Sir,
The neuroanatomical basis of autism spectrum disorder (ASD) remains undeciphered. Neural system disconnection of the brain is hypothesized as causative. A substrate of this disconnection is agenesis of corpus callosum (AgCC). It is a very rare condition and is consistently reported with autism. However, cause–effect relationship remains to be established. A meta-analysis of 10 studies on magnetic resonance imaging (MRI) of 253 patients with AgCC and ASD showed a reduction in the size of corpus callosum.[1]
Corpus callosum is responsible for functional interaction between the hemispheres in cognitive processes such as executive functions, abstract reasoning, speed of processing, and problem solving. It is also important for the development of social competence, emotional maturity, and communication of emotions.[2] However, AgCC can be asymptomatic or present with one or more neurodevelopmental disorders.[3] While symptoms of autism have been reported in children with AgCC, syndromic ASD has never been reported. We report a case of a toddler with AgCC meeting Diagnostic and Statistical Manual 5 criteria for ASD.
CASE HISTORY
A 2-year-old male child was brought to the Child Psychiatry Out Patient Department of our tertiary care centre with symptoms of hyperactivity, impulsivity, and inability to speak. Often, he would be moving aimlessly, flapping his hands. He would be fidgety and would not engage in any play activity for long. He would not play with any child and would not respond to being called. He made poor eye contact and would be engaged in solitary activities of arranging and stacking up objects. He would never share his interests or excitement, would not point at things of his interest, nor would he look at things shown by his mother. He would indicate his needs by pulling his mother's hands and using them for pointing. He would demand immediate fulfilment of his needs, and in case of any delay, would start banging his head.
He was born of a nonconsanguineous marriage, with uneventful antenatal and postnatal course. His birth cry was delayed, with significantly difficult labor, but no other significant postnatal adverse events. He had delayed development in motor, speech, communication, and social domains.
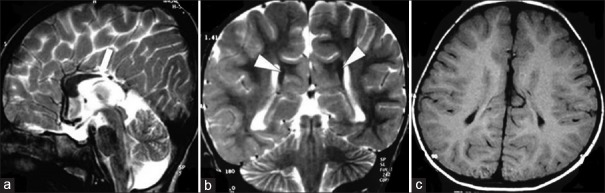
Currently, he was able to walk independently and would utter a few bi-syllables. He would not recognize his parents and would be hardly bothered by their absence. Childhood Autism Rating Scale score was 34, indicating moderate autism.[4] On Vineland Social Maturity Scale, he had the social age of 20 months, with Social Quotient (SQ) of 49, indicating moderate intellectual disability.[5] He had macrocephaly (head circumference was 51 cm, above WHO third percentile), but no other dysmorphic features were noticed. Macrocephaly prompted an evaluation for a structural neurological cause. T1 and T2-weighted MRI images showed partial agenesis of CC [Figure 1].
Figure 1.
Cranial MRI, (a) Sagittal T2W MRI showing absent posterior body and splenium of corpus callosum (arrow), cingulate gyrus and the medial hemispheric sulci reaching upto the 3rd ventricular surface. (b) Coronal T2WI showing Probst bundle indenting medial aspect of the body of lateral ventricles. (c) Axial T1WI showing parallel orientation of ventricles
He met the DSM 5 criteria for ASD, intellectual disability, and attention deficit hyperactivity disorder.[6] Absence of characteristic dysmorphic features and a normal karyotype ruled out genetic syndromes. A hearing evaluation was within normal limits, and he did not have any history of seizures. His thiamine and pyridoxine levels and thyroid profile were within normal limits. We could not find any genetic or toxic cause for AgCC in our case, nor could we identify any other independent risk factor for developmental delay. Hence, we considered a diagnosis of ASD and intellectual disability secondary to AgCC. We started risperidone at 0.5 mg/day for managing hyperactivity and repetitive motor behavior. Speech therapy, occupational therapy, and behavioral therapy were also started. The child is on regular follow-up in our centre: his hyperactivity is currently manageable, and he is being engaged in multiple behavioral and educational interventions.
DISCUSSION
Our patient had socio-communicative deficits with stimming behavior characteristic of ASD before 3 years of age, which is considered to be a diagnostic hallmark of syndromic ASD. He also had moderate intellectual disability. Presence of partial AgCC could be understood as the proximal risk factor for the autistic symptoms. The absence of posterior body can explain his moderate autism as this is the region vital for self-referential and social cognitive development.[7] Presence of Probst bundle is further evidence of AgCC, as the white matter tract, which has failed to form interhemispheric connection, has instead remained in the longitudinal orientation. This structural evidence of partial disconnection of the corpus callosum can be considered causative of ASD symptoms in the index case.
Symptoms of ASD have been reported in AgCC on parent-reported scales and screening instruments; syndromic ASD has never been reported in children.[8,9] Only two adult cases with syndromic ASD in association with AgCC have been reported till date, which includes “Rainman” Kim Peek.[7] AgCC associated with extracallosal brain lesions is associated with poor prognosis and has an adverse impact on clinical outcome. ASD with AgCC is associated with a partial/total reduction of corpus callosum volume; structural dysconnectivity dysfunction is hypothesized to be causal for ASD.[7]
Our case is unique by the fact that the diagnosis of ASD and comorbid intellectual disability has been made with AgCC in early childhood, reinforcing the structural etiological role of corpus callosum. Recent neuroimaging findings have corroborated the role of the corpus callosum in sociocognitive and self-referential deficits in autism. AgCC is being increasingly understood as a neurological model for deficits of autism. However, exact mechanisms still remain to be identified.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Frazier TW, Hardan AY. A meta-analysis of the corpus callosum in autism. Biol Psychiatry. 2009;66:935–41. doi: 10.1016/j.biopsych.2009.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Paul LK, Corsello C, Kennedy DP, Adolphs R. Agenesis of the corpus callosum and autism: A comprehensive comparison. Brain. 2014;137:1813–29. doi: 10.1093/brain/awu070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Margari L, Palumbi R, Campa MG, Operto FF, Buttiglione M, Craig F, et al. Clinical manifestations in children and adolescents with corpus callosum abnormalities. J Neurol. 2016;263:1939–45. doi: 10.1007/s00415-016-8225-x. [DOI] [PubMed] [Google Scholar]
- 4.Schopler E, Reichler RJ, Renner BR. Los Angeles: Western Psychological Services Inc; 1988. The Childhood Autism Rating Scale (CARS) [Google Scholar]
- 5.Doll EA. Circle Pines, Minnesota: American Guidance Services Inc; 1965. Vineland Social Maturity Scale. [Google Scholar]
- 6.American Psychiatric Association. Washington, D.C: American Psychiatric Association; 2013. Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM5) [Google Scholar]
- 7.Lombardo MV, Chakrabarti B, Lai MC, Baron-Cohen S MRC AIMS Consortium. Self-referential and social cognition in a case of autism and agenesis of the corpus callosum. Mol Autism. 2012;3:14. doi: 10.1186/2040-2392-3-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Badaruddin DH, Andrews GL, Bölte S, Schilmoeller KJ, Schilmoeller G, Paul LK, et al. Social and behavioral problems of children with agenesis of the corpus callosum. Child Psychiatry Hum Dev. 2007;38:287–302. doi: 10.1007/s10578-007-0065-6. [DOI] [PubMed] [Google Scholar]
- 9.Lau YC, Hinkley LB, Bukshpun P, Strominger ZA, Wakahiro ML, Baron-Cohen S, et al. Autism traits in individuals with agenesis of the corpus callosum. J Autism Dev Disord. 2013;43:1106–18. doi: 10.1007/s10803-012-1653-2. [DOI] [PMC free article] [PubMed] [Google Scholar]