). The control group consisted of 25 patients (13 females and 12 males) who only received conventional physical therapy plus placebo PEMF for 4 weeks. The experimental group of 25 patients (12 females and 13 males) who received the same conventional physical therapy, in addition to PEMF for 4 weeks. All randomized patients completed the trial. Statistical analysis using mixed design MANOVA revealed that there were significant within subject effect (F = 40.391, p = 0.0001) and treatment*time effect (F = 10.51, p = 0.0001*). As well as, there was significant between subject effect (F = 1.626, p = 0.0001*). Table 2, Table 3 present descriptive statistics, within and between groups differences for the effects of interventions for the all dependent variables. Regarding between subject effects multiple pairwise comparisons revealed that there was significant difference of pain, function disability, and lumbar right, and left side bending and significant increase between both groups (p < 0.05) and this significant reduction in pain, disability, and lumbar right, and left side bending and significant increase in lumbar flexion and extension in favor to the experimental group.
Figure 1.
Flow chart of the randomized controlled trial in accordance with the CONSORT statement.
Table 2.
Descriptive characteristics for the all dependent variables for both groups at different training periods.
| Variables | Control group |
Study group |
||
|---|---|---|---|---|
| Pre | Post | Pre | Post | |
| Pain severity | 8.05 ± 7.93 | 4.11 ± 0.12 | 7.66 ± 8.23 | 5.24 ± 0.75 |
| Function disability | 50.67 ± 1.32 | 29.33 ± 7.92 | 48.73 ± 2.03 | 35.53 ± 4.59 |
| Flexion | 3.23 ± .77 | 6.1 ± 0.14 | 3.20 ± .67 | 4.8 ± 0.14 |
| Extension | 1.36 ± .44 | 2.83 ± 0.15 | 1.53 ± .51 | 1.9 ± 0.12 |
| Right side bending | 68.53 ± 3.89 | 17.40 ± 4.15 | 67.8 ± 2.96 | 24.87 ± 3.98 |
| Left side bending | 69.47 ± 4.02 | 17.87 ± 3.60 | 66.93 ± 3.10 | 25.73 ± 3.82 |
Values of all dependent variables are expressed as mean ± SD.
Table 3.
Between-group differences at 95% CI for the effects of interventions.
| Variables | Between-group differences |
|
|---|---|---|
| Mean difference (95% CI) | MCID | |
| Pain intensity | 1.52 (−0.34 to 3.35)a | 0.85 |
| Disability | 8.14 (6.5 to 9.96)a | 0.79 |
| ROM flexion | −1.27 (−1.09 to −1.45)a | 0.08 |
| ROM extension | −1.1 (−0.97 to −1.23)a | 0.06 |
| ROM right side bending | 8.2 (6.56 to 9.84)a | 0.74 |
| ROM left side bending | 10.4 (8.81 to 11.99)a | 0.71 |
CI: Confidence Interval, MCID: Minimal Clinically Important Difference, ROM; range of motion
The mean difference is significant at the 0.05 level.
Adverse events
There are no adverse events occurred during the study.
Discussion
This Randomized Controlled Trial (RCT) study was conducted to investigate the effects of pulsed electromagnetic field therapy with 50 Hz frequency, low intensity of 20 Gauss compared to conventional non-invasive treatment modalities in patients with chronic non-specific low back pain. The findings of the current study revealed that combination PEMF of 50 Hz frequency, with low intensity of 20 Gauss to the conventional physical therapy protocol improved pain intensity, disability and lumbar range of motion.
The different results obtained from the previous studies, may be referred to the different parameters applied. Many studies used high intensity and frequency of the PEMF, while others applied low parameters of the PEMF.4, 7 Another reason may lead to the difference in the outcome may be due to the inclusion of acute or chronic patients. The present study was conducted with a frequency of 50 Hz with low intensity 20 Gauss (2 mT) of (PEMF) which is the recommended parameters by the World Health Organization.22
These parameters were effective to decrease pain and disability as well as to increase range of motion.16 There is strong scientific evidence that the best therapeutic use of magnetic field for treating musculoskeletal disorders involves using pulsed magnetic field over 10 Gauss which support our result. Using specific extremely low frequency pulsed magnetic field, recent investigations have shown that increased analgesia. Rats exposed to a 5 mTMF displayed greater analgesic effects relative to rats in control, saline injection, morphine injection, and naloxone injection groups.23 In treating lumbar arthritis with 35–40 mT PEMFs, for 20 min daily for 20–25 days successfully treat back pain. Pain greatly diminished with the reduction of secondary neurologic symptoms.24
In controversy to our results, a study examined the efficacy of the magnetic field treatment combined with conservative treatment of musculoskeletal chronic low back pain symptoms in military service members, there was neither clinically or statistically significant difference between the groups in reducing pain.10 Some studies did not support the use of magnet therapy in musculoskeletal conditions. Cater et al.25 concluded that the use of a magnet of 1000 Gauss for reducing pain in carpal tunnel syndrome was no more effective than the use of the placebo device. Trock et al.26 treated knee osteoarthritis and cervical spondylosis with the pulsating electromagnetic field (10–20 Gauss), these authors reported a significant decline in pain and augmented functional performance of treated patients implementing the effectiveness of PEMF in relieving symptoms in patients with osteoarthritis.
In contrary to our results, Krammer et al.,6 found that applying PEMF of low-dose (0.03 mT), pulsating electromagnetic field with a frequency of 27.12 MHz, in combination with the routine physical therapy treatment add no benefit in patients acute non-specific LBP. Weintraub et al.27 studied the effect of simultaneous constant application of permanent magnets with magnetic field at the center of the device was 250 Gauss to the back and feet to disrupt and modulate neuropathic pain, but it did not demonstrate any statistical clinical benefit. They explained their result that current devices generated a magnetic field that is not deep enough to penetrate or influence the spinal nerves.
The use of opened sealed envelopes that contained a computer generated randomization card together with single blinding and no subjects drop out were some of the strengths of this study. However, the non guideline approaches and not using double blinding were considered as the weak points of this study.
One of the strengths of the current study in relation to other studies was using the sham device to control for the potential confounders as recommended by Nayback-Beebe et al.10 Future reviews are required to state the evidence for the recommended parameters of (PEMF) in treating patients with chronic low back pain.
Study limitation
There are some limitations of this study. Firstly, the treatment protocol that applied to both groups is non guideline approaches (in terms of using TENS and Ultrasound).1 Secondly, the lack of follow-up for patients with chronic low back pain for several periods post rehabilitation programs to evaluate the long term effect of the PEMF therapy in pain, disability, and ROM.
Clinical trials registry
Pan African Clinical Trials Registry (PACTR): PACTR201805003393380 (https://pactr.samrc.ac.za/TrialDisplay.aspx?TrialID=3393)
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors declare no potential conflicts of interest.
References
- 1.Sowden G., Hill J.C., Morso L., Louw Q., Foster N.E. Advancing practice for back pain through stratified care (STarT Back) Braz J Phys Ther. 2018;22(4):255–264. doi: 10.1016/j.bjpt.2018.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Louw Q.A., Morris L.D., Grimmer-Somers K. The prevalence of low back pain in Africa: a systematic review. BMC Musculoskelet Disord. 2007;8(1):105. doi: 10.1186/1471-2474-8-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mohamed R.A., AL-Disoky S., EL-Ghoul Y.M., Heissam K.S. Prevalence of low back pain and its effect on quality of life among patients attending Abokhalefa Center, Ismailia Governorate. Med J Cairo Univ. 2015;83(1):385–394. [Google Scholar]
- 4.Krath A., Klüter T., Stukenberg M. Electromagnetic transduction therapy in non-specific low back pain: a prospective randomised controlled trial. J Orthop. 2017;14(3):410–415. doi: 10.1016/j.jor.2017.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Foster N.E., Anema J.R., Cherkin D. Prevention and treatment of low back pain: evidence, challenges, and promising directions. Lancet. 2018;391(10137):2368–2383. doi: 10.1016/S0140-6736(18)30489-6. [DOI] [PubMed] [Google Scholar]
- 6.Krammer A., Horton S., Tumilty S. Pulsed electromagnetic energy as an adjunct to physiotherapy for the treatment of acute low back pain: a randomised controlled trial. N Z J Physiother. 2015;43:16–22. [Google Scholar]
- 7.Andrade R., Duarte H., Pereira R. Pulsed electromagnetic field therapy effectiveness in low back pain: a systematic review of randomized controlled trials. Porto Biomed J. 2016;1(5):156–163. doi: 10.1016/j.pbj.2016.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li S., Yu B., Zhou D., He C., Zhuo Q., Hulme J.M. Electromagnetic fields for treating osteoarthritis. Cochrane Database Syst Rev. 2013;(12):CD003523. doi: 10.1002/14651858.CD003523.pub2. [DOI] [PubMed] [Google Scholar]
- 9.Huang L.-Q., He H.-C., He C.-Q., Chen J., Yang L. Clinical update of pulsed electromag-netic fields on osteoporosis. Chin Med J. 2008;121:2095–2099. [PubMed] [Google Scholar]
- 10.Nayback-Beebe A.M., Yoder L.H., Goff B.J., Arzola S., Weidlich C. The effect of pulsed electromagnetic frequency therapy on health-related quality of life in military service members with chronic low back pain. Nurs Outlook. 2017;65(5S):S26–S33. doi: 10.1016/j.outlook.2017.07.012. [Epub 2017 Jul 20] [DOI] [PubMed] [Google Scholar]
- 11.Verma Y., Goyal M., Narkeesh Pain, range of motion and back strength in chronic mechanical low back pain before & after lumbar mobilisation. Int J Physioth Res. 2013;(3):48–57. [Google Scholar]
- 12.Thiese M.S., Hughes M., Biggs J. Electrical stimulation for chronic non-specific low back pain in a working-age population: a 12-week double blinded randomized controlled trial. BMC musculoskeldisord. 2013;14(1):117. doi: 10.1186/1471-2474-14-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brain V., Ashikage T., Braden C.F., Nancy J.Z. The effect of ultrasound and stretch on knee ligament Extensibility. JOSPT. 2000;30(6):341–347. doi: 10.2519/jospt.2000.30.6.341. [DOI] [PubMed] [Google Scholar]
- 14.Aure O.F., Nilsen J.H., Vasseljen O. Manual therapy and exercise therapy in patients with chronic low back pain: a randomized, controlled trial with 1-year follow-up. Spine. 2003;28(6):525–531. doi: 10.1097/01.BRS.0000049921.04200.A6. [DOI] [PubMed] [Google Scholar]
- 15.Hayden J.A., Van Tulder M.W., Tomlinson G. Systematic review: strategies for using exercise therapy to improve outcomes in chronic low back pain. Ann Intern Med. 2005;142(9):776–785. doi: 10.7326/0003-4819-142-9-200505030-00014. [DOI] [PubMed] [Google Scholar]
- 16.Atya A.M., Ahmed G.M. Pulsed magnetic field versus ultrasonic in treatment of patients with chronic mechanical low back pain. Bullet Facul Phys Ther. 2008;13:2. [Google Scholar]
- 17.Koes B.W., Van Tulder M.W., Thomas S. Diagnosis and treatment of low back pain. Brit Med J. 2006;332(7555):1430. doi: 10.1136/bmj.332.7555.1430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chiarotto A., Ostelo R.W., Turk D.C., Buchbinder R., Boers M. Core outcome sets for research and clinical practice. Braz J Phys Ther. 2017;21(2):77–84. doi: 10.1016/j.bjpt.2017.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chiarotto A., Boers M., Deyo R.A. Core outcome measurement instruments for clinical trials in nonspecific low back pain. Pain. 2018;159(3):481. doi: 10.1097/j.pain.0000000000001117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ramzy R. Stellenbosch University; Doctoral dissertation, Stellenbosch: 2008. Validation of the Arabic Version of the Oswestry Disability Index Developed in Tunisia for low back pain patients in the UAE. [Google Scholar]
- 21.Yen Y.R., Luo J.F., Liu M.L., Lu F.J., Wang S.R. The anthropometric measurement of Schober's test in normal Taiwanese population. Bio Med Res Intern. 2015 doi: 10.1155/2015/256365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ponte D.J., Jensen G.T., Kent B.E. A preliminary report on the use of McKenzie protocol versus Williams's protocol in the treatment of low back pain. JOSPT. 1984;6(2):130–139. doi: 10.2519/jospt.1984.6.2.130. [DOI] [PubMed] [Google Scholar]
- 23.Frontera C., García-Muñoz J.L., Carrillo A.E., Caneiro A. Spin state and magnetic interactions of Co3+ in PrBaCO2O5. J Magnet Magnet Mater. 2007;316(2):e731–e733. [Google Scholar]
- 24.Fleming J.L., Persinger M.A., Koren S.A. Magnetic pulses elevate nociceptive thresholds: comparisons with opiate receptor compounds in normal and seizure-induced brain-damaged rats. Electro Magnetobiol. 1994;13:67–75. [Google Scholar]
- 25.Carter R., Hall T., Aspy C.B., Mold J. The effectiveness of magnet therapy for treatment of wrist pain attributed to carpal tunnel syndrome. J Fam Pract. 2002;51(1):38–40. [PubMed] [Google Scholar]
- 26.Trock D.H., Bollet A.J., Dyer R.H., Jr., Fielding L.P., Miner W.K., Markoll R. A double-blind trial of the clinical effects of pulsed electromagnetic fields in osteoarthritis. J Rheumatol. 1993;20:456–460. [PubMed] [Google Scholar]
- 27.Weintraub M.I., Steinberg R.B., Cole S. The role of cutaneous magnetic stimulation in failed back syndrome. Semin Integ Med. 2005;3(3):101–103. [WB Saunders] [Google Scholar]