Abstract
Background
Rapid diagnostic tests (RDTs) for Plasmodium falciparum malaria use antibodies to detect either HRP‐2 antigen or pLDH antigen, and can improve access to diagnostics in developing countries.
Objectives
To assess the diagnostic accuracy of RDTs for detecting P. falciparum parasitaemia in persons living in endemic areas who present to ambulatory healthcare facilities with symptoms suggestive of malaria by type and brand.
Search methods
We undertook a comprehensive search of the following databases: Cochrane Infectious Diseases Group Specialized Register; MEDLINE; EMBASE; MEDION; Science Citation Index; Web of Knowledge; African Index Medicus; LILACS; IndMED; to January 14, 2010.
Selection criteria
Studies comparing RDTs with a reference standard (microscopy or polymerase chain reaction) in blood samples from a random or consecutive series of patients attending ambulatory health facilities with symptoms suggestive of malaria in P. falciparum endemic areas.
Data collection and analysis
For each study, a standard set of data was extracted independently by two authors, using a tailored data extraction form. Comparisons were grouped hierarchically by target antigen, and type and brand of RDT, and combined in meta‐analysis where appropriate.
Main results
We identified 74 unique studies as eligible for this review and categorized them according to the antigens they detected. Types 1 to 3 include HRP‐2 (fromP. falciparum) either by itself or with other antigens. Types 4 and 5 included pLDH (from P. falciparum) either by itself or with other antigens. In comparisons with microscopy, we identified 71 evaluations of Type 1 tests, eight evaluations of Type 2 tests and five evaluations of Type 3 tests. In meta‐analyses, average sensitivities and specificities (95% CI) were 94.8% (93.1% to 96.1%) and 95.2% (93.2% to 96.7%) for Type 1 tests, 96.0% (94.0% to 97.3%) and 95.3% (87.3% to 98.3%) for Type 2 tests, and 99.5% (71.0% to 100.0%) and 90.6% (80.5% to 95.7%) for Type 3 tests, respectively.
Overall for HRP‐2, the meta‐analytical average sensitivity and specificity (95% CI) were 95.0% (93.5% to 96.2%) and 95.2% (93.4% to 99.4%), respectively.
For pLDH antibody‐based RDTs verified with microscopy, we identified 17 evaluations of Type 4 RDTs and three evaluations of Type 5 RDTs. In meta‐analyses, average sensitivity for Type 4 tests was 91.5% (84.7% to 95.3%) and average specificity was 98.7% (96.9% to 99.5%). For Type 5 tests, average sensitivity was 98.4% (95.1% to 99.5%) and average specificity was 97.5% (93.5% to 99.1%).
Overall for pLDH, the meta‐analytical average sensitivity and specificity (95% CI) were 93.2% (88.0% to 96.2%) and 98.5% (96.7% to 99.4%), respectively.
For both categories of test, there was substantial heterogeneity in study results. Quality of the microscopy reference standard could only be assessed in 40% of studies due to inadequate reporting, but results did not seem to be influenced by the reporting quality.
Overall, HRP‐2 antibody‐based tests (such as the Type 1 tests) tended to be more sensitive and were significantly less specific than pLDH‐based tests (such as the Type 4 tests). If the point estimates for Type 1 and Type 4 tests are applied to a hypothetical cohort of 1000 patients where 30% of those presenting with symptoms have P. falciparum, Type 1 tests will miss 16 cases, and Type 4 tests will miss 26 cases. The number of people wrongly diagnosed with P. falciparum would be 34 with Type 1 tests, and nine with Type 4 tests.
Authors' conclusions
The sensitivity and specificity of all RDTs is such that they can replace or extend the access of diagnostic services for uncomplicated P. falciparum malaria. HRP‐2 antibody types may be more sensitive but are less specific than pLDH antibody‐based tests, but the differences are small. The HRP‐2 antigen persists even after effective treatment and so is not useful for detecting treatment failures.
23 April 2019
No update planned
Other
Good evidence of benefit and further research is unlikely to change our confidence in the estimates of test accuracy. All eligible published studies found in the last search (14 Jan, 2010) were included.
Keywords: Humans; Endemic Diseases; Plasmodium falciparum; Plasmodium falciparum/enzymology; Plasmodium falciparum/immunology; Antigens, Protozoan; Antigens, Protozoan/analysis; Biomarkers; Biomarkers/analysis; Diagnostic Tests, Routine; Diagnostic Tests, Routine/methods; L‐Lactate Dehydrogenase; L‐Lactate Dehydrogenase/analysis; Malaria, Falciparum; Malaria, Falciparum/diagnosis; Malaria, Falciparum/epidemiology; Malaria, Falciparum/immunology; Parasitemia; Parasitemia/diagnosis; Parasitemia/epidemiology; Parasitemia/immunology; Protozoan Proteins; Protozoan Proteins/analysis; Sensitivity and Specificity
Plain language summary
Rapid diagnostic tests for diagnosing malaria
Fever is common in malarial areas, and getting the diagnosis right (ie deciding if it is due to malaria or other causes) and treating correctly helps save lives, particularly in children. The World Health Organization (WHO) now recommends that all patients with fever suspected of being malaria are properly diagnosed before any treatment begins. This ensures that highly effective antimalarial drugs such as artemisinin‐based combination treatments (ACTs) are properly used to prevent unnecessary treatments, untoward risks, and resistance developing.
Standard diagnosis of malaria in the past has depended on blood microscopy, but this requires a technician and a laboratory, and is often not feasible for basic health services in many areas. Sometimes in research studies, another technique called polymerase chain reaction (PCR) is used, but again this requires equipment and trained staff, and cannot be used routinely. Technological advances have led to rapid diagnostic tests (RDTs) for malaria. These detect parasite‐specific antigens in the blood, are simple to use, and can give results as a simple positive or negative result, within 15 minutes.
This review evaluates the accuracy of RDTs compared with microscopy and PCR for detecting Plasmodium falciparum parasites in the blood. It includes 74 studies, giving a total of 111 RDT evaluations (of which 104 compared RDTs with microscopy), reporting a total of 60,396 RDT results. Results are presented by type of test, classified by the malaria antigen that they are designed to detect (either histidine‐rich protein‐2 (HRP‐2), or plasmodium lactate dehydrogenase (pLDH)).
The results indicate that RDTs can be very accurate compared to microscopy and PCR. The performance of RDT types varied but the differences were not large. HRP‐2‐based tests tended to be more sensitive (ie they identified more true cases of malaria) and less specific (ie they wrongly identified more malaria that was not present) than pLDH‐based tests. Choice will depend on prevalence of malaria, and we provide data in this review to assist these decisions, although policy makers will also take into account other factors relating to cost and test stability.
Summary of findings
Summary of findings'. 'New Summary of results table.
| What is the diagnostic accuracy of Rapid Diagnostic Tests for detecting malaria? What are the best types of tests? | ||||||
| Patients/populations | People presenting with symptoms suggestive of uncomplicated malaria | |||||
| Prior testing | None | |||||
| Settings | Ambulatory healthcare settings in P. falciparum malaria endemic areas in Asia, Africa and South America | |||||
| Index tests | Immunochromatography‐based rapid diagnostic tests for P. falciparum malaria | |||||
| Reference standard | Conventional microscopy or PCR | |||||
| Importance | Accurate and fast diagnosis allows appropriate and quick treatment for malaria to be provided | |||||
| Studies | Consecutive series of patients; 74 studies presented 111 test evaluations based on 60,396 patient test results | |||||
| Quality concerns | Poor reporting of patient characteristics, sampling method and reference standard methods were common concerns | |||||
| Test types | Quantity of evidence | Brands (studies) | Average pooled results | Consequences in a cohort of 1000 | ||
| P. falciparum prevalence | Missed cases | Overtreated non‐cases | ||||
| HRP‐2 antibody‐based tests compared with microscopy | ||||||
|
Type 1 HRP‐2 (P. falciparum specific) |
71 evaluations 40,062 participants 11,966 malaria cases |
Paracheck‐Pf (27), ParaSight (17), ICT Malaria Pf (16), ParaHIT‐F (4), PATH (2), Determine Malaria Pf (1), Rapid Test Malaria (1), Diaspot Malaria (1), New mini‐Pf (1), and Hexagon Malaria (1) | sens = 94.8% (93.1% to 96.1%) | 30% | 16 | 34 |
| spec = 95.2% (93.2% to 96.7%) | 50% | 26 | 24 | |||
|
Type 2 HRP‐2 (P. falciparum specific) and aldolase (pan‐specific) |
8 evaluations 3397 participants 790 malaria cases |
ICT Malaria Pf/Pv (6) and NOW ICT Malaria (2) | sens = 96.0% (94.0% to 97.3%) | 30% | 12 | 33 |
| spec = 95.3% (87.3% to 98.3%) | 50% | 20 | 24 | |||
|
Type 3 HRP‐2 (P. falciparum specific) and pLDH (pan‐specific) |
5 evaluations 958 participants 330 malaria cases |
SD Malaria Antigen Bioline (2), Parascreen (2), and First Response Malaria (1) | sens = 99.5% (71.0% to 100.0%) | 30% | 12 | 62 |
| spec = 90.6% (80.5% to 95.7%) | 50% | 20 | 44 | |||
| pLDH antibody‐based tests compared with microscopy | ||||||
|
Type 4 pLDH (P. falciparum specific) and pLDH (pan‐specific) |
17 evaluations 13,010 participants 4274 malaria cases |
OptiMAL (10), OptiMAL‐IT(3), Parabank (2) and Carestart Malaria Pf/Pan (2) | sens = 91.5% (84.7% to 95.3%) | 30% | 26 | 9 |
| spec = 98.7% (96.9% to 99.5%) | 50% | 43 | 7 | |||
|
Type 5 pLDH (P. falciparum specific) and pLDH (P. vivax‐specific) |
3 evaluations 1777 participants 400 malaria cases |
Carestart Pf/Pv (2), and ParaSight Pf/Pv (1) | sens = 98.4% (95.1% to 99.5%) | 30% | 5 | 18 |
| spec = 97.5% (93.5% to 99.1%) | 50% | 8 | 13 | |||
| Comparisons | ||||||
| Comparison | Comparison type | Quantity of evidence and overall finding | Sensitivity | Specificity | ||
| Type 1 vs Type 4 | All studies | 65 Type 1 vs 16 Type 4 Overall significant difference in accuracy P = 0.009 |
Type 1 3.3% more sensitive than Type 4 (P = 0.20) | Type 4 3.5% more specific than Type 1 (P < 0.001) | ||
| Within studies | 7 comparative studies No overall significant difference in accuracy P = 0.26 |
Type 1 2.5% more sensitive than Type 4 (P = 0.51) | Type 4 2.9% more specific than Type 1 (P = 0.31) | |||
| HRP‐2 vs pLDH | All studies | 75 HRP‐2 vs 19 pLDH Overall significant difference in accuracy P = 0.01 |
HRP‐2 1.8% more sensitive than pLDH (P = 0.34) | pLDH 3.3% more specific than HRP‐2 (P = 0.01) | ||
| Within studies | 9 comparative studies No overall significant difference in accuracy P = 0.35 |
HRP‐2 0.8% more sensitive than pLDH (P = 0.60) | pLDH 2.3% more specific than HRP‐2 (P = 0.22) | |||
Background
Target condition being diagnosed
Malaria is a life‐threatening illness, caused by the asexual form of the parasitic protozoan Plasmodium. Most cases of malaria are uncomplicated, commonly presenting with fever and sometimes with other non‐specific symptoms including headache, and aches and pains elsewhere in the body (Gilles 1991; WHO 2003). A few people develop severe malaria, with confusion, weakness, coma and other life‐threatening complications. Malaria is curable, and early, prompt and accurate diagnosis followed by appropriate treatment helps to reduce illness and death, (WHO 2003) and is central to current malaria control policy (Bell 2006; WHO 2005).
The two most common species of malaria parasite are Plasmodium falciparum andPlasmodium vivax. P. falciparum malaria is by far the most common type of malaria in Africa, and is also endemic in parts of Asia and South America. It is the most common cause of severe malaria, is responsible for almost all malaria deaths, and can cause other complications such as anaemia and, in pregnancy, low birth‐weight babies. Vivax malaria is a relapsing form, which is rarely fatal but can cause serious anaemia in children. Less common human malaria parasite species include P. malariae and P. ovale.
In 2008, there were between 190 million and 311 million cases of malaria worldwide (WHO 2009a). Around 85% of these cases were in Africa; 10% were in South East Asia; 4% were in the Eastern Mediterranean region; and 1% were in South America (WHO 2009a). In the same year, there were between 708,000 and 1,003,000 deaths from malaria; 89% were in Africa and 85% were children under the age of five years (WHO 2009a).
People who are repeatedly exposed to malaria infection develop a partial and incomplete immunity. In highly endemic areas, those most at risk are children under the age of five, who have not yet had the chance to develop immunity. In less endemic areas, or areas of seasonal or epidemic transmission, older children and adults are also at risk due to less developed immunity. Travellers from non‐endemic to endemic countries are at highest risk because they have no immunity at all.
Index test(s)
Rapid diagnostic tests (RDTs) (WHO 2003) detect parasite‐specific antigens in a drop of fresh blood through lateral flow immunochromatography (WHO 2006). The World Health Organization (WHO) currently lists 96 commercially‐available test kits meeting ISO13485:2003 manufacturing standards (WHO 2009). RDTs do not require a laboratory or any special equipment (WHO 2006); they are simple to use and can give results as a simple positive/ negative result, within 15 minutes (Talman 2007). RDTs are therefore, in general, suitable for remote areas with limited facilities and relatively untrained staff. However, they have a limited shelf life, and need to be kept dry and away from extremes of temperature. They may also fail to detect malaria in cases where there are low levels of parasites in the blood, and false positives are possible due to cross reactions or gametocytaemia (infection with the sexual stage of the parasite only) (Kakkilaya 2003).
RDTs use antibodies to detect one or several antigens. The most commonly used antibodies react to histidine‐rich protein‐2 (HRP‐2), aldolase and plasmodium lactate dehydrogenase (pLDH) (Talman 2007). HRP‐2 is a marker for P. falciparum, while pLDH antibodies can be specific for P. falciparum, orP. vivax, or may detect all species (including P. ovale and P. gambiae) or other combinations of these species. Aldolase antibodies are pan‐specific, detecting all types of malaria parasite but not differentiating between them. Until recently, there were seven main types of commercially‐available test, using different antigen combinations as described in Table 2 below (Bell 2006).
1. Types of malaria RDTs by antibody combination and parasite species detected.
| Type of Test | Antibody Combinations | Possible Results |
| Type 1 | HRP‐2 (P. falciparum specific) | No Pf; Pf; invalid |
| Type 2 | HRP‐2 (P. falciparum specific) and aldolase (pan‐specific) | No malaria; Pf or mixed; Pv, Pf and/or Pm; invalid |
| Type 3 | HRP‐2 (P. falciparum specific) and pLDH (pan‐specific) | No malaria; Pf or mixed; Pv, Pf and/or Pm; invalid |
| Type 4 | pLDH (P. falciparum specific) and pLDH (pan‐specific) | No malaria; Pf or mixed; Pv, Pf and/or Pm; invalid |
| Type 5 | pLDH (P. falciparum specific) and pLDH (P. vivax‐specific) | No malaria; Pf; Pv; Pf and Pv; invalid |
| Type 6 | HRP‐2 (P. falciparum specific), pLDH (pan‐specific) and pLDH (P. vivax specific) | No malaria; Pf and Pv =/‐ Po and/or Pm; Pf +/‐ Po and/or Pm; Pv +/‐ Po and/or Pm; Po and/or Pm; invalid |
| Type 7 | Aldolase (pan‐specific) | No malaria; Pf, Pv, Po and/or Pm; invalid |
Pf P. falciparum; Pv P. vivax; Pm P. malariae; Po P .ovale
Since this classification was developed, the following test types have also become available.
Pan pLDH antibodies only, with the following possible results: no malaria; P. falciparum, P. vivax, P. ovale and/or P. malariae; and invalid (as for Type 7 tests).
P. vivax‐specific pLDH antibodies only.
pLDH antibody lines detecting P. vivax, P. ovale and P. malariae in combination.
The different test types detect different malaria species and combinations of species; the choice of RDT used will therefore depend on which species are endemic in the area. Table 3 shows the type of tests that are appropriate for use in the different malaria 'zones' of the world.
2. Malaria 'zones' by endemic parasite species and RDT type appropriate for each.
| Zone | Endemic malaria parasites | Geographic area | Appropriate test type |
| 1 | P. falciparum only or other species almost always as a mixed infection | Most of sub‐Saharan Africa; lowland Papua New Guinea | Tests using HRP‐2 to detect P. falciparum only (Type 1) |
| 2 | Both P. falciparum and P. vivax, most commonly as a single species |
Asia and the Americas; Ethiopian highlands |
Combination RDTs which detect all species and distinguish between P. falciparum and P. vivax (Types 2 to 6) |
| 3 | Non‐falciparum only |
Vivax only areas of East Asia and Central Asia; some highland areas elsewhere | Pan‐specific or vivax‐specific RDTs (Type 7; Pan‐pLDH only; vivax‐pLDH only) |
HRP‐2 can stay in the blood for up to 28 days after starting antimalarial therapy (Kakkilaya 2003). Because of this 'persistent antigenaemia', it is not possible to use these tests for assessing parasite clearance following treatment, and false positive results may be found in patients who have recently been treated for malaria. In contrast, pLDH is rapidly cleared from the blood following parasite death; in fact, it may clear more rapidly than the dead parasites (WHO 2009), but may persist in the presence of gametocytes.
Reference tests
Microscopic examination of Giemsa‐stained thick and thin blood films remains the conventional laboratory method for malaria diagnosis, but needs to be conducted by microscopists with adequate training and equipment. Microscopic examination displays a good sensitivity and specificity, and allows species and stage differentiations and quantification of parasites, all of which are important in assessing the disease severity and prescribing appropriate therapy. Intensive examination is more likely to reveal parasitaemia, so the test is carried out by examining a fixed number of fields; infections may be missed if slides are not examined carefully (Wongsrichalanai 2007). Very low parasitaemia may be missed even by good quality microscopy; the limit of detection of thick smear microscopy has been estimated at between around four and 20 asexual parasites per μl, although under field conditions a threshold of between 50 and 100 asexual parasites per μl is more realistic (Wongsrichalanai 2007). On the whole, false positive results are the result of poor slide preparation or reading (Wongsrichalanai 2007).
Molecular DNA amplification via polymerase chain reaction (PCR) is the most accurate method of detecting parasites in the blood. It eliminates observer error and is more sensitive at low levels of parasitaemia, with limits of detection as low as 0.004 asexual parasites per μl (Hanscheid 2002; Snounou 1993). However, whether this increased ability to detect low level parasitaemias makes it a better diagnostic test is uncertain, as sub‐microscopic parasitaemias are of unknown clinical significance and the prevalence of asymptomatic sub‐microscopic infection is high in some areas (May 1999). In addition, PCR may be prone to false positive results due to contamination of samples if laboratory standards are not sufficiently high. PCR is currently not widely available outside of research settings, as it needs specially‐trained technicians and a well‐equipped laboratory.
Rationale
Diagnostic tests for malaria in endemic areas are now recommended as routine by the WHO in all patients suspected of malaria before any treatment begins (WHO 2010). This is due to a shift in drug treatment policy away from cheap, often relatively ineffective, drugs, towards artemisinin‐based combination treatment (ACTs), which are highly effective, expensive, and need to be used properly to prevent resistance developing.
There is a long‐standing recognition that good quality, standard malaria microscopy is relatively expensive and difficult to deliver in many basic, primary health care settings in developing countries, while RDTs for malaria have now become widely available and affordable.
RDTs in malaria could dramatically increase access to prompt diagnosis in primary health care. The question of how a package of care (diagnosis using RDTs with positive cases treated with drugs versus presumptive treatment of all cases with symptoms suggestive of malaria) impacts on health outcomes is to be addressed in a separate forthcoming review (Odaga 2011). However, important policy questions remain to be answered
a) How well do RDTs perform compared to the previous standard of microscopy in diagnosing symptomatic patients?
b) What are the differences in accuracy between different types of commercial test, and individual brands of commercial tests?
This information will help to inform choice, although factors, such as price, product consistency, stability and shelf life will also influence those decisions.
This review is the first of a series of three reviews: the second will examine the accuracy of RDTs for diagnosing uncomplicated P. vivax and other non‐falciparum malaria; and the third will assess trials that incorporate RDTs into treatment protocols (Odaga 2011). Previous published reviews have examined travellers only (Marx 2005) or just one particular test (Cruciani 2004).
Objectives
To assess the diagnostic accuracy of RDTs for detecting clinical P. falciparum malaria (symptoms suggestive of malaria plus P. falciparum parasitaemia detectable by microscopy) in persons living in malaria endemic areas who present to ambulatory healthcare facilities with symptoms of malaria, and to identify which types and brands of commercial test best detect clinical P. falciparum malaria.
Investigation of sources of heterogeneity
We planned to investigate heterogeneity in relation to the index test (by commercial test, test type and grouped by HRP‐2/pLDH) and reference tests (microscopy vs PCR), as well as the study participants' age, endemicity of malaria, and geographic area (by continent).
Methods
Criteria for considering studies for this review
Types of studies
Studies evaluating one or more RDTs in a consecutive series of patients, or a randomly‐selected series of patients, were eligible. Where the report did not explicitly state that sampling was consecutive, but consecutive sampling was judged most probable, the study was included. Studies were excluded if they did not present sufficient data to allow us to extract or calculate absolute numbers of true positives, false positives, false negatives, and true negatives. Studies were also excluded if they were not available in English, or if they presented insufficient information to fully assess their eligibility.
Participants
Studies recruiting people living in P. falciparum malaria endemic areas who attended ambulatory healthcare settings with symptoms of uncomplicated malaria. This included patients attending malaria clinics with self‐assessed symptoms.
We excluded studies if participants:
1. were non‐immune persons returning from endemic countries or were mainly recent migrant or displaced populations from non‐endemic or very low endemicity areas;
2. had been treated for malaria and the test was performed to assess treatment outcome;
3. had symptoms suggestive of severe malaria;
4. did not have symptoms suggestive of malaria;
5. were recruited through active case finding (for example, door‐to‐door surveys).
In studies with broader inclusion criteria but which presented results stratified by subgroups, we included the data relevant to our inclusion criteria. If studies included some participants with severe malaria, and data specific to a subgroup of participants with uncomplicated malaria could not be extracted, the study was included if 90% or more of the participants had uncomplicated malaria.
Index tests
Studies evaluating any immunochromatography‐based RDTs specifically designed to detect P. falciparum malaria.
Commerical tests no longer available were included because they may use the same antibodies, and very similar technology, to tests that are currently available or may become available in the future. Older and more recently available versions of the same test, and tests available in both dipstick and cassette format, were included separately. Late prototype tests corresponding to one of the commercially‐available types were also included.
Comparator tests
Studies were included regardless of whether they made comparisons with other RDT tests.
Target conditions
Studies aimed to detect P. falciparum malaria parasitaemia. Studies that presented RDT results relating only to all types of malaria without distinction by species, but where over 98% of malaria infections by reference standard were associated with P. falciparum, were included in this review and analysed as for P. falciparum.
Reference standards
Studies were required to diagnose P. falciparum malaria using at least one of the following two reference standards.
Conventional microscopy of thick blood smears, thin blood smears or both. Presence of asexual P. falciparum parasites of any density was regarded as a positive smear.
PCR test.
We required that the reference standard was carried out on blood samples taken at the same time and from the same person as the index tests. Where studies used more than one reference standard, we presented data relating to comparisons with each.
Search methods for identification of studies
We used a single search strategy for all reviews in the series.
Electronic searches
To identify all relevant studies, we searched the following databases using the search terms and strategy identified in Appendix 1. The date of the last search was 14 January 2010.
Cochrane Infectious Diseases Group Specialized Register; MEDLINE; EMBASE; MEDION; Science Citation Index; Web of Knowledge; African Index Medicus; LILACS; IndMED. We used the following MeSH, full text and keyword terms: malaria, Plasmodium, reagent kits, diagnosis, diagnostics, RDT, dipstick, MRDD, OptiMal, Binax Now, Parasight, Immumochromatography, antigen detection, antigen test, Combo card. We restricted the searches to human studies. We did not limit the search by language or publication status.
Data collection and analysis
Selection of studies
A single selection procedure was initially used to identify studies for inclusion in either of the two diagnostic test accuracy reviews in the series. The inclusion criteria between the reviews differed only in the target condition and parasite species. Parasite species was therefore the last aspect of the study characteristics to be assessed. One author (KA) initially assessed the titles identified by the search, excluding those obviously irrelevant to the diagnosis of malaria using RDTs.
Letters, review articles, and articles clearly irrelevant based on examination of the abstract and other notes were next excluded and the eligibility of the remaining potentially relevant articles was judged on full text publications independently by two authors (KA SJ) using a proforma. These excluded studies are listed in Characteristics of excluded studies. Any discrepancy was resolved by discussion. Where agreement could not be reached, we consulted a third author (PG or PO). Where it remained unclear whether a study was eligible for inclusion, it was excluded, and we excluded study reports in non‐English language reports for logistical reasons.
Studies were named according to the surname of their first author and the year of publication. The study naming used in this review uniquely identifies multiple study cohorts from within each study report (for example as 'Bell 2001a' and 'Bell 2001b'), each of which use different reference standards or present data separately for more than one population with different characteristics. A slightly different notation (for example, 'Singh 1997(a)' and 'Singh 1997(b)') was used to refer to completely separate studies published by an author of the same name in the same year. Note that more that one RDT may be evaluated in each study cohort, thus the number of test evaluations exceeds the number of study cohorts, which exceeds the number of study reports.
Data extraction and management
A standard set of data was extracted from each study cohort, using a tailored data extraction form. Two authors from a pool of three (KA SJ CMN) independently extracted data, and any discrepancies were resolved by discussion. In cases of studies where only a subgroup of participants met the review inclusion criteria, data was extracted and presented only for that particular subgroup. Where two versions of one reference standard or index test were used, for example local clinic and expert standard microscopy or field versus laboratory testing, only the one most likely to yield the highest quality results was included in the review.
For each study, we systematically extracted data on the characteristics of the study, as shown in Appendix 2.
For each comparison of index test with reference test, data were extracted on the number of true positives, true negatives, false positives and false negatives in the form of a two by two table. RDT results are dichotomous; microscopy results were deemed positive at any level of asexual P. falciparum parasitaemia; and PCR results used the cut‐off points presented by the study authors. Gametocyte‐only parasitaemia was considered negative; where a study was unclear on how they had classed gametocyte‐only parasitaemia, they were assumed to have used the same classification as ourselves and the data were included in the study. In cases of minor disagreement (within 2%) between two by two table data presented in a study report and reported study sample sizes or calculated accuracies, the data in the table were taken as correct. In cases where there was a large discrepancy, the data were not included in the review.
Data were extracted (Smidt 2008) using current manufacturers' instructions in interpreting the RDT results. P. falciparum only andP. falciparum as part of a mixed infection were not distinguished and were classed as positive. Non‐falciparum malaria only was classed as negative for this review. Where study authors interpreted test results or presented data differently, we used all the information presented in the paper to extract data consistent with our own methods; if we were unable to do this, we did not include the data in the analyses.
Reference standard positive was defined as 'P. falciparum or mixed infection' and reference standard negative as 'no malaria parasitaemia or non‐falciparum malaria parasitaemia only'.
Assessment of methodological quality
Two authors from a pool of three (KA SJ CMN) independently assessed the quality of each individual study using the checklist adapted from the QUADAS tool (Whiting 2003). Each question on the checklist was answered with a yes/no response, or noted as unclear if insufficient information was reported to allow a judgement to be made, and the reasons for the judgement made were documented. The criteria used are summarized in Appendix 3.
Statistical analysis and data synthesis
The comparisons made in this review can be considered in a hierarchy. The highest level comparison groups tests by antibody type (HRP‐2 versus pLDH) and is formed by combining the test types into two groups: HRP‐2 antibody‐based (Types 1, 2, 3 and 6) and pLDH antibody‐based (Types 4 and 5). However, the data on each test type is classified in the primary studies according to commercial brands. In order to provide a coherent description of the studies contributing to each analysis, the results are structured first by grouping studies according to their commercial brand, then grouping brands to form test types, and finally grouping test types by antibody.
The analytical strategy thus compared the test accuracy of commercial brands within each test type before making comparisons between test types, and then between antibodies. Comparative analyses first included all studies with relevant data, and were then restricted to studies that made direct comparisons between tests with the same participants, where such studies existed.
For each test type, we plotted estimates of the observed sensitivities and specificities in forest plots and in receiver‐operating characteristic (ROC) space. These plots demonstrate the variation in accuracy between studies.
Meta‐analyses were undertaken where adequate data were available. Hierarchical summary ROC models (HSROC) that included a random‐effects term for variation in accuracy and threshold between studies, and non‐symmetrical underlying ROC curves, were fitted. The average operating point for each test was identified on each curve, and average sensitivities and specificities computed. Comparisons between tests were made by adding a covariate for brand, test type or antigen to the accuracy and threshold parameters, assuming a common underlying shape. The impact of test type and antibody on the variability of random‐effects of accuracy and thresholds was also investigated and separate variance terms included where required. The significance of the difference in test performance was assessed by a likelihood ratio test comparing models with and without covariate terms for accuracy and threshold. Where inadequate studies were available to estimate all parameters, the HSROC model was simplified by assuming a symmetrical shape to the summary ROC curve or fixed‐effect estimates.
Where more than one commercial test of the same type was tested on the same patients against the same reference standard, we selected one type at random from the analysis by test type, in order to avoid bias due to inclusion of the same participants more than once in the analysis. We included both types in any analyses comparing commercial brands.
Investigations of heterogeneity
We investigated heterogeneity for Type 1 tests because this was the only test category for which there were sufficient studies available. We investigated variation in sensitivity and specificity by adding to the meta‐analysis models covariates indicating the following characteristics: age group; P. falciparum endemicity; continent where the study took place; and adequacy of the reference standard.
Age group was classified as: children only; adults only; mixed adults and children; and 'not stated'. Studies including, for example, all ages over the age of five years were classified as 'mixed adults and children'. The age cut‐off between adults and children was as used by the study authors.
Endemicity was divided into two categories: high and low. We classified endemicity as 'high' if described by the authors as 'holoendemic', 'hyperendemic' or 'high'; and 'low' if described as 'hypoendemic', 'mesoendemic', 'low' or 'epidemic‐prone'. In the case of studies where a reported endemicity was not available, we imputed endemicity using geographical location information provided in the report. This involved mapping the location using 'Google Earth' onto country maps of mean parasite rate in children aged two to ten years in 2007 (Hay 2009) provided by the Malaria Atlas Project (www.map.ox.ac.uk). An example map produced during this process is shown in Figure 1. Study sites with a mean parasite rate of less than 50% were classified as 'low' endemicity to correspond with endemicities of hypoendemic and mesoendemic; study sites with a mean parasite rate of 50% and above were classified as 'high' (Hay 2008). Where the endemicity was unclear and borderline between 'high' and 'low' we assigned it 'high'. Where multiple sites of differing endemicity class were included, and separate results by site were not available, the endemicity assigned to that study was 'mixed'.
1.
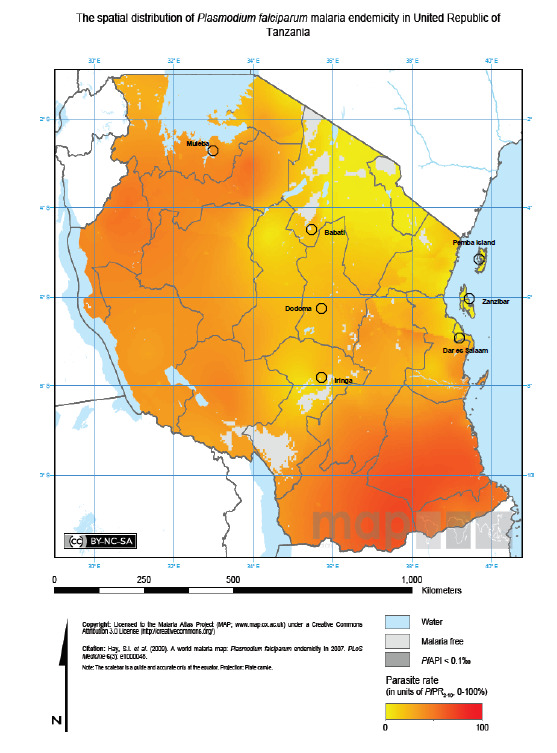
Example map showing P. falciparum malaria endemicities and study locations
For continent classification, where multi‐site studies were conducted across continents and results were not available for different sites separately, the location of the study was classified according to the continent with the largest number of participants.
Sensitivity analyses
Sensitivity analyses were undertaken to investigate the impact of the reference standard method (PCR and PCR‐adjusted microscopy) on the results obtained by microscopy alone.
Results
Results of the search
The search identified 3971 titles, of which 3418 were excluded on the basis of title alone. A further 168 were excluded without obtaining full‐text articles; 29 were excluded because they were letters; and 139 were excluded on the basis of their abstract. We were unable to obtain one article in full‐text form. Full‐text articles were retrieved for 384 titles, of which 307 were excluded: 254 because they were initially assessed as ineligible; 17 because the reports did not present sufficient detail for us to be sure of their eligibility or ineligibility; 18 because they were available only in non‐English languages; 12 because we were unable to extract absolute numbers of true positives, false positives, false negatives and true negatives; and six because they did not present data on P. falciparum malaria, although they were eligible for other reviews in this series.
Two further studies were included as they were identified as eligible during an earlier, scoping stage of the review process but were not identified by the final search.
A total of 74 unique studies described in 79 study reports are therefore included in the review. However, as some of these studies were divided for the purposes of the review (for example, because they used two different reference standards or were conducted in two communities with differing characteristics), 89 separate study cohorts are identified. Fourteen of the 89 study cohorts evaluated more than one test: one compared seven tests, three compared three tests and ten compared two tests. Thus, there are a total of 111 test evaluations reporting a total of 60,396 test results. Microscopy was the reference standard for 104 test evaluations, PCR‐adjusted microscopy for two and PCR alone for five,
Sixty‐five study cohorts (40,062 participants) assessed the accuracy of Type 1 tests using microscopy as the reference standard; 16 study cohorts (13,010 participants) did the same for a Type 4 test, eight for a Type 2 test (3397 participants), five for a Type 3 test (958 participants) and three for a Type 5 test (1777 participants). Seventy‐five cohorts (43,307 participants) assessed the accuracy of HRP‐2 antibody‐based tests and 19 cohorts (14,787) assessed the accuracy of pLHD antibody‐based tests. Only four studies used PCR and one used PCR‐adjusted microscopy. A summary of the numbers of studies assessing each RDT type using microscopy, PCR or PCR‐adjusted microscopy is shown in Table 4.
3. Number of studies verifying each RDT type with reference standard.
| Type of RDT | Number of study cohorts (test evaluations if different) by reference standard | ||
| Microscopy | PCR | PCR‐adjusted microscopy | |
| Type 1 | 65 (71) | 2 | 1 |
| Type 4 | 16 (17) | 1 | 0 |
| Type 2 | 8 | 0 | 0 |
| Type 3 | 5 | 1 | 1 |
| Type 5 | 3 | 0 | 0 |
| Type 6 | 0 | 1 | 0 |
Methodological quality of included studies
The overall methodological quality of all included study cohorts is summarized in Figure 2. Just over 50% clearly included a representative spectrum of participants attending ambulatory care settings with symptoms suggestive of malaria; the majority of the remaining studies were unclear, in most cases because they had not described the sampling methods. Around 40% reported an acceptable reference standard, 40% were unclear about the microscopy method, and 20% reported an unacceptable quality reference standard (heterogeneity relating to this criteria is investigated below). As expected, almost all the included studies reported avoidance of partial verification and differential verification, and all reported avoidance of incorporation bias. Around 65% of study cohorts reported blinding of the reference standard to the results of the index test, and around 70% reported blinding of the index test to the results of the reference standard. Only around 25% of studies reported on uninterpretable results while around 60% either explained any withdrawals or were clear that there were no withdrawals.
2.
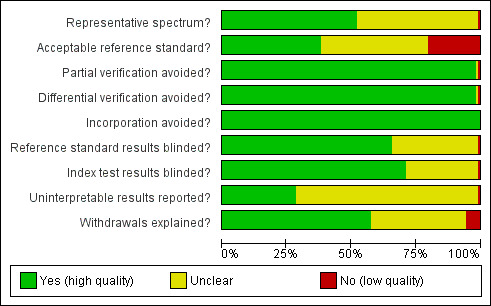
Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.
Twenty‐four of the included studies gave details of the number of uninterpretable or invalid RDT results. Eight reported no uninterpretable RDT results; one reported that 14% of tests needed to be repeated; and 15 reported small numbers of uninterpretable test results (<1% to 5%), which were excluded from the analysis. Four studies reported small numbers of uninterpretable microscopy slides, which were excluded from the analysis.
Four key quality items (representative spectrum, adequate reference standard, blinding of reference test, and index test) are used to evaluate each RDT type in Table 5. A lower proportion of those studies assessing Type 1 and Type 4 RDTs reported an adequate reference standard than those assessing other RDT types (P=0.05) (only 25% of Type 1 evaluations and 29% of Type 2 evaluations were judged to be adequate).
4. Methodological quality by RDT type.
| Test type | Test evaluations | Representative spectrum | Adequate reference standard | Blinded reference standard | Blinded index test |
| Type 1 | 71 | 38 (54%) | 18 (25%) | 44 (62%) | 50 (70%) |
| Type 2 | 8 | 2 (25%) | 4 (50%) | 6 (75%) | 7 (88%) |
| Type 3 | 5 | 4 (80%) | 2 (40%) | 4 (80%) | 4 (80%) |
| Type 4 | 17 | 9 (53%) | 5 (29%) | 10 (59%) | 12 (71%) |
| Type 5 | 3 | 1 (33%) | 3 (100%) | 2 (67%) | 3 (100%) |
| Test for difference between types | P = 0.54 | P = 0.05 | P = 0.93 | P = 0.84 |
Findings
PRIMARY COMPARISONS ‐ MICROSCOPY AS THE REFERENCE STANDARD
HRP‐2 antibody‐based tests
Type 1 tests
There were 71 evaluations of Type 1 RDTs verified with microscopy (based on data from 40,062 individuals in 65 cohorts described in 55 publications); forty‐one were conducted in Africa, 28 in Asia and two in South America. The median sample size was 269 (range 30 to 7000), and the median prevalence of falciparum malaria parasitaemia was 30% (range 1% to 92%). Only nine of the 71 evaluations were undertaken exclusively in children under the age of five. Ten different RDT brands were evaluated: Paracheck‐Pf (27), ParaSight (17), ICT Malaria Pf (16), ParaHIT‐F (4), PATH (2), Determine Malaria Pf (1), Rapid Test Malaria (1), Diaspot Malaria (1), New mini‐Pf (1), and Hexagon Malaria (1). The earliest study was published in 1996, with the majority published between 1999 and 2007.
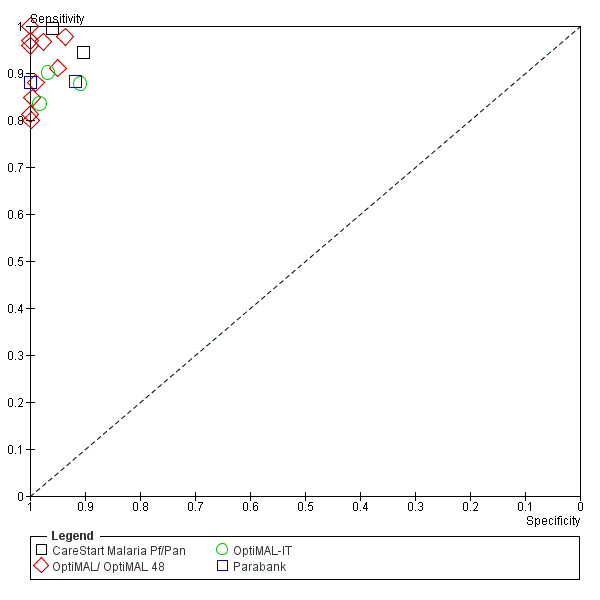
Sensitivities of the tests ranged from 42% to 100%, specificities from 65% to 100% (Figure 3). The meta‐analytical average sensitivity and specificity (95% confidence interval (CI)) were 94.8% (93.1% to 96.1%) and 95.2% (93.2% to 96.7%), respectively, but heterogeneity was noted between studies. Comparing the ten RDT brands in an analysis of the 71 evaluations revealed no statistically significant differences (P = 0.18), although differences may be masked by the high between study heterogeneity (Table 6, see Appendix 4 for extra figures). In an analysis restricted only to the four brands evaluated in more than 1000 patients (Paracheck‐Pf, ParaSight, ICT Malaria Pf, ParaHIT‐F), pairwise comparisons indicated that ICT Malaria Pf was significantly more sensitive than Paracheck‐Pf and ParaSight‐F (97.7% compared to 93.3% and 94.2%, respectively), whilst ParaHIT‐F was significantly more specific than Paracheck‐Pf, ParaSight‐F, and ICT Malaria Pf (98.9% compared to 95.7%, 94.5% and 94.5%, respectively) (see Appendix 5). However, these differences were small and are based on between‐study comparisons, so may have been due to differences between the studies rather than true differences between the test brands.
3.
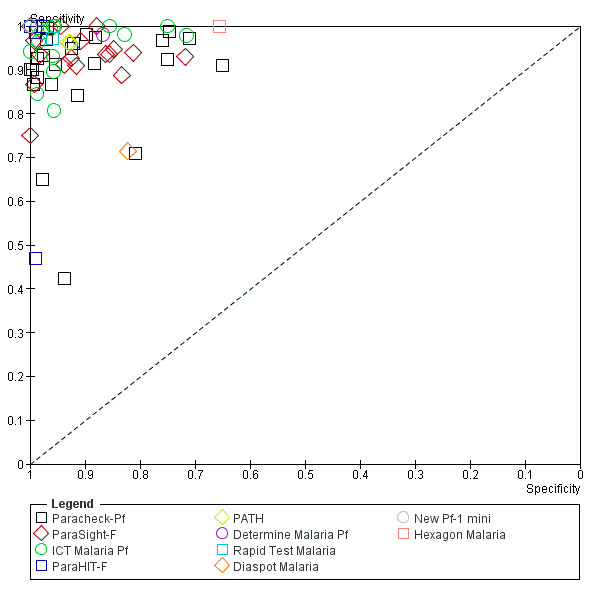
Study results of Type 1 RDTs plotted in ROC space (by RDT brand)
5. RDT types and brands verified with microscopy.
| RDT Brand | Study cohorts (n) | Patients (n) | P. falciparum cases (n) | Pooled sensitivity (95% CI) | Pooled specificity (95% CI) | Test1 |
| Type 1 Brands | ||||||
| Paracheck‐Pf | 27 | 22,319 | 6929 | 93.2 (89.7, 95.6) | 95.6 (92.8, 97.3) | P = 0.15 |
| ParaSight‐F | 17 | 12,521 | 3261 | 94.1 (89.9, 96.6) | 94.6 (90.4, 96.8) | |
| ICT Malaria‐Pf | 16 | 2955 | 1200 | 97.6 (95.5, 98.8) | 94.5 (90.5, 96.9) | |
| ParaHIT‐F | 4 | 1119 | 192 | 92.3 (74.9, 98.0) | 98.9 (94.9, 99.8) | |
| Determine Malaria‐Pf | 1 | 526 | 262 | 98.2 (85.4, 99.8) | 86.8 (35.1, 98.8) | |
| PATH | 2 | 378 | 180 | 96.6 (83.8, 99.3) | 93.3 (68.6, 98.9) | |
| Rapid Test Malaria | 1 | 306 | 36 | 97.8 (70.1, 100.0) | 96.1 (65.6, 99.7) | |
| DiaSpot Malaria | 1 | 153 | 63 | 71.8 (23.1, 95.6) | 82.6 (27.3, 98.4) | |
| Hexagon Malaria | 1 | 119 | 32 | 100.0 (.) | 65.7 (13.4, 96.0) | |
| New Pf‐1 mini | 1 | 10 | 6 | 100.0 (0, 100.0) | 100.0 (.) | |
| Combined2 | 65 | 40,062 | 11,966 | 94.8 (93.1, 96.1) | 95.2 (93.2, 96.7) | |
| Type 2 Brands | ||||||
| ICT Malaria Pf/Pv | 6 | 2255 | 600 | 96.0 (93.6, 97.5) | 95.6 (86.1, 98.7) | P = 1.0 |
| Now Malaria ICT | 2 | 1142 | 190 | 96.0 (91.6, 98.1) | 94.1 (66.6, 99.2) | |
| Combined | 8 | 3397 | 790 | 96.0 (94.0, 97.3) | 95.3 (87.3, 98.3) | |
| Type 3 (too few studies to stratify by brand) | ||||||
| Combined | 5 | 958 | 330 | 99.5 (71.0, 100.0) | 90.6 (80.5, 95.7) | |
| Type 4 Brands | ||||||
| OptiMAL | 10 | 3393 | 833 | 90.1 (86.3, 92.9) | 99.3 (98.0, 99.8) | P = 0.009 |
| Carestart Pf/Pan | 2 | 537 | 240 | 97.8 (94.1, 99.2) | 92.2 (72.4, 98.1) | |
| OptiMAL‐IT | 3 | 1356 | 280 | 87.4 (79.9, 92.4) | 97.0 (88.4, 99.3) | |
| Parabank | 2 | 7918 | 2992 | 87.9 (82.0, 92.0) | 98.8 (90.9, 99.9) | |
| Combined3 | 16 | 13,010 | 4274 | 91.5 (84.7, 95.3) | 98.7 (96.9, 99.5) | |
| Type 5 Brands (too few studies to stratify by brand) | ||||||
| Combined4 | 3 | 1777 | 400 | 98.4 (95.1, 99.5) | 97.5 (93.5, 99.1) | |
1 Likelihood ratio test for evidence of a difference between brands.
2 65 study cohorts evaluated 71 different tests. Only one test (selected randomly) from each cohort is included in the combined analysis.
3 16 study cohorts evaluated 17 different tests. Only one test (selected randomly) from each cohort is included in the overall analysis.
4 HSROC model fitted assuming no correlation between sensitivity and specificity.
Type 2 tests
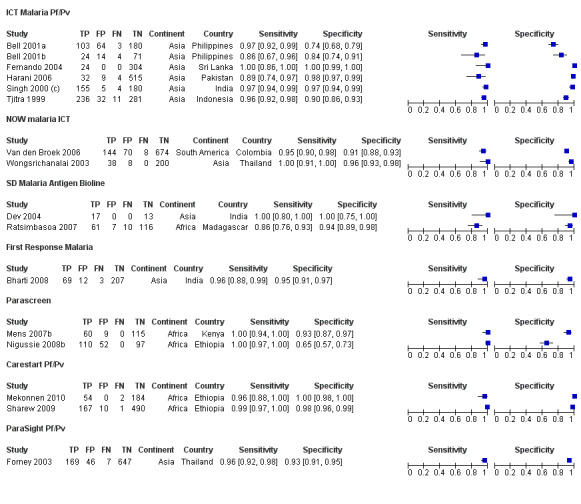
There were eight evaluations of Type 2 RDTs verified with microscopy (based on data from 3397 individuals in eight cohorts described in seven publications); seven were conducted in Asia and one in South America. The median sample size was 347 (range 113 to 896), and the median prevalence of falciparum malaria parasitaemia was 21% (range 6% to 46%). None of the evaluations were undertaken exclusively in children under the age of five. Two different RDT brands were evaluated: ICT Malaria Pf/Pv (6) and NOW ICT Malaria (2). The earliest study was published in 1999, with the majority published between 2000 and 2005.
Sensitivities of the tests ranged from 86% to 100%, specificities from 74% to 100% (Figure 4). The meta‐analytical average sensitivity and specificity (95% CI) were 96.0% (94.0% to 97.3%) and 95.3% (87.3% to 98.3%), respectively. Comparing the two RDT brands in an analysis of the eight evaluations showed no statistically significant differences (P = 1.0) (Table 6, see Appendix 4 for extra figures).
4.
Forest plot of study results of Type 2, 3 and 5 RDTs (by RDT brand)
Type 3 tests
There were five evaluations of Type 3 RDTs verified with microscopy (based on data from 958 individuals in five cohorts described in five publications); three were conducted in Africa and two in Asia. The median sample size was 194 (range 30 to 291), and the median prevalence of falciparum malaria parasitaemia was 37% (range 25% to 57%). One of the evaluations was undertaken exclusively in children under the age of five. Three different RDT brands were evaluated: SD Malaria Antigen Bioline (2), Parascreen (2), and First Response Malaria (1). The earliest study was published in 2004.
Sensitivities of the tests ranged from 86% to 100%, specificities from 65% to 100% (Figure 4). The meta‐analytical average sensitivity and specificity (95% CI) were 99.5% (71.0% to 100%) and 90.6% (80.5% to 95.7%), respectively. There were inadequate data on each RDT brand to make formal statistical comparisons (see Appendix 4 for extra figures).
Type 6 tests
No studies assessed the accuracy of Type 6 RDTs verified with microscopy.
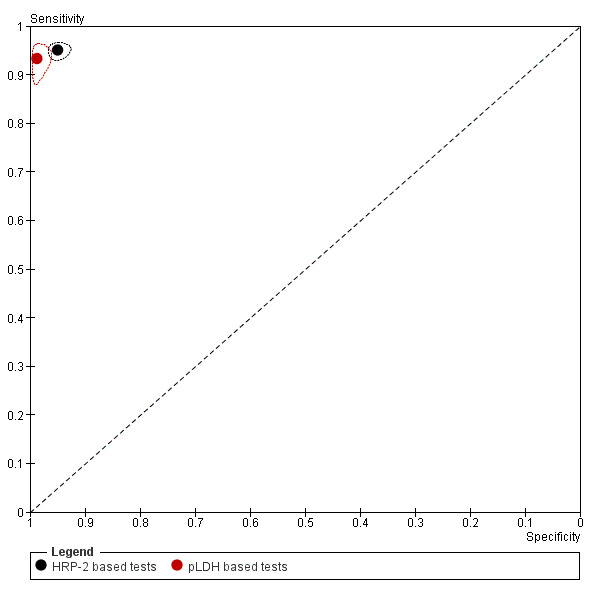
All HRP‐2 antibody based tests
There were 84 evaluations of HRP‐2 tests verified with microscopy (based on data from 43,307 individuals in 75 cohorts described in 64 publications); forty‐two cohorts were conducted in Africa, 31 in Asia and two in South America. The median sample size was 291 (range 30 to 7000), and the median prevalence of falciparum malaria parasitaemia was 26% (range 1% to 84%). Nine of the evaluations were undertaken exclusively in children under the age of five. Sensitivities of the tests ranged from 42% to 100%, and specificities ranged from 65% to 100%. The meta‐analytical average sensitivity and specificity (95% CI) were 95.0% (93.5% to 96.2%) and 95.2% (93.4% to 99.4%), respectively.
pLDH antibody based tests
Type 4 tests
There were 17 evaluations of Type 4 RDTs verified with microscopy (based on data from 13,010 individuals in 16 cohorts described in 14 publications); eight were conducted in Africa, eight in Asia and one in South America. The median sample size was 305 (range 75 to 7000), and the median prevalence of falciparum malaria parasitaemia was 32% (range 2% to 61%). Only four of the 17 evaluations were undertaken exclusively in children under the age of five. Four different brands were assessed: OptiMAL (10), OptiMAL‐IT (3), Parabank (2) and Carestart Malaria Pf/Pan (2). The earliest study was published in 1999, with the majority published between 2003 and 2007.
Sensitivities of the tests ranged from 80% to 100%, specificities from 90% to 100% (Figure 5). The meta‐analytical average sensitivity and specificity (95% CI) were 91.5% (84.7% to 95.3%) and 98.7% (96.9% to 99.5%), respectively. Comparing the four RDT brands in an analysis of the 17 evaluations revealed statistically significant differences (P = 0.009) (Table 6). Carestart Malaria Pf/Pan was observed to have a higher sensitivity and lower specificity than either OptiMAL, OptiMAL‐IT or Parabank (sensitivity of 97.8% compared with 90.1%, 87.4% and 87.9%, respectively; specificity of 92.2% compared with 99.3%, 97.0% and 98.8%, respectively). See Appendix 4 for extra figures. These differences are based on between‐study comparisons, so may have been due to differences between the studies rather than true differences between test brands.
5.
Study results of Type 4 RDTs plotted in ROC space (by RDT brand)
Type 5 tests
There were three evaluations of Type 5 RDTs verified with microscopy (based on data from 1777 individuals in three cohorts described in three publications); two were conducted in Africa, one in Asia and none in South America. The median sample size was 668 (range 240 to 869), and the median prevalence of falciparum malaria parasitaemia was 23% (range 20% to 25%). None of the evaluations were undertaken exclusively in children under the age of five. Two different RDT brands were evaluated: Carestart Pf/Pv (2), and ParaSight Pf/Pv (1). The earliest study was published in 2003.
Sensitivities of the tests ranged from 96% to 99%, specificities from 93% to 100% (Figure 4). The meta‐analytical average sensitivity and specificity (95% CI) were 98.4% (95.1% to 99.5%) and 97.5% (93.5% to 99.1%), respectively. There were inadequate data on each RDT brand to make formal statistical comparisons. See Appendix 4 for extra figures.
All pLDH antibody based tests
There were 20 evaluations of pLDH antibody‐based tests verified with microscopy (based on data from 14,787 individuals in 19 cohorts described in 17 publications); nine cohorts were conducted in Africa, nine in Asia and one in South America. The median sample size was 343 (range 75 to 7000) and the median prevalence of falciparum malaria parasitaemia was 28% (range 2% to 58%). Four of the evaluations were undertaken exclusively in children under the age of five.
Sensitivities of the tests ranged from 80% to 100% and specificities ranged from 90% to 100%. The meta‐analytical average sensitivity and specificity (95% CI) were 93.2% (88.0% to 96.2%) and 98.5% (96.7% to 99.4%), respectively.
Comparisons between RDT types
Statistical comparisons could only be made between Type 1 and Type 4 tests, as the number of studies evaluating other test types was inadequate to provide stable estimates of comparisons in the meta‐analytical models. Models were fitted allowing for different degrees of heterogeneity for the two test types: results for Type 1 were more heterogeneous than Type 4. Significant differences in test accuracy (P = 0.009) were noted between Type 1 and Type 4 RDTs: Type 4 tests tended to have slightly lower sensitivity (P = 0.34) but significantly higher specificity (P < 0.001) than Type 1 tests in the comparisons based on all data (shown graphically in Figure 6). When the analysis was restricted to the seven studies with direct comparisons, the same patterns were evident, but none were statistically significant (Table 7). Based on estimates from all studies, Type 1 tests detect on average three more cases out of every 100 people with malaria than Type 4 tests (P = 0.20), but give on average three more false positive diagnoses for every 100 people without malaria (P < 0.001).
6.
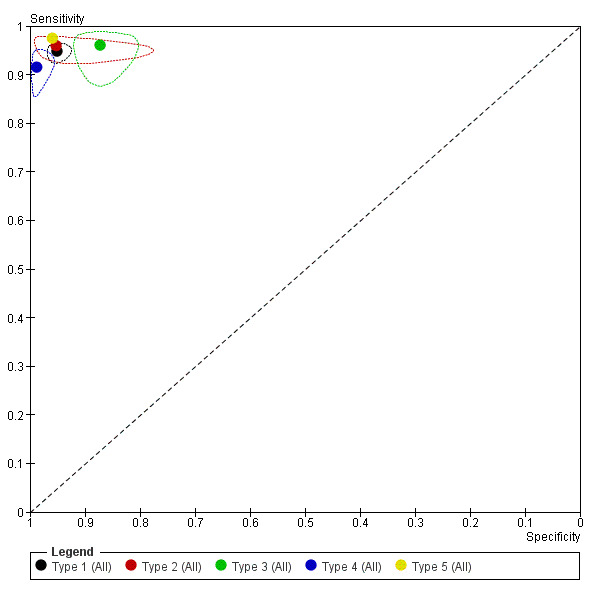
Summary ROC Plot comparing different RDT types verified with microscopy (points are meta‐analytical estimates, regions are 95% confidence regions, no regions could be computed for Type 2 and 5 due to small numbers of studies)
6. Comparison of antibody and RDT types verified with microscopy.
| Number of studies | Number of patients | Number of P. falciparum cases | Pooled sensitivity (95% CI) | Pooled specificity (95% CI) | Test 1 | |
| Antibody‐based test: indirect comparison (using all studies) | ||||||
| HRP‐2 based | 75 | 43,307 | 12,857 | 95.0 (93.5, 96.2) | 95.2 (93.4, 96.6) | |
| pLDH based | 19 | 14,787 | 4674 | 93.2 (88.0, 96.2) | 98.5 (96.7, 99.4) | |
| Ratio | 0.98 (0.94, 1.02), P = 0.34 | 1.03 (1.02, 1.05), P < 0.001 | P = 0.01 | |||
| Antibody‐based test: direct comparison (using only studies that directly compared the two) | ||||||
| HRP‐2 based | 9 | 10,626 | 3672 | 95.6 (90.0, 98.1) | 95.8 (84.7, 98.9) | |
| pLDH based | 9 | 10,623 | 3672 | 94.8 (84.1, 98.2) | 98.1 (87.8, 99.7) | |
| Ratio | 0.99 (0.94, 1.04) P = 0.60 | 1.02 (0.98, 1.07), P = 0.22 | P = 0.35 | |||
| Test type: indirect comparison (using all studies of Type 1 and 4) | ||||||
| Type 1 | 65 | 40,062 | 11,966 | 94.8 (93.0, 96.1) | 95.2 (93.2, 96.7) | |
| Type 4 | 16 | 1,3010 | 4274 | 91.5 (84.7, 95.3) | 98.7 (96.9, 99.5) | |
| Ratio | 0.96 (0.91, 1.02), P = 0.20 | 1.04 (1.02, 1.06), P < 0.001 | P = 0.009 | |||
| Test type: direct comparison (using only comparative studies of Type 1 and 4) | ||||||
| Type 1 | 7 | 9764 | 3433 | 94.5 (88.6, 97.4) | 95.7 (72.2, 99.5) | |
| Type 4 | 7 | 9761 | 3433 | 92.0 (85.7, 94.8) | 98.6 (80.0, 99.9) | |
| Ratio | 0.97 (0.87, 1.09), P = 0.51 | 1.03 (0.95, 1.11), P = 0.31 | P = 0.26 | |||
1Likelihood ratio test for evidence of a difference between test accuracy estimates between antigen and RDT types.
Four further studies provided direct comparisons between tests (Appendix 6). One study showed Type 2 to have higher sensitivity than Type 4, but lower specificity than both Type 4 and Type 1; another study showed that Type 3 tests had higher sensitivity than Type 1. The remaining studies showed no significant differences between types. As these comparisons are based on single small studies, their results should be interpreted with caution.
Comparisons between HRP‐2 and pLDH antibody based RDT Types
RDT types 1 to 3 are all based on HRP‐2 antibodies, while types 4 and 5 are related to detection of pLDH antigen. The process of grouping types based on this antibody classification is dominated by the results of the Type 1 tests (which constitute 65 out of 75 of the included HRP‐2 antibody‐based test studies) and Type 4 tests (which constitute 16 out of 19 of the included pLDH antibody‐based test studies). Nine studies provide direct within‐participant comparisons of HRP‐2 and pLDH test types, eight of which are comparisons of a Type 1 test with a Type 4 test. As for Type 1 and Type 4 tests, it was necessary to allow for different heterogeneity between the test types in the meta‐analytical model.
On average, HRP‐2 antibody‐based tests tend to have slightly higher sensitivity (P = 0.34) but significantly lower specificity (P<0.001) than pLDH antibody‐based tests, based on analysis of all data (Table 7; Figure 7). Differences based on direct comparisons showed the same pattern, but none of the differences were statistically significant. For every 100 malaria cases, around two more are detected with HRP‐2 antibody‐based tests than pLDH antibody‐based tests (P = 0.34 in analysis based on all data, P=0.60 in analysis based on within‐study comparisons), but this is at the cost of four false positives for every 100 people without malaria (P < 0.001 in analysis based on all data, P = 0.22 in analysis based on within‐study comparisons).
7.
Summary ROC Plot comparing HRP‐2‐based and pLDH‐based RDTs across all studies verified with microscopy (points are meta‐analytical estimates, regions are 95% confidence regions)
Investigations of heterogeneity
Heterogeneity investigations were undertaken to test for differences in RDT performance related to age, endemicity, geographical location and the use of an adequate reference standard. Analyses were restricted to the 65 test cohorts in which RDTs of Type 1 were evaluated. Results are presented in Table 8.
7. Investigations of heterogeneity between studies of Type 1 RDTs.
| Number of studies | Number of patients | Number of P. falciparum cases | Pooled sensitivity (95% CI) | Pooled specificity (95% CI) | Test 1 | |
| Age | ||||||
| Mixed ages | 29 | 23,967 | 7536 | 93.8 (90.6, 96.0) | 94.2 (90.7, 96.5) | P = 0.41 |
| Children only | 9 | 2261 | 907 | 94.1 (87.2, 97.4) | 93.4 (84.6, 97.3) | |
| Not stated | 27 | 13,834 | 3523 | 95.9 (93.4, 97.5) | 96.2 (93.7, 97.8) | |
| Endemicity | ||||||
| Low | 51 | 29,305 | 7671 | 95.1 (93.1, 96.6) | 95.9 (94.1, 97.2) | P = 0.22 |
| High | 10 | 1824 | 806 | 93.7 (87.0, 97.1) | 89.6 (78.3, 95.3) | |
| Mixed | 4 | 8933 | 3489 | 93.2 (81.1, 97.8) | 92.5 (76.5, 97.9) | |
| Adequate reference standard | ||||||
| No | 15 | 5499 | 1869 | 93.7 (88.6, 96.6) | 95.5 (91.1, 97.7) | P = 0.34 |
| Unclear | 32 | 13,481 | 3439 | 95.4 (92.8, 97.1) | 96.2 (93.9, 97.7) | |
| Yes | 18 | 21,082 | 6658 | 94.6 (90.9, 96.9) | 92.1 (86.0, 95.7) | |
| Continent | ||||||
| Africa | 39 | 21,958 | 7445 | 94.0 (91.3, 95.9) | 93.0 (89.8, 95.3) | P = 0.01 |
| Asia | 24 | 1,5810 | 4060 | 96.7 (93.7, 97.8) | 96.7 (94.4, 98.1) | |
| South America | 2 | 2294 | 461 | 88.7 (61.9, 97.4) | 99.4 (96.4, 100.0) | |
| Continent (South America excluded) | ||||||
| Africa | 39 | 21,958 | 7445 | 94.0 (91.2, 96.0) | 93.1 (89.7, 95.3) | P = 0.03 |
| Asia | 24 | 15,810 | 4060 | 96.4 (93.7, 97.9) | 96.6 (94.0, 98.1) | |
1Likelihood ratio test for model with and without the covariate.
Nine study cohorts only recruited children aged five years or under, 28 recruited mixed age groups, and in 27 age distributions were not described. No difference in test accuracy was noted by age category (P = 0.41).
Fifty‐one study cohorts were in low endemicity areas, 10 in high areas, and three were categorized as being in areas of mixed endemicity. Although specificity appeared to be lower in high endemicity areas, the differences were not statistically significant (P = 0.22).
Significant differences were seen by continent, with lower sensitivity (by 2.7%) and specificity (by 3.7%) in Africa than Asia (P = 0.01). Results from the South American studies showed very high specificity (99.4%) and low sensitivity (88.7%), but should be judged with caution due to only two studies being available.
Fifteen of the Type 1 study cohorts used inadequate reference standards and in 32 the reference standard was unclear, but their results did not differ significantly from the 17 with adequate reference standards (P = 0.34).
Sensitivity analysis
For all the above analyses, a sensitivity analysis was undertaken by including the one study in the review (Hopkins 2008b) that used PCR‐adjusted microscopy as the reference standard; its inclusion made no difference to any of the findings.
OTHER ANALYSES
Use of PCR as a reference standard
Five study cohorts (from four studies) used PCR as a reference standard: two Type 1 RDTs (ParaSight‐F and ParaHIT‐F), one Type 3 RDT (SD Malaria Antigen Bioline), one Type 4 RDT (OptiMAL‐IT) and one Type 6 RDT (PALUTOP). Comparisons were made with the corresponding microscopy evaluations for the first four of these tests (Appendix 7). Use of PCR as a reference standard reduced estimates of the sensitivity of the RDTs but increased estimates of specificity compared with the microscopy‐based reference standard for three of the four studies in which comparison was possible.
For two studies, results are available separately using microscopy and PCR reference standards (Banchongaksorn 1996b; Nicastri 2009b). In one study (Banchongaksorn 1996a; Banchongaksorn 1996b), both sensitivity and specificity for PCR and microscopy were within 1% of each other. In the other (Nicastri 2009a; Nicastri 2009b), specificities were 99% when verified by microscopy and 100% when verified by PCR; sensitivity verified with microscopy was 47% (95% CI 29% to 65%) compared with 72% (95% CI, 51% to 88%) for PCR. In this study with 336 participants, 26 were positive for malaria by PCR, 32 by microscopy and 18 by RDT, suggesting a relatively high rate of false positives for microscopy in the context of a low prevalence.
Five of the included studies presented data, in addition to the comparisons included in the review, on the accuracy of their microscopy reference standard against PCR (excluding one study with only two microscopy positive cases). In three studies, where the quality of the microscopy was unclear (Gaye 1999; Mens 2007b; Nicastri 2009b), sensitivity of microscopy against PCR varied between 69% and 89%; in two studies with adequate quality microscopy (Banchongaksorn 1996b; Rakotonirina 2008), sensitivity varied between 90% and 96%. Specificity of microscopy against PCR was high in all five studies, varying between 96% and 100%.
Comparing the accuracy of RDTs and local standard microscopy
In addition to the comparison of RDT against the 'gold standard' microscopy, seven of the included studies presented a comparison of local microscopy against reference standard microscopy. These studies reported widely differing results: one study showed local microscopy services to be slightly more accurate than RDTs (Kolaczinski 2004); three studies showing local microscopy to be extremely inaccurate, with very low specificities of 0% (A‐Elgayoum 2009) to 25% (Tagbo 2007), or a sensitivity so low that only around half of cases were detected (De Oliveira 2009); and the others were intermediate but favouring RDTs. The findings of the two studies with an adequate reference standard are presented in Appendix 8.
Discussion
Malaria diagnosis and treatment policies have shifted rapidly over the past few years. In 2006, in its guidelines on malaria treatment, the WHO abandoned presumptive treatment with ineffective or only partly effective treatments for the new ACTs. Now, in the second (2010) edition of these guidelines, parasitological diagnosis is expected (WHO 2010): "prompt parasitological confirmation by microscopy or alternatively by RDTs is recommended in all patients suspected of malaria before treatment is started". In primary care in most developing countries, prompt, accurate results from microscopy can't be delivered efficiently, and so demonstrating the sensitivity and specificity of these tests helps reassure policy makers pushing investment in and purchase of this technology.
For P. falciparum malaria, targeting treatment will help to reduce unnecessary drug use and thus help to avoid the development of drug resistance. The test will also help health workers exclude malaria as a cause of fever and thus improve the diagnosis and treatment of other infections. In addition, as malaria control improves as a result of all the new approaches including use of ACTs (Sinclair 2009) and other preventive measures such as impregnated mosquito nets (Lengeler 2004), transmission will drop, immunity will drop and thus prompt detection and treatment becomes even more important for reducing severe illness.
Thus, the current policy question is: how well do RDTs perform in diagnosing symptomatic patients compared to the previous standard of microscopy? There are subsidiary questions about how well the various types and individual commercial tests perform against microscopy and against each other. This information will help to inform choice, although factors such as price, product consistency, stability, and shelf life will also influence those decisions. In addition, areas vary in relation to malaria species not detected by these tests (P. vivax and other non‐falciparum malaria species). Thus the choice of commercial product will also depend on whether it is important for clinicians to detect these species. For example, as malaria eradication proceeds and endemicity of malaria falls, being able to detect P. vivax is likely to become more important. In these circumstances, the sensitivity and specificity of the commercial product to P. vivax may be a factor in the choice of product. This is the subject of a forthcoming Cochrane review.
Summary of main results
The main results are summarized in the Summary of Results table (Table 1).
There is a large volume of research on the accuracy of RDTs in malaria endemic countries that required meta‐analysis.
In diagnosing P. falciparum malaria, all tests performed reasonably well. Most studies identified for the current review were carried out on Type 1 (HRP‐2) and Type 4 (pLDH) test, with fewer reports available on the other HRP‐2 tests (Types 2 and 3) and the other pLDH tests (Type 5).
There is a trade‐off between sensitivity and specificity for Type 1 and Type 4 tests. Type 1 tests were falsely negative in about 5% of P. falciparum cases and were falsely positive in about 5% of people without P. falciparum. Type 4 tests were falsely negative in 8% to 9% of cases but were falsely positive only in about 1% of non‐malaria cases. The results are mirrored by the available direct within‐study comparisons between tests (although results were not statistically significant). There were only two brands of Type 1 and Type 4 tests that failed to follow these patterns. These findings support the results of laboratory‐based testing undertaken by WHO (WHO 2010a), and probably reflect the different antigens used by different test types. The lower specificity of Type 1 tests may be due to the use of HRP‐2 antibodies, which can give a false positive result in cases where a person has recently been successfully treated for P. falciparum malaria, due to persistent antigenaemia. Analysis of all HRP‐2 antibody‐based tests and all pLDH antibody‐based tests was undertaken and gave similar results, but was dominated by Type 1 and Type 4 tests.
The sensitivities and specificities of Type 2, Type 3 and Type 5 tests were similar to those of Type 1 and Type 4 tests, but these three types have not been evaluated widely and robust comparisons are not possible.
Studies of Type 1 tests conducted in Africa reported slightly lower estimates of sensitivity and specificity than those conducted in Asia. The reasons for this are unclear, and may relate to the relative quality of the studies conducted in different locations, but are most likely due to higher rates of transmission and persistent antigenaemia in Africa.
Reporting of studies is variable: 40% reported an adequate reference standard, 40% did not provide enough information to assess the quality of the reference standard and 20% reported an inadequate reference standard. Other published studies were excluded from the review due to inadequate reporting. It would be helpful in the future for diagnostic test accuracy studies to be more carefully reported on, using the STARD (Bossuyt 2003) criteria, to ensure their inclusion in meta‐analyses.
Application of meta‐analysis to hypothetical cohort
Table 1 (Table 1) summarizes the findings of the review and applies them to two hypothetical cohorts of 1000 symptomatic patients. In one of the cohorts, the prevalence of P. falciparum malaria parasitaemia is 30%, while in the other cohort it is 50%.
Falciparummalaria prevalence at 30%: on average, a Type 1 test would miss 16 P. falciparum cases, while a Type 4 test would miss 26 cases. In contrast, a Type 1 test would wrongly identify 34 non‐cases as having falciparum malaria, whereas a Type 4 test would only wrongly identify nine non‐cases as falciparum malaria.
Falciparummalaria prevalence at 50%: on average, a Type 1 test would miss 26 cases of falciparum malaria, while a Type 4 test would miss 43 cases. In contrast, a Type 1 test would wrongly identify 24 non‐cases as having falciparum malaria, whereas a Type 4 test would only wrongly identify seven non‐cases as falciparum malaria.
At very low and very high falciparum malaria prevalence: the sensitivity advantage of Type 1 tests, in terms of cases not missed, is less. For example, where prevalence is 10%, Type 1 tests would result in five cases being missed and 43 non‐cases incorrectly identified as falciparum malaria. At higher prevalence, the greater sensitivity of Type 1 tests makes a greater difference; at 80% prevalence, Type 1 tests would result in 42 missed cases compared with 68 missed cases with Type 4 tests.
The numbers of false positives presented should be viewed with caution, as some RDTs may be more sensitive than microscopy.
Strengths and weaknesses of the review
The results of this review are based on strict and careful searching, study inclusion, and data extraction. The strength of this review is that it allows an assessment to be made between types and brands of test, and also provides an accurate assessment of the trade‐offs.
Completeness of evidence
This is a reasonably complete data set. We excluded 18 potentially eligible studies not published in English, 17 studies that did not provide enough information to accurately assess whether they met our inclusion criteria, and 12 studies that gave only calculated values where imputation was not possible. However, it is known that studies of diagnostic test accuracy tend to be poorly indexed (Whiting 2009), and we may therefore have missed some studies despite the comprehensive search; in fact, two of the included studies were identified only in an earlier, scoping search.
Accuracy of the reference standards used:
Microscopy is regarded as the gold standard for malaria, and hence is the primary comparison, although PCR may be more sensitive. Comparisons of microscopy and PCR showed that microscopy was highly accurate when the microscopy methods were classified as 'adequate', but less accurate when the microscopy methods were of poorer quality. However, the quality of the microscopy did not explain any heterogeneity in the meta‐analysis of Type 1 tests and therefore is unlikely to be an important factor in the interpretation of the study findings.
Quality and quality of reporting of the included studies:
Many of the included studies was not well reported. For example, reference standards were often not well described, there was often insufficient methodological detail, and numbers sometimes did not add up.
Only 40% of the included studies reported an adequate reference standard and 20% reported an inadequate reference standard. In Type 1 test studies, which were generally older and of lower quality, only 25% reported an adequate reference standard. As the quality of the reference standard did not explain heterogeneity in this analysis, it seems unlikely that including studies with an unclear or inadequate reference standard caused any kind of bias. In addition, only half of the included studies were explicit about patient recruitment involving a consecutive or random series of patients. Blinding of the index and reference tests was reported in the majority of studies (65% and 70%, respectively). Only 60% of studies explained withdrawals or stated that there were none. Sampling did not seem to be a significant problem, as the tests were taken at the same time, and few lost or uninterpretable test results were reported.
Interpretability of subgroup analyses:
The subgroup analysis is interpreted in relation to the antigen type, test type, and brand, and appears to make sense, although a confounding effect of quality over time cannot be excluded with the newer tests. The differences in specificity observed between HRP‐2 and pLDH antibody‐based tests are significant and replicate those found in systematic laboratory‐based in vitro studies (WHO 2010a).
Completeness and relevance of the review:
This review covers P. falciparum malaria only, and stands alone as relevant to areas where P. falciparum malaria predominates. A further Cochrane diagnostic review in this series will cover P. vivax and other non‐falciparum malaria species.
Applicability of findings to the review question
We found no important differences in accuracy between different RDT brands within the same type. Where significant differences between tests were found, these differences were small, and were based on weaker between‐study comparisons. For some types, there were insufficient data to analyse differences between brands.
We found Type 1 RDTs to be more sensitive than Type 4, and HRP‐2 antibody‐based tests to be more sensitive than pLDH antibody‐based tests, although the differences were not statistically significant. The direction of this finding corresponds closely with a similar analysis in a diagnostic test accuracy review of RDTs for travellers with fever returning from malaria endemic areas to non‐endemic areas(Marx 2005). It also corresponds with laboratory‐based testing undertaken by WHO (WHO 2010a), where Type 1 tests had a lower threshold for detection of parasitaemia than Type 4 tests. However, Type 4 tests and pLDH antibody‐based tests tended to be more specific, and this difference was significant.
This research assesses sensitivity and specificity in applied research settings. In the field, the quality of microscopy is likely to be lower and the RDTs may not be read so accurately (Hawkes 2009). Further research is required on effective implementation of RDTs, as they can only influence clinical practice if the results are believed and acted upon. There may be a reluctance on the part of both health providers and patients to believe negative RDT results, leading to unnecessary prescribing of antimalarials for negative cases (Tavrow 2000). Trials in this area are in the process of being summarized (Odaga 2011).
The consequences of a false positive are that someone may be treated for malaria when they are not infected. The consequences of a false negative in an endemic area, particularly when related to low parasitaemia, means the patient is unlikely to die. The infection may clear by itself, as people living in endemic areas have partial immunity; if it does not, the illness will recur and they would seek care again.
Authors' conclusions
Implications for practice.
The high sensitivity and specificity of RDTs means they can replace or augment microscopy for diagnosing P. falciparum malaria.
The performance of RDT types varied but the differences were not large. HRP‐2‐based tests tended to be more sensitive and were significantly less specific than pLDH‐based tests. Choice will depend on prevalence of malaria, and we provide data in this review to assist these decisions, although policy makers will also take into account other factors relating to cost and test stability.
Implications for research.
Future studies should include comparisons between new RDTs and commonly‐used Type 1 and/or Type 4 RDTs in the same patients.
Studies should be reported according to the STARD guidelines (Bossuyt 2003), which will also facilitate incorporation into meta‐analysis.
Further research on effective implementation of RDTs within routine clinical practice is needed.
Feedback
Duplication of test, 3 August 2011
Summary
In the background section, under the heading Alternative tests, the same information is repeated as in the previous section Reference tests.
Reply
The duplicated text has been removed and the problem resolved. Many thanks for pointing this out.
Contributors
K Abba
What's new
| Date | Event | Description |
|---|---|---|
| 1 December 2011 | Feedback has been incorporated | An observant reader noticed that one paragraph in the background section was repeated. This has been removed. |
History
Protocol first published: Issue 4, 2009 Review first published: Issue 7, 2011
| Date | Event | Description |
|---|---|---|
| 6 July 2011 | Amended | Plain language summary added. |
Notes
The CIDG editors responsible for editing this review were Dr Hasifa Bukirwa and Dr Hellen Gelband.
Acknowledgements
This research was funded through a grant from the UK Department for International Development (DFID) for the benefit of developing countries.
Appendices
Appendix 1. Appendix 1. Search strategy
| Search set | MEDLINE | EMBASE | |||
| 1 | Exp Malaria[MeSH] | Exp Malaria [Emtree] | |||
| 2 | Exp Plasmodium [MeSH] | Exp Plasmodium [Emtree] | |||
| 3 | Malaria ti, ab | Malaria ti, ab | |||
| 4 | 1 or 2 or 3 | 1 or 2 or 3 | |||
| 5 | Exp Reagent kits, diagnostics [MeSH] | Exp Diagnostic procedures [Emtree] | |||
| 6 | rapid diagnos* test* ti, ab | rapid diagnos$ test$ ti, ab | |||
| 7 | RDT ti, ab | RDT ti, ab | |||
| 8 | Dipstick* ti, ab | Dipstick$ ti, ab | |||
| 9 | Rapid diagnos* device* ti, ab | Rapid diagnos$ device$ ti, ab | |||
| 10 | MRDD ti, ab | MRDD ti, ab | |||
| 11 | OptiMal ti, ab | OptiMal ti, ab | |||
| 12 | Binax NOW ti, ab | Binax NOW ti, ab | |||
| 13 | ParaSight ti, ab | ParaSight ti, ab | |||
| 14 | Immunochromatograph* ti, ab | Immunochromatography [Emtree] | |||
| 15 | Antigen detection method* ti, ab | Antigen detection method$ ti, ab | |||
| 16 | Rapid malaria antigen test* ti, ab | Rapid malaria antigen test$ ti, ab | |||
| 17 | Combo card test* ti, ab | Combo card test$ ti, ab | |||
| 18 | Immunoassay [MeSH] | Immunoassay [Emtree] | |||
| 19 | Chromatography [MeSH] | Chromatography [Emtree] | |||
| 20 | Enzyme‐linked immunosorbent assay [MeSH] | Enzyme‐linked immunosorbent assay [Emtree] | |||
| 21 | Rapid test* ti, ab | Rapid test$ ti, ab | |||
| 22 | Card test* ti, ab | Card test$ ti, ab | |||
| 23 | Rapid AND (detection* or diagnos*) ti, ab | Rapid AND (detection$ or diagnos$) ti, ab | |||
| 24 | 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 | 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 | |||
| 25 | 4 and 19 | 4 and 19 | |||
| 26 | Limit 20 to Humans | Limit 20 to Human | |||
| Search set | Web of Science | LILACS | Medion | African Index medicus | IndMed |
| 1 | Malaria (topic) | Malaria | Malaria | Malaria | Malaria |
| 2 | Plasmodium falciparum (topic) | Plasmodium falciparum | Diagnos* Or RDT OR (rapid diagnos*) | Plasmodium | Plasmodium |
| 3 | 1 or 2 | 1 or 2 | 1 or 2 | 1 or 2 | |
| 4 | Rapid diagnostic test* (topic) | Rapid diagnostic test$ | Diagnos* | Diagnos* | |
| 5 | RDT (topic) | RDT | dipstick | dipstick | |
| 6 | Parasight (topic) | Parasight | combo | combo | |
| 7 | Immunochromatography (topic) | Immunochromatograp$ | Card test | Card test | |
| 8 | Parasight (topic) | Parasight | parasight | parasight | |
| 9 | Dipstick (topic) | Dipstick | RDT | RDT | |
| 10 | Binax (topic) | Binax | 4 or 5 or 6 or 7 or 8 or 9 | 4 or 5 or 6 or 7 or 8 or 9 | |
| 11 | 4 or 5 or 6 or 7 or 8 or 9 or 10 | 4 or 5 or 6 or 7 or 8 or 9 or 10 | 3 and 10 | 3 and 10 | |
| 12 | 3 and 11 | 3 and 11 |
Appendix 2. Data extraction: characteristic of included studies
| Study ID | First author, year of publication |
| Clinical features and settings | Presenting signs and symptoms, previous treatments for malaria, clinical setting |
| Participants | Sample size, age, sex, co‐morbidities or pregnancy, country and locality, P. falciparum malaria endemicity, endemic malaria species, average parasite density in microscopy positive cases |
| Study design | Were consecutive patients enrolled retrospectively or prospectively? |
| Whether the sampling method was consecutive or random, or whether the method was not described but consecutive sampling was most probable | |
| If the study evaluated more than one RDT, how were tests allocated to individuals, or did each individual receive all the tests? | |
| Target condition | Malaria parasitaemia |
| Reference standard | The reference standard test(s) used |
| If microscopy was used, who performed it, and where? | |
| If microscopy was used, how many high power fields were looked at? | |
| If microscopy was used, how many observers or repeats were used? | |
| If microscopy was used, how were discrepancies between observers resolved? | |
| Index tests | The parasite species the test was designed to detect, the commercial name, and the type of test. Batch numbers if provided. Transport and storage conditions. Details of the test operators, including any special training provided. |
| Notes | Source of funding. |
Appendix 3. Data extraction and criteria for judgement: methodological quality
| Quality Indicator | Notes |
| Was the spectrum of patients representative of the spectrum of patients who will receive the test in practice? | 'Yes' if the inclusion criteria clearly stipulated people attending an ambulatory healthcare setting with symptoms of malaria, and the sampling method was consecutive or random. 'No' if the sample was unrepresentative of people with uncomplicated malaria in general (for example, if the majority of participants also had some other presenting health problem, such as pneumonia). Where a proportion of potential participants were excluded due to recent antimalarial use, well defined co‐morbidities or pregnancy, the sample could be classed as representative, because these groups may also be excluded from testing as normal clinical practice, depending on local policy and practice. 'Unclear' if the source or characteristics of participants was not adequately described; or if the sampling method was not described. |
| Is the reference standard likely to correctly identify the target condition? | 'Yes' if microscopy was undertaken by experienced microscopists with adequate laboratory facilities. Laboratory facilities were assumed to be adequate unless the study report indicated otherwise. Slides were viewed by at least two independent observers, either for all slides or for those where there were discordant results between the index and the reference test. At least 100 microscopic fields were viewed before declaring a slide negative. 'Yes' if reference standard was PCR. 'No' if microscopy was undertaken by insufficiently trained individuals, by one individual only, or in a situation with inadequate equipment, or if they viewed less than 100 microscopic fields before declaring negative. 'Unclear' if insufficient information was provided. |
| Is partial verification avoided? | 'Yes' if all participants who received the index test also received the reference test. 'No' if not all the participants who received the index test also received the reference test. 'Unclear' if insufficient information was provided to assess this. If not all participants received the reference test, we reported how many did not. |
| Is differential verification avoided? | 'Yes' if the same reference test was used regardless of the index test results. 'No' if different reference tests were used depending on the results of the index test. 'Unclear' if insufficient information was provided. If any participants received a different reference test, we reported the reasons stated for this, and how many participants were involved. |
| Is incorporation avoided? (the index test does not form part of the reference standard) | Should be ‘Yes’ for all studies, as the reference standard is defined in the inclusion criteria as microscopy or PCR. |
| Are the reference standard test results blinded? | 'Yes' if the person undertaking the reference test did not know the results of the index tests, if the two tests were carried out in different places, or it was clear that the reference test was undertaken and the results recorded before the index test. 'No' if the same person performed both tests, or if the results of the index tests were known to the person undertaking the reference tests. 'Unclear' if insufficient information was provided. |
| Are the index test results blinded? | 'Yes' if the person undertaking the index test did not know the results of the reference tests, or if the two tests were carried out in different places, or it was clear that the index test was undertaken and the results recorded before the reference test. 'No' if the same person performed both tests, or if the results of the index tests were known to the person undertaking the reference tests. 'Unclear' if insufficient information was provided. |
| Were uninterpretable results reported? | 'Yes' if the paper stated whether there were any uninterpretable or invalid results, and how those were handled; for example whether they were repeated until a valid result was obtained, or excluded from the analysis. 'No' if the number of participants presented in the analysis did not match the number of participants originally enrolled in the study, and insufficient explanation was provided for any discrepancy. 'Unclear' if uninterpretable or invalid test results were not mentioned, but the number of participants presented in the analysis corresponded to the number of participants reported to be originally recruited into the study, or if insufficient information was given to permit this judgement; for example if the original number of participants recruited into the study was unclear. We reported how many results were uninterpretable (of the total), and how these were handled in the analysis. |
| Were any withdrawals explained? | 'Yes' if it was clear that no participants were excluded from the analysis (the number of participants originally enrolled was clearly stated, and corresponded to the number presented in the analysis) or if exclusions were adequately described. 'No' if there were participants missing or excluded from the analysis and there was no explanation given; usually where the number of participants reported to have been enrolled and the number presented in the analysis did not correspond. 'Unclear' if not enough information was given to assess whether any participants were excluded from the analysis; for example if the original number of participants recruited into the study was unclear. We reported how many participants were excluded from the analysis. |
Appendix 4. Extra figures
Estimates of average sensitivity and specificity for Type 1 RDT brands (Figure 48)
8.
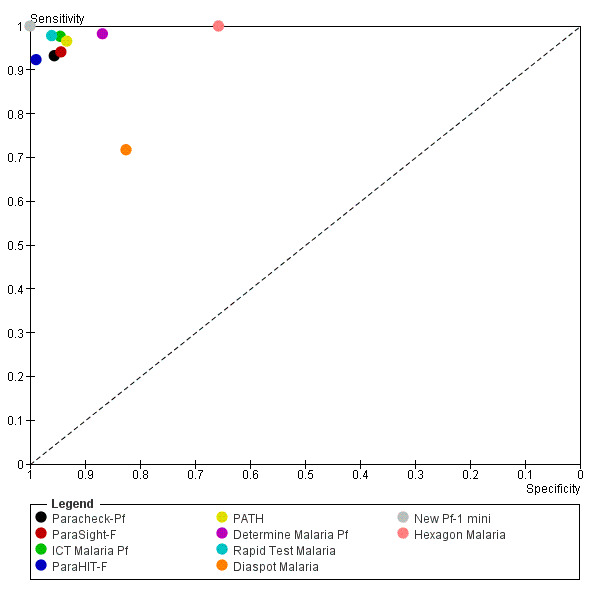
Summary estimates of Type 1 RDTs plotted in ROC space (by RDT brand)
Estimates of average sensitivity and specificity for Type 4 RDT brands (Figure 49)
9.
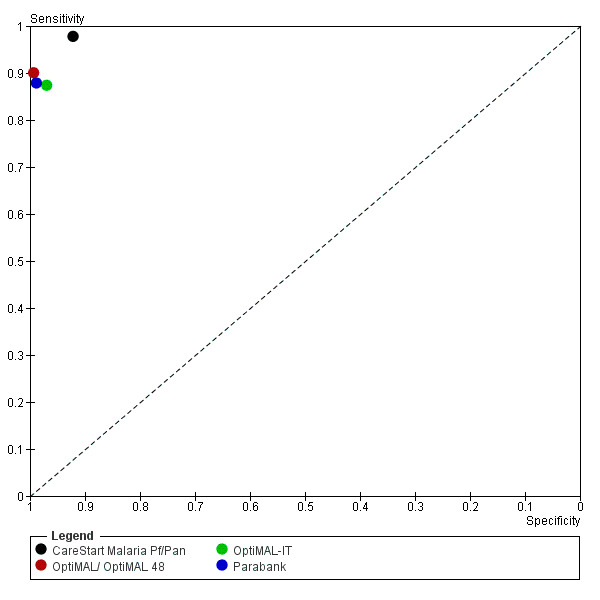
Summary estimates of Type 4 RDTs plotted in ROC space (by RDT brand)
ROC plot of study results for Type 2, 3 and 5 RDT brands (Figure 50)
10.
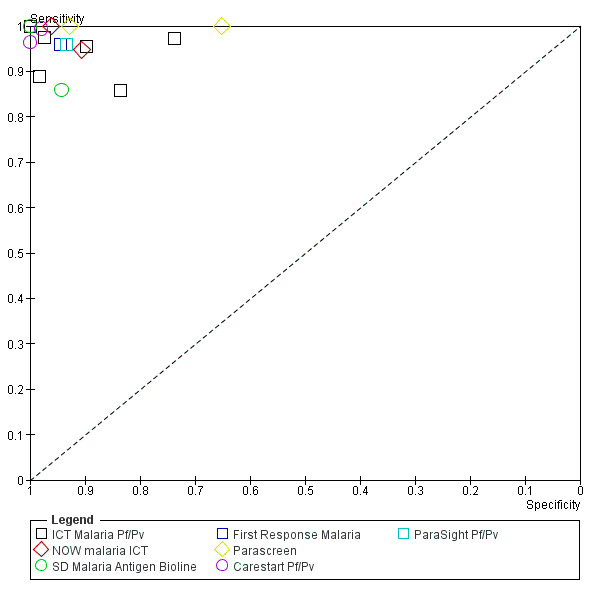
Study results of Type 2, 3 and 5 RDTs plotted in ROC space (by RDT brand)
Study results and estimates of average sensitivity and specificity for Type 2 RDTs (Figure 51)
11.
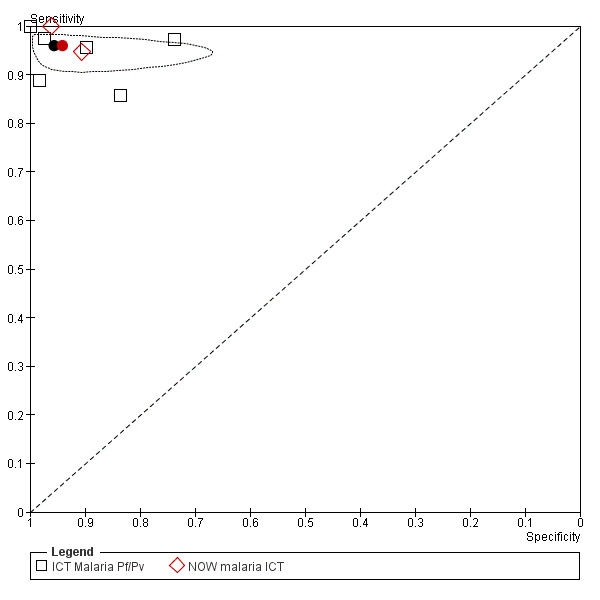
Summary estimates of Type 2 RDTs and study results plotted in ROC space (by RDT brand)
Study results and estimates of average sensitivity and specificity for Type 3 RDTs (Figure 52)
12.
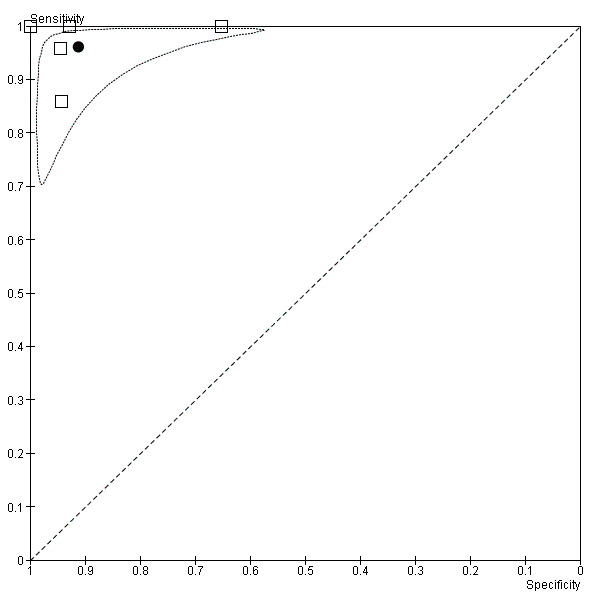
Summary estimates of Type 3 RDTs and study results plotted in ROC space
Study results and estimates of average sensitivity and specificity for Type 5 RDTs (Figure 53)
13.
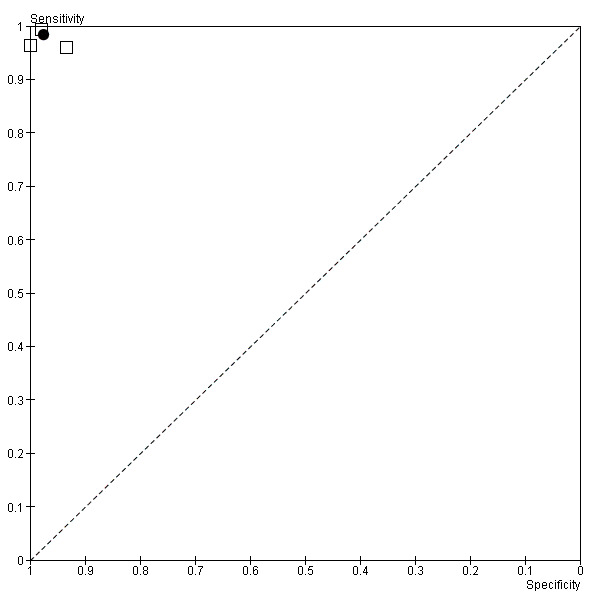
Summary estimates of Type 5 RDTs and study results plotted in ROC space
ROC plot of paired results which compare Type 1 and Type 4 RDT brands (Figure 54)
14.
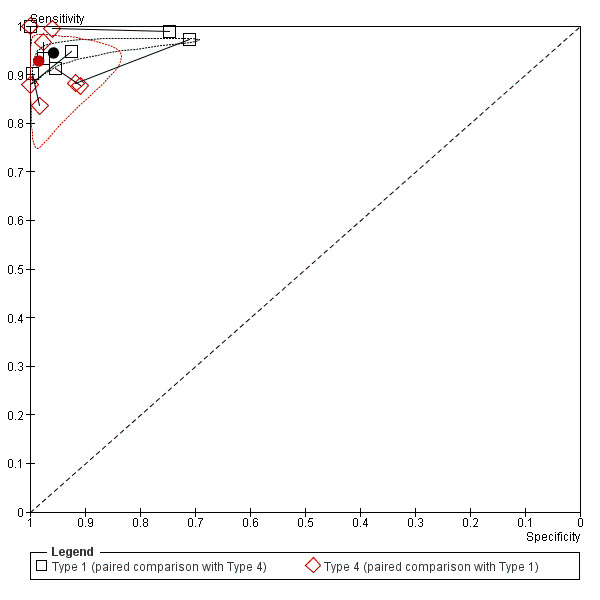
Paired comparison of Type 1 and Type 4 RDTs. Connecting lines link the direct comparison of pairs of tests in each study.
ROC plot of paired results which compare HRP‐2‐based tests and pLDH‐based tests(Figure 55)
15.
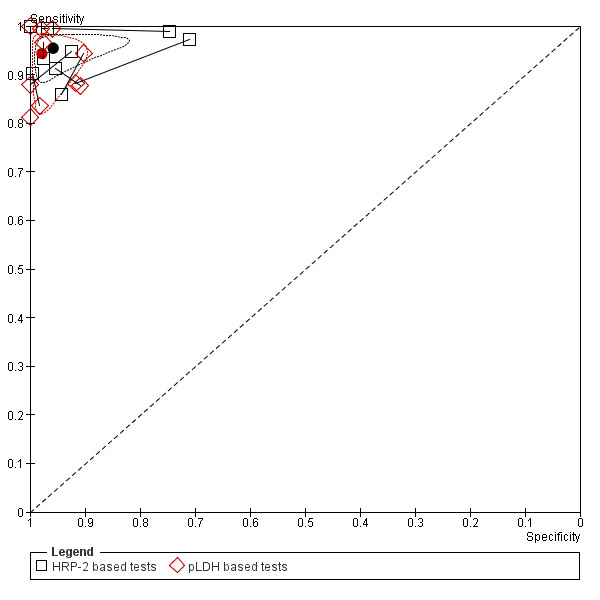
Paired comparison of HRP‐2‐based tests and pLDH‐based tests. Connecting lines link the direct comparison of pairs of tests in each study.
Appendix 5. Type 1 RDT brands evaluated in more than 1000 participants
|
Ratio of sensitivity (95% CI) P value for comparison Ratio of specificity (95% CI) P value for comparison |
Paracheck‐Pf | ParaSight‐F | ICT Malaria‐Pf | ||
| Studies (participants) | 27 (22,319) | 17 (12,591) | 16 (2955) | ||
| Studies (participants) |
Sensitivity % (95% CI) Specificity % (95% CI) |
93.3 (89.7,95.7) 95.7 (92.7,97.5) |
94.2 (89.8,96.8) 94.5 (90.3,96.9) |
97.7 (95.5,98.8) 94.5 (90.4,97.0) |
|
| ParaSight‐F | 17 (12,591) | 94.2 (90.1,96.7) 94.9 (91.0,97.1) |
1.01 (0.96,1.06) P = 0.67 0.99 (0.95,1.03) P = 0.67 |
‐ | ‐ |
| ICT Malaria‐Pf | 16 (2955) | 97.7 (95.5,98.8) 94.7 (90.7,97.1) |
1.05 (1.01,1.08) P = 0.01 0.99 (0.95,1.03) P = 0.63 |
1.04 (1.00,1.07) P = 0.05 1.00 (0.97,1.03) P = 0.93 |
‐ |
| ParaHIT‐F | 4 (1119) | 92.6 (74.3,98.2) 98.9 (94.4,99.8) |
0.99 (0.89,1.11) P = 0.89 1.03 (1.00,1.07), P = 0.03 |
0.98 (0.88,1.10) P = 0.76 1.04 (1.01,1.08) P = 0.02 |
0.95 (0.85,1.06) P = 0.33 1.04 (1.01,1.08) P = 0.02 |
Appendix 6. Additional direct comparisons between test types
| Sensitivity | Specificity | |||||||
| TP/diseased | P value | change | TN/not diseased | P value | change | |||
| Type 2 vs Type 1 | Type 2 | Type 1 | Type 2 | Type 1 | ||||
| Van den Broek 2006 | 144/152 | 137/152 | P = 0.19 | +4.6% (‐1.3% to +10.5%) | 674/744 | 740/744 | P < 0.001 | ‐8.9% (‐11.0% to ‐6.7%) |
| Type 2 vs Type 4 | Type 2 | Type 4 | Type 2 | Type 4 | ||||
| Van den Broek 2006 | 144/152 | 127/152 | P = 0.003 | +11.1% (+4.3% to +18.1%) | 674/744 | 731/744 | P < 0.001 | ‐7.7% (‐10.0% to ‐5.4%) |
| Type 3 vs Type 1 | Type 3 | Type 1 | Type 3 | Type 1 | ||||
| Mens 2007b | 60/60 | 113/127 | P = 0.006 | +11.0% (+5.6% to +16.5%) | 115/124 | 678/711 | P = 0.26 | ‐2.6% (‐7.4% to +2.2%) |
| Dev 2004 | 17/17 | 21/21 | P = 1.00 | 0% (not estimable) | 13/13 | 9/9 | P = 1.00 | 0% (not estimable) |
| Type 3 vs Type 4 | Type 3 | Type 4 | Type 3 | Type 4 | ||||
| Mens 2007b | 60/60 | 58/60 | P = 0.50 | +3.3% (‐1.2% to +7.9%) | 115/124 | 121/124 | P = 0.14 | ‐4.8% (‐10.1% to +0.5%) |
| Dev 2004 | 17/17 | 69/85 | P = 0.07 | +18.8% (+10.5% to +27.1%) | 13/13 | 54/54 | P = 1.00 | 0% (not estimable) |
| Type 5 vs Type 1 | Type 5 | Type 1 | Type 5 | Type 1 | ||||
| Sharew 2009 | 167/168 | 167/168 | P = 1.00 | 0% (‐1.6% to 1.6%) | 490/500 | 484/500 | P = 0.32 | +1.2% (‐0.8% to +3.2%) |
Appendix 7. Summary of results by RDT type and reference standard
| Microscopy | PCR | |||||||
| Type and RDT brand | Number of studies | Number of patients | Pooled sensitivity (95% CI) | Pooled specificity (95% CI) | Number of studies | Number of patients | Sensitivity (95% CI) | Specificity (95% CI) |
| Type 1, ParaSight‐F | 17 | 12,521 | 94.7 (92.0, 96.5) |
94.6 (91.6, 96.6) |
1 | 520 | 92 (86, 95) |
99 (98, 100) |
| Type 1, ParaHIT‐F | 4 | 1119 | 97.0 (92.2, 98.9) |
97.2 (92.2, 99.1) |
1 | 336 | 72 (51, 88) |
100 (99, 100) |
| Type 4, OptiMAL‐IT | 3 | 1356 | 87.4 (80.0, 92.4) |
96.9 (88.4, 99.3) |
1 | 313 | 73 (62, 81) |
99 (97, 100) |
| Type 3, SD Malaria Antigen Bioline | 2 | 224 | Dev 2004: 100 (80, 100) Ratsimbasoa 2007: 86 (76, 93) |
Dev 2004: 100 (75, 100) Ratsimbasoa 2007: 94 (89, 98) |
1 | 198 | 94 (88, 98) |
92 84, 96) |
| Type 6, PALUTOP | 0 | 0 | ‐ | ‐ | 1 | 313 | 95 (88, 98) |
97 (94, 99) |
Appendix 8. Comparison of local microscopy and RDTs verified with good quality microscopy
| Study | RDT | Local microscopy | RDT | ||
| Sensitivity | Specificity | Sensitivity | Specificity | ||
| Kolaczinski 2004 | OptiMAL | 85.2 | 99.7 | 79.3 | 99.7 |
| De Oliveira 2009 | Paracheck‐Pf | 52.5 | 77.0 | 91.7 | 96.7 |
Data
Presented below are all the data for all of the tests entered into the review.
Tests. Data tables by test.
1. Test.
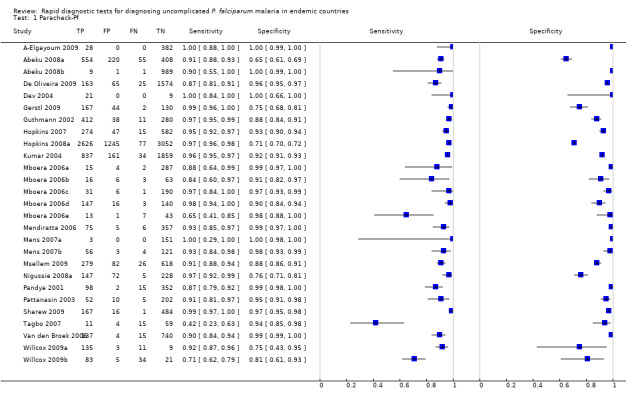
Paracheck‐Pf.
2. Test.
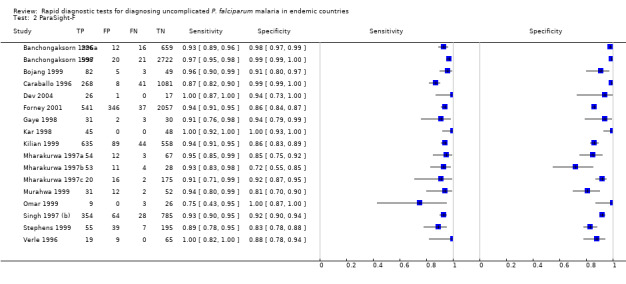
ParaSight‐F.
3. Test.
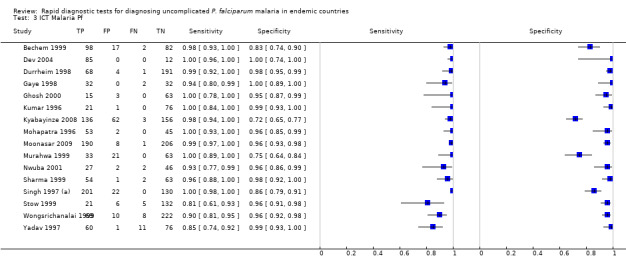
ICT Malaria Pf.
4. Test.
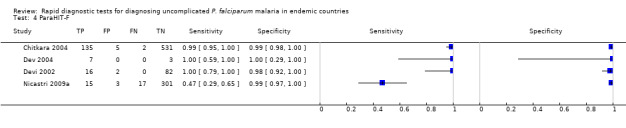
ParaHIT‐F.
5. Test.
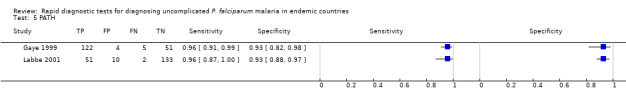
PATH.
6. Test.
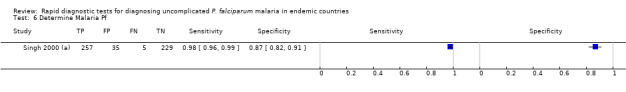
Determine Malaria Pf.
7. Test.

Rapid Test Malaria.
8. Test.
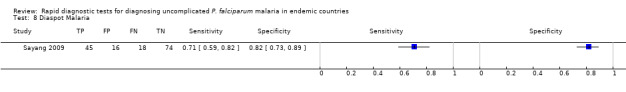
Diaspot Malaria.
9. Test.
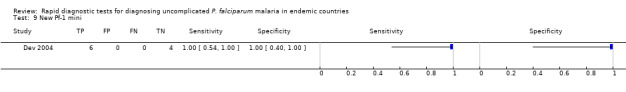
New Pf‐1 mini.
10. Test.
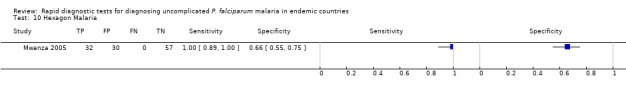
Hexagon Malaria.
11. Test.
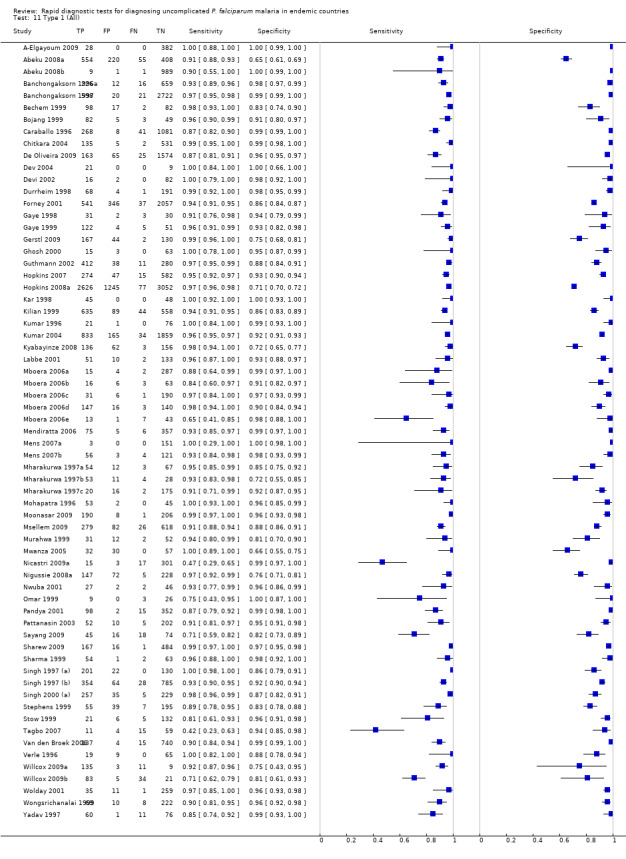
Type 1 (All).
12. Test.
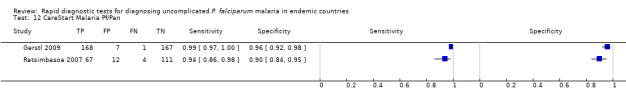
CareStart Malaria Pf/Pan.
13. Test.
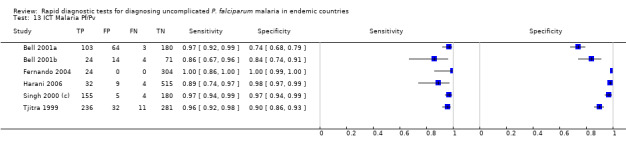
ICT Malaria Pf/Pv.
14. Test.
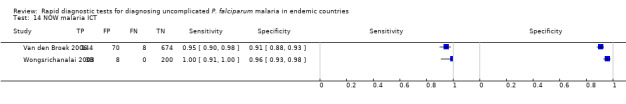
NOW malaria ICT.
15. Test.
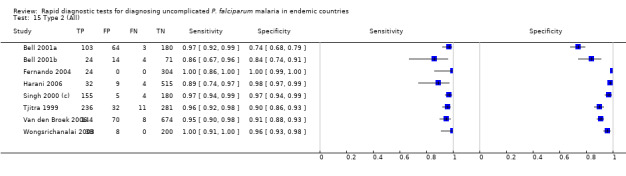
Type 2 (All).
16. Test.
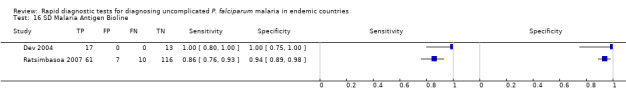
SD Malaria Antigen Bioline.
17. Test.
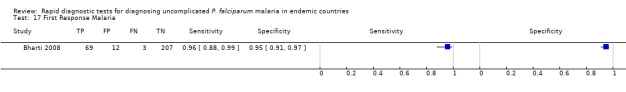
First Response Malaria.
18. Test.
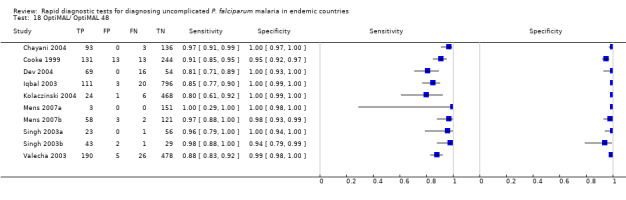
OptiMAL/ OptiMAL 48.
19. Test.

Parascreen.
20. Test.
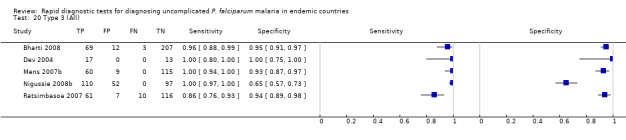
Type 3 (All).
21. Test.
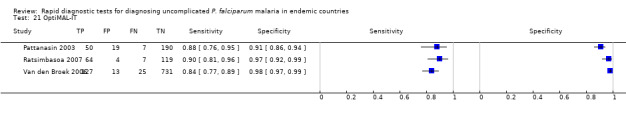
OptiMAL‐IT.
22. Test.
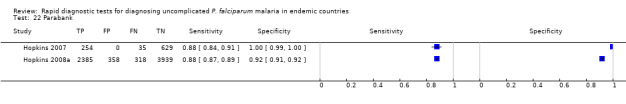
Parabank.
23. Test.
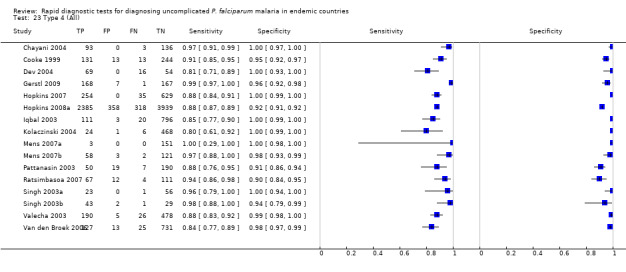
Type 4 (All).
24. Test.

Carestart Pf/Pv.
25. Test.
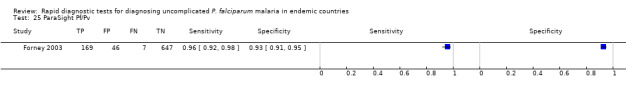
ParaSight Pf/Pv.
26. Test.
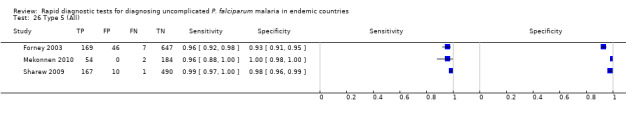
Type 5 (All).
27. Test.
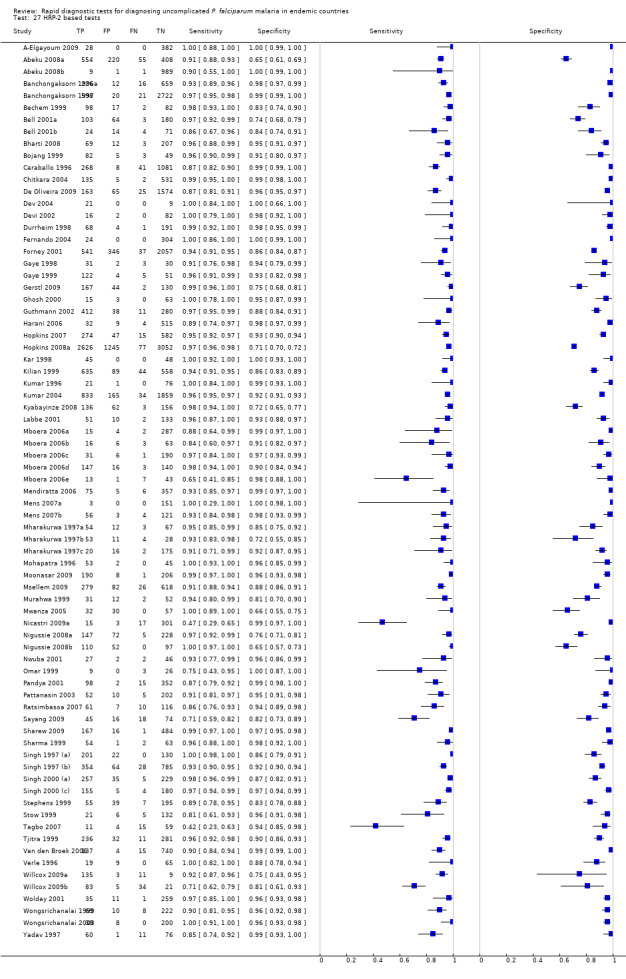
HRP‐2 based tests.
28. Test.
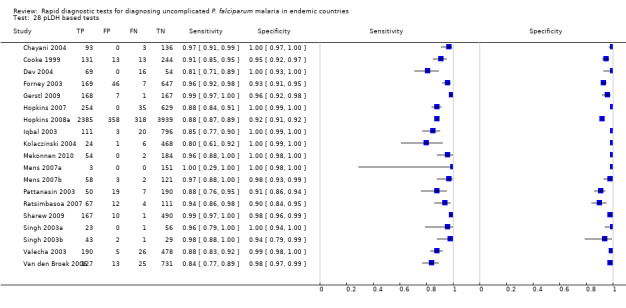
pLDH based tests.
29. Test.
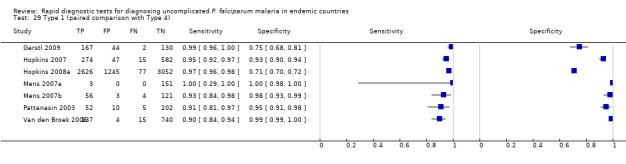
Type 1 (paired comparison with Type 4).
30. Test.
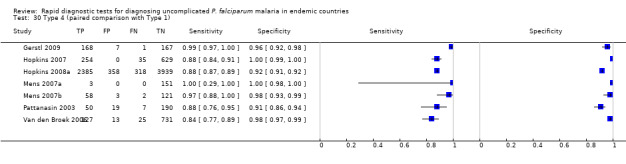
Type 4 (paired comparison with Type 1).
31. Test.
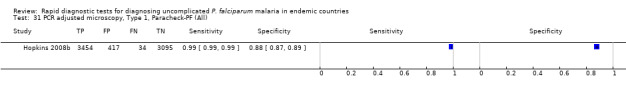
PCR adjusted microscopy, Type 1, Paracheck‐PF (All).
32. Test.
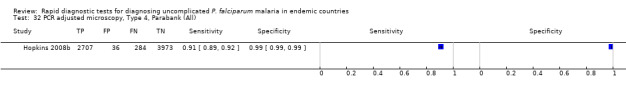
PCR adjusted microscopy, Type 4, Parabank (All).
33. Test.
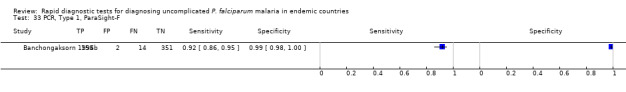
PCR, Type 1, ParaSight‐F.
34. Test.
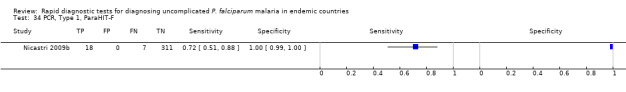
PCR, Type 1, ParaHIT‐F.
35. Test.
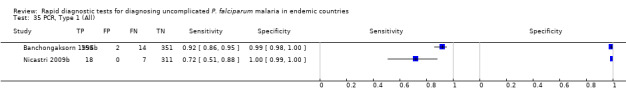
PCR, Type 1 (All).
36. Test.
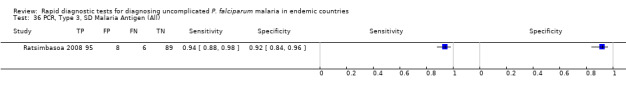
PCR, Type 3, SD Malaria Antigen (All).
37. Test.
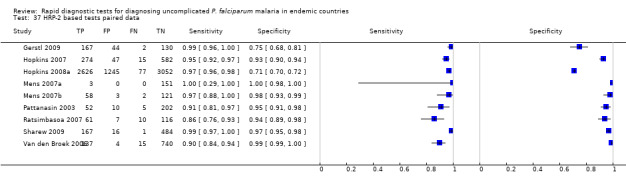
HRP‐2 based tests paired data.
38. Test.
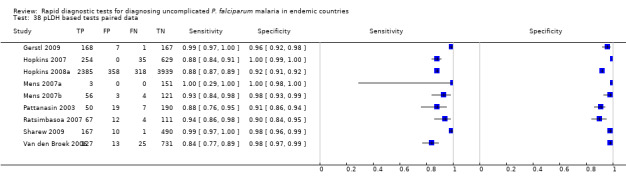
pLDH based tests paired data.
71. Test.
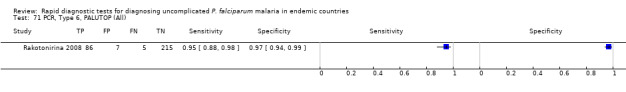
PCR, Type 6, PALUTOP (All).
72. Test.
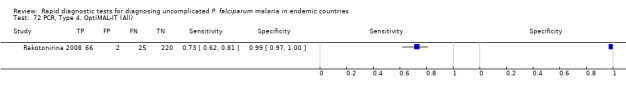
PCR, Type 4, OptiMAL‐IT (All).
Characteristics of studies
Characteristics of included studies [ordered by study ID]
A‐Elgayoum 2009.
| Clinical features and settings |
Presenting signs and symptoms: Clinically suspected malaria Previous treatment for malaria: No exclusions based on previous treatment. Information on previous treatment collected, but actual data not provided. Clinical setting: Primary healthcare facilities Country: Khartoum state, central Sudan Malaria endemicity: Seasonal and low Malaria endemic species:P. falciparum |
|
| Participants |
Sample size: 410 Age: All age groups eligible. Mean age 21 years. Sex: Both males and females eligible. Actual proportions of males and females in the participant population not stated. Co‐morbidities and pregnancy: No exclusion criteria based on co‐morbidities or pregnancy. No details of the frequency of these conditions in the participant population is presented. Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrolment was consecutive and prospective. One RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood films Person(s) performing microscopy: Expert malaria microscopist Microscopy setting: Quality Assurance Laboratory Number of high power fields examined before declaring negative: 300 Number of observer or repeats: Not stated Resolution of discrepancies between observers: Not stated |
|
| Index and comparator tests |
Commerical name of RDT: Paracheck Pf (Orchid Biomedical Systems, Goa, India) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Not stated Person(s) performing RDT: Technicians RDT setting: Primary healthcare facilities |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: PhD financial support from the Ministry of Higher Education and Scientific Research | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Participants were a consecutive sample of people presenting at healthcare facilities with clinically suspected malaria |
| Acceptable reference standard? All tests | Unclear | Unclear how many observer repeats were used, but the microscopy was described as the 'gold standard' |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | Reported that the tests were performed blindly |
| Index test results blinded? All tests | Yes | Reported that the tests were performed blindly |
| Uninterpretable results reported? All tests | Unclear | Number enrolled in the study was explicitly stated and corresponded to the number presented in the analysis; therefore no withdrawals due to invalid results |
| Withdrawals explained? All tests | Yes | Number enrolled in the study was explicitly stated and corresponded to the number presented in the analysis; therefore no withdrawals |
Abeku 2008a.
| Clinical features and settings |
Presenting signs and symptoms: Clinically diagnosed malaria based on fever or history of fever and absence of any other obvious cause of fever Previous treatment for malaria: No exclusions based on previous malaria treatment. Information on previous treatment collected, but data not presented. Clinical setting: Government health centres Country: Uganda Malaria endemicity: Incidence 359.8 per 1,000 per year Malaria endemic species:P. falciparum |
|
| Participants |
Sample size: 1237 Age: All age groups eligible. Actual age profile of participant population not presented, but it is clear that the sample contains both children and adults. Sex: Both males and females eligible. Actual proportions of males and females in the participant population not stated. Co‐morbidities and pregnancy: No exclusion criteria based on co‐morbidities or pregnancy. No details of the frequency of these conditions in the participant population is presented. Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was consecutive and prospective. One RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood films Person(s) performing microscopy: Experienced microscopists Microscopy setting: Not stated Number of high power fields examined before declaring negative: 200 Number of observer or repeats: Two independent microscopists Resolution of discrepancies between observers: By a third microscopist, who had the final say |
|
| Index and comparator tests |
Commerical name of RDT: Paracheck Pf (Orchid Biomedical Systems, Goa, India) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Stored at room temperature within the temperature range recommended by the manufacturer and used within 24 months Person(s) performing RDT: Laboratory staff who had been trained in their use RDT setting: Health centres |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Gates malaria Partnership and UK DFID | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Participants were a consecutive series of people attending health centres with clinically suspected malaria |
| Acceptable reference standard? All tests | Yes | Two independent experienced microscopists examined at least 200 high power fields before declaring samples negative. Discordant results were resolved by a third microscopist in a double‐blind manner. |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | Study report states that microscopists were blinded to the RDT results |
| Index test results blinded? All tests | Yes | All RDTs were undertaken and the results known before microscopy |
| Uninterpretable results reported? All tests | Unclear | The number of participants originally enrolled in the study was not clear; therefore unclear whether there were any withdrawals due to invalid results |
| Withdrawals explained? All tests | Unclear | The number of participants originally enrolled in the study was not clear; therefore unclear whether there were any withdrawals |
Abeku 2008b.
| Clinical features and settings |
Presenting signs and symptoms: Clinically diagnosed malaria based on fever or history of fever and absence of any other obvious cause of fever Previous treatment for malaria: No exclusions based on previous treatment. Information on previous treatment collected, but data not presented. Clinical setting: Government health centres Country: Kenya Malaria endemicity: Incidence 43.2 per 1,000 per year Malaria endemic species:P. falciparum |
|
| Participants |
Sample size: 1000 Age: All age groups eligible. Actual age profile of participant population not presented. Sex: Both males and females eligible. Actual proportions of males and females in the participant population not stated. Co‐morbidities and pregnancy: No exclusion criteria based on co‐morbidities or pregnancy. No details of the frequency of these conditions in the participant population is presented. Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrolment was consecutive and prospective. One RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood films Person(s) performing microscopy: Experienced microscopists Microscopy setting: Not stated Number of high power fields examined before declaring negative: 200 Number of observer or repeats: Two independent microscopists Resolution of discrepancies between observers: By a third microscopist, who had the final say |
|
| Index and comparator tests |
Commerical name of RDT: Paracheck Pf (Orchid Biomedical Systems, Goa, India) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Stored at room temperature within the temperature range recommended by the manufacturer and used within 24 months Person(s) performing RDT: Laboratory staff who had been trained in their use RDT setting: Health centres |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Gates malaria Partnership and UK DFID | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Participants were a consecutive series of people attending health centres with clinically suspected malaria |
| Acceptable reference standard? All tests | Yes | Two independent experienced microscopists examined at least 200 high power fields before declaring samples negative. Discordant results were resolved by a third microscopist in a double‐blind manner. |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | Study report states that microscopist were blinded to the RDT results |
| Index test results blinded? All tests | Yes | All RDTs were undertaken and the results known before microscopy |
| Uninterpretable results reported? All tests | Unclear | The number of participants originally enrolled in the study was not explicitly stated; therefore unclear whether there were any withdrawals due to invalid results |
| Withdrawals explained? All tests | Unclear | The number of participants originally enrolled in the study was not explicitly stated; therefore unclear whether there were any withdrawals |
Banchongaksorn 1996a.
| Clinical features and settings |
Presenting signs and symptoms: All patients attending malaria clinics Previous treatment for malaria: No exclusions based on previous treatment. Information on previous treatment collected, but actual data not provided. Clinical setting: Two malaria clinics Country: Thailand (Tak Province and Trat province, East Thailand) Malaria endemicity: Not stated Malaria endemic species:P. falciparum andP. vivax |
|
| Participants |
Sample size: 520 Age: All age groups eligible. Actual age profile of participant population not presented. Sex: Both males and females eligible. Actual proportions of males and females in the participant population not stated. Co‐morbidities and pregnancy: No exclusion criteria based on co‐morbidities or pregnancy. No details of the frequency of these conditions in the participant population is presented. Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was consecutive and prospective. One RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood films Person(s) performing microscopy: Microscopist and consultant Microscopy setting: Regional and national malaria centres Number of high power fields examined before declaring negative: 100 Number of observer or repeats: Two Resolution of discrepancies between observers: Not clear, 'the data were compared and confirmed' |
|
| Index and comparator tests |
Commerical name of RDT: ParaSight‐F (Beckton Dickinson, Franklin Lakes, NJ, US) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: The study team RDT setting: Malaria clinics |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: WHO Regional Office for South East Asia, new Delhi, India. Also Dr Joe Perrone of Becton Dickinson provided the ParaSight‐F kits | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Participants were attending malaria clinics and therefore suspected themselves that they had malaria. It was a consecutive sample. |
| Acceptable reference standard? All tests | Yes | Two independent microscopists based at a central laboratory examined at least 100 high power fields before declaring a slide negative |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | Report states that different tests were undertaken "independently" |
| Index test results blinded? All tests | Yes | Report states that different tests were undertaken "independently" |
| Uninterpretable results reported? All tests | Unclear | Number enrolled in the study was explicitly stated and corresponded to the number presented in the analysis; therefore no withdrawals due to invalid results |
| Withdrawals explained? All tests | Yes | Number enrolled in the study was explicitly stated and corresponded to the number presented in the analysis; therefore no withdrawals |
Banchongaksorn 1996b.
| Clinical features and settings |
Presenting signs and symptoms: All patients attending malaria clinics Previous treatment for malaria: No exclusions based on previous treatment. Information on previous treatment collected, but actual data not provided. Clinical setting: Two malaria clinics Country: Thailand (Tak Province and Trat province, East Thailand) Malaria endemicity: Not stated Malaria endemic species:P. falciparum andP. vivax |
|
| Participants |
Sample size: 520 Age: All age groups eligible. Actual age profile of participant population not presented. Sex: Both males and females eligible. Actual proportions of males and females in the participant population not stated Co‐morbidities and pregnancy: No exclusion criteria based on co‐morbidities or pregnancy. No details of the frequency of these conditions in the participant population is presented. Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was consecutive and prospective. One RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: PCR |
|
| Index and comparator tests |
Commerical name of RDT: ParaSight‐F (Beckton Dickinson, Franklin Lakes, NJ, US) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: The study team RDT setting: Malaria clinics |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: WHO Regional Office for South East Asia, new Delhi, India. Also Dr Joe Perrone of Becton Dickinson provided the ParaSight‐F kits | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | All participants were attending malaria clinics and therefore suspected themselves that they had malaria. Sampling was consecutive. |
| Acceptable reference standard? All tests | Yes | Reference standard was PCR |
| Partial verification avoided? All tests | No | 913 participants received the index test, 520 received the reference tests |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | Report states that different tests were undertaken "independently" |
| Index test results blinded? All tests | Yes | Report states that different tests were undertaken "independently" |
| Uninterpretable results reported? All tests | Unclear | The number of participants originally enrolled in the study was not explicitly stated; therefore unclear whether there were any withdrawals due to invalid results |
| Withdrawals explained? All tests | Unclear | The number of participants originally enrolled in the study was not explicitly stated; therefore unclear whether there were any withdrawals |
Banchongaksorn 1997.
| Clinical features and settings |
Presenting signs and symptoms: Fever over 37.5 °C by oral thermometer Previous treatment for malaria: Not mentioned, but no indication of any exclusion criteria based on previous antimalarial use Clinical setting: 34 health centres and 22 mobile health units Country: Thailand (Chiang Mai and Mae Hong Son provinces) Malaria endemicity: Not stated Malaria endemic species:P. falciparum and P. vivax |
|
| Participants |
Sample size: 3361 Age: All age groups eligible. Actual age profile of participant population not presented. Sex: Both males and females eligible. Actual proportions of males and females in the participant population not stated. Co‐morbidities and pregnancy: No exclusion criteria based on co‐morbidities or pregnancy. No details of the frequency of these conditions in the participant population is presented. Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was prospective. The sampling method was not described. One RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood films Person(s) performing microscopy: Expert microscopists Microscopy setting: Malaria Regional Centre, Chiang Mai Number of high power fields examined before declaring negative: Not stated Number of observer or repeats: Not stated Resolution of discrepancies between observers: Not applicable |
|
| Index and comparator tests |
Commerical name of RDT: ParaSight‐F (Beckton Dickinson, Franklin Lakes, NJ, US) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: Performed by health workers with 3 hours training, but results confirmed by experts at the Malaria Regional Centre RDT setting: Health centres and mobile health units |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Not stated | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | All participants were attending malaria clinics with fever, but the sampling method was not described |
| Acceptable reference standard? All tests | Unclear | Microscopy was undertaken by experts at a central laboratory, but there were no details provided about the processes used |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | Microscopy was undertaken at a different location than the RDTs |
| Index test results blinded? All tests | Yes | RDTs were undertaken at a different location than the microscopy |
| Uninterpretable results reported? All tests | Unclear | Number of participants enrolled in the study was explicitly stated and corresponded to the number presented in the analysis; therefore there were no withdrawals due to invalid results |
| Withdrawals explained? All tests | Yes | Number of participants enrolled in the study was explicitly stated and corresponded to the number presented in the analysis; therefore there were no withdrawals |
Bechem 1999.
| Clinical features and settings |
Presenting signs and symptoms: Fever of >38 °C Previous treatment for malaria: No exclusion criteria based on antimalarial use. Approximately 55% of the children had been given one or more antimalarial drugs between onset of symptoms and presentation at the hospital. Clinical setting: Paediatric Unit of Central Hospital Country: Cameroon (Yaounde) Malaria endemicity: Not stated Malaria endemic species: Not stated |
|
| Participants |
Sample size: 199 Age: Children 2.5 months to 16 years Sex: Both males and females eligible. Actual proportions of males and females in the participant population not stated. Co‐morbidities and pregnancy: No criteria based on co‐morbidities. No details of the frequency of these conditions in the participant population were presented. Parasite density of microscopy positive cases: Range 90 to 456,000 parasites per μl, geometric mean 7620 |
|
| Study design | Enrollment was consecutive and prospective. One RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy of thick and thin blood smears Person(s) performing microscopy: Microscopists Microscopy setting: Research laboratory Number of high power fields examined before declaring negative: 100 Number of observer or repeats: Two; however their method of working together was not described Resolution of discrepancies between observers: Not described |
|
| Index and comparator tests |
Commerical name of RDT: ICT Malaria Pf (ICTDiagnostics, Brookvale, NSW, Australia) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: Physician RDT setting: Paediatric unit |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Not stated | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Consecutive sample presenting to a paediatric unit with fever |
| Acceptable reference standard? All tests | Unclear | Although it states that there were 2 microscopists it does not mention how they were working |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | Reference tests were carried out in the laboratory, RDTs were carried out in the clinic |
| Index test results blinded? All tests | Yes | Reference tests were carried out in the laboratory, RDTs were carried out in the clinic |
| Uninterpretable results reported? All tests | Yes | One participant was excluded from the analysis because their blood slide was unreadable |
| Withdrawals explained? All tests | Yes | One participant was excluded from the analysis because their blood slide was unreadable |
Bell 2001a.
| Clinical features and settings |
Presenting signs and symptoms: History of fever, headache, chills or rigors occurring within the preceding three days; or more distant history of fever or non‐specific signs suggestive of malaria. Previous treatment for malaria: Participants who had recently taken antimalarials were not excluded; 5% of participants reported prior antimalarial use. Clinical setting: Village health workers in five barangaya (districts) Country: Philippines (Agusan del Sur Province in the northeast of the island of Maindano) Malaria endemicity: Generally low perennial transmission, with pockets of high transmission Malaria endemic species:P. falciparum andP. vivax |
|
| Participants |
Sample size: 350 Age: Eligible age range not stated. Mean age of the participants was 19.5 years. Sex: Both males and females eligible. There were 171 male and 179 female participants. Co‐morbidities and pregnancy: Not mentioned, either an exclusion criteria or characteristic of included participants Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was prospective. The sampling method was not described. One RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy of thick and thin blood smears Person(s) performing microscopy: An experienced local microscopist for all slides; selected slides were also read by an experienced parasitologist Microscopy setting: Local laboratory and hospital laboratory in Australia Number of high power fields examined before declaring negative: 100 Number of observer or repeats: One, except in discordant cases where RDT and microscopy results differed, all cases RDT‐positive for P. vivax and 20% of cases negative by slide and RDT, in which case a second reader was used Resolution of discrepancies between observers: The second, off‐site reading was taken as the correct one |
|
| Index and comparator tests |
Commerical name of RDT: ICT Malaria Pf/Pv (Amrad‐ICT, Sydney, Australia) Parasite(s) designed to detect:P. falciparum or mixed infection, non‐falciparum malaria species only Designated Type: Type 4 Batch numbers: Not stated Transport and storage conditions: Refrigerated until two weeks before use Person(s) performing RDT: Researchers RDT setting: Study villages |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: The Australian National Health and Medical Research Council | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | All participants had approached village health workers with symptoms suggestive of malaria, but the sampling method was not described |
| Acceptable reference standard? All tests | Yes | An experienced microscopist viewed at least 100 high powered fields and discordant results were re‐examined |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | "Slides were read by a local microscopist who was not aware of the results of the ICT tests" |
| Index test results blinded? All tests | Yes | RDTs were performed two to four weeks before microscopy |
| Uninterpretable results reported? All tests | Yes | The paper reported that there was one uninterpretable microscopy result |
| Withdrawals explained? All tests | Unclear | The number of participants originally enrolled in the study was not stated; therefore it is unclear whether there were any withdrawals |
Bell 2001b.
| Clinical features and settings |
Presenting signs and symptoms: History of fever, headache, child or rigors occurring within the preceding 3 days; or more distant history of fever or non‐specific signs suggestive of malaria Previous treatment for malaria: Patients treated with antimalarials during the four weeks preceding the test were excluded from the analysis Clinical setting: Health centre in Visaya Country: Philippines (Agusan del Sur Province in the northeast of the island of Maindano) Malaria endemicity: Generally low perennial transmission, with pockets of high transmission Malaria endemic species:P. falciparum andP. vivax |
|
| Participants |
Sample size: 113 Age: Eligible age range not stated. Mean age of the participants was 19.8 years. Sex: Both males and females eligible. There were 73 male and 40 female participants. Co‐morbidities and pregnancy: Not mentioned, either as an exclusion criteria or characteristic of included participants Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was prospective. The sampling method was not described. One RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy of thick and thin blood smears Person(s) performing microscopy: Not stated Microscopy setting: Regional Health Units Number of high power fields examined before declaring negative: Not stated, but probably 100 as in the other trial reported together in the same paper Number of observer or repeats: Not stated Resolution of discrepancies between observers: Not applicable |
|
| Index and comparator tests |
Commerical name of RDT: ICT Malaria Pf/Pv (Amrad‐ICT, Sydney, Australia) Parasite(s) designed to detect:P. falciparum or mixed infection, non‐falciparum malaria species only Designated Type: Type 4 Batch numbers: Not stated Transport and storage conditions: Stored by barangya health workers at room temperature, averaging about 25 °C for up to six months Person(s) performing RDT: Barangay health workers RDT setting: Health centre |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: The Australian National Health and Medical Research Council | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | All participants were attending a health centre with history of fever, headache, child or rigours within the preceding 3 days; more distant history of fever or non‐specific signs suggestive of malaria; but the sampling method was not described |
| Acceptable reference standard? All tests | Unclear | No details given of the microscopy process |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | Clear that blinding had taken place, as it was not possible to match up all the RDT and microscopy results by name and date |
| Index test results blinded? All tests | Yes | Clear that blinding had taken place, as it was not possible to match up all the RDT and microscopy results by name and date |
| Uninterpretable results reported? All tests | Yes | 25 of 393 tests done were considered invalid because of an indistinct control band. Invalid results were excluded from the analysis. |
| Withdrawals explained? All tests | Yes | Only 113 microscopy results could be matched with RDT results by name and date; the others were lost from the analysis |
Bharti 2008.
| Clinical features and settings |
Presenting signs and symptoms: Fever or history of fever, and suspicion of malaria Previous treatment for malaria: No exclusions based on previous treatment; it was undertaken in a remote area with no medical facilities Clinical setting: Mobile field clinics in 10 villages Country: India (Remote forested region of Jabalpur during the peak monsoon season) Malaria endemicity: Low endemic areas with higher transmission during the monsoon Malaria endemic species:P. falciparum andP. vivax |
|
| Participants |
Sample size: 291 Age: All age groups eligible. Actual age range of participants 1 to 60 years. Sex: Both males and females eligible. Male: female ratio 1:1.15. Co‐morbidities and pregnancy: No criteria based on co‐morbidities or pregnancy. No details of the frequency of these conditions in the participant population presented. Parasite density of microscopy positive cases: Range 80 to 111,920 parasites per cul, mean 8011, Standard Deviation 21,595 |
|
| Study design | Enrollment was consecutive and prospective. One RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick blood films Person(s) performing microscopy: Experienced microscopist Microscopy setting: Laboratory of NIMR Number of high power fields examined before declaring negative: 100 Number of observer or repeats: One for all samples, two independent readers for samples discordant between microscopy and RDT Resolution of discrepancies between observers: Where the second reading gave a different result from the first, the results of the second reading were confirmed by a third examination by another technician |
|
| Index and comparator tests |
Commerical name of RDT: First Response Combo Malaria Ag card test (Premier Medical Corporation Ltd, Mumbai, India) Parasite(s) designed to detect:P. falciparum or mixed infection, non‐falciparum malaria species only Designated Type: Type 3 Batch numbers: 61F0107 Transport and storage conditions: RDTs were stored properly, at temperature of 4 °C to 30 °C, and used within their shelf life Person(s) performing RDT: Field laboratory assistants. Independent staff re‐read the saved tests after two months and matched them with the originally recorded results RDT setting: Field laboratory |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Indian Council of Medical Research, Delhi. Test kits provided by Premier Medical Corporation Ltd. | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Participants were a consecutive sample of people attending mobile field clinics with fever or history of fever, and suspicion of malaria |
| Acceptable reference standard? All tests | Yes | An experienced microscopist viewed at least 100 high power fields before declaring a slide negative, and results discordant with RDT were independently re‐examined by a second microscopist, and a third if necessary |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | Microscopy was undertaken "without reference to the RDT" |
| Index test results blinded? All tests | Yes | RDTs were undertaken on site, and the results recorded before the microscopy results became available |
| Uninterpretable results reported? All tests | Yes | The paper reported that there were no invalid results |
| Withdrawals explained? All tests | Yes | The number of participants enrolled in the study was clearly stated, and corresponded to the number presented in the analysis; therefore there were no withdrawals |
Bojang 1999.
| Clinical features and settings |
Presenting signs and symptoms: Temperature of 37.5 °C or higher, or a recent history of fever Previous treatment for malaria: No exclusions based on previous treatment and no information presented on previous treatment, except for those with false positive results on RDT Clinical setting: Malaria outpatient clinic Country: The Gambia (Basse, Upper River Division) Malaria endemicity: Not stated Malaria endemic species:P. falciparum |
|
| Participants |
Sample size: 139 Age: Inclusion criteria stipulated all were children; actual age range not stated Sex: Not mentioned either as an inclusion criteria or a characteristic of included participants Co‐morbidities and pregnancy: Not mentioned either as an inclusion criteria or a characteristic of included participants Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrolment was prospective. The sampling method was not described. One RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick blood smear Person(s) performing microscopy: Not stated Microscopy setting: Not stated Number of high power fields examined before declaring negative: Not stated Number of observer or repeats: Not stated Resolution of discrepancies between observers: Not applicable |
|
| Index and comparator tests |
Commerical name of RDT: ParaSight‐F (Beckton Dickinson, Franklin Lakes, NJ, US) Parasite(s) designed to detect:P. falciparum Designated Type: Type I Batch numbers: Not stated Transport and storage conditions: Not stated Person(s) performing RDT: Field staff who had attended three training session RDT setting: Malaria clinic |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Medical Research Council Laboratories, The Gambia | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | All participants were attending a malaria clinic with fever or history of fever, but the sampling method was not described |
| Acceptable reference standard? All tests | Unclear | Not details given of the microscopy process |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Unclear | Blinding not described |
| Index test results blinded? All tests | Yes | "Test performed without reference to the results of the corresponding thick blood smear" |
| Uninterpretable results reported? All tests | Unclear | The number of participants enrolled was explicitly stated and corresponded to the number presented in the analysis; therefore there were no participants excluded due to invalid results |
| Withdrawals explained? All tests | Yes | The number of participants enrolled was explicitly stated and corresponded to the number presented in the analysis; therefore there were no withdrawals |
Caraballo 1996.
| Clinical features and settings |
Presenting signs and symptoms: Fever and suspicion of malaria Previous treatment for malaria: No exclusions based on previous treatment and no information presented on previous treatment, except for those with false positive results on RDT Clinical setting: Malaria diagnostic post Country: Venezuela ‐ Bolivar state. Gold‐mining area. Malaria endemicity: Annual parasite index 352/1000 Malaria endemic species:P. falciparum |
|
| Participants |
Sample size: 1398 Age: All ages eligible; actual age range 3 months to 84 years Sex: Both males and females eligible: actual sample 81.2% male, 18.8% female Co‐morbidities and pregnancy: Not mentioned, either as an inclusion criteria or characteristic of included participants Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was prospective. The sampling method was not described. One RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick blood smear Person(s) performing microscopy: Trained malaria microscopists Microscopy setting: Central Headquarters of the Venezuelan Malaria Programme Number of high power fields examined before declaring negative: 100 Number of observer or repeats: Two Resolution of discrepancies between observers: Not stated |
|
| Index and comparator tests |
Commerical name of RDT: ParaSight‐F (Beckton Dickinson, Franklin Lakes, NJ, US) Parasite(s) designed to detect:P. falciparum Designated Type: Type I Batch numbers: Not stated Transport and storage conditions: Not stated Person(s) performing RDT: Rural visitor from the Malaria Programme RDT setting: Malaria diagnostic post |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: UNDP/World Bank/WHO‐TDR (Project number 930439), Beckton Dickinson Advanced Diagostics provided the supplies to carry out this work | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | All participants were attending diagnostics facilities with fever and suspicion of malaria, but the sampling method was not described. |
| Acceptable reference standard? All tests | Unclear | Two trained microscopists at a central laboratory viewed 100 high power fields before declaring negative; however it is not clear whether the microscopists worked independently of each other |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | Blinding described in detail |
| Index test results blinded? All tests | Yes | Index test undertaken and results recorded before reference test |
| Uninterpretable results reported? All tests | Unclear | The number of participants originally enrolled in the study was unclear; therefore it is not possible to judge whether any were excluded from the analysis due to invalid test results |
| Withdrawals explained? All tests | Unclear | The number of participants originally enrolled in the study was unclear; therefore it is not possible to judge whether there were any withdrawals |
Chayani 2004.
| Clinical features and settings |
Presenting signs and symptoms: Specific symptoms: rigor, chills, rise of high temperature and profuse sweating; or irregular fever, joint pain and jaundice Previous treatment for malaria: No explicit exclusions based on previous treatment and no information presented on previous treatment. Clinical setting: Diagnostic and research centre (takes referrals from physicians for the diagnosis of malaria) Country: Orissa, India Malaria endemicity: Not stated Malaria endemic species: In sample, 78.6% P. falciparum, 21.4% P. vivax |
|
| Participants |
Sample size: 232 Age: Not mentioned, either as inclusion criteria or characteristic of participants Sex: Not mentioned, either as inclusion criteria or characteristic of participants Co‐morbidities and pregnancy: Not mentioned, either as inclusion criteria or characteristic of participants Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was prospective. The sampling method was unclear. One RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood smear Person(s) performing microscopy: Microscopists Microscopy setting: Diagnostic and research centre Number of high power fields examined before declaring negative: 200 Number of observer or repeats: Two independent observers Resolution of discrepancies between observers: A third microscopist's opinion was taken into account |
|
| Index and comparator tests |
Commerical name of RDT: OptiMAL (DiaMed AG, Cressier, Switzerland) Parasite(s) designed to detect:P. falciparum or mixed infection, non‐falciparum malaria species only Designated Type: Type 4 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: Not stated RDT setting: Not stated |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Not stated | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | All participants were attending an ambulatory clinic with rigor, chills, rise of high temperature and profuse sweating; or irregular fever, joint pain and jaundice. However the sampling method was not described. |
| Acceptable reference standard? All tests | Yes | Two independent microscopists viewed 200 high powered fields before declaring a slide negative |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Unclear | Blinding not described |
| Index test results blinded? All tests | Unclear | Blinding not described |
| Uninterpretable results reported? All tests | Unclear | The number of participants originally enrolled in the study was not explicitly stated; therefore it is not possible to judge whether any were excluded from the analysis due to invalid test results |
| Withdrawals explained? All tests | Unclear | The number of participants originally enrolled in the study was not explicitly stated; therefore it is not possible to judge whether there were any withdrawals |
Chitkara 2004.
| Clinical features and settings |
Presenting signs and symptoms: Fever Previous treatment for malaria: No exclusions based on previous treatment and no information presented on previous treatment, although this data was collected as part of the study Clinical setting: Temporary fever treatment camp Country: India (Assam and Arunachal Pradesh) Malaria endemicity: Varied Malaria endemic species: mainly P. falciparum, someP. vivax |
|
| Participants |
Sample size: 673 Age: All age groups eligible; actual age range not reported Sex: Both males and females eligible; actual proportions in the sample not reported Co‐morbidities and pregnancy: No exclusions based on co‐morbidities or pregnancy; actual frequency of these conditions in the same not reported Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was consecutive and prospective. One RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood smear Person(s) performing microscopy: Chief microscopist of the District Malaria Office and two pathologists of Assam Medical College Microscopy setting: District Malaria Office and Assam Medical College Number of high power fields examined before declaring negative: Not stated Number of observer or repeats: All positive slides and 20% of negative slides were independently read by the pathologists from Assam Medical College Resolution of discrepancies between observers: Not described |
|
| Index and comparator tests |
Commerical name of RDT: ParaHIT‐F (Span diagnostics Ltd, Surat, India) Parasite(s) designed to detect:P .falciparum Designated Type: Type I Batch numbers: Not stated Transport and storage conditions: Not stated Person(s) performing RDT: Laboratory technicians RDT setting: Temporary fever treatment camp |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Span Diagnostics provided the RDT test kits free of charge | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Participants were a consecutive sample attending a temporary treatment camp with fever |
| Acceptable reference standard? All tests | Unclear | Unclear, as the numbers of high power fields viewed before declaring negative was not stated. However, the microscopy was undertaken by expert microscopists in a central malaria laboratory. |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | Two different technicians did the microscopic examination and the ParaHIT‐f test and the results of their observations were compared later. |
| Index test results blinded? All tests | Yes | Two different technicians did the microscopic examination and the ParaHIT‐f test and the results of their observations were compared later. |
| Uninterpretable results reported? All tests | Unclear | The number of participants originally enrolled in the study was not explicitly stated; therefore it is not possible to judge whether any were excluded from the analysis due to invalid test results |
| Withdrawals explained? All tests | Unclear | The number of participants originally enrolled in the study was not explicitly stated; therefore it is not possible to judge whether there were any withdrawals |
Cooke 1999.
| Clinical features and settings |
Presenting signs and symptoms: Fever or history of fever and a suspected diagnosis of malaria Previous treatment for malaria: No exclusions based on previous treatment and no information presented on previous treatment Clinical setting: Outpatient clinic Country: The Gambia (Fajara) Malaria endemicity: Not stated: study undertaken during period of seasonal high transmission Malaria endemic species: mainly P. falciparum |
|
| Participants |
Sample size: 409 Age: Over the age of one year Sex: No exclusions based on sex; actual proportions of males and females in the sample not stated Co‐morbidities and pregnancy: No exclusions based on co‐morbidities or pregnancy; actual proportions with these conditions in the sample not stated Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was consecutive and prospective. One RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick blood smear. Thin blood smear in the case of discordant results between RDT and blood smear. Person(s) performing microscopy: Experienced microscopist at the clinic laboratory. In the case of discordant results between the RDT and microscopy, a second expert technician at the main laboratory re‐examined the slides. Microscopy setting: Clinic laboratory and central laboratory. Number of high power fields examined before declaring negative: 100 at the clinic, 500 at the main laboratory Number of observer or repeats: One, except in the case of discordant results, where a second observer was used Resolution of discrepancies between observers: Where index and reference test results were discordant the blood film at the main laboratory was read and this result used |
|
| Index and comparator tests |
Commerical name of RDT: OptiMAL (DiaMed AG, Cressier, Switzerland) Parasite(s) designed to detect:P. falciparum or mixed infection, non‐falciparum malaria species only Designated Type: Type 4 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: A member of the study team RDT setting: Outpatient clinic |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: The OptiMAL assays were provided by FLOW Inc. | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Participants were a consecutive sample of people attending an outpatient clinic with fever or a history of fever suspected to be malaria |
| Acceptable reference standard? All tests | Yes | All slides were examined by an experienced microscopist viewing 100 high power fields before declaring negative. Where RDT and microscopy gave discordant results, slides were re‐examined by another microscopist viewing at least 500 high power fields |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | The study number and laboratory number were only matched after the blood film examination and OptiMAL test had been completed |
| Index test results blinded? All tests | Yes | The study number and laboratory number were only matched after the blood film examination and OptiMAL test had been completed |
| Uninterpretable results reported? All tests | Yes | Of 409 participants recruited, one was excluded from the analysis because the test strip failed to give a results |
| Withdrawals explained? All tests | Yes | Of 409 participants, seven were excluded because the results were not recorded in the clinic book, and one because the index test failed to give a results |
De Oliveira 2009.
| Clinical features and settings |
Presenting signs and symptoms: Suspected malaria Previous treatment for malaria: No exclusions based on previous treatment and no information presented on previous treatment Clinical setting: Various health facilities including 7 hospitals, 23 health centres and 30 dispensaries Country: Kenya (Karicho, Bondo and Siaya Districts) Malaria endemicity: 30 health facilities in seasonal areas, 30 in perennial areas Malaria endemic species:P. falciparum |
|
| Participants |
Sample size: 1827 Age: Five years or over Sex: Both males and females eligible. Actual proportions of males and females in the participant population not stated. Co‐morbidities and pregnancy: No exclusions criteria based on co‐morbidities or pregnancy. No details of the frequency of these conditions in the participant population is presented. Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was consecutive and prospective. One RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood smears Person(s) performing microscopy: Expert microscopists, who receive regular training at the Malaria Diagnostics and Control Centre of Excellence of the US Army Medical Research Unit in Kenya and consistently attain acceptable competency scores during such training sessions Microscopy setting: Malaria laboratories of the Kenya Medical Research Institute (KEMRI) and US Centres for Disease Control and Prevention (CDC) in Kisumu Number of high power fields examined before declaring negative: 100 Number of observer or repeats: Two independent observers Resolution of discrepancies between observers: A third microscopist, blinded to all previous blood tests, reviewed the smear |
|
| Index and comparator tests |
Commerical name of RDT: Paracheck Pf (Orchid Biomedical Systems, Goa, India) Parasite(s) designed to detect:P. falciparum Designated Type: Type I Batch numbers: 31422 Transport and storage conditions: Kept at health facilities during the study. Study staff recommended that they be stored in a cool and dry place and provided thermometers to monitor daily storage temperatures. Person(s) performing RDT: Laboratory technicians who were trained to perform the tests according to the manufacturer's instructions RDT setting: Health facilities |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: US Centres for Disease Control and Prevention | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Participants were a consecutive series of people attending health facilities with suspected malaria |
| Acceptable reference standard? All tests | Yes | Two independent expert microscopists each viewed 100 high power fields before declaring a slide negative |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | Microscopists reported to be blinded to the results of the RDTs |
| Index test results blinded? All tests | Yes | RDTs undertaken and results recorded at the health facilities before microscopy |
| Uninterpretable results reported? All tests | Unclear | There were no withdrawals, and no reports of uninterpretable results |
| Withdrawals explained? All tests | Yes | Participants were excluded from the analysis if they refused to give blood samples or complete clinical information |
Dev 2004.
| Clinical features and settings |
Presenting signs and symptoms: Fever Previous treatment for malaria: No information presented on previous treatment; no suggestion of any exclusions based on previous treatment Clinical setting: Malaria clinics Country: India (Assam) Malaria endemicity: Mesendemic Malaria endemic species:P. falciparum and P. vivax |
|
| Participants |
Sample size: 336; but varied by RDT evaluated (10 to 139) Age: Infants under 12 months excluded; actual age range 1 to 60 years Sex: Both males and females eligible. Actual proportions of males and females in the participant population not stated. Co‐morbidities and pregnancy: No exclusion criteria based on co‐morbidities or pregnancy were stated, and no details of the frequency of these conditions in the participant population is presented Parasite density of microscopy positive cases: Range 300 to 350,000 parasites per μl, mean 59,842, Standard Deviation 78,780 |
|
| Study design | Enrollment was prospective. The sampling method was not described. Seven RDTs were evaluated; it is unclear how each RDT was allocated, as no participant received all the tests. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood smears Person(s) performing microscopy: Technician; all positive slides and 20% of negative slides were also examined by the senior technician for confirmation of result. Microscopy setting: Laboratory at the malaria clinics Number of high power fields examined before declaring negative: 100 Number of observer or repeats: One in the case of most smears judged negative by the technician. Two in the case of 20% of those initially judged negative, and all those judged positive. Resolution of discrepancies between observers: The judgement of the senior technician was used |
|
| Index and comparator tests |
Commerical name of RDT: Paracheck Pf (Orchid Biomedical Systems, Goa, India) ParaSight‐F (Beckton Dickinson, Franklin Lakes, NJ, US) ParaHIT‐F (Span diagnostics Ltd, Surat, India) ICT Malaria Pf (ICT Diagnostics, Sydney, Australia) New Pf‐1 mini (Monozyme India Ltd, Secundrabad, India) SD Malaria Pf/Pv (SD Diagnostics Inc, Korea) Diamed OptiMAL (Flow Inc., Portland, OR, US) Parasite(s) designed to detect: Paracheck Pf ‐ P. falciparum ParaSight‐F ‐ P. falciparum ParaHIT‐F ‐ P. falciparum ICT Malaria Pf ‐ P. falciparum New Pf‐1 mini ‐ P. falciparum SD Malaria Pf/Pv ‐ P. falciparum or mixed infection, non‐falciparum malaria species only Diamed OptiMAL ‐ P. falciparum or mixed infection, non‐falciparum malaria species only Designated Type: Paracheck Pf ‐ Type I ParaSight‐F ‐ Type I ParaHIT‐F ‐ Type I ICT Malaria Pf ‐ Type I New Pf‐1 mini ‐ Type I SD Malaria Pf/Pv ‐ Type 3 Diamed OptiMAL ‐ Type 4 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: The laboratory attendant performed the test and recorded his or her interpretation. The test kit result was then re‐read for verification by the senior technician. RDT setting: Malaria clinic laboratory |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Main source of funding not stated. Test kits supplied by the Government of Assam. | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | All participants were attending malaria clinics with fever. However, during the study period, 6663 blood smears were examined, but only 336 were evaluated with RDT kits, and the sampling method for RDT evaluation was unclear. |
| Acceptable reference standard? All tests | Unclear | Two observers were used in the vast majority of cases; however, it is unclear whether the observers worked independently |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | Microscopy and RDT results were compared by an independent observer |
| Index test results blinded? All tests | Yes | Microscopy and RDT results were compared by an independent observer |
| Uninterpretable results reported? All tests | Unclear | No information presented on numbers initially allocated each RDT, so not possible to judge this |
| Withdrawals explained? All tests | Unclear | No information presented on numbers initially allocated each RDT, so not possible to judge this |
Devi 2002.
| Clinical features and settings |
Presenting signs and symptoms: Fever and referred for malaria diagnosis by physicians Previous treatment for malaria: No exclusions based on previous treatment and no information presented on previous treatment Clinical setting: Exact setting unclear, but based at M.S. Ramaiah Medical Teaching Hospital, Bangalore Country: India, Bangalore Malaria endemicity: Not stated Malaria endemic species: mainly P. falciparum some P. vivax |
|
| Participants |
Sample size: 100 Age: All age groups eligible. Actual age structure of the study sample not described. Sex: Both males and females eligible. Actual proportions of males and females in the participant population not stated. Co‐morbidities and pregnancy: No exclusions criteria based on co‐morbidities or pregnancy. No details of the frequency of these conditions in the participant population is presented. Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was random and prospective. One RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood smears Person(s) performing microscopy: Not stated Microscopy setting: Large teaching hospital, in a malaria endemic area Number of high power fields examined before declaring negative: Not stated Number of observer or repeats: Not stated Resolution of discrepancies between observers: Not applicable |
|
| Index and comparator tests |
Commerical name of RDT: ParaHIT‐f (Span Diagnostics, India) Parasite(s) designed to detect:P. falciparum Designated Type: Type I Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: Not stated RDT setting: Large teaching hospital, in a malaria endemic area |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Not stated | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | All participants had a fever and were referred to the study site for diagnosis of malaria; however it is unclear how participants were selected for referral |
| Acceptable reference standard? All tests | Unclear | No details given of the microscopy process |
| Partial verification avoided? All tests | Yes | All participants received both the index and the reference tests |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Unclear | Blinding not described |
| Index test results blinded? All tests | Unclear | Blinding not described |
| Uninterpretable results reported? All tests | Unclear | The number of participants originally enrolled in the study was not explicitly stated; therefore it is not possible to judge whether any were excluded from the analysis due to invalid test results |
| Withdrawals explained? All tests | Unclear | The number of participants originally enrolled in the study was not explicitly stated; therefore it is not possible to judge whether there were any withdrawals |
Durrheim 1998.
| Clinical features and settings |
Presenting signs and symptoms: Clinical signs and symptoms compatible with malaria Previous treatment for malaria: No exclusions based on previous treatment and no information presented on previous treatment Clinical setting: Outpatient clinic Country: South Africa (Lowveld region) Malaria endemicity: Seasonal Malaria endemic species:P. falciparum |
|
| Participants |
Sample size: 264 Age: All age groups eligible. Actual age structure of the study sample not described. Sex: Both males and females eligible. Actual proportions of males and females in the participant population not stated. Co‐morbidities and pregnancy: No exclusion criteria based on co‐morbidities or pregnancy. No details of the frequency of these conditions in the participant population is presented. Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was consecutive and prospective. One RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick blood film Person(s) performing microscopy: Experienced laboratory technologist Microscopy setting: Reference malaria laboratory Number of high power fields examined before declaring negative: Not stated Number of observer or repeats: One Resolution of discrepancies between observers: Not applicable |
|
| Index and comparator tests |
Commerical name of RDT: ICT Malaria Pf (ICT Diagnostics, Sydney, Australia) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: Clinic nurse checked by skilled reader RDT setting: Outpatient clinic |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Not stated | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Participants were a consecutive series of patients attending clinics with clinical signs and symptoms of malaria |
| Acceptable reference standard? All tests | No | Only one observer was used |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | Microscopy was reported to be done with no prior knowledge of the results of the RDT |
| Index test results blinded? All tests | Yes | The RDT was reported to be performed before the microscopy results were available |
| Uninterpretable results reported? All tests | Unclear | The number of participants enrolled in the study is explicitly stated and corresponds to the number presented in the analysis; therefore there were no exclusions from the analysis due to invalid test results |
| Withdrawals explained? All tests | Yes | The number of participants enrolled in the study is explicitly stated and corresponds to the number presented in the analysis; therefore there were no withdrawals |
Fernando 2004.
| Clinical features and settings |
Presenting signs and symptoms: Fever or history of fever Previous treatment for malaria: No exclusions because of prior antimalarial use, and no data presented on the frequency of recent antimalarial use in the participants Clinical setting: A malaria research station and a malaria clinic Country: Sri Lanka Malaria endemicity: Not stated Malaria endemic species:P. vivax (70%) and P. falciparum |
|
| Participants |
Sample size: 328 Age: All ages above five years eligible; mean age 28.3 years (range 5 to 72 years) Sex: Both males and females eligible; 64% of the participants were males Co‐morbidities and pregnancy: No exclusion criteria based on co‐morbidities or pregnancy. No details of the frequency of these conditions in the participant population is presented. Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was consecutive and prospective. One RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and think blood films Person(s) performing microscopy: Trained microscopists Microscopy setting: At the clinics and in a laboratory Number of high power fields examined before declaring negative: 400 Number of observer or repeats: Two independent readers; one at the clinics and another in a laboratory Resolution of discrepancies between observers: There were no discrepancies between the two microscopists |
|
| Index and comparator tests |
Commerical name of RDT: ICT Malaria Pf/Pv (Amrad‐ICT, Sydney, Australia) Parasite(s) designed to detect:P. falciparum or mixed infection, non‐falciparum malaria species only Designated Type: Type 2 Batch numbers: Not stated Transport and storage conditions: Stored and used at room temperature, which often exceeds 30 °C Person(s) performing RDT: The researchers RDT setting: At the clinics |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: National Science Foundation, Sri Lanka | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Participants were a consecutive sample of people attending clinics with fever or history of fever |
| Acceptable reference standard? All tests | Yes | Twp independent trained microscopists viewed 400 high power fields before declaring a slide negative |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Unclear | Blinding not described |
| Index test results blinded? All tests | Unclear | Blinding not described |
| Uninterpretable results reported? All tests | Unclear | The number of participants enrolled was clearly stated, and the number included in the analysis corresponds to this number, indicating no withdrawals |
| Withdrawals explained? All tests | Yes | The number of participants enrolled was clearly stated, and the number included in the analysis corresponds to this number, indicating no withdrawals |
Forney 2001.
| Clinical features and settings |
Presenting signs and symptoms: Fever over 38 °C or headache or history of fever in the previous 72 hrs Previous treatment for malaria: Patients who were currently taking antimalarial therapy or who had been treated with antimalarial drugs within the previous two weeks were excluded Clinical setting: Outpatient malaria clinics Country: Iquitos, Peru (28% of participants); Mae Sod, Thailand (72% of participants) Malaria endemicity: Seasonal Malaria endemic species:P. falciparum and P.vivax |
|
| Participants |
Sample size: 3006 enrolled, 2993 had blood collected, 2988 included (2162 Thailand, 838 Peru) Age: 15 years or over (Thailand, 72% of participants); one year or over (Peru, 28% of participants) Sex: Both males and females eligible. Actual proportions of males and females in the participant population not stated. Co‐morbidities and pregnancy: No exclusion criteria based on co‐morbidities or pregnancy. No details of the frequency of these conditions in the participant population is presented. Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was consecutive and prospective. One RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood film Person(s) performing microscopy: Trained, certified microscopist Microscopy setting: Malaria testing station Number of high power fields examined before declaring negative: 200 Number of observer or repeats: Two independent observers Resolution of discrepancies between observers: A third senior microscopist examined both microscopist A's and microscopist B's slides, and gave the final judgement |
|
| Index and comparator tests |
Commerical name of RDT: ParaSight‐F (Beckton Dickinson, Franklin Lakes, NJ, US) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: Trained investigator and technician, with quality control checks by the principal investigator RDT setting: Malaria testing station |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Main funding source not stated. RDT kits provided by the manufacturer. | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Participants were a consecutive series of people attending malaria clinics with fever over 38 °C or headache or history of fever in the previous 72 hrs |
| Acceptable reference standard? All tests | Yes | Two independent trained microscopists viewed at least 200 high powered fields before declaring negative |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | In all cases, the results of the ParaSight‐F test were determined prior to diagnostic microscopy, with strict blinding between the rapid test results and technicians performing the microscopy |
| Index test results blinded? All tests | Yes | In all cases, the results of the ParaSight‐F test were determined prior to diagnostic microscopy, with strict blinding between the rapid test results and technicians performing the microscopy |
| Uninterpretable results reported? All tests | Yes | Tests whose results were reported as uninterpretable after the initial procedure were repeated in an attempt to resolve the discrepant event. Repeatedly uninterpretable results were reported as such and were incorporated into calculation of sensitivity and specificity as 'false' results. There were a total of seven uninterpretable results; all were negative for P. falciparum by blood slide. |
| Withdrawals explained? All tests | Yes | There were five withdrawals after collection of blood samples; reasons were documented in all cases. |
Forney 2003.
| Clinical features and settings |
Presenting signs and symptoms: Fever over 38 °C or history of fever over the previous 72 h, or headaches Previous treatment for malaria: Patients who had taken antimalarials recently were included. No data is presented on the actual number who reported recent antimalarial use. Clinical setting: Outpatient malaria clinics Country: Thailand (Mae Sod) and Peru (Iquitos) Malaria endemicity: Not stated; study conducted in endemic areas during peak transmission seasons Malaria endemic species:P. falciparum andP. vivax |
|
| Participants |
Sample size: 477 in Thailand, 393 in Peru Age: Eligibility criteria for age not stated; in practice, although younger patients were eligible, all participants were over the age of 18 Sex: Not mentioned, either as inclusion criteria or characteristics of participants Co‐morbidities and pregnancy: Not mentioned, either as inclusion criteria or characteristics of participants Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was prospective. The sampling method was not described. Three prototype RDTs were evaluated; only the most recent is presented. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood smear Person(s) performing microscopy: Skilled, certified technicians Microscopy setting: Malaria testing station Number of high power fields examined before declaring negative: 200 Number of observer or repeats: Two independent observers; three for discordant slides and 5% of concordant slides Resolution of discrepancies between observers: A third senior microscopist examined both microscopist A's and microscopist B's slides, and gave the final judgement |
|
| Index and comparator tests |
Commerical name of RDT: ParaSight Pf/Pv Final Prototype FV99‐2 (Becton Dickinson, Franklin Lakes, NJ, USA) Parasite(s) designed to detect:P. falciparum and P. vivax Designated Type: Unknown Batch numbers: Not applicable (prototype) Transport and storage conditions: Not described Person(s) performing RDT: Not stated RDT setting: Not stated |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Not stated | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | All participants were all attending clinics with fever or headaches, but the sampling method was not described |
| Acceptable reference standard? All tests | Yes | Two independent, trained microscopists viewed at least 200 high power fields before declaring a slide negative |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | "In all cases the results of the ParaSight Pf/Pv tests were determined prior to the completion of diagnostic microscopy" |
| Index test results blinded? All tests | Yes | "The technicians examining the stained smears were strictly blinded to the rapid test results" |
| Uninterpretable results reported? All tests | Yes | Uninterpretable test results were excluded from the analysis (1 participant) |
| Withdrawals explained? All tests | Yes | The number of participants enrolled in the study was clearly stated, and corresponded to the number included in the analysis, with the exception of one participant not included because of uninterpretable test results |
Gaye 1998.
| Clinical features and settings |
Presenting signs and symptoms: Malaria symptoms Previous treatment for malaria: No exclusion criteria relating to prior antimalarial drug use. Data collected but only presented in the case of false positives. Clinical setting: Outpatient clinic Country: Senegal (Dakar) Malaria endemicity: Hypoendemic and seasonal Malaria endemic species: PredominantlyP. falciparum |
|
| Participants |
Sample size: 66 Age: All ages eligible. Actual age range 1 to 65 years Sex: Both males and females eligible. Actual proportions of males and females in the participant population 35 female, 31 male. Co‐morbidities and pregnancy: Not mentioned Parasite density of microscopy positive cases: Range 500 to 86,286 parasites per μl |
|
| Study design | Enrollment was prospective. The sampling method was not described. Three RDTs were evaluated and all participants received all three tests. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick blood film Person(s) performing microscopy: Not stated Microscopy setting: Not stated Number of high power fields examined before declaring negative: Not stated Number of observer or repeats: Not stated Resolution of discrepancies between observers: Not applicable |
|
| Index and comparator tests |
Commerical name of RDT: ICT Malaria Pf (ICT Diagnostics, Sydney, Australia) ParaSight‐F (Beckton Dickinson, Franklin Lakes, NJ, US) Malaria IgG CELISA (CelLabs Sydney, Australia) (excluded as not eligible for inclusion in this review) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: Not stated RDT setting: Not stated |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Not stated | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | All participants were presenting to an outpatient clinic with malaria symptoms, but the sampling method was not described |
| Acceptable reference standard? All tests | Unclear | No details given of the microscopy process |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Unclear | Blinding not described |
| Index test results blinded? All tests | Unclear | Blinding not described |
| Uninterpretable results reported? All tests | Unclear | The numbers of participants originally enrolled in the study was clearly stated, and corresponds to the number presented in the analysis; therefore there were no exclusions due to invalid test results |
| Withdrawals explained? All tests | Yes | The numbers of participants originally enrolled in the study was clearly stated, and corresponds to the number presented in the analysis; therefore there were no withdrawals |
Gaye 1999.
| Clinical features and settings |
Presenting signs and symptoms: Malaria symptoms Previous treatment for malaria: Not mentioned, either as an exclusion criteria or characteristic of included participants Clinical setting: Outpatient clinic Country: Senegal (North Senegal, Richard‐Toll) Malaria endemicity: Not stated Malaria endemic species: Not stated |
|
| Participants |
Sample size: 182 Age: All ages eligible. Actual age range 1 to 55 years Sex: Not mentioned, either as an inclusion criteria or characteristic of included participants Co‐morbidities and pregnancy: Not mentioned, either as an inclusion criteria or characteristic of included participants Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was prospective. The sampling method was not described. One test was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick blood film Person(s) performing microscopy: Not stated Microscopy setting: Not stated Number of high power fields examined before declaring negative: Not stated Number of observer or repeats: Not stated Resolution of discrepancies between observers: Not applicable |
|
| Index and comparator tests |
Commerical name of RDT: PATH Falciparum Malaria Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: Not stated RDT setting: Not stated |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Not stated | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | All participants were presenting to an outpatient clinic with malaria symptoms, but the sampling method was not described |
| Acceptable reference standard? All tests | Unclear | Not details given of the microscopy process |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Unclear | Blinding not described |
| Index test results blinded? All tests | Unclear | Blinding not described |
| Uninterpretable results reported? All tests | Unclear | The numbers of participants originally enrolled in the study was clearly stated, and corresponds to the number presented in the analysis; therefore there were no exclusions due to invalid test results |
| Withdrawals explained? All tests | Yes | The numbers of participants originally enrolled in the study was clearly stated, and corresponds to the number presented in the analysis; therefore there were no withdrawals |
Gerstl 2009.
| Clinical features and settings |
Presenting signs and symptoms: Fever (axillary temperature >37.5 °C) or history of fever in the previous 72 h and no signs of severe disease Previous treatment for malaria: Not mentioned, either as an inclusion criteria or characteristic of included participants Clinical setting: MSF community health centre Country: Sierra Leone (Bo District, Eastern Sierra Leone) Malaria endemicity: Hyperendemic Malaria endemic species:P. falciparum |
|
| Participants |
Sample size: 345 Age: Inclusion criteria 2 to 59 months Sex: Both males and females eligible Co‐morbidities: No exclusions based on co‐morbidities; no information presented about the frequency of co‐morbid conditions in the study sample Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was consecutive and prospective. One test was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy Person(s) performing microscopy: Not stated Microscopy setting: Not stated Number of high power fields examined before declaring negative: Not stated Number of observer or repeats: Not stated Resolution of discrepancies between observers: Not applicable |
|
| Index and comparator tests |
Commerical name of RDT: ParaCheck‐Pf (Orchid Biomedical Systems, Goa, India) Carestart Pf/Pan Parasite(s) designed to detect: ParaCheck‐Pf ‐ P. falciparum Carestart Pf/Pan ‐ P. falciparum or mixed infection, non‐falciparum malaria species only Designated Type: ParaCheck‐Pf ‐ Type 1 Carestart 3 line ‐ Type 4 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: Not stated RDT setting: Not stated |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Not stated | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Participants were a consecutive sample of children presenting to a community health centre with fever |
| Acceptable reference standard? All tests | Unclear | No information was provided about the microscopy process |
| Partial verification avoided? All tests | Unclear | Not enough information presented to assess this |
| Differential verification avoided? All tests | Unclear | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Unclear | Blinding not described |
| Index test results blinded? All tests | Unclear | Blinding not described |
| Uninterpretable results reported? All tests | Unclear | Not enough information presented to enable assessment of this |
| Withdrawals explained? All tests | Unclear | Not enough information presented to enable assessment of this |
Ghosh 2000.
| Clinical features and settings |
Presenting signs and symptoms: Febrile illness Previous treatment for malaria: Not mentioned, either as an inclusion criteria or characteristic of included participants Clinical setting: Unclear (PHC Banavara district Hassan, Karnataka) Country: India (Karnataka) Malaria endemicity: Not stated Malaria endemic species: Not stated |
|
| Participants |
Sample size: 100 Age: Malaria cases were aged 5 years to 80 years Sex: Both males and females were included Co‐morbidities and pregnancy: Not mentioned, either as an inclusion criteria or characteristic of included participants Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was prospective. The sampling method was not described. One test was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin smears Person(s) performing microscopy: One set was immediately examined in the field while the second one was stained in the laboratory and examined carefully Microscopy setting: Field and laboratory (unclear which is the reference standard) Number of high power fields examined before declaring negative: About 200 Number of observer or repeats: Unclear Resolution of discrepancies between observers: Unclear/Not applicable |
|
| Index and comparator tests |
Commerical name of RDT: ICT Malaria (ICT Diagnostics, Australia) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: Not stated RDT setting: Not stated |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Not stated | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | All participants were attending health facilities with febrile illnesses; however the exact setting was unclear, and the sampling method was not described |
| Acceptable reference standard? All tests | Unclear | Microscopy was undertaken under field conditions and also examined carefully in a laboratory and it was unclear which was the reference standard |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Unclear | Blinding not described |
| Index test results blinded? All tests | Unclear | Blinding not described |
| Uninterpretable results reported? All tests | Unclear | The number of participants originally enrolled in the study is not clearly stated, therefore it is unclear whether any may have been excluded from the analysis, and the reasons for this |
| Withdrawals explained? All tests | Unclear | The number of participants originally enrolled in the study is not clearly stated, therefore it is unclear whether any may have been withdrawn or excluded from the analysis, and the reasons for this |
Guthmann 2002.
| Clinical features and settings |
Presenting signs and symptoms: Clinical suspicion of malaria, diagnosed by the clinical officer Previous treatment for malaria: No exclusion criteria based on antimalarial use and no data collected on this Clinical setting: Outpatient department of a reference hospital Country: Mbarara, Uganda Malaria endemicity: Not stated Malaria endemic species:P. falciparum |
|
| Participants |
Sample size: 742 Age: All age groups eligible; 315 were aged less than 5 years Sex: Both males and females eligible. Actual proportions of males and females in the participant population not stated Co‐morbidities and pregnancy: No exclusions were made, and there was no information presented on pregnancy or co‐morbidities Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was consecutive and prospective. Five RDTs were tested, and most participants received all the tests. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood films Person(s) performing microscopy: Trained malaria technician Microscopy setting: Not stated Number of high power fields examined before declaring negative: 200 Number of observer or repeats: One, except in the case of discordant results between microscopy and RDTs Resolution of discrepancies between observers: All discordant results, all slides where only gametocytes were detected and a random sample of 20% of the remaining slides were checked blind by an independent trained laboratory technician |
|
| Index and comparator tests |
Commerical name of RDTs: Paracheck Pf dipstick (Orchid Biomedical Systems, Goa, India) Paracheck Pf device (Orchid Biomedical Systems, Goa, India) (data not included in review as duplicates Paracheck Pf dipstick) ParaHIT‐f (Span diagnostics Ltd, Surat, India) (excluded as required data could not be extracted) BIO P.F (excluded as required data could not be extracted) Malaria Rapid (excluded as required data could not be extracted) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: Two independent readers (persons unspecified) RDT setting: The research clinic |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Medicins sans Frontieres, French section. Laboratories provided the tests kits free of charge. | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Participants were a consecutive series of people suspected to have malaria and attending an outpatient clinic |
| Acceptable reference standard? All tests | No | Microscopy was undertaken by trained microscopists viewing 200 high powered fields before declaring negative, but their findings were not confirmed by a second independent observer |
| Partial verification avoided? All tests | Yes | All participants who received the index tests also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | Report states that the results were blind |
| Index test results blinded? All tests | Yes | Readers were kept blinded to the results of the microscopy examination |
| Uninterpretable results reported? All tests | Yes | A small number of test results (one each for Paracheck dipstick and cassette, four for paraHIT, three for BIO PF and 21 for Malaria Rapid) were invalid, and these are presented as participants missing from the analysis |
| Withdrawals explained? All tests | Yes | Of the 742 participants who received microscopy, 741 received Paracheck Pf, 738 received ParaHIT Pf, 739 received BIO PF and 721 received Malaria Rapid. All withdrawals after tests were given represent invalid RDTresults |
Harani 2006.
| Clinical features and settings |
Presenting signs and symptoms: Clinical symptoms of malaria and history of fever over 37.5 °C. People with known causes of fever other than malaria were excluded. Previous treatment for malaria: Patients who had been treated for malaria in the previous 4 weeks were excluded from the study Clinical setting: Outpatient department of a reference hospital Country: Pakistan Malaria endemicity: Not stated Malaria endemic species:P. falciparum and P. vivax |
|
| Participants |
Sample size: 560 Age: All age groups eligible; actual age range of included participants 2 to 73 years Sex: Both males and females eligible. Participants included 339 males and 221 females. Co‐morbidities and pregnancy: Not mentioned, either as an inclusion criteria or characteristic of included participants Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was prospective. The sampling method was not described. One RDT was tested. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood films Person(s) performing microscopy: Senior technologist and principle author Microscopy setting: Department of Pathology and Microbiology, Aga Khan University Number of high power fields examined before declaring negative: 200 Number of observer or repeats: Unclear, two microscopists were used but how they divided the work between them was not described Resolution of discrepancies between observers: Not applicable |
|
| Index and comparator tests |
Commerical name of RDT: ICT Malaria Pf/Pv (Binax Inc., Portland, Maine, US) Parasite(s) designed to detect:P. falciparum or mixed infection, non‐falciparum malaria species only Designated Type: Type 2 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: The second author RDT setting: Microbiology section of Aga Khan University |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Not stated | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | All participants were presenting at an outpatients department with symptoms of malaria and history of fever, but the sampling method was not described |
| Acceptable reference standard? All tests | Unclear | Two microscopists at a University laboratory viewed 200 high power fields before declaring a slide negative; however, it is unclear how the two microscopists worked together |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | "The microscopists were unaware of the microscopy results" |
| Index test results blinded? All tests | Yes | "These results were read by the second author who was blind to the microscopy results" |
| Uninterpretable results reported? All tests | Unclear | The number of participants originally enrolled in the study was clearly stated, and corresponds with the number presented in the analysis; therefore there were no exclusions due to invalid results |
| Withdrawals explained? All tests | Yes | The number of participants originally enrolled in the study was clearly stated, and corresponds with the number presented in the analysis; therefore there were no withdrawals due to invalid results |
Hopkins 2007.
| Clinical features and settings |
Presenting signs and symptoms: Fever Previous treatment for malaria: No exclusion criteria based on antimalarial use and no data collected on this Clinical setting: Clinic specially set up as part of a longitudinal study, based within a main public hospital Country: Uganda (Kampala) Malaria endemicity: Not stated Malaria endemic species:P. falciparum |
|
| Participants |
Sample size: 918 Age: Children aged 1.5 to 11.5 years Sex: Both males and females eligible. Actual proportions of males and females in the participant population not stated. Co‐morbidities: No exclusions were made, and there was no information presented on co‐morbidities Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was consecutive and prospective. Two RDTs were tested, and all participants received both tests. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood films Person(s) performing microscopy: Experienced laboratory technologists Microscopy setting: Hospital laboratory Number of high power fields examined before declaring negative: 100 Number of observer or repeats: Two; all smears were read a second time by study laboratory staff to confirm results Resolution of discrepancies between observers: Discrepant readings were resolved by a third reader |
|
| Index and comparator tests |
Commerical name of RDTs: Paracheck Pf (Orchid Biomedical Systems, Goa, India) Parabank (Zephyr Biomedicals, Goa, India) Parasite(s) designed to detect: Paracheck Pf (Orchid Biomedical Systems, Goa, India) ‐ P. falciparum Parabank (Zephyr Biomedicals, Goa, India) ‐ P. falciparum or mixed infection, non‐falciparum malaria species only Designated Type: Paracheck: Type 1 Parabank: Type 4 Batch numbers: Not stated Transport and storage conditions: Obtained directly from the manufacturer and stored in their original packaging at room temperature in the clinic. The temperature ranged from 19 °C to 29 °C over the course of the study. Person(s) performing RDT: Laboratory technicians. RDT setting: The research clinic |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: US National Institute of Health, with additional support from the Doris Duke Charitable Foundation | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Participants were a consecutive series of children attending a clinic with fever in a malaria endemic area |
| Acceptable reference standard? All tests | Yes | Two independent experienced microscopists viewed 100 high powered fields before declaring negative |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | Microscopy was undertaken at a different location to the RDTs |
| Index test results blinded? All tests | Yes | Readers were unaware of the microscopy results at the time they undertook the study |
| Uninterpretable results reported? All tests | Unclear | The number of participants who received the tests was explicitly stated and corresponded to the number included in the analysis; therefore there were no exclusions due to invalid results |
| Withdrawals explained? All tests | Yes | RDTs were not performed in 15 episodes: nine at the discretion of the physician during follow‐up for non‐febrile illness, and six because of protocol errors |
Hopkins 2008a.
| Clinical features and settings |
Presenting signs and symptoms: Outpatients who had been referred to the laboratory for malaria blood smears in accordance with the usual standard of are. Previous treatment for malaria: No exclusion criteria based on antimalarial use and no data collected on this Clinical setting: Health centres Country: Uganda Malaria endemicity: 7 different sites of varying endemicity. Results not presented separately. Malaria endemic species:P. falciparum |
|
| Participants |
Sample size: 7000 Age: All ages included. 3161 participants were under the age of 5 years. No separate analysis available by age. Sex: Both males and females eligibles. Actual proportions of males and females in the participant population not stated. Co‐morbidities and pregnancy: No exclusions were made, and there was no information presented on co‐morbidities or pregnancy Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was consecutive and prospective. Two RDTs were tested, and all participants received both tests. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood films Person(s) performing microscopy: Health centre laboratory staff and expert microscopists at a central laboratory Microscopy setting: Health centre staff and central hospital laboratory Number of high power fields examined before declaring negative: 100 Number of observer or repeats: Two; all smears were read by both the health centre laboratory staff and expert microscopists at the central laboratory Resolution of discrepancies between observers: Discrepant readings between the health centre and expert central laboratory microscopists were resolved by a second expert microscopist |
|
| Index and comparator tests |
Commerical name of RDTs: Paracheck Pf (Orchid Biomedical Systems, Goa, India) Parabank (Zephyr Biomedicals, Goa, India) Parasite(s) designed to detect: Paracheck Pf ‐ P. falciparum Parabank ‐ P. falciparum or mixed infection, non‐falciparum malaria species only Designated Type: Paracheck: Type 1 Parabank: Type 4 Batch numbers: Not stated Transport and storage conditions: Obtained directly from the manufacturer and stored in their original packaging at room temperature in the clinic. The temperature ranged from 19 °C to 31 °C over the course of the study, and relative humidity from 39% to 87%. Person(s) performing RDT: Study staff RDT setting: Health centres |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: US National Institute of Health, with additional support from the Doris Duke Charitable Foundation | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | All participants were referred for microscopy for suspected malaria under usual care protocols |
| Acceptable reference standard? All tests | Yes | Two microscopists, including one expert microscopist at a central laboratory, read each smear. They examined 100 high powered fields before declaring negative. |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Unclear | Blinding not described |
| Index test results blinded? All tests | Unclear | Blinding not described |
| Uninterpretable results reported? All tests | Unclear | The number of participants originally enrolled in the study was clearly stated, and corresponds with the number presented in the analysis; therefore there were no exclusions due to invalid results |
| Withdrawals explained? All tests | Yes | The number of participants originally enrolled in the study was clearly stated, and corresponds with the number presented in the analysis; therefore there were no withdrawals due to invalid results |
Hopkins 2008b.
| Clinical features and settings |
Presenting signs and symptoms: Outpatients who had been referred to the laboratory for malaria blood smears in accordance with the usual standard of care Previous treatment for malaria: No exclusion criteria based on antimalarial use and no data collected on this Clinical setting: Health centres Country: Uganda Malaria endemicity: 7 different sites of varying endemicity. Results not presented separately. Malaria endemic species:P. falciparum |
|
| Participants |
Sample size: 7000 Age: All ages included. 3161 participants were under the age of 5 years. Sex: Both males and females eligible. Actual proportions of males and females in the participant population not stated. Co‐morbidities and pregnancy: No exclusions were made, and there was no information presented on co‐morbidities or pregnancy Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was consecutive and prospective. Two RDTs were tested, and all participants received both tests. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy corrected by PCR (discordant results between microscopy and RDTs were re‐analysed using PCR) Person(s) performing microscopy: Health centre laboratory staff and expert microscopists at a central laboratory Microscopy setting: Health centre staff and central hospital laboratory Number of high power fields examined before declaring negative: 100 Number of observer or repeats: Two. All smears were read by both the health centre laboratory staff and expert microscopists at the central laboratory Resolution of discrepancies between observers: Discrepant readings between the health centre and expert central laboratory microscopists were resolved by a second expert microscopist |
|
| Index and comparator tests |
Commerical name of RDTs: Paracheck Pf (Orchid Biomedical Systems, Goa, India) Parabank (Zephyr Biomedicals, Goa, India) Parasite(s) designed to detect: Paracheck Pf ‐ P. falciparum Parabank ‐ P. falciparum or mixed infection, non‐falciparum malaria species only Designated Type: Paracheck: Type 1 Parabank: Type 4 Batch numbers: Not stated Transport and storage conditions: Obtained directly from the manufacturer and stored in their original packaging at room temperature in the clinic. The temperature ranged from 19 °C to 31 °C over the course of the study, and relative humidity from 39% to 87%. Person(s) performing RDT: Study staff RDT setting: Health centres |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: US National Institute of Health, with additional support from the Doris Duke Charitable Foundation | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | All participants were referred for microscopy for suspected malaria under usual care protocols |
| Acceptable reference standard? All tests | Yes | Two microscopists, including one expert microscopist at a central laboratory, read each smear. They examined 100 high powered fields before declaring negative. Discordant results between expert microscopy and RDTs were then re‐examined using PCR, and the PCR results taken as the 'gold standard'. |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | No | Discordant results between expert microscopy and RDTs were re‐examined using PCR, and the PCR results taken as the 'gold standard' |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Unclear | Blinding not described |
| Index test results blinded? All tests | Unclear | Blinding not described |
| Uninterpretable results reported? All tests | Unclear | The number of participants originally enrolled in the study was clearly stated, and corresponds with the number presented in the analysis; therefore there were no exclusions due to invalid results |
| Withdrawals explained? All tests | Yes | The number of participants originally enrolled in the study was clearly stated, and corresponds with the number presented in the analysis; therefore there were no withdrawals due to invalid results |
Iqbal 2003.
| Clinical features and settings |
Presenting signs and symptoms: History of fever for 2 to 3 days and possible malaria infection Previous treatment for malaria: Patients with a history of antimalarial use in the previous 4 weeks were excluded Clinical setting: Basic health units Country: Pakistan (central areas of Punjab) Malaria endemicity: Seasonal Malaria endemic species:P. falciparum andP. vivax |
|
| Participants |
Sample size: 930 Age: Range 2 to 55 years (not clear whether this was an inclusion criteria or characteristic of included participants) Sex: Not mentioned, either as an inclusion criteria or a characteristic of the participants Co‐morbidities and pregnancy: Not mentioned, either as an inclusion criteria or a characteristic of the participants Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was prospective. The sampling method was not described. One RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick blood films Person(s) performing microscopy: Experienced microscopist Microscopy setting: District Health Centre Number of high power fields examined before declaring negative: 200 Number of observer or repeats: One; however for quality assessment, 100 random slides were sent to the Microbiology Unit, University of Kuwait, for a second reading; these results were comparable to the District Health Centre results Resolution of discrepancies between observers: Not applicable |
|
| Index and comparator tests |
Commerical name of RDT: OptiMAL (Flow Inc., Portland, Oregon, USA) Parasite(s) designed to detect:P. falciparum or mixed infection, non‐falciparum malaria species only Designated Type: Type 4 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: Laboratory staff RDT setting: District Health Centre |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Kuwait University | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | All participants were attending basic health units with symptoms of malaria and history of fever, but the sampling method was not described |
| Acceptable reference standard? All tests | No | An microscopist working at a district laboratory viewed at least 200 high power fields before declaring a slide negative; however their findings were not verified by an independent observer |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | "tests were performed in a double‐blind manner" |
| Index test results blinded? All tests | Yes | "tests were performed in a double‐blind manner" |
| Uninterpretable results reported? All tests | Unclear | The numbers of participants originally enrolled in the study was not clearly stated, therefore it is unclear whether there were any exclusions due to invalid test results |
| Withdrawals explained? All tests | Unclear | The numbers of participants originally enrolled in the study was not clearly stated, therefore it is unclear whether there were any withdrawals |
Kar 1998.
| Clinical features and settings |
Presenting signs and symptoms: People attending a malaria clinic Previous treatment for malaria: No exclusion criteria based on prior antimalarial drug use; this information was recorded for each participants, but no data is presented Clinical setting: Malaria Clinic at a Malaria Research Centre Country: India (Chennai, Tamil Nadu) Malaria endemicity: Perennial Malaria endemic species:P. falciparum and P. vivax |
|
| Participants |
Sample size: 93 Age: Not mentioned either as an inclusion criteria or characteristic of participants Sex: Not mentioned either as an inclusion criteria or characteristic of participants Co‐morbidities and pregnancy: No information presented on co‐morbidities or pregnancy Parasite density of microscopy positive cases: Less than 100 parasites per μl in 3 cases; between 100 and 1000 in 8 cases, over 1000 in 34 cases |
|
| Study design | Enrolment was prospective. The sampling method was not described. One RDT was tested. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick blood films Person(s) performing microscopy: Not stated Microscopy setting: Malaria clinic at malaria research centre Number of high power fields examined before declaring negative: Not stated Number of observer or repeats: Not stated Resolution of discrepancies between observers: Not applicable |
|
| Index and comparator tests |
Commerical name of RDTs: ParaSight‐F (Beckton Dickinson, Franklin Lakes, NJ, USA) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: Not stated RDT setting: Malaria clinic at malaria research centre |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Not stated | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | All participants were attending a malaria clinic, but their symptoms were not described and the sampling method was not described |
| Acceptable reference standard? All tests | Unclear | Study report did not state who performed the microscopy, how many observers or repeats were used, or how many high power fields were viewed before declaring a slide negative |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Unclear | Blinding not described |
| Index test results blinded? All tests | Unclear | Blinding not described |
| Uninterpretable results reported? All tests | Unclear | The numbers of participants originally enrolled in the study was not clearly stated, therefore it is unclear whether there were any exclusions due to invalid test results |
| Withdrawals explained? All tests | Unclear | The numbers of participants originally enrolled in the study was not clearly stated, therefore it is unclear whether there were any withdrawals |
Kilian 1999.
| Clinical features and settings |
Presenting signs and symptoms: Suspected uncomplicated malaria Previous treatment for malaria: There were no explicit exclusion criteria based on previous use of antimalarials, and no data on previous antimalarial use of the participants was presented Clinical setting: District malaria control programme health facilities and hospital outpatient clinic Country: Uganda (Kaborole District) Malaria endemicity: Various locations with varying endemicities Malaria endemic species: Mainly P. falciparum |
|
| Participants |
Sample size: 1326 Age: Included 336 infants and 710 adults; plus 180 with ages not stated Sex: Included 124 pregnant women; number of other female participants was not stated Co‐morbidities and pregnancy: Included 124 pregnant women and 586 people with previous malaria treatment failure Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrolment was prospective. Sampling was purposive to include mainly people of high risk groups. One RDT was tested. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick blood films Person(s) performing microscopy: Not stated Microscopy setting: Central malaria laboratory Number of high power fields examined before declaring negative: 100 Number of observer or repeats: At the hospital, all slides were read independently by two microscopists; at two health centres a second reading was only performed where RDT and microscopy results disagreed Resolution of discrepancies between observers: In the case of the second slide reading differing from the first, a third independent reading was carried out by a senior microscopist and this was considered true |
|
| Index and comparator tests |
Commerical name of RDT: ParaSight‐F (Becton Dickinson Tropical Disease Diagnostics, Sparks, MD, USA) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: At the hospital, tests were carried out and read by an experienced laboratory assistant. At the health centres, the tests were carried out by health workers after training, and within one week were re‐read by an experienced laboratory assistant blind to the evaluation of the health care staff. RDT setting: Two health units and a hospital. |
|
| Follow‐up | Not applicable | |
| Notes |
Source of funding: The ParaSight‐F tests were provided by both Becton‐Dickinson and the Malaria Unit, Ministry of Health, Uganda. The study was financially supported by the Federal Ministry of Economic Cooperation and Development, Germany, through Project PN 94.2195.9. Additional Information: This study was part of a larger study which included a group of people who had been treated for malaria but where treatment had failed. |
|
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | No | The majority of participants were purposively selected as members of high‐risk groups (infants, pregnant women and people with treatment failure) |
| Acceptable reference standard? All tests | Yes | Two independent microscopists viewed at least 100 high power fields before declaring a slide negative |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | RDT and microscopy undertaken at different locations |
| Index test results blinded? All tests | Yes | RDT and microscopy undertaken at different locations |
| Uninterpretable results reported? All tests | Unclear | The numbers of participants originally enrolled in the study was not clearly stated, therefore it is unclear whether there were any exclusions due to invalid test results. The text "complete data were available for 1326 patients" suggests some missing data |
| Withdrawals explained? All tests | Unclear | The numbers of participants originally enrolled in the study was not clearly stated, therefore it is unclear whether there were any withdrawals. The text "complete data were available for 1326 patients" suggests some missing data. |
Kolaczinski 2004.
| Clinical features and settings |
Presenting signs and symptoms: Suspected malaria/febrile illness Previous treatment for malaria: No exclusion criteria based on previous use of antimalarials, and no data on previous antimalarial use of the participants was presented Clinical setting: Basic health units within an Afghan refugee camp Country: Pakistan (North West Frontier Province) Malaria endemicity: Not stated Malaria endemic species: 80% P. vivax, 20%P. falciparum |
|
| Participants |
Sample size: 499 Age: All age groups eligible for inclusion; actual age range of the participants not stated Sex: Both males and females eligible for inclusion; actual age range of the participants not stated Co‐morbidities and pregnancy: No exclusions based on co‐morbidities or pregnancy, and no data presented on the frequency of these conditions in the study population Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was consecutive and prospective. One RDT was tested. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood films Person(s) performing microscopy: Microscopists Microscopy setting: Basic health units within an Afghan refugee camp and HNI's reference laboratory in Peshawar Number of high power fields examined before declaring negative: 100 Number of observer or repeats: Two, one at the BHU and one at the reference laboratory Resolution of discrepancies between observers: Not clear, "all of the smears checked by the microscopist at each BHU were cross checked at HNI's reference laboratory at Pashawar" |
|
| Index and comparator tests |
Commerical name of RDT: OptiMAL (DiaMed AG, Cressier, Switzerland) Parasite(s) designed to detect:P. falciparum or mixed infection, non‐falciparum malaria species only Designated Type: Type 4 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: Microscopists RDT setting: Basic health units |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Not stated | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Participants were a consecutive series of patients attending a basic health unit with suspected malaria |
| Acceptable reference standard? All tests | Yes | Two microscopists, one working in a central laboratory, viewed at least 100 high power fields before declaring a slide negative |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | No | The index test and reference test were undertaken by the same person |
| Index test results blinded? All tests | No | The index test and reference test were undertaken by the same person |
| Uninterpretable results reported? All tests | Unclear | The number of participants originally enrolled in the study was clearly stated, and corresponded to the number presented in the analysis; therefore there were no exclusions due to invalid test results |
| Withdrawals explained? All tests | Yes | The number of participants originally enrolled in the study was clearly stated, and corresponded to the number presented in the analysis; therefore there were no withdrawals |
Kumar 1996.
| Clinical features and settings |
Presenting signs and symptoms: Febrile patients Previous treatment for malaria: No exclusion criteria based on prior use of antimalarials; relevant data collected but presented only for false positives Clinical setting: Clinic of the Malaria Research Centre Country: India (Goa) Malaria endemicity: Not stated Malaria endemic species:P. vivax andP. falciparum |
|
| Participants |
Sample size: 98 Age: Not mentioned, either as an inclusion criteria or characteristic of included participants Sex: Not mentioned, either as an inclusion criteria or characteristic of included participants Co‐morbidities and pregnancy: Not mentioned, either as an exclusion criteria or characteristic of included participants Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was prospective. The sampling method was not described. One RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood smears Person(s) performing microscopy: Not stated Microscopy setting: Clinic of the Malaria Research Centre Number of high power fields examined before declaring negative: Not stated Number of observer or repeats: Not stated Resolution of discrepancies between observers: Not applicable |
|
| Index and comparator tests |
Commerical name of RDTs: ICT Malaria‐Pf (ICT Diagnostics, Brookvale, NSW, Australia) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Stored at 4 °C prior to use Person(s) performing RDT: Not stated RDT setting: Clinic of the Malaria Research Centre |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Not stated | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | All participants were attending a Malaria Research Clinic with fever; however the sampling method was not described |
| Acceptable reference standard? All tests | Unclear | The microscopy process was not described |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Unclear | Blinding not described |
| Index test results blinded? All tests | Unclear | Blinding not described |
| Uninterpretable results reported? All tests | Unclear | The numbers of participants originally enrolled in the study was not clearly stated; therefore it is unclear whether there were any exclusions due to invalid test results |
| Withdrawals explained? All tests | Unclear | The numbers of participants originally enrolled in the study was not clearly stated; therefore it is unclear whether there were any withdrawals |
Kumar 2004.
| Clinical features and settings |
Presenting signs and symptoms: Fever Previous treatment for malaria: No mention of previous treatment for malaria, either as an exclusion criteria or a characteristic of included participants Clinical setting: Primary health centres Country: India (Karnataka state) Malaria endemicity: Not stated Malaria endemic species: Mainly P. falciparum, some P. vivax |
|
| Participants |
Sample size: 2891 Age: Not mentioned either as an exclusion criteria or a characteristic of included participants Sex: Not mentioned either as an exclusion criteria or a characteristic of included participants Co‐morbidities and pregnancy: Not mentioned either as an exclusion criteria or a characteristic of included participants Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was prospective. The sampling method was not described. One RDTs was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood film Person(s) performing microscopy: Laboratory technicians Microscopy setting: Initially undertaken at the primary health centres and later cross‐checked at the Central Malaria Laboratory Number of high power fields examined before declaring negative: Not stated Number of observer or repeats: Two Resolution of discrepancies between observers: Not described |
|
| Index and comparator tests |
Commerical name of RDT: Paracheck‐Pf (Orchid Biomedical Systems, Goa, India) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Stored at 4 °C and brought to room temperature before performing the test Person(s) performing RDT: Not stated RDT setting: Not stated |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Not stated | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | All participants were attending health centres with fever, but the sampling methods were not described |
| Acceptable reference standard? All tests | Unclear | Two independent microscopists read the slides; however the number of high power fields viewed before declaring a slide negative was not stated |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Unclear | Blinding not described |
| Index test results blinded? All tests | Unclear | Blinding not described |
| Uninterpretable results reported? All tests | Unclear | The numbers of participants originally enrolled in the study was not clearly stated; therefore it is unclear whether there were any exclusions due to invalid test results |
| Withdrawals explained? All tests | Unclear | The numbers of participants originally enrolled in the study was not clearly stated; therefore it is unclear whether there were any withdrawals |
Kyabayinze 2008.
| Clinical features and settings |
Presenting signs and symptoms: History of fever in the previous 24 h or axillary temperature 37.5 °C or over; no evidence of concomitant febrile illness; no danger signs or evidence of severe malaria Previous treatment for malaria: No exclusion criteria based on antimalarial use; data collected on prior antimalarial use but not presented for the study sample Clinical setting: Regional referral hospital outpatient department Country: Uganda Malaria endemicity: Hyperendemic Malaria endemic species: Mainly P. falciparum |
|
| Participants |
Sample size: 357 Age: Inclusion criteria over the age of six months; 46% were under the age of five; median age 11 years (range 1 to 28 years) Sex: Both males and females eligible; 60% were female and 40% male Co‐morbidities and pregnancy: People with evidence of concomitant febrile illness were excluded from the study Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was consecutive and prospective. One RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood smears Person(s) performing microscopy: Hospital microscopists Microscopy setting: Hospital laboratory Number of high power fields examined before declaring negative: 100 Number of observer or repeats: Two in most cases. A third microscopist read a random 10% of slides for quality control. Resolution of discrepancies between observers: A third external microscopist, unaware of the first two results, resolved any discordant results |
|
| Index and comparator tests |
Commerical name of RDTs: ICT Malaria‐Pf (ICT Diagnostics, Brookvale, NSW, Australia) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Storage temperature ranged from 22 °C to 29 °C, and a single spike temperature of 38 °C was recorded during transportation Person(s) performing RDT: Two independent readings by trained staff RDT setting: Hospital laboratory |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: UK DFID through the COMDIS research programme consortium | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Participants were a consecutive series of people with fever attending outpatient clinics |
| Acceptable reference standard? All tests | Yes | Two microscopists working in a central laboratory viewed at least 100 high power fields before declaring a slide negative |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Unclear | Blinding not described |
| Index test results blinded? All tests | Unclear | Blinding not described |
| Uninterpretable results reported? All tests | Yes | 7 enrolled participants were excluded due to uninterpretable blood smears |
| Withdrawals explained? All tests | Yes | 7 enrolled participants were excluded due to uninterpretable blood smears; otherwise there were no withdrawals |
Labbe 2001.
| Clinical features and settings |
Presenting signs and symptoms: Fever or history of fever in the previous 24 h Previous treatment for malaria: Excluded if gave a history of ingestion of antimalarials in the preceding month or a history of chloroquine intolerance Clinical setting: Local malaria clinics run by the Laos Institute Malariology, Parasitology and Entomology Country: Lao PDR, Vang Vieng district of Vientiane province Malaria endemicity: Not stated Malaria endemic species: Not stated |
|
| Participants |
Sample size: 196 Age: Excluded children less than one year old. No more details are given about the age presentation of the participants. Sex: Both males and females eligible. Actual proportions of males and females in the participant population not stated. Co‐morbidities and pregnancy: Participants were excluded if known to be pregnant Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was prospective. The sampling method was not described. One RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood films Person(s) performing microscopy: Expert microscopist Microscopy setting: National malaria reference centre (IMPE in Vientiane) Number of high power fields examined before declaring negative: 100 Number of observer or repeats: Unclear text states "were read by expert microscopists" Resolution of discrepancies between observers: Not applicable or unclear |
|
| Index and comparator tests |
Commerical name of RDT: PATH‐developed dipstick Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Not stated Person(s) performing RDT: Trained local healthcare providers RDT setting: Local malaria clinics |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Supported in part by the Banjamin H Kean Fellowship awarded by the American Society of Tropical Medicine and Hygiene, the Bayers Healthcare/University of Toronto fellowship in Medical Microbiology, and a Career Scientist Award from the Ontorio Ministry of Health. Development of the PATH PfHRP‐2 assay was funded by the United States Agency for International Development under the Technologies for Health Programme (Cooperative Agreement No. HRN‐A‐0096‐90007). | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | All participants were attending malaria clinic with fever symptoms, however the sampling method was unclear |
| Acceptable reference standard? All tests | Unclear | An expert microscopist viewed at least 100 high power fields before declaring a slide negative, however it is unclear whether their findings were conformed by a second reader |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | "All testing was performed blinded to the results of the other assay" |
| Index test results blinded? All tests | Yes | "All testing was performed blinded to the results of the other assay" |
| Uninterpretable results reported? All tests | Unclear | The number of participants originally enrolled in the study was clearly stated, and corresponded to the number presented in the analysis; therefore there were no exclusions due to invalid test results |
| Withdrawals explained? All tests | Yes | The number of participants originally enrolled in the study was clearly stated, and corresponded to the number presented in the analysis; therefore there were no withdrawals |
Mboera 2006a.
| Clinical features and settings |
Presenting signs and symptoms: Fever Previous treatment for malaria: No exclusions based on previous treatment, and no data presented on previous use of antimalarials Clinical setting: Hospitals, health centres and dispensaries Country: Tanzania, Babati Malaria endemicity: Prevalence of infection varying from 1.3% in highlands to 62% in the lowlands Malaria endemic species:P. falciparum |
|
| Participants |
Sample size: 308 Age: All age groups eligible. Actual age profile of participant population not presented. Sex: Both males and females eligible. Actual proportions of males and females in the participant population not stated. Co‐morbidities and pregnancy: No exclusion criteria based on co‐morbidities or pregnancy. No details of the frequency of these conditions in the participant population is presented. Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was consecutive and prospective. One RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood films Person(s) performing microscopy: Experienced microscopists Microscopy setting: Not stated Number of high power fields examined before declaring negative: 200 Number of observer or repeats: One Resolution of discrepancies between observers: Not applicable |
|
| Index and comparator tests |
Commerical name of RDT: Paracheck Pf (Orchid Biomedical Systems, Goa, India) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Stored at 4 °C and used within one month of purchase Person(s) performing RDT: Local study team trained in the use of the RDT RDT setting: Not stated |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Italian cooperation and international water management institute through the system‐wide initiative in malaria and agriculture. Also the Sir Halley Stewart Trust for one author. | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Participants were a consecutive series who had a fever and were seeking treatment for suspected malaria |
| Acceptable reference standard? All tests | No | An experienced microscopist viewed at least 200 high power fields before declaring a slide negative; however their results were not verified by a second, independent reader |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | "The blood smears were examined by experienced microscopists who were unaware which samples had been found positive in the RDT and which negative" |
| Index test results blinded? All tests | Yes | "Local team member read the results independently and without knowledge of the microscopy results" |
| Uninterpretable results reported? All tests | Unclear | The numbers of participants originally enrolled in the study was not clearly stated, therefore it is unclear whether there were any exclusions due to invalid test results |
| Withdrawals explained? All tests | Unclear | The numbers of participants originally enrolled in the study was not clearly stated, therefore it is unclear whether there were any withdrawals |
Mboera 2006b.
| Clinical features and settings |
Presenting signs and symptoms: Fever Previous treatment for malaria: No exclusions based on previous treatment, and no data presented on previous use of antimalarials Clinical setting: Hospitals, health centres and dispensaries Country: Tanzania, Dodoma Malaria endemicity: Prevalence of infection approximately 25% Malaria endemic species:P. falciparum |
|
| Participants |
Sample size: 88 Age: All age groups eligible. Actual age profile of participant population not presented. Sex: Both males and females eligible. Actual proportions of males and females in the participant population not stated. Co‐morbidities and pregnancy: No exclusion criteria based on co‐morbidities or pregnancy. No details of the frequency of these conditions in the participant population is presented. Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was consecutive and prospective. One RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood films Person(s) performing microscopy: Experienced microscopists Microscopy setting: Not stated Number of high power fields examined before declaring negative: 200 Number of observer or repeats: One Resolution of discrepancies between observers: Not applicable |
|
| Index and comparator tests |
Commerical name of RDT: Paracheck Pf (Orchid Biomedical Systems, Goa, India) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Stored at 4 °C and used within one month of purchase Person(s) performing RDT: Local study team trained in the use of the RDT. RDT setting: Not stated |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Italian cooperation and international water management institute through the system‐wide initiative in malaria and agriculture. Also the Sir Halley Stewart Trust for one author. | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Participants were a consecutive series who had a fever and were seeking treatment for suspected malaria |
| Acceptable reference standard? All tests | No | An experienced microscopist viewed at least 200 high power fields before declaring a slide negative; however their results were not verified by a second, independent reader |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | "The blood smears were examined by experienced microscopists who were unaware which samples had been found positive in the RDT and which negative" |
| Index test results blinded? All tests | Yes | Local team member read the results independently and without knowledge of the microscopy results. |
| Uninterpretable results reported? All tests | Unclear | The numbers of participants originally enrolled in the study was not clearly stated, therefore it is unclear whether there were any exclusions due to invalid test results |
| Withdrawals explained? All tests | Unclear | The numbers of participants originally enrolled in the study was not clearly stated, therefore it is unclear whether there were any withdrawals |
Mboera 2006c.
| Clinical features and settings |
Presenting signs and symptoms: Fever Previous treatment for malaria: No exclusions based on previous treatment, and no data presented on previous use of antimalarials Clinical setting: Hospitals, health centres and dispensaries Country: Tanzania, Iringa Malaria endemicity: Prevalence of infection over 73% in the lowlands, no malaria in the highlands Malaria endemic species:P. falciparum |
|
| Participants |
Sample size: 228 Age: All age groups eligible. Actual age profile of participant population not presented. Sex: Both males and females eligible. Actual proportions of males and females in the participant population not stated. Co‐morbidities and pregnancy: No exclusion criteria based on co‐morbidities or pregnancy. No details of the frequency of these conditions in the participant population is presented. Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was consecutive and prospective. One RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood films Person(s) performing microscopy: Experienced microscopists Microscopy setting: Not stated Number of high power fields examined before declaring negative: 200 Number of observer or repeats: One Resolution of discrepancies between observers: Not applicable |
|
| Index and comparator tests |
Commerical name of RDT: Paracheck Pf (Orchid Biomedical Systems, Goa, India) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Stored at 4 °C and used within one month of purchase Person(s) performing RDT: Local study team trained in the use of the RDT RDT setting: Not stated |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Italian cooperation and international water management institute through the system‐wide initiative in malaria and agriculture. Also the Sir Halley Stewart Trust for one author. | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Participants were a consecutive series who had a fever and were seeking treatment for suspected malaria |
| Acceptable reference standard? All tests | No | An experienced microscopist viewed at least 200 high power fields before declaring a slide negative; however their results were not verified by a second, independent reader |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | "The blood smears were examined by experienced microscopists who were unaware which samples had been found positive in the RDT and which negative" |
| Index test results blinded? All tests | Yes | Local team member read the results independently and without knowledge of the microscopy results |
| Uninterpretable results reported? All tests | Unclear | The numbers of participants originally enrolled in the study was not clearly stated, therefore it is unclear whether there were any exclusions due to invalid test results |
| Withdrawals explained? All tests | Unclear | The numbers of participants originally enrolled in the study was not clearly stated, therefore it is unclear whether there were any withdrawals |
Mboera 2006d.
| Clinical features and settings |
Presenting signs and symptoms: Fever Previous treatment for malaria: No exclusions based on previous treatment, and no data presented on previous use of antimalarials Clinical setting: Hospitals, health centres and dispensaries Country: Tanzania, Muleba Malaria endemicity: Prevalence of infection 40% to 44% Malaria endemic species:P. falciparum |
|
| Participants |
Sample size: 306 Age: All age groups eligible. Actual age profile of participant population not presented. Sex: Both males and females eligible. Actual proportions of males and females in the participant population not stated. Co‐morbidities and pregnancy: No exclusion criteria based on co‐morbidities or pregnancy. No details of the frequency of these conditions in the participant population is presented. Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was consecutive and prospective. One RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood films Person(s) performing microscopy: Experienced microscopists Microscopy setting: Not stated Number of high power fields examined before declaring negative: 200 Number of observer or repeats: One Resolution of discrepancies between observers: Not applicable |
|
| Index and comparator tests |
Commerical name of RDT: Paracheck Pf (Orchid Biomedical Systems, Goa, India) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Stored at 4 °C and used within one month of purchase Person(s) performing RDT: Local study team trained in the use of the RDT RDT setting: Not stated |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Italian cooperation and international water management institute through the system‐wide initiative in malaria and agriculture. Also the Sir Halley Stewart Trust for one author. | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Participants were a consecutive series who had a fever and were seeking treatment for suspected malaria |
| Acceptable reference standard? All tests | No | An experienced microscopist viewed at least 200 high power fields before declaring a slide negative; however their results were not verified by a second, independent reader |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | "The blood smears were examined by experienced microscopists who were unaware which samples had been found positive in the RDT and which negative" |
| Index test results blinded? All tests | Yes | Local team member read the results independently and without knowledge of the microscopy results. |
| Uninterpretable results reported? All tests | Unclear | The numbers of participants originally enrolled in the study was not clearly stated, therefore it is unclear whether there were any exclusions due to invalid test results |
| Withdrawals explained? All tests | Yes | The numbers of participants originally enrolled in the study was not clearly stated, therefore it is unclear whether there were any withdrawals |
Mboera 2006e.
| Clinical features and settings |
Presenting signs and symptoms: Fever Previous treatment for malaria: No exclusions based on previous treatment, and no data presented on previous use of antimalarials Clinical setting: Hospitals, health centres and dispensaries Country: Tanzania, Mvovera Malaria endemicity: Prevalence of infection about 43% Malaria endemic species:P. falciparum |
|
| Participants |
Sample size: 64 Age: All age groups eligible. Actual age profile of participant population not presented. Sex: Both males and females eligible. Actual proportions of males and females in the participant population not stated. Co‐morbidities and pregnancy: No exclusion criteria based on co‐morbidities or pregnancy. No details of the frequency of these conditions in the participant population is presented. Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was consecutive and prospective. One RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood films Person(s) performing microscopy: Experienced microscopists Microscopy setting: Not stated Number of high power fields examined before declaring negative: 200 Number of observer or repeats: One Resolution of discrepancies between observers: Not applicable |
|
| Index and comparator tests |
Commerical name of RDT: Paracheck Pf (Orchid Biomedical Systems, Goa, India) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Stored at room temperature for 12 months Person(s) performing RDT: Local study team trained in the use of the RDT RDT setting: Not stated |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Italian cooperation and international water management institute through the system‐wide initiative in malaria and agriculture. Also the Sir Halley Stewart Trust for one author. | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Participants were a consecutive series who had a fever and were seeking treatment for suspected malaria |
| Acceptable reference standard? All tests | No | An experienced microscopist viewed at least 200 high power fields before declaring a slide negative; however their results were not verified by a second, independent reader |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | "The blood smears were examined by experienced microscopists who were unaware which samples had been found positive in the RDT and which negative" |
| Index test results blinded? All tests | Yes | Local team member read the results independently and without knowledge of the microscopy results |
| Uninterpretable results reported? All tests | Unclear | The numbers of participants originally enrolled in the study was not clearly stated, therefore it is unclear whether there were any exclusions due to invalid test results |
| Withdrawals explained? All tests | Unclear | The numbers of participants originally enrolled in the study was not clearly stated, therefore it is unclear whether there were any withdrawals |
Mekonnen 2010.
| Clinical features and settings |
Presenting signs and symptoms: Febrile, clinically suspected for malaria Previous treatment for malaria: No exclusions based on previous treatment, and no relevant data presented Clinical setting: Outpatient department of a health centre Country: Ethiopia (Jimma, South‐West), 300 km south‐west of Addis Ababa, 1760 m above sea level Malaria endemicity: Not stated: transmission takes place throughout the year Malaria endemic species:P. falciparum and P. vivax |
|
| Participants |
Sample size: 240 Age: Eligible age range not stated. Actual age range of participants was 1 to 60 years, with a mean age of 25 years Sex: Both males and females eligible: 57.5% of the study participants were male, 42.5% female Co‐morbidities and pregnancy: Not mentioned, either as an exclusion criteria or characteristic of the included participants Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was prospective. The sampling method was not described. One RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood films Person(s) performing microscopy: Experienced malaria technicians Microscopy setting: Not stated Number of high power fields examined before declaring negative: 300 Number of observer or repeats: Discordant results between RDTs and slides were repeated Resolution of discrepancies between observers: Not described |
|
| Index and comparator tests |
Commerical name of RDT: CareStart Malaria Pf/Pv Combo (Access Bio Inc, Monmouth Junction, New Jersey, USA) Parasite(s) designed to detect:P. falciparum and P. vivax Designated Type: Type 5 Batch numbers: Not stated Transport and storage conditions: Stored according to the guidelines of the manufacturer and quality of package desiccant was checked before use Person(s) performing RDT: Experienced malaria technicians RDT setting: Not stated |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Recieved financial support from the School of Laboratory Studies of the Jimma Univeristy and the VLIR‐IUC program between Flanders and Jimma Univeristy. Access Bio Ltd donated the CareStart Malaria Pf/Pv Combo test kit. | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | All participants were attending a clinic with fever and suspected malaria, but the sampling method was not described |
| Acceptable reference standard? All tests | Yes | Experienced technicians independently viewed 300 high power fields before declaring a slide negative. Discordant results were repeated independently. |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | Blinding not described |
| Index test results blinded? All tests | Yes | "Results of the CareStart tests were determined prior to microscopic results with strict blinding to the microscopic examination of the blood film" |
| Uninterpretable results reported? All tests | Unclear | The number of participants originally enrolled in the study was clearly stated, and corresponded to the number presented in the analysis; therefore there were no exclusions due to invalid test results |
| Withdrawals explained? All tests | Yes | The number of participants originally enrolled in the study was clearly stated, and corresponded to the number presented in the analysis; therefore there were no withdrawals |
Mendiratta 2006.
| Clinical features and settings |
Presenting signs and symptoms: Clinically suspected to be suffering from malaria Previous treatment for malaria: No exclusions based on previous treatment, and no data presented on previous use of antimalarials, except for retrospective analysis in the case of false positive results Clinical setting: Not clear Country: Sevagram, India Malaria endemicity: Not stated Malaria endemic species:P. falciparum |
|
| Participants |
Sample size: 443 Age: Age profile of participant population not presented. Does not mention age as inclusion criteria. Sex: Both males and females eligible. Actual proportions of males and females in the participant population not stated. Co‐morbidities and pregnancy: No exclusion criteria based on co‐morbidities or pregnancy. No details of the frequency of these conditions in the participant population presented. Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was consecutive and prospective. One RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood films Person(s) performing microscopy: Experienced microscopists Microscopy setting: Department of Microbiology, Mahatma Ghandi Institute of Medical Sciences, Sevagram Number of high power fields examined before declaring negative: Not stated Number of observer or repeats: Two independent observers Resolution of discrepancies between observers: Not described |
|
| Index and comparator tests |
Commerical name of RDT: Paracheck Pf (Orchid Biomedical Systems, Goa, India) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: Not stated RDT setting: Department of Microbiology, Mahatma Ghandi Institute of Medical Sciences, Sevagram |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Not stated | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | Participants were a consecutive sample of people with fever and clinically suspected malaria; however the setting is unclear |
| Acceptable reference standard? All tests | Unclear | Microscopy undertaken by two trained microscopists, but it is was not stated how many high power fields they viewed before declaring a slide negative |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Unclear | Blinding not described |
| Index test results blinded? All tests | Unclear | Blinding not described |
| Uninterpretable results reported? All tests | Unclear | The number of participants originally enrolled in the study was clearly stated, and corresponded to the number presented in the analysis; therefore there were no exclusions due to invalid test results |
| Withdrawals explained? All tests | Yes | The number of participants originally enrolled in the study was clearly stated, and corresponded to the number presented in the analysis; therefore there were no withdrawals |
Mens 2007a.
| Clinical features and settings |
Presenting signs and symptoms: Suspected uncomplicated malaria, fever or history of fever in the previous 24 h Previous treatment for malaria: No exclusions based on previous treatment, and no data presented on previous use of antimalarials Clinical setting: Health centre Country: Tanzania Malaria endemicity: Hypoendemic Malaria endemic species:P. falciparum |
|
| Participants |
Sample size: 154 Age: 6 months to 12 years Sex: Both males and females eligible; Male:female ratio 1.8:1 Co‐morbidities and pregnancy: No exclusion criteria based on co‐morbidities. No details of the frequency of these conditions in the participant population is presented. Parasite density of microscopy positive cases: 3 cases: 160, 120 and 1000 parasites per μl |
|
| Study design | Enrollment was consecutive and prospective. Three RDTs were tested. All individuals received all three tests. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood films Person(s) performing microscopy: Experienced microscopists Microscopy setting: Not stated Number of high power fields examined before declaring negative: Not stated. Parasite density was counted against 200 leukocytes. Number of observer or repeats: Two Resolution of discrepancies between observers: Report stated that there were no discordant results between the two microscopists |
|
| Index and comparator tests |
Commerical name of RDT: Paracheck Pf (Orchid Biomedical Systems, Goa, India) OptiMAL (Diamed AG, Switzerland) ‐ P. falciparum or mixed infection, non‐falciparum malaria species only Parasite(s) designed to detect: Paracheck Pf ‐ P. falciparum OptiMAL ‐ P. falciparum or mixed infection, non‐falciparum malaria species only Designated Type: Paracheck Pf ‐ Type 1 OptiMAL ‐ Type 4 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: Two independent readers RDT setting: Not mentioned |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: The Hubrecht‐Janssen Fund, KIT, Amsterdam, Netherlands | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Participants were a consecutive sample of children with fever or history of fever in the past 24 h |
| Acceptable reference standard? All tests | Unclear | Two independent microscopists examined the slides. Unclear how many high power fields were examined before declaring a slide negative. |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | Report states that microscopists were blinded to the results of the others tests performed |
| Index test results blinded? All tests | Yes | Report states that readers were blinded to the results of the other tests performed |
| Uninterpretable results reported? All tests | Yes | Paracheck: 4 failures; OptiMAL: 4 failures |
| Withdrawals explained? All tests | No | Unclear whether test failures were repeated, or whether they were included or excluded in the analysis |
Mens 2007b.
| Clinical features and settings |
Presenting signs and symptoms: Suspected uncomplicated malaria, fever or history of fever in the previous 24 h Previous treatment for malaria: No exclusions based on previous treatment, and no data presented on previous use of antimalarials Clinical setting: Hospital outpatients Country: Kenya Malaria endemicity: Mesoendemic Malaria endemic species:P. falciparum |
|
| Participants |
Sample size: 184 Age: 6 months to 12 years Sex: Both males and females eligible; male: female ratio 1:1 Co‐morbidities and pregnancy: No exclusions based on co‐morbidities. No details of the frequency of these conditions in the participant population presented. Parasite density of microscopy positive cases: Range 400 to 828,800 parasites per μl, mean 18,680 |
|
| Study design | Enrollment was consecutive and prospective. Three RDTs were tested. All individuals received all three tests. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood films Person(s) performing microscopy: Experienced microscopists Microscopy setting: Not stated Number of high power fields examined before declaring negative: Not stated. Parasite density was counted against 200 leukocytes. Number of observer or repeats: Two Resolution of discrepancies between observers: Report stated that there were no discordant results between the two microscopists |
|
| Index and comparator tests |
Commerical name of RDT: Paracheck Pf (Orchid Biomedical Systems, Goa, India) OptiMAL (Diamed AG, Switzerland) Parascreen (Zephyr Biomedical, Verna, Goa, India) Parasite(s) designed to detect: Paracheck Pf ‐ P. falciparum OptiMAL ‐ P. falciparum or mixed infection, non‐falciparum species only Parascreen ‐ P. falciparum or mixed infection, non‐falciparum species only Designated Type: Paracheck Pf ‐ Type 1 OptiMAL ‐ Type 4 Parascreen ‐ Type 3 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: Two independent readers RDT setting: Not mentioned |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: The Hubrecht‐Janssen Fund, KIT, Amsterdam, Netherlands | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Participants were a consecutive sample of children with fever or history of fever in the past 24 h |
| Acceptable reference standard? All tests | Unclear | Two independent microscopists examined the slides. Unclear how many high power fields were examined before declaring a slide negative. |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | Report states that microscopists were blinded to the results of the other tests performed |
| Index test results blinded? All tests | Yes | Report states that readers were blinded to the results of the other tests performed |
| Uninterpretable results reported? All tests | Yes | Paracheck: 4 failures; OptiMAL: 5 failures; Parascreen: 1 failure |
| Withdrawals explained? All tests | No | Unclear whether test failures were repeated, or whether they were included or excluded in the analysis |
Mharakurwa 1997a.
| Clinical features and settings |
Presenting signs and symptoms: Clinical symptoms of malaria Previous treatment for malaria: No exclusions based on previous treatment, and no data presented on previous use of antimalarials, although this data was collected as part of the study Clinical setting: Primary health care centres Country: Hurungwe, Zimbabwe Malaria endemicity: Hyperendemic Malaria endemic species:P. falciparum |
|
| Participants |
Sample size: 136 Age: All age groups eligible. Actual age structure of the study sample not stated. Sex: Both males and females eligible. Actual ratio of males and females not stated. Co‐morbidities and pregnancy: No exclusion criteria based on co‐morbidities. No details of the frequency of these conditions in the participant population is presented. Parasite density of microscopy positive cases: Geometric mean 52 parasites per μl |
|
| Study design | Enrollment was consecutive and prospective. One RDT was tested. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood films Person(s) performing microscopy: Not stated Microscopy setting: Not stated Number of high power fields examined before declaring negative: 100 Number of observer or repeats: Not stated Resolution of discrepancies between observers: Not applicable |
|
| Index and comparator tests |
Commerical name of RDT: ParaSight‐F (Beckton Dickinson, Franklin Lakes, NJ, USA) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: Nurses who had been trained to use the test RDT setting: Primary health care centre |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Not stated | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Participants were a consecutive sample of people attending health centres with clinical symptoms of malaria |
| Acceptable reference standard? All tests | Unclear | It is unclear how many observer repeats were done, who did the microscopy and where the microscopy was done. However, it is clear that 100 high power fields were viewed before declaring a slide negative. |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | Microscopy was undertaken at a different site to the RDTs |
| Index test results blinded? All tests | Yes | RDTs were undertaken and the results recorded on‐site before microscopy was done off‐site |
| Uninterpretable results reported? All tests | Unclear | The numbers of participants originally enrolled in the study was not clearly stated, therefore it is unclear whether there were any exclusions due to invalid test results |
| Withdrawals explained? All tests | Unclear | The numbers of participants originally enrolled in the study was not clearly stated, therefore it is unclear whether there were any withdrawals |
Mharakurwa 1997b.
| Clinical features and settings |
Presenting signs and symptoms: Clinical symptoms of malaria Previous treatment for malaria: No exclusions based on previous treatment, and no data presented on previous use of antimalarials, although this data was collected as part of the study Clinical setting: Primary health care centres Country: Mutasa, Zimbabwe Malaria endemicity: Mesoendemic Malaria endemic species:P. falciparum |
|
| Participants |
Sample size: 96 Age: All age groups eligible. Actual age structure of the study sample not described. Sex: Both males and females eligible. Actual ratio of males and females not described. Co‐morbidities and pregnancy: No exclusion criteria based on co‐morbidities. No details of the frequency of these conditions in the participant population is presented. Parasite density of microscopy positive cases: Geometric mean 188 parasites per μl |
|
| Study design | Enrollment was consecutive and prospective. One RDT was tested. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood films Person(s) performing microscopy: Not stated Microscopy setting: Not stated Number of high power fields examined before declaring negative: 100 Number of observer or repeats: Not stated Resolution of discrepancies between observers: Not applicable |
|
| Index and comparator tests |
Commerical name of RDT: ParaSight‐F (Beckton Dickinson, Franklin Lakes, NJ, USA) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: Nurses who had been trained to use the test RDT setting: Primary health care centre |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Not stated | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Participants were a consecutive sample of people attending health centres with clinical symptoms of malaria |
| Acceptable reference standard? All tests | Unclear | It is unclear how many observer repeats were done, who did the microscopy and where the microscopy was done. However, it is clear that 100 high power fields were viewed before declaring a slide negative. |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | Microscopy was undertaken at a different site to the RDTs |
| Index test results blinded? All tests | Yes | RDTs were undertaken and the results recorded on‐site before microscopy was done off‐site |
| Uninterpretable results reported? All tests | Unclear | The numbers of participants originally enrolled in the study was not clearly stated, therefore it is unclear whether there were any exclusions due to invalid test results |
| Withdrawals explained? All tests | Unclear | The numbers of participants originally enrolled in the study was not clearly stated, therefore it is unclear whether there were any withdrawals |
Mharakurwa 1997c.
| Clinical features and settings |
Presenting signs and symptoms: Specimens sent to the Public Health Laboratory for malaria diagnosis Previous treatment for malaria: No exclusions based on previous treatment, and no data presented on previous use of antimalarials, although this data was collected as part of the study Clinical setting: Primary health care centres Country: Harare, Zimbabwe Malaria endemicity: Hypoendemic Malaria endemic species:P. falciparum |
|
| Participants |
Sample size: 213 Age: All age groups eligible. Actual age structure of the study sample not described. Sex: Both males and females eligibles. Actual ratio of males and females not described. Co‐morbidities and pregnancy: No exclusion criteria based on co‐morbidities. No details of the frequency of these conditions in the participant population is presented. Parasite density of microscopy positive cases: Geometric mean 2 parasites per μl |
|
| Study design | Enrollment was consecutive and prospective. One RDT was tested. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood films Person(s) performing microscopy: Not stated Microscopy setting: Not stated Number of high power fields examined before declaring negative: 100 Number of observer or repeats: Not stated Resolution of discrepancies between observers: Not applicable |
|
| Index and comparator tests |
Commerical name of RDT: ParaSight‐F (Beckton Dickinson, Franklin Lakes, NJ, US) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: Nurses who had been trained to use the test RDT setting: Primary health care centre |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Not stated | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | Participants included all people who had a blood sample sent to the Public Health Laboratory for diagnosis of malaria ‐ the criteria for referral is unclear |
| Acceptable reference standard? All tests | Unclear | It is unclear how many observer repeats were done, who did the microscopy and where the microscopy was done. However, it is clear that 100 high power fields were viewed before declaring a slide negative. |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | Microscopy was undertaken at a different site to the RDTs |
| Index test results blinded? All tests | Yes | RDTs were undertaken and the results recorded on‐site before microscopy was done off‐site |
| Uninterpretable results reported? All tests | Unclear | The numbers of participants originally enrolled in the study was not clearly stated; therefore it is unclear whether there were any exclusions due to invalid test results |
| Withdrawals explained? All tests | Unclear | The numbers of participants originally enrolled in the study was not clearly stated; therefore it is unclear whether there were any withdrawals |
Mohapatra 1996.
| Clinical features and settings |
Presenting signs and symptoms: Clinical symptoms of malaria Previous treatment for malaria: No exclusions based on previous treatment, and no data presented on previous use of antimalarials, although this data was collected as part of the study Clinical setting: Malaria clinics set up in the field Country: India, Assam Malaria endemicity: Highly endemic Malaria endemic species: Mainly P. falciparum |
|
| Participants |
Sample size: 100 Age: All age groups eligible; actual age range of the participants not reported Sex: Both males and females eligible; numbers of male and female participants not reported Co‐morbidities and pregnancy: No exclusion criteria based on pregnancy or comorbidity, and no relevant data presented for the included participants Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was random and prospective. One RDT was tested. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood films Person(s) performing microscopy: Not stated Microscopy setting: Malaria clinic set up in the field Number of high power fields examined before declaring negative: Not stated Number of observer or repeats: Not stated Resolution of discrepancies between observers: Not applicable |
|
| Index and comparator tests |
Commerical name of RDT: ICT Malaria Pf (ICT Diagnostics, Sydney, Australia) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: Not stated RDT setting: Malaria clinic set up in the field |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Not stated | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | All participants were a random sample of people attending malaria clinics with clinical symptoms of malaria. |
| Acceptable reference standard? All tests | Unclear | There is no information presented on who performed the test, the number of observers, or the number of high power fields viewed before declaring a slide negative |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Unclear | Blinding not described |
| Index test results blinded? All tests | Unclear | Blinding not described |
| Uninterpretable results reported? All tests | Unclear | The number of participants enrolled in the study was clearly stated, and corresponded to the number presented in the analysis, therefore there were no exclusions due to invalid test results |
| Withdrawals explained? All tests | Yes | The number of participants enrolled in the study was clearly stated, and corresponded to the number presented in the analysis, therefore there were no withdrawals |
Moonasar 2009.
| Clinical features and settings |
Presenting signs and symptoms: Fever or headache or chills Previous treatment for malaria: Patients who had recent malaria or had recently been on malaria treatment were excluded Clinical setting: Clinics Country: South Africa (Vhembe district, Limpopo province) Malaria endemicity: Not stated. The study was conducted during the high‐transmission season in an area chosen because it had the highest incidence of malaria in the province for the previous nine years. Malaria endemic species: Mainly P. falciparum |
|
| Participants |
Sample size: 405 Age: All ages eligible for inclusion; actual age range was 1 to 81 years, median 24.5 years Sex: Both males and females eligible for inclusion; 56% of included participants were male Co‐morbidities and pregnancy: Severely ill patients needing referral; patients with an obvious non‐malarial fever and pregnant women were excluded Parasite density of microscopy positive cases: Range 440 to >20,000 parasites per μl. Median 25,680. |
|
| Study design | Enrollment was consecutive and prospective. One RDT was tested. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood films Person(s) performing microscopy: Specialised malaria microscopists Microscopy setting: Health Centre Number of high power fields examined before declaring negative: 100 (stated that "standard techniques" were used and gave an appropriate reference) Number of observer or repeats: Two independent readers Resolution of discrepancies between observers: In the case of discordant results between microscopy and RDT, a medical technologist at the Limpopo Department of Health reference centre who was highly skilled in malaria microscopy and blinded to previous results re‐read the slides. This result was taken to be correct. |
|
| Index and comparator tests |
Commerical name of RDT: ICT Malaria Pf (ICT Diagnostics, Sydney, Australia) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: Nurses trained in RDT testing RDT setting: Outpatient clinic |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Ernest Oppenheimer Trust provided financial assistance in conducting the study | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Participants were a consecutive series of people attending a health centre with fever, headache or chills |
| Acceptable reference standard? All tests | Yes | Two experienced microscopists (3 in the case of discordant results between microscopy and RDT) independently viewed at least 100 high power fields before declaring a slide negative |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | The microscopists were blinded to the RDT results and read the thin and thick films independently |
| Index test results blinded? All tests | Yes | RDTs were carried out first and result recorded by the nurse at the clinic |
| Uninterpretable results reported? All tests | Unclear | The number enrolled is clearly stated and corresponds to the number included in the analysis; therefore we can assume that there were no exclusions due to invalid results |
| Withdrawals explained? All tests | Yes | The number enrolled is clearly stated and corresponds to the number included in the analysis; therefore we can assume that there were no withdrawals |
Msellem 2009.
| Clinical features and settings |
Presenting signs and symptoms: Fever in the previous 24 h and symptoms compatible with uncomplicated malaria Previous treatment for malaria: No exclusions based on previous antimalarial use, and no data presented for the study sample Clinical setting: Four primary health care units Country: Zanzibar (Muyuno and Uzini on Unguja Island and Kinyasini and Mzambarauni on Pemba Island) Malaria endemicity: Recorded parasite rates between 10% and 50% in different age groups. The four study sites aimed to provide a representative picture of Zanzibar with regard to malaria epidemiology. The study was conducted during both the low transmission and high transmission seasons. Malaria endemic species:P. falciparum |
|
| Participants |
Sample size: 1005 were allocated to receive RDTs Age: All ages eligible for inclusion; 55% of participants were under the age of five years Sex: Both males and females eligible for inclusion; actual proportions of males and females in the study sample not stated Co‐morbidities and pregnancy: There were no exclusions based on co‐morbidities or pregnancy; and no data presented on the frequency of these conditions in the study participants Parasite density of microscopy positive cases: Geometric mean 3840 parasites per μl, range 10 to 457,236, 95% CI 3150 to 4681 |
|
| Study design | Enrollment into the study was consecutive and participants were allocated to receive RDTs according to the week of the study (quasi‐randomly). Enrollment was prospective. One RDT was tested. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick blood films Person(s) performing microscopy: Qualified microscopists Microscopy setting: Central laboratory Number of high power fields examined before declaring negative: 100 Number of observer or repeats: Two independent readers Resolution of discrepancies between observers: Examined by the third reader (decision rule not stated) |
|
| Index and comparator tests |
Commerical name of RDT: ParaCheck‐Pf (Orchid Biomedical Systems, India) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: Nurses trained in RDT testing RDT setting: Outpatient clinic |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Not stated | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Participants were consecutively sampled from people attending clinic with fever in the previous 24 h and with symptoms compatible with uncomplicated malaria |
| Acceptable reference standard? All tests | Yes | Two independent microscopists working in a central laboratory viewed 100 high power field before declaring a slide negative |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | The microscopy was undertaken at a different location to the RDTs |
| Index test results blinded? All tests | Yes | RDTs were undertaken and results recorded before the microscopy results became available |
| Uninterpretable results reported? All tests | Unclear | There were no reports of any uninterpretable results, and the number enrolled was clearly stated and corresponds with the number presented in the analysis |
| Withdrawals explained? All tests | Yes | There were no withdrawals; the number enrolled in the study was clearly stated and corresponds with the number presented in the analysis |
Murahwa 1999.
| Clinical features and settings |
Presenting signs and symptoms: Clinical signs and symptoms associated with malaria Previous treatment for malaria: Not mentioned, either as an exclusion criteria or characteristic of included participants Clinical setting: Local clinic Country: Zimbabwe (Burma Valley, Mutarre District, Manicaland) Malaria endemicity: Mesoendemic Malaria endemic species:P. falciparum |
|
| Participants |
Sample size: 123 for ICT Malaria Pf, 100 for ParaSight‐F Age: Not mentioned, either as an exclusion criteria or characteristic of included participants Sex: Not mentioned, either as an exclusion criteria or characteristic of included participants Co‐morbidities and pregnancy: Not mentioned, either as an exclusion criteria or characteristic of included participants Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was prospective. The sampling method was not described. One RDT was tested. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood films Person(s) performing microscopy: Microscopists Microscopy setting: Not stated Number of high power fields examined before declaring negative: Not stated. However, the alternative quality measure of viewing 300 white blood cells (WBCs) before declaring a slide negative was used. Number of observer or repeats: Two independent readers Resolution of discrepancies between observers: Not described |
|
| Index and comparator tests |
Commerical name of RDT: ParaSight‐F (Beckton Dickinson, Franklin Lakes, NJ, USA) ICT Malaria Pf (ICT Diagnostics, Brookvale, NSW, Australia) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: Not stated RDT setting: Not stated |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Not stated | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | Participants were all people presenting at an outpatient clinic with clinical signs and symptoms of malaria, but the sampling method was not described |
| Acceptable reference standard? All tests | Unclear | Two independent microscopists viewed at least 300 WBCs. Unclear if this is equivalent to 100 high power fields. |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | RDT tests results were coded and recorded separately for each test; two microscopists examined the slides blindly |
| Index test results blinded? All tests | Yes | RDT tests were performed and results recorded before microscopy was undertaken |
| Uninterpretable results reported? All tests | Yes | Six ICT Malaria tests and three ParaSight‐F tests gave invalid results and were excluded from the analysis |
| Withdrawals explained? All tests | No | Unclear why only 100 of 123 participants received ParaSight‐F |
Mwanza 2005.
| Clinical features and settings |
Presenting signs and symptoms: Fever Previous treatment for malaria: Not mentioned, either as an exclusion criteria or characteristic of included participants Clinical setting: Outpatient clinics Country: Zambia (copper belt, Ndola and Kitwe) Malaria endemicity: Not stated Malaria endemic species: Not stated |
|
| Participants |
Sample size: 119 Age: Inclusion criteria: adults and children aged over 60 months Sex: Not reported, no mention of sex as inclusion or exclusion criteria Co‐morbidities and pregnancy: Not reported, no mention of these conditions as inclusion or exclusion criteria Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was prospective. The sampling method was not described. One RDT was tested. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy Person(s) performing microscopy: Not stated Microscopy setting: Not stated Number of high power fields examined before declaring negative: Not stated Number of observer or repeats: Not stated Resolution of discrepancies between observers: Not applicable |
|
| Index and comparator tests |
Commerical name of RDT: Hexagon Malaria Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: Not stated RDT setting: Not stated |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Not stated | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | Participants were all attending outpatient clinics with fever, however the sampling method was not described |
| Acceptable reference standard? All tests | Unclear | Microscopy process is not described |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Unclear | Blinding not described |
| Index test results blinded? All tests | Unclear | Blinding not described |
| Uninterpretable results reported? All tests | Unclear | The number of participants originally enrolled in the study was not clearly stated, therefore it is unclear whether there were any exclusions due to invalid test results |
| Withdrawals explained? All tests | Unclear | The number of participants originally enrolled in the study was not clearly stated, therefore it is unclear whether there were any withdrawals |
Nicastri 2009a.
| Clinical features and settings |
Presenting signs and symptoms: Fever over 38 °C for less than 10 days Previous treatment for malaria: Participants with previous antimalarial treatment (timescale not stated) were excluded Clinical setting: Outpatient clinics at two peripheral hospitals Country: Tanzania (Pemba Island and Iringa) Malaria endemicity: Not stated Malaria endemic species:P. falciparum |
|
| Participants |
Sample size: 336 Age: Inclusion criteria: adults and children aged over 12 months Sex: Not reported, no mention of sex as inclusion or exclusion criteria Co‐morbidities and pregnancy: Excluded patients with signs of severe malaria, or with diagnoses of mental illness, measles, chickenpox, otitis, infected wounds or pneumonia Parasite density of microscopy positive cases: Not presented. |
|
| Study design | Enrolment was prospective. The sampling method was not described. One RDT was tested. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood smears Person(s) performing microscopy: Laboratory technician trained and supported with blood slide reading Microscopy setting: Hospital laboratory Number of high power fields examined before declaring negative: 200 Number of observer or repeats: Not stated Resolution of discrepancies between observers: Not applicable |
|
| Index and comparator tests |
Commerical name of RDT: ParaHIT‐f (Span Diagnostics Ltd, Surat, India) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: Laboratory technician RDT setting: Hospital laboratory |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Part of the activities carried out by the Programme Aid 8282 in Tanzania, funded by the Italian Cooperation and Ministry of Foreign Affairs of Italy. The American Society of Tropical Medicine and Hygiene assisted with the publication expenses. | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | All participants were attending an outpatient department with fever, but the sampling method was not described |
| Acceptable reference standard? All tests | Unclear | Skilled technicians viewed up to 200 high powered fields before declaring negative; however it is unclear how many observers or repeats were used |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Unclear | Blinding not described |
| Index test results blinded? All tests | Unclear | Blinding not described |
| Uninterpretable results reported? All tests | Yes | There do not appear to be any uninterpretable results, as the number of participants recruited into the study is clearly presented and corresponds with the number presented in the analysis |
| Withdrawals explained? All tests | Yes | There do not appear to be any withdrawals, as the number of participants recruited into the study is clearly presented and corresponds with the number presented in the analysis |
Nicastri 2009b.
| Clinical features and settings |
Presenting signs and symptoms: Fever over 38 °C for less than 10 days Previous treatment for malaria: Participants with previous antimalarial treatment (timescale not stated) were excluded Clinical setting: Outpatient clinics at two peripheral hospitals Country: Tanzania (Pemba Island and Iringa) Malaria endemicity: Not stated Malaria endemic species:P. falciparum |
|
| Participants |
Sample size: 336 Age: Inclusion criteria: adults and children aged over 12 months Sex: Not reported, no mention of sex as inclusion or exclusion criteria Co‐morbidities and pregnancy: Excluded patients with signs of severe malaria, or with diagnoses of mental illness, measles, chickenpox, otitis, infected wounds or pneumonia Parasite density of microscopy positive cases: Not clear |
|
| Study design | Enrollment was prospective. The sampling method was not described. One RDT was tested. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: PCR |
|
| Index and comparator tests |
Commerical name of RDT: ParaHIT‐f (Span Diagnostics Ltd, Surat, India) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: Laboratory technician RDT setting: Hospital laboratory |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Part of the activities carried out by the Programme Aid 8282 in Tanzania, funded by the Italian Cooperation and Ministry of Foreign Affairs of Italy. The American Society of Tropical Medicine and Hygiene assisted with the publication expenses | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | All participants were attending an outpatient department with fever, but the sampling method was not described |
| Acceptable reference standard? All tests | Yes | Reference standard was PCR |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Unclear | Blinding not described |
| Index test results blinded? All tests | Unclear | Blinding not described |
| Uninterpretable results reported? All tests | Unclear | There do not appear to be any uninterpretable results, as the number of participants recruited into the study is clearly presented and corresponds with the number presented in the analysis |
| Withdrawals explained? All tests | Yes | There do not appear to be any withdrawals, as the number of participants recruited into the study is clearly presented and corresponds with the number presented in the analysis |
Nigussie 2008a.
| Clinical features and settings |
Presenting signs and symptoms: Acutely febrile patients Previous treatment for malaria: No exclusions based on previous treatment; 220 participants were interviewed regarding previous antimalarial use and 24 of these (11%) reported antimalarial use in the previous month Clinical setting: Health centre outpatient departments Country: Ethiopia (Wondo‐Genet) Malaria endemicity: Not stated Malaria endemic species:P. falciparum and P. vivax |
|
| Participants |
Sample size: 460 enrolled, 452 received the test Age: All ages eligible. Actual age range 1 to 60 years. Sex: 242 males (52.6%), 218 females (47.4%) Co‐morbidities and pregnancy: No exclusion criteria based on co‐morbidities. No details of the frequency of these conditions in the participant population is presented. Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was consecutive and prospective. Two RDTs were tested in the study, these are reported separately in this review. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood films Person(s) performing microscopy: Technicians who were members of the research team, and independent readers at a central laboratory Microscopy setting: Health centres and Akilu Lemma Institute of Pathobiology parasitology laboratory Number of high power fields examined before declaring negative: 100 Number of observer or repeats: Two, one at the health centre and one at the central laboratory Resolution of discrepancies between observers: There were no discordant results |
|
| Index and comparator tests |
Commerical name of RDT: Paracheck Pf (Orchid Biomedical Systems, Goa, India) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: Two well experienced technicians who were part of the research team RDT setting: Health centres |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Paracheck Pf kits were provided by the Federal Democratic Republic of Ethiopia Ministry of Health | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Participants were a consecutive sample of people attending health centre outpatient departments with an acute fever |
| Acceptable reference standard? All tests | Yes | Two independent readers viewed at least 100 high power fields before declaring a slide negative. One reader was based at a central laboratory, and there were no discordant results between readers. |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Unclear | Blinding not described |
| Index test results blinded? All tests | Unclear | Blinding not described |
| Uninterpretable results reported? All tests | Yes | Eight participants were excluded due either to incomplete information on either the Paracheck test or the malaria slide |
| Withdrawals explained? All tests | Yes | The number of participants enrolled in the study is clearly stated and corresponds to the number presented in the analysis minus the number reported to have invalid test results or incomplete data |
Nigussie 2008b.
| Clinical features and settings |
Presenting signs and symptoms: Acutely febrile patients Previous treatment for malaria: No exclusions based on previous treatment; 220 participants were interviewed regarding previous antimalarial use and 24 of these (11%) reported antimalarial use in the previous month Clinical setting: Health centre outpatient departments Country: Ethiopia (Wondo‐Genet) Malaria endemicity: Not stated Malaria endemic species:P. falciparum and P. vivax |
|
| Participants |
Sample size: 259 received RDT, although 460 were enrolled in the study Age: All ages eligible. Actual age range 1 to 60 years. Sex: Males and females eligible for the study, actual numbers who received Parascreen not presented Co‐morbidities and pregnancy: No exclusions criteria based on co‐morbidities. No details of the frequency of these conditions in the participant population is presented. Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was consecutive and prospective. Two RDTs were tested in the study, these are reported separately in this review | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood films Person(s) performing microscopy: Technicians who were members of the research team, and independent readers at a central laboratory Microscopy setting: Health centres and Akilu Lemma Institute of Pathobiology parasitology laboratory Number of high power fields examined before declaring negative: 100 Number of observer or repeats: Two, one at the health centre and one at the central laboratory Resolution of discrepancies between observers: There were no discordant results |
|
| Index and comparator tests |
Commerical name of RDT: Parascreen Pan/Pf (Zephyr Biomedical, Verna, Goa, India) Parasite(s) designed to detect:P. falciparum or mixed infection, non‐falciparum species only Designated Type: Type 3 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: Two well experienced technicians who were part of the research team RDT setting: Health centres |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: The Global Fund to fight AIDS, TB and Malaria through the Federal Democratic Republic Ethiopian Ministry of Health | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | Due to a shortage of test kits, only 259 of the 460 participants enrolled in the study received this RDT test, and it is not clear how these participants were selected |
| Acceptable reference standard? All tests | Yes | Two independent readers viewed at least 100 high power fields before declaring a slide negative. One reader was based at a central laboratory and there were no discordant results between readers. |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Unclear | Blinding not described |
| Index test results blinded? All tests | Unclear | Blinding not described |
| Uninterpretable results reported? All tests | Yes | Eight participants were excluded due either to incomplete information on either the Paracheck test or the malaria slide |
| Withdrawals explained? All tests | Yes | The number of participants enrolled in the study is clearly stated and corresponds to the number presented in the analysis minus the number reported to have invalid test results or incomplete data |
Nwuba 2001.
| Clinical features and settings |
Presenting signs and symptoms: Fever 38 °C or above, or other symptoms indicative of malaria Previous treatment for malaria: No exclusions based on previous treatment. Approximately 60% of participants had taken antimalarial drugs one day to three weeks prior to the hospital visit. Clinical setting: Paediatric outpatient clinic, University College Hospital Country: Nigeria, Ibadan Malaria endemicity: Not stated Malaria endemic species: Not stated |
|
| Participants |
Sample size: 77 Age: Children only. Age range not stated. Sex: Both males and females eligible. Actual proportions of males and females in the participant population not stated. Co‐morbidities and pregnancy: No exclusion criteria based on co‐morbidities. No details of the frequency of these conditions in the participant population is presented. Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was prospective. The sampling method was not described. One RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood films Person(s) performing microscopy: Stated as "workers" Microscopy setting: Hospital laboratory Number of high power fields examined before declaring negative: 200 Number of observer or repeats: Two independent microscopists Resolution of discrepancies between observers: Not stated |
|
| Index and comparator tests |
Commerical name of RDT: ICT Malaria Pf (ICT Diagnostics, Sydney, Australia) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Not described. Person(s) performing RDT: Not stated RDT setting: Paediatric outpatient clinic |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Not stated | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | The study included 77% of children presenting to an outpatient clinic during the study period with fever or other symptoms of malaria; the method of selection of these patients was not described |
| Acceptable reference standard? All tests | Yes | The independent microscopists viewed at least 200 high power fields before declaring a slide negative. Level of training of the "two workers" is not described, but microscopy was undertaken in a major hospital environment, and we therefore assumed experienced microscopists. |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | Report stated that the microscopists had no knowledge of the RDT test results |
| Index test results blinded? All tests | Yes | The test was carried out prior to the microscopy. |
| Uninterpretable results reported? All tests | Unclear | The number of participants originally enrolled in the study was not clearly stated, therefore it is unclear whether there were any exclusions due to invalid test results |
| Withdrawals explained? All tests | Unclear | The number of participants originally enrolled in the study was not clearly stated, therefore it is unclear whether there were any withdrawals |
Omar 1999.
| Clinical features and settings |
Presenting signs and symptoms: Febrile or other commonly associated malaria symptoms Previous treatment for malaria: Not mentioned either as an exclusion criteria or characteristic of included participants Clinical setting: Outpatient clinic at a Primary Healthcare Centre Country: Saudi Arabia Malaria endemicity: Not stated Malaria endemic species: 90% P. falciparum |
|
| Participants |
Sample size: 38 Age: Included participants aged 7 to 80 years Sex: Male:Female ratio 3:1 Co‐morbidities and pregnancy: Not mentioned Parasite density of microscopy positive cases: Mean 7476 parasites per μl |
|
| Study design | Enrollment was prospective. The sampling method was not described. One RDT was evaluated | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick blood film Person(s) performing microscopy: Microscopist checked by consultant Microscopy setting: Parasitology laboratory Number of high power fields examined before declaring negative: Not stated Number of observer or repeats: Two observers but unclear whether they worked independently Resolution of discrepancies between observers: Not stated |
|
| Index and comparator tests |
Commerical name of RDT: ParaSIght‐F (Beckton Dickinson, Franklin Lakes, NJ, USA) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Not described. Person(s) performing RDT: Two investigators RDT setting: Not stated |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Not stated | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | Participants were attending outpatient clinics with fever or other symptoms of malaria, but the sampling method was not described |
| Acceptable reference standard? All tests | Unclear | Unclear how many high power fields were examined before declaring a slide negative and unclear if the two observers worked independently |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Unclear | Blinding not described |
| Index test results blinded? All tests | Unclear | Blinding not described |
| Uninterpretable results reported? All tests | Unclear | The number of participants originally enrolled in the study was not clearly stated, therefore it is unclear whether there were any exclusions due to invalid test results |
| Withdrawals explained? All tests | Unclear | The number of participants originally enrolled in the study was not clearly stated, therefore it is unclear whether there were any withdrawals |
Pandya 2001.
| Clinical features and settings |
Presenting signs and symptoms: Fever Previous treatment for malaria: No exclusions based on previous treatment and no data presented on previous treatment Clinical setting: Regional Health and Family Welfare Office Malaria Clinic Country: India (Gujarat) Malaria endemicity: Not stated Malaria endemic species:P. falciparum and P. vivax |
|
| Participants |
Sample size: 468 Age: 10 aged under 5 years, 458 aged 5 and older Sex: 298 males, 170 females Co‐morbidities and pregnancy: No exclusions due to co‐morbidities or pregnancy, and actual numbers of participants with these conditions not presented Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment appeared to be consecutive, but may have been based only on those for whom a blood slide had been taken (criteria for taking blood slide unclear). Enrollment was prospective. One RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick blood film Person(s) performing microscopy: Not stated Microscopy setting: Not stated Number of high power fields examined before declaring negative: Not stated Number of observer or repeats: Not stated Resolution of discrepancies between observers: Not applicable |
|
| Index and comparator tests |
Commerical name of RDT: Paracheck‐Pf (Orchid Biomedical Systems, Goa, India) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Not described. Person(s) performing RDT: Not stated RDT setting: Not stated |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Not stated | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | All participants were children attending a clinic with fever, but the sampling method was unclear |
| Acceptable reference standard? All tests | Unclear | No description of the microscopy process provided |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Unclear | Blinding not described |
| Index test results blinded? All tests | Unclear | Blinding not described |
| Uninterpretable results reported? All tests | No | One enrolled individual is missing from the results table. The reason for this is unclear. |
| Withdrawals explained? All tests | No | One enrolled individual is missing from the results table. The reason for this is unclear. |
Pattanasin 2003.
| Clinical features and settings |
Presenting signs and symptoms: Fever or history of fever and suspected diagnosis of uncomplicated malaria Previous treatment for malaria: No mention of previous treatment for malaria, either as an exclusion criteria or a characteristic of included participants Clinical setting: Not stated Country: Thailand (Mae Sod) Malaria endemicity: Not stated, peak transmission season Malaria endemic species:P. falciparum and P. vivax |
|
| Participants |
Sample size: 271 Age: Children aged under 2 years were excluded. The study included participants aged two to 81 years; 71% were aged under 15 years. Sex: Male: female ratio was 1.7:1 Co‐morbidities and pregnancy: Pregnant women were excluded Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrolment was prospective. The sampling method was not described. Two RDTs were evaluated, the vast majority of participants received both RDTs. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood film Person(s) performing microscopy: Not stated Microscopy setting: Not stated Number of high power fields examined before declaring negative: Not stated Number of observer or repeats: Not stated Resolution of discrepancies between observers: Not applicable |
|
| Index and comparator tests |
Commerical name of RDT: Paracheck‐Pf (Orchid Biomedical Systems, Goa, India) OptiMAL‐IT (DiaMed AG, Cressier, Switzerland) Parasite(s) designed to detect: Paracheck‐Pf ‐ P. falciparum OptiMAL‐IT ‐ P. falciparum or mixed infection, non‐falciparum species only Designated Type: Paracheck‐Pf ‐ Type 1 OptiMAL‐IT ‐ Type 4 Batch numbers: Not stated Transport and storage conditions: Kept at room temperature and opened just before performing the test to avoid humidity Person(s) performing RDT: Not stated RDT setting: Not stated |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Not stated | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | All participants had a fever and suspected malaria, but the exact clinical setting and the sampling method were not described |
| Acceptable reference standard? All tests | Unclear | No details of the microscopy process given |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Unclear | Blinding not described |
| Index test results blinded? All tests | Yes | Test results were recorded without reference to the microscopy results |
| Uninterpretable results reported? All tests | Yes | Doubtful and invalid results were reported (4 of 271) |
| Withdrawals explained? All tests | Unclear | Almost all participants were reported to receive the same index and reference tests (271 participants in total: 266 received OptMAL, 269 received Paracheck‐Pf); the numbers presented in the analysis correspond |
Rakotonirina 2008.
| Clinical features and settings |
Presenting signs and symptoms: Fever over 37.5 °C or history of fever in the previous 24 h Previous treatment for malaria: Participants with recent antimalarial use were not excluded from the study; 34% of participants declared antimalarial use Clinical setting: Two primary health centres Country: Madagascar (Tsiroanomandidy on the west foothill areas of the Highlands) Malaria endemicity: Low and predominantly seasonal Malaria endemic species:P. falciparum (80%) andP. vivax |
|
| Participants |
Sample size: 313 Age: All age groups were eligible for inclusion; the actual age range of the included participants was 6 months to 79 years (median age 10 years) Sex: Male: Famale ratio was 1.2:1 Co‐morbidities and pregnancy: Pregnant women were excluded, as were people with signs of severe or complicated malaria Parasite density of microscopy positive cases: Range 32 to 52,750 parasites per μl, mean 4104, Standard Deviation 7894 |
|
| Study design | Enrolment was consecutive and prospective. Two RDTs were evaluated; all participants received both RDTs. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: PCR |
|
| Index and comparator tests |
Commerical name of RDT: OptiMAL‐IT (DiaMed AG, Cressier, Switzerland) PALUTOP Parasite(s) designed to detect: OptiMAL‐IT ‐ P. falciparum or mixed infection, non‐falciparum species only PALUTOP ‐ P. falciparum, P.vivax and other malaria types Designated Type: OptiMAL‐IT ‐ Type 4 PALUTOP ‐ Type 6 Batch numbers: OptiMAL‐IT ‐ 46110.85.01 PALUTOP ‐ 91014 Transport and storage conditions: Transported and maintained at the study sites (primary health centres) at room temperature and opened just before use to avoid humidity damage Person(s) performing RDT: Trained technician RDT setting: Primary health centres |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Global Fund Project for Madagascar, Round 3 | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Participants were a consecutive sample of patients attending primary health centres with fever or history of fever in the previous 24 h |
| Acceptable reference standard? All tests | Yes | Reference standard was PCR |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | Stated that the PCR operator was blind to the results of the other tests performed |
| Index test results blinded? All tests | Yes | Stated that the test readers were blind to the results of the other tests performed |
| Uninterpretable results reported? All tests | Yes | There were no test failures with either RDT |
| Withdrawals explained? All tests | Yes | The number of participants enrolled in the study is clearly stated and corresponds to the number presented in the analysis |
Ratsimbasoa 2007.
| Clinical features and settings |
Presenting signs and symptoms: Fever over 37.5 °C or history of fever in the previous 24 h, with typical malaria symptoms. Patients with signs of severe or complicated malaria were excluded. Previous treatment for malaria: Participants with recent antimalarial use were not excluded from the study; 17% of participants reported antimalarial use Clinical setting: Primary health centres Country: Madagascar. Rural areas of Mahasolo (western foothills areas of the highlands) and Saharevo (eastern foothills areas of the highlands). Malaria endemicity: Low and predominantly seasonal in both areas Malaria endemic species: Predominantly P. falciparum; someP. vivax |
|
| Participants |
Sample size: 194 Age: All groups eligible for inclusion not stated; actual age range of the included participants was 1 to 79 years (mean age 15.2 years); 12.9% were under five years of age Sex: Male: female ratio was 0.98:1 Co‐morbidities and pregnancy: Pregnant women were excluded, as were people with signs of severe or complicated malaria Parasite density of microscopy positive cases: Range 16 to 233,600 parasites per μl, mean 6564, Standard Deviation 26,553 |
|
| Study design | Enrolment was prospective. The sampling method was not described. Two RDTs were evaluated, all participants received both RDTs. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood films Person(s) performing microscopy: An experienced technician Microscopy setting: Not stated Number of high power fields examined before declaring negative: 200 Number of observer or repeats: One Resolution of discrepancies between observers: Not applicable |
|
| Index and comparator tests |
Commerical name of RDT: CareStart Malaria Pf/Pan (Access Bio Inc., Monmouth Junction, NJ, USA) SD Malaria Antigen Bioline Pf/Pan (Standard Diagnostics, Suwon City, South Korea) OptiMAL‐IT (DiaMed AG, Cressier, Switzerland) Parasite(s) designed to detect:P. falciparum or mixed infection, non‐falciparum species only Designated Type: Type 4 Batch numbers: CareStart Malaria ‐ J25IL, J35IL, J45IL, J55IL SD Malaria Antigen Bioline ‐ T5001, T5002, T5003, T5004 OptiMAL‐IT ‐ 46110.73.01, 46110.74.01, 46110.75.01 Transport and storage conditions: Transported and maintained at the study sites (primary health centres) at room temperature and opened just before use to avoid humidity damage Person(s) performing RDT: A technician RDT setting: Not stated |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Global Fund Project for Madagascar, Round 3. The manufacturers supplied the test kits. | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | All participants were attending primary health centres with fever and symptoms of malaria, but the sampling method was not described |
| Acceptable reference standard? All tests | No | An expert technician viewed 200 high power fields before declaring a slide negative; however their findings were not verified by a second independent reader |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | "Analyzed without reference to the RDT results" |
| Index test results blinded? All tests | Yes | The RDTs were undertaken before the microscopy |
| Uninterpretable results reported? All tests | Unclear | The number recruited into the study was clearly stated, and corresponded with the number presented in the analysis |
| Withdrawals explained? All tests | Yes | The number recruited into the study was clearly stated, and corresponded with the number presented in the analysis |
Ratsimbasoa 2008.
| Clinical features and settings |
Presenting signs and symptoms: Fever or fever in the previous 24 h with typical malaria symptoms Previous treatment for malaria: Participants with recent antimalarial use were not excluded from the study; 13% of participants declared antimalarial use Clinical setting: Primary Health Centre Country: Madagascar (Ampasimpotsy, Central Highlands) Malaria endemicity: Transmission is low and predominantly seasonal. This study was carried out in the low season. Malaria endemic species:P. falciparum (approximately 75%) andP. vivax |
|
| Participants |
Sample size: 200 Age: Eligible age range not stated; actual age range of the included participants was 6 months to 73 years (40% under 5 years, 26.5% 5 to 15 years) Sex: Male:female ratio was 1.2:1 Co‐morbidities and pregnancy: Pregnant women were excluded, as were people with signs of severe or complicated malaria Parasite density of microscopy positive cases: Range 16 to 285,00 parasites per μl, mean 16,757, Standard Deviation 42,631 |
|
| Study design | Enrolment was prospective. The sampling method was not described. Two RDTs were evaluated, all participants received both RDTs. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: PCR |
|
| Index and comparator tests |
Commerical name of RDT: SD Bioline Malaria Ag Pf (Standard Diagnostics Inc., Suwon City, South Korea) (excluded as required data could not be extracted) SD Bioline Malaria Ag Pf/Pan (Standard Diagnostics Inc., Suwon City, South Korea) Parasite(s) designed to detect: SD Bioline Malaria Ag Pf ‐ P. falciparum SD Bioline Malaria Ag Pf/Pan ‐ P. falciparum or mixed infection, non‐falciparum species only Designated Type: SD Bioline Malaria Ag Pf ‐ Type 1 SD Bioline Malaria Ag Pf/Pan ‐ Type 3 Batch numbers: SD Bioline Malaria Ag Pf ‐ 05FK50 SD Bioline Malaria Ag Pf/Pan ‐ 05FK60 Transport and storage conditions: All tests were kept at room temperature and opened just before use to avoid humidity damage. Person(s) performing RDT: Not stated RDT setting: Not stated |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Kozone, representing Standard Diagnostics Inc in Madagascar | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | Participants were all attending a health centre with fever and typical symptoms of malaria, but the sampling method was not described, |
| Acceptable reference standard? All tests | Yes | The reference standard was PCR |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | PCR was carried out by technicians blind to the results of RDT testing |
| Index test results blinded? All tests | Yes | RDTs were undertaken before the results of PCR were known |
| Uninterpretable results reported? All tests | Yes | Uninterpretable results are reported and excluded from the analysis. There were 2 invalid results for Bioline Pf and 1 for Bioline Pf/Pan |
| Withdrawals explained? All tests | No | There was one participant missing from the analysis for Bioline Pf/Pan, with no explanation |
Sayang 2009.
| Clinical features and settings |
Presenting signs and symptoms: Fever or history of fever in the previous 24 h, and nurse's suspicion of malaria Previous treatment for malaria: Patients who reported taking antimalarial drugs in the previous two weeks were excluded Clinical setting: Primary health centre Country: Yoaunde, Cameroon Malaria endemicity: Reported to be high Malaria endemic species:P. falciparum |
|
| Participants |
Sample size: 153 Age: Both adults and children were included; there is no indication of the proportion of adults and children in the sample Sex: Not mentioned either as an exclusion criteria or a characteristic of included participants Co‐morbidities and pregnancy: Not mentioned either as an exclusion criteria or a characteristic of included participants Parasite density of microscopy positive cases: Range 40 to 125,000 parasites per μl. Geometric mean: age 0‐2 = 2869; age 3‐5 = 6440; age 6‐10 = 1580; age over 11 = 1535 |
|
| Study design | Enrollment was prospective. The sampling method was initially consecutive, from which a random sample of patients assigned to RDTs. One RDTs was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy Person(s) performing microscopy: Not stated Microscopy setting: Laboratory not further described Number of high power fields examined before declaring negative: Not stated Number of observer or repeats: Not stated Resolution of discrepancies between observers: Not applicable |
|
| Index and comparator tests |
Commerical name of RDT: Diaspot cassette device (Acumen Diagnostics Inc, USA) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: Nurses trained in the use of the device RDT setting: Primary Health Centre |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Supported by the Service de Cooperation et d'Action Culturelle of the French Embassy in Yaounde, European Union (READ‐UP project, STREP, contract no. 018602) and the Centre de Formation et Recherche en Medicine et Sante Tropicale, Marseille, France | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Participants were all attending health centre, had fever and a nurse suspected that they might have malaria. Enrolment into the main study was consecutive, and allocation to RDT study was random. |
| Acceptable reference standard? All tests | Unclear | No details given of number of high power fields viewed before declaring negative, or number of observers or repeats |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | Microscopy undertaken at a different site to RDTs |
| Index test results blinded? All tests | Yes | RDTs undertaken before microscopy, and at a different site |
| Uninterpretable results reported? All tests | Unclear | The number of participants originally enrolled in the study was not clearly stated, therefore it is unclear whether there were any exclusions due to invalid test results |
| Withdrawals explained? All tests | Unclear | The number of participants originally enrolled in the study was not clearly stated, therefore it is unclear whether there were any withdrawals |
Sharew 2009.
| Clinical features and settings |
Presenting signs and symptoms: Febrile patients, clinically suspected for malaria Previous treatment for malaria: No exclusions based on previous treatment. Information on previous treatment collected, but actual data not provided. Clinical setting: Outpatient departments of two health centres Country: Ethiopia (Southern ‐ Wondo Genet) Malaria endemicity: Takes place throughout the year Malaria endemic species:P. falciparum and P. vivax |
|
| Participants |
Sample size: 668 Age: All age groups eligible. Actual age range 6 months to 75 years. Sex: 361 (54%) males, 307 (46%) females Co‐morbidities and pregnancy: No exclusion criteria based on co‐morbidities or pregnancy. No details of the frequency of these conditions in the participant population is presented. Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was consecutive and prospective. Two different RDTs were evaluated, and each participant received both tests. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood films Person(s) performing microscopy: Experienced malaria technicians Microscopy setting: Not stated, but in the Wondo Genet area Number of high power fields examined before declaring negative: 100 Number of observer or repeats: Two independent technicians, also checked by the team leader Resolution of discrepancies between observers: All discordant results between microscopy and RDTs were repeated |
|
| Index and comparator tests |
Commerical name of RDT: Paracheck Pf (Orchid Biomedical Systems, Goa, India) CareStart Malaria Pf/Pv Combo test (Access Bio Inc., New Jersey, USA) Parasite(s) designed to detect:P. falciparum Paracheck Pf ‐ P. falciparum CareStart Malaria Pf/Pv Combo test ‐ P. falciparum, P. vivax or mixed infection Designated Type: Paracheck Pf ‐ Type 1 CareStart Malaria Pf/Pv Combo test ‐ Type 5 Batch numbers: Not stated Transport and storage conditions: As per the instructions of the manufacturer Person(s) performing RDT: Not stated RDT setting: Two health centres |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: School of Graduate Studies of the Addis Adaba University through the Graduate Programme in Tropical and Infectious Diseases, Aklilu Lemma Institute of Pathobiology and from the Federal Ministry of Health of Ethiopia. Federal Ministry of Health of Ethiopia and Access Bio Inc. donated the test kits. | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Participants were a consecutive sample of febrile patients attending health centres with suspected malaria |
| Acceptable reference standard? All tests | Yes | Two experienced microscopists independently viewed 100 high power fields before declaring a slide negative |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Unclear | Not described |
| Index test results blinded? All tests | Yes | Strict blinding with the results available before microscopy reported |
| Uninterpretable results reported? All tests | Yes | If a test was uninterpretable then it was repeated |
| Withdrawals explained? All tests | Yes | The number of participants enrolled in the study was clearly stated and corresponds to the number included in the analysis; therefore there were no withdrawals |
Sharma 1999.
| Clinical features and settings |
Presenting signs and symptoms: Clinical symptoms of malaria Previous treatment for malaria: No exclusions based on previous treatment. Information on previous treatment collected, but actual data not provided except in the case of false positive results. Clinical setting: Malaria Clinics Country: Orissa, India Malaria endemicity: Not stated Malaria endemic species: Mainly P. falciparum, some P. vivax |
|
| Participants |
Sample size: 125 Age: Not mentioned either as an inclusion criteria or characteristic of the included participants Sex: Not mentioned either as an inclusion criteria or characteristic of the included participants Co‐morbidities and pregnancy: No exclusion criteria based on co‐morbidities or pregnancy. No details of the frequency of these conditions in the participant population is presented. Parasite density of microscopy positive cases: Range 40 to 36,000 parasites per μl |
|
| Study design | Enrollment was prospective. Random sampling was used, but exact method used to obtain a random sample was not stated. One RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood films Person(s) performing microscopy: Not stated Microscopy setting: Not stated Number of high power fields examined before declaring negative: Not stated Number of observer or repeats: Results discordant between microscopy and RDT were re‐examined for confirmation of the results Resolution of discrepancies between observers: Not described |
|
| Index and comparator tests |
Commerical name of RDT: ICT Malaria Pf (ICT Diagnostics, Sydney, Australia) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: Various clinic staff RDT setting: Malaria clinics |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Not stated | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Participants were a random sample of people attending a clinic with clinical symptoms of malaria |
| Acceptable reference standard? All tests | Unclear | Discordant results between RDTs and microscopy were re‐examined; however it is unclear how many high power fields were viewed before declaring a slide negative |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | "Evaluation was double blind" |
| Index test results blinded? All tests | Yes | "Evaluation was double blind" |
| Uninterpretable results reported? All tests | Yes | There were five uninterpretable test results; these were excluded from the analysis |
| Withdrawals explained? All tests | Yes | The numbers enrolled in the study and the numbers with data presented for them correspond, with the exception of the five excluded from the analysis due to uninterpretable test results |
Singh 1997 (a).
| Clinical features and settings |
Presenting signs and symptoms: Fever Previous treatment for malaria: No exclusions based on previous treatment. Data was collected on previous treatment, but was only presented in the case of false positive results. Clinical setting: Field workers in villages Country: India (Maldla District, Central India) Malaria endemicity: Seasonal Malaria endemic species:P. falciparum andP. vivax, but during the seasons the study was undertaken, mainly P. falciparum |
|
| Participants |
Sample size: 353 Age: Not mentioned either as an inclusion criteria or characteristic of the included participants Sex: Not mentioned either as an inclusion criteria or characteristic of the included participants Co‐morbidities and pregnancy: Not mentioned either as an exclusion criteria or characteristic of the included participants Parasite density of microscopy positive cases: Range 60 to 7,000 parasites per μl |
|
| Study design | Enrollment was consecutive and prospective. One RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick blood films Person(s) performing microscopy: Microscopist at central research centre Microscopy setting: Blood films were prepared in villages and examined by at the Malaria Research Centre in Delhi Number of high power fields examined before declaring negative: Not stated; 250 WBCs were examined before classifying a slide as negative. All negative slides were re‐examined by counting up to 2500 WBCs. Number of observer or repeats: One, although intimally negative slides were re‐examined Resolution of discrepancies between observers: Not applicable |
|
| Index and comparator tests |
Commerical name of RDT: ICT Malaria Pf (ICT Diagnostics, Sydney, Australia) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: Field workers RDT setting: Villages (actual setting not well described) |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Not stated | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | It is unclear as to whether passive or active case‐finding was used, as field workers went into villages |
| Acceptable reference standard? All tests | No | Only one observer was used, and the number of high power fields viewed before declaring a slide negative was not stated |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | "without reference to the result of the ICT" |
| Index test results blinded? All tests | Yes | Index test results were available before the reference test results |
| Uninterpretable results reported? All tests | Unclear | The number of participants originally enrolled in the study was clearly stated and the number presented in the analysis corresponded; therefore there were no exclusions due to uninterpretable test results |
| Withdrawals explained? All tests | Yes | The number of participants originally enrolled in the study was clearly stated and the number presented in the analysis corresponded; therefore there were no withdrawals |
Singh 1997 (b).
| Clinical features and settings |
Presenting signs and symptoms: Fever Previous treatment for malaria: No exclusions based on previous treatment. No data presented on numbers who had previously been treated, although this information was recorded for each participant. Clinical setting: Malaria clinic established within a Primary Health Centre specifically for the study Country: India (Maldla District, Central India) Malaria endemicity: Seasonal Malaria endemic species:P. falciparum andP. vivax, but during the seasons the study was undertaken, mainly P. falciparum |
|
| Participants |
Sample size: 1231 Age: Not mentioned either as an inclusion criteria or characteristic of the included participants Sex: Not mentioned either as an inclusion criteria or characteristic of the included participants Co‐morbidities and pregnancy: Not mentioned either as exclusion criteria or as characteristics of the included participants Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was consecutive and was prospective. One RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick blood films Person(s) performing microscopy: Microscopist Microscopy setting: Not stated Number of high power fields examined before declaring negative: Not stated. 1000 white blood cells were initially counted before declaring negative, with a repeat looking at 4000 WBCs if initially negative Number of observer or repeats: Negative slides were checked by another observer. Resolution of discrepancies between observers: Not described. |
|
| Index and comparator tests |
Commerical name of RDT: ParaSight‐F (Beckton Dickinson, Franklin Lakes, NJ, US) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: Two independent technicians RDT setting: Malaria clinic |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: WHO Special Program for Research and Training in Tropical Diseases | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Participants were a consecutive sample of people attending a malaria clinic with fever |
| Acceptable reference standard? All tests | No | Only one observer was used for slides initially found positive. Unclear whether 100 high power fields viewed before declaring negative, although an alternative criteria of 4000 WBCs was used |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Unclear | Blinding not described |
| Index test results blinded? All tests | Unclear | Blinding not described |
| Uninterpretable results reported? All tests | Unclear | The number of participants originally enrolled in the study was clearly stated and the number presented in the analysis corresponded; therefore there were no exclusions due to uninterpretable test results |
| Withdrawals explained? All tests | Yes | The number of participants originally enrolled in the study was clearly stated and the number presented in the analysis corresponded; therefore there were no withdrawals |
Singh 2000 (a).
| Clinical features and settings |
Presenting signs and symptoms: Clinically suspected malaria, including fever Previous treatment for malaria: No exclusions based on previous treatment, and no data reported; however the study was undertaken in a remote area with little access to malaria treatment Clinical setting: Mobile field clinic and laboratory Country: India Malaria endemicity: epidemic‐prone forest villages in Madhya Pradesh, central India Malaria endemic species:P. falciparum (83.7% of positives) and P. vivax |
|
| Participants |
Sample size: 526 Age: All age groups eligible. Adults and children included, but actual age profile of participant population not presented. Sex: Both males and females eligible. Actual proportions of males and females in the participant population not stated. Co‐morbidities and pregnancy: No exclusion criteria based on co‐morbidities or pregnancy. No details of the frequency of these conditions in the participant population is presented. Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was consecutive and prospective. One RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood films Person(s) performing microscopy: Microscopists Microscopy setting: Mobile laboratory Number of high power fields examined before declaring negative: Not stated Number of observer or repeats: One, but negative blood smears were re‐examined if the corresponding RDT result was positive or if P. vivax was diagnosed Resolution of discrepancies between observers: Not applicable |
|
| Index and comparator tests |
Commerical name of RDT: Determine malaria P.f. (Abbott Laboratories, Tokyo, Japan) Parasite(s) designed to detect:P. falciparum Designated type: Type 1 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: Members of the field team of the malaria research centre undertook the test after receiving one hour of training. A technician interpreted all the test results. RDT setting: Mobile laboratory |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Not stated. DP Medical Diagnostics (Ahmedaba Gujarat) supplied the RDTs free of charge. | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Participants were a consecutive sample of people with clinically suspected malaria, presenting at an ambulatory clinic in an endemic area |
| Acceptable reference standard? All tests | No | Microscopy was undertaken by a single microscopist. There was no report of the number of high power fields viewed before declaring a slide negative. |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | Study report states that microscopists were blinded to the RDT results |
| Index test results blinded? All tests | Yes | All RDTs were undertaken and the results known before microscopy |
| Uninterpretable results reported? All tests | Unclear | The number of participants originally enrolled in the study was clearly stated and the number presented in the analysis corresponded; therefore there were no exclusions due to uninterpretable test results |
| Withdrawals explained? All tests | Yes | The number of participants originally enrolled in the study was clearly stated and the number presented in the analysis corresponded; therefore there were no withdrawals |
Singh 2000 (c).
| Clinical features and settings |
Presenting signs and symptoms: Fever suspected to be malaria Previous treatment for malaria: There were no exclusions based on previous treatment, and no information presented; this was an outbreak in a rural area Clinical setting: Mobile field laboratory Country: India (forest villages in Chhindwara, central India) Malaria endemicity: Outbreak situation Malaria endemic species:P. falciparum and P. vivax |
|
| Participants |
Sample size: 344 Age: All age groups eligible. Actual age range 6 months to 65 years. Sex: Both males and females eligible. Actual proportions of males and females in the participant population not stated. Co‐morbidities and pregnancy: No exclusion criteria based on co‐morbidities or pregnancy. No details of the frequency of these conditions in the participant population is presented. Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was consecutive and prospective. One RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick blood film Person(s) performing microscopy: Experienced microscopist for all slides; expert microscopist for re‐examined slides Microscopy setting: Mobile field laboratory for all slides; Malaria Research Centre at Jabalur for re‐examined slides Number of high power fields examined before declaring negative: Not stated. However, 200 WBCs were counted as an alternative indicator; or 500 WBCs for slides that were re‐examined. Number of observer or repeats: One, but negative blood smears were re‐examined if the patient was having severe symptoms, the corresponding RDT result was positive, or if P. vivax was diagnosed Resolution of discrepancies between observers: Not described, most likely accepted the findings of second microscopist |
|
| Index and comparator tests |
Commerical name of RDT: ICT Malaria Pf/Pv (AMRAD, Australia) Parasite(s) designed to detect:P. falciparum or mixed infection, non‐falciparum species only Designated type: Type 2 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: Field laboratory assistants RDT setting: Mobile field laboratory |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Becton Dickinson provided financial support and supplied the RDTs free of charge | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | All participants were attending an ambulatory setting with fever suspected to be malaria, and enrolment was consecutive |
| Acceptable reference standard? All tests | No | Microscopy was undertaken by one microscopist only; and the number of high power fields viewed was unclear (200 WBCs) |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | "Blood films were examined...without reference to the results of ICT" |
| Index test results blinded? All tests | Yes | "All specimens were tested...who were blinded to the results of the blood smear tests" |
| Uninterpretable results reported? All tests | Unclear | The number of participants originally enrolled in the study was clearly stated and the number presented in the analysis corresponded; therefore there were no exclusions due to uninterpretable test results |
| Withdrawals explained? All tests | Yes | The number of participants originally enrolled in the study was clearly stated and the number presented in the analysis corresponded; therefore there were no withdrawals |
Singh 2003a.
| Clinical features and settings |
Presenting signs and symptoms: Fever or history of fever Previous treatment for malaria: No explicit exclusions based on previous treatment, and no data reported Clinical setting: Hospital malaria clinic Country: India, Jabalpur Malaria endemicity: Not stated Malaria endemic species:P. falciparum and P. vivax in roughly equal proportions |
|
| Participants |
Sample size: 80 Age: All age groups eligible. Adults and children included; mean age 27.7 (SD 16.42) for males and 29 (SD 12.8) for females Sex: Both males and females eligible; included 28 males and 18 females Co‐morbidities and pregnancy: No explicit exclusion criteria based on co‐morbidities or pregnancy. No details of the frequency of these conditions in the participant population is presented. Parasite density of microscopy positive cases: Range 40 to 370,574 parasites per μl for P. falciparum and 318 to 9970 for P. vivax |
|
| Study design | Enrollment was prospective. The sampling method was not described. Only one RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick blood films Person(s) performing microscopy: Not stated Microscopy setting: Hospital laboratory Number of high power fields examined before declaring negative: Not stated Number of observer or repeats: If the results of the OptiMAL conflicted with that of microscopy for any sample, the blood smear was re‐examined by a different technician Resolution of discrepancies between observers: If the re‐examination of discordant results gave a different result to the first examination, the second result was confirmed by yet another technician |
|
| Index and comparator tests |
Commerical name of RDT: OptiMAL Parasite(s) designed to detect:P. falciparum or mixed infection, non‐falciparum species only Designated type: Type 4 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: A technician RDT setting: Hospital clinic or laboratory |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Not stated. | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | Participants were all attending a clinic with fever or history of fever, but the sampling method was not described |
| Acceptable reference standard? All tests | Unclear | Discordant results between RDT and microscopy were re‐examined; however the number of high power fields viewed before declaring a sample negative was not stated |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Unclear | Blinding not described |
| Index test results blinded? All tests | Yes | Technicans were blinded to the results of the blood smear examination |
| Uninterpretable results reported? All tests | Unclear | The number of participants originally enrolled in the study was clearly stated and the number presented in the analysis corresponded; therefore there were no exclusions due to uninterpretable test results |
| Withdrawals explained? All tests | Yes | The number of participants originally enrolled in the study was clearly stated and the number presented in the analysis corresponded; therefore there were no withdrawals |
Singh 2003b.
| Clinical features and settings |
Presenting signs and symptoms: Fever and chills of several days' duration Previous treatment for malaria: No explicit exclusions based on previous treatment, and no data reported Clinical setting: Field clinics Country: India, villages in the Jabalpur district Malaria endemicity: Not stated Malaria endemic species:P. falciparum and P. vivax in roughly equal proportions |
|
| Participants |
Sample size: 75 Age: All age groups eligible. Adults and children included; mean age 20.4 (SD 17.00) for males and 25.9 (SD 17.9) for females Sex: Both males and females eligible; included 25 males and 32 females Co‐morbidities and pregnancy: No explicit exclusion criteria based on co‐morbidities or pregnancy. No details of the frequency of these conditions in the participant population is presented. Parasite density of microscopy positive cases: Range 100 to 90,000 parasites per μl for P. falciparum, 835 to 4320 for P. vivax |
|
| Study design | Enrollment was prospective. The sampling method was not described. One RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick blood films Person(s) performing microscopy: Not stated Microscopy setting: Not stated Number of high power fields examined before declaring negative: Not stated Number of observer or repeats: If the results of the OptiMAL conflicted with that of microscopy for any sample, the blood smear was re‐examined by a different technician Resolution of discrepancies between observers: If the re‐examination of discordant results gave a different result to the first examination, the second result was confirmed by yet another technician |
|
| Index and comparator tests |
Commerical name of RDT: OptiMAL (DiaMed AG, Cressier, Switzerland) Parasite(s) designed to detect:P. falciparum or mixed infection, non‐falciparum species only Designated type: Type 4 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: Not stated RDT setting: Not stated |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Not stated. | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | All participants were attending a field clinic with fever and chills of several days' duration, but the sampling method was not described |
| Acceptable reference standard? All tests | Unclear | Discordant results between RDT and microscopy were re‐examined; however the number of high power fields viewed before declaring a sample negative was not stated |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Unclear | Blinding not described |
| Index test results blinded? All tests | Unclear | Blinding not described |
| Uninterpretable results reported? All tests | Unclear | The number of participants originally enrolled in the study was clearly stated and the number presented in the analysis corresponded; therefore there were no exclusions due to uninterpretable test results |
| Withdrawals explained? All tests | Yes | The number of participants originally enrolled in the study was clearly stated and the number presented in the analysis corresponded; therefore there were no withdrawals |
Stephens 1999.
| Clinical features and settings |
Presenting signs and symptoms: Unclear; participants were selected by triage from people presenting themselves at a hospital Previous treatment for malaria: No exclusions based on previous treatment; data presented on previous treatment only covers false positive cases Clinical setting: Hospital outpatient clinic Country: Thailand (North West ‐ Mae Hong Son) Malaria endemicity: Perennial with seasonal peaks Malaria endemic species:P. falciparum and P. vivax |
|
| Participants |
Sample size: 301 enrolled, 296 received RDT Age: All age groups eligible. Actual age range from less than one month to 81 years Sex: Male: female ratio 6:4 Co‐morbidities and pregnancy: No explicit exclusion criteria based on co‐morbidities or pregnancy. No details of the frequency of these conditions in the participant population is presented. Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was prospective. The sampling method was not described. One RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood films Person(s) performing microscopy: Microscopists Microscopy setting: Hospital laboratory Number of high power fields examined before declaring negative: Not stated Number of observer or repeats: Two; one viewed the thick film and another viewed the thin film. The two microscopists worked independently and their findings compared at the end of the study. Resolution of discrepancies between observers: Not described |
|
| Index and comparator tests |
Commerical name of RDT: ParaSight‐F (Becton Dickinson Tropical Disease Diagnostics, Sparks, MD, US) Parasite(s) designed to detect:P. falciparum Designated type: Type 1 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: Not stated RDT setting: Hospital clinic or laboratory |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Supported by Dr Surang Tanpridist, Director, Malaria Division, Ministry for Public Health, Nonthaburi, and Dr Somsak Prajakwongse, Director, Malaria Region 2, Chiang Mai, Thailand, and the DFID‐funded Malaria Work Programme of the Liverpool School of Tropical Medicine | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | The presenting symptoms and sampling methods were unclear |
| Acceptable reference standard? All tests | Unclear | No details of the number of high power fields viewed before declaring a slide negative, and no information on how the findings of the two microscopists were compared |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Unclear | Blinding not described |
| Index test results blinded? All tests | Unclear | Blinding not described |
| Uninterpretable results reported? All tests | Unclear | The number of participants originally enrolled in the study was clearly stated and the number presented in the analysis corresponded; therefore there were no exclusions due to uninterpretable test results |
| Withdrawals explained? All tests | Yes | Five of the participants originally enrolled did not received RDTs. With the exception of these five, the number of participants originally enrolled in the study was clearly stated and the number presented in the analysis corresponded. |
Stow 1999.
| Clinical features and settings |
Presenting signs and symptoms: Symptoms suggestive of malaria Previous treatment for malaria: Not mentioned Clinical setting: Hospital outpatient department Country: Kenya Malaria endemicity: Catchment area varied from holoendemic to seasonally endemic Malaria endemic species:P. falciparum |
|
| Participants |
Sample size: 164 Age: Not mentioned either as an inclusion criteria or characteristic of included participants Sex: Males and females included Co‐morbidities and pregnancy: Not reported, no mention of these conditions as inclusion or exclusion criteria Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was prospective. The sampling method was not described. One RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood films Person(s) performing microscopy: Expert microscopist Microscopy setting: Westmead Hospital, Sydney, Australia Number of high power fields examined before declaring negative: Not stated (examined for ten minutes) Number of observer or repeats: One Resolution of discrepancies between observers: Not applicable |
|
| Index and comparator tests |
Commerical name of RDT: ICT Malaria Pf (ICT Diagnostics, Sydney, Australia) Parasite(s) designed to detect:P. falciparum Designated type: Type 1 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: Not stated RDT setting: Hospital outpatient department |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Not stated. | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | All participants had symptoms suggestive of malaria, but the sampling method was not described |
| Acceptable reference standard? All tests | No | Only one microscopist was used, and the number of high power fields viewed before declaring negative was not specified (search time 10 minutes) |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | Report stated that microscopists were blind to the results of the ICT test |
| Index test results blinded? All tests | Yes | The RDT was always performed and recorded before microscopy |
| Uninterpretable results reported? All tests | Unclear | The number of participants originally enrolled in the study was clearly stated and the number presented in the analysis corresponded; therefore there were no exclusions due to uninterpretable test results |
| Withdrawals explained? All tests | Yes | The number of participants originally enrolled in the study was clearly stated and the number presented in the analysis corresponded; therefore there were no withdrawals |
Tagbo 2007.
| Clinical features and settings |
Presenting signs and symptoms: History of fever and body temperature 37.5 °C or higher Previous treatment for malaria: No exclusions based on previous antimalarial use, and no data presented on the numbers that previously used antimalarials Clinical setting: Outpatient department of all small private hospital for children Country: Nigeria Malaria endemicity: Holoendemic Malaria endemic species:P. falciparum |
|
| Participants |
Sample size: 89 Age: Children only, mean age 3.6 years, range 2 weeks to 14 years Sex: 50 males and 39 females Co‐morbidities and pregnancy: No exclusion criteria based on co‐morbidities or pregnancy; 83 of the 89 included participants had a clinical diagnosis of malaria, the remaining 6 had other infections diagnosed clinically. Of the 83 with diagnosed malaria, 29 had acute respiratory infection, 4 had gastroenteritis and 4 had otitis media. Parasite density of microscopy positive cases: Mean 9058 parasites per μl |
|
| Study design | Enrollment was consecutive and prospective. One RDT was tested. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood smears Person(s) performing microscopy: Certified medical laboratory scientists Microscopy setting: Nigeria Institute for Medical Research at Lagos Number of high power fields examined before declaring negative: at least 100 Number of observer or repeats: One Resolution of discrepancies between observers: Not applicable |
|
| Index and comparator tests |
Commerical name of RDT: Paracheck Pf (Orchid Biomedical Systems, Goa, India) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: 32037E Transport and storage conditions: Stored at room temperatures within the range of 4 °C and 30 °C recommended by the manufacturers Person(s) performing RDT: The study authors RDT setting: Outpatient clinic |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Not stated | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Participants were a consecutive sample of children with fever attending an outpatients clinic |
| Acceptable reference standard? All tests | No | Certified microscopists viewed at least 100 high power fields before declaring a slide negative, however their results were not verified by a second independent reader |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | Reports that the laboratory was blinded to the results of the RDT |
| Index test results blinded? All tests | Yes | RDT was undertaken before the microscopy reference standard |
| Uninterpretable results reported? All tests | Unclear | The number of participants originally enrolled in the study was clearly stated and the number presented in the analysis corresponded; therefore there were no exclusions due to uninterpretable test results |
| Withdrawals explained? All tests | Yes | The number of participants originally enrolled in the study was clearly stated and the number presented in the analysis corresponded; therefore there were no withdrawals |
Tjitra 1999.
| Clinical features and settings |
Presenting signs and symptoms: Symptomatic with a presumptive clinical diagnosis of malaria: fever or history of fever in the last 24 h and no other obvious cause of fever Previous treatment for malaria: Prior use of antimalarials was not an exclusion criteria. Approximately half of the participants reported use of antimalarials within the previous 4 weeks. Clinical setting: Primary health centre Country: Indonesia (Laratama sub district, West Sumba, East Nusa Tenggara Province, Eastern Indonesia) Malaria endemicity: Infection rate in children 0 to 9 years of 5.1% Malaria endemic species:P. falciparum and P. vivax |
|
| Participants |
Sample size: 560 Age: All ages eligible. Actual age range of the participants 0 to 80 years. Sex: Males and females eligible; 289 males and 271 females included Co‐morbidities: Not mentioned either as an exclusion criteria or a characteristic of the included participants Parasite density of microscopy positive cases:P. vivax mean 7157 parasites per μl |
|
| Study design | Enrollment was prospective. The sampling method was not described. One RDT was tested. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood smears Person(s) performing microscopy: Expert microscopists with over 20 years experience each Microscopy setting: One local (exact setting not stated); cross‐checking was done in Darwin, Australia Number of high power fields examined before declaring negative: At least 100 for all slides, at least 200 for those cross‐checked Number of observer or repeats: One observer for the majority of slides; discordant results between microscopy and RDT and 20% of slides with concordant results were cross‐checked by a second microscopist, blind to the results of first microscopy and RDT Resolution of discrepancies between observers: Not described |
|
| Index and comparator tests |
Commerical name of RDT: ICT Malaria Pf/Pv Parasite(s) designed to detect:P. falciparum or mixed infection, non‐falciparum species only Designated Type: Type 2 Batch numbers: 100088 for the first 393 tests, and 041388 for the remaining 167 tests Transport and storage conditions: Not described Person(s) performing RDT: Performed by trained health workers and read by a study physician blinded to the microscopy results RDT setting: Primary health centre |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Financial assistance received from the Northern Territory Government 50th Anniversary of Indonesian Independence Malaria‐Tuberculosis Research Fellowships. ICT Pf/Pv kits and some logistical costs were supported by AMRAD‐ICT Sydney, New South Wales, Australia. | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | Participants were all attending a primary health care centre with fever and symptoms of malaria, but the sampling method was not described |
| Acceptable reference standard? All tests | Yes | All slides were read by an experienced microscopist viewing at least 100 high power fields, and results discordant with RDT were re‐examined by another, independent microscopist |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | "The microscopist was unaware of the immunochromatographic test result" |
| Index test results blinded? All tests | Yes | "The results were read by a study physician who was blinded to the microscopy results" |
| Uninterpretable results reported? All tests | Unclear | The number of participants enrolled in the study was clearly stated and corresponded to the number presented in the analysis; therefore there were no exclusions due to uninterpretable test results |
| Withdrawals explained? All tests | Yes | The number of participants enrolled in the study was clearly stated and corresponded to the number included in the analysis; therefore there were no withdrawals |
Valecha 2003.
| Clinical features and settings |
Presenting signs and symptoms: Fever or history of fever Previous treatment for malaria: Not mentioned, either as an exclusion criteria or a characteristic of included participants Clinical setting: Malaria clinics and village health workers Country: India (Delhi, Nadiad, Jabalpur and Sonapur) Malaria endemicity: Four sites of different endemicities Malaria endemic species:P. falciparum and P. vivax |
|
| Participants |
Sample size: 699 Age: All ages eligible; age range of included participants 1 to 75 years (mean 22.8) Sex: Included 395 males and 304 females Co‐morbidities: Not mentioned, either as an exclusion criteria or a characteristic of included participants Parasite density of microscopy positive cases:P. vivax range 40 to 44,000 parasites per μl, median 1020; P. falciparum range 120 to 68,480 parasites per μl, median 2000 |
|
| Study design | Enrollment was prospective. The sampling method was not described. One RDT was tested. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy Person(s) performing microscopy: Microscopist Microscopy setting: Not stated Number of high power fields examined before declaring negative: 100 Number of observer or repeats: One for most slides. All results discordant with RDT results and 20% of concordant results were cross‐checked. Negative slides which tested positive by kit were re‐examined by counting up to 2000 WBCs. Resolution of discrepancies between observers: In the case of initially negative slides looked at in more detail because of discordant results, the second reading was taken as true |
|
| Index and comparator tests |
Commerical name of RDT: OptiMAL (DiaMed AG, Cressier, Switzerland) Parasite(s) designed to detect:P. falciparum or mixed infection, non‐falciparum species only Designated Type: Type 4 Batch numbers: 46050.24.05 Transport and storage conditions: Stored below 30 °C Person(s) performing RDT: Not stated RDT setting: At the study sites (clinic and villages) |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Not stated | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | All participants were all attending clinics or approaching village health workers with fever or history of fever, but the sampling method was not described |
| Acceptable reference standard? All tests | Unclear | Microscopists viewed 100 high power fields before declaring a slide negative, and results discordant with RDTs were cross‐checked. However, it is not clear whether the person doing the cross‐checking was a different microscopist working independently |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | "Microscopists were blinded to the rapid test results" |
| Index test results blinded? All tests | Yes | The RDT was done before the microscopy |
| Uninterpretable results reported? All tests | Unclear | The number of participants originally enrolled in the study was not explicitly stated; therefore it is unclear whether there were any exclusions due to uninterpretable test results |
| Withdrawals explained? All tests | Unclear | The number of participants originally enrolled in the study was not explicitly stated; therefore it is unclear whether there were any withdrawals |
Van den Broek 2006.
| Clinical features and settings |
Presenting signs and symptoms: New episode of suspected malaria, which could include fever, history or other complaints indicating possible malaria infection Previous treatment for malaria: Excluded if malaria confirmed (treated or untreated) within the previous four weeks Clinical setting: Malaria outpatient centre Country: Colombia Malaria endemicity: Hypoendemic, annual parasite rate 2% to 5% Malaria endemic species:P. vivax (54%), P. falciparum (46%) |
|
| Participants |
Sample size: 896 Age: All ages eligible. Actual numbers of children and adults not stated, although the report mentions that many workers were included. Sex: Both males and females eligible. Most of the participants were male (646, 79%) Co‐morbidities and pregnancy: No exclusion criteria based on co‐morbidities. No details of the frequency of these conditions in the participant population is presented. Parasite density of microscopy positive cases: Geometric mean approximately 2300 parasites per μl for both P. falciparum and P. vivax |
|
| Study design | Enrollment was prospective. The sampling method was not described. Three RDTs were tested. All individuals received all three tests. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood smears Person(s) performing microscopy: Well trained, experienced microscopists Microscopy setting: Not stated Number of high power fields examined before declaring negative: At least 200 Number of observer or repeats: One, except for about one third of the slides (especially low density parasitaemias and mixed infections). In this case, another microscopist viewed the slide and discordant results between microscopists or between slides and RDTs were sent to the University of Antioquia for external cross‐checking. Resolution of discrepancies between observers: Disagreements between the internal and external results were sent to a third laboratory: the National Health Institute in Bogota. In cases where both external laboratories disagreed with the internal laboratory, results were corrected accordingly. |
|
| Index and comparator tests |
Commerical name of RDT: Paracheck Pf (Orchid Biomedical Systems, Goa, India) OptiMAL‐IT (Diamed AG, Switzerland) NOW Malaria ICT (Binax, Portland, USA) Parasite(s) designed to detect: Paracheck Pf ‐ P. falciparum OptiMAL‐IT ‐ P. falciparum or mixed infection, non‐falciparum species only NOW Malaria ICT ‐ P. falciparum or mixed infection, non‐falciparum species only Designated Type: Paracheck Pf ‐ Type 1 OptiMAL ‐ IT ‐ Type 4 Now Malaria ICT ‐ Type 2 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: A bacteriologist. Where the result was ambiguous, two bacteriologists read the test results. RDT setting: At the malaria centre |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Medicins Sans Frontieres and its donors. The American Society of Tropical Medicine and Hygiene assisted with publication expenses. | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | All participants were patients presenting with suspected malaria, but the sampling method was not described |
| Acceptable reference standard? All tests | No | Microscopists viewed at least 200 high power fields before declaring a slide negative; however the findings were only verified by a second independent reader for a third of slides |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | Report states that microscopists were blinded to the results of RDTs |
| Index test results blinded? All tests | Yes | Report states that RDTs were blinded to the results of microscopy |
| Uninterpretable results reported? All tests | Yes | There were no uninterpretable results; and weak lines were scored as positive |
| Withdrawals explained? All tests | Unclear | The number of participants originally enrolled in the study was not explicitly stated; therefore it was not possible to assess whether there were any withdrawals |
Verle 1996.
| Clinical features and settings |
Presenting signs and symptoms: Fever or history of fever in previous days Previous treatment for malaria: No exclusion criteria based on prior antimalarial drug use. Data collected and reported only for participants who were found to be false positive or true negative (5 out of 6 false positives, 11 out of 65 true negatives) Clinical setting: Community health centre. Villagers who felt ill during a malaria epidemic were invited to attend. Country: Vietnam (Ha Giang Province Northern Vietnam) Malaria endemicity: Mostly hypoendemic, but there is contact with focal areas endemic for malaria, and the study was undertaken during an epidemic Malaria endemic species:P. vivax and P. falciparum |
|
| Participants |
Sample size: 93 Age: All ages eligible. Actual numbers of children and adults not stated. Sex: Both males and females eligible. Actual numbers of males and females not stated. Co‐morbidities and pregnancy: No exclusion criteria based on co‐morbidities. No details of the frequency of these conditions in the participant population is presented. Parasite density of microscopy positive cases:P. falciparum geometric mean 6457 parasites per μl, range 2240 to 33,160 |
|
| Study design | Enrollment was consecutive and prospective. One RDT was tested. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick blood smears Person(s) performing microscopy: An experienced technician Microscopy setting: Not stated Number of high power fields examined before declaring negative: 100 Number of observer or repeats: One Resolution of discrepancies between observers: Not applicable |
|
| Index and comparator tests |
Commerical name of RDT: ParaSight‐F (Beckton Dickinson, Franklin Lakes, NJ, SA) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Not described Person(s) performing RDT: Not stated RDT setting: Community health centre |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Belgian Agency for Development Co‐operation and the Compagnie Maritime Belge | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Participants were a consecutive series of patients attending a health centre with fever during a malaria epidemic |
| Acceptable reference standard? All tests | No | The microscopist was experienced and viewed at least 100 high power fields, however their findings were not verified by a second independent reader |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | Report states that microscopy was undertaken by a technician unaware of the results of the RDT |
| Index test results blinded? All tests | Yes | The RDT was undertaken straight away at the health centre, before microscopy results became available |
| Uninterpretable results reported? All tests | Unclear | The number of participants originally enrolled in the study was not explicitly stated; therefore it was not possible to assess whether there were any exclusions due to uninterpretable test results |
| Withdrawals explained? All tests | Unclear | The number of participants originally enrolled in the study was not explicitly stated; therefore it was not possible to assess whether there were any withdrawals |
Willcox 2009a.
| Clinical features and settings |
Presenting signs and symptoms: Symptoms of uncomplicated malaria, primarily fever Previous treatment for malaria: No exclusion criteria based on previous antimalarial use, and no data presented on the numbers that previously used antimalarials Clinical setting: Village healthworker Country: Mali Malaria endemicity: Mesoendemic Malaria endemic species: Mainly P. falciparum |
|
| Participants |
Sample size: 158 under the age of five years (301 total) Age: All ages eligible for the study. Refers only to the analysis including children under the age of five years. Sex: Both males and females eligible. Co‐morbidities and pregnancy: No exclusions criteria based on co‐morbidities. No details of the frequency of these conditions in the participant population are presented. Parasite density of microscopy positive cases: Geometric mean 2323 parasites per μl, 95% CI 1492 to 3616 |
|
| Study design | Enrollment was consecutive and prospective. One RDT was tested. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood smears Person(s) performing microscopy: Experienced microscopists Microscopy setting: Field laboratory Number of high power fields examined before declaring negative: 100 Number of observer or repeats: Two independent microscopists Resolution of discrepancies between observers: Cross checked until both microscopists agreed. |
|
| Index and comparator tests |
Commerical name of RDT: Paracheck Pf (Orchid Biomedical Systems, Goa, India) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Stored at room temperatures of up to 40 °C. Person(s) performing RDT: A clinician and a laboratory technician from the research team RDT setting: Field laboratory |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Swiss Agency for Development and Co‐operation. Orchid Biomedical Systems supplied the Paracheck Pf tests free of charge. | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Participants were a consecutive series of patients presenting with suspected malaria |
| Acceptable reference standard? All tests | Yes | Two independent experienced microscopists viewed 100 high power fields before declaring a slide negative |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | Reported that microscopists were blinded to the results of the RDTs |
| Index test results blinded? All tests | Yes | Dipsticks were labelled with random numbers so that the people recording the results did not know which people the tests belonged to |
| Uninterpretable results reported? All tests | Yes | There were no uninterpretable test results (the control line was positive in all cases) |
| Withdrawals explained? All tests | Yes | The number of participants enrolled was explicitly stated and corresponded to the number presented in the analysis; therefore there were no withdrawals |
Willcox 2009b.
| Clinical features and settings |
Presenting signs and symptoms: Symptoms of uncomplicated malaria, primarily fever Previous treatment for malaria: No exclusion criteria based on previous antimalarial use, and no data presented on the numbers that previously used antimalarials Clinical setting: Village health worker Country: Mali Malaria endemicity: Mesoendemic Malaria endemic species: mainly P. falciparum |
|
| Participants |
Sample size: 143 aged five or over (301 total) Age: All ages included in the study. Refers only to the analysis of participants over the age of five years. Sex: Both males and females eligible. Co‐morbidities and pregnancy: No exclusion criteria based on co‐morbidities. No details of the frequency of these conditions in the participant population is presented. Parasite density of microscopy positive cases: Geometric mean 267 parasites per μl, 95% CI 172 to 413 |
|
| Study design | Enrollment was consecutive and prospective. One RDT was tested. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood smears Person(s) performing microscopy: Experienced microscopists Microscopy setting: Field laboratory Number of high power fields examined before declaring negative: 100 Number of observer or repeats: Two independent microscopists Resolution of discrepancies between observers: Cross checked until both microscopists agreed. |
|
| Index and comparator tests |
Commerical name of RDT: Paracheck Pf (Orchid Biomedical Systems, Goa, India) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Stored at room temperatures of up to 40°C Person(s) performing RDT: A clinician and a laboratory technician from the research team RDT setting: Field laboratory |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Swiss Agency for Development and Co‐operation. Orchid Biomedical Systems supplied the Paracheck Pf tests free of charge. | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Participants were a consecutive series of patients presenting with suspected malaria |
| Acceptable reference standard? All tests | Yes | Two experienced microscopists viewed 100 high power fields before declaring a slide negative |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | Reported that microscopists were blinded to the results of the RDTs |
| Index test results blinded? All tests | Yes | Dipsticks were labelled with random numbers so that the people recording the results did not know which people the tests belonged to |
| Uninterpretable results reported? All tests | Yes | There were no uninterpretable test results (the control line was positive in all cases) |
| Withdrawals explained? All tests | Yes | The number of participants enrolled was explicitly stated and corresponded to the number presented in the analysis; therefore there were no withdrawals |
Wolday 2001.
| Clinical features and settings |
Presenting signs and symptoms: Self‐referred to a malaria clinic Previous treatment for malaria: No exclusions based on previous antimalarial use; data recorded on previously used antimalarials, but not presented for the sample Clinical setting: Malaria clinic Country: Ethiopia (Debre Zeit, Addis Ababa) Malaria endemicity: Parasite prevalence approximately 40% Malaria endemic species:P. falciparum andP. vivax. The study was undertaken in the season when P. vivax predominated. |
|
| Participants |
Sample size: 306 Age: All ages included in the study. Range 1 to 70 years, mean age 15.2 years Sex: 112 (36.6%) females Co‐morbidities and pregnancy: No exclusion criteria based on co‐morbidities. No details of the frequency of these conditions in the participant population is presented. Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was consecutive and prospective. One RDT was tested. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood smears Person(s) performing microscopy: Experienced technicians and parasitologists Microscopy setting: Malaria laboratory Number of high power fields examined before declaring negative: 300 Number of observer or repeats: Two technicians confirmed by two parasitologists Resolution of discrepancies between observers: Not stated |
|
| Index and comparator tests |
Commerical name of RDT: Rapid test malaria (Quorum Diagnostics Inc., Vancouver, BC, Canada) Parasite(s) designed to detect:P. falciparum Designated Type: Type 1 Batch numbers: Not stated Transport and storage conditions: Not stated Person(s) performing RDT: Person doing the test not stated. Dipstick readings were done by three independent observers RDT setting: Field laboratory |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: "We thank Quorum Diagnostics Inc (Vancouver, BC, Canada) for the support of this project" | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Participants were a consecutive series of patients who had self‐referred to a malaria clinic |
| Acceptable reference standard? All tests | Yes | Two independent, experienced microscopists viewed at least 300 high power fields before declaring a slide negative |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | The blood smears were read before the RDTs |
| Index test results blinded? All tests | Yes | Report states that blinding was undertaken |
| Uninterpretable results reported? All tests | Unclear | The number of participants originally enrolled was not explicitly stated; therefore it was not possible to assess whether there were any exclusions due to uninterpretable test results |
| Withdrawals explained? All tests | Unclear | The number of participants originally enrolled was not explicitly stated; therefore it was not possible to assess whether there were any withdrawals |
Wongsrichanalai 1999.
| Clinical features and settings |
Presenting signs and symptoms: Symptomatic patients self‐referring for initial malaria diagnosis Previous treatment for malaria: Participants were excluded if they were known to have taken antimalarial drugs within the last 15 days Clinical setting: District malaria clinic and hospital outpatients Country: Thailand, on the international borders Malaria endemicity: Hypoendemic, with seasonal variation Malaria endemic species:P. falciparum 50% to 60%,P. vivax 40% to 50% |
|
| Participants |
Sample size: 309 Age: All age groups eligible. Mean age 29 years. Sex: Both males and females eligible. 245 males and 64 females included. Co‐morbidities and pregnancy: No stated exclusion criteria based on co‐morbidities or pregnancy. No details of the frequency of these conditions in the participant population is presented. Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was consecutive and prospective. Only one RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood films Person(s) performing microscopy: Experienced microscopists Microscopy setting: Armed Forces Research Institute of Medical Sciences Number of high power fields examined before declaring negative: 200 Number of observer or repeats: Two independent microscopists Resolution of discrepancies between observers: By a third microscopist, who had the final say |
|
| Index and comparator tests |
Commerical name of RDT: ICT test (AMARD/ ICT, Sydney, Australia) Parasite(s) designed to detect:P. falciparum Designated type: Type 1 Batch numbers: Not stated Trasport and storage conditions: Not described Person(s) performing RDT: Laboratory staff RDT setting: The study sites |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Half of the RDTs were supplied free of charge by the manufacturer. No other source of funding described. | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Participants were a consecutive series of symptomatic new patients self‐referring for diagnosis of malaria in an endemic area |
| Acceptable reference standard? All tests | Yes | Two independent experienced microscopists examined at least 200 high power fields before declaring a slide negative. Discordant results were resolved by a third microscopist in a double‐blind manner. |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | RDTs and microscopy were undertaken at different locations |
| Index test results blinded? All tests | Yes | RDTs and microscopy were undertaken at different locations |
| Uninterpretable results reported? All tests | Yes | One RDT failed due to operator error. 100 RDT results were re‐read blindly with 100% concordance. |
| Withdrawals explained? All tests | Yes | The number of participants originally enrolled was explicitly stated and corresponded with the number included in the analysis; therefore there were no withdrawals |
Wongsrichanalai 2003.
| Clinical features and settings |
Presenting signs and symptoms: Oral temperature over 38 °C, headache or a history of fever in the previous 72 h Previous treatment for malaria: No exclusions based on previous episodes or treatment for malaria; no data presented on recent antimalarial use in the children Clinical setting: Malaria clinics Country: Thailand (Maesod) Malaria endemicity: Not stated Malaria endemic species:P. falciparum andP. vivax. |
|
| Participants |
Sample size: 246 Age: Inclusion criteria stipulated over 20 years old Sex: Both males and females were eligible Co‐morbidities and pregnancy: Not mentioned, either as an exclusion criteria or characteristic of the included participants Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was prospective. The sampling method was not described. One RDT was tested. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy thick and thin blood smears Person(s) performing microscopy: Experienced microscopists Microscopy setting: Armed Forces Research Institute of Medical Sciences Number of high power fields examined before declaring negative: 200 Number of observer or repeats: Two independent observers, blinded to each others findings Resolution of discrepancies between observers: Resolved by a third expert microscopist, whose reading was accepted as final. Where there was species discrepancy between microscopy and NOW ICT, PCR was conducted. |
|
| Index and comparator tests |
Commerical name of RDT: NOW ICT Malaria Pf/Pv Parasite(s) designed to detect:P. falciparum or mixed infection, non‐falciparum species only Designated Type: Type 2 Batch numbers: 030611 Transport and storage conditions: Not described Person(s) performing RDT: Technician RDT setting: Armed Forces Research Institute of Medical Sciences |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: US Army Medical Material Development Activity | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | All participants were attending malaria clinics with temperature over 38 °C, headache or a history of fever in the previous 72 h, but the sampling method was not adequately described |
| Acceptable reference standard? All tests | Yes | Two independent microscopists at a research laboratory viewed at least 200 high power fields before declaring a slide negative |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Yes | "read by two microscopists blinded to.. the NOW ICT results" |
| Index test results blinded? All tests | Yes | The RDT was carried out before microscopy |
| Uninterpretable results reported? All tests | Yes | The RDTs had to be repeated in 39 of 285 assays. A successful test was eventually completed for each sample. |
| Withdrawals explained? All tests | Yes | The number of participants enrolled in the study was clearly stated and corresponded with the number included in the analysis, indicating no withdrawals |
Yadav 1997.
| Clinical features and settings |
Presenting signs and symptoms: Participants who attended at malaria clinic or who were selected from the villages based on clinical condition Previous treatment for malaria: No explicit exclusion criteria based on antimalarial use, and no relevant data presented for included participants Clinical setting: Malaria clinic and in the field Country: Gujarat, India Malaria endemicity: Not stated Malaria endemic species:P. falciparum and P. vivax |
|
| Participants |
Sample size: 148 Age: All age groups eligible. Sample included 79 children and 69 adults. Sex: 73 males and 75 females included Co‐morbidities and pregnancy: No stated exclusion criteria based on co‐morbidities or pregnancy. No details of the frequency of these conditions in the participant population is presented. Parasite density of microscopy positive cases: Not presented |
|
| Study design | Enrollment was prospective. The selection and sampling methods were not described. One RDT was evaluated. | |
| Target condition and reference standard(s) |
Target condition: Malaria parasitaemia Reference standard: Microscopy Person(s) performing microscopy: Microscopists Microscopy setting: Not stated Number of high power fields examined before declaring negative: Not stated. The microscopist counted 300 WBCs before declaring a slide negative. A negative slide that tested positive by RDT was re‐examined, counting up to 2000 WBCs. Number of observer or repeats: A negative slide that tested positive by RDT was re‐examined, counting up to 2000 WBCs. A positive slide that tested negative by RDT was re‐examined and confirmed by another person by staining the duplicate film. Resolution of discrepancies between observers: Not described |
|
| Index and comparator tests |
Commerical name of RDT: ICT test (AMARD/ ICT, Sydney, Australia) Parasite(s) designed to detect:P. falciparum Designated type: Type 1 Batch numbers: Not stated Trasport and storage conditions: Test kits were carried into the field under cold conditions in the containers that are commonly used for carrying vaccines. Person(s) performing RDT: Not states RDT setting: Malaria clinic and in the field in villages |
|
| Follow‐up | Not applicable | |
| Notes | Source of funding: Not stated | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Unclear | The selection criteria and sampling methods were not described; however all participants had either identified symptoms of malaria or were attending a malaria clinic |
| Acceptable reference standard? All tests | No | Microscopists did not explicitly view 100 high power fields before declaring a slide negative. However, they had an alternative criteria of 300 WBCs. Re‐examination by a second microscopist was done for results discordant for RDT and microscopy. |
| Partial verification avoided? All tests | Yes | All participants who received the index test also received the reference test |
| Differential verification avoided? All tests | Yes | The same reference test was used regardless of the index test results |
| Incorporation avoided? All tests | Yes | The index test does not form part of the reference standard |
| Reference standard results blinded? All tests | Unclear | Blinding not described |
| Index test results blinded? All tests | Yes | The ICT test was performed "blind" |
| Uninterpretable results reported? All tests | Unclear | The number of participants originally included in the analysis was not explicitly stated; therefore it was not possible to assess whether any participants may have been excluded from the analysis due to uninterpretable test results |
| Withdrawals explained? All tests | Unclear | The number of participants originally included in the analysis was not explicitly stated; therefore it was not possible to assess whether there were any withdrawals |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| A‐Elgayoum 2009 (b) | Not a study of rapid diagnostic tests (compared usual with expert microscopy) |
| Abul 2000 | Participants had cerebral malaria |
| Afzaal 2001 | Review or narrative |
| Ahmad 2003 | Eligibility unclear due to lack of published information |
| Anonymous 2005 | Review or narrative |
| Ansah 2008 | Eligibility unclear due to lack of published information |
| Araz 2000 | Some participants did not have symptoms of malaria |
| Arcanjo 2007 | European foreign language study |
| Arora 2003 | Participants have severe or complicated malaria |
| Arrospide 2004 | European foreign language study |
| Arrospide 2004 (a) | Majority of participants have no symptoms of malaria |
| Arrospide 2006 | European foreign language study |
| Ashley 2009 | Not able to extract or calculate absolute numbers of true positives, false positives, false negatives and true negatives |
| Aslan 2001 | Participants were hospital inpatients |
| Assal 1999 | Not rapid immunochromatographic tests |
| Avila 2002 | Participants were travellers returning from an endemic to a non‐endemic region |
| Azazy 2004 | Only participants with malaria positive blood films by microscopy received the RDT |
| Babacar 2008 | Not a diagnostic test accuracy study |
| Bartoloni 1998 | Single case study |
| Bassene 2009 | Not a diagnostic test accuracy study |
| Bassett 1991 | Not a diagnostic test accuracy study |
| Beadle 1994 | Majority of participants did not have symptoms of malaria |
| Beg 2005 | All participants were positive for malaria by microscopy |
| Belizario 2005 | Participants were recruited by active case finding |
| Bell 2005 | Not a consecutive sample: excluded a random sample of participants who were negative for malaria by microscopy |
| Bell 2006 | Review or narrative |
| Bellagra 1998 | Participants are travellers returning from an endemic to a non‐endemic area |
| Bendezu 2008 | Not able to extract or calculate absolute numbers of true positives, false positives, false negatives and true negatives |
| Berens‐Riha 2009 | Participants were dead |
| Bhandari 2008 | All participants were positive for malaria by microscopy |
| Bhatt 1994 | Review or narrative |
| Birku 1999 | Participants had severe or complicated malaria |
| Bisoffi 2009 | Not a diagnostic test accuracy study |
| Bisoffi 2009a | Review or narrative |
| Biswas 2004 | Not a diagnostic test accuracy study |
| Biswas 2006 | Not an immunochromatographic test |
| Bouchaud 2000 | Participants were travellers returning from endemic to non‐endemic areas |
| Brenier‐Pinchart 2000 | Participants were travellers returning from endemic to non‐endemic areas |
| Bruxvoort 2008 | Participants were recruited by active case finding |
| Bualombai 2003 | No usable data for P. falciparum malaria |
| Bualombai 2006 | Eligibility unclear due to lack of published information |
| Buchachart 2004 | Participants are hospital in‐patients |
| Bujanover 2002 | Not a diagnostic test accuracy study |
| Cabezas 2004 | Not a diagnostic test accuracy study (compares 'field' and laboratory RDT results) |
| Cavallo 1997 | Participants are travellers returning from an endemic to a non‐endemic area |
| Chatterjee 2008 | Eligibility unclear due to lack of published information |
| Cheng 2006 | Review or narrative |
| Chilton 2006 | Not a diagnostic test accuracy study |
| Chiodini 1998 | Review or narrative |
| Chiodini 2005 | Not a diagnostic test accuracy study |
| Cho 2001 | Not undertaken in a malaria endemic area |
| Coleman 2002a | Majority of participants did not have symptoms of malaria |
| Coleman 2002b | Majority of participants did not have symptoms of malaria |
| Cong Le 2002 | Article written in Russian only |
| Craig 1997 | Tested blood films with artificially cultured and diluted malaria parasites |
| Craig 2002 | The participants were positive for malaria by microscopy |
| Cropley 2000 | Participants were travellers returning from endemic to non‐endemic areas |
| Cuadros 2007 | Participants were travellers returning from endemic to non‐endemic areas |
| De Carsalade 2009 | European foreign language study |
| De Dominguez 1996 | Not a diagnostic test accuracy study |
| De Monbrison 2004 | Participants were travellers returning from endemic to non‐endemic areas |
| Delaunay 2008 | Review or narrative |
| Deletoille 1987 | Participants are travellers returning from an endemic to a non‐endemic area |
| Di Perry 1997 | All participants were positive for malaria by microscopy |
| Dietze 1995 | Some participants did not have symptoms of malaria |
| Drakeley 2009 | Review or narrative |
| Dubarry 1990 | Not evaluating an immunochromatographic rapid diagnostic test |
| Durand 2005 | Participants were travellers returning from endemic to non‐endemic areas |
| Durand 2005a | Review or narrative |
| Dyer 2000 | All participants were positive for malaria by microscopy |
| Eisen 2000 | Not undertaken in a malaria endemic area |
| El‐Moamly 2007 | Participants were travellers returning from a malaria endemic to a non‐endemic area |
| Elmardi 2009 | Not a diagnostic test accuracy study |
| Endeshaw 2008 | Majority of participants did not have symptoms of malaria |
| Fan 2000 | Written in Chinese only |
| Farcas 2003 | Participants were travellers returning from endemic to non‐endemic areas |
| Farcas 2004 | Not an immunochromatographic test |
| Ferro 2002 | Participants were travellers returning from an endemic area to a non‐endemic area |
| Figueiredo 2003 | All participants were positive for malaria by microscopy |
| Fogg 2008 | No usable data for P. falciparum malaria |
| Fryauff 1997 | Eligibility unclear due to lack of published information |
| Fryauff 2000 | Participants did not have symptoms of malaria |
| Funk 1999 | Participants were travellers returning from endemic to non‐endemic areas |
| Garavelli 2002 | Participants were travellers returning from endemic to non‐endemic areas |
| Garcia 1996 | Eligibility unclear due to lack of published information |
| Gatti 2002 | Participants were travellers returning from endemic to non‐endemic areas |
| Gatti 2007 | Participants were travellers returning from endemic to non‐endemic areas |
| Ghanchi 2009 | Not a diagnostic test accuracy study |
| Gillet 2009 (a) | Participants were travellers returning from endemic to non‐endemic areas |
| Gillet 2009 (b) | Not a diagnostic test accuracy study |
| Gillet 2009 (c) | Participants were travellers returning from an endemic to a non‐endemic area |
| Gogtay 1999 | Participants had severe or complicated malaria |
| Gogtay 2003 | Participants were all positive for malaria by blood smear |
| Gonzales‐Ceron 2005 | Evaluates P. vivax only |
| Grobusch 1999 | Not undertaken in a malaria endemic area |
| Grobusch 2002 | Not undertaken in a malaria endemic area |
| Grobusch 2003 | Participants were travellers returning from endemic to non‐endemic areas |
| Grobusch 2003b | Participants were travellers returning from endemic to non‐endemic areas |
| Gupta 2001 | Some participants had severe or complicated malaria |
| Gutierrez 2005 | Not a diagnostic test accuracy study |
| Haditsch 2004 | Review or narrative |
| Hance 2005 | Review or narrative |
| Hanscheid 1999 | Review or narrative |
| Happi 2004 | All participants were positive for malaria by microscopy |
| Hashizume 2006 | Participants were displaced persons from mainly very low endemicity areas |
| Hernandes 2001 | Participants were travellers returning from endemic to non‐endemic areas |
| Holmberg 1992 | Not a diagnostic test accuracy study |
| Hossain 2008 | Participants had severe or complicated malaria |
| Houze 2009 | All participants were positive for malaria by microscopy |
| Humar 1997 | Participants were travellers returning from endemic to non‐endemic areas |
| Huong 2002 | Not based on a consecutive sample; included a group malaria positive by microscopy, and an asymptomatic malaria negative control group |
| Iqbal 2000 | Not a consecutive sample: participants were selected to have a high risk of rheumatoid factor |
| Iqbal 2001 | Participants were travellers returning from endemic to non‐endemic areas |
| Iqbal 2002 | Participants were travellers returning from endemic to non‐endemic areas |
| Iqbal 2004 | All participants were positive for malaria by microscopy |
| Jelinek 1996 | Does not evaluate an immunochromatographic rapid diagnostic test for malaria |
| Jelinek 1999 | Participants were travellers returning from endemic to non‐endemic areas |
| Jelinek 2000 | Participants were travellers returning from endemic to non‐endemic areas |
| Jelinek 2001 | Participants were travellers returning from endemic to non‐endemic areas |
| Jeurissen 1999 | Review or narrative |
| John 1998 | All participants were positive for malaria by microscopy |
| Joshi 2004 | Not evaluating an immunochromatographic rapid diagnostic test |
| Kaewsonthi 1996 | Not a diagnostic test accuracy study |
| Kahama‐Maro 2008 | Eligibility unclear due to lack of published information |
| Kakkilaya 2003 | Review or narrative |
| Kamugisha 2008 | Majority of participants did not have symptoms of malaria |
| Karbwang 1996 | All participants were positive for malaria by microscopy |
| Kaur 2000 | All participants had cerebral malaria |
| Kaushal 1995 | Tested for P. knowlesi infection in monkeys |
| Kaushal 1997 | Review or narrative |
| Kawai 2009 | Tested for P. knowlesi infection in monkeys |
| Keating 2009 | Majority of participants did not have symptoms of malaria |
| Khairnar 2009 | Participants were travellers returning from an endemic to a non‐endemic area |
| Khan 2004 | Participants were hospital inpatients |
| Kilian 1997 | Not able to extract or calculate absolute numbers of true positives, false positives, false negatives and true negatives |
| Kim 2008 | Includes a symptomatic group with malaria infection identified by microscopy, and an asymptomatic group with no malaria infection by microscopy |
| Knappik 2002 | Participants were travellers returning from endemic to non‐endemic areas |
| Kodisinghe 1997 | Some participants did not have symptoms of malaria |
| Kumar 2000 | Participants were migrants from a very low endemicity area |
| Lee 1999 | Some participants did not have symptoms of malaria |
| Lee 2008 | Participants were soldiers usually residing in non‐endemic areas |
| Lema 1999 | Some participants were attending for follow‐up of a previously diagnosed and treated case of malaria |
| Lepere 2004 | Not a diagnostic test accuracy study |
| Lim 2001 | Half the participants had malaria confirmed by microscopy before enrolment |
| Llanos Zavalaga 2000 | Not a diagnostic test accuracy study |
| Llanos‐Zavalaga 2002 | European foreign language study |
| Mahajan 2000 | Participants were hospital inpatients |
| Makler 1998 | Review or narrative |
| Makler 2009 | Review or narrative |
| Malik 2004 | Study was based at a tertiary referral centre with a high percentage of patients with complicated malaria |
| Mankhambo 2002 | Majority of participants did not have symptoms of malaria |
| Mason 2002 | Some participants did not have symptoms of malaria |
| Mayxay 2004 | Not able to extract or calculate absolute numbers of true positives, false positives, false negatives and true negatives |
| McCutchan 2008 | Review or narrative |
| Meena 2009 | Participants were all hospital inpatients |
| Menan 1996 | Not a study of rapid diagnostic tests |
| Mendoza 2007 | Eligibility unclear due to lack of published information |
| Mengesha 1999 | Not able to extract or calculate absolute numbers of true positives, false positives, false negatives and true negatives |
| Metzger 2008 | Participants were recruited by active case finding |
| Mharakurwa 1997 | Participants had all been recently treated for malaria |
| Miller 2001 | Letter |
| Miller 2008 | Not able to extract or calculate absolute numbers of true positives, false positives, false negatives and true negatives |
| Mills 1999 | Participants were travellers returning from endemic to non‐endemic areas |
| Mills 2007 | Eligibility unclear due to lack of published information |
| Mills 2009 | Not a consecutive sample; selected HIV positive participants only |
| Minodier 2005 | Review or narrative |
| Mishra 1999 | Not a consecutive sample; comprised a malaria positive group by microscopy, and negative control groups |
| Mishra 2007 | Eligibility unclear due to lack of published information |
| Mohanty 1999 | Eligibility unclear due to lack of published information |
| Montoya 2008 | European foreign language study |
| Moody 2000 | Participants were travellers returning from endemic to non‐endemic areas |
| Moody 2002 | Review or narrative |
| Moody 2002a | RDTs tested on artificially cultured blood samples |
| Moonasar 2007 | Not a diagnostic test accuracy study |
| Moulin 2009 | Review or narrative |
| Mueller 2007 | Participants not representative of people presenting to ambulatory care setting with symptoms of malaria |
| Munier 2009 | European foreign language study |
| Murray 2003 | Review or narrative |
| Murray 2008 | Review or narrative |
| Myjak 2004 | Participants were travellers returning from endemic to non‐endemic areas |
| Naing 2002 | No usable data for P. falciparum malaria |
| Nema 2004 | All participants were positive for malaria by microscopy |
| Neumann 2008 | Majority of participants did not have symptoms of malaria |
| Ochola 2006 | Review or narrative |
| OMS 1999 | Not a diagnostic test accuracy study |
| Onile 2005 | Review or narrative |
| Ozbilge 2006 | Not an immunochromatographic test |
| Pabon 2007 | European foreign language study |
| Palmer 1998 | Eligibility unclear due to lack of published information |
| Palmer 1999 | All participants were positive for malaria by microscopy |
| Palmer 2003 | Participants were travellers returning from endemic to non‐endemic areas |
| Pammenter 1988 | Review or narrative |
| Pandey 1995 | Review or narrative |
| Park 2003 | Not a consecutive sample; included a known malaria group and negative control group by microscopy |
| Park 2006 | Written in Korean only |
| Parra 1991 | Not a diagnostic test accuracy study |
| Penhalbel 2005 | Not a consecutive sample; included a known malaria group and negative control group by microscopy |
| Perez 2007 | Review or narrative |
| Peyron 1999 | Review or narrative |
| Pica 2005 | Review or narrative |
| Pieroni 1998 | Participants were travellers returning from endemic to non‐endemic areas |
| Pinto 1999 | All participants had previously tested negative for malaria and had symptoms that meant complicated malaria could not be ruled out |
| Piper 1999 | Half the participants lived in non‐endemic areas |
| Pividal 1994 | Not a diagnostic test accuracy study (blood samples from one patient were serially diluted and tested) |
| Planche 2001 | Review or narrative |
| Playford 2002 | Participants were travellers returning from endemic to non‐endemic areas |
| Popov 2000 | Written in Russian only |
| Popov 2004 | Written in Russian only |
| Premji 1994 | Participants did not have symptoms of malaria |
| Prou 1988 | Not an immunochromatographic test |
| Proux 2001 | Majority of participants did not have symptoms of malaria |
| Quintana 1998 | Eligibility unclear due to lack of published information |
| Rabinovich 2006 | Written in Russian only |
| Radrianasolo 2007 | European foreign language study |
| Rahim 2002 | All participants were positive for malaria by microscopy |
| Rajendran 2006 | Eligibility unclear due to lack of published information |
| Ratnawati 2008 | Many participants were recruited by active case finding |
| Rehlis 2004 | Written in Polish only |
| Reyburn 2007 | Not a diagnostic test accuracy study |
| Ricci 2000 | Participants were travellers returning from endemic to non‐endemic areas |
| Richardson 2002 | Participants were travellers returning from endemic to non‐endemic areas |
| Richter 2004 | Review or narrative |
| Richter 2004a | Participants were travellers returning from endemic to non‐endemic areas |
| Roche 1995 | Not an immunochromatographic test |
| Rodriguez‐Iglesias 2005 | Review or narrative |
| Rodulfo 2007 | Some of the participants did not have symptoms of malaria |
| Rolland 2006 | Not a diagnostic test accuracy study |
| Rubio 2001 | Participants were travellers returning from endemic to non‐endemic areas |
| Ryan 2002 | Not a diagnostic test accuracy study |
| Samal 1998 | Not an immunochromatographic test |
| Saranya 2003 | Review or narrative |
| Schmidt 2003 | Review or narrative |
| Seidahmed 2008 | Not a diagnostic test accuracy study |
| Sezibera 2009 | Not a diagnostic test accuracy study |
| Shah 2004 | All participants were positive for malaria by microscopy |
| Shamsi 1999 | Eligibility unclear due to lack of published information |
| Sharma 2008 | Some participants did not have symptoms of malaria |
| She 2007 | Not undertaken in a malaria endemic area |
| Shenoi 1996 | Eligibility unclear due to lack of published information |
| Shiff 1993 | Some participants did not have symptoms of malaria |
| Shillcutt 2008 | Not a diagnostic test accuracy study |
| Shirayama 2008 | Not a diagnostic test accuracy study |
| Shujatullah 2006 | Participants had severe or complicated malaria |
| Shujatullah 2009 | Participants were hospital inpatients |
| Singer 2004 | Majority of participants did not have symptoms of malaria |
| Singh 2000 (b) | Some participants did not have symptoms of malaria |
| Singh 2001 | Participants were recruited by active case finding |
| Singh 2002 | Majority of participants did not have symptoms of malaria |
| Singh 2002(b) | All participants were positive for malaria by microscopy |
| Singh 2004 | Participants had severe or complicated malaria |
| Singh 2005 (a) | Majority of participants did not have symptoms of malaria |
| Singh 2005 (b) | Not able to extract or calculate absolute numbers of true positives, false positives, false negatives and true negatives |
| Singh 2005c | Some participants did not have symptoms of malaria |
| Singh 2007 | Majority of participants did not have symptoms of malaria |
| Skarbinski 2009 | Not a diagnostic test accuracy study |
| Smego 2000 | Review or narrative |
| Sotimehin 2007 | Majority of participants did not have symptoms of malaria |
| Srinivasan 2000 | Participants were travellers returning from endemic to non‐endemic areas |
| Stauffer 2005 | Participants were refugees from an endemic to a non‐endemic country |
| Stauffer 2006 | Participants were travellers returning from endemic to non‐endemic areas |
| Stauffer 2009 | Participants were all travellers returning from an endemic to a non‐endemic area |
| Sturenburg 2009 | Review or narrative |
| Susi 2005 | Participants were all travellers returning from an endemic to a non‐endemic area |
| Swarthout 2007 | All participants were positive for malaria by microscopy |
| Tagbor 2008 | Majority of participants did not have symptoms of malaria |
| Tarazona 2004 | Not able to extract or calculate absolute numbers of true positives, false positives, false negatives and true negatives |
| Tarimo 1999 | Not able to extract or calculate absolute numbers of true positives, false positives, false negatives and true negatives |
| Tarimo 2001 | Not able to extract or calculate absolute numbers of true positives, false positives, false negatives and true negatives |
| Taylor 2002 | All participants were positive for malaria by microscopy |
| Tham 1999 | Participants were all travellers returning from an endemic to a non‐endemic area |
| Thepsamarn 1997 | All participants were positive for malaria by microscopy |
| Tietche 1996 | Not a diagnostic test accuracy study (study of the probability of malaria in febrile children) |
| Tjitra 2001a | All participants were positive for malaria by microscopy |
| Tjitra 2001b | All participants were positive for malaria by microscopy |
| Trachsler 1999 | Not a diagnostic test accuracy study |
| Uguen 1995 | Participants were travellers returning from endemic to non‐endemic areas |
| Uneke 2008 | Not a diagnostic test accuracy study |
| Uneke 2008a | Review or narrative |
| Uzuchukwu 2009 | No usable data for P. falciparum malaria |
| Valea 2009 | No usable data for P. falciparum malaria |
| Valecha 1998 | Eligibility unclear due to lack of published information |
| Valecha 2002 | Participants were recruited by active case finding |
| Van den Ende 1998 | Participants were travellers returning from endemic to non‐endemic areas |
| Van der Palen 2009 | Participants were travellers returning from endemic to non‐endemic areas |
| Van Dijk 2009 | Participants are travellers returning from an endemic to a non‐endemic area |
| Van Hellemond 2009 | Not a diagnostic test accuracy study |
| VanderJagt 2005 | Majority of participants had no symptoms of malaria |
| Venkatesh 2007 | Participants had severe or complicated malaria |
| Voller 1993 | Review or narrative |
| Waltz 2007 | Review or narrative |
| Wang J‐Y 2007 | Not a commercial test kit |
| Wanji 2008 | Participants did not have symptoms of malaria |
| WHO 1996 | Review or narrative |
| Wiese 2006 | Participants were travellers returning from endemic to non‐endemic areas |
| Williams 2008 | Not a diagnostic test accuracy study |
| Win 2001 | Review or narrative |
| Wongsrichanalai 2001 | Review or narrative |
| Wongsrichanalai 2007 | Review or narrative |
| Wu 2005 | Not an immunochromatographic rapid diagnostic test kit |
| Yavo 2002 | European foreign language study |
| Zakai 2003 | Review or narrative |
| Zerpa 2007 | Not able to extract or calculate absolute numbers of true positives, false positives, false negatives and true negatives |
| Zheng 1999 | Written in Chinese only |
| Zhu 1998 | Written in Chinese only |
| Zikusooka 2008 | Not a diagnostic test accuracy study |
| Zurovac 2008 | Not a diagnostic test accuracy study |
Differences between protocol and review
We intended to consider RDTs for detecting all species of malaria in a single review. We subsequently decided to split the review into two to make it more readable.
We had intended to handsearch reference lists of included articles, contact test manufacturers for any unpublished studies, handsearch conference proceedings, and contact authors and other experts for information on ongoing and unpublished studies. However, due to the number of citations returned by our search (over 4000), these activities were not required.
We added four further exclusion criteria: studies that used active case detection to recruit participants; studies that did not present absolute numbers; studies not published in English; and studies not presenting sufficient information to enable a full assessment of their eligibility.
Contributions of authors
The Cochrane Editorial Team identified this review as a priority topic for a Cochrane review. The protocol was developed jointly by the authors. Katharine Abba, Sally Jackson, and Cho‐Min Naing applied inclusion criteria, extracted data and entered the data, with guidance from Paul Garner, Piero Olliaro, and Jon Deeks. Statistical analysis was carried out by Yemsi Takwoingi, Sarah Donegan and Jon Deeks. Katharine Abba wrote the first draft of the review. All authors contributed to the final manuscript.
Sources of support
Internal sources
-
International Medical University, Malaysia.
Research grant ID 134/2007
Liverpool School of Tropical Medicine, UK.
External sources
-
Department for International Development, UK.
Research Programme Grant
NIHR Cochrane Diagnostic Test Accuracy Support Unit, Not specified.
Declarations of interest
There are no known conflicts of interest.
Unchanged, comment added to review
References
References to studies included in this review
A‐Elgayoum 2009 {published data only}
- A‐Elgayoum SME, El‐Karim A, El‐Feki A, Mahgoub BA, El‐Rayah E‐A, Giha HA. Malaria overdiagnosis and burden of malaria misdiagnosis in the suburbs of central Sudan: special emphasis on artemisinin‐based combination therapy era. Diagnostic Microbiology and Infectious Disease 2009;64:20‐6. [DOI] [PubMed] [Google Scholar]
Abeku 2008a {published data only}
- Abeku TA, Kristan M, Jones C, Beard J, Mueller DH, Okia M. Determinants of the accuracy of rapid diagnostic tests in malaria case management: evidence from low and moderate transmission settings in the East African highlands. Malaria Journal 2002;7:202. [DOI] [PMC free article] [PubMed] [Google Scholar]
Abeku 2008b {published data only}
- Abeku TA, Kristan M, Jones C, Beard J, Mueller DH, Okia M. Determinants of the accuracy of rapid diagnostic tests in malaria case management: evidence from low and moderate transmission settings in the East African highlands. Malaria Journal 2002;7:202. [DOI] [PMC free article] [PubMed] [Google Scholar]
Banchongaksorn 1996a {published data only}
- Banchongakasorn T, Yomokgui P, Panyim S, Rooney W, Vickers P. A field trial of the ParaSight‐F test for the diagnosis of Plasmodium falciparum infection. Transactions of the Royal Society of Tropical Medicine and Hygiene 1996;90:244‐5. [DOI] [PubMed] [Google Scholar]
Banchongaksorn 1996b {published data only}
- Banchongakasorn T, Yomokgui P, Panyim S, Rooney W, Vickers P. A field trial of the ParaSight‐F test for the diagnosis of Plasmodium falciparum infection. Transactions of the Royal Society of Tropical Medicine and Hygiene 1996;90:244‐5. [DOI] [PubMed] [Google Scholar]
Banchongaksorn 1997 {published data only}
- Banchongaksorn T, Prajakwong S, Rooney W, Vickers P. Operational trial of ParaSight‐F (dipstick) in the diagnosis of falciparummalaria at the primary health care level. Southeast Asian Journal of Tropical Medicine and Public Health 1997;28(2):243‐6. [PubMed] [Google Scholar]
Bechem 1999 {published data only}
- Bechem NN, Leke RFG, Tietche F, Taylor DW. Evaluation of a rapid test for histidine rich protein 2 for diagnosis of Plasmodium falciparum infection in Cameroonian children. Transactions of the Royal Society of Tropical Medicine and Hygiene 1999;93:46. [DOI] [PubMed] [Google Scholar]
Bell 2001a {published data only}
- Bell D, Go R, Miguel C, Walker J, Cacal L, Saul A. Diagnosis of malaria in a remote area of the Philippines: comparison of techniques and their acceptance by health workers and the community. Bulletin of the World Health Organization 2001;79(10):933‐41. [PMC free article] [PubMed] [Google Scholar]
Bell 2001b {published data only}
- Bell D, Go R, Miguel C, Walker J, Cacal L, Saul A. Diagnosis of malaria in a remote area of the Philippines: comparison of techniques and their acceptance by health workers and the community. Bulletin of the World Health Organization 2001;79(10):933‐41. [PMC free article] [PubMed] [Google Scholar]
Bharti 2008 {published data only}
- Bharti PK, Silawat N, Singh PP, Singh MP, Shukla M, Ghand G, et al. The usefulness of a new rapid diagnostic test, the First Response Malaria Combo (pLDH/HRP2) card test, for malaria diagnosis in the forested belt of central India. Malaria Journal 2008;7:126. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bojang 1999 {published data only}
- Bojang KA. The diagnosis of Plasmodium falciparum infection in Gambian children, by field staff using the rapid, manual, ParaSight‐F test. Annals of Tropical Medicine and Parasitology 1999;93(7):685‐7. [DOI] [PubMed] [Google Scholar]
Caraballo 1996 {published data only}
- Caraballo A, Ache A. The evaluation of a dipstick test for Plasmodium falciparum in mining areas of Venezuela. American Journal of Tropical Medicine and Hygiene 1996;55(5):482‐4. [DOI] [PubMed] [Google Scholar]
Chayani 2004 {published data only}
- Chayani N, Das B, Sur M, Bajoria S. Comparison of parasite lactate dehydrogenase based immunochromatographic antigen detection assay (OptiMAL) with microscopy for the detection of malaria parasites. Indian Journal of Medical Microbiology 2004;22(2):104‐6. [PubMed] [Google Scholar]
Chitkara 2004 {published data only}
- Chitkara A, Ahmed FU. Test for rapid diagnosis of Plasmodium falciparum infection. Indian Journal of Community Medicine 2004;23:173‐4. [Google Scholar]
Cooke 1999 {published data only}
- Cooke AH, Chiodini PL, Doherty T, Moody AH, Ries J, Pinder M. Comparison of a parasite lactate dehydrogenase‐based immunochromatographic antigen detection assay (OptiMAL) with microscopy of the detection of malaria parasites in human blood samples. American Journal of Tropical Medicine and Hygeine 1999;60(2):173‐6. [DOI] [PubMed] [Google Scholar]
De Oliveira 2009 {published data only}
- Oliveira AM, Skarbinski J, Ouma P, Kariuki S, Barnwell J, Otieno K, et al. Malaria rapid diagnostic test use and performance by facility‐based health workers in western Kenya. American Journal of Tropical Medicine and Hygiene 2007;77:338. [Google Scholar]
- Oliveira AM, Skarbinski J, Ouma PO, Kariuki S, Barnwell JW, Otieno K, et al. Performance of malaria rapid diagnostic tests as part of routine malaria case management in Kenya. American Journal of Tropical Medicine and Hygiene 2009;80(3):470‐4. [PubMed] [Google Scholar]
Dev 2004 {published data only}
- Dev V. Relative utility of dipsticks for diagnosis of malaria in mesoendemic area for Plasmodium falciparum and P. vivax in Northeastern India. Vector‐Borne and Zoonotic Diseases 2004;4(2):123‐30. [DOI] [PubMed] [Google Scholar]
Devi 2002 {published data only}
- Devi G, Indumathi VA, Sridharan D, Srinivas BPR, Sandhya BMR. Evaluation of ParaHIT strip test for diagnosis of malaria infection. Indian Journal of Medical Sciences 2002;56(10):489‐94. [PubMed] [Google Scholar]
Durrheim 1998 {published data only}
- Durrheim DN, Govere J, Grange JJP, Mabuza A. Rapid immunochromatographic diagnosis and Rolling Back Malaria ‐ experiences from an African control program. African Journal of Medicine and Medical Sciences 2001;30 Suppl:21‐4. [PubMed] [Google Scholar]
- Durrheim DN, Grange JJP, Govere J, Mngomezulu NM. Accuracy of a rapid immunochromatographic card test for Plasmodium falciparum in a malaria control programme in South Africa. Transactions of the Royal Society of Tropical Medicine and Hygiene 1998;92:32‐3. [DOI] [PubMed] [Google Scholar]
Fernando 2004 {published data only}
- Fernando SD, Karunaweera ND, Fernando WP. Evaluation of a rapid whole blood immunochromatographic assay for the diagnosis of Plasmodium falciparum and Plasmodium vivax malaria. Ceylon Medical Journal 2004;49(1):7‐10. [DOI] [PubMed] [Google Scholar]
- Fernando SD, Karunaweera ND, Fernando WP, Attanayake N, Wickremasinghe AR. A cost analysis of the use of the rapid, whole‐blood, immunochromatographic Pf/Pv assay for the diagnosis of Plasmodium vivax malaria in rural areas of Sri Lanka. Annals of Tropical Medicine and Parasitology 2004;98(1):5‐13. [DOI] [PubMed] [Google Scholar]
Forney 2001 {published data only}
- Forney JR, Magill AJ, Wongsrichanalai C, Sirichaisinthop J, Bautista CT, Heppner DG, et al. Malaria rapid diagnostic devices: performance characteristics of the ParaSight F device determined in a multisite field study. Journal of Clinical Microbiology 2001;39 (8):2884‐90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magill AJ, Wongrichalanai C, Forney JR, Bautista C, Sirichasinthop A, Andersen EM, et al. Performance characteristics of a prototype malaria rapid diagnostic device (MRDD) for the detection of Plasmodium falciparum and Plasmodium vivax. Clinical Infectious Diseases 2000;31(1):472. [Google Scholar]
Forney 2003 {published data only}
- Forney JR, Wongsrichanalai C, Magill AJ, Craig LG, Sirichaisinthop J, Bautista CT, et al. Devices for rapid diagnosis of malaria: evaluation of prototype assays that detect Plasmodium falciparum histidine‐rich protein 2 and a Plasmodium vivax‐specific antigen. Journal of Clinical Microbiology 2003;41(6):2358‐66. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gaye 1998 {published data only}
- Gaye O, Diouf M, Dansokho EF, Mclaughlin G, Diallo S. Diagnosis of Plasmodium falciparum malaria using ParaSight F, ICT Malaria Pf and Malaria IgG CELISA assays. Parasite 1998;5:189‐92. [DOI] [PubMed] [Google Scholar]
Gaye 1999 {published data only}
- Gaye O, Diouf M, Diallo S. A comparison of thick smears, QBC Malaria, PCR and PATH Falciparum Malaria Test Trip in Plasmodium falciparum diagnosis. Parasite 1999;6:273‐5. [DOI] [PubMed] [Google Scholar]
Gerstl 2009 {published data only}
- Gerstl S, Dunkley S, Mukhtar A, Smet M, Baker A, Maikers J. Assessment of two malaria rapid diagnostic tests, with follow‐up of positive pLDH test results, in a hyperendemic falciparum malaria area. Tropical Medicine and International Health 2009;14(Suppl 2):92. [Google Scholar]
Ghosh 2000 {published data only}
- Ghosh SK, Titus Burk E, Valecha N, Murugendrappa MV, Sharma VP. Evaluation of a Rapid Immunochromatographic Test (ICT) for Detection of Plasmodium falciparum Malaria in Karnataka, India. Journal of Parasitic Diseases 2000;24:39‐42. [Google Scholar]
Guthmann 2002 {published data only}
- Guthmann JP, Ruiz A, Priotto G, Kiguli J, Bonte L, Legros D. Validity, reliability and ease of use in the field of five rapid tests for the diagnosis of Plasmodium falciparum malaria in Uganda. Transactions of the Royal Society of Tropical Medicine and Hygiene 2002;96:254‐7. [DOI] [PubMed] [Google Scholar]
Harani 2006 {published data only}
- Harani MS, Beg MA, Khaleeq L, Adil SN, Kakepoto GN, Khurshid M. Role of ICT Malaria immunochromatographic test for rapid diagnosis of malaria. Journal of the Pakistan Medical Association 2006;56(4):167‐71. [PubMed] [Google Scholar]
Hopkins 2007 {published data only}
- Hopkins H, Kambale W, Kamya MR, Staedke SG, Dorsey G, Rosenthal PJ. Comparison of HRP2 and pLDH‐based rapid diagnostic tests for malaria with longitudinal follow‐up in Kampala, Uganda. American Journal of Tropical Medicine and Hygeine 2007;76(6):1092‐7. [PubMed] [Google Scholar]
Hopkins 2008a {published data only}
- Hopkins H, Bebell L, Kambales W, Dokomajilar C, Rosenthal PJ, Dorsey G. Rapid diagnostic tests for malaria at sites of varying transmission intensity in Uganda. The Journal of Infectious Diseases 2008;197:510‐8. [DOI] [PubMed] [Google Scholar]
Hopkins 2008b {published data only}
- Hopkins H, Bebell L, Kambales W, Dokomajilar C, Rosenthal PJ, Dorsey G. Rapid diagnostic tests for malaria at sites of varying transmission intensity in Uganda. The Journal of Infectious Diseases 2008;197:510‐8. [DOI] [PubMed] [Google Scholar]
Iqbal 2003 {published data only}
- Iqbal J, Muneer A, Khalid N, Ahmed MA. Performance of the OptiMAL test for malaria diagnosis among suspected malaria patients at the rural health centres. American Journal of Tropical Medicine and Hygiene 2003;68(5):624‐8. [DOI] [PubMed] [Google Scholar]
Kar 1998 {published data only}
- Kar I, Eapen A, Adak T, Sharma VP. Trial with ParaSight‐F in the detection of Plasmodium falciparum infection in Chennai (Tamil Nadu) India. Indian Journal of Malariology 1998;35:160‐2. [PubMed] [Google Scholar]
Kilian 1999 {published data only}
- Kilian AHD, Kabagambe G, Byamukama W, Langi P, Weis P, Sonnenburg F. Application of the ParaSight‐F dipstick test for malaria diagnosis in a district control programme. Acta Tropica 1999;72:281‐293. [DOI] [PubMed] [Google Scholar]
Kolaczinski 2004 {published data only}
- Kolaczinski J, Mohammed N, Ali A, Ali M, Khan N, Ezard N, et al. Comparison of the OptiMAL rapid antigen test with field microscopy for the detection of Plasmodium vivax and P. falciparum: considerations for the application of the rapid test in Afghanistan. Annals of Tropical Medicine and Parasitology 2004;98(1):15‐20. [DOI] [PubMed] [Google Scholar]
Kumar 1996 {published data only}
- Kumar A, Sharma VP, Thavaselvam D, Sumodan PK. Clinical Trials of a new immunochromatographic test for diagnosis of Plasmodium falciparum malaria in Goa. Indian Journal of Malariology 1996;33:166‐72. [PubMed] [Google Scholar]
Kumar 2004 {published data only}
- Kumar KR, Sudarshan KS. Clinical evaluation of a rapid diagnostic kit (Paracheck‐Pf) for diagnosis of Plasmodium falciparum in Karnataka state of India. Indian Journal of Preventive and Social Medicine 2004;35(1):10‐4. [Google Scholar]
Kyabayinze 2008 {published data only}
- Kyabayinze DJ. Field validity and comparative persistent antigenicity of HRP‐2 rapid diagnostic tests for malaria in a hyperendemic region of Uganda. American Journal of Tropical Medicine and Hygiene 2008;79(6):884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kyabayinze DJ, Tibenderana JK, Odong GW, Rwakimari JB, Counihan H. Operational accuracy and comparative persistent antigenicity of HRP2 rapid diagnostic tests for Plasmodium falciparum malaria in a hyperendemic region of Uganda. Malaria Journal 2008;7(221). [DOI] [PMC free article] [PubMed] [Google Scholar]
Labbe 2001 {published data only}
- Labbe AC, Pillai DR, Hongvangthing B, Vanisaveth V, Pomphida S, Inkathone S, et al. The performance and utility of rapid diagnostic assays for Plasmodium falciparum malaria in a field setting in the Lao People's Democratic Republic. Annals of Tropical Medicine and Parasitology 95;7:671‐7. [DOI] [PubMed] [Google Scholar]
Mboera 2006a {published data only}
- Mboera LEG, Fanello CI, Malima RC, Talbert A, Fogliati P, Bobbio F, et al. Comparison of the Paracheck‐Pf test with microscopy, for the confirmation of Plasmodium falciparum malaria in Tanzania. Annals of Tropical Medicine and Parasitology 2006;100(2):115‐22. [DOI] [PubMed] [Google Scholar]
Mboera 2006b {published data only}
- Mboera LEG, Fanello CI, Malima RC, Talbert A, Fogliati P, Bobbio F, et al. Comparison of the Paracheck‐Pf test with microscopy, for the confirmation of Plasmodium falciparum malaria in Tanzania. Annals of Tropical Medicine and Parasitology 2006;100(2):115‐22. [DOI] [PubMed] [Google Scholar]
Mboera 2006c {published data only}
- Mboera LEG, Fanello CI, Malima RC, Talbert A, Fogliati P, Bobbio F, et al. Comparison of the Paracheck‐Pf test with microscopy, for the confirmation of Plasmodium falciparum malaria in Tanzania. Annals of Tropical Medicine and Parasitology 2006;100(2):115‐22. [DOI] [PubMed] [Google Scholar]
Mboera 2006d {published data only}
- Mboera LEG, Fanello CI, Malima RC, Talbert A, Fogliati P, Bobbio F, et al. Comparison of the Paracheck‐Pf test with microscopy, for the confirmation of Plasmodium falciparum malaria in Tanzania. Annals of Tropical Medicine and Parasitology 2006;100(2):115‐22. [DOI] [PubMed] [Google Scholar]
Mboera 2006e {published data only}
- Mboera LEG, Fanello CI, Malima RC, Talbert A, Fogliati P, Bobbio F, et al. Comparison of the Paracheck‐Pf test with microscopy, for the confirmation of Plasmodium falciparum malaria in Tanzania. Annals of Tropical Medicine and Parasitology 2006;100(2):115‐22. [DOI] [PubMed] [Google Scholar]
Mekonnen 2010 {published data only}
- Mekonnen Z, Ali S, Belay G, Suleman S, Chatterjee S. Evaluation of the performance of Carestart Malaria Pf/Pf Combo rapid diagnostic test for the diagnosis of malaria in Jimma, Southwestern Ethiopia. Acta Tropica 2010;113:285‐8. [DOI] [PubMed] [Google Scholar]
Mendiratta 2006 {published data only}
- Mendiratta DK, Bhutada K, Narang R, Narang P. Evaluation of different methods for diagnosis of P falciparum malaria. Indian Journal of Medical Microbiology 2006;24(1):49‐51. [DOI] [PubMed] [Google Scholar]
Mens 2007a {published data only}
- Mens P, Spieker N, Omar S, Heijnen M, Schallig H, Kager PA. Is molecular biology the best alternative for diagnosis of malaria to microscopy? A comparison between microscopy, antigen detection and molecular tests in rural Kenya and urban Tanzania. Tropical Medicine and International Health 2007;12(2):238‐44. [DOI] [PubMed] [Google Scholar]
Mens 2007b {published data only}
- Mens P, Spieker N, Omar S, Heijnen M, Schallig H, Kager PA. Is molecular biology the best alternative for diagnosis of malaria to microscopy? A comparison between microscopy, antigen detection and molecular tests in rural Kenya and urban Tanzania. Tropical Medicine and International Health 2007;12(2):238‐44. [DOI] [PubMed] [Google Scholar]
Mharakurwa 1997a {published data only}
- Mharakurwa S, Manyame B, Shiff CJ. Trial of ParaSight‐F test for malaria diagnosis in the primary health care system, Zimbabwe. Tropical Medicine & International Health 1997;2(6):544‐60. [DOI] [PubMed] [Google Scholar]
Mharakurwa 1997b {published data only}
- Mharakurwa S, Manyame B, Shiff CJ. Trial of ParaSight‐F test for malaria diagnosis in the primary health care system, Zimbabwe. Tropical Medicine & International Health 1997;2(6):544‐60. [DOI] [PubMed] [Google Scholar]
Mharakurwa 1997c {published data only}
- Mharakurwa S, Manyame B, Shiff CJ. Trial of ParaSight‐F test for malaria diagnosis in the primary health care system, Zimbabwe. Tropical Medicine & International Health 1997;2(6):544‐60. [DOI] [PubMed] [Google Scholar]
Mohapatra 1996 {published data only}
- Mohapatra PK, Prakash A, Khan AM, Bhattacharyya DR, Goswami BK, Mahanta J. Evaluation of a manual immunochromatographic test for detection of Plasmodium falciparum HRP‐2 antigen. Indian Journal of Medical Microbiology 1996;14(4):193‐5. [Google Scholar]
Moonasar 2009 {published data only}
- Moonasar D, Goga AE, Kruger PS, Cock C, Maharaj R, Frean J, et al. Field evaluation of a malaria rapid diagnostic test (ICT Pf). South African Medical Journal 2009;99(11):810‐3. [PubMed] [Google Scholar]
Msellem 2009 {published data only}
- Msellem MI, Martensson A, Rotllant G, Bhattarai A, Stromberg J, Kahigwa E, et al. Influence of rapid malaria diagnostic tests on treatment and health outcome in fever patients, Zanzibar: a crossover validation study. PLoS Medicine / Public Library of Science 2009;6(4):p. e1000070. [DOI] [PMC free article] [PubMed] [Google Scholar]
Murahwa 1999 {published data only}
- Murahwa FC, Mharakurwa S, Mutambu SL, Rangarira R, Musana BJ. Diagnostic performance of two antigen capture tests for the diagnosis of Plasmodium falciparum malaria in Zimbabwe. Central African Journal of Medicine 1999;45(4):97‐100. [DOI] [PubMed] [Google Scholar]
Mwanza 2005 {published data only}
- Mwanza S, Njunju E, Mbewe B, Chileshe N, Mataa N, Kalungwana N. Evaluation of the hexagon malaria rapid diagnostic test kit in five communities on the copperbelt province of Zambia. Acta Tropica 2005;95S:S303‐4. [Google Scholar]
Nicastri 2009a {published data only}
- Nicastri E, Bevilacqua N, Schepisi SM, Paglia MG, Meschi S, Ame SM, et al. Accuracy of malaria diagnosis by microscopy, rapid diagnostic test, and PCR methods and evidence of antimalarial overprescription in non‐severe febrile patients in two Tanzanian hospitals. American Journal of Tropical Medicine and Hygiene 2009;80(5):712‐7. [PubMed] [Google Scholar]
Nicastri 2009b {published data only}
- Nicastri E, Bevilacqua N, Schepisi SM, Paglia MG, Meschi S, Ame SM, et al. Accuracy of malaria diagnosis by microscopy, rapid diagnostic test, and PCR methods and evidence of antimalarial overprescription in non‐severe febrile patients in two Tanzanian hospitals. American Journal of Tropical Medicine and Hygiene 2009;80(5):712‐7. [PubMed] [Google Scholar]
Nigussie 2008a {published data only}
- Nigussie D, Legesse M, Animut A, Mariam AH, Mulu A. Evaluation of Paracheck Pf and Parascreen Pan/Pf tests for the diagnosis of malaria in an endemic area, South Ethiopia. Ethiopian Medical Journal 2008;46(4):375‐81. [PubMed] [Google Scholar]
Nigussie 2008b {published data only}
- Nigussie D, Legesse M, Animut A, Mariam AH, Mulu A. Evaluation of Paracheck Pf and Parascreen Pan/Pf tests for the diagnosis of malaria in an endemic area, South Ethiopia. Ethiopian Medical Journal 2008;46(4):375‐81. [PubMed] [Google Scholar]
Nwuba 2001 {published data only}
- Nwuba RI, Anumuda CI, Omosun YO, Sodeinde O, Nwagwu M. Evaluation of a rapid immunochromatographic card test for Plasmodium falciparum in Ibadan, Nigeria. African Journal of Medical Science 2001;30:123‐4. [PubMed] [Google Scholar]
Omar 1999 {published data only}
- Omar MS, Malik GM, Al‐Amari OM, Abdalla SE, Moosa RA. The rapid manual ParaSight‐F test for diagnosing Plasmodium falciparum malaria in Saudi Arabia. Annals of Saudi Medicine 1999;2:159‐62. [DOI] [PubMed] [Google Scholar]
Pandya 2001 {published data only}
- Pandya AP, Sahu GC, Anjan JK. The Para Check ‐ PC Test: ‐ A simple rapid dip stick test to detect Plasmodium falciparum infection. Journal of Communicable Diseases 2001;33 (3):224‐5. [PubMed] [Google Scholar]
Pattanasin 2003 {published data only}
- Pattanasin S, Proux S, Chompasuk D, Luwiradaj K, Jacquier P, Looareesuwan, et al. Evaluation of a new plasmodium lactate dehydrogenase assay (OptiMAL‐IT) for the detection of malaria. Transactions of the Royal Society of Tropical Medicine and Hygiene 2003;97:672‐4. [DOI] [PubMed] [Google Scholar]
Rakotonirina 2008 {published data only}
- Rakotonirina H, Barnadas C, Raherijafy R, Andrianantenaina H, Ratsimbasoa A, Randrianasolo L, et al. Accuracy and reliability of malaria diagnostic techniques for guiding febrile outpatient treatment in malaria‐endemic countries. American Journal of Tropical Medicine and Hygiene 2008;78(2):217‐21. [PubMed] [Google Scholar]
Ratsimbasoa 2007 {published data only}
- Ratsimbasoa A, Randriamanantena A, Raherinjafy R, Rasoarilalao N, Menard D. Which malaria rapid test for Madagascar? Field and laboratory evaluation of three test and expert microscopy of samples from suspected malaria patients in Madagascar. American Journal Of Tropical Medicine and Hygiene 2007;76(3):481‐5. [PubMed] [Google Scholar]
Ratsimbasoa 2008 {published data only}
- Ratsimbasoa A, Fanazava L, Radrianjafy R, Ramilijaona J, Rafanomezantsoa H, Menard D. Short report: Evaluation of two new immunochromatographic assays for diagnosis of malaria. American Journal of Tropical Medicine and Hygiene 2008;79(5):670‐2. [PubMed] [Google Scholar]
Sayang 2009 {published data only}
- Sayang C, Soula G, Tahar R, Basco LK, Gazin P, Moyou‐Somo R, et al. Use of a histidine‐rich protein 2‐based rapid diagnostic test for malaria by health personnel during routine consultation of febrile outpatients in a peripheral health facility in Yaounde, Cameroon. American Journal of Tropical Medicine and Hygiene 2009;81(2):343‐7. [PubMed] [Google Scholar]
Sharew 2009 {published data only}
- Sharew B, Legesse M, Animut A, Jima D, Medhim G, Erkko B. Evaluation of the performance of CareStart Malaria Pf/Pv Combo and Paracheck Pf tests for the diagnosis of malaria in Wondo Genet, southern Ethiopia. Acta Tropica 2009;111:321‐4. [DOI] [PubMed] [Google Scholar]
Sharma 1999 {published data only}
- Sharma SK, Tyagi PK, Haque MA, Padhan K. Field studies on the sensitivity and specificity of an immunochromatographic test for the detection of Plasmodium falciparum malaria in tribal areas of Orissa. Indian Journal of Malariology 1999;36:65‐9. [PubMed] [Google Scholar]
Singh 1997 (a) {published data only}
- Singh N, Valecha N, Sharma VP. Malaria diagnosis by field workers using an immunochromatographic test. Transactions of the Royal Society of Tropical Medicine and Hygiene 1997;91:396‐7. [DOI] [PubMed] [Google Scholar]
Singh 1997 (b) {published data only}
- Singh N, Singh MP, Sharma VP. The use of a dipstick antigen‐capture assay for the diagnosis of Plasmodium falciparum infection in a remote forested area of Central India. American Journal of Tropical Medicine and Hygiene 1997;56(2):188‐91. [DOI] [PubMed] [Google Scholar]
Singh 2000 (a) {published data only}
- Singh N, Valecha N. Evaluation of a rapid diagnostic test, 'Determine malaria pf', in epidemic‐prone, forest villages of central India. Annals of Tropical Medicine and Parasitology 2000;94(5):421‐7. [DOI] [PubMed] [Google Scholar]
Singh 2000 (c) {published data only}
- Singh N, Saxena A, Valecha N. Field evaluation of the ICT Malaria Pf/Pv immunochromatographic test for diagnosis of Plasmodium falciparum and P vivax infection in forest villages in Chhindwara, central India . Tropical Medicine and International Health 2000;5(11):765‐70. [DOI] [PubMed] [Google Scholar]
Singh 2003a {published data only}
- Singh N, Valecha N, Nagpal AC, Mishra SS, Varma HS, Subbaro SK. The hospital and field‐based performances of the OptiMAL tests, for malaria diagnosis and treatment monitoring in central India. Annals of Tropical Medicine and Parasitology 2003;97(1):5‐13. [DOI] [PubMed] [Google Scholar]
Singh 2003b {published data only}
- Singh N, Valecha N, Nagpal AC, Mishra SS, Varma HS, Subbaro SK. The hospital and field‐based performances of the OptiMAL tests, for malaria diagnosis and treatment monitoring in central India. Annals of Tropical Medicine and Parasitology 2003;97(1):5‐13. [DOI] [PubMed] [Google Scholar]
Stephens 1999 {published data only}
- Stephens JK, Phanart K, Rooney W, Barnish G. A comparison of three malaria diagnostic tests, under field conditions in North‐West Thailand. Southeast Asian Journal of Tropical Medicine and Public Health 1999;30(4):625‐30. [PubMed] [Google Scholar]
Stow 1999 {published data only}
- Stow NW, Torrens JK, Walker J. An assessment of the accuracy of clinical diagnosis, local microscopy and a rapid immunochromatographic card test in comparison with expert microscopy in the diagnosis of malaria in rural Kenya. Transactions of the Royal Society of Tropical Medicine and Hygiene 1999;93:519‐20. [DOI] [PubMed] [Google Scholar]
Tagbo 2007 {published data only}
- Tagbo O, Henrietta UO. Compariaons of clinical, microscopic and rapid diagnostic test methods in the diagnosis of Plasmodium falciparum malaria in Enugu, Nigeria. Nigerian Postgradulate Medical Journal 2007;14(4):285‐9. [PubMed] [Google Scholar]
Tjitra 1999 {published data only}
- Tjitra E, Suprianto S, Dyer M, Currie BJ, Anstey NM. Field evaluation of the ICT malaria Pf/Pv immunochromatographic test in detection of Plasmodium falciparum and Plasmodium vivax in patients with a presumptive clinical diagnosis of malaria in Eastern Indonesia . Journal of Clinical Microbiology 1999;37(8):2412‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Valecha 2003 {published data only}
- Valecha N, Singh N, Yadav RS, Dev V, Aggarwal A, Subbarao SK. Field evaluation of OptiMAL48 rapid malaria diagnostic test in India. Acta Parasitologica 2003;48(3):229‐32. [Google Scholar]
Van den Broek 2006 {published data only}
- Broek I, Hill O, Gordillo F, Angarita B, Hamade P, Counihan H, et al. Evaluation of three rapid tests for diagnosis of P falciparum and P vivax malaria in Colombia. American Journal of Tropical Medicine and Hygiene 2006;75(6):1209‐15. [PubMed] [Google Scholar]
Verle 1996 {published data only}
- Verle P, Binh LN, Lieu TT, Yen PT, Coosemans M. ParaSight‐F test to diagnose malaria in hypoendemic and epidemic prone regions of Vietnam. Tropical Medicine and International Health 1996;6:794‐6. [DOI] [PubMed] [Google Scholar]
Willcox 2009a {published data only}
- Willcox ML, Sanogo F, Graz B, Forster M, Dakouo F, Sidibe O, et al. Rapid diagnostic tests for the home‐based management of malaria, in a high‐transmission area. Annals of Tropical Medicine and Parasitology 2009;103(1):3‐16. [DOI] [PubMed] [Google Scholar]
Willcox 2009b {published data only}
- Willcox ML, Sanogo F, Graz B, Forster M, Dakouo F, Sidibe O, et al. Rapid diagnostic tests for the home‐based management of malaria, in a high‐transmission area. Annals of Tropical Medicine and Parasitology 2009;103(1):3‐16. [DOI] [PubMed] [Google Scholar]
Wolday 2001 {published data only}
- Wolday D, Balca F, Fessehaye G, Birku Y, Shepherd A. Field trial of the RTM dipstick method for the rapid diagnosis of malaria based on the detection of Plasmodium falciparum HRP‐2 antigen in whole blood. Tropical Doctor 2001;31:18‐21. [PubMed] [Google Scholar]
Wongsrichanalai 1999 {published data only}
- Wongsrichanalai C, Chuanak N, Tulyayon S, Thanoosingha N, Laoboonchai A, Thimasarn K. Comparison of a rapid field immunochromatographic test to expert microscopy for the detection of Plasmodium falciparum asexual parasitemia in Thailand. Acta Tropica 1999;73(3):263‐73. [DOI] [PubMed] [Google Scholar]
Wongsrichanalai 2003 {published data only}
- Wongrichalanai G, Arevalo I, Laoboonchai A, Yingyuen K, Miller RS, Magill AJ, et al. Rapid diagnostic devices for malaria: field evaluation of a new prototype immunochromatographic assay for the detection of Plasmodium falciparum and non‐falciparum plasmodium. American Journal of Tropical Medicine and Hygeine 2003;69(1):26‐30. [PubMed] [Google Scholar]
Yadav 1997 {published data only}
- Yadav RS, Sharma VP, Srivastava HC. Field evaluation of an antigen detection immunochromatographic test for diagnosis of Plasmodium falciparum malaria in India. Tropical Medicine 1997;39(2):45‐9. [Google Scholar]
References to studies excluded from this review
A‐Elgayoum 2009 (b) {published data only}
- A‐Elgayoum SME, El‐Feki EAKA, Mahgoub BA, El‐Rayah EA, Giha HA. Malaria overdiagnosis and burden of malaria misdiagnosis in the suburbs of central Sudan: special emphasis on artemisinin‐based combination therapy era. Diagnostic Microbiology and Infectious Disease 2009;64(1):28‐34. [DOI] [PubMed] [Google Scholar]
Abul 2000 {published data only}
- Abul Faiz M, Rashid R, Palit R, Rahman M R, BinYunus E, Hussain A, et al. ParaSight‐F test results in cerebral malaria patients before and after treatment in Chittagong Medical College Hospital, Bangladesh. Transactions of the Royal Society of Tropical Medicine and Hygiene 2000;94:56‐7. [DOI] [PubMed] [Google Scholar]
Afzaal 2001 {published data only}
- Afzaal S, Singh M, Fatima S, Koshy A A. Rapid diagnostic tests for malaria. Journal of the Association of Physicians of India 2001;49:261‐5. [PubMed] [Google Scholar]
Ahmad 2003 {published data only}
- Ahmad SQ, Abbasi SA, Tariq MA, Mirza SA, Salamat A. Evaluation of plasmodium lactate dehydrogenase based immunochromatographic kit for the diagnosis of malaria. Journal of the College of Physicians and Surgeons of Pakistan 2003;13(3):176‐7. [PubMed] [Google Scholar]
Anonymous 2005 {published data only}
- Anonymous. Micro moves against malaria. New Scientist 2005;187(2517):53. [Google Scholar]
Ansah 2008 {published data only}
- Ansah EK. A comparison of microscopy with rapid diagnostic tests for malaria in rural Ghana. American Journal of Tropical Medicine and Hygiene 2008;79(6):91. [Google Scholar]
Araz 2000 {published data only}
- Araz E, Tanyuksel M, Ardic N, Tabuk C. Performance of a commercial immunochromatographic test for the diagnosis of vivax malaria in Turkey. Transactions of the Royal Society of Tropical Medicine and Hygiene 2000;94:55‐6. [DOI] [PubMed] [Google Scholar]
Arcanjo 2007 {published data only}
- Arcanjo AL, Lacerda MVG, Alecrim WD, Alecrim MDC. Evaluation of the Optimal‐IT (R) and ICT P.f./P.v (R) rapid dipstick tests for diagnosing malaria within primary healthcare in the municipality of Manaus, Amazonas. Revista Da Sociedade Brasileira de Medicina Tropical 2007;40(1):88‐90. [DOI] [PubMed] [Google Scholar]
Arora 2003 {published data only}
- Arora S, Gaiha M, Arora A. Role of the Parasight‐F test in the diagnosis of complicated Plasmodium falciparum malarial infection. Brazilian Journal of Infectious Diseases 2003;7(5):332‐8. [DOI] [PubMed] [Google Scholar]
Arrospide 2004 {published data only}
- Arrospide NV, Marquino QWO, Gutierrez SG. [Evaluacion de una prueba inmunocromatografica ICT P.f/P.v para el diagnostico de malaria por Plasmodium falciparum y Plasmodium vivax en establecimientos de la macroregion norte del Peru]. Revista Peruana de Medicina Experimental y Salud Publica 2004;21(3):134‐8. [Google Scholar]
Arrospide 2004 (a) {published data only}
- Arrospide N, Puray C, Guzman E, Verano M, Medina S, Mendiz Bal S, Gonzales S. [Uso de pruebas rapidas immunocromatograficas para la deteccion de Plasmodium falciparum en donantes de sangre en Peru]. Revista Peruana de Medicina Experimental y Salud Publica 2004;21(2):76‐82. [Google Scholar]
Arrospide 2006 {published data only}
- Arrospide V, Flores P, Ruiz C. [Evaluacion de una prueba rapida basada en la deteccion de pLDH para el diagnostico de malaria en areas endemicas del Peru]. Revista Peruana de Medicina Experimental y Salud Publica 2006;23(2):81‐6. [Google Scholar]
Ashley 2009 {published data only}
- Ashley EA, Touabi M, Ahrer M, Hutagalung R, Htun K, Luchavez J, et al. Evaluation of three parasite lactate dehydrogenase‐based rapid diagnostic tests for the diagnosis of falciparum and vivax malaria. Malaria Journal 2009;8(241). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashley EA, Touabi M, Ahrer M, Hutagalung R, Htun K, Lwin M, et al. Evaluation of 3 rapid diagnostic tests: CareStart Malaria 3 line pLDH (pan, Pf) and Carestart 2 line pLDH (pan) for the diagnosis of malaria in Myanmar. American Journal of Tropical Medicine and Hygiene 2008;79(6):966. [Google Scholar]
Aslan 2001 {published data only}
- Aslan G, Ulukanligil M, Seyrek A, Erel O. Diagnostic performance characteristics of rapid dipstick test for Plasmodium vivax malaria. Memorias do Instituto Oswaldo Cruz 2001;96(5):683‐6. [DOI] [PubMed] [Google Scholar]
Assal 1999 {published data only}
- Assal A, Kauffmann‐Lacroix C, Rodier MH, Darde ML, Houssay D, Jacquemin JL. Comparison of two techniques for detection of anti‐Plasmodium falciparum antibodies: Falciparum‐spot IF (Biomerieux) and Malaria IgG Celisa (BMD). Transfusion Clinique et Biologique 1999;6:119‐23. [DOI] [PubMed] [Google Scholar]
Avila 2002 {published data only}
- Avila PE, Kirchgatteri K, Brunialti KCS. Evaluation of a rapid dipstick test, Malar‐check, for the diagnosis of Plasmodium falciparum malaria in Brazil. Revista do Instituto de Medicina Tropical de Sao Paulo 2002;44(5):293‐6. [DOI] [PubMed] [Google Scholar]
Azazy 2004 {published data only}
- Azazy AA. Performance and accuracy of an immunodiagnostic antigen detection test in diagnosing Plasmodium falciparum among Yemeni patients. Annals of Saudi Medicine 2004;24:50‐1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Babacar 2008 {published data only}
- Babacar F, Ndiaye JL, Diallo I, Tine RC, Seck I, Ba‐Fall F, et al. Feasibility of the rapid diagnostic tests (RDTs) field use for malaria case management in Senegal. American Journal of Tropical Medicine and Hygiene 2008;79(6):967. [Google Scholar]
Bartoloni 1998 {published data only}
- Bartoloni A, Strohmeyer M, Sabatinelli G, Benucci M, Serni U, Paradisi F. False positive ParaSight‐F test for malaria in patients with rheumatoid factor. Transactions of the Royal Society of Tropical Medicine and Hygiene 1998;92:33‐4. [DOI] [PubMed] [Google Scholar]
Bassene 2009 {published data only}
- Bassene H, Kenge P, Ndiath MO, Sokhna C, Dupressoir T, Fontenille D, Trape JF. Comparison of PCR, ELISA‐CSP and direct microscopic observation methods for the detection of Plasmodium falciparum sporozoites in Anopheles gambiae in Sengal. Buletin of the Exotic Pathology Society 2009;102(4):233‐7. [PubMed] [Google Scholar]
Bassett 1991 {published data only}
- Bassett MT, Taylor P, Bvirakare J, Chiteka F, Govera E. Clinical diagnosis of malaria: can we improve?. Journal of Tropical Medicine and Hygiene 1991;94:65‐9. [PubMed] [Google Scholar]
Beadle 1994 {published data only}
- Beadle C, Long GW, Weiss WR, McElroy PD, Maret SM, Oloo AJ, et al. Diagnosis of malaria by detection of Plasmodium falciparum HRP‐2 antigen with a rapid dipstick antigen‐capture assay. The Lancet 1994;343:564‐8. [DOI] [PubMed] [Google Scholar]
Beg 2005 {published data only}
- Beg MA, Ali SS, Haqqee R, Khan MA, Qasim Z, Hussain R, et al. Rapid immunochromatography‐based detection of mixed‐species malaria infection in Pakistan. Southeast Asian Journal of Tropical Medicine and Public Health 2005;36(3):562‐4. [PubMed] [Google Scholar]
Belizario 2005 {published data only}
- Belizario VY, Psay CJ, Bersabe MJ, Leon WU, Guerrero DM, Bugaoisan VM. Field evaluation of malaria rapid diagnostic tests for the diagnosis of P. falciparum and non‐P. falciparum infections. Southeast Asian Journal of Tropical Medicine and Public Health 2005;36(3):552‐561. [PubMed] [Google Scholar]
Bell 2005 {published data only}
- Bell DR, Wilson DW, Martin LB. False‐positive results of a Plasmodium falciparum histidine‐rich protein 2‐detecting malaria rapid diagnostic test due to high sensitivity in a community with fluctuating low parasite density. American Journal of Tropical Medicine and Hygiene 2005;73(1):199‐203. [PubMed] [Google Scholar]
Bell 2006 {published data only}
- Bell D, Peeling RW, Pacific/TDR W HO‐Regional Office for the Western. Evaluation of rapid diagnostic tests: malaria. Nature 2006;4:S34‐8. [DOI] [PubMed] [Google Scholar]
Bellagra 1998 {published data only}
- Bellagra N, Ajana F, Caillaux M. ParaSight F in the diagnosis of Plasmodium falciparum malaria. Pathologie Biologie 1998;46(5):301‐6. [PubMed] [Google Scholar]
Bendezu 2008 {published data only}
- Bendezu J. Field evaluation of a rapid malaria diagnostic test (Parascreen) for malaria diagnosis in the Peruvian Amazon. American Journal of Tropical Medicine and Hygiene 2008;79(6):960. [Google Scholar]
Berens‐Riha 2009 {published data only}
- Beren‐Riha N, Sinicina E, Fleischmann E, Loscher T. Comparison of different methods for delayed post‐mortem diagnosis of falciparum malaria. Malaria Journal 2009;8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bhandari 2008 {published data only}
- Bhandari TS, Rai S, Naik R, Raghuveer CV. Specificity and sensitivity of rapid diagnostic test in the detection of falciparum malaria. Indian Journal of Medical Research 2008;127:638. [Google Scholar]
Bhatt 1994 {published data only}
- Bhatt KM. Laboratory diagnosis of malaria: an overview. African Journal of General Practice 1994;1(1):12. [PubMed] [Google Scholar]
Birku 1999 {published data only}
- Birku Y, Welday D, Ayele D, Shepherd A. Rapid diagnosis of severe malaria based on the detection of Pf‐HRP‐2 antigen. Ethiopian Medical Journal 1999;37(3):173‐9. [PubMed] [Google Scholar]
Bisoffi 2009 {published data only}
- Bisoffi Z, Sirima BS, Angheben A, Lodesani C, Gobbi F, Tinto H, Ende J. Rapid malaria diagnostic tests vs. clinical management of malaria in rural Burkina Faso: safety and effect on clinical decisions: A randomized trial. Tropical Medicine and International Health 2009;14(5):491‐8. [DOI] [PubMed] [Google Scholar]
Bisoffi 2009a {published data only}
- Bisoffi Z, Gobbi F, Angheben A, Ende J. The role of rapid diagnostic tests in managing malaria. PLoS Medicine 2009;6:e1000063. [DOI] [PMC free article] [PubMed] [Google Scholar]
Biswas 2004 {published data only}
- Biswas S. Inter‐test comparison between filter paper absorbed blood eluate and serum for malaria serology by enzyme immunoassay: an operational feasibility. Journal of Immunoassay and Immunochemistry 2004;25(4):399‐410. [DOI] [PubMed] [Google Scholar]
Biswas 2006 {published data only}
- Biswas S. Assessment of immunometric parameters in malaria: role of enzyme immunoassay. Journal of Immunoassay and Immunochemistry 2006;27(4):341‐50. [DOI] [PubMed] [Google Scholar]
Bouchaud 2000 {published data only}
- Bouchaud O, Houze S, Longuet C, Piazza J.P, Ruggieri C, Secardin Y, et al. Use of the Parasight‐F diagnostic test for imported malaria in a travel clinic. American Journal of Tropical Medicine and Hygiene 2000;63(1‐2):76‐9. [DOI] [PubMed] [Google Scholar]
Brenier‐Pinchart 2000 {published data only}
- Brenier‐Pinchart MP, Pinel C, Croisonnier A, Brion JP, Faure O, Ponard D, et al. Diagnosis of malaria in non‐endemic countries by the ParaSight‐F test. American Journal of Tropical Medicine and Hygiene 2000;63(3‐4):150‐2. [DOI] [PubMed] [Google Scholar]
Bruxvoort 2008 {published data only}
- Bruxvoort K, Khatib RA, Abdulah SM, Kahigwa E, Kachur SP, McMorrow ML. Variable sensitivity of malaria rapid diagnostic tests in household surveys ‐ Tanzania 2006. American Journal of Tropical Medicine and Hygiene 2008;79(6):957. [Google Scholar]
Bualombai 2003 {published data only}
- Bualombai P, Prajakwong S, Aussawatheerakui N, Congpuong K, Sudathip S, Thimasarn K, et al. Determining cost‐effectiveness and cost‐component of three malaria diagnostic models being used in remote non‐microscope areas. Southeast Asian Journal of Tropical Medicine and Public Health 2003;34(2):322‐3. [PubMed] [Google Scholar]
Bualombai 2006 {published data only}
- Bualombai P, Balachandra K, Dhepaksorn P, Congpuong K, Satimai W. The validation of DMSC Malaria Pf/Pv rapid diagnostic device for the detection of non‐falciparum malaria in Thailand in 2006. American Journal of Tropical Medicine and Hygiene 2008;79(6):958. [Google Scholar]
Buchachart 2004 {published data only}
- Buchachart K, Krudsood S, Nacher M, Chindanond D, Rungmatcha P, Kano S, et al. Evaluation of the KAT‐Quick Malaria Rapid Test for rapid diagnosis of falciparum malaria in Thailand. Southeast Asian Journal of Tropical Medicine and Public Health 35;1:35‐7. [PubMed] [Google Scholar]
Bujanover 2002 {published data only}
- Bujanover S, Shwartz E. Quick detection of malaria. Israel Medical Association Journal 2002;4(12):1167. [PubMed] [Google Scholar]
Cabezas 2004 {published data only}
- Cabezas SCA, Arrospide V, Marquino QWO, Gutierrez SS, Alvarez M, Chuquipiondo R. [Evaluacion del uso de una prueba rapida inmunocromatografica en promotores de salud para el diagnostico de la malaria en areas rurales de la Amazonia peruana]. Revista Peruana de Medicina Experimental y Salud Publica 2004;21(1):4‐11. [Google Scholar]
Cavallo 1997 {published data only}
- Cavallo JD, Hernandez E, Gerome P, Plotton N, Debord T, Vagueresse R. Serum HRP‐2 antigens and imported Plasmodium falciparum malaria: comparison of ParaSight‐F and ICT malaria P. Medecine Tropicale 1997;57:353‐6. [PubMed] [Google Scholar]
Chatterjee 2008 {published data only}
- Chatterjee K, Chand P. Evaluation of the Rapid in Bios malaria kit for the detection of malaria LDH antigen in human blood. Vox Sanguinis 2008;95:31. [Google Scholar]
Cheng 2006 {published data only}
- Cheng A, Bell D. Evidence behind the WHO guidelines: hospital care for children: what is the precision of rapid diagnostic tests for malaria?. Journal of Tropical Pediatrics 2006;52:386‐9. [DOI] [PubMed] [Google Scholar]
Chilton 2006 {published data only}
- Chilton D, Malik ANJ, Armstrong M, Kettelhut M, Parker‐Williams J, Chiodini PL. Use of rapid diagnostic tests for diagnosis of malaria in the UK. Journal of Clinical Pathology 2006;59(8):862‐866. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chiodini 1998 {published data only}
- Chiodini PL. Non‐microscopic methods for diagnosis of malaria. The Lancet 1998;351:80‐1. [DOI] [PubMed] [Google Scholar]
Chiodini 2005 {published data only}
- Chiodini PL. New diagnostics in parasitology. Infectious Disease Clinics of North America 2005;19(1):267‐70. [DOI] [PubMed] [Google Scholar]
Cho 2001 {published data only}
- Cho D, Kim KH, Park SC, Kim YL, Lee KN, Lim CS. Evaluation of rapid immunocapture assays for diagnosis of Plasmodium vivax in Korea. Parasitology Research 2001;87:445‐8. [DOI] [PubMed] [Google Scholar]
Coleman 2002a {published data only}
- Coleman RE, Maneechai N, Ponlawat A, Kumpitak C, Rachapaew N, Miller RS, Sattabongkot J. Short report: Failure of the OptiMAL rapid malaria test as a tool for the detection of asymptomatic malaria in an area of Thailand endemic for Plasmodium falciparum and P vivax. American Journal of Tropical Medicine and Hygiene 2002;67(6):563‐5. [DOI] [PubMed] [Google Scholar]
Coleman 2002b {published data only}
- Coleman RE, Maneechai N, Rachapaew N, Kumpitak C, Soyseng V, Miller R S, et al. Field evaluation of the ICT Malaria Pf/Pv immunochromatographic test for the detection of asymptomatic malaria in a Plasmodium falciparum/ vivax endemic area in Thailand. American Journal of Tropical Medicine and Hygiene 2002;66(4):379‐83. [DOI] [PubMed] [Google Scholar]
Cong Le 2002 {published data only}
- Cong Le D, Sergiev VP, Rabinovich SA, Nhah DH, Huong NV, Morozov EN, et al. Efficiency and specificity of the KAT‐test for rapid diagnosis of falciparum malaria. Meditsinskaia Parazitologiia i Parazitarnye Bolezni 2002;2:17‐20. [PubMed] [Google Scholar]
Craig 1997 {published data only}
- Craig MH, Sharp BL. Comparative evaluation of four techniques for the diagnosis of Plasmodium falciparum infections. Transactions of the Royal Society and Tropical Medicine and Hygiene 1997;91:279‐82. [DOI] [PubMed] [Google Scholar]
Craig 2002 {published data only}
- Craig MH, Bredenkamp BL, Williams CHV, Rossouw EJ, Kelly VJ, Kleinschmidt I, et al. Field and laboratory comparative evaluation of ten rapid malaria diagnostic tests. Transactions of the Royal Society of Tropical Medicine and Hygiene 2002;96:258‐65. [DOI] [PubMed] [Google Scholar]
Cropley 2000 {published data only}
- Cropley IM, Lockwood DN, Mack D, Pasvol G, Davidson R.N. Rapid diagnosis of Falciparum malaria by using the ParaSight F test in travellers returning to the United Kingdom: prospective study. British Medical Journal 2000;321(7259):484‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cuadros 2007 {published data only}
- Cuadros J, Martin‐Rabadan P, Merino FJ, Delgado‐Irribarren A, Garcia‐Bujalance S, Rubio JM. Malaria diagnosis by NOW ICT and expert microscopy in comparison with multiplex polymerase chain reaction in febrile returned travellers. European Journal of Clinical Microbiology and Infectious Diseases 2007;26(9):671‐3. [DOI] [PubMed] [Google Scholar]
De Carsalade 2009 {published data only}
- Carsalade GY, Lam Kam R, Lepere JF, Brettes A, Peyramond D. Can the thick drop/smear examination for malaria be replaced by a rapid diagnostic test in first intention? The Mayotte experience. Medecine et Maladies Infectieuses 2009;39:36‐40. [DOI] [PubMed] [Google Scholar]
De Dominguez 1996 {published data only}
- Dominguez N, Rodriguez‐Acosta A. Glutamate dehydrogenase antigen detection in Plasmodium falciparum infections. Korean Journal of Parasitology 1996;34(4):239‐246. [DOI] [PubMed] [Google Scholar]
De Monbrison 2004 {published data only}
- Monbrison F, Gerome P, Chaulet JF, Wallon M, Picot S, Peyron F. Comparative diagnostic performance of two commercial rapid tests for malaria in a non‐endemic area. European Journal of Clinical Microbiology and Infectious Diseases 2004;23(10):784‐6. [DOI] [PubMed] [Google Scholar]
Delaunay 2008 {published data only}
- Delaunay P, Estran‐Pomares C, Marty P. Malaria diagnosis: thickdrop and bloodsmear examination, and rapid test. Medecine et Maladies Infectieuses 2008;38 Suppl 2:S121‐3. [DOI] [PubMed] [Google Scholar]
Deletoille 1987 {published data only}
- Deletoille P, Prou O. Value of rapid diagnosis of Plasmodium falciparum using indirect monoclonal immunofluorescence. Bulletin de la Societe de Pathologie Exotique et de Ses Filiales 1987;80:569‐80. [PubMed] [Google Scholar]
Di Perry 1997 {published data only}
- Perry G, Olliaro P, Nardi S, Allegranzi B, Deganello R, Vento S, et al. The Parasight‐F rapid dipstick antigen capture assay for monitoring parasite clearance after drug treatment for Plasmodium falciparum malaria. Transactions of the Royal Society of Tropical Medicine and Hygiene 1997;91:403‐5. [DOI] [PubMed] [Google Scholar]
Dietze 1995 {published data only}
- Dietze R, Perkins M, Boulos M, Luz F, Reller B, Corey GR. The diagnosis of Plasmodium falciparum infection using a new antigen detection system. American Journal of Tropical Medicine and Hygiene 1995;52:45‐9. [DOI] [PubMed] [Google Scholar]
Drakeley 2009 {published data only}
- Drakeley C, Reyburn H. Out with the old, in with the new: the utility of rapid diagnostic tests for malaria diagnosis in Africa. Transactions of the Royal Society of Tropical Medicine and Hygiene 2009;103(4):333‐7. [DOI] [PubMed] [Google Scholar]
Dubarry 1990 {published data only}
- Dubarry M, Luilier M, Malot N, Bayard P, Lambin P, Prou O. Enzyme immunoassays for detection of malarial antigens in human plasma by Plasmodium falciparum monoclonal antibodies. American Journal of Tropical Medicine and Hygiene 1990;43(2):116‐23. [DOI] [PubMed] [Google Scholar]
Durand 2005 {published data only}
- Durand F, Crassous B, Fricker‐Hidalgo H, Carpentier F, Brion JP, Grillot R, et al. Performance of the Now Malaria rapid diagnostic test with returned travellers: a 2‐year retrospective study in a French teaching hospital. Clinical Microbiology and Infection 2007;11(11):903‐7. [DOI] [PubMed] [Google Scholar]
Durand 2005a {published data only}
- Durand F, Faure O, Brion JP, Pelloux H. Invalid result of Plasmodium falciparum malaria detection with the Binax NOW Malaria rapid diagnostic test. Journal of Medical Microbiology 2005;54:1115. [DOI] [PubMed] [Google Scholar]
Dyer 2000 {published data only}
- Dyer ME, Tjitra E, Currie BJ, Anstey NM. Failure of the ‘pan‐malarial’ antibody of the ICT Malaria P.f/P.v immunochromatographic test to detect symptomatic Plasmodium malariae infection. Transactions of the Royal Society of Tropical Medicine and Hygiene 2000;94(5):518. [DOI] [PubMed] [Google Scholar]
Eisen 2000 {published data only}
- Eisen DP, Saul A. Disappearance of pan‐malarial antigen reactivity using the ICT Malaria P.f/P.v (TM) kit parallels decline of patent parasitaemia as shown by microscopy. Transactions of the Royal Society of Tropical Medicine and Hygiene 2000;94:169‐70. [DOI] [PubMed] [Google Scholar]
El‐Moamly 2007 {published data only}
- Moamly AMAR. Antigen capture immuno‐chromatographic strip format in detecting parasite‐specific lactate dehydrogenase to diagnose malaria in non‐immune patients. Journal of the Egyptian Society of Parasitology 2007;37(3):1017‐30. [PubMed] [Google Scholar]
Elmardi 2009 {published data only}
- Elmardi KA, Malik EM, Abdelgadir T, Ali SH, Elsyed AH, Mudather MA, et al. Feasibility and acceptability of home‐based management of malaria strategy adapted to Sudan's conditions using artemisinin‐based combination therapy and rapid diagnostic test. Malaria Journal 2009;8:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
Endeshaw 2008 {published data only}
- Endeshaw TG, Teshome NJ, Graves PaM, Shargie EB, Ejigsemahu Y, et al. Evaluation of light microscopy and rapid diagnostic test for the detection of malaria under operational field conditions: a household survey in Ethiopia. Malaria Journal 2008;7:118. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fan 2000 {published data only}
- Fan B, Zhang ZX, Wen RS. Diagnosis of falciparum malaria using ICT. Chinese Journal of Parasitology and Parasitological Diseases 2000;18(5):281. [PubMed] [Google Scholar]
Farcas 2003 {published data only}
- Farcas GA, Zhong KJY, Lovegrove FE, Graham CM, Kain KC. Evaluation of the Binax NOW ICT test versus polymerase chain reaction and microscopy for the detection of malaria in returned travellers. American Journal of Tropical Medicine and Hygiene 2003;69(6):589‐92. [PubMed] [Google Scholar]
Farcas 2004 {published data only}
- Farcas GA, Zhong KJY, Mazzulli T, Kain KC. Evaluation of the RealArt Malaria LC real‐time PCR assay for malaria diagnosis. Journal of Clinical Microbiology 2004;42(2):636‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ferro 2002 {published data only}
- Ferro BE, Gonzalez IJ, Carvajal F, Palma GI, Saravia NG. Performance of OptiMAL in the diagnosis of Plasmodium vivax and Plasmodium falciparum infections in a malaria referral centre in Colombia. Memorias do Instituto Oswaldo Cruz, Rio de Janeiro 2002;97(5):731‐5. [DOI] [PubMed] [Google Scholar]
Figueiredo 2003 {published data only}
- Figueiredo FAF, Figueredo MC, Nascimento JM, Calvosa VSP, Povoa MM, Machado RLD. Performance of an immunochromatography test for vivax malaria in the Amazon region, Brazil. Revista de Saude Publica 2003;37:390‐2. [DOI] [PubMed] [Google Scholar]
Fogg 2008 {published data only}
- Fogg C, Twesigye R, Batwala V, Piola P, Nabasumba C, Kiguli J, et al. Assessment of three new parasite lactate dehydrogenase (pan‐pLDH) tests for diagnosis of uncomplicated malaria. Transactions of the Royal Society of Tropical Medicine and Hygiene 2008;102:25‐31. [DOI] [PubMed] [Google Scholar]
Fryauff 1997 {published data only}
- Fryauff DJ, Gomez‐Saladin E, Purnomo, Sumawinata I, Sutamihardja MA, Tuti S, et al. Comparative performance of the ParaSight F test for detection of Plasmodium falciparum in malaria‐immune and nonimmune populations in Irian Jaya, Indonesia. Bulletin of the World Health Organization 1997;75:547‐52. [PMC free article] [PubMed] [Google Scholar]
Fryauff 2000 {published data only}
- Fryauff DJ, Purnomo, Sutamihardja MA, Elyazar IR, Susanti I, Krisin BS, et al. Performance of the OptiMAL assay for detection and identification of malaria infections in asymptomatic residents of Irian Jaya, Indonesia. American Journal of Tropical Medicine and Hygiene 2000;63:139‐45. [DOI] [PubMed] [Google Scholar]
Funk 1999 {published data only}
- Funk M, Schlagenhauf P, Tschopp A, Steffen R. MalaQuick versus ParaSight F as a diagnostic aid in travellers' malaria. Transactions of the Royal Society of Tropical Medicine and Hygiene 1999;93(3):268‐72. [DOI] [PubMed] [Google Scholar]
Garavelli 2002 {published data only}
- Garavelli PL. Diagnosis of malaria with immunochromatographic test: The Novara experience. Recenti Progressi in Medicina 2002;93(12):682. [PubMed] [Google Scholar]
Garcia 1996 {published data only}
- Garcia M, Marlborough D. A rapid immunochromatographic tests (ICT) for the diagnosis of Plasmodium falciparum malaria. Journal of Parasitic Diseases 1996;20(1):64. [Google Scholar]
Gatti 2002 {published data only}
- Gatti S, Bernuzzi AM, Bisoffi Z, Raglio A, Gulletta M, Scaglia M, et al. Multicentre study in patients with imported malaria, on the sensitivity and specificity of a dipstick test (ICT Malaria P.f./P.v.) compared with expert microscopy. Annals of Tropical Medicine and Parasitology 2002;96(1):15‐8. [DOI] [PubMed] [Google Scholar]
Gatti 2007 {published data only}
- Gatti S, Gramegna M, Bisoffi Z, Raglio A, Gulletta M, Klersy C. A comparison of three diagnostic techniques for malaria: a rapid diagnostic test (NOW Malaria), PCR and microscopy. Annals of Tropical Medicine and Parasitology 2007;101(3):195‐204. [DOI] [PubMed] [Google Scholar]
Ghanchi 2009 {published data only}
- Ghanchi NK, Beg MA, Hussain R. Estimation of parasite load using rapid diagnostic test ICT (R) Now Malaria P.f/P.v in Plasmodium falciparum malaria . Scandinavian Journal of Infectious Diseases 2009;41:597‐601. [DOI] [PubMed] [Google Scholar]
Gillet 2009 (a) {published data only}
- Gillet P, Bosselaers K, Cnops L, Bottieau E, Esbroeck M, Jacobs J. Evaluation of the SD FK70 malaria Ag Plasmodium vivax rapid diagnostic test in a non‐endemic setting. Malaria Journal 2009;8:129. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gillet 2009 (b) {published data only}
- Gillet P, Mori M, Esbroeck M, Ende J, Jacobs J. Assessment of the prozone effect in malaria rapid diagnostic tests. Malaria Journal 2009;8:271. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gillet 2009 (c) {published data only}
- Gillet P, Dijk DP, Bottieau E, Cnops L, Esbroeck M, Jacobs J. Test characteristics of the SD FK80 Plasmodium falciparum/ Plasmodium vivax malaria rapid diagnostic test in a non‐endemic setting. Malaria Journal 2009;8:262. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gogtay 1999 {published data only}
- Gogtay NJ, Kotwani RN, Rajgor D, Kanbur A, Karnad DR, Kshirsagar NA. Serial ParaSight‐F test in patients with severe malaria. Indian Journal of Malariology 1999;36(3‐4):94‐5. [PubMed] [Google Scholar]
Gogtay 2003 {published data only}
- Gogtay NJ, Dalvi SS, Rajgor D, Chogle AR, Karnad DR, Ramdas M, et al. Diagnostic and prognostic utility of rapid strip (OptiMAL and Paracheck) versus conventional smear microscopy in adult patients of acute, uncomplicated P falciparum malaria in Mumbai, India. Journal of the Association of Physicians of India 2003;51:762‐4. [PubMed] [Google Scholar]
Gonzales‐Ceron 2005 {published data only}
- Gonzalez‐Ceron L, Rodriguez MH, Betanzos AF, Abadia A. Efficacy of a rapid test to diagnose Plasmodium vivax in symptomatic patients of Chiapas, Mexico. Salud Publica de Mexico 2005;47(4):282‐7. [DOI] [PubMed] [Google Scholar]
Grobusch 1999 {published data only}
- Grobusch MP, Alpermann U, Schwenke S, Jelinek T, Warhurst DC. False‐positive rapid tests for malaria in patients with rheumatoid factor. The Lancet 1999;353:297. [DOI] [PubMed] [Google Scholar]
Grobusch 2002 {published data only}
- Grobusch MP, Hanscheid T, Zoller T, Jelinek T, Burchard GD. Rapid immunochromatographic malarial antigen detection unreliable for detecting Plasmodium malariae and Plasmodium ovale. European Journal of Clinical Microbiology and Infectious Diseases 2002;21:818‐20. [DOI] [PubMed] [Google Scholar]
Grobusch 2003 {published data only}
- Grobusch MP, Hanscheid T, Gobels K, Slevogt H, Zoller T, Rogler G, et al. Sensitivity of P vivax rapid antigen detection tests and possible implications for self‐diagnostic use. Travel Medicine and Infectious Disease 2003;1(2):119‐22. [DOI] [PubMed] [Google Scholar]
Grobusch 2003b {published data only}
- Grobusch MP, Hanscheid T, Gobels K, Slevogt H, Zoller T, Rogler G, et al. Comparison of three antigen detection tests for diagnosis and follow‐up of falciparum malaria in travellers returning to Berlin, Germany. Parasitology Research 2003;89(5):354‐7. [DOI] [PubMed] [Google Scholar]
Gupta 2001 {published data only}
- Gupta MK, Misra RN, Chawla N, Mani H, Chowdhry CN, Singh SP. Immunochromatographic test: a new dimensions in diagnosis of Plasmodium falciparum malaria. Medical Journal of the Armed Forces of India 2001;57(3):188‐90. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gutierrez 2005 {published data only}
- Gutierrez Y, Paco G, Romero L, Gonzales J‚ Penar LM, Gimenez T. [Fluorometria; un metodo rapido y sencillo para evaluar la Actividad Antipaludica]. Biofarbo 2005;13(13):3‐10. [Google Scholar]
Haditsch 2004 {published data only}
- Haditsch M. Quality and reliability of current malaria diagnostic methods. Travel Medicine and Infectious Disease 2004;2(3‐4):149‐60. [DOI] [PubMed] [Google Scholar]
Hance 2005 {published data only}
- Hance P, Garnotel E, Pina JJ, Vedy S, Ragot C, Chadli M, Morillon M. Rapid immunochromatographic tests for detection of malaria: principles and strategies for use. Medecine Tropicale 2005;65(4):389‐93. [PubMed] [Google Scholar]
Hanscheid 1999 {published data only}
- Hanscheid T. Diagnosis of malaria: a review of alternatives to conventional microscopy. Clinical and Laboratory Haematology 1999;21(4):235‐45. [DOI] [PubMed] [Google Scholar]
Happi 2004 {published data only}
- Happi CT, Gbotosho GO, Sowunmi A, Falade CO, Akinboye DO, Oladepo O, et al. Malaria diagnosis: false negative ParaSight‐F tests in falciparum malaria patients in Nigeria. African Journal of Medical Science 2004;33:15‐8. [PubMed] [Google Scholar]
Hashizume 2006 {published data only}
- Hasizume M, Kondo H, Murakami T, Kodama M, Nakahara S, Lucas MES, et al. Use of rapid diagnostic tests for malaria in an emergency situation after the flood disaster in Mozambique. Public Health 2006;120:444‐7. [DOI] [PubMed] [Google Scholar]
Hernandes 2001 {published data only}
- Hernandez E, Pina JJ, Fabre R, Garrabe E, Raphenon G, Cavallo JD. Evaluation of the OptiMal test in the diagnosis of imported malarial outbreak. Medecine Tropicale 2001;61(2):153‐7. [PubMed] [Google Scholar]
Holmberg 1992 {published data only}
- Holmberg M, Wahlberg J, Lundeberg J, Pettersson U, Uhlen M. Colorimetric detection of Plasmodium falciparum and direct sequencing of amplified gene fragments using a solid phase method. Molecular and Cellular Probes 1992;6(3):201‐8. [DOI] [PubMed] [Google Scholar]
Hossain 2008 {published data only}
- Hossain MA, Afroj S, Rahman MR, Yunus EB, Samad R, Asna ZH. Evaluation of alternative diagnostic techniques for diagnosis of cerebral malaria in a tertiary referral hospital in Bangladesh. Mymensingh Medical Journal 2008;17(2):180‐5. [PubMed] [Google Scholar]
Houze 2009 {published data only}
- Houze S, Boly MD, Bras J, Deloron P, Faucher J‐F. PfHRP‐2 and PfLDH antigen detection for monitoring the efficacy of artemisinin‐based combination therapy (ACT) in the treatment of uncomplicated falciparum malaria. Malaria Journal 2009;8(211). [DOI] [PMC free article] [PubMed] [Google Scholar]
Humar 1997 {published data only}
- Humar A, Ohrt C, Harrington MA, Pillai D, Kain KC. Parasight‐F test compared with the polymerase chain reaction and microscopy for the diagnosis of Plasmodium falciparum malaria in travelers. American Journal of Tropical Medicine and Hygiene 1997;56(1):44‐8. [DOI] [PubMed] [Google Scholar]
Huong 2002 {published data only}
- Huong NM, Davis TME, Hewitt S, Huong N, Uyen TT, Nhan DH, et al. Comparison of three antigen detection methods for diagnosis and therapeutic monitoring of malaria: a field study from southern Vietnam. Tropical Medicine and International Health 2002;7:304‐8. [DOI] [PubMed] [Google Scholar]
Iqbal 2000 {published data only}
- Iqbal J, Sher A, Rab A. Plasmodium falciparum histidine‐rich protein 2‐based immunocapture diagnostic assay for malaria: cross‐reactivity with rheumatoid factors. Journal of Clinical Microbiology 2000;38(3):1184‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Iqbal 2001 {published data only}
- Iqbal J, Hira PR, Sher A, Al Enezi AA. Diagnosis of imported malaria by Plasmodium lactate dehydrogenase (pLDH) and histidine‐rich protein 2 (PfHRP‐2)‐based immunocapture assays. American Journal of Tropical Medicine and Hygiene 2001;64(1‐2):20‐3. [DOI] [PubMed] [Google Scholar]
Iqbal 2002 {published data only}
- Iqbal J, Khalid N, Hira R. Comparison of two commercial assays with expert microscopy for confirmation of symptomatically diagnosed malaria. Journal of Clinical Microbiology 2002;40:4675‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Iqbal 2004 {published data only}
- Iqbal J, Siddique A, Jameel M, Hira PR. Persistent histidine‐rich protein 2, parasite lactate dehydrogenase, and panmalarial antigen reactivity after clearance of Plasmodium falciparum monoinfection. Journal of Clinical Microbiology 2004;42(9):4237‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jelinek 1996 {published data only}
- Jelinek T, Kilian AH, Henk M, Mughusu EB, Nothdurft HD, Loscher T, et al. Parasite‐specific lactate dehydrogenase for the diagnosis of Plasmodium falciparum infection in an endemic area in west Uganda. Tropical Medicine and International Health 1996;1(2):227‐30. [DOI] [PubMed] [Google Scholar]
Jelinek 1999 {published data only}
- Jelinek T, Grobusch MP, Schwenke S, Steidl S, Sonnenburg F, Nothdurft HD, et al. Sensitivity and specificity of dipstick tests for rapid diagnosis of malaria in nonimmune travelers. Journal of Clinical Microbiology 1999;37(3):721‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jelinek 2000 {published data only}
- Jelinek T, Grobusch MP, Nothdurft HD. Use of dipstick tests for the rapid diagnosis of malaria in nonimmune travelers. Journal of Travel Medicine 2000;7(4):175‐9. [DOI] [PubMed] [Google Scholar]
Jelinek 2001 {published data only}
- Jelinek T, Grobusch MP, Harms G. Evaluation of a dipstick test for the rapid diagnosis of imported malaria among patients presenting within the network TropNetEurop. Scandinavian Journal of Infectious Diseases 2001;33(10):752‐4. [DOI] [PubMed] [Google Scholar]
Jeurissen 1999 {published data only}
- Jeurissen A, Beert J. Two rapid tests for the detection of Plasmodium falciparum [Twee sneltests ter detectie van Plasmodium falciparum]. Tijdschr. voor Geneeskunde 1999;55:1088‐92. [Google Scholar]
John 1998 {published data only}
- John SM, Sudarsanam A, Sitaram U, Moody AH. Evaluation of OptiMAL, a dipstick test for the diagnosis of malaria. Annals of Tropical Medicine and Parasitology 1998;92:621‐2. [DOI] [PubMed] [Google Scholar]
Joshi 2004 {published data only}
- Joshi HH, Mahakunkijcharoen Y, Tantivanich S, Sharma AP, Khusmith S. Detection of P vivax antigens in malaria endemic populations of Nepal by ELISA using monoclonal antibodies raised against Thai isolates. Southeast Asian Journal of Tropical Medicine and Public Health 2004;35(4):828‐33. [PubMed] [Google Scholar]
Kaewsonthi 1996 {published data only}
- Kaewsonthi S, Harding AG, Kidson C, Indaratna K. Assessing the economic impact of a rapid on‐site malaria diagnostic test. Southeast Asian Journal of Tropical Medicine and Public Health 1996;27(2):210‐5. [PubMed] [Google Scholar]
Kahama‐Maro 2008 {published data only}
- Kahama‐Maro J, D'Acremont V, Mtasiwa D, Genton B, Lengeler C. Low quality of routine microscopy for malaria at different health systems levels in Dar es Salaam: rapid diagnostic tests should also be implemented in hospitals and urban settings. American Journal of Tropical Medicine and Hygiene 2008;79(6):394. [Google Scholar]
Kakkilaya 2003 {published data only}
- Kakkilaya BS. Rapid diagnosis of malaria. Laboratory Medicine 2003;34(8):602‐8. [Google Scholar]
Kamugisha 2008 {published data only}
- Kamugisha ML, Msangeni H, Beale E, Malecela EK, Akida JI, Lemnge MM. Paracheck Pf compared with microscopy for diagnosis of Plasmodium falciparum malaria among children in Tanga City, north‐eastern Tanzania. Tanzania Journal of Health Research 2008;10(1):14‐9. [DOI] [PubMed] [Google Scholar]
Karbwang 1996 {published data only}
- Karbwang J, Tasanor O, Kanda T, Wattanagoon Y, Ibrahim M, Na‐Bangchang K, et al. ParaSight‐F test for the detection of treatment failure in multidrug resistant Plasmodium falciparum malaria. Transactions of the Royal Society of Tropical Medicine and Hygiene 1996;90:513‐5. [DOI] [PubMed] [Google Scholar]
Kaur 2000 {published data only}
- Kaur H, Mani A. Evaluation & usefulness of a immunochromatographic test for rapid detection of Plasmodium falciparum infection. Indian Journal of Medical Sciences 2000;54:421‐4. [PubMed] [Google Scholar]
Kaushal 1995 {published data only}
- Kaushal DC, Kaushal N, Chandra D, Palni R. Immunodiagnosis of malaria based on detection of parasite enzyme. Journal of Parasitic Diseases 1995;19:21‐4. [Google Scholar]
Kaushal 1997 {published data only}
- Kaushal DC, Kaushal NA. Immunodiagnosis of malaria. Journal of Parasitic Diseases 1997;21(1):31‐40. [Google Scholar]
Kawai 2009 {published data only}
- Kawai S, Hirai M, Haruki K, Tanabe K, Chigusa Y. Cross‐reactivity in rapid diagnostic tests between human malaria and zoonotic simian malaria parasite Plasmodium knowlesi infections. Parasitology International 2009;58:300‐2. [DOI] [PubMed] [Google Scholar]
Keating 2009 {published data only}
- Keating J, Miller JM, Bennett A, Moonga HB, Eisele TP. Plasmodium falciparum parasite infection prevalence from a household survey in Zambia using microscopy and a rapid diagnostic test: implications for monitoring and evaluation. Acta Tropica 2009;112(3):277‐82. [DOI] [PubMed] [Google Scholar]
Khairnar 2009 {published data only}
- Khairnar K, Martin D, Lau R, Ralevski F, Pillai DR. Multiplex real‐time quantitative PCR, microscopy and rapid diagnostic immuno‐chromatographic tests for the detection of Plasmodium Spp: performance, limit of detection analysis and quality assurance. Malaria Journal 2009;8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Khan 2004 {published data only}
- Khan SA, Anwar M, Hussain S, Qureshi AH, Ahmad A, Afzal S. Comparison of OptiMAL malarial test with light microscopy for the diagnosis of malaria. Journal of the Pakistan Medical Association 2004;54(8):404‐7. [PubMed] [Google Scholar]
Kilian 1997 {published data only}
- Kilian AHD, Mughusu EB, Kabagambe G, Sonnenburg F. Comparison of two rapid, HRP‐2‐based diagnostic tests for Plasmodium falciparum. Transactions of the Royal Society of Tropical Medicine and Hygiene 1997;91:666‐7. [DOI] [PubMed] [Google Scholar]
Kim 2008 {published data only}
- Kim SH, Nam MH, Roh KH, Park HC, Nam DH, Park GH, et al. Evaluation of a rapid diagnostic test specific for Plasmodium vivax. Tropical Medicine and International Health 2008;13:1495‐500. [DOI] [PubMed] [Google Scholar]
Knappik 2002 {published data only}
- Knappik M, Peyerl‐Hoffmann G, Jelinek T. Plasmodium falciparum: use of a NANP19 antibody‐test for the detection of infection in non‐immune travellers. Tropical Medicine and International Health 7;8:652‐6. [DOI] [PubMed] [Google Scholar]
Kodisinghe 1997 {published data only}
- Kodisinghe HM, Perera KL, Premawansa S, Naotunne T, Wickramasinghe A R, Mendis KN. The ParaSight‐F dipstick test as a routine diagnostic tool for malaria in Sri Lanka. Transactions of the Royal Society of Tropical Medicine and Hygiene 1997;91:398‐402. [DOI] [PubMed] [Google Scholar]
Kumar 2000 {published data only}
- Kumar A, Sumodan PK, Sharma VP. Clinical trials of an indigenous diagnostic kit Paracheck‐F for the diagnosis of Plasmodium falciparum malaria in Goa. Journal of Parasitic Diseases 2000;24:43‐5. [Google Scholar]
Lee 1999 {published data only}
- Lee MA, Aw LT, Singh M. A comparison of antigen dipstick assays with polymerase chain reaction (PCR) technique and blood film examination in the rapid diagnosis of malaria. Annals Academy of Medicine Singapore 1999;28:498‐501. [PubMed] [Google Scholar]
Lee 2008 {published data only}
- Lee SW, Jeon K, Jeon BR, Park I. Rapid diagnosis of vivax malaria by the SD Bioline Malaria Antigen test when thrombocytopenia is present. Journal of Clinical Microbiology 2008;46:939‐42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lema 1999 {published data only}
- Lema OE, Carter JY, Nagelkerke N, Wangai MW, Kitenge P, Gikunda SM, et al. Comparison of five methods of malaria detection in the outpatient setting. American Journal of Tropical Medicine and Hygiene 1999;60(2):177‐82. [DOI] [PubMed] [Google Scholar]
Lepere 2004 {published data only}
- Lepere JF, Macarry A. Malaria diagnosis and treatment in a rural Health Centre in Mayotte (Comoro archipelago, 2002). Sante 2004;14:5‐10. [PubMed] [Google Scholar]
Lim 2001 {published data only}
- Lim HS, Kim HS. Evaluation of diagnostic methods of re‐emerging malaria in Korean patients. Yonsei Medical Journal 2001;42:84‐90. [DOI] [PubMed] [Google Scholar]
Llanos Zavalaga 2000 {published data only}
- Llanos Zavalaga LF, Huayta Zacarias E, Mendoza Requena D, Rosas Aguirre A, Contreras Rios C, Peinada Rodriguez J. [Conocimientos y percepciones de los trabajadores de salud de zona endemica de malaria en el Peru sobre la prueba de diagnostico rapido ParaSight‐F]. Revista Medica Herediana 2000;11(4):115‐21. [Google Scholar]
Llanos‐Zavalaga 2002 {published data only}
- Llanos‐Zavalaga LF, Villacorta V, Reyes LRC, Lecca GL, Mendoza RD, Mayca P, et al. [Evaluacion de la prueba ICT Malaria P.f/P.v (AMRAD) para la deteccion de P. falciparum y P. vivax en una zona endemica de la Amazonia peruana]. Revista Peruana de Medicina Experimental y Salud Publica 2002;19(1):39‐42. [Google Scholar]
Mahajan 2000 {published data only}
- Mahajan SK, Siwach SR, Kishore K, Chaudhry D, Sen R, Aggarwal HK, et al. Evaluation of a rapid dipstick antigen capture assay for the diagnosis of falciparum malaria. The Indian Practitioner 2009;53(5):325‐9. [Google Scholar]
Makler 1998 {published data only}
- Makler MT, Piper RC, Milhous WK. Lactate dehydrogenase and the diagnosis of malaria. Parasitology Today 1998;14(9):376‐7. [DOI] [PubMed] [Google Scholar]
Makler 2009 {published data only}
- Makler MT, Piper RC. Rapid malaria tests: where do were go after 20 years?. American Journal of Tropical Medicine and Hygiene 2009;81:921‐6. [DOI] [PubMed] [Google Scholar]
Malik 2004 {published data only}
- Malik S, Khan S, Das A, Samantaray JC. Plasmodium lactate dehydrogenase assay to detect malarial parasites. The National Medical Journal of India 2004;17(5):237‐9. [PubMed] [Google Scholar]
Mankhambo 2002 {published data only}
- Mankhambo L, Kanjala M, Rudman S, Lema VM, Rogerson SJ. Evaluation of the OptiMAL rapid antigen test and species‐specific PCR to detect placental Plasmodium falciparum infection at delivery. Journal of Clinical Microbiology 2008;85(11):544‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mason 2002 {published data only}
- Mason DP, Kawamoto F, Lin K, Laoboonchai A, Wongsrichanalai C. A comparison of two rapid field immunochromatographic tests to expert microscopy in the diagnosis of malaria. Acta Tropica 2002;82:51‐9. [DOI] [PubMed] [Google Scholar]
Mayxay 2004 {published data only}
- Mayxay M, Newton PN, Yeung S, Pongvongsa T, Phompida S, Phetsouvanh T, White NJ. Short communication: An assessment of the use of malaria rapid tests by village health volunteers in rural Laos. Tropical Medicine and International Health 2004;9(3):325‐9. [DOI] [PubMed] [Google Scholar]
McCutchan 2008 {published data only}
- McCutchan TF, Piper RC, Makler MT. Use of malaria rapid diagnostic test to identify Plasmodium knowlesi infection. Emerging Infectious Diseases 2008;14:1750‐2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Meena 2009 {published data only}
- Meena M, Joshi D, Joshi R, Sridhar S, Waghdhare S, Gangane N, et al. Accuracy of a multispecies rapid diagnostic test kit for detection of malarial parasite at the point of care in a low endemicity region. Transactions of the Royal Society of Tropical Medicine and Hygeine 2009;103:1237‐44. [DOI] [PubMed] [Google Scholar]
Menan 1996 {published data only}
- Menan EIH, Adou‐Bryn KD, Mobio SP, Cisse M, Penali K, Kone M. [Bilan des examens parasitologiques du sang pour la recherche du paludisme a l'Institut Pasteur de Cote d'Ivoire (I.P.C.I) en 1992: impact de la chimiotherapie sur les resultats de laboratoire]. Medecine d'Afrique Noire 1996;43(3):129‐33. [Google Scholar]
Mendoza 2007 {published data only}
- Mendoza NM, Garcia M, Cortes LJ, Vela C, Erazo R, Perez P, et al. Evaluation of two rapid diagnostic tests, NOW ICT Malaria Pf/Pv and OptiMAL, for diagnosis of malaria. Biomedica 2007;27:571‐80. [PubMed] [Google Scholar]
Mengesha 1999 {published data only}
- Mengesha T, Gebreselassie H, Mohammed T, Assefa T, Woldemichael T. ParaSight‐F dipstick antigen tests in the diagnosis of falciparum malaria in Ethiopia. East African Medical Journal 1999;76(11):626‐9. [PubMed] [Google Scholar]
Metzger 2008 {published data only}
- Metzger WG, Vivas‐Martinez S, Rodriguez I, Goncalves J, Bongard E, Fanello CI, et al. Malaria diagnosis under field conditions in the Venezuelan Amazon. Transactions of the Royal Society of Tropical Medicine and Hygiene 2008;102:2‐24. [DOI] [PubMed] [Google Scholar]
Mharakurwa 1997 {published data only}
- Mharakurwa S, Shiff CJ. Post treatment sensitivity studies with the ParaSight‐F test for malaria diagnosis in Zimbabwe. Tropical Medicine and International Health 1997;66:61‐7. [DOI] [PubMed] [Google Scholar]
Miller 2001 {published data only}
- Miller RS, McDaniel P, Wongsrichanalai C. Following the course of malaria treatment by detecting parasite lactate dehydrogenase enzyme. British Journal of Haematology 2001;113:558‐62. [DOI] [PubMed] [Google Scholar]
Miller 2008 {published data only}
- Miller RS. Comparison of performance characteristics of the Binax NOW Malaria test using venous and fingerstick samples. American Journal of Tropical Medicine and Hygiene 2008;79(6):533. [Google Scholar]
Mills 1999 {published data only}
- Mills CD, Burgess DC, Taylor HJ, Kain KC. Evaluation of a rapid and inexpensive dipstick assay for the diagnosis of Plasmodium falciparum malaria. Bulletin of the World Health Organization 1999;77(7):553‐9. [PMC free article] [PubMed] [Google Scholar]
Mills 2007 {published data only}
- Mills LA, Blank LR, Kagaayi J, Aluma S, Shott J, Bwanika JB, et al. Performance of malaria rapid diagnostic test versus traditional microscopy among rural Ugandan outpatients. American Journal of Tropical Medicine and Hygiene 2006;75(5):96. [Google Scholar]
Mills 2009 {published data only}
- Mills LA, Kagaayi J, Shott JP, Newell K, Bwanika JB, Ssempijja V, et al. Performance of a prototype malaria rapid diagnostic test versus thick film microscopy among HIV‐positive subjects in rural Rakai, Uganda. Transactions of the Royal Society of Tropical Medicine and Hygiene 2009;77(5 (Abstract book)):96. [DOI] [PMC free article] [PubMed] [Google Scholar]
Minodier 2005 {published data only}
- Minodier P. Malaria diagnosis: rapid detection tests. Clinical Microbiology Reviews 2005;18(8):386‐8. [Google Scholar]
- Minodier P, Noel G, Blanc P, Retornaz K, Garnier JM. Tests for rapid diagnosis of malaria. Archives de Pediatrie 2005;12(6):697‐9. [DOI] [PubMed] [Google Scholar]
Mishra 1999 {published data only}
- Mishra B, Samantaray JC, Mirdha BR. Evaluation of a rapid antigen capture assay for the diagnosis of falciparum malaria. Indian Journal of Medical Research 1999;109:16‐9. [PubMed] [Google Scholar]
Mishra 2007 {published data only}
- Mishra MN, Misra RN. Immunochromatographic methods in malaria diagnosis. Medical Journal Armed Forces India 2006;63(2):127‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mohanty 1999 {published data only}
- Mohanty S, Mishra SK, Mohanty A, Das BS. Immunochromatographic test for the diagnosis of P falciparum malaria. Journal of the Association of Physicians of India 1999;47(2):201‐2. [PubMed] [Google Scholar]
Montoya 2008 {published data only}
- Montoya AE, Menco J, Osorio N, Zuluaga MA, Duque J, Torres G, et al. Concordance between thick blood smear, immunochromatography and polymerase chain reaction for malaria diagnosis. Biomedica 2008;28:252‐61. [PubMed] [Google Scholar]
Moody 2000 {published data only}
- Moody A, Hunt‐Cooke A, Gabbett E, Chiodini P. Performance of the OptiMAL malaria antigen capture dipstick for malaria diagnosis and treatment monitoring at the Hospital for Tropical Diseases, London. British Journal of Haematology 2000;109(4):891‐4. [DOI] [PubMed] [Google Scholar]
Moody 2002 {published data only}
- Moody A. Rapid diagnostic tests for malaria parasites. Clinical Microbiology Reviews 2002;15(1):66‐78. [DOI] [PMC free article] [PubMed] [Google Scholar]
Moody 2002a {published data only}
- Moody AH, Chiodini PL. Non‐microscopic method for malaria diagnosis using OptiMAL IT, a second‐generation dipstick for malaria pLDH antigen detection. British Journal of Biomedical Science 2002;59:228‐31. [DOI] [PubMed] [Google Scholar]
Moonasar 2007 {published data only}
- Moonasar D, Goga AE, Frean J, Kruger P, Chandramohan D. An exploratory study of factors that affect the performance and usage of rapid diagnostic tests for malaria in the Limpopo Province, South Africa. Malaria Journal 2007;6:74. [DOI] [PMC free article] [PubMed] [Google Scholar]
Moulin 2009 {published data only}
- Moulin F, Gendrel D. Imported malaria: diagnostic traps and rapid tests. Archives de Pediatrie 2009;16:S89‐S92. [DOI] [PubMed] [Google Scholar]
Mueller 2007 {published data only}
- Mueller I, Betuela I, Ginny M, Reeder JC, Genton B. The sensitivity of the OptiMAL rapid diagnostic test to the presence of Plasmodium falciparum gametocytes compromises its ability to monitor treatment outcomes in an area of Papua New Guinea in which malaria is endemic. Journal of Clinical Microbiology 2007;45(2):627‐30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Munier 2009 {published data only}
- Munier A, Diallo A, Sokhna C, Chippaux JP. Assessment of a rapid diagnostic test for malaria in rural health care facilities in Senegal. Medicine Tropicale 2009;69(5):496‐500. [PubMed] [Google Scholar]
Murray 2003 {published data only}
- Murray CK, Bell D, Gasser RA, Wongsrichanalai C. Rapid diagnostic testing for malaria. Tropical Medicine and International Health 2003;8(10):876‐83. [DOI] [PubMed] [Google Scholar]
Murray 2008 {published data only}
- Murray CK, Gasser RAJ, Magill AJ, Miller RS. Update on rapid diagnostic testing for malaria. Clinical Microbiology Reviews 2008;21(1):97‐110. [DOI] [PMC free article] [PubMed] [Google Scholar]
Myjak 2004 {published data only}
- Myjak P, Nahorski W, Zarnowska‐Prymek H, Pietkiewicz H. Usefulness of the "OptiMAL Rapid Malaria test" for rapid detection of malaria imported to Poland. Wiadomosci Parazytologiczne 2004;50(2):193‐9. [PubMed] [Google Scholar]
Naing 2002 {published data only}
- Naing C‐M, Gatton ML. Performance appraisal of rapid on‐site malaria diagnosis (ICT Malaria Pf/Pv tests) in relation to human resources at village level in Myanmar. Acta Tropica 2002;81:13‐19. [DOI] [PubMed] [Google Scholar]
Nema 2004 {published data only}
- Nema SK, Chopra GS, Gupta RM, Rai R, Diwan RN. Diagnosis of malaria infection using non‐radioactive malaria diagnostic system (NOMADS). Medical Journal Armed Forces India 2005;61(4):336‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Neumann 2008 {published data only}
- Neumann CG, Bwibo NO, Siekmann JH, McLean ED, Browdy B, Drorbaugh N. Comparison of blood smear microscopy to a rapid diagnostic test for in‐vitro testing for P falciparum malaria in Kenyan school children. East African Medical Journal 2008;85(11):544‐9. [DOI] [PubMed] [Google Scholar]
Ochola 2006 {published data only}
- Ochola LB, Vounatsou P, Smith T, Mabaso MLH, Newton CRJC. The reliability of diagnostic techniques in the diagnosis and management of malaria in the absence of a gold standard. The Lancet Infectious Diseases 2006;6(9):582‐8. [DOI] [PubMed] [Google Scholar]
OMS 1999 {published data only}
- Organisation Mondiale de la Sante USAID. Directives pour l'evaluation rapide: reconnaissance des symptoms de maladies pour le paludisme grave et complique. Organisation Mondiale de la Sante USAID, 1999. [Google Scholar]
Onile 2005 {published data only}
- Onile B, Taiwo S. Recent advances in the laboratory diagnosis of malaria. African Journal of Clinical and Experimental Microbiology 2005;6(2):113‐23. [Google Scholar]
Ozbilge 2006 {published data only}
- Ozbilge H, Kurcer MA, Dogan N, Zeyrek F. Comparison with Pan Malaria IgG assays for malaria diagnosis and direct microscopy among suspected malaria patients in Sanliurfa. Tropical Doctor 2006;36:25‐6. [DOI] [PubMed] [Google Scholar]
Pabon 2007 {published data only}
- Pabon A, Alvarez G, Yanez J, Cespedes C, Rodriguez Y, Restrepo A, et al. Evaluation of ICT malaria immunochromatographic Binax NOW (R) ICT P.f/P.v test for rapid diagnosis of malaria in a Colombian endemic area. Biomedica 2007;27:225‐35. [PubMed] [Google Scholar]
Palmer 1998 {published data only}
- Palmer CJ, Lindon JF, Klaskala WI, Quesada JA, Kaminsky R, Baum MK, et al. Evaluation of the OptiMAL test for rapid diagnosis of Plasmodium vivax and Plasmodium falciparum malaria. Journal of Clinical Microbiology 1998;36(1):203‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Palmer 1999 {published data only}
- Palmer CJ, Validum L, Lindo J, Campa A, Validum C, Makler M, et al. Field evaluation of OptiMAL rapid malaria diagnostic test during anti‐malarial therapy in Guyana. Transactions of the Royal Society of Tropical Medicine and Hygiene 1999;93:517‐8. [DOI] [PubMed] [Google Scholar]
Palmer 2003 {published data only}
- Palmer CJ, Bonilla JA, Bruckner DA, Barnett ED, Miller NS, Haseeb MA, et al. Multicenter study to evaluate the OptiMAL test for rapid diagnosis of malaria in U.S hospitals. Journal of Clinical Microbiology 2003;41(11):5178‐82. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pammenter 1988 {published data only}
- Pammenter MD. Techniques for the diagnosis of malaria. South African Medical Journal 1988;74(2):55‐7. [PubMed] [Google Scholar]
Pandey 1995 {published data only}
- Pandey J, Talib VH, Ranga S, Gulati IRA, Pandey J, Ranga S. Diagnosis of malaria: an overview. Journal of Parasitic Diseases 1995;19(1):21‐4. [Google Scholar]
Park 2003 {published data only}
- Park SK, Lee KW, Hong SH, Kim DS, Lee JH, Jeon BH, et al. Development and evaluation of an immunochromatographic kit for the detection of antibody to Plasmodium vivax infection in South Korea. Yonsei Medical Journal 2003;44:747‐50. [DOI] [PubMed] [Google Scholar]
Park 2006 {published data only}
- Park TS, Kim JH, Kang CI, Lee BH, Jeon BR, Lee SM, et al. Diagnostic usefulness of SD malaria antigen and antibody kits for differential diagnosis vivax malaria in patients with fever of unknown origin. Korean Journal of Laboratory Medicine 2006;26:241‐5. [DOI] [PubMed] [Google Scholar]
Parra 1991 {published data only}
- Parra ME, Evans CB, Taylor DW. Identification of Plasmodium falciparum histidine‐rich protein 2 in the plasma of humans with malaria. Journal of Clinical Microbiology 1991;29(8):1629‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Penhalbel 2005 {published data only}
- Penhalbel R, Souza R, Fugikaha E, Lorenzetti A, Alves RT, Cavasini CE, et al. Evaluation of an immunochromatography test for malaria diagnosis under different storage conditions. Revista da Sociedad Brasileira de Medicina Tropical 2005;38(2):194‐5. [DOI] [PubMed] [Google Scholar]
Perez 2007 {published data only}
- Perez H, Bracho C, Rosa M. [El paludismo y las pruebas r pidas de diagnostico]. Boletin de Malariologia y Salud Ambiental 2007;47(1):3‐13. [Google Scholar]
Peyron 1999 {published data only}
- Peyron F. Parasitologic diagnosis of malaria: Routine and new laboratory techniques. Medecine et Maladies Infectieuses 1999;29(Suppl 3):295‐301. [Google Scholar]
Pica 2005 {published data only}
- Pica R, Castellano C. Looking for parasitic infection and disease: the Plasmodium falciparum malaria model. Clinica Terapeutica 2005;156(3):131‐134. [PubMed] [Google Scholar]
Pieroni 1998 {published data only}
- Pieroni P, Mills CD, Ohrt C, Harrington MA, Kain KC. Comparison of the ParaSight‐F test and the ICT Malaria Pf test with the polymerase chain reaction for the diagnosis of Plasmodium falciparum malaria in travellers. Transactions of the Royal Society of Tropical Medicine and Hygiene 1998;92(2):166‐9. [DOI] [PubMed] [Google Scholar]
Pinto 1999 {published data only}
- Pinto MJW, Pereira NF, Rodrigues S, Kharangate NV, Verenkar MP. Rapid diagnosis of falciparum malaria by detection of Plasmodium falciparum HRP‐2 antigen. Journal of the Association of Physicians of India 1999;47(11):1076‐8. [PubMed] [Google Scholar]
Piper 1999 {published data only}
- Piper R, Lebras J, Wentworth L, Hunt‐Cooke A, Houze S, Chiodini P, et al. Immunocapture diagnostic assays for malaria using Plasmodium lactate dehydrogenase (pLDH). American Journal of Tropical Medicine and Hygiene 1999;60(1):109‐18. [DOI] [PubMed] [Google Scholar]
Pividal 1994 {published data only}
- Pividal J, Monjane AL, Gomes A, Street E, Barreto A. [Avaliacao e seleccao de tecnicas de diagnostico directo na malaria]. Revista Medica de Mocambique 1994;5(3):27‐32. [Google Scholar]
Planche 2001 {published data only}
- Planche T, Krishna S, Kombila M, Engel K, Faucher JF, Ngou‐Milama E, et al. Comparison of methods for the rapid laboratory assessment of children with malaria. American Journal of Tropical Medicine and Hygiene 2001;65(5):599‐602. [DOI] [PubMed] [Google Scholar]
Playford 2002 {published data only}
- Playford EG, Walker J. Evaluation of the ICT malaria P.f/P.v and the OptiMal rapid diagnostic tests for malaria in febrile returned travellers. Journal of Clinical Microbiology 2002;40(11):4166‐71. [DOI] [PMC free article] [PubMed] [Google Scholar]
Popov 2000 {published data only}
- Popov AF, Popova NI. Rapid methods for the diagnosis of tropical malaria. Meditsinskaia Parazitologiia i Parazitarnye Bolezni 2000;2:38‐9. [PubMed] [Google Scholar]
Popov 2004 {published data only}
- Popov AF, Nikiforov ND, Ivanis VA, Barkun SP, Sanin BI, Fedekina LI. Diagnosis of malaria by express methods. Klinicheskaia Laboratornaia Diagnosis 2004;1:46‐8. [PubMed] [Google Scholar]
Premji 1994 {published data only}
- Premji Z, Minjas JN, Shiff CJ. Laboratory diagnosis of malaria by village health workers using the rapid manual ParaSight‐F test. Transactions of the Royal Society of Tropical Medicine and Hygiene 1994;88:418. [DOI] [PubMed] [Google Scholar]
Prou 1988 {published data only}
- Prou O, Deletoille P. Rapid detection of Plasmodium falciparum antigens by monofluo Kit Plasmodium falciparum. Medecine et Maladies Infectieuses 1988;18(2):75‐9. [Google Scholar]
Proux 2001 {published data only}
- Proux S, Hkirijareon L, Ngamngonkiri C, McConnell S, Nosten F. Short communication: Paracheck‐Pf: A new, inexpensive and reliable rapid test for Plasmodium falciparum malaria. Tropical Medicine and International Health 2001;6:99‐101. [DOI] [PubMed] [Google Scholar]
Quintana 1998 {published data only}
- Quintana M, Piper R, Boling HL, Makler M, Sherman C, Gill E, et al. Malaria diagnosis by dipstick assay in a Honduran population with coendemic Plasmodium falciparum and Plasmodium vivax. American Journal of Tropical Medicine and Hygiene 1998;59(6):868‐71. [DOI] [PubMed] [Google Scholar]
Rabinovich 2006 {published data only}
- Rabinovich SA, Kong LD, HA N, Morozov YN, Toropov DY, Kukina IV, et al. Efficiency of Kat‐Quick P.F test (Lat Medical, SAr) among the populations of drug‐resistant parasites. Meditsinskaia Parazitologiia i Parazitarnye Bolezni 2006;2:10‐2. [PubMed] [Google Scholar]
Radrianasolo 2007 {published data only}
- Radrianasolo L, Tafangy PB, Raharimalala LA, Ratsimbasoa AC, Randriamanantena A, Randrianarivelojosia M. Rapid diagnostic test for malaria: preliminary study in Madagascar in 2003. Cahiers Sante 2007;17(2):69‐73. [PubMed] [Google Scholar]
Rahim 2002 {published data only}
- Rahim F, Haq HA, Jamal S. Comparison of amradict test with microscopic examinations for rapid diagnosis of malaria. Journal of the College of Physicians and Surgeons Pakistan 2002;12(9):530‐3. [Google Scholar]
Rajendran 2006 {published data only}
- Rajendran C, Dube S. Field evaluation of rapid immunochroatographic test kit for the diagnosis of Plasmodium falciparum and non‐falciparum malaria parasites for Sontipur Distric, Assam. Journal of Parasitic Diseases 2006;30(1):94‐7. [Google Scholar]
Ratnawati 2008 {published data only}
- Ratnawati MH, Smits HL. Point‐of‐care testing for malaria outbreak management. Transactions of the Royal Society of Tropical Medicine and Hygiene 2008;102:699‐704. [DOI] [PubMed] [Google Scholar]
Rehlis 2004 {published data only}
- Rehlis N, Javor IP. [Interpretacja testow immunochromatographiczynch z antygenem HRP‐2 dzieci do lat 5 w rejonie o wysokim ryzyku transmisji zimnicy w Papua Nowej Gwinei]. Wiadomosci Parazytologiczne 2004;50(2):201‐8. [PubMed] [Google Scholar]
Reyburn 2007 {published data only}
- Reyburn H, Mbakilwa H, Mwangi R, Mwerinde O, Olomi R, Drakeley C, et al. Rapid diagnostic tests compared with malaria microscopy for guiding outpatient treatment of febrile illness in Tanzania: randomised trial. BMJ 2007;334:403. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ricci 2000 {published data only}
- Ricci L, Viani I, Piccolo G, Fabio A, Calderaro A, Galati L, et al. Evaluation of OptiMAL Assay test to detect imported malaria in Italy. New Microbiologica 23;4(12):4528‐30. [PubMed] [Google Scholar]
Richardson 2002 {published data only}
- Richardson DC, Ciach M, Zhong KJY, Crandall I, Kain KC. Evaluation of the Makromed dipstick assay versus PCR for diagnosis of Plasmodium falciparum malaria in returned travelers. Journal of Clinical Microbiology 2002;23(4):391‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Richter 2004 {published data only}
- Richter J, Gobels K, Muller‐Stover I, Hoppenheit B, Haussinger D. Co‐reactivity of plasmodial histidine‐rich protein 2 and aldolase on a combined immuno‐chromatographic‐malaria dipstick (ICT) as a potential semi‐quantitative marker of high Plasmodium falciparum parasitaemia. Parasitology Research 2004;94:384‐5. [DOI] [PubMed] [Google Scholar]
Richter 2004a {published data only}
- Richter J, Harms G, Muller‐Stover I, Gobels K, Haussinger D. Performance of an immunochromatographic test for the rapid diagnosis of malaria. Parasitology Research 2004;92:518‐9. [DOI] [PubMed] [Google Scholar]
Roche 1995 {published data only}
- Roche J, Benito A, Ayecaba S, Amela C, Molina R, Alvar J. Field evaluation of fluorescence microcopy (QBC) for malaria diagnosis. Bulletin de Liaison et de Documentation de L'OCEAC 1995;28(1):26‐9. [Google Scholar]
Rodriguez‐Iglesias 2005 {published data only}
- Rodriguez‐Iglesias M. Rapid serological techniques. Enfermedades Infecciosas y Microbiologia Clinica Monografias 2005;4(2):69‐71. [Google Scholar]
Rodulfo 2007 {published data only}
- Rodulfo H, Donato M, Mora R, Gonzalez L, Contreras CE. Comparison of the diagnosis of malaria by microscopy, immunochromatography and PCR in endemic areas of Venezuela. Brazilian Journal of Medical and Biological Research 2007;40:535‐43. [DOI] [PubMed] [Google Scholar]
Rolland 2006 {published data only}
- Rolland E, Checchi F, Pinoges L, Balkan S, Guthmann JP, Guerin PJ. Operational response to malaria epidemics: are rapid diagnostic tests cost‐effective?. Tropical Medicine and International Health 2006;11(4):398‐408. [DOI] [PubMed] [Google Scholar]
Rubio 2001 {published data only}
- Rubio JM, Buhigas I, Subirats M, Baquero M, Puente S, Benito A. Limited level of accuracy provided by available rapid diagnosis tests for malaria enhances the need for PCR‐based reference laboratories. Journal of Clinical Microbiology 2001;39(7):2736‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ryan 2002 {published data only}
- Ryan JR, Dave K, Collins KM, Hochberg L, Sattabongkot J, Coleman RE, et al. Extensive multiple test centre evaluation of the VecTest malaria antigen panel assay. Medical and Veterinary Entomology 2002;16(3):321‐7. [DOI] [PubMed] [Google Scholar]
Samal 1998 {published data only}
- Samal KK, Agarwalla A. Intradermal smear vs peripheral blood smear in diagnosis of malaria. Indian Practitioner 1998;51(1):27‐8. [Google Scholar]
Saranya 2003 {published data only}
- Saranya N. Rapid diagnostic tests, benefits and pitfalls. Indian Journal of Practical Pediatrics 2003;5(2):111‐7. [Google Scholar]
Schmidt 2003 {published data only}
- Schmidt WP. Malaria rapid diagnostic tests ‐ perspectives for malaria endemic and non‐endemic regions. Laboratoriums Medizin 2003;27(7‐8):296‐301. [Google Scholar]
Seidahmed 2008 {published data only}
- Seidahmed OME, Mohamedein MMN, Elsir AA, Ali FT, Malik EF, Ahmed ES. End‐user errors in applying two malaria rapid diagnostic tests in a remote area of Sudan. Tropical Medicine and International Health 2008;13(3):406‐9. [DOI] [PubMed] [Google Scholar]
Sezibera 2009 {published data only}
- Sezibera C. [Fievre et traitement du paludisme: importance d'une strategie de diagnostic‐traitement au niveau des services de sante de premier echelon]. Thesis Unknown.
Shah 2004 {published data only}
- Shah I, Deshmukh CT. A bedside dipstick method to detect Plasmodium falciparum. Indian Pediatrics 2004;41(11):1148‐51. [PubMed] [Google Scholar]
Shamsi 1999 {published data only}
- Shamsi TS, Ahmed A, Farooqui AI, Waraich S. Rapid diagnosis of malaria: a new approach. Journal of the Pakistan Medical Association 1999;49(1):16‐7. [PubMed] [Google Scholar]
Sharma 2008 {published data only}
- Sharma MK, Rao VK, Agarwal GS, Rai GP, Gopalan N, Prakash S. Highly sensitive amperometric immunosensor for detection of Plasmodium falciparum histidine‐rich protein 2 in serum of humans with malaria: comparison with a commercial kit. Journal of Clinical Microbiology 2008;46(11):3759‐65. [DOI] [PMC free article] [PubMed] [Google Scholar]
She 2007 {published data only}
- She RC, Rawlins ML, Mohl R, Perkins SL, Hill HR, Litwin CM. Comparison of immunofluorescence antibody testing and two enzyme immunoassays in the serologic diagnosis of malaria. Journal of Travel Medicine 2007;14:105‐11. [DOI] [PubMed] [Google Scholar]
Shenoi 1996 {published data only}
- Shenoi UD. Laboratory diagnosis of malaria. Indian Journal of Pathology and Microbiology 1996;39(5):443‐5. [PubMed] [Google Scholar]
Shiff 1993 {published data only}
- Shiff CJ, Minjas J, Premji Z. The ParaSight‐F test: a simple rapid manual dipstick test to detect Plasmodium falciparum infection. Parasitology Today 1994;10(12):494‐5. [DOI] [PubMed] [Google Scholar]
- Shiff CJ, Premji Z, Minjas JN. The rapid manual ParaSight‐F test. A new diagnostic tool for Plasmodium falciparum malaria . Transactions of the Royal Society of Tropical Medicine and Hygiene 1993;87:646‐8. [DOI] [PubMed] [Google Scholar]
Shillcutt 2008 {published data only}
- Shillcutt S, Morel C, Goodman C, Coleman P, Bell D, Whitty CJM, et al. Cost‐effectiveness of malaria diagnostic methods in sub‐Saharan Africa in an era of combination therapy. Bulletin of the World Health Organization 2008;86(2):101‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shirayama 2008 {published data only}
- Shirayama Y, Phompida S, Kuroiwa C. Monitoring malaria control in Khammouane province, Laos: an active case detection survey of Plasmodium falciparum malaria using the Paracheck rapid diagnostic test. Transactions of the Royal Society of Tropical Medicine and Hygiene 2008;102(8):743‐50. [DOI] [PubMed] [Google Scholar]
Shujatullah 2006 {published data only}
- Shujatullah F, Malik A, Khan HM, Malik A. Comparison of different diagnostic techniques in Plasmodium falciparum cerebral malaria. Journal of Vector Borne Diseases 2006;43(4):186‐90. [PubMed] [Google Scholar]
Shujatullah 2009 {published data only}
- Shujatullah F, Khan HM, Malik A, Malik A. Evaluation of ParaSight‐F test in Diagnosis of Plasmodium falciparum infection. J K Science 2009;11(1):16‐9. [Google Scholar]
Singer 2004 {published data only}
- Singer LM, Newman RD, Diarra A, Moran AlC, Huber CS, Stennies G, et al. Evaluation of a malaria rapid diagnostic test for assessing the burden of malaria during pregnancy. American Journal of Tropical Medicine and Hygiene 2004;70(5):481‐5. [PubMed] [Google Scholar]
Singh 2000 (b) {published data only}
- Singh N. Usefulness of a dipstick test (ParaSight‐F) in high‐risk groups for Plasmodium falciparum in Central India. Current Science 2000;79(4):406‐7. [Google Scholar]
Singh 2001 {published data only}
- Singh N, Shukla M. An assessment of the usefulness of a rapid immuo‐chromatographic test 'Determine malaria Pf' in evaluation of intervention measures in forest villages of central India. BMC Infectious Diseases 2001;1(10). [DOI] [PMC free article] [PubMed] [Google Scholar]
Singh 2002 {published data only}
- Singh N, Saxena A, Sharma VP. Usefulness of an inexpensive, Paracheck test in detecting asymptomatic infectious reservoir of Plasmodium falciparum during dry season in an inaccessible terrain in central India. Journal of Infection 2002;45(3):165‐8. [DOI] [PubMed] [Google Scholar]
Singh 2002(b) {published data only}
- Singh N, Shukla MM. Short report: Field evaluation of posttreatment sensitivity for monitoring parasite clearance of Plasmodium falciparum malaria by use of the Determine Malaria Pf test in Central India. American Journal of Tropical Medicine and Hygiene 2002;66(3):314‐6. [DOI] [PubMed] [Google Scholar]
Singh 2004 {published data only}
- Singh N, Nagpal AC. Performance of the OptiMAL dipstick test for management of severe and complicated malaria cases in a tertiary hospital, central India. Journal of Infection 2004;48(4):364‐5. [DOI] [PubMed] [Google Scholar]
Singh 2005 (a) {published data only}
- Singh N, Saxena A, Awadhia SB, Shrivastava R, Singh MP. Evaluation of a rapid diagnostic test for assessing the burden of malaria at delivery in India. American Journal of Tropical Medicine and Hygiene 2005;73(5):855‐8. [PubMed] [Google Scholar]
Singh 2005 (b) {published data only}
- Singh N, Mishra AK, Shukla MM, Chand SK, Bharti PK. Diagnostic and prognostic utility of an inexpensive rapid on site malaria diagnostic test (ParaHIT f) among ethnic tribal population in areas of high, low and no transmission in central India. BMC Infectious Diseases 2005;5(50). [DOI] [PMC free article] [PubMed] [Google Scholar]
Singh 2005c {published data only}
- Singh N, Saxena A. Usefulness of a rapid on‐site Plasmodium falciparum diagnosis (Paracheck PF) in forest migrants and among the indigenous population at the site of their occupational activities in central India. American Journal of Tropical Medicine and Hygiene 2005;72:26‐9. [PubMed] [Google Scholar]
Singh 2007 {published data only}
- Singh PP, Ahmed R, Singh MP, Terlouw D.J, Ter Kuile FO, Desai MR, et al. Evaluation of the new malaria rapid diagnostic test First Response (R) Pf/Pv, when used as a screening tool for malaria during pregnancy in central India. American Journal of Tropical Medicine and Hygiene 2007;77(5):341. [Google Scholar]
Skarbinski 2009 {published data only}
- Skarbinski J, Ouma PO, Causer LM, Kariuki SK, Barnwell JW, Alaii JA, et al. Effect of malaria rapid diagnostic tests on the management of uncomplicated malaria with artemether‐lumefantrine in Kenya: a cluster randomized trial. American Journal of Tropical Medicine and Hygiene 2009;80(6):919‐26. [PubMed] [Google Scholar]
Smego 2000 {published data only}
- Smego RAJ, Beg A. Rapid diagnostic modalities for malaria. Journal of the Pakistan Medical Association 2000;50(12):398‐9. [PubMed] [Google Scholar]
Sotimehin 2007 {published data only}
- Sotimehin SA, Runsewe‐Abiodun TI, Oladapo OT, Njokanma OF, Olanrewaju DM. Performance of a rapid antigen test for the diagnosis of congenital malaria. Annals of Tropical Paediatrics 2007;27(4):297‐301. [DOI] [PubMed] [Google Scholar]
Srinivasan 2000 {published data only}
- Srinivasan S, Moody AH, Chiodini PL. Comparison of blood‐film microscopy, the OptiMAL dipstick, Rhodamine‐123 fluorescence staining and PCR, for monitoring antimalarial treatment. Annals of Tropical Medicine and Parasitology 2000;94(3):227‐32. [DOI] [PubMed] [Google Scholar]
Stauffer 2005 {published data only}
- Stauffer WM, Newberry A, Cartwright C, Rosenblatt J, Hanson K, Sloan L, et al. Evaluation of malaria screening in Liberian refugees by blood smear and rapid antigen capture assay (Binax (TM)). Preliminary results. American Journal of Tropical Medicine and Hygiene 2005;73:603. [Google Scholar]
Stauffer 2006 {published data only}
- Stauffer WM, Newberry AM, Cartwright CP, Rosenblatt JE, Hanson KL, Sloan L, et al. Evaluation of malaria screening in newly arrived refugees to the United States by microscopy and rapid antigen capture enzyme assay. Pediatric Infectious Disease Journal 2006;25(10):948‐50. [DOI] [PubMed] [Google Scholar]
Stauffer 2009 {published data only}
- Stauffer WM, Cartwright CP, Olson DA, Juni BA, Taylor CM, Bowers, et al. Diagnostic performance of rapid diagnostic tests versus blood smears for malaria in US clinical practice. Clinical Infectious Diseases 2009;49(6):908‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sturenburg 2009 {published data only}
- Sturenburg E, Junker R. Point‐of‐care testing in microbiology: the advantages and disadvantages of immunochromatographic test strips. Deutsches Arzteblatt International 2009;106(4):48‐54. [DOI] [PMC free article] [PubMed] [Google Scholar]
Susi 2005 {published data only}
- Susi B, Whitman T, Blazes DL, Burgess TH, Martin GJ, Freilich D. Rapid diagnostic test for Plasmodium falciparum in 32 Marines medically evacuated from Liberia with a febrile illness. Annals of Internal Medicine 2005;142:476‐7. [DOI] [PubMed] [Google Scholar]
Swarthout 2007 {published data only}
- Swarthout TD, Counihan H, Senga RK, Broek I. Paracheck‐Pf accuracy and recently treated Plasmodium falciparum infections: is there a risk of over‐diagnosis?. Malaria Journal 2007;6:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tagbor 2008 {published data only}
- Tagbor H, Bruce J, Browne E, Greenwood B, Chandramohan D. Performance of the OptiMAL dipstick in the diagnosis of malaria infection in pregnancy. Therapeutics and Clinical Risk Management 2008;4(3):631‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tarazona 2004 {published data only}
- Tarazona AS, Zerpa LS, Requena DM, Llano‐Cuentas A, Magill A. Evaluation of the rapid diagnostic test OptiMAL for diagnosis of malaria due to Plasmodium vivax. Brazilian Journal of Infectious Diseases 2004;8(2):151‐5. [DOI] [PubMed] [Google Scholar]
Tarimo 1999 {published data only}
- Tarimo DS, Moshiro C, Mpembeni R, Minjas JN. Field trial of the direct acridine orange method and ParaSight‐F test for the rapid diagnosis of malaria at district hospitals in Dar es Salaam, Tanzania. Transactions of the Royal Society of Tropical Medicine and Hygiene 1999;93(5):521‐2. [DOI] [PubMed] [Google Scholar]
Tarimo 2001 {published data only}
- Tarimo DS, Minjas JN, Bygberg IC. Malaria diagnosis and treatment under the strategy of the integrated management of childhood illness (IMCI): relevance of laboratory support from the rapid immunochromatographic tests of ICT Malaria P.f/P.v and OptiMAL. Annals of Tropical Medicine and Parasitology 2001;95(5):437‐44. [DOI] [PubMed] [Google Scholar]
Taylor 2002 {published data only}
- Taylor WRJ, Widjaja H, Basri H, Fryauff DJ, Ohrt CT, Tjitra E, et al. Assessing the ParaSight F test in Northeastern Papua, Indonesia, an area of mixed Plasmodium falciparum and Plasmodium vivax transmission. American Journal of Tropical Medicine and Hygiene 2002;66:649‐52. [DOI] [PubMed] [Google Scholar]
Tham 1999 {published data only}
- Tham JM, Lee SH, Tan TM, Ting RC, Kara UA. Detection and species determination of malaria parasites by PCR: comparison with microscopy and with ParaSight‐F and ICT malaria Pf tests in a clinical environment. Journal of Clinical Microbiology 1999;37:1269‐73. [DOI] [PMC free article] [PubMed] [Google Scholar]
Thepsamarn 1997 {published data only}
- Thepsamarn P, Prayoollawongsa N, Puksupa P, Puttoom P, Thaidumrong P, Wongchai S, et al. The ICT Malaria Pf: a simple, rapid dipstick test for the diagnosis of Plasmodium falciparum malaria at the Thai‐Myanmar border. South East Asian Journal of Tropical Medicine and Public Health 1997;28:723‐6. [PubMed] [Google Scholar]
Tietche 1996 {published data only}
- Tietche F, Teguia S, Tetanye E, Louis FJ, Mbonda E, Epee MF. [Diagnostic presomptif d'acces palustre et positivite de la goutte epaisse chez l'enfant de 0 a 5 ans a Yaounde (Cameroun)]. Medecine d'Afrique Noire 1996;43(6):318‐21. [Google Scholar]
Tjitra 2001a {published data only}
- Tjitra E, Suprianto S, Dyer ME, Currie BJ, Anstey NM. Detection of histidine rich protein 2 and panmalarial ICT Malaria Pf/Pv test antigens after chloroquine treatment of uncomplicated malaria does not reliably predict treatment outcome in eastern Indonesia. American Journal of Tropical Medicine and Hygiene 2001;65(5):593‐8. [DOI] [PubMed] [Google Scholar]
Tjitra 2001b {published data only}
- Tjitra A, Suprianto S, McBroom J, Currie BJ, Anstey NM. Persistent ICT malaria P.f/P.v. panmalarial and HRP2 antigen reactivity after treatment of Plasmodium falciparum malaria is associated with gametocytemia and results in false‐positive diagnoses of Plasmodium vivax in convalescence. Journal of Clinical Microbiology 2001;39(3):1025‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Trachsler 1999 {published data only}
- Trachsler M, Schlagenhauf P, Steffen R. Feasibility of a rapid dipstick antigen‐capture assay for self‐testing of travellers' malaria. Tropical Medicine and International Health 1999;4(6):442‐7. [DOI] [PubMed] [Google Scholar]
Uguen 1995 {published data only}
- Uguen C, Rabodonirina M, Pina JJ, Vigier JP, Martet G, Maret M, et al. ParaSight‐F rapid manual diagnostic test of Plasmodium falciparum infection. Bulletin of the World Health Organization 1995;73(5):643‐9. [PMC free article] [PubMed] [Google Scholar]
Uneke 2008 {published data only}
- Uneke CJ, Lyare FE, Oke P, Duhlinska DD. Assessment of malaria in pregnancy using rapid diagnostic tests and its association with HIV infection and hematologic parameters in South‐Eastern Nigeria. Haematologica 2008;93(1):143‐4. [DOI] [PubMed] [Google Scholar]
Uneke 2008a {published data only}
- Uneke CJ. Diagnosis of Plasmodium falciparum malaria in pregnancy in sub‐Saharan Africa: the challenges and public health implications. Parasitology Research 2008;102(3):333‐42. [DOI] [PubMed] [Google Scholar]
Uzuchukwu 2009 {published data only}
- Uzuchukwu BSC, Obikeze EN, Onwujekwe OE, Onoka CA, Griffiths UK. Cost‐effectiveness analysis of rapid diagnostic test, microscopy and syndromic approach in the diagnosis of malaria in Nigeria: implications for scaling‐up deployment of ACT. Malaria Journal 2009;8:265. [DOI] [PMC free article] [PubMed] [Google Scholar]
Valea 2009 {published data only}
- Valea I, Tinto H, Nikiema M, Yamuah L, Rouamba N, Drabo M, et al. Performance of OptiMAL compared to microscopy, for malaria detection in Burkina Faso. Tropical Medicine and International Health 2009;14(3):338‐40. [DOI] [PubMed] [Google Scholar]
Valecha 1998 {published data only}
- Valecha N, Sharma VP, Devi CU. A rapid immunochromatographic Test (ICT) for Diagnosis of Plasmodium falciparum. Diagnostic Microbiology and Infectious DIseases 1998;30:257‐60. [DOI] [PubMed] [Google Scholar]
Valecha 2002 {published data only}
- Valecha N, Eapen A, Devi CU, Ravindran J, Aggarwal J, Ravindran J. Field evaluation of the ICT Malaria Pf/Pv immunochromatographic test in India. Annals of Tropical Medicine and Parasitology 2002;96(3):333‐6. [DOI] [PubMed] [Google Scholar]
Van den Ende 1998 {published data only}
- Ende J, Vervoort T, Gompel A, Lynen L. Evaluation of two tests based on the detection of histidine rich protein 2 for the diagnosis of imported Plasmodium falciparum malaria. Transactions of the Royal Society of Tropical Medicine and Hygiene 1998;92(3):285‐8. [DOI] [PubMed] [Google Scholar]
Van der Palen 2009 {published data only}
- Palen M, Gillet P, Bottieau E, Cnops L, Esbroeck M, Jacobs J. Test characteristics of two rapid antigen detection tests (SD FK50 and SD FK60) for the diagnosis of malaria in returned travellers. Malaria Journal 2009;8:90. [DOI] [PMC free article] [PubMed] [Google Scholar]
Van Dijk 2009 {published data only}
- Dijk DP, Gillet P, Vlieghe E, Cnops L, Esbroeck M, Jacobs J. Evaluation of the Palutop+4 malaria rapid diagnostic test in a non‐endemic setting. Malaria Journal 2009;8:293. [DOI] [PMC free article] [PubMed] [Google Scholar]
Van Hellemond 2009 {published data only}
- Hellemond JJ, Rutten M, Koelewinj R, Zeeman AM, Verweij JJ, Wismans PJ, et al. Human Plasmodium knowlesi infection detected by rapid diagnostic tests for malaria. Emerging Infectious Diseases Journal 2009;15(9):1578‐80. [DOI] [PMC free article] [PubMed] [Google Scholar]
VanderJagt 2005 {published data only}
- VanderJagt TA, Ikeh EI, Ujah IOA, Belmonte J, Glew RH, VanderJagt DJ. Short communication: Comparison of the OptiMAL rapid test and microscopy for detection of malaria in pregnant women in Nigeria. Tropical Medicine and International Health 2005;10(1):39‐41. [DOI] [PubMed] [Google Scholar]
Venkatesh 2007 {published data only}
- Venkatesh V, Patibandla PK, Agarwal GG, Awasthi S, Ahuja RC, Nag VL. Performance characteristics of a rapid diagnostic test for malaria, when used to confirm cerebral malaria in children and young adults. Annals of Tropical Medicine and Parasitology 2007;101(1):85‐7. [DOI] [PubMed] [Google Scholar]
Voller 1993 {published data only}
- Voller A. Immunoassays for tropical parasitic infections. Transactions of the Royal Society of Tropical Medicine and Hygiene 1993;87:497‐8. [DOI] [PubMed] [Google Scholar]
Waltz 2007 {published data only}
- Waltz E. Practical malaria tests promise results in remote regions. Nature Medicine 2007;13:6. [DOI] [PubMed] [Google Scholar]
Wang J‐Y 2007 {published data only}
- Wang J‐Y, Shi F, Yang Y‐T, Gao C‐H, Bao Y‐F, Tang L‐H. Establishment and evaluation of colloid gold labelled immunochromatographic strip tests for rapid diagnosis of malaria. Chinese Journal of Parasitological Diseases 2007;25(5):415‐8. [PubMed] [Google Scholar]
Wanji 2008 {published data only}
- Wanji S, Kimbi HK, Eyong JE, Tendongfor N, Ndamukong JL. Performance and usefulness of the Hexagon rapid diagnostic test in children with asymptomatic malaria living in the Mount Cameroon region. Malaria Journal 2008;7:89. [DOI] [PMC free article] [PubMed] [Google Scholar]
WHO 1996 {published data only}
- World Health Organization. A rapid dipstick antigen capture assay for the diagnosis of falciparum malaria. Bulletin of the World Health Organization 1996;74(1):47‐54. [PMC free article] [PubMed] [Google Scholar]
Wiese 2006 {published data only}
- Wiese L, Bruun B, Baek L, Friis‐Moller A, Gahrn‐Hansen B, Hansen J, et al. Bedside diagnosis of imported malaria using the Binax Now malaria antigen detection test. Scandinavian Journal of Infectious Diseases 2006;38(11‐12):1063‐8. [DOI] [PubMed] [Google Scholar]
Williams 2008 {published data only}
- Williams HA, Causer L, Metta E, Malila A, O'Reilly T, Abdulla S, et al. Dispensary level pilot implementation of rapid diagnostic tests: an evaluation of RDT acceptance and usage by providers and patients; Tanzania, 2005. Malaria Journal 2005;7:239. [DOI] [PMC free article] [PubMed] [Google Scholar]
Win 2001 {published data only}
- Win TT, Tantular IS, Pusarawati S, Kerong H, Lin K, Matsuoka H, et al. Detection of Plasmodium ovale by the ICT malaria Pf/Pv rapid diagnostic test. Acta Tropica 2001;80:283‐4. [DOI] [PubMed] [Google Scholar]
Wongsrichanalai 2001 {published data only}
- Wongsrichanalai C. Rapid diagnostic techniques for malaria control. Trends in Parasitology 2001;17(7):307‐9. [DOI] [PubMed] [Google Scholar]
Wongsrichanalai 2007 {published data only}
- Wongsrichanalai C, Barcus MJ, Muth S, Sutamihardja A, Wernsdorfer WH. A review of malaria diagnostic tools: microscopy and rapid diagnostic test (RDT). American Journal of Tropical Medicine and Hygiene 2007;77(6 suppl):119‐27. [PubMed] [Google Scholar]
Wu 2005 {published data only}
- Wu Y‐S, Lei L‐M, Li M. Evaluation of a parasite lactate dehydrogenase‐based colloid gold‐immunochromatography assay for diagnosis of Plasmodium falciparum. Journal of the First Military Medical University 2005;25(7):761‐5. [PubMed] [Google Scholar]
Yavo 2002 {published data only}
- Yavo W, Ackra KN, Menan EIH, Barro‐Kiki PC, Kassi RR, Adjetey TAK. Comparative study of four techniques used in Cote d'Ivoire for malaria's biological diagnosis. Bulletin de la Societe de Pathologie Exotique 2002;95(4):238‐40. [PubMed] [Google Scholar]
Zakai 2003 {published data only}
- Zakai HA. Methods used in the diagnosis of malaria: where do we stand?. Journal of the Egyptian Society of Parasitology 2003;33(3):979‐90. [PubMed] [Google Scholar]
Zerpa 2007 {published data only}
- Zerpa N, Pabo R, Wide A, Gavidia M, Medina M, Cacere JL. Evaluation of the OptiMAL test for diagnosis of malaria in Venezuela. Investigacion Clinica 2007;49(1):93‐101. [PubMed] [Google Scholar]
Zheng 1999 {published data only}
- Zengh X, Tang L, Xu Y, Meng F, Zhu W, Gu Z, et al. Evaluation of immunochromatographic test in the diagnosis of Plasmodium falciparum and Plasmodium vivax malaria. Chinese Journal of Parasitology and Parasitological Diseases 1999;17(4):234‐6. [PubMed] [Google Scholar]
Zhu 1998 {published data only}
- Zhu W, Tang L, Zheng X, Luo M, Gu Z, Qian H, et al. Diagnosis of falciparum malaria by immunochromatographic test . Chinese Journal of Parasitology and Parasitological Diseases 1998;16(2):94‐6. [PubMed] [Google Scholar]
Zikusooka 2008 {published data only}
- Zikusooka CM, McIntyre D, Barnes KI. Should countries implementing an artemisinin‐based combination malaria treatment policy also introduce rapid diagnostic tests?. Malaria Journal 2008;7:176. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zurovac 2008 {published data only}
- Zurovac D, Larson BA, Skarbinski J, Slutsker L, Snow RW, Hamel MJ. Modeling the financial and clinical implications of malaria rapid diagnostic tests in the case‐management of older children and adults in Kenya. American Journal of Tropical Medicine and Hygiene 2008;78(6):884‐91. [PMC free article] [PubMed] [Google Scholar]
Additional references
Bell 2006
- Bell D, Wongsrichanalai C, Barnwell JW. Evaluating diagnostics: ensuring quality and access for malaria diagnosis: how can it be achieved?. Nature Reviews Microbiology September 2006;4:S7‐S20. [DOI: 10.1038/nrmicro1525] [DOI] [PubMed] [Google Scholar]
Bossuyt 2003
- Bossuyt PM, Reitsma JB, Bruns DE, Gatsonis PP, Glasziou PP, Irwig LM, et al. Standards for reporting of diagnostic accuracy. Towards complete and accurate reporting of studies of diagnostic test accuracy: the STARD initiative. British Medical Journal 2003;326:41‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cruciani 2004
- Cruciani M, Nardi S, Malena M, Bosco O, Serpelloni G, Mengoli C. Systematic review of the accuracy of the ParaSight‐F tests in the diagnosis of Plasmodium falciparum malaria. Medical Science Monitor: International Medical Journal of Experimental and Clinical Research 2004;10(7):MT81‐8. [PubMed] [Google Scholar]
Gilles 1991
- Gilles HM. Management of severe malaria: a practical handbook. Second edition. Geneva: World Health Organization, 2000. [Google Scholar]
Hanscheid 2002
- Hanscheid T, Grobusch MP. How useful is PCR in the diagnosis of malaria?. Trends in Parasitology 2002;18(9):395‐8. [DOI] [PubMed] [Google Scholar]
Hawkes 2009
- Hawkes M, Katsuva JP, Musambuko CL. Use and limitations of malaria rapid diagnostic testing by community health workers in war‐torn Democratic Republic of Congo. Malaria Journal 2009;8:308. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hay 2008
- Hay SI, Smith DL, Snow RW. Measuring malaria endemicity from intense to interrupted transmission. The Lancet Infectious Diseases 2008;8:369‐78. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hay 2009
- Hay SI, Guerra CA, Gething PW, Patil AP, Tatem AJ, Noor AM. A world malaria map: Plasmodium falciparum endemicity in 2007. PLoS Medicine 2009; Vol. 6, issue 3:e1000048. [DOI] [PMC free article] [PubMed]
Kakkilaya 2003
- Kakkilaya BS. Rapid diagnosis of malaria. Laboratory Medicine 2003;34:602‐8. [Google Scholar]
Lengeler 2004
- Lengeler C. Insecticide‐treated bed nets and curtains for preventing malaria. Cochrane Database of Systematic Reviews 2004, Issue Issue 2. Art. No.: CD000363. [DOI: 10.1002/14651858] [DOI] [PubMed] [Google Scholar]
Marx 2005
- Marx A, Pewsner D, Egger M, Nuesch R, Heiner C, Bucher MD, et al. Meta‐analysis: Accuracy of rapid tests for malaria in travellers returning from endemic areas. Annals of Internal Medicine 2005;142:836‐46. [DOI] [PubMed] [Google Scholar]
May 1999
- May J, Mockenhaupt FP, Ademowo OG, Falusi AG, Olumese PE, Bienzle U, et al. High rate of mixed and subpatent malarial infections in Southwest Nigeria. American Journal of Tropical Medicine and Hygiene 1999;61(2):339‐43. [DOI] [PubMed] [Google Scholar]
Odaga 2011
- Odaga J, Lokong JA. Rapid Diagnostic Tests versus clinical diagnosis for treating malaria. Cochrane Database of Systematic Reviews 2011, Issue 2. DOI: 10.1002/14651858.CD008998. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sinclair 2009
- Sinclair D, Zani B, Bukirwa H, Donegan S, Olliaro O, Garner P. Artemisinin‐based combination therapy for treating uncomplicated malaria. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007483.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Smidt 2008
- Smidt N, Deeks J, Moore T. Chapter 4: Guide to the contents of a Cochrane review and protocol. The Cochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy (Version 0.4) [Updated September 2008]. The Cochrane Collaboration, 2008. [Google Scholar]
Snounou 1993
- Snounou G, Viriyakasol S, Zhu XP, Jarra W, Pinheiro L, do Rosario VE, et al. High sensitivity of detection of human malaria parasites by the use of nested polymerase chain reaction. Molecular Biochemistry and Parasitology 1993;61:315‐20. [DOI] [PubMed] [Google Scholar]
Talman 2007
- Talman AM, Duval L, Legrans E, Hubert V, Yen S, Bell B, et al. Evaluation of the intra and inter‐specific genetic variability of Plasmodium lactate dehydrogenase. Malaria Journal October 2007;6:140. [DOI: 10.1186/1475-2875-6-140] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tavrow 2000
- Tavrow P, Knebel E, Cogswell L. Using quality design to improve malaria rapid diagnostic tests in Malawi. Published for the United States Agency for International Development (USAID) by the Quality Assurance Project (QAP); Bethesda, Maryland 2000; Vol. Operations Research Results 1(4).
Whiting 2003
- Whiting P, Rutjes AWS, Reitsma JB, Bossuyt PMM, Kleinjen J. The development of QUADAS: a tool for the quality assessment of studies of diagnostic test accuracy included in systematic reviews. BMC Medical Research Methodology 2003;3(25):DOI: 10.1186/1471‐2288‐3‐25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Whiting 2009
- Whiting P, Westwood M, Burke M, Sterne J, Glanville J. Systematic reviews of test accuracy should search a range of databases to identify primary studies. Journal of Clinical Epidemiology 2009;61(4):357. [DOI] [PubMed] [Google Scholar]
WHO 2003
- World Health Organization. Malaria rapid diagnosis: making it work: World Health Organization meeting report 20‐23 January Manila. Geneva: World Health Organization, 2003. [Google Scholar]
WHO 2005
- World Health Organization. Prevention and control of malaria. Strategic orientation paper. Geneva: World Health Organization, 2005. [Google Scholar]
WHO 2006
- World Health Organization. Towards quality testing of malaria rapid diagnostic tests: evidence and methods. Proceedings of the WHO Informal Consultation on development and methods for testing malaria rapid diagnostic tests 28 February ‐ 2 March 2006. Geneva: World Health Organization, 2006. [Google Scholar]
WHO 2009
- World Health Organization. List of known commercially‐available antigen‐detecting malaria RDTs: Information for national public health services and UN Agencies wishing to procure RDTs. http://www.wpro.who.int/NR/rdonlyres/990245C0‐F157‐417A‐90C7‐B08A7E1A50BA/0/TotallistofISO131485criteria_Rev_24MAR09.pdf 2009.
WHO 2009a
- World Health Organization. World Malaria Report 2009. Geneva: World Health Organization, 2009. [Google Scholar]
WHO 2010
- World Health Organization. Guidelines for the treatment of malaria. Guidelines for the treatment of malaria (2nd edition). Geneva: World Health Organization, 2010. [Google Scholar]
WHO 2010a
- World Health Organization. Malaria rapid diagnostic test performance: results of the WHO product testing of malaria RDTs: Round 1 (2008). Malaria rapid diagnostic test performance: results of WHO product testing of malaria RDTs: Round 2 (2009). Geneva: World Health Organization on behalf of the Special Programme for Research and Training in Tropical Diseases (TDR), 2010. [Google Scholar]
Wongsrichalanai 2007
- Wongsrichalanai C, Barcus MJ, Muth S, Sutamihardja, Wernsdorfer WH. A review of malaria diagnostic tools: microscopy and rapid diagnostic test (RDT). American Journal of Tropical Medicine and Hygiene 2007;77(Suppl 6):119‐27. [PubMed] [Google Scholar]


