Abstract
Objectives
To compare outcomes of total knee replacement (TKR) and total hip replacement (THR) for individuals with RA and OA.
Methods
We performed a cohort study using routinely collected data. Oxford Knee Score, Oxford Hip Score, and EuroQol 5-dimension 3-level (EQ-5D-3L) questionnaires were collected before and 6 months after surgery. Multivariable regressions were used to estimate the association between diagnosis and post-operative scores after controlling for pre-operative scores and patient characteristics.
Results
Study cohorts included 2070 OA and 142 RA patients for TKR and 2030 OA and 98 RA patients for THR. Following TKR, the median Oxford Knee Score was 37 [interquartile range (IQR) 29–43] for OA and 36 (27–42) for RA while the median EQ-5D-3L was 0.76 (0.69–1.00) and 0.69 (0.52–0.85), respectively. After THR, the Oxford Hip Score was 42 (IQR 36–46) for OA and 39 (30–44) for RA while the EQ-5D-3L was 0.85 (0.69–1.00) and 0.69 (0.52–1.00), respectively. The estimated effect of RA, relative to OA, on post-operative scores was −0.05 (95% CI −1.57, 1.48) for the Oxford Knee Score, −0.09 (−0.13, −0.06) for the EQ-5D-3L following TKR, −1.35 (−2.93, −0.22) for the Oxford Hip Score, and −0.08 (−0.12, −0.03) for the EQ-5D-3L following THR.
Conclusion
TKR and THR led to substantial improvements in joint-specific scores and overall quality of life. While diagnosis had no clinically meaningful effect on joint-specific outcomes, improvements in general quality of life were somewhat less for those with RA, which is likely due to the systemic and multijoint nature of rheumatoid disease.
Keywords: rheumatoid arthritis, osteoarthritis, outcome measures, quality of life, surgery
Rheumatology key messages
Individuals with osteoarthritis and rheumatoid arthritis achieve substantial health gains from knee and hip replacement.
Individuals with osteoarthritis and rheumatoid arthritis get similar improvements in joint-specific outcomes.
Gains in overall quality of life are somewhat less for those with rheumatoid arthritis.
Introduction
The most common indication for total knee replacement (TKR) and total hip replacement (THR) is OA. OA is the clinical syndrome of failure of the joint [1], and joint replacement is considered when non-surgical alternatives have failed. In such cases, TKR and THR typically relieve pain and improve function, leading to substantial gains in an individual’s quality of life [2, 3]. Consequently, the procedures are considered cost effective, with their costs justified by the expected health gains for the individuals receiving them [2, 3].
TKR and THR are also performed on individuals with inflammatory rheumatic diseases. RA is the most common of these. RA can destroy cartilage and erode bone and the involvement of many joints is common [4]. As with OA, pain, loss of function and damaged structure are all indications for joint replacement for those with RA [4]. However, while pain remains the foremost indication, function and structure play an increased role. Guidelines promote referral for early surgical opinion where persistent pain, worsening joint function, progressive deformity or persistent localized synovitis have not responded optimally to non-surgical treatment [5].
Whether individuals with RA achieve equivalent gains from undergoing TKR and THR as those with OA is not yet known. Given multiple joint involvement, systemic comorbidity and polypharmacy [4], it is plausible that outcomes for individuals with RA may be worse than for those with OA. Moreover, as it is recommended that hip replacement should generally precede knee replacement for those with RA [6], the relationship between RA and outcomes could differ depending on the procedure.
The success of TKR and THR have traditionally been measured by implant survival. There is, however, an increased awareness that patient-reported outcome measures (PROMs) provide a more appropriate indicator of effectiveness and are more closely tied to the reasons for performing surgery [7]. The Oxford Knee Score (OKS) and Oxford Hip Score (OHS) are joint-specific PROMs for knee and hip replacement, respectively, with questions on both pain and function [8, 9]. Meanwhile, the EuroQol 5-dimension 3-level (EQ-5D-3L) questionnaire measures overall health-related quality of life [10].
In this study we compared the effectiveness of TKR and THR for individuals with RA and OA in terms of both joint-specific measures and overall health-related quality of life.
Methods
Setting, data sources and study participants
Primary care, inpatient hospital and PROMs data from the National Health Service (NHS) in England informed this study. The Clinical Practice Research Datalink (CPRD) provided primary care records and demographic details. Around 7% of the UK population is included in the CPRD, with those included broadly representative of the general population [11]. The Hospital Episode Statistics Admitted Patient Care (HES APC) provided inpatient hospital data. The HES APC contains data on all NHS-funded hospital admissions in England and includes both clinical and demographic information [12]. The NHS provided routinely collected PROMs with OKS and EQ-5D-3L data from patients receiving TKR and OHS and EQ-5D-3L data for those undergoing THR. These PROMs are completed before and ∼6 months after surgery, with all patients undergoing TKR and THR funded by the English NHS invited to participate [13]. Ethical approval for the study was granted by the CPRD Independent Scientific Advisory Committee.
We established knee-related and hip-related diagnosis cohorts based on clinical codes within the CPRD records. Individuals entered the knee-related cohort if they had an incident (newly recorded) diagnosis of RA or knee OA. Similarly, individuals entered the hip-related cohort if they had an incident diagnosis of RA or hip OA in their primary care records. Where an individual had both a diagnosis of both RA and OA, RA was taken as the index diagnosis. Individuals could be in both the knee-related and hip-related cohorts.
HES APC records were then linked to these cohorts. TKR or THR following the index diagnosis was identified using the HES APC on the basis of procedure codes. Individuals who received bilateral surgery, where both the left and right knee joints were replaced simultaneously or staged, were excluded from the analysis. If an individual received a second TKR or THR following diagnosis, only the first was included in the analysis.
The HES PROMs were then linked to the identified TKR and THR procedures in the HES APC. Individuals were included if they had complete scores recorded for OKS/OHS and EQ-5D-3L before and after surgery. We assessed the potential impact of this decision by comparing the characteristics of individuals missing and not missing PROM scores.
Measurement of variables
The main exposure of interest was patient diagnosis of RA or OA and these diagnoses were identified using CPRD records. The date of a procedure recorded in the HES APC was used to identify the year of surgery and, given an individual’s year of birth recorded in CPRD, age at surgery was inferred. Gender was obtained from CPRD records. Diagnosis codes in the HES APC were used to identify conditions included in the Royal College of Surgeons Charlson score [14]. This score provides a summary measure of comorbidities. RA was omitted from calculations of the Charlson score, as it was considered separately in the analysis. Indices of Multiple Deprivation (IMD) quintiles were based on postcodes recorded in the CPRD. IMD quintiles provide a measure of socio-economic status, with 5 implying the highest level of deprivation. BMI and smoking status were taken from the CPRD. The values of BMI and smoking status closest to surgery were identified and included if they were recorded in the year leading up to surgery.
PROMs
The OKS and OHS are joint-specific questionnaires whose scores range from 0 (worst) to 48 (best) [15]. The EQ-5D-3L questionnaire covers general health-related quality of life, with questions covering five dimensions with three possible response levels. The dimensions include mobility, self-care, usual activities, pain/discomfort and anxiety/depression. Responses are classified as either no problems, some problems or extreme problems [10]. The combination of these dimensions and responses can be summarized as an index value, which ranges from −0.59 (worst) to 1 (best) after applying preference-based utility weights obtained from the general UK population [16].
Statistical methods
Comparing patient characteristics
The characteristics of those with RA and OA and those with and without missing PROMs were compared. Standardized mean difference was used to assess whether there was balance in a characteristic, with a mean difference <0.1 indicating a negligible difference in the mean of a covariate between groups [17].
Comparing observed PROMs
The OKS/OHS and EQ-5D-3L index reported by individuals with OA and RA before and after TKR and THR were compared, with both the absolute change in scores and the percentage of potential change (PoPC) achieved calculated. The PoPC accounts for differences in baseline scores by summarizing how much an individual has improved (or worsened) relative to how much they potentially could have improved (or worsened) [18]. The PoPC ranges between −100% (i.e. an individual has worsened to the lowest possible score) and 100% (i.e. an individual has improved to the best possible score), with a value of 0% indicating no change.
As well as considering the EQ-5D-3L index, changes between pre- and post-operative time points in individual dimensions and the overall profile were summarized by diagnosis. Each dimension was either better, had no change or was worse following surgery. Meanwhile, the overall profile was either better (i.e. at least one dimension had improved, with none worse), had a mixed change (i.e. some dimensions had improved but others had worsened), had no change or was worse (i.e. at least one dimension had worsened, with none improving).
Estimating the association between RA, relative to OA and post-operative PROMs
Ordinary least squares regressions were used to assess the impact of diagnosis (RA or OA) on post-operative scores, controlling for both pre-operative scores and patient characteristics. The outcome variable was post-operative score. Univariable models with only diagnosis and multivariable models with age, gender, Charlson score, IMD quintile, BMI, smoking status and pre-operative score also included as explanatory variables were estimated. Restricted cubic splines were used to incorporate non-linearity in continuous variables where the Bayesian information criterion (BIC) was lower than that of a model with a linear relationship fitted, with BIC also used to decide on how many knots to include if a non-linear relationship was incorporated [19]. As there were few study participants with multiple comorbidities, the Charlson score was dichotomized to 0 and 1+.
There were missing data for three of the explanatory variables included in the analysis: IMD, BMI and smoking status. While IMD was missing for only two participants, BMI and smoking status were missing in higher proportions ranging from 39% to 58% among the various cohorts. We used multiple imputation to account for these missing values. This was based on the assumption that data were missing at random, where the probability of data being missing does not depend on the unobserved data, conditional on the observed data [20]. Explanatory variables and outcomes were used to impute 50 datasets.
Pooled model coefficients and corresponding 95% CIs were calculated using Rubin’s rules. The coefficients reflect the expected change in the outcome variable based on a given change in the explanatory variable, while other explanatory variables are fixed. The coefficients for diagnosis, for example, reflect the estimated effect of RA relative to OA on post-operative score, controlling for differences in pre-operative scores and patient characteristics.
Results
Study participants
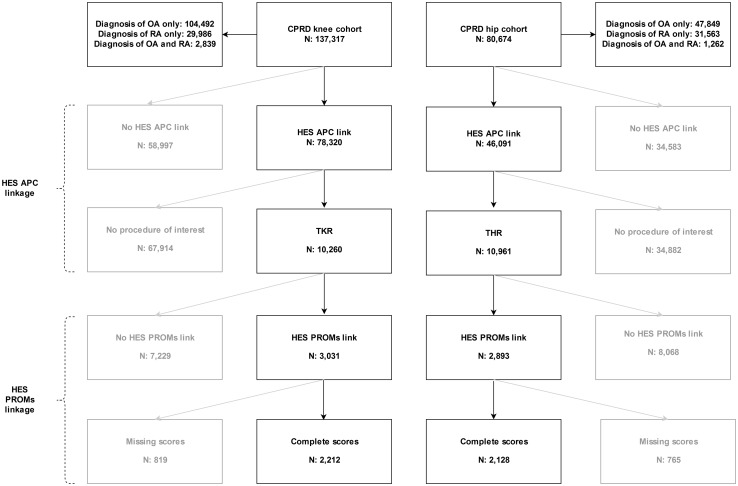
A total of 2212 (2070 with OA and 142 with RA) and 2128 (2030 with OA and 98 with RA) individuals were included in the study cohorts for TKR and THR, respectively. The study inclusion flow chart is shown in Fig. 1 and the baseline (pre-operative) characteristics of study participants are summarized in Table 1. Further details on those with missing data are provided in Supplementary Figures S2 and S3 and Supplementary Table S1, available at Rheumatology online.
Fig. 1.
Study inclusion flow chart
Table 1.
Patient characteristics
| Characteristics | TKR | THR | ||||
|---|---|---|---|---|---|---|
| OA | RA | SMD | OA | RA | SMD | |
| N | 2070 | 142 | 2030 | 98 | ||
| Age, years, median (IQR) | 70 (64–76) | 69 (62–75) | 0.16 | 69 (63–76) | 70 (61–76) | 0.01 |
| Gender, female, n (%) | 1113 (54) | 87 (61) | 0.15 | 1145 (56) | 75 (77) | 0.44 |
| Charlson score, n (%) | 0.13 | 0.03 | ||||
| 0 | 1466 (71) | 92 (65) | 1507 (74) | 74 (76) | ||
| 1+ | 604 (29) | 50 (35) | 523 (26) | 24 (25) | ||
| BMI, median (IQR) | 30 (27–35) | 30 (27–35) | 0.03 | 29 (25–32) | 28 (25–31) | 0.02 |
| BMI missing, n (%) | 987 (48) | 73 (51) | 0.07 | 1048 (52) | 57 (58) | 0.13 |
| Smoking status, n (%) | 0.28 | 0.21 | ||||
| Non-smoker | 606 (29) | 30 (21) | 559 (28) | 21 (21) | ||
| Ex-smoker | 576 (28) | 39 (28) | 496 (24) | 24 (25) | ||
| Current smoker | 82 (4) | 14 (10) | 126 (6) | 11 (11) | ||
| Missing | 806 (39) | 59 (42) | 849 (42) | 42 (43) | ||
| IMD quintile, n (%) | 0.09 | 0.29 | ||||
| 1 | 471 (23) | 33 (23.2) | 551 (27) | 25 (26) | ||
| 2 | 536 (26) | 36 (25.4) | 509 (25) | 23 (24) | ||
| 3 | 497 (24) | 32 (22.5) | 488 (24) | 18 (18) | ||
| 4 | 380 (18) | 25 (17.6) | 339 (17) | 17 (17) | ||
| 5 | 185 (9) | 16 (11.3) | 142 (7) | 15 (15) | ||
| Missing | 1 (0) | 0 (0) | 1 (0) | 0 (0) | ||
Comparison of the characteristics of individuals, split by diagnosis of OA and RA recorded prior to and following TKR and THR.
SMD: standardized mean difference.
Association between RA and post-operative PROMs
OKS following TKR
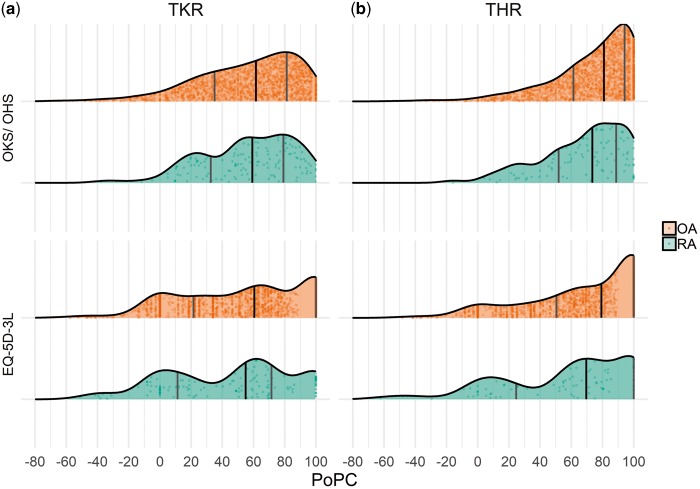
Individuals with OA improved in the OKS after TKR from a median of 19 [interquartile range (IQR) 14–24] to 37 (29–43), a change of 16 (9–23) and a PoPC realized of 62% (35% to 81%). Meanwhile, individuals with RA improved in the OKS from 15 (IQR 10–22) to 36 (27–42), a change of 18 (11–24) and a PoPC realized of 59% (33% to 79%). See Table 2 for a summary of the OKS by diagnosis and Fig. 2 for the distribution of the PoPC by diagnosis. After controlling for differences in pre-operative score and patient characteristics, the estimated effect of RA relative to OA on post-operative OKS was −0.05 (−1.57–1.48), as shown in Table 4.
Table 2.
Joint-specific (OKS/OHS) and generic (EQ-5D-3L utility index) PROMs according to diagnosis
| Diagnosis | Pre-operative, median (IQR) | Post-operative, median (IQR) | Change, median (IQR) | PoPC, median (IQR) | |
|---|---|---|---|---|---|
| TKR | |||||
| OKS | OA | 19 (14–24) | 37 (29–43) | 16 (9– 23) | 62 (35–81) |
| RA | 15 (10–22) | 36 (27–42) | 18 (11–24) | 59 (33–79) | |
| EQ-5D-3L index | OA | 0.59 (0.12–0.69) | 0.76 (0.69–1.00) | 0.31 (0.07–0.59) | 61 (21–100) |
| RA | 0.16 (0.00–0.65) | 0.69 (0.52–0.85) | 0.31 (0.07–0.60) | 55 (11–71) | |
| THR | |||||
| OHS | OA | 18 (12–24) | 42 (36–46) | 23 (16–29) | 81 (61–94) |
| RA | 12 (7–20) | 39 (30–44) | 24 (15–31) | 73 (52–89) | |
| EQ-5D-3L index | OA | 0.52 (0.06–0.66) | 0.85 (0.69–1.00) | 0.41 (0.20–0.74) | 79 (50–100) |
| RA | 0.06 (−0.07–0.59) | 0.69 (0.52–1.00) | 0.47 (0.13–0.76) | 70 (25–100) |
The OKS and OHS range from 0 to 48 while the EQ-5D-3L index ranges from −0.59 to 1, with higher scores being better for both.
Fig. 2.
Distribution of percentage of potential change
Kernel density distributions with points showing observed data and solid vertical lines denoting the 25th percentile, 50th percentile (median) and 75th percentile from the observed data.
Table 4.
Estimated effects of RA, relative to OA, on post-operative PROMs
| Measure | TKR | THR | ||
|---|---|---|---|---|
| Univariable model | Multivariable model | Univariable model | Multivariable model | |
| OKS/ OHS | −1.65 (−3.27, −0.03) | −0.05 (−1.57, 1.48) | −3.48 (−5.16, −1.81) | −1.35 (−2.93, 0.22) |
| EQ-5D-3L index | −0.13 (−0.17, −0.09) | −0.09 (−0.13, −0.06) | −0.14 (−0.19, −0.09) | −0.08 (−0.12, −0.03) |
Data presented as coefficients with 95% CIs. Dependent variables were post-operative scores. In addition to diagnosis (RA or OA), multivariable models also included age at surgery, gender (male or female), Charlson score, IMD quintile, pre-operative score for the corresponding dependent variable, BMI and smoking status as explanatory variables.
EQ-5D-3L following TKR
Regarding overall health-related quality of life, 75% of those with OA had a better EQ-5D-3L profile following TKR, 8% had a mixed change, 10% had no change and 6% were worse than before surgery. Their EQ-5D-3L index improved from 0.59 (IQR 0.12–0.69) to 0.76 (0.69–1.00), a mean change of 0.31 (0.07–0.59) and a PoPC of 61% (21% to 100%). In total, 67% of those with RA had a better EQ-5D-3L profile following TKR, 15% had a mixed change, 8% had no change, and 11% were worse. Their EQ-5D-3L index improved from 0.16 (IQR −0.00–0.65) to 0.69 (0.52–0.85) for a change of 0.31 (0.07–0.60) and a PoPC of 55% (11% to 71%). Table 2 reports a summary of EQ-5D-3L indices and Table 3 reports the change in dimension scores by diagnosis, with further details on the dimension scores given in Supplementary Table S2, available at Rheumatology online. While both individuals with OA and those with RA achieved substantial improvements in their usual activities, pain/discomfort and mobility dimensions, those with RA were less likely to report no problems on these dimensions following surgery compared with those with OA. After controlling for differences in pre-operative score and patient characteristics, the estimated effect of RA relative to OA on the post-operative EQ-5D-3L index was −0.09 (95% CI −0.13, −0.06), as detailed in Table 4.
Table 3.
Change in EQ-5D-3L dimension scores by diagnosis
| Characteristics | TKR | THR | ||
|---|---|---|---|---|
| OA, n (%) | RA, n (%) | OA, n (%) | RA, n (%) | |
| Dimensions | ||||
| Usual activities | ||||
| Better | 977 (47) | 56 (39) | 1282 (63) | 55 (56) |
| No change | 1019 (49) | 80 (56) | 712 (35) | 39 (40) |
| Worse | 74 (4) | 6 (4) | 36 (2) | 4 (4) |
| Anxiety/ depression | ||||
| Better | 480 (23) | 38 (27) | 638 (31) | 43 (44) |
| No change | 1460 (71) | 86 (61) | 1318 (65) | 49 (50) |
| Worse | 130 (6) | 18 (13) | 74 (4) | 6 (6) |
| Pain/ discomfort | ||||
| Better | 1242 (60) | 88 (62) | 1540 (76) | 72 (73) |
| No change | 789 (38) | 49 (35) | 471 (23) | 23 (23) |
| Worse | 39 (2) | 5 (4) | 19 (1) | 3 (3) |
| Mobility | ||||
| Better | 993 (48) | 44 (31) | 1190 (59) | 35 (36) |
| No change | 1046 (51) | 96 (68) | 824 (41) | 61 (62) |
| Worse | 31 (1) | 2 (1) | 16 (1) | 2 (2) |
| Self-care | ||||
| Better | 385 (19) | 29 (20) | 821 (40) | 40 (41) |
| No change | 1567 (76) | 100 (70) | 1146 (56) | 55 (56) |
| Worse | 118 (6) | 13 (9) | 63 (3) | 3 (3) |
| Overall profile | ||||
| Better | 1561 (75) | 95 (67) | 1738 (86) | 78 (80) |
| Mixed change | 161 (8) | 21 (15) | 115 (6) | 10 (10) |
| No change | 215 (10) | 11 (8) | 110 (5) | 4 (4) |
| Worse | 133 (6) | 15 (11) | 67 (3) | 6 (6) |
Study participants’ pre- and post-operative EQ-5D-3L profiles were compared. For each dimension, an individual either had a better score post-operatively, no change or a worse score than what they reported pre-operatively. An individual’s overall profile was either better (i.e. at least one dimension had improved, with none worse), had a mixed change (i.e. some dimensions had improved but others had worsened), had no change or was worse (i.e. at least one dimension had worsened, with none improving).
OHS following THR
Following THR, individuals with OA had an improved OHS from 18 (IQR 12–24) to 42 (36–46), a change of 23 (16–29) and a PoPC of 81% (61% to 94%). Meanwhile, individuals with RA had an improved OHS from 12 (IQR 7–20) to 39 (30–44) for a change of 24 (15–31) and a PoPC of 73% (52% to 89%). See Table 2 for a summary of the OHS by diagnosis and Fig. 1 for the distribution of the PoPC by diagnosis. After controlling for differences in pre-operative score and patient characteristics, the estimated effect of RA relative to OA on post-operative OHS was −1.35 (95% CI −2.93, 0.22) (Table 4).
EQ-5D-3L following THR
Of the study participants with OA, 86% had a better EQ-5D-3L profile following THR, 6% had a mixed change, 5% had no change and 3% were worse after surgery. Their EQ-5D-3L index improved from 0.52 (IQR 0.06–0.66) to 0.85 (0.69–1.00) for a change of 0.41 (0.20–0.74) and a PoPC of 79% (50% to 100%). A total of 80% of those with RA had a better EQ-5D-3L profile following TKR, 10% had a mixed change, 4% had no change and 6% were worse. Their EQ-5D-3L index improved from 0.06 (IQR −0.07–0.59) to 0.69 (0.52–1.00) for a change of 0.47 (0.13–0.76) and a PoPC of 70% (25% to 100%). Table 2 shows a summary of EQ-5D-3L indices and Table 3 the change in dimension scores by diagnosis, with further details on the dimension scores given in Supplementary Table S2, available at Rheumatology online. As with TKR, although both those with OA and RA achieved substantial improvements in the usual activities, pain/discomfort and mobility dimensions, those with RA were less likely to report no problems on these dimensions following surgery compared with those with OA. After controlling for differences in pre-operative score and patient characteristics, the estimated effect of RA relative to OA on the post-operative EQ-5D-3L index was −0.08 (95% CI −0.12, −0.03), as summarized in Table 4.
Association between other explanatory factors and post-operative PROMs
The estimated effects of other explanatory variables from the ordinary least squares regressions are provided in Supplementary Table A3, available at Rheumatology online, and the partial effect at the mean of diagnosis and pre-operative score, age and BMI are plotted in Supplementary Figures S7–S12, available at Rheumatology online. Pre-operative scores had the largest impact on post-operative scores, with these expected to increase as pre-operative scores improved. A non-linear relationship was estimated for the OKS, OHS and EQ-5D-3L index following THR, with the size of the increase in post-operative score generally reduced as pre-operative scores reached higher levels. Older age, male gender, being in a more deprived IMD quintile, comorbidities, higher BMI and being a smoker were, in general, associated with worse post-operative scores, although in many cases these differences were not statistically significant.
Discussion
Key findings
Individuals with OA and RA had substantial improvements in the OKS, OHS and EQ-5D-3L index following TKR and THR. The absolute change in scores (the journey) indicated clinically meaningful improvements in health [21, 22]. The PoPC (the proportion of journey towards perfect health completed) achieved indicated that, on average, patients reached >50% of their potential improvement. Indeed, those with OA reached >80% of their potential improvement in the OHS following THR.
While those with RA had an absolute change in scores similar or better than those with OA, the PoPC for those with RA was generally lower, particularly for the EQ-5D-3L index. This was likely because individuals with RA had worse pre-operative scores and hence greater potential for improvement. After accounting for the difference in baseline scores and patient characteristics, diagnosis of RA relative to OA had little effect on post-operative joint-specific scores. However, RA was associated with a reduction in the post-operative EQ-5D-3L index of 0.09 and 0.08 for TKR and THR, respectively.
Study findings in context
A relatively small number of studies have compared joint-specific PROMs of people with RA and OA following TKR and THR, and the findings of the studies that have are somewhat mixed. One study, with study participants recruited from the practices of rheumatologists, compared outcomes following TKR of 834 individuals with RA and 315 with OA and found RA to be associated with reduced improvements in knee pain following TKR relative to OA [23]. However, another study, based on 1991 individuals of whom 45 had RA at a large orthopaedic centre in England, found RA to be associated with significantly greater improvements in knee pain compared with OA [24]. Meanwhile, in line with our findings, another study of 4456 participants (136 with RA) undergoing TKR at one hospital found those with RA had similar pain and function scores following surgery despite having worse pre-operative scores [25]. Another study compared outcomes following THR for 62 individuals with OA and 35 with RA [26] and found that the gains in joint-specific scores appeared to be slightly less for those with RA compared with those with OA, although, given the small sample size, potential confounders could not be considered.
As with joint-specific outcomes, few studies have been performed comparing overall quality of life following TKR and THR for OA and RA. The aforementioned study by Borstlap et al. [26] found that those with RA achieved a smaller gain in overall quality of life following THR than those with OA. Another study compared outcomes for 130 TKR (76 OA and 54 RA) and 205 THR (164 OA and 41 RA) patients in one English hospital [27], finding that those with OA generally achieved greater improvements than those with RA. These findings are in line with those from our study.
Study strengths and limitations
While previous studies have typically been based on single centres, this study was informed by PROMs routinely collected across the English NHS. These data were linked to individuals’ hospital and primary care records. While there is often concern about the accuracy of coding when using routinely collected data, RA was identified from primary care records using validated diagnostic clinical codes [28]. As well as providing generalizable findings, the sample size and variables collected allowed for the control of potentially key confounding variables. Moreover, the modelling approach used in this study did not categorize continuous variables and incorporated non-linearity where merited.
In this study we assessed PROMs for joint-specific outcomes and overall quality of life. However, these outcome measures were only recorded at one point in time following surgery. Consequently, it was not possible to consider whether the effect of diagnosis varies with time since surgery. While this would be of interest, our analysis can be expected to have captured the effect of diagnosis on the peak gain from surgery. Previous studies have found that the full gains from undergoing TKR and THR have typically been realized by 6 months following surgery [29].
Only those individuals with both pre- and post-operative PROMs were included in the analysis. Bias may have arisen if those who did not complete PROMs were systematically different from those who did. However, a comparison of the patient characteristics with and without PROMs recorded found these groups to be broadly similar.
Lastly, in this study we provide a broad comparison of PROMs for those with a diagnosis of OA or RA. However, individuals with these diagnoses are not homogeneous and patient experiences are likely to vary depending on disease-specific factors, such as disease severity and treatment history. Analysis of such factors was beyond the scope of this study, with few disease-specific factors recorded in routinely collected data. Thorough analysis of the impact of disease-specific factors would require prospectively collected data.
Study implications
Joint-specific outcomes appear to be similar for those with OA and RA following TKR and THR, but improvements in overall quality of life following surgery appear to be somewhat less for those with RA. This is likely because the health of individuals with RA is being limited due to other issues beyond the targeted joint, with RA being a systemic inflammatory disease that involves multiple joints and typically necessitates polypharmacy. Consequently, while TKR and THR are likely addressing the main health problem of most patients with OA, it is only addressing one of a number of health problems for many patients with RA, thus limiting the potential improvement in overall health from ‘fixing’ the targeted joint. Indeed, it has previously been observed that although TKR and THR improve disease activity scores for individuals with RA, they do not generally result in disease activity reaching remission [30].
Regardless of the diagnosis, we found that TKR and THR typically lead to substantial and clinically meaningful improvements in both joint-specific measures and overall health-related quality of life. While the procedures should not be seen as a cure-all, particularly for those with RA, they offer a valuable treatment option for those individuals with appropriate indications.
Supplementary Material
Acknowledgments
The authors would like to thank Susan Thwaite (National Rheumatoid Arthritis Society) for her role as the patient and public representative and her role on the study steering committee. This article presents independent research funded by the National Institute for Health Research (NIHR). The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
Funding: This work was supported by an NIHR Clinician Scientist award (CS-2013-13-012) received by DPA. This work was supported by the NIHR Biomedical Research Centre, Oxford.
Disclosure statement: NKA has received personal fees from Freshfields Bruckhaus Deringer, Bioventus, Flexion, Merck and Regeneron, all outside the submitted work. DPA reports grants from Amgen, Servier and UCB Biopharma and non-financial support from Amgen, all outside the submitted work. The other authors declared no conflicts of interest.
References
- 1. Cooper C, Adachi JD, Bardin T. et al. How to define responders in osteoarthritis. Curr Med Res Opin 2013;29:719–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Pivec R, Johnson AJ, Mears SC, Mont MA.. Hip arthroplasty. Lancet 2012;380:1768–77. [DOI] [PubMed] [Google Scholar]
- 3. Carr AJ, Robertsson O, Graves S. et al. Knee replacement. Lancet 2012;379:1331–40. [DOI] [PubMed] [Google Scholar]
- 4. Wilkinson JM, Stanley D, Getty CJM.. Surgical management of the rheumatoid patient. Curr Orthop 2004;18:357–70. [Google Scholar]
- 5.National Institute for Health and Clinical Excellence. Rheumatoid arthritis in adults: management. NG100. London: National Institute for Health and Clinical Excellence, 2009.
- 6. Clement ND, Breusch SJ, Biant LC.. Lower limb joint replacement in rheumatoid arthritis. J Orthop Surg Res 2012;7:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Price AJ, Longino D, Rees J. et al. Are pain and function better measures of outcome than revision rates after TKR in the younger patient? Knee 2010;17:196–9. [DOI] [PubMed] [Google Scholar]
- 8. Harris KK, Price AJ, Beard DJ. et al. Can pain and function be distinguished in the Oxford Hip Score in a meaningful way?: an exploratory and confirmatory factor analysis. Bone Joint Res 2014;3:305–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Harris K, Dawson J, Doll H. et al. Can pain and function be distinguished in the Oxford Knee Score in a meaningful way? An exploratory and confirmatory factor analysis. Qual Life Res 2013;22:2561–8. [DOI] [PubMed] [Google Scholar]
- 10. Devlin NJ, Parkin D, Browne J.. Patient-reported outcome measures in the NHS: new methods for analysing and reporting EQ-5D data. Health Econ 2010;19:886–905. [DOI] [PubMed] [Google Scholar]
- 11. Herrett E, Gallagher AM, Bhaskaran K. et al. Data resource profile: Clinical Practice Research Datalink (CPRD). Int J Epidemiol 2015;44:827–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Herbert A, Wijlaars L, Zylbersztejn A, Cromwell D, Hardelid P.. Data resource profile: hospital episode statistics admitted patient care (HES APC). Int J Epidemiol 2017;46:1093–3i. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Secondary Care Analysis (PROMs) NHS Digital. Patient Reported Outcome Measures (PROMs) in England: A guide to PROMs methodology. Leeds: 2017.
- 14. Armitage JN, Van Der Meulen JH.. Identifying co-morbidity in surgical patients using administrative data with the Royal College of Surgeons Charlson score. Br J Surg 2010;97:772–81. [DOI] [PubMed] [Google Scholar]
- 15. Murray DW, Fitzpatrick R, Rogers K. et al. The use of the Oxford hip and knee scores. J Bone Jt Surg Br 2007;89:1010–4. [DOI] [PubMed] [Google Scholar]
- 16. Dolan P. Modeling valuation for EuroQol health states. Med Care 1997;35:1095–108. [DOI] [PubMed] [Google Scholar]
- 17. Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar Behav Res 2011;46:399–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kiran A, Hunter DJ, Judge A. et al. A novel methodological approach for measuring symptomatic change following total joint arthroplasty. J Arthroplasty 2014;29:2140–5. [DOI] [PubMed] [Google Scholar]
- 19. Harrell FE. Regression modeling strategies. Cham, Switzerland: Springer International, 2015. [Google Scholar]
- 20. White IR, Royston P, Wood AM.. Multiple imputation using chained equations: issues and guidance for practice. Stat Med 2011;30:377–99. [DOI] [PubMed] [Google Scholar]
- 21. Beard DJ, Harris K, Dawson J. et al. Meaningful changes for the Oxford hip and knee scores after joint replacement surgery. J Clin Epidemiol 2015;68:73–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Walters SJ, Brazier JE.. Comparison of the minimally important difference for two health state utility measures: EQ-5D and SF-6D. Qual Life Res 2005;14:1523–32. [DOI] [PubMed] [Google Scholar]
- 23. Dusad A, Pedro S, Mikuls TR. et al. Impact of total knee arthroplasty as assessed using patient-reported pain and health-related quality of life indices: rheumatoid arthritis versus osteoarthritis. Arthritis Rheumatol 2015;67:2503–11. [DOI] [PubMed] [Google Scholar]
- 24. Judge A, Arden NK, Cooper C. et al. Predictors of outcomes of total knee replacement surgery. Rheumatol 2012;51:1804–13. [DOI] [PubMed] [Google Scholar]
- 25. Goodman SM, Johnson B, Zhang M. et al. Patients with rheumatoid arthritis have similar excellent outcomes after total knee replacement compared with patients with osteoarthritis. J Rheumatol 2016;43:46–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Borstlap M, Zant JL, Van Soesbergen M, Van der Korst JK.. Effects of total hip replacement on quality of life in patients with osteoarthritis and in patients with rheumatoid arthritis. Clin Rheumatol 1994;13:45–50. [DOI] [PubMed] [Google Scholar]
- 27. Kirwan JR, Currey HLF, Freeman MAR, Snow S, Young PJ.. Overall long-term impact of total hip and knee joint replacement surgery on patients with osteoarthritis and rheumatoid arthritis. Rheumatology 1994;33:357–60. [DOI] [PubMed] [Google Scholar]
- 28. Hawley S, Delmestri A, Judge A. et al. Total hip and knee replacement among incident osteoarthritis and rheumatoid arthritis patients within the UK Clinical Practice Research Datalink (CPRD) compared to Hospital Episode Statistics (HES): a validation study. Pharmacoepidemiol Drug Saf 2016;25:251. [Google Scholar]
- 29. Schilling C, Dowsey MM, Clarke PM, Choong PF.. Using patient-reported outcomes for economic evaluation: getting the timing right. Value Health 2016;19:945–50. [DOI] [PubMed] [Google Scholar]
- 30. Momohara S, Inoue E, Ikari K. et al. Efficacy of total joint arthroplasty in patients with established rheumatoid arthritis: improved longitudinal effects on disease activity but not on health-related quality of life. Mod Rheumatol 2011;21:476–81. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.