Abstract
Background
Targeting epitopes derived from neo-antigens (or “neo-epitopes”) represents a promising immunotherapy approach with limited off-target effects. However, most peptides predicted using MHC binding prediction algorithms do not induce a CD8 + T cell response, and there is a crucial need to refine the predictions to readily identify the best antigens that could mediate T-cell responses. Such a response requires a high enough number of epitopes bound to the target MHC. This number is correlated with both the peptide-MHC binding affinity and the number of peptides reaching the ER. Beyond this, the response may be affected by the properties of the neo-epitope mutated residues.
Methods
Herein, we analyzed several experimental datasets from cancer patients to elaborate better predictive algorithms for T-cell reactivity to neo-epitopes.
Results
Indeed, potent classifiers for epitopes derived from neo-antigens in melanoma and other tumors can be developed based on biochemical properties of the mutated residue, the antigen expression level and the peptide processing stage.
Among MHC binding peptides, the present classifiers can remove half of the peptides falsely predicted to activate T cells while maintaining the absolute majority of reactive peptides.
Conclusions
The classifier properties further highlight the contribution of the quantity of peptides reaching the ER and the mutation type to CD8 + T cell responses. These classifiers were then validated on neo-antigens obtained from other datasets, confirming the validity of our prediction.
Algorithm Availability: http://peptibase.cs.biu.ac.il/Tcell_predictor/ or by request from the authors as a standalone code.
Keywords: T cell activation, Machine Learning, Neoantigen, MHC-binding peptides
Introduction
CD8 T cell activation by either exogenous or endogenous epitopes is induced by binding of the T cell receptor to epitopes presented on host MHC class I proteins. Such peptides are usually the product of cytosolic protein or DRIP eventually digested by the proteasome [1]. The cellular TAP apparatus transfers cleaved peptides from the cytosol to the ER, where they can bind the MHC protein (for TAP dependent MHC binding). The probability of each of the above steps is often determined by the peptide linear sequence. This strongly simplifies the prediction of these stages by computational tools. We and others have developed multiple such tools for MHC binding, TAP binding and proteasomal cleavage [2, 3]. However, recent evidence suggests that most peptides predicted or measured to bind the MHC do not necessarily induce a T cell response when tested in vitro with a given patient’s T cells. Understanding the underlying reasons for this lack of optimal predictions represents an important challenge in T cell based anti-tumor treatments.
Progress in the understanding of immune components and their function has led to the implementation of successful immunotherapeutic approaches [4] based on checkpoint inhibitors or the adoptive transfer of tumor–specific T-cells. These strategies were shown to mediate regression of large tumor masses and remission in terminally-ill patients with different malignancies [5]. T-cells targeting cancer cells can recognize antigens which can be classified into two broad categories. The first class are non-mutated proteins or “tumor associated antigens” whose restricted tissue expression pattern probably allows for an immune response in patients [6]. The second class, on which we focus herein, are antigens derived from mutated proteins that could be recognized as foreign, commonly termed “neo-antigens”. These antigens have been shown to be relevant in efficient CPI (Check-point inhibitors) treatment and in T-cell based therapies [4]. Neoantigens can be used to identify tumor specific T-cells [7] or generate vaccines [8]. While advances in genomic sequencing have enabled a better characterization of DNA mutations and these antigens, an in silico approach to predict potent T-cell epitopes is lacking [9]. Experimental verifications are therefore needed [10], and these have revealed that most MHC-binding peptides are not recognized by T-cells. This could be the result of “holes” in the T cell repertoire or from properties of the peptides or the antigen from which they originated (e.g., protein expression level or biochemical properties of the peptides). Mass spectrometry can be applied for direct identification of epitopes [11], though the yield is often low and necessitates large amounts of tumor cells which are not always available.
Thus, we sought here to devise a novel algorithm based on experimentally acquired data to predict which MHC binding peptide would also induce a T cell response.
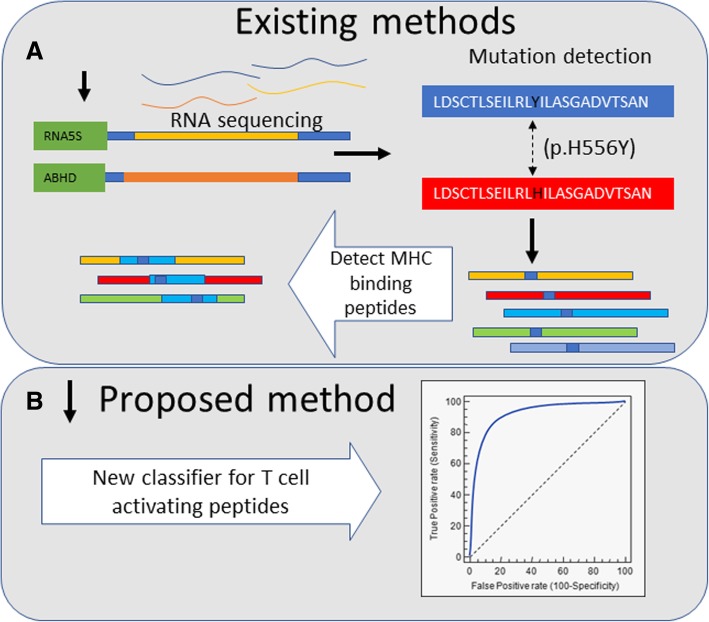
The most natural and expected prediction filter for neo-antigens is their binding to MHC, and multiple tools were developed to predict this binding [2, 3] with high precision and fidelity. Indeed, an accuracy of over 95% of predicting whether a peptide would induce a response can be obtained using only MHC binding [12, 13]. In parallel, methods were developed to study the immunogenicity of presented peptides. In contrast with epitope presentation, epitope immunogenicity is a function of the TCR recognition of MHC-I/epitope complex, and does not rely only on the peptide binding per se. Recent results show that large and aromatic R-chains in certain positions in the peptides can affect T cell activation [14]. Hydrophobicity has also been shown to induce immunogenicity, while polarity seems negatively correlated to immunogenicity. Multiple predictors were developed for the immunogenicity of peptides [15]. However, those are here shown to be of limited use in neoantigens, and there is currently a need for tools to predict the activation of T cells by MHC binding peptides. The novel algorithm presented here is intended to be used after the majority of peptides not binding MHC have been discarded using MHC binding predictions [16, 17] to improve on those (Fig. 1).
Fig. 1.
Existing methods and proposed new classifier (a) Current approaches for neo-antigen detection involve three main stages: RNA sequencing, detection of mutations in tumor cells and the computation of MHC binding peptides in such mutated regions. We propose a new stage (b) the detection among the MHC binding peptides of those that manage to induce a T cell response
Several groups have studied specific class I epitopes in neo-antigens and have also shown that epitopes from low expression proteins or from poorly preprocessed proteins do not induce a response [18, 19]. Other studies focused on the difference of the activation of the immune system between the W.T. and the mutant peptide by sequence property (with known algorithms), and involved other measures of the mutant peptide. Such methods report an Area Under Curve (AUC) of 0.63 [20].
Beyond MHC binding, the next candidate for affecting T cell response is the number of peptides reaching the Endoplasmic Reticulum (ER). This number determines the number of candidate MHC binding peptides, and in viral responses, we have shown it to be tightly related to the escape mutations [21]. We thus test the effect of the amount of such predecessors on the T cell response. Moreover, the response may be affected by the properties of the mutations producing the neo-antigen. Such properties were thus also added to the analysis.
Results
Correlation between neo-antigen features and T cell activation
In order to study the factors affecting T cell activation by presented peptides and to develop a classifier for such peptides, we analyzed the response of T-cell cultures derived from eight metastatic melanoma patients and published positive epitopes against sets of predicted-HLA binders as previously described [7] (further denoted the Me. Dataset). We also studied existing large scale datasets of T cell activating peptides, such as the Tantigen [22] dataset (further denoted the M.T. database). Finally, we tested three new melanoma patients studied in different experimental protocols to ascertain that our methods maintain their validity when applied to data produced by different experimental methodologies (Table 1).
Table 1.
Summary of the datasets used
| Source | HLA | Total no. of predicted samples | Confirmed Positive samples | Confirmed Negative samples |
|---|---|---|---|---|
| Melanoma (Me.) | A*02:01 | 485 | 35 | 450 |
| Melanoma Patient 1 |
A*02 B*18, B*35 C*07, C*05 |
187 | 7 | 180 |
| Melanoma Patient 2 |
A*11, A*23 B*14, B*41 |
56 | 3 | 53 |
| Melanoma Patient 3 |
A*02, A*24 B*15, B*38 |
68 | 3 | 65 |
| Tantigen [44] | mix | 24 | 0 |
For each dataset the name of the dataset, the number of positives and negatives epitopes in the data, and the HLA composition of the data are presented. The Melanoma patients were used for validation of the model and the results
Multiple tools were previously developed to predict T cell activation by MHC binding peptides [2, 3], the main one being the IEDB Class I Immunogenicity tool [23]. However, when we tested the quality of this predictor in the specific context of neo-antigen datasets, the results obtained were an AUC of 0.51 (i.e., random).
To develop an accurate predictor for T-cell activation, we computed seven measures per peptide, including the expression level of the specific gene in tumor tissues in this specific type of tumor (taken from gene expression measurements), four measures representing differences between the mutant candidate epitope and the non-mutated sequence, including size, hydrophobicity, charge, and polarity. The parameters of size, hydrophobicity, and charge represent the absolute value of the change. The last two measures are the candidate epitope cleavage and tap binding probabilities (Table 2).
Table 2.
First column is the score name, second column is the description of the score
| Feature name | Description | Notes |
|---|---|---|
| Expression level | The average expression level by cell line in melanoma tissue | http://www.ebi.ac.uk/ |
| Size difference | The absolute difference in size between the W.T. amino acid and the mutant | By Dalton units |
| Hydrophobicity | The absolute difference in hydrophobicity index between the W.T. amino acid and the mutant | Kyte J, Doolittle RF |
| Charge difference | The absolute difference in charge between the W.T. amino acid and the mutant | Values at ph = 7.4 |
| Polar change | Categorical variable for the polarity change between the W.T. amino acid the mutant | Values at ph = 7.4 |
| Cleavage score | Estimated cleavage probability of a full peptide. | Vider et al. |
| Tap score | Estimated TAP binding energy | Peters et al. |
Third column is a description of the score and the reference for the score
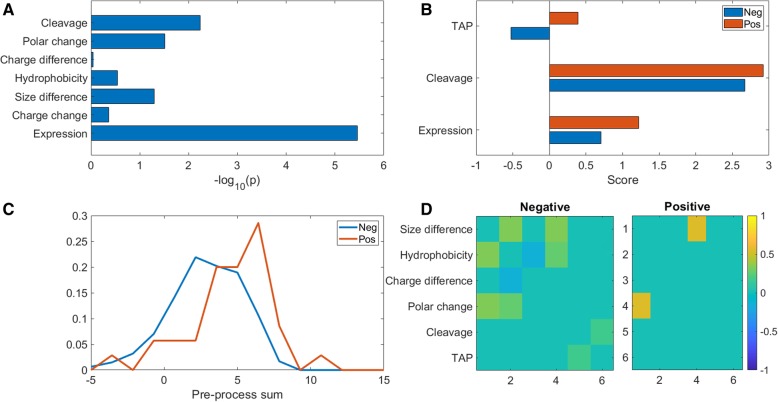
To test whether the measures above differed between peptide inducing and not inducing a T cell response, we computed the distance of the distributions of each measure in MHC binding peptides activating and not-activating T cells. We used the Kolmogorov Smirnov (KS) distance and found five features significantly different between activating and non-activating peptides (Fig. 2a), mainly expression level, TAP and cleavage scores. Thus, as expected the main element differentiating between epitopes that can and cannot induce a response is the number of peptides reaching the ER. To test that peptides inducing a T cell response have higher RNA expression levels and cleavage and TAP binding probability, the average of the positive and negative groups was computed for all three measures. We observed that the positive (T cell response inducing) peptides have higher averages on all scores (Fig. 2b). To further demonstrate this point, we computed the histogram of the sum of the three scores showing a clear difference between peptides inducing a response (Pos) and peptides not inducing one (Neg) in Fig. 2c.
Fig. 2.
a. -log 10 of p value for Kolmogorov Smirnov test for similarity between distribution of positive and negative peptides (peptides inducing and not inducing a T cell response). b. Average values for positive and negative groups of all measures with significant differences between groups. c. Histogram of sum of log expression, TAP binding score and cleavage score. One can clearly see a difference between the groups. d. Correlation heatmap of positive and negative groups for all measures. Only correlations with a p value below 0.005 were plotted Rows with no significant correlations were removed. The row and columns are the same properties
It is important to note that the MHC binding level was not included in the current analysis, since in all studied peptides (both positive and negative) were predicted to bind MHC. We repeated the analysis for a combined dataset containing the Me. and the epitopes from the Tantigen database of peptides from different tumors, with similar results (data not shown). We focused on MHC binding peptides and thus eliminated peptides that had low score/chance to bind to the specific MHC of this patient. It is worthy to note that including non-MHC binding peptides in the negative set would significantly increase the precision of a resulting classifier (e.g. Kim et al. [12]), but the goal of the current analysis is to add another layer of prediction beyond MHC binding, and thus such peptides were removed.
Beyond the number of peptides reaching the ER, we tested whether the properties of the mutation could affect the T cell response. While there were no significant differences in the average of each studied property, the correlation between these properties (listed in Table 2) differed between the positive and negative groups (i.e., peptides inducing/not inducing a response) - Fig. 2d.
Machine learning based classifier
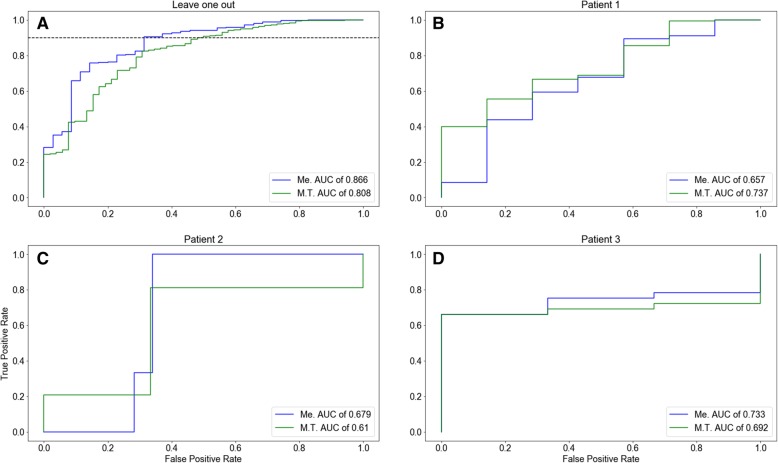
We have used the features above and produced two binary classifiers for the induction of a T cell response by neo-antigens for the Melanoma (Me.) and M.T. datasets. We also utilized the features in Table 2 as the input for a Random Forest classifier, developed with a Leave One Out approach. The resulting AUC was 0.86 (Fig. 3a) (the train AUC was 0.98) for the Me. classifier. For the M.T. classifier, a slightly lower AUC of 0.80 was obtained. However, as we show, when tested on datasets accumulated in a different experimental setup, both perform similarly. In both cases (Me. and M.T.), a 50% TN (True Negatives) and approximately 90% TP (True Positives) can be achieved in both classifiers (dashed line in Fig. 3a); thus, a fast pre-screening stage can be done with no loss of sensitivity. Such a prescreening stage can be highly useful for testing only half the peptide for T cell activation.
Fig. 3.
Subplots of ROC curves (a) Leave one out test for each one of the datasets. The AUC for the test on melanoma dataset is 0.86. b-d In the ROC curve for three different patients, the prediction was with the classifiers used to generate the test in (a). The horizonal dashed line in (a) indicates the threshold of 90% of the data to be true positive
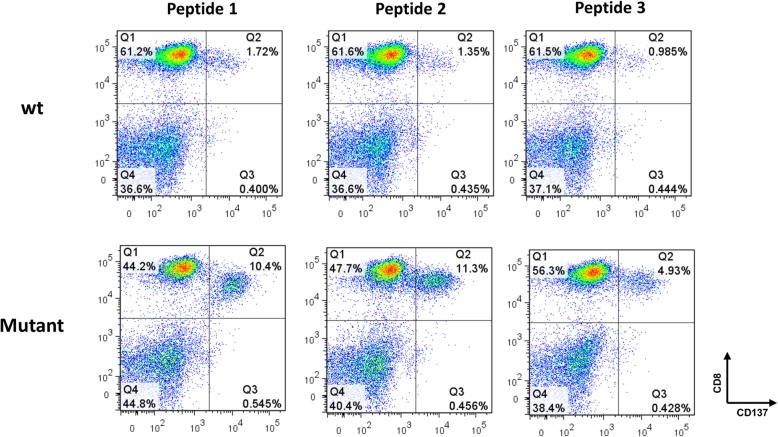
Finally, to verify our classifier, we screened exome data from 3 additional melanoma patients; the residues surrounding the amino acids resulting from non-synonymous mutations (total length of 25 aa) were screened to identify putative mutated epitopes that could trigger cognate T-cell activation. T cells from these patients were co-cultured overnight with EBV-transformed autologous B cells (B-LCL), pulsed with predicted reactive peptides. Following co-incubation, the upregulation of a T-cell activation marker as a surrogate for T-cell activation, CD137 (41BB) was determined on T cells by flow cytometry [24]. In Fig. 4, we show an example of the staining of TIL cultures derived from patient 1 that were previously incubated with 3 different predicted neo-peptides and their W.T. counterparts. We observed a significant upregulation of CD137 ranging between 4.9–11.3% in T-cells co-cultured with neoepitopes compared to background staining (around 1–2%) seen with W.T. peptides. These results exemplify the existence of T-cells specific for the predicted neoepitopes in TIL cultures.
Fig. 4.
Experimental validation of T cell response. TIL culture of patient 1 recognized 3 neoantigens, but not the corresponding wildtype peptides. Following pulsing with 10 μg/ml of 25-mer mutant or wt peptide overnight, EBV-transformed autologous B cells B-LCL were co-cultured with T-cells from TIL culture from patient 1. 16 h after the beginning of the co-culture, these cells were co-stained for CD137 (41BB) and CD8+ and analyzed by flow cytometry. The double positive population is indicated in quadrant Q2
We examined each patient individually (Fig. 3b-d), and obtained AUC values of 0.73, 0.67 and 0.65 for the three melanoma patients tested (Fig. 3). The origin of the large differences between this experiment and the first two datasets is the completely different experimental setups. The significant AUC in the validation is evidence for the robustness of our prediction to variation in the experimental settings.
To further test the applicability of the method, we computed for the test set in each sample different measures, including the AUC, the accuracy, F1, as well as the fraction of positive samples maintained when 50% of negatives were removed, and similarly the fraction of negative samples remaining when keeping 50% of positives (Table 3). One can clearly see that the vast majority of negative peptides can be removed, maintaining half the positive peptides, and similarly, the vast majority of positive peptides can be maintained, while removing 50% of negative peptides.
Table 3.
Classifier properties
| ME | M.T. | Pat 1 | Pat. 2 | Pat. 3 | |
|---|---|---|---|---|---|
| AUC | 0.809 | 0.868 | 0.657 | 0.679 | 0.733 |
| Fraction of Negatives kept when loosing 50% of positives | 0.101 | 0.051 | 0.322 | 0.000 | 0.246 |
| Fraction of positives kept when loosing 50% of negatives | 0.865 | 0.914 | 0.714 | 0.660 | 1.000 |
| Accuracy | 0.753 | 0.810 | 0.662 | 0.830 | 0.831 |
| F1 | 0.391 | 0.331 | 0.207 | 0.795 | 0.214 |
For each dataset we provide, the AUC and F1 value as well as the max accuracy on the test set. Similarly, we provide the fraction of negatives maintained when keeping 50% of negative and the fraction of positives when removing 50% of negatives
Discussion
CD8+ T-cells are undoubtedly central to the anti-tumor response against cancer whether when considering the impact of immune contexture [25], immune checkpoint or using adoptive transfer of tumor specific T-cells [26–29]. In this context, we and others have shown that a major target for anti-tumor T-cells are neo-epitopes derived from mutated antigens [30–32]. To detect such epitopes, one can employ a strategy encompassing 2 or possibly 3 mains steps:
-
A)
Identification of missense mutations using deep-sequencing,
-
B)
detection of MHC binding peptide appropriate for the host, and sometimes,
-
C)
prediction which of these peptides are properly processed by the Proteasome and bind TAP.
While highly precise algorithms exists for these three stages [2, 3, 33, 34], the resulting predicted MHC binding neo-peptides do not induce a CD8 T cell response in the majority of cases [4, 35, 36]. This can be due to the fact that either T-cells specific for these epitopes never existed to begin with, were eliminated during negative selection, underwent anergy or ceased to exist. Another possibility is that the epitope itself is not potent enough to generate a detectable reactivity.
In the present work, we have shown that it is possible to predict the immunogenicity of neoepitopes based on a fourth layer for this analysis, which is a prediction of the peptide passing the filters above that can induce such a T-cell response, using the properties of the protein and of the mutation. We propose to add this layer to peptide prediction pipelines to improve current methodologies.
A crucial element affecting the response is the expression level of the protein carrying the peptide. We have here shown that such an association is also critical for T cell stimulation/activation by neo-antigens [19]. Another important element is the charge difference of the mutation itself. Such a difference may represent the important effect of charge on T cell-epitope binding [37].
An alternative approach would be to optimize the MHC binding ignoring the other elements. It has been shown that immunogenicity is associated with strong MHC binding [38–40]. However, this approach limits the scope of the possible neo-antigen to excellent binders, and such binders are not always found for all HLA alleles.
While CD8+ T-cells are considered a central driver of the anti-tumor activity of the immune response, recent reports suggest that the adoptive transfer of CD4+ T-cells can lead to tumor cytotoxicity and clinical response, both in animal models and in patient studies [41]. There are currently limited prediction algorithms for MHC class II epitope presentation and pre-processing [42, 43].
In conclusion, we have developed and used herein a novel predictive algorithm that would enable the more precise identification of neo-epitopes that can facilitate CD8+ T-cell activation. We trust that this algorithm will contribute to the design of more precise and potent immunotherapies targeting neo-epitopes.
Methods
Datasets studied
Me. dataset: we previously described our experimental screening methodology [7]. Briefly, following exomic sequencing and RNA-Seq analysis of tumor samples collected from eight metastatic melanoma patients, we predicted candidate nine and ten amino acid peptides containing mutated residues derived from proteins with a minimum FPKM of 1 using the IEDB prediction algorithm available. T cells were tested for reactivity to T2 cells pulsed with predicted epitopes in cytokine release assays at an effector to target ratio of 1:1. Epitopes were deemed positives if yielding repetitive (n > 3) significant cytokine secretion of at least 3 times above background.
M.T. dataset: we download from the Tantigen database published neoepitope epitopes that were published in previous papers [22]. Those epitopes are from a wide variety of tissues, not limited only for melanoma tissue and not only for a specific MHC class. We combined the first dataset (Me.) and the epitopes from Tantigen to one dataset.
Prediction of neoantigens
Analysis of whole exome sequencing identified non-synonymous mutations from tumor and matched normal tissue. RNA-seq narrowed down the selection using threshold of expression level. The NetMHCpan predication algorithm was applied to further eliminate peptides by prediction of the Ic50 for to the specific HLA-molecules of the patient.
Detection of neoantigen specific –T-cells
For each candidate, neoantigen 2 × 10e6 EBV-transformed autologous B cells B-LCL were pulsed with 10 μg/ml of a 25-mer mutant peptide in a 96-well plate and incubated overnight at 37 °C and then washed twice. Co-culture assays were performed by adding 0.5 × 10e5 T cells to each well, followed by an overnight incubation at 37 °C. Reactivity of neo-antigen specific T cells was determined by CD137 expression measured by flow cytometric analysis. WT peptides served as control.
Statistical methods
We used the Mann Whitney score to compare the median values of each measure in the distributions. To further test for differences in the distribution not apparent in the median, we used the Kolmogorov-Smirnov Distance.
Learning and evaluation
The TCR binds to the epitope and to the MHC. The vast majority of presented epitopes do not induce a T cell` response. We developed a predictor of T cell activation for MHC binding peptidesbased on the biochemical character of the peptide presented and on the expression level of the antigen. We calculated the difference in the following parameters between the unmutated peptide. and the mutant at the mutation site: Charge, hydrophobicity, size, polarity.
We used a Random Forest algorithm (Matlab) with the following hyper-parameters 5000 estimators, min leaf size (minimum number of observations per tree leaf) 10, cost matrix (penalty) [[0, 0.15], [1, 0]]. To evaluate the performance, we used a leave one out method on the positives (the amount of the positives is much smaller than the negatives). In order to get accurate and unbiased results, we maximized the positives in the train). We had 35 positives samples and 450 negatives samples??that?? we??learned?? 35 times on 34 positives and 435 negatives and validated on the remains. The ROC curve is the score for the all data obtained from the validation method. The negative fraction in the test was 1:12.
The main measure we used to examine the performance is the area under the curve (also known as c-statistics) obtained from the surface under the curve describing the FPR (false positive rate) vs the TPR (true positive rate).
Acknowledgements
None.
Funding
No funding to declare.
Availability of data and materials
Code is available as server and standalone version.
Authors’ contributions
HB developed the code, SY, EMS, CJC performed the analysis on human patient samples. HB performed the analysis on the patients used for the ML development. YL led the research and YL and CJC wrote the manuscript. All authors read and approved the final manuscript.
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent for publication
All authors agreed to submit the current manuscript to JITC.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Cyrille J. Cohen, Email: cohency@biu.ac.il
Yoram Louzoun, Email: louzouy@math.biu.ac.il.
References
- 1.Yewdell JW, Reits E, Neefjes J. Making sense of mass destruction: quantitating MHC class I antigen presentation. Nat Rev Immunol [Internet]. 2003 [cited 2018 Jan 30];3(12):952–961. Available from: http://www.nature.com/doifinder/10.1038/nri1250 [DOI] [PubMed]
- 2.Singh SP, Mishra BN. Major histocompatibility complex linked databases and prediction tools for designing vaccines. Hum Immunol [Internet]. 2016 [cited 2017 Nov 29];77(3):295–306. Available from: http://www.sciencedirect.com/science/article/pii/S0198885915005650 [DOI] [PubMed]
- 3.Luo H, Ye H, Ng HW, Shi L, Tong W, Mendrick DL, et al. Machine Learning Methods for Predicting HLA-Peptide Binding Activity. Bioinform Biol Insights [Internet]. 2015 [cited 2017 Nov 29];9(Suppl 3):21–29. Available from: https://journals.sagepub.com/doi/pdf/10.4137/BBI.S29466. [DOI] [PMC free article] [PubMed]
- 4.Tran E, Robbins PF, Rosenberg SA. “Final common pathway” of human cancer immunotherapy: targeting random somatic mutations. Nat Immunol [Internet]. 2017 [cited 2017 Nov 29];18(3):255–262. Available from: http://www.nature.com/doifinder/10.1038/ni.3682 [DOI] [PMC free article] [PubMed]
- 5.Sharma P, Allison JP. The future of immune checkpoint therapy. Science [Internet]. 2015 [cited 2017 Nov 20];348(6230):56–61. Available from: https://science.sciencemag.org/content/348/6230/56.long. [DOI] [PubMed]
- 6.Restifo NP, Dudley ME, Rosenberg SA. Adoptive immunotherapy for cancer: harnessing the T cell response. Nat Rev Immunol [Internet]. 2012 [cited 2017 Nov 20];12(4):269–281. Available from: http://www.nature.com/doifinder/10.1038/nri3191 [DOI] [PMC free article] [PubMed]
- 7.Cohen CJ, Gartner JJ, Horovitz-Fried M, Shamalov K, Trebska-McGowan K, Bliskovsky V V, et al. Isolation of neoantigen-specific T cells from tumor and peripheral lymphocytes. J Clin Invest [Internet]. 2015 [cited 2017 Nov 21];125(10):3981–3991. Available from: https://www.jci.org/articles/view/82416. [DOI] [PMC free article] [PubMed]
- 8.Ott PA, Hu Z, Keskin DB, Shukla SA, Sun J, Bozym DJ, et al. An immunogenic personal neoantigen vaccine for patients with melanoma. Nature [Internet]. 2017 [cited 2017 Nov 21];547(7662):217–221. Available from: http://www.nature.com/doifinder/10.1038/nature22991 [DOI] [PMC free article] [PubMed]
- 9.The problem with neoantigen prediction. Nat Biotechnol [Internet]. 2017 [cited 2017 Nov 21];35(2):97–97. Available from: http://www.nature.com/doifinder/10.1038/nbt.3800 [DOI] [PubMed]
- 10.Vitiello A, Zanetti M. Neoantigen prediction and the need for validation. Nat Biotechnol [Internet]. 2017 [cited 2017 Nov 21];35(9):815–817. Available from: http://www.nature.com/doifinder/10.1038/nbt.3932 [DOI] [PubMed]
- 11.Kalaora S, Barnea E, Merhavi-Shoham E, Qutob N, Teer JK, Shimony N, et al. Use of HLA peptidomics and whole exome sequencing to identify human immunogenic neo-antigens. Oncotarget [Internet]. 2016 [cited 2018 Apr 29];7(5):5110–5117. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26819371. [DOI] [PMC free article] [PubMed]
- 12.Kim S, Kim HS, Kim E, Lee MG, Shin E, Paik S, et al. Neopepsee: accurate genome-level prediction of neoantigens by harnessing sequence and amino acid immunogenicity information. Ann Oncol [Internet]. 2018 [cited 2018 Apr 29];29(4):1030–1036. Available from: http://academic.oup.com/annonc/advance-article/doi/10.1093/annonc/mdy022/4817339 [DOI] [PubMed]
- 13.Eklund AC, Szallasi Z. Computational prediction of neoantigens: do we need more data or new approaches? Ann Oncol [Internet]. 2018 [cited 2018 Apr 29];29(4):799–801. Available from: https://academic.oup.com/annonc/article/29/4/799/4897993 [DOI] [PubMed]
- 14.Calis JJA, Maybeno M, Greenbaum JA, Weiskopf D, De Silva AD, Sette A, et al. Properties of MHC Class I Presented Peptides That Enhance Immunogenicity. Asquith B, editor. PLoS Comput Biol [Internet]. 2013 [cited 2017 Nov 29];9(10):e1003266. Available from: http://dx.plos.org/10.1371/journal.pcbi.1003266 [DOI] [PMC free article] [PubMed]
- 15.Chowell D, Krishna S, Becker PD, Cocita C, Shu J, Tan X, et al. TCR contact residue hydrophobicity is a hallmark of immunogenic CD8+ T cell epitopes. Proc Natl Acad Sci U S A [Internet]. 2015 [cited 2017 Nov 29];112(14):E1754–E1762. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25831525. [DOI] [PMC free article] [PubMed]
- 16.Liberman G, Vider-Shalit T, Louzoun Y. Kernel Multi Label Vector Optimization (kMLVO): A Unified Multi-Label Classification Formalism. [cited 2018 Jan 8]; Available from: https://link.springer.com/content/pdf/10.1007%2F978-3-642-44973-4_15.pdf
- 17.Jurtz V, Paul S, Andreatta M, Marcatili P, Peters B, Nielsen M. NetMHCpan-4.0: Improved Peptide-MHC Class I Interaction Predictions Integrating Eluted Ligand and Peptide Binding Affinity Data. J Immunol [Internet]. 2017 [cited 2018 may 6];199(9):3360–3368. Available from: http://www.jimmunol.org/content/199/9/3360.long. [DOI] [PMC free article] [PubMed]
- 18.Maman Y, Blancher A, Benichou J, Yablonka A, Efroni S, Louzoun Y. Immune-induced evolutionary selection focused on a single reading frame in overlapping hepatitis B virus proteins. J Virol [Internet]. 2011 [cited 2018 mar 20];85(9):4558–4566. Available from: https://jvi.asm.org/content/85/9/4558.long. [DOI] [PMC free article] [PubMed]
- 19.Daniel S, Caillat-Zucman S, Hammer J, Bach JF, van Endert PM. Absence of functional relevance of human transporter associated with antigen processing polymorphism for peptide selection. J Immunol [Internet]. 1997 [cited 2017 Nov 29];159(5):2350–2357. Available from: http://www.jimmunol.org/content/159/5/2350.long. [PubMed]
- 20.Bjerregaard AM, Nielsen M, Hadrup SR, Szallasi Z, Eklund AC, et al. MuPeXI: prediction of neo-epitopes from tumor sequencing data Abbreviations AUC Area under the curve MuPeXI Mutant peptide extractor and informer NGS Next generation sequencing NSCLC Non-small cell lung cancer RNA-seq RNA sequencing ROC Receiver operator characteristic SNV Single nucleotide variant VCF Variant call format VEP Variant effect predictor WXS Whole exome sequencing. Cancer Immunol Immunother [Internet]. 2001 [cited 2018 May 29];66:1123–1130. Available from: https://link.springer.com/content/pdf/10.1007%2Fs00262-017-2001-3.pdf
- 21.Maman Y, Blancher A, Benichou J, Yablonka A, Efroni S, Louzoun Y. Immune-induced evolutionary selection focused on a single reading frame in overlapping hepatitis B virus proteins. J Virol [Internet]. 2011 [cited 2018 Oct 4];85(9):4558–4566. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21307195. [DOI] [PMC free article] [PubMed]
- 22.Olsen LR, Tongchusak S, Lin H, Reinherz EL, Brusic V, Zhang GL. TANTIGEN: a comprehensive database of tumor T cell antigens. Cancer Immunol Immunother [Internet]. 2017 [cited 2018 Mar 20];66(6):731–735. Available from: http://link.springer.com/10.1007/s00262-017-1978-y [DOI] [PMC free article] [PubMed]
- 23.Tran E, Turcotte S, Gros A, Robbins PF, Lu Y, Dudley ME, et al. Cancer Immunotherapy Based on. Science (80- ) 2014;9(May):641–645. doi: 10.1126/science.1251102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tal Y, Yaakobi S, Horovitz-Fried M, Safyon E, Rosental B, Porgador A, et al. An NCR1-based chimeric receptor endows T-cells with multiple anti-tumor specificities. Oncotarget [Internet]. 2014 [cited 2018 Apr 29];5(21):10949–10958. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25431955. [DOI] [PMC free article] [PubMed]
- 25.Church SE, Galon J. Regulation of CTL Infiltration Within the Tumor Microenvironment. In Springer, Cham; 2017 [cited 2018 Jan 30]. p. 33–49. Available from: http://link.springer.com/10.1007/978-3-319-67577-0_3 [DOI] [PubMed]
- 26.Ankri C, Cohen CJ. Out of the bitter came forth sweet. Oncoimmunology [Internet]. 2014 [cited 2018 Jan 30];3(2):e27399. Available from: http://www.tandfonline.com/doi/abs/10.4161/onci.27399 [DOI] [PMC free article] [PubMed]
- 27.Tal Y, Yaakobi S, Horovitz-Fried M, Safyon E, Rosental B, Porgador A, et al. An NCR1-based chimeric receptor endows T-cells with multiple anti-tumor specificities. Oncotarget [Internet]. 2014 [cited 2018 Jan 30];5(21):10949–10958. Available from: http://www.oncotarget.com/fulltext/1919 [DOI] [PMC free article] [PubMed]
- 28.Shamalov K, Levy SN, Horovitz-Fried M, Cohen CJ. The mutational status of p53 can influence its recognition by human T-cells. Oncoimmunology [Internet]. 2017 [cited 2018 Jan 30];6(4):e1285990. Available from: https://www.tandfonline.com/doi/full/10.1080/2162402X.2017.1285990 [DOI] [PMC free article] [PubMed]
- 29.Eisenberg V, Shamalov K, Meir S, Hoogi S, Sarkar R, Pinker S, et al. Targeting Multiple Tumors Using T-Cells Engineered to Express a Natural Cytotoxicity Receptor 2-Based Chimeric Receptor. Front Immunol [Internet]. 2017 [cited 2018 Jan 30];8:1212. Available from: http://journal.frontiersin.org/article/10.3389/fimmu.2017.01212/full [DOI] [PMC free article] [PubMed]
- 30.Wirth TC, Kühnel F. Neoantigen Targeting—Dawn of a New Era in Cancer Immunotherapy? Front Immunol [Internet]. 2017 [cited 2018 Jan 30];8:1848. Available from: http://journal.frontiersin.org/article/10.3389/fimmu.2017.01848/full [DOI] [PMC free article] [PubMed]
- 31.Cohen CJ, Gartner JJ, Horovitz-Fried M, Shamalov K, Trebska-McGowan K, Bliskovsky V V., et al. Isolation of neoantigen-specific T cells from tumor and peripheral lymphocytes. J Clin Invest [Internet]. 2015 [cited 2018 Jan 30];125(10):3981–3991. Available from: https://www.jci.org/articles/view/82416 [DOI] [PMC free article] [PubMed]
- 32.Hu Z, Ott PA, Wu CJ. Towards personalized, tumour-specific, therapeutic vaccines for cancer. Nat Publ Gr [Internet]. 2017 [cited 2018 Jan 30]; Available from: https://www.nature.com/articles/nri.2017.131.pdf [DOI] [PMC free article] [PubMed]
- 33.Ginodi I, Vider-Shalit T, Tsaban L, Louzoun Y. Precise score for the prediction of peptides cleaved by the proteasome. Bioinformatics [Internet]. 2008 [cited 2017 Nov 29];24(4):477–483. Available from: https://academic.oup.com/bioinformatics/article-lookup/doi/10.1093/bioinformatics/btm616 [DOI] [PubMed]
- 34.Holzhütter Björn Peters H-G, Bulik S, Tampe R, van PM, Peters B, van Endert PM, et al. Epitope Precursors Predicting the TAP Transport Efficiency of Identifying MHC Class I Epitopes by Identifying MHC Class I Epitopes by Predicting the TAP Transport Efficiency of Epitope Precursors. J Immunol [Internet]. 2003 [cited 2017 Nov 29];171:1741–1749. Available from: http://www.jimmunol.org/content/171/4/1741 [DOI] [PubMed]
- 35.Bareli R, Cohen CJ. MHC-multimer guided isolation of neoepitopes specific T cells as a potent-personalized cancer treatment strategy. Oncoimmunology [Internet]. 2016 [cited 2018 Jan 30];5(7):e1159370. Available from: https://www.tandfonline.com/doi/full/10.1080/2162402X.2016.1159370 [DOI] [PMC free article] [PubMed]
- 36.Tran E, Ahmadzadeh M, Lu Y-C, Gros A, Turcotte S, Robbins PF, et al. Immunogenicity of somatic mutations in human gastrointestinal cancers. Science [Internet]. 2015 [cited 2018 Jan 30];350(6266):1387–1390. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26516200. [DOI] [PMC free article] [PubMed]
- 37.Zeng J, Treutlein HR, Rudy GB. Predicting sequences and structures of MHC-binding peptides: a computational combinatorial approach. J Comput Aided Mol Des [Internet]. 2001 [cited 2018 Jan 30];15:573–586. Available from: https://link.springer.com/content/pdf/10.1023%2FA%3A1011145123635.pdf [DOI] [PubMed]
- 38.Ghorani E, Rosenthal R, McGranahan N, Reading JL, Lynch M, Peggs KS, et al. Differential binding affinity of mutated peptides for MHC class I is a predictor of survival in advanced lung cancer and melanoma. Ann Oncol [Internet]. 2018 [cited 2018 Mar 20];29(1):271–279. Available from: https://academic.oup.com/annonc/article/29/1/271/4561624 [DOI] [PMC free article] [PubMed]
- 39.Saini SK, Rekers N, Hadrup SR. OUP accepted manuscript. Ann Oncol [Internet]. 2017 [cited 2018 Mar 20];28(suppl_12):xii3-xii10. Available from: http://fdslive.oup.com/www.oup.com/pdf/production_in_progress.pdf [DOI] [PubMed]
- 40.Parkhurst MR, Salgaller ML, Southwood S, Robbins PF, Sette A, Rosenberg SA, et al. Improved induction of melanoma-reactive CTL with peptides from the melanoma antigen gp100 modified at HLA-A*0201-binding residues. J Immunol [Internet]. 1996 [cited 2018 mar 20];157(6):2539–2548. Available from: http://www.ncbi.nlm.nih.gov/pubmed/8805655. [PubMed]
- 41.Vogelstein B, Papadopoulos N, Velculescu VE, Zhou S, Diaz LA, Kinzler KW, et al. Cancer genome landscapes. Science [Internet]. 2013 [cited 2018 mar 20];339(6127):1546–1558. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23539594. [DOI] [PMC free article] [PubMed]
- 42.Nielsen M, Lund O, Buus S, Lundegaard C. MHC class II epitope predictive algorithms. Immunology [Internet]. 2010 [cited 2018 mar 20];130(3):319–328. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20408898. [DOI] [PMC free article] [PubMed]
- 43.Hoze E, Tsaban L, Maman Y, Louzoun Y. Predictor for the effect of amino acid composition on CD4 + T cell epitopes preprocessing. J Immunol Methods [Internet]. 2013 [cited 2018 Mar 20];391(1–2):163–173. Available from: https://www.sciencedirect.com/science/article/pii/S0022175913000628 [DOI] [PMC free article] [PubMed]
- 44.Olsen LR, Tongchusak S, Lin H, Reinherz EL, Brusic V, Zhang GL. TANTIGEN: a comprehensive database of tumor T cell antigens. Cancer Immunol Immunother [Internet]. 2017 [cited 2017 Nov 29];66(6):731–735. Available from: http://link.springer.com/10.1007/s00262-017-1978-y [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Code is available as server and standalone version.