Abstract
Background
Neurocysticercosis is an infection of the brain by the larval stage of the pork tapeworm. In endemic areas it is a common cause of epilepsy. Anthelmintics (albendazole or praziquantel) may be given to kill the parasites. However, there are potential adverse effects, and the parasites may eventually die without treatment.
Objectives
To assess the effectiveness and safety of anthelmintics for people with neurocysticercosis.
Search methods
In May 2009 we searched the Cochrane Infectious Diseases Group Specialized Register, CENTRAL (The Cochrane Library 2009, Issue 2), MEDLINE, EMBASE, LILACS, and the mRCT.
Selection criteria
Randomized controlled trials comparing anthelmintics with placebo, no anthelmintic, or other anthelmintic regimen for people with neurocysticercosis.
Data collection and analysis
Two authors independently selected trials, extracted data, and assessed each trial's risk of bias. We calculated risk ratios (RR) for dichotomous variables, with 95% confidence intervals (CI). We pooled data from trials with similar interventions and outcomes.
Main results
For viable lesions in children, there were no trials. For viable lesions in adults, no difference was detected for albendazole compared with no treatment for recurrence of seizures (116 participants, one trial); but fewer participants with albendazole had lesions at follow up (RR 0.56, 95% CI 0.45 to 0.70; 192 participants, two trials).
For non‐viable lesions in children, seizures recurrence was less common with albendazole compared with no treatment (RR 0.49, 95% CI 0.32 to 0.75; 329 participants, four trials). There was no difference detected in the persistence of lesions at follow up (570 participants, six trials). For non‐viable lesions in adults, there were no trials.
In trials including viable, non‐viable or mixed lesions (in both children and adults), headaches were more common with albendazole alone (RR 9.49, 95% CI 1.40 to 64.45; 106 participants, two trials), but no difference was detected in one trial giving albendazole with corticosteroids (116 participants, one trial).
Authors' conclusions
In patients with viable lesions, evidence from trials of adults suggests albendazole may reduce the number of lesions. In trials of non‐viable lesions, seizure recurrence was substantially lower with albendazole, which is counter‐intuitive. It may be that steroids influence headache during treatment, but further research is needed to test this.
22 March 2019
Update pending
Authors currently updating
The update is due to be published in 2019.
Plain language summary
Treatment for illness caused by tapeworm larvae in the brain
If people eat eggs from the pork tapeworm (Taenia solium), these eggs can move from the gut and then lodge in different tissues of the body forming cysts. When these cysts form in the brain, this is called neurocysticercosis. Some people may have no symptoms if this happens, but others may suffer from seizures, headaches, or more rarely from confusion, loss of balance or brain swelling. More rarely still, someone may die.
The condition is mainly found where people live in close contact with pigs and where the sanitation is poor. It affects around 50 million people worldwide, and in some areas is the leading cause of adult‐onset epilepsy.
The number, size and location of the cysts help to guide treatment of neurocysticercosis, as do the patient’s symptoms; for example, giving anticonvulsants to someone with seizures. Two drugs, praziquantel and albendazole, can be used specifically in neurocysticercosis to help kill the parasite; these drugs are known as anthelmintics. Some cysts, called non‐viable lesions are generally in the process of degenerating and resolving spontaneously; many experts recommend not treating this type of cyst. However, treating viable lesions (ie those lesions that may or may not resolve spontaneously) with these drugs may help kill the parasite, although treatment remains controversial due to the potential side effects and the fact the parasite may die without treatment.
In this review of 21 relevant randomized controlled trials, most studies examined the effects of albendazole. In patients with viable lesions, there is only evidence available for adult patients; this suggests that albendazole may reduce the number of lesions. In patients with non‐viable lesions, there is only evidence available for children; this suggests that seizure recurrence was lower with albendazole, which goes against the opinions of some experts. There is insufficient evidence available to assess praziquantel.
Background
Neurocysticercosis is an infection of the central nervous system by the larval stage of the pork tapewormTaenia solium. If eggs (cysticerci) from the faeces of humans infected with the intestinal parasites are ingested, they can migrate from the gut to lodge in various tissues of the body, where they form cysts (cysticercosis). This review is confined to treating neurocysticercosis, where the cysts lodge in the brain.
The cysts naturally evolve, over a period of years, through stages beginning with viable larvae and ending with the death of the parasite and resorption or calcification of the cyst. Individuals may have one or more cysticerci in the brain. The following types of neurocysticercosis have been recognized, depending on where the cysts are lodged: parenchymal; intraventricular; racemose type found in the basal cisterns; and spinal. Symptoms may or may not occur, depending on the number, location, and stage of the cysts, as well as the infected person's immune response. Seizures are the most common symptom, present in most of the presenting cases, followed by headaches. Rarely, it causes confusion, lack of attention to people and surroundings, difficulty with balance, paralysis, swelling of the brain, and very rarely, death. Symptoms may be associated with the host's immune response or due to calcifications left once the cysts have been eliminated (Leite 2000).
The condition is found where people live in close contact with pigs and where sanitation is poor. It is common in much of South and Central America, China, the Indian subcontinent and South‐East Asia, and sub‐Saharan Africa. It affects around 50 million people worldwide (Kossoff 2005), with men and women equally affected, and has a peak of incidence at the ages of 30 to 40 years (Burneo 2005). In endemic areas, it is the leading cause of adult‐onset epilepsy and an important cause of seizures in children (Roman 2000). It has also been estimated to cause at least 50,000 deaths worldwide each year (Roman 2000). It is therefore a significant public health problem, with significant associated costs in health care and lost productivity.
The cysts in the brain can be visualized using CT or MRI scanning. Over the course of the infection, radiological images change from 'non‐enhancing' (after intravenous injection of a radiographic contrast), indicating a viable cyst with little host immune response, to 'ring‐enhancing' indicating a degenerating cyst with surrounding immune response, to calcification or total resolution (DeGiorgio 2004). Cysts may be located in the parenchyma (brain tissue) or within structures and spaces around the brain (extraparenchymal cysts). Infection burden varies widely; a recently published guideline classified infection burdens from mild (one to five cysts) to moderate (five to 99 cysts) to heavy (more than 100 cysts) (Garcia 2002).
Treatment options depend on the number, size, and location of the cysts, and on the symptoms. Initial symptomatic treatment includes anticonvulsant drugs for seizures and analgesics for headache. Some extraparenchymal cysts are treated with surgery, either to remove the cyst or to relieve intracranial pressure. Where serious inflammation of the brain is present (usually associated with degeneration of the cysts), corticosteroids may be prescribed.
Cysts may degenerate and resolve spontaneously. For this reason, specific anthelmintics are usually considered for people with viable cysts, as the treatment may help kill the parasites. When lesions are non‐viable, many experts do not recommend these drugs.
There are two anthelmintics used in neurocysticercosis: praziquantel, available since 1979, and albendazole, available since 1987. If anthelmintics are used, corticosteroids are often prescribed with them to prevent inflammation of the brain caused by the host immune response to the destroyed parasites.
Treatment with anthelmintics remains controversial, due to potential adverse events and the natural history of the parasite, which may eventually die without treatment. The original version of this Cochrane Review found no evidence that the potential benefits of treatment outweigh the potential harms (Salinas 1999). This review was undertaken as a substantive update of the original Cochrane Review to take trials published since 1999 into account. We have stratified patients by age (children and adult) and by whether patients have predominantly viable or non‐viable cysts, given the natural history and assumptions about when anthelmintics may or may not be effective.
Objectives
To assess the effects of anthelmintics for people with neurocysticercosis.
Methods
Criteria for considering studies for this review
Types of studies
Randomized controlled trials.
Types of participants
People with symptomatic or asymptomatic neurocysticercosis defined by viable or non‐viable lesions in the brain, identified as 'non‐enhancing' or 'ring‐enhancing' on medical imaging..
Types of interventions
Intervention
Anthelmintics plus usual treatment.
Anthelmintics plus corticosteroids plus usual treatment.
Control
Usual treatment only.
Corticosteroids plus usual treatment.
Another anthelmintic plus usual treatment.
Another dose or duration of anthelmintic, plus usual treatment.
We included trials irrespective of the type of anthelmintic used, or the dosage and duration of treatment.
Types of outcome measures
Primary
Free of seizures for one year after treatment.
Recurrence of seizures at follow‐up.
Number of seizures during follow‐up period.
Seizure free at follow‐up following withdrawal of anticonvulsant drugs.
Secondary
Health status indicators
All‐cause death.
Hospital admission for any cause.
Any neurological symptoms or signs (includes headache, paralysis, visual disturbance).
Need for surgery.
Resumption of normal activities at follow up; or time to resumption of normal activities.
Resolution of symptoms.
Radiological changes at follow up
Persistence of lesions.
Reduction in number of lesions.
Reduction in ventricular size.
Adverse events
Any adverse events.
Adverse event requiring withdrawal of anthelmintic drugs.
Search methods for identification of studies
We attempted to identify all relevant trials regardless of language or publication status (published or unpublished, in press, or in progress).
Databases
We searched the following databases using the search terms and strategy described in Appendix 1: the Cochrane Infectious Diseases Group Specialized Register (May 2009); the Cochrane Central Register of Controlled Trials (CENTRAL), published in The Cochrane Library (2009, Issue 2); MEDLINE (1966 to May 2009); EMBASE (1988 to May 2009); and LILACS (1982 to May 2009). We also searched the metaRegister of Controlled Trials (mRCT) using the term 'neurocysticercosis' May 2009).
Reference lists
We also checked the reference lists of all trials and review articles identified by the above method.
Data collection and analysis
Selection of studies
Two authors (KA and LR) independently screened all citations and abstracts, using an eligibility form to apply the selection criteria to identify relevant studies. Where there was uncertainty over the eligibility of a particular study, we obtained the full‐text article. We resolved any differences in opinion by discussion or, where necessary, by discussion with the third author (SR). We excluded studies that did not meet the criteria, and documented the reasons for exclusion in the table 'Characteristics of excluded studies'.
Data extraction and management
One author (KA) extracted data using a tailored data extraction form, and a second author (LR) checked this extracted data, after which any disagreements were resolved by discussion. We summarized data on study design, participant characteristics, interventions, and outcomes and entered these into Review Manager 5.
Assessment of risk of bias in included studies
Two review authors independently assessed the risk of bias of the included trials using a pro forma. In case of disagreement, we planned to consult a third person. We categorized the generation of the allocation sequence and allocation concealment as adequate, unclear, or inadequate as in Jüni 2001. We assessed whether the participants, care providers and investigators were blinded to which participants received which drug regimen. For all outcomes, we assessed that incomplete outcome data had been adequately addressed if 85% or more of the participants were included in the analysis, or if less than 85% were included but adequate steps were taken to ensure or demonstrate that this did not bias the results. We also examined the trial reports for any evidence of selective reporting of outcomes or any other issues that may bias the results. We reported the results of the assessment in a table.
Assessment of reporting biases
We planned to assess the probability of publication bias by examining the funnel plot for asymmetry, using one of the primary outcomes of seizure recurrence with the largest number of contributing trials. However, there were not enough trials reporting on the same primary outcomes to present a meaningful analysis.
Data synthesis
We analysed the data using Review Manager 5. We calculated risk ratio (RR) for dichotomous data and mean difference (MD) for continuous data. We measured precision using 95% confidence intervals (CI). Where more than one trial included similar participants and interventions, without significant clinical or methodological diversity or statistical heterogeneity, we undertook a meta‐analysis using a fixed‐effect model. Highly skewed data (where the standard deviation was greater than the mean) were presented in the text. Analyses were based on the number of available participants at each stage of follow up; there was no adjustment for loss to follow up.
We stratified the results by treatment comparison and type of lesion; viable (non‐enhancing) or non‐viable (enhancing).
Subgroup analysis and investigation of heterogeneity
We assessed heterogeneity between trials by examining the forest plot for overlapping confidence intervals, and using the I2 statistic for heterogeneity. We investigated potential sources of heterogeneity by performing subgroup analyses by co‐medications or treatments used and, where possible, length of follow up. We planned also to investigate potential sources of heterogeneity by performing subgroup analyses for participant age (adults or children), and number of lesions, but there were insufficient trials to enable this.
Sensitivity analysis
Where sufficient trial data were available, we undertook sensitivity analyses by excluding trials without adequate reported allocation concealment.
Results
Description of studies
Eligibility
We included 21 completed trials. (see 'Characteristics of included studies') We excluded nine studies (see reasons in 'Characteristics of excluded studies'). Three studies are classified as awaiting assessment because it was unclear from the reports whether or not they were randomized. We have emailed and written to the authors for more detailed information about the methods.The search also identified one ongoing trial that met the inclusion criteria (see 'Characteristics of ongoing studies').
In detail, the search strategy identified 48 potentially relevant reports of completed studies; of these, 35 initially seemed relevant, and we obtained the full texts. One was in Portuguese (Antoniuk 1991), the others in English. We obtained the help of a Portuguese reader to assess the relevant report for inclusion. Two reports were unclear as to whether the groups were randomly allocated: we attempted to contact the trial authors for clarification but were unsuccessful; these trials are reported as 'awaiting classification'. Following inspection of the reference lists of the included reports, we identified a further two relevant trials for inclusion (Padma 1994; Sotelo 1990), and another report that initially seemed relevant but did not meet the inclusion criteria (Medina 1993).
Trial location and setting
The included trials were conducted in Ecuador (five trials), Mexico (three trials), Peru (two trials), and India (11 trials). All were carried out within hospital settings, with treatment provided on an in‐patient basis.
Trial participants
Viable lesions
Six trials included 322 participants (151 males, 148 females, 23 sex not reported) with viable lesions, or a combination of viable and non‐viable lesions. Among these, four trials were conducted in adults (274 participants) and two trials included both children and adults (48 participants). Two trials did not specify the number of lesions, one trial included participants with up to three lesions, one trial with up to six lesions, and two trials with less than 20 lesions. All lesions in these studies were located in the parenchyma of the brain. None of the trials mentioned including or excluding people who were HIV positive.
Non‐viable lesions
Nine trials included 941 participants (44 males, 321 females and 176 sex not reported) with non‐viable lesions only. Among these, seven trials were conducted in children (763 participants) and two included both adults and children (178 participants). Six trials included only participants with single lesions, one trial included those with up to two lesions, one included those with up to three lesions, and one did not specify number of lesions. All lesions in these studies were located in the parenchyma of the brain. None of the trials mentioned including or excluding people who were HIV positive.
Mixed viable and non‐viable lesions
Seven trials included 676 participants (392 male, 280 female and four sex not reported) whose type of lesion was unspecified. Among these five trials were conducted in adults (469 participants) and two trials included both adults and children (207 participants). Five trials did not specify the number of lesions in each participant, while two trials included only participants with more than one lesion. Five trials included parenchymal lesions only, while one included only subarachnoid and intraventricular lesions and another included parenchymal, subarachnoid and intraventricular lesions. None of the trials mentioned including or excluding people who were HIV positive.
Interventions
Viable lesions
The comparisons included in the trials included:
Albendazole versus placebo or no drug (four trials) (Alarcon 1989; Garcia 1997; Alarcon 2001; Garcia 2004).
Albendazole versus praziquantel (two trials) (Sotelo 1990; Del Brutto 1999).
Albendazole: longer versus shorter duration of treatment (four trials) (Alarcon 1989; Sotelo 1990; Garcia 1997; Alarcon 2001).
Praziquantel: same daily dose given for different durations (one trial) (Sotelo 1990).
In addition to anthelmintics, three trials also used corticosteroids; two in all the comparison groups (Garcia 1997; Del Brutto 1999) and one in the treatment groups only (Garcia 2004). Most trials reported providing anticonvulsant drugs for all patients who were having seizures, whichever treatment group they were randomized to.
Non‐viable lesions
The comparisons included in the trials included:
Albendazole versus placebo or no drug (six trials) (Padma 1994; Baranwal 1998; Singhi 2000; Gogia 2003; Kalra 2003; De Souza 2009).
Albendazole plus praziquantel versus albendazole plus placebo (one trial) (Kaur 2009).
Albendazole: longer versus shorter duration of treatment (one trial) (Singhi 2003).
Albendazole with corticosteroids versus albendazole without corticosteroids (one trial) (Singhi 2004).
In addition to anthelmintics, five trials also used corticosteroids; three in the treatment and control groups (Baranwal 1998; Gogia 2003; Kaur 2009), one in the treatment groups only (Kalra 2003), and one in the control group and one of two intervention groups (Singhi 2004). Most trials reported providing anticonvulsant drugs for all patients who were having seizures, whichever treatment group they were randomized to.
Mixed viable and non‐viable lesions
The comparisons included in the trials included:
Albendazole versus placebo or no drug (five trials) (Sotelo 1988; Padma 1995; Garcia 1997; Das 2007; Carpio 2008).
Praziquantel versus placebo or no drug (one trial) (Sotelo 1988).
Albendazole versus praziquantel (one trial) (Sotelo 1988).
Albendazole: longer versus shorter duration of treatment (two trials) (Cruz 1995; Garcia 1997).
Albendazole: different doses given over a one‐day period (one trial) (Gongora‐Rivera 2006).
In addition to anthelmintics, five trials also used corticosteroids; three in the treatment and control groups (Garcia 1997; Gongora‐Rivera 2006; Carpio 2008), one in the treatment groups only (Das 2007), and one in the control group only (Sotelo 1988). Most trials reported providing anticonvulsant drugs for all patients who were having seizures, whichever treatment group they were randomized to.
One ongoing study is comparing albendazole plus corticosteroid with placebo (Gilman 2007).
Outcomes
Viable lesions
Three of the included trials reported outcomes relating to the presence or severity of seizures at follow up. A further trial reported on the presence or severity of any symptoms. All the trials reported on radiologically visible changes to the numbers or sizes of lesions.
Non‐viable lesions
Seven of the included trials reported outcomes relating to the presence or severity of seizures at follow up. All the trials reported on radiologically visible changes to the numbers or sizes of lesions.
Mixed viable and non‐viable lesions
Three of the included trials reported outcomes relating to the presence or severity of seizures at follow up. A further two reported on the presence or severity of any symptoms. All the included trials reported on radiologically visible changes to the numbers or sizes of lesions.
There were no trials reporting on freedom from seizures for one year, resumption of normal activities, reduction in ventricular size, or adverse events requiring withdrawal of anthelmintic drugs.
Risk of bias in included studies
Details of the methods used in each trial are available in the table 'Characteristics of included studies'.
Generation of allocation sequence
Viable lesions
Two trials described an adequate method of generating a truly random allocation sequence. Four trials did not report how they generated group allocation sequences (assessed as 'unclear'), but all were described as 'randomized'.
Non‐viable lesions
Seven trials described an adequate method of generating a truly random allocation sequence. Two trials did not report how they generated group allocation sequences (assessed as 'unclear'), but all were described as 'randomized'.
Mixed viable and non‐viable lesions
Three trials described an adequate method of generating a truly random allocation sequence. Four trials did not report how they generated group allocation sequences (assessed as 'unclear'), but all were described as 'randomized'.
Allocation concealment
Viable lesions
One trial reported an adequate method of ensuring allocation concealment. Five trials did not report enough information to allow allocation concealment to be assessed.
Non‐viable lesions
Four trials reported an adequate method of ensuring allocation concealment. Five trials did not report enough information to allow allocation concealment to be assessed.
Mixed viable and non‐viable lesions
Two trials reported an adequate method of ensuring allocation concealment. Five trials did not report enough information to allow allocation concealment to be assessed.
Blinding
Viable lesions
Three trials reported blinding of participants, personnel and outcomes assessors for all main outcomes. It was unclear whether blinding was done for the other three trials.
Non‐viable lesions
Five trials reported blinding of participants, personnel and outcomes assessors for all main outcomes. It was unclear whether blinding was done for three trials. One trial did not use blinding.
Mixed viable and non‐viable lesions
Four trials reported blinding of participants, personnel and outcomes assessors for all main outcomes. It was unclear whether blinding was done for three trials.
Addressing incomplete outcomes data
Viable lesions
Five trials either included 85% or over of the participants in the analysis, or included fewer than 85% of participants, but showed that participants who were not included were similar to those included. One trial did not meet this criteria.
Non‐viable lesions
Six trials either included 85% or over of the participants in the analysis, or included fewer than 85% of participants, but showed that participants who were not included were similar to those included. Two trials did not meet this criteria, while in one trial this was unclear.
Mixed viable and non‐viable lesions
Seven trials either included 85% or over of the participants in the analysis, or included fewer than 85% of participants, but showed that participants who were not included were similar to those included.
Effects of interventions
1. Albendazole versus placebo or no drug
1.1. Recurrence of seizures
Viable lesions
One small trial with adequate allocation concealment, including adults only, reported on recurrence of seizures by end of follow up, showing no significant effect of albendazole treatment (116 participants, Analysis 1.1).
1.1. Analysis.
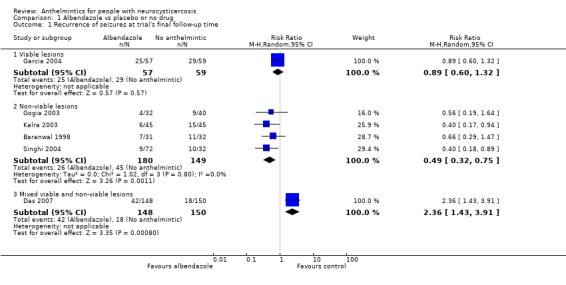
Comparison 1 Albendazole vs placebo or no drug, Outcome 1 Recurrence of seizures at trial's final follow‐up time.
Non‐viable lesions
Four trials reported data on this outcome that could be included within meta‐analysis. All four non‐viable lesions included only children with one or two lesions. Albendazole showed a significant benefit (relative risk 0.49, 95% confidence interval (CI) 0.32 to 0.75; 329 participants, Analysis 1.1). One of the included trials (Gogia 2003) excluded seizures occurring during the first week of the trial, but is included in the analysis because its exclusion did not change the finding. In a sensitivity analysis, including only the three trials with adequate allocation concealment, this significant benefit remained (RR 0.53, 95% CI 0.31 to 0.88; 125 participants). One additional trial (103 participants, De Souza 2009) reported no significant differences in seizure recurrence between the albendazole and no anthelmintic groups, but did not present data.
Mixed viable and non‐viable lesions
One trial, with unclear allocation concealment, reported on this outcome, showing a harmful effect of albendazole (RR 2.36, 95% CI 1.43 to 3.91; 298 participants, one trial, Analysis 1.1). Another trial, with adequate allocation concealment, presented data on the number of participants who remained free of seizures at 12 months, using Kaplan‐Meier survival analysis, and found no significant difference between the albendazole and placebo groups (Carpio 2008).
One trial reported on the successful withdrawal of anticonvulsants during a two‐year follow‐up period (Garcia 2004); there was no significant difference between the albendazole and control groups (116 participants, Analysis 1.2).
1.2. Analysis.
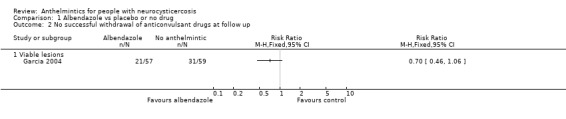
Comparison 1 Albendazole vs placebo or no drug, Outcome 2 No successful withdrawal of anticonvulsant drugs at follow up.
1.2. Deaths and hospital admissions
Viable lesions
No trials reported on these outcomes.
Non‐viable lesions
No trials reported on these outcomes.
Mixed viable and non‐viable lesions
Two trials reported a total of nine deaths (Analysis 1.3). There was no significant difference between albendazole and treatment groups in the number of deaths overall (470 participants, two trials).
1.3. Analysis.
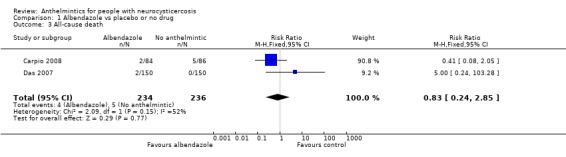
Comparison 1 Albendazole vs placebo or no drug, Outcome 3 All‐cause death.
One trial (Das 2007) reported on hospital re‐admissions after treatment (Analysis 1.4). Participants treated with albendazole had a higher risk of hospital admission during the periods up to three months (RR 2.53, 95% CI 1.54 to 4.17; 298 participants), three to six months (RR 5.07, 95% CI 2.17 to 11.82), and six to 12 months (RR 4.56, 95% CI 1.58 to 13.16). There was no significant difference between the albendazole and control groups during periods one to two years, two to three years, or three to four years.
1.4. Analysis.
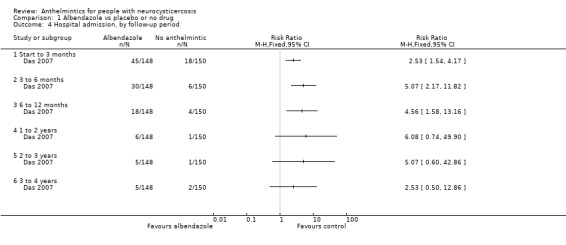
Comparison 1 Albendazole vs placebo or no drug, Outcome 4 Hospital admission, by follow‐up period.
1.3. Resolution of symptoms
Viable lesions
In one very small trial, fewer participants receiving albendazole had no resolution of symptoms ('symptom' not defined by the trial authors) at three months than in the control group (RR 0.25, 95% CI 0.07 to 0.93; 15 participants, Analysis 1.5).
1.5. Analysis.
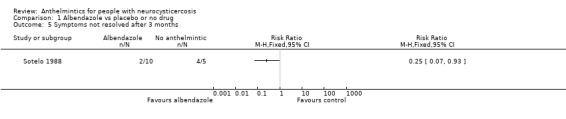
Comparison 1 Albendazole vs placebo or no drug, Outcome 5 Symptoms not resolved after 3 months.
Non‐viable lesions
No trials in non‐viable lesions reported on these outcomes.
Mixed viable and non‐viable lesions
One trial reported on presence of symptoms of encephalopathy (headache, vomiting, and altered sensorium) during different time periods. The albendazole group had a higher risk of symptoms during the period up to three months (RR 3.04, 95% CI 1.77 to 5.21; 298 participants, Analysis 1.6), but there was no significant difference between the groups during other periods of time up to four years.
1.6. Analysis.
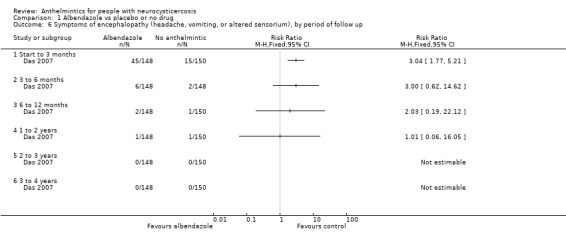
Comparison 1 Albendazole vs placebo or no drug, Outcome 6 Symptoms of encephalopathy (headache, vomiting, or altered sensorium), by period of follow up.
1.4. Persistence of radiological lesions
For the purposes of this review, persistence of lesions relates to the presence of cysts or lesions in any form, including calcified or nodular lesions.
Viable lesions
In trials including only adults with viable lesions, participants treated with albendazole compared with no anthelmintic had a lower risk of persistence of lesions at follow up (RR 0.56, 95% CI 0.45 to 0.70; 114 participants, two trials, Analysis 1.7)
1.7. Analysis.
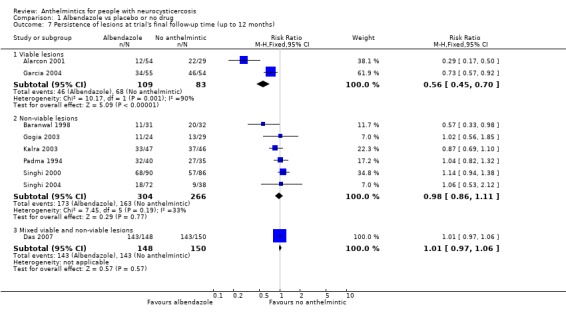
Comparison 1 Albendazole vs placebo or no drug, Outcome 7 Persistence of lesions at trial's final follow‐up time (up to 12 months).
Non‐viable lesions
In trials including mainly children with non‐viable lesions (one trial also included adults), there was no difference between the albendazole and no anthelmintic groups in persistence of lesions at follow up (570 participants, six trials, Analysis 1.7). A trial in adults and children (103 participants, De Souza 2009) reported no significant difference in cyst disappearance between the albendazole and no anthelmintic groups but did not present the data.
Mixed viable and non‐viable lesions
In one trial including adults with both viable and non‐viable lesions, there was no difference between the albendazole and no anthelmintic groups in persistence of lesions at follow up (298 participants, Analysis 1.7).
1.5. Adverse events during treatment
All types of lesion
There were no significant differences detected between the albendazole and no anthelmintic groups in the numbers of participants with headache during treatment in trials with viable lesions only (139 participants, two trials, Analysis 1.8), non‐viable lesions only (83 participants, one trial, Analysis 1.8), or mixed viable and non‐viable lesions (170 participants, one trial, Analysis 1.8). Overall, headache during treatment was more frequent in participants treated with albendazole than those not receiving anthelmintics (RR 1.37, 95% CI 1.08 to 1.73; 392 participants, four trials, Analysis 1.8).
1.8. Analysis.
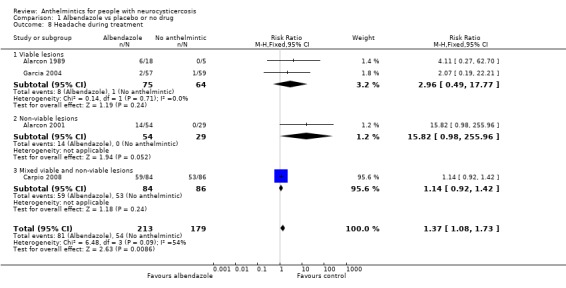
Comparison 1 Albendazole vs placebo or no drug, Outcome 8 Headache during treatment.
In a subgroup analysis by use of corticosteroids, there was a significant difference between the albendazole and no anthelmintic groups in headache during treatment when the albendazole group did not receive corticosteroids (RR 9.49, 95% CI 1.4 to 64.45; 106 participants, two trials, Analysis 1.9), but no significant difference in trials where participants in the albendazole group received corticosteroids.
1.9. Analysis.
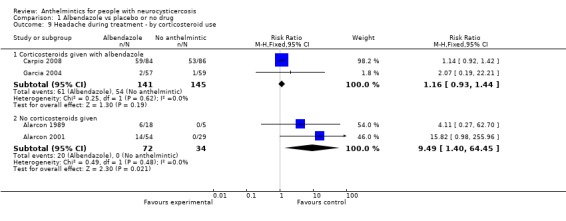
Comparison 1 Albendazole vs placebo or no drug, Outcome 9 Headache during treatment ‐ by corticosteroid use.
In analyses not separating trials by types of lesion, there was a greater risk of adverse events with albendazole for dizziness during treatment (Analysis 1.10), and nausea, vomiting and abdominal pain (Analysis 1.11). There was no significant difference between the albendazole and no anthelmintic groups in occurrence of seizures during treatment (455 participants, five trials, Analysis 1.12)
1.10. Analysis.
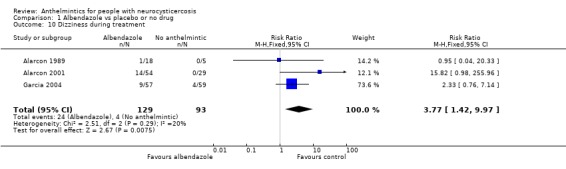
Comparison 1 Albendazole vs placebo or no drug, Outcome 10 Dizziness during treatment.
1.11. Analysis.
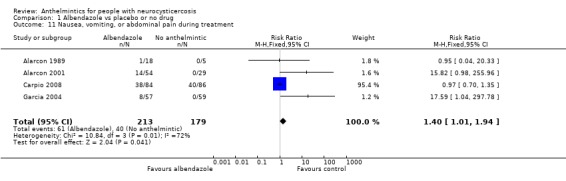
Comparison 1 Albendazole vs placebo or no drug, Outcome 11 Nausea, vomiting, or abdominal pain during treatment.
1.12. Analysis.
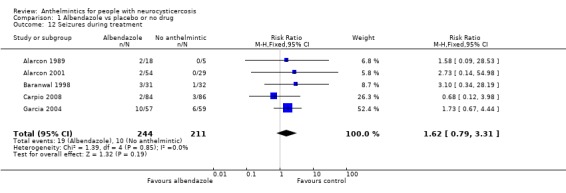
Comparison 1 Albendazole vs placebo or no drug, Outcome 12 Seizures during treatment.
2. Praziquantel versus placebo or no drug
One small trial made this comparison (15 participants, Sotelo 1988). The trial included participants with viable lesions, non‐viable lesions, or both. It did not report on recurrence of seizures, deaths or hospital admissions.
2.1. Resolution of symptoms
There was no significant difference between praziquantel and no anthelmintic for continuing presence of symptoms at three months (15 participants, Analysis 2.1).
2.1. Analysis.
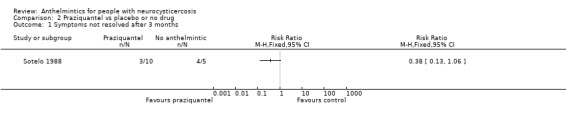
Comparison 2 Praziquantel vs placebo or no drug, Outcome 1 Symptoms not resolved after 3 months.
2.2. Radiological changes at follow up
There was a significant difference between praziquantel and no anthelmintic in persistence of lesions at follow up (RR 0.15, 95% CI 0.03 to 0.67, 15 participants, Analysis 2.2). More participants treated with praziquantel than no anthelmintic had a reduction in the number of lesions at three months follow up (RR 0.15, 95% CI 0.03 to 0.67; 15 participants, Analysis 2.3).
2.2. Analysis.
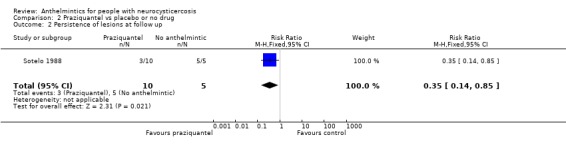
Comparison 2 Praziquantel vs placebo or no drug, Outcome 2 Persistence of lesions at follow up.
2.3. Analysis.
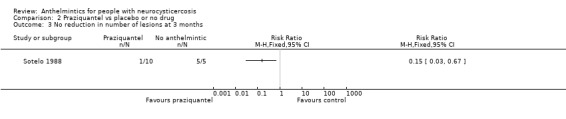
Comparison 2 Praziquantel vs placebo or no drug, Outcome 3 No reduction in number of lesions at 3 months.
2.3. Adverse events during treatment
More participants treated with praziquantel compared with no anthelmintic reported any adverse event during treatment, although the difference was not significant (15 participants, Analysis 2.4).
2.4. Analysis.
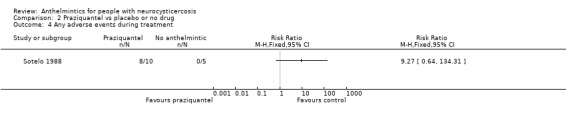
Comparison 2 Praziquantel vs placebo or no drug, Outcome 4 Any adverse events during treatment.
3. Albendazole versus praziquantel
Three trials reported on this comparison (Sotelo 1988; Sotelo 1990; Del Brutto 1999). All three trials included only participants with viable lesions.
3.1. Recurrence of seizures
In one small trial, there was no significant difference in the risk of recurrence of seizures with albendazole treatment compared with praziquantel (19 participants, Analysis 3.1).
3.1. Analysis.
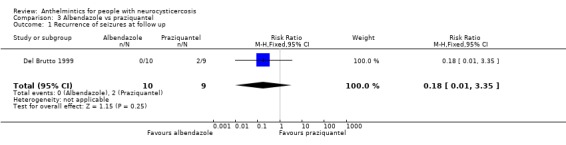
Comparison 3 Albendazole vs praziquantel, Outcome 1 Recurrence of seizures at follow up.
3.2. Resolution of symptoms
Fewer participants treated with albendazole compared with praziquantel still had symptoms of neurocysticercosis (types of symptoms not specified in the reports) three months after treatment (RR 0.58, 95% CI 0.36 to 0.92; 121 participants, two trials, Analysis 3.2).
3.2. Analysis.
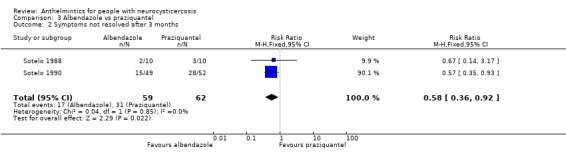
Comparison 3 Albendazole vs praziquantel, Outcome 2 Symptoms not resolved after 3 months.
3.3. Persistence of radiological lesions at follow up
There was a significant benefit of albendazole over praziquantel in the number of participants with persistence of lesions at follow up at three to six months (RR 0.64, 95% CI 0.45 to 0.91; 154 participants, three trials, Analysis 3.3).
3.3. Analysis.
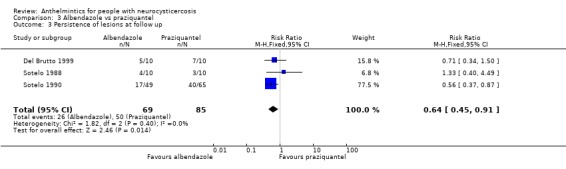
Comparison 3 Albendazole vs praziquantel, Outcome 3 Persistence of lesions at follow up.
Significantly fewer participants in the albendazole group had more lesions, or the same number of lesions, at follow up than before treatment (RR 0.41, 95% CI 0.19 to 0.92; 149 participants, three trials, Analysis 3.4).
3.4. Analysis.
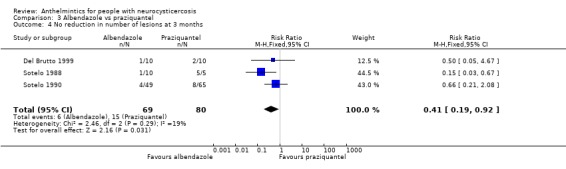
Comparison 3 Albendazole vs praziquantel, Outcome 4 No reduction in number of lesions at 3 months.
3.4. Adverse events during treatment
There were no significant differences between albendazole and praziquantel in the number of adverse events during treatment (Analysis 3.5).
3.5. Analysis.
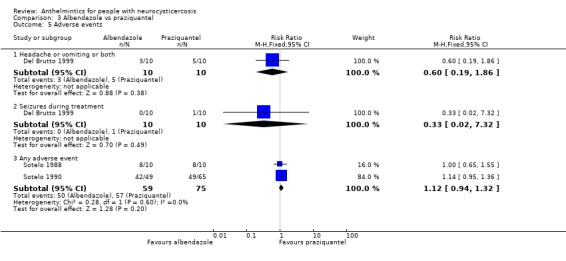
Comparison 3 Albendazole vs praziquantel, Outcome 5 Adverse events.
4. Albendazole combined with praziquantel versus albendazole alone
One trial, including only children with single non‐viable lesions, reported on this comparison.
4.1. Recurrence of seizures
There was no significant difference between the groups in recurrence of seizures at six months (112 participants, Analysis 4.1).
4.1. Analysis.
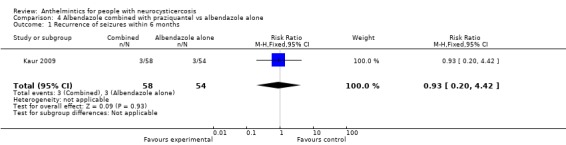
Comparison 4 Albendazole combined with praziquantel vs albendazole alone, Outcome 1 Recurrence of seizures within 6 months.
4.2 Persistence of radiological lesions
Albendazole combined with praziquantel was associated with lower risk of persistence of lesions at six months compared with albendazole alone (RR 0.59, 95% CI 0.35 to 0.99; 103 participants, Analysis 4.2). At one month and three months there was no significant difference between the groups, but there was a trend towards benefit of albendazole combined with praziquantel.
4.2. Analysis.
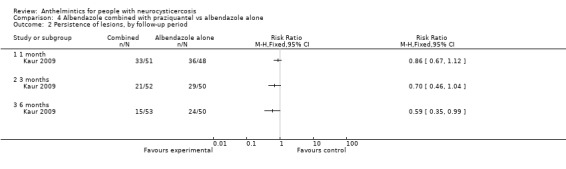
Comparison 4 Albendazole combined with praziquantel vs albendazole alone, Outcome 2 Persistence of lesions, by follow‐up period.
4.3 Adverse events
Three children receiving albendazole combined with praziquantel and two children receiving albendazole alone developed headache on day three to four of treatment lasting for one or two days. None reported any gastrointestinal symptoms. There were no signs of raised intracranial pressure and none of the children required withdrawal of drugs.
5. Albendazole: longer versus shorter duration of treatment
Six trials reported on this comparison (Alarcon 1989; Sotelo 1990; Cruz 1995; Garcia 1997; Alarcon 2001; Singhi 2003). This included three trials where participants had only viable lesions (Alarcon 1989; Sotelo 1990; Alarcon 2001), one trial including non‐viable lesions only (Singhi 2003), and two trials where participants had viable, non‐viable or both types of lesion (Cruz 1995; Garcia 1997).
5.1. Recurrence of seizures and resolution of symptoms
Viable lesions
One trial (Alarcon 2001) assessed the mean number of seizures at 12 months after treatment. The results were highly skewed, but there was no apparent difference between groups treated for eight days and groups treated for three days (54 participants, 0.3 (+/‐ 0.5) compared with 0.5 (+/‐1.0)).
One trial assessed the resolution of symptoms (not clearly defined in the trial report) three months after treatment. There was no difference between groups treated for up to eight days and more than eight days in the number of participants whose symptoms had not resolved (49 participants, Analysis 5.1).
5.1. Analysis.
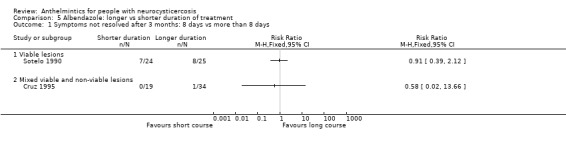
Comparison 5 Albendazole: longer vs shorter duration of treatment, Outcome 1 Symptoms not resolved after 3 months: 8 days vs more than 8 days.
Non‐viable lesions
No trials made this comparison.
Mixed viable and non‐viable lesions
One trial assessed the resolution of symptoms (not clearly defined in the trial report) three months after treatment. There was no difference between groups treated for up to eight days and more than eight days in the number of participants whose symptoms had not resolved (53 participants, Analysis 5.1).
5.2. Persistence of radiological lesions
Viable lesions
There was no significant difference in persistence of lesions at final follow up between groups receiving albendazole for seven or eight days and longer than seven or eight days (103 participants, two trials, Analysis 5.2). There was also no significant difference between groups given albendazole for three days or eight days (54 participants, one trial).
5.2. Analysis.
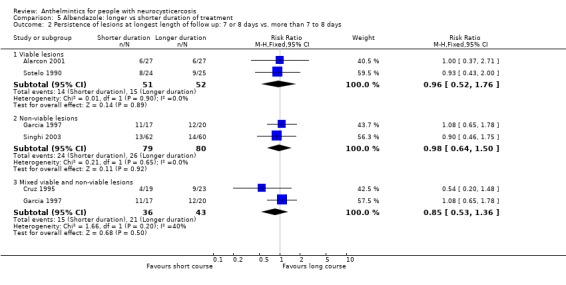
Comparison 5 Albendazole: longer vs shorter duration of treatment, Outcome 2 Persistence of lesions at longest length of follow up: 7 or 8 days vs. more than 7 to 8 days.
Non‐viable lesions
There was no significant difference in persistence of lesions at final follow up between groups receiving albendazole for seven or eight days and longer than seven or eight days (159 participants, two trials, Analysis 5.2).
Mixed viable and non‐viable lesions
There was no significant difference in persistence of lesions at final follow up between groups receiving albendazole for seven or eight days and longer than seven or eight days (79 participants, two trials, Analysis 5.2).
5.3. Adverse events
All types of lesion
In analyses not separating trials by type of lesion, participants receiving shorter treatment durations reported fewer cases of nausea or other gastrointestinal symptoms than those receiving longer treatments (RR 0.54, 95% CI 0.30 to 0.97; 244 participants, four trials, Analysis 5.4).
5.4. Analysis.
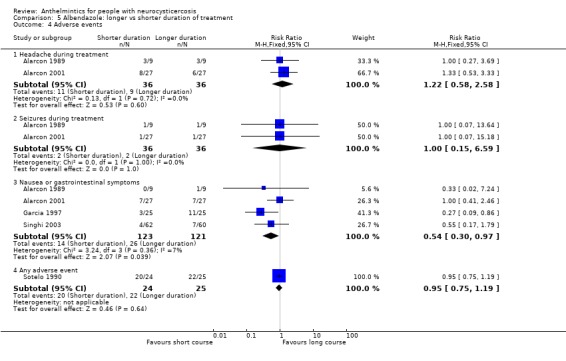
Comparison 5 Albendazole: longer vs shorter duration of treatment, Outcome 4 Adverse events.
6. Albendazole: with corticosteroids versus without corticosteroids
One trial, including participants with non‐viable lesions only (Singhi 2004), made this comparison.
6.1 Recurrence of seizures
There was no significant difference between in recurrence of seizures during weeks one to 72 after treatment (72 participants, Analysis 6.1).
6.1. Analysis.
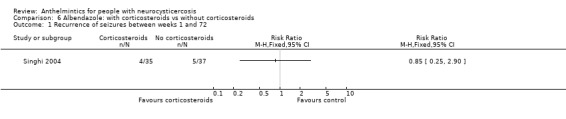
Comparison 6 Albendazole: with corticosteroids vs without corticosteroids, Outcome 1 Recurrence of seizures between weeks 1 and 72.
6.2 Radiological resolution of lesions
There was no significant difference between albendazole alone and albendazole with corticosteroids in the persistence of lesions at six months after treatment (72 participants, Analysis 6.2).
6.2. Analysis.
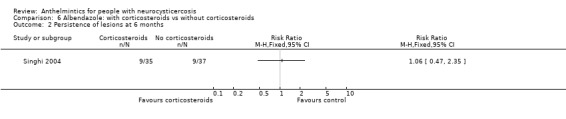
Comparison 6 Albendazole: with corticosteroids vs without corticosteroids, Outcome 2 Persistence of lesions at 6 months.
6.3 Adverse events
This trial did not report on adverse events.
Discussion
Summary of main results
The results of trials comparing anthelmintic treatment with no anthelmintic are mixed and therefore difficult to interpret. Most trials assessed albendazole, which has largely taken over from praziquantel. We found only one small trial comparing praziquantel with no active treatment from which we could not come to any meaningful conclusions on its efficacy. Reduction in seizures with albendazole did not appear to correlate with radiological clearance of lesions. Findings for the three major outcomes categories of this review are described below.
Seizure recurrence
For seizure recurrence, most trials tended towards a benefit of albendazole, and this benefit was significant in the case of children with a single, non‐viable lesion. This finding runs counter to most expert opinion which is of a view that treatment is unlikely to be beneficial for cases with non‐viable lesions only. There was no significant benefit shown for people with viable lesions only, which seems counter‐intuitive, but only one small trial reported on this outcome, hence a larger study is needed to ascertain the efficacy of albendazole in this group. One trial, including participants with both viable and non‐viable lesions (Das 2007), showed a harmful effect of albendazole. This trial, which combined albendazole with steroids, also showed increased encephalopathy and admission to hospital with albendazole, and two deaths from encephalopathy.
Radiological clearance of lesions
For radiological clearance of lesions during the first 12 months, trials including people with viable lesions only showed a significant benefit of albendazole, while trials including only people with non‐viable lesions, or a mixture of viable and non‐viable lesions, showed no significant effect of albendazole. The majority of trials on viable lesions involved adults only, while those on non‐viable lesions involved only children; the observed differences between trial results may also have been affected by the ages of the participants.
Our analysis showed no significant effect of duration of treatment on persistence of lesions at follow up. Assuming that presence of symptoms is associated with presence of lesions (Murthy 2006), these results suggest that a shorter duration of treatment is as effective as a longer course. Shorter courses were also associated with fewer cases of nausea or other gastrointestinal symptoms during treatment. One trial assessed albendazole in combination with praziquantel compared with albendazole alone; the findings suggested that the combination of two anthelmintics was better in the short term.
Adverse events
Participants treated with either albendazole or praziquantel experienced significantly more adverse events during treatment than those receiving no active treatment. Albendazole was associated with headache, dizziness, and nausea, vomiting and abdominal pain. There is some indirect (weak) evidence that corticosteroids used in conjunction with albendazole may protect against headache during treatment, as in trials using corticosteroids there was no significant difference between albendazole and no active treatment in this outcome.
Overall completeness and applicability of evidence
We identified 21 relevant published trials. Most were published since the last update of this Cochrane Review (Salinas 1999). We also identified one relevant ongoing trial. All the trials were small; the largest enrolled 300 participants and the smallest enrolled 18. All trials, published and ongoing, were based in Central and South America and South‐East Asia; there were no trials from Africa or China, where the disease is also endemic.
The trial participants varied, including children and adults and people with different numbers and types of lesions, although trials in children tended to include only non‐viable lesions, while trials in adults mostly included only viable lesions. Together the trials included very few people with large numbers of lesions, or with lesions other than parenchymal cysts or lesions.
Treatment comparisons of the included trials were wide ranging, enabling analysis by type of drug (albendazole or praziquantel) and duration of treatment. We were also able to indirectly compare the frequencies of adverse events during treatment when anthelmintics were administered with or without corticosteroids.
Two comparisons reported by the included trials are not presented in the analysis because their comparisons did not fit into its structure. Gongora‐Rivera 2006 compared only different doses of albendazole given for just one day; this was not presented as we had no other trials using albendazole for just one day, and hence no evidence that it was better than placebo. Sotelo 1990 compared praziquantel given for different durations; this comparison was not presented because we found no evidence that praziquantel was effective in treating neurocysticercosis.
Just over half of the included trials reported on the presence or severity of seizures, which are probably the most important outcomes to most patients. Three other trials reported on symptom severity or presence of symptoms, of which seizures would be the most common, and one trial reported separately on symptoms other than seizures. All the trials assessed and reported on the radiological presence or changes in the neurocysticerci, which may not be directly correlated with the presence or severity of seizures or other symptoms. Radiological outcomes are easy to assess, specific to neurocysticercosis, and perhaps clinically useful, as there is evidence that anti‐epileptic drugs can usually be withdrawn following radiological clearance of lesions, and this may be a criteria for withdrawing anti‐epileptic drugs in some patients and practices (Murthy 2006). However, in this review, children with a single non‐viable lesion, and treated with albendazole compared with no anthelmintic, had a lowered risk of recurrence of seizures despite no difference in the radiological persistence of lesions.
Quality of the evidence
The risk of bias varied between trials, with the trials published most recently tending to be assessed as better for all indicators. Six trials reported an adequate method of allocation concealment; one trial including viable lesions only, four including non‐viable lesions only, and two including both viable and non‐viable lesions.
Potential biases in the review process
All of the included trials were small. In addition, unexplained heterogeneity was introduced by one relatively large, but poorly reported trial (Das 2007) with results mostly running in the opposite direction to those reported in other trials.
Agreements and disagreement with other studies and reviews
Our results slightly vary from other recent meta‐analyses assessing albendazole compared with placebo or usual care, but the conclusions reached are similar.
A meta‐analysis in children (four trials, 400 participants) with neurocysticercosis revealed a higher remission of seizures in those treated with albendazole compared to controls (RR 1.26, 95% CI 1.09 to 1.46). This agrees with our findings in children with non‐viable lesions only. The authors also reviewed 10 observational studies and found conflicting results (Mazumdar 2007).
Del Brutto and colleagues (Del Brutto 2006) reported a meta‐analysis of 11 randomized trials of patients with neurocysticercosis located in or adjacent to the cerebral parenchyma. Anthelmintic drug therapy was associated with complete resolution of viable lesions (44% versus 19%; P = 0.025) at follow up. Trials on non‐viable lesions showed a trend toward lesion resolution favouring anthelmintic drugs (72% versus 63%; P = 0.38), but this was not significant. In patients with non‐viable lesions, risk for seizure recurrence was lower after anthelmintic treatment (14% versus 37%; P < 0.001). The single trial evaluating the frequency of seizures in patients with non‐viable lesions showed a 67% reduction in the rate of generalized seizures with treatment (P = 0.006).
As far as we know, there have been no other meta‐analyses undertaken to compare different durations of treatment.
Ongoing trials are still using regimens of 10 days albendazole (Gilman 2007) despite evidence that shorter treatment durations may be as effective. These findings have implications relating to cost and patient choice and adherence in what may be an expensive disease to treat; a recent study in India reported that the total costs per patient of treating seizures associated with a single cysticerci in the brain may be equivalent to around half the per capita Gross National Product of the country (Murthy 2007).
Current consensus guidelines for the treatment of neurocysticercosis (Garcia 2002; Nogales‐Gaete 2006) do not give any definitive advice on anthelmintic treatment for patients with five or fewer, or more than 100, viable lesions, or fewer than 100 non‐viable lesions. This review presents evidence that albendazole treatment may reduce the recurrence of seizures in children with a single non‐viable lesion, and reduce the persistence of lesions in neuroimaging in persons with small numbers of viable lesions. We did not find enough evidence to draw any conclusions on the safety and effectiveness of treatment for heavy parenchymal infection or extra‐parenchymal (subarachnoid or ventricular) neurocysticercosis. There is also no current consensus on the use of corticosteroids when anthelmintics are used in cases of five or fewer viable cysts, or fewer than 100 non‐viable lesions. This review presents evidence that corticosteroids may reduce the incidence of adverse events during treatment, even in people with only non‐viable lesions or with small numbers of viable lesions.
Authors' conclusions
Implications for practice.
For children with parenchymal neurocysticercosis, and with small numbers of non‐viable neurocysticercosis lesions in the brain, albendazole treatment at the standard dose may reduce the risk of recurrence of seizures in the medium term (six to 18 months). However, it is still unclear whether and how different groups benefit from albendazole treatment. There is some evidence that parasite clearance may be speeded up in patients with viable lesions, but no evidence that this has any impact on seizure recurrence. Short courses of seven days or less are as effective as longer courses, although there is not enough evidence to say what the optimum duration of treatment is. Adverse events during treatment, including headache, dizziness, and gastrointestinal symptoms, are common. There is some indirect evidence that they may be reduced by giving corticosteroids with the albendazole and prescribing albendazole for the minimum effective duration, but this needs to be evaluated through randomized comparisons.
There is not enough evidence available to assess the effects of praziquantel treatment in any group, or albendazole treatment in people with moderate or heavy infections or extra‐parenchymal cysts. It is not known whether people who are HIV positive will respond to treatment in the same way, as it is assumed that most participants in the included studies were HIV negative.
Implications for research.
Further good quality, randomized controlled trials are needed to assess the effectiveness of albendazole treatment in different groups of patients, including adults and children, and people with different stages and numbers of lesions (less than five, five to 100 and more than 100). Some trials should include participants with heavy parenchymal infections, and those with any kind of extra‐parenchymal infection. At least one trial should also include participants who are HIV positive, as HIV infection is common in Africa where neurocysticercosis is also common. Trials should carefully assess, record, and analyse the outcomes likely to be of most interest to the patient, including adverse events during treatment, recurrence of seizures, and successful withdrawal of anti‐epileptic drugs.
Once it is clear which groups might benefit from albendazole treatment, trials should assess the optimal dosage and duration of albendazole treatment for different groups of people with different forms of neurocysticercosis. These should compare treatment of seven days duration with shorter durations, including treatment for as few as three days.
What's new
| Date | Event | Description |
|---|---|---|
| 15 February 2010 | Amended | corrected search dates in abstract |
| 1 September 2009 | New citation required and conclusions have changed | This review replaces an earlier Cochrane Review 'Drugs for treating neurocysticercosis (tapeworm infection of the brain)' (Salinas 1999), which was withdrawn from The Cochrane Library in 2005 due to the availability of new trial evidence. A new team of authors worked on this review. The criteria for inclusion of trials has changed. |
History
Protocol first published: Issue 4, 2006 Review first published: Issue 2, 1996
| Date | Event | Description |
|---|---|---|
| 5 May 2009 | New search has been performed | Search updated; see 'Search methods for identification of studies'. |
Acknowledgements
This review replaces the Salinas 1999 Cochrane Review. The authors are grateful to Rodrigo Salinas and colleagues for having the opportunity to update this review by drafting a new protocol for the update. The authors would like to acknowledge that much of this protocol is based upon the Salinas 1999 Cochrane Review.
This document is an output from a project funded by the UK Department for International Development (DFID) for the benefit of developing countries. The views expressed are not necessarily those of DFID.
Appendices
Appendix 1. Search methods: detailed search strategies
| Search set | CIDG SRa | CENTRAL | MEDLINEb | EMBASEb | LILACSb |
| 1 | Taenia solium | NEUROCYSTICERCOSIS | Taenia solium | Taenia solium | Taenia solium |
| 2 | cysticercosis | Taenia solium | cysticercosis | neurocysticercosis | neurocysticercosis |
| 3 | neurocysticercosis | 1 or 2 | neurocysticercosis | BRAIN CYSTICERCOSIS | 1 or 2 |
| 4 | — | — | 1 or 2 or 3 | 1 or 2 or 3 | albendazole |
| 5 | — | — | albendazole | albendazole | praziquantel |
| 6 | — | — | praziquantel | praziquantel | metrifonate |
| 7 | — | — | pyquiton | metrifonate | 4 or 5 or 6 |
| 8 | — | — | metrifonate | 5 or 6 or 7 | 3 and 7 |
| 9 | — | — | 5 or 6 or 7 or 8 | 3 and 8 | — |
| 10 | — | — | 4 and 9 | Limit 9 to human | — |
| 11 | — | — | Limit 10 to human | — | — |
aCochrane Infectious Diseases Group Specialized Register. bSearch terms used in combination with the search strategy for retrieving trials developed by The Cochrane Collaboration (Lefebvre 2008); upper case: MeSH or EMTREE heading; lower case: free text term.
Appendix 2. Trial description: lesion type
| Lesion type | No. trials | Trial |
| Viable, non‐enhancing, or without surrounding oedema, or, if mixed, at least one viable lesion per participant | 7 | Alarcon 1989; Sotelo 1990; Garcia 1997; Del Brutto 1999; Alarcon 2001; Garcia 2004 |
| Non‐viable, enhancing or with surrounding oedema | 9 | Padma 1994; Baranwal 1998; Singhi 2000; Gogia 2003; Kalra 2003; Singhi 2003; Singhi 2004; De Souza 2009; Kaur 2009 |
| Any stage of lesion(s) or types of lesion not described | 7 | Sotelo 1988; Cruz 1995; Padma 1995; Garcia 1997; Gongora‐Rivera 2006; Carpio 2008; Das 2007 |
Data and analyses
Comparison 1. Albendazole vs placebo or no drug.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Recurrence of seizures at trial's final follow‐up time | 6 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 Viable lesions | 1 | 116 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.60, 1.32] |
| 1.2 Non‐viable lesions | 4 | 329 | Risk Ratio (M‐H, Random, 95% CI) | 0.49 [0.32, 0.75] |
| 1.3 Mixed viable and non‐viable lesions | 1 | 298 | Risk Ratio (M‐H, Random, 95% CI) | 2.36 [1.43, 3.91] |
| 2 No successful withdrawal of anticonvulsant drugs at follow up | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 Viable lesions | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 All‐cause death | 2 | 470 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.24, 2.85] |
| 4 Hospital admission, by follow‐up period | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.1 Start to 3 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 3 to 6 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 6 to 12 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.4 1 to 2 years | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.5 2 to 3 years | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.6 3 to 4 years | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Symptoms not resolved after 3 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6 Symptoms of encephalopathy (headache, vomiting, or altered sensorium), by period of follow up | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6.1 Start to 3 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 3 to 6 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.3 6 to 12 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.4 1 to 2 years | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.5 2 to 3 years | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.6 3 to 4 years | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Persistence of lesions at trial's final follow‐up time (up to 12 months) | 9 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.1 Viable lesions | 2 | 192 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.45, 0.70] |
| 7.2 Non‐viable lesions | 6 | 570 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.86, 1.11] |
| 7.3 Mixed viable and non‐viable lesions | 1 | 298 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.97, 1.06] |
| 8 Headache during treatment | 4 | 392 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.37 [1.08, 1.73] |
| 8.1 Viable lesions | 2 | 139 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.96 [0.49, 17.77] |
| 8.2 Non‐viable lesions | 1 | 83 | Risk Ratio (M‐H, Fixed, 95% CI) | 15.82 [0.98, 255.96] |
| 8.3 Mixed viable and non‐viable lesions | 1 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.14 [0.92, 1.42] |
| 9 Headache during treatment ‐ by corticosteroid use | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 9.1 Corticosteroids given with albendazole | 2 | 286 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [0.93, 1.44] |
| 9.2 No corticosteroids given | 2 | 106 | Risk Ratio (M‐H, Fixed, 95% CI) | 9.49 [1.40, 64.45] |
| 10 Dizziness during treatment | 3 | 222 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.77 [1.42, 9.97] |
| 11 Nausea, vomiting, or abdominal pain during treatment | 4 | 392 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.40 [1.01, 1.94] |
| 12 Seizures during treatment | 5 | 455 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.62 [0.79, 3.31] |
Comparison 2. Praziquantel vs placebo or no drug.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Symptoms not resolved after 3 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Persistence of lesions at follow up | 1 | 15 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.14, 0.85] |
| 3 No reduction in number of lesions at 3 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4 Any adverse events during treatment | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Comparison 3. Albendazole vs praziquantel.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Recurrence of seizures at follow up | 1 | 19 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.18 [0.01, 3.35] |
| 2 Symptoms not resolved after 3 months | 2 | 121 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.58 [0.36, 0.92] |
| 3 Persistence of lesions at follow up | 3 | 154 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.45, 0.91] |
| 4 No reduction in number of lesions at 3 months | 3 | 149 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.41 [0.19, 0.92] |
| 5 Adverse events | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 Headache or vomiting or both | 1 | 20 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.6 [0.19, 1.86] |
| 5.2 Seizures during treatment | 1 | 20 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.02, 7.32] |
| 5.3 Any adverse event | 2 | 134 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.94, 1.32] |
Comparison 4. Albendazole combined with praziquantel vs albendazole alone.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Recurrence of seizures within 6 months | 1 | 112 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.20, 4.42] |
| 2 Persistence of lesions, by follow‐up period | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 1 month | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 3 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 6 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 5. Albendazole: longer vs shorter duration of treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Symptoms not resolved after 3 months: 8 days vs more than 8 days | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Viable lesions | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Mixed viable and non‐viable lesions | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Persistence of lesions at longest length of follow up: 7 or 8 days vs. more than 7 to 8 days | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 Viable lesions | 2 | 103 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.52, 1.76] |
| 2.2 Non‐viable lesions | 2 | 159 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.64, 1.50] |
| 2.3 Mixed viable and non‐viable lesions | 2 | 79 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.53, 1.36] |
| 3 No reduction in number of lesions at 3 months follow up, by length of treatment comparison | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 8 days vs > 8 days | 2 | 102 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.17, 2.74] |
| 4 Adverse events | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 Headache during treatment | 2 | 72 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.22 [0.58, 2.58] |
| 4.2 Seizures during treatment | 2 | 72 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.15, 6.59] |
| 4.3 Nausea or gastrointestinal symptoms | 4 | 244 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.54 [0.30, 0.97] |
| 4.4 Any adverse event | 1 | 49 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.75, 1.19] |
| 5 Persistence of lesions (viable lesions only): 3 days vs 8 days | 1 | 54 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.37, 2.71] |
5.3. Analysis.
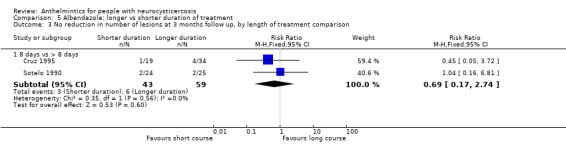
Comparison 5 Albendazole: longer vs shorter duration of treatment, Outcome 3 No reduction in number of lesions at 3 months follow up, by length of treatment comparison.
5.5. Analysis.
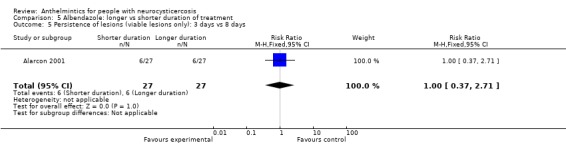
Comparison 5 Albendazole: longer vs shorter duration of treatment, Outcome 5 Persistence of lesions (viable lesions only): 3 days vs 8 days.
Comparison 6. Albendazole: with corticosteroids vs without corticosteroids.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Recurrence of seizures between weeks 1 and 72 | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Persistence of lesions at 6 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Alarcon 1989.
| Methods | Randomized controlled trial Duration: dates not supplied. Participants followed up for 4 months |
|
| Participants | Number: 23 enrolled; numbers of males and females not presented Inclusion criteria: adults and children aged > 13 years, with 1 to 3 parenchymal cysts > 10 mm without perilesional oedema, good general health and stable neurological disease Exclusion criteria: parenchymal cysts with ring enhancement and oedema surrounding the lesions, pregnant women Type of lesion: viable |
|
| Interventions | Group 1. Albendazole: 15 mg/kg bodyweight for 3 days Group 2. Albendazole: 15 mg/kg bodyweight for 30 days Group 3. No albendazole | |
| Outcomes | Included in the review: number of cysts and total diameter of cysts at baseline and 1 day, 30 days, and 3 months after treatment finishes. Adverse events | |
| Notes | Location: Ecuador Source of funding: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Quote: "randomly allocated" Decision: probably done, but unclear |
| Allocation concealment? | Unclear risk | Not described |
| Blinding? All outcomes | Unclear risk | Not described. Placebos were not used and different groups received follow‐up scans at different times Decision: unclear, probably not done |
| Incomplete outcome data addressed? All outcomes | Low risk | 23 randomized and follow‐up data available for all (100%) |
| Free of selective reporting? | Low risk | No evidence of selective reporting; outcomes reported individually for all participants |
| Free of other bias? | Low risk | No evidence of other bias |
Alarcon 2001.
| Methods | Randomized controlled trial Duration: participants recruited between January 1989 and December 1996, and followed up for 12 months |
|
| Participants | Number: 95 enrolled, data available for 83 (36 male, 47 female) Inclusion criteria: adults with neurological signs and symptoms and 1 to 6 non‐enhancing parenchymal cysts without perilesional oedema Exclusion criteria: ring or nodular cysts, oedema surrounding the lesions, subarachnoid or intraventricular cysts, hydrocephalus, previous treatment with albendazole or praziquantel, pregnant women, intracranial hypertension Type of lesion: viable |
|
| Interventions | Group 1. Albendazole: 15 mg per kg bodyweight for 3 days Group 2. Albendazole: 15 mg per kg bodyweight for 8 days Group 3. No albendazole | |
| Outcomes | Included in the review: number of cysts at baseline, 3 months, and 6 months; persistence of cysts at 3 months and 12 months; number of seizures per year at baseline and 12 months; adverse events associated with treatment | |
| Notes | Location: Ecuador Source of funding: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Method not described, but trial described as 'randomized' Decision: unclear, but probably done |
| Allocation concealment? | Unclear risk | Not described Decision: unclear |
| Blinding? All outcomes | Low risk | Quote: "Evaluation of the number of cysts on CT at baseline and at follow‐up was performed by a single neuroradiologist blinded to the treatment allocation" |
| Incomplete outcome data addressed? All outcomes | Low risk | 95 participants randomized; 8 excluded before starting treatment, 4 lost to follow up (87% included in the analysis) |
| Free of selective reporting? | Low risk | No evidence of selective reporting |
| Free of other bias? | Low risk | No evidence of other bias |
Baranwal 1998.
| Methods | Randomized controlled trial Duration: dates not supplied. Participants followed up for 24 months. |
|
| Participants | Number: 63 enrolled, 57 included in analysis (33 male, 24 female) Inclusion criteria: children aged 2 years to 12 years with a single small enhancing lesion in brain parenchyma plus seizures for less than 3 months Exclusion criteria: neurologic deficit or suspected tuberculosis Type of lesion: non‐viable |
|
| Interventions | Group 1. Albendazole: 15 mg per kg bodyweight for 28 days, plus 1 to 2 mg prednisolone per day for 5 days Group 2. Placebo, plus 1 to 2 mg prednisolone per day for 5 days | |
| Outcomes | Included in the review: recurrence of seizures at 3 months after treatment; persistence of lesion at 1 month and 3 months; recurrence of seizures 8 months after tapering anticonvulsants after 18 to 24 months seizure‐free following treatment Not included in the review: calcification of lesion at 3 months; lesion diameter at baseline and 1 month |
|
| Notes | Location: India Source of funding: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Quote: "...numbered in a random sequence using a random number table" Decision: done |
| Allocation concealment? | Low risk | Quote: "Envelopes containing albendazole or placebo capsules for the full course of therapy were prepared in advance and numbered in a random sequence" Decision: done |
| Blinding? All outcomes | Low risk | Quote: "All persons involved in the study i.e. patient, clinical investigator and neuroradiologist were blind to the random allocation. Results were decoded after completion of 6 months of study to identify the groups" Decision: done |
| Incomplete outcome data addressed? All outcomes | Low risk | 63 randomized, 6 lost to follow up (90% included in the analysis) |
| Free of selective reporting? | Low risk | No evidence of selective reporting |
| Free of other bias? | Low risk | No evidence of other bias |
Carpio 2008.
| Methods | Randomized controlled trial Duration: dates not supplied. Participants followed up for 12 months Inclusion of randomized participants in the analysis: 161/178 = 90% (in addition, 7 died) |
|
| Participants | Number: 178 enrolled, 97 male, 77 female; 4 with missing data on sex Inclusion criteria: any age or gender with new onset symptoms associated with neurocysticercosis within 2 months prior to recruitment, and neurocysticercosis cysts an axial CT or MRI imaging of the brain. Could include 1 or more active parenchymal cysts, degenerative or transitional parenchymal cysts, or cysts with a extra‐parenchymal location. Exclusion criteria: having only calcified cysts, pregnancy, papilloedema, active tuberculosis, syphilis, ocular cysticercosis, active gastric ulcers or any progressive or life‐threatening disorder Type of lesion: viable or non‐viable cysts, or a combination of the two |
|
| Interventions | Group 1: For participants weighing more than 50 kg, 400 mg of albendazole every 12 hours for 8 days. For participants weighing less than 50 kg, including children, 15 mg per kg bodyweight per day for 8 days. Participants weighing over 50 kg also received 75 mg prednisolone daily for 8 days, then 50 mg per day for 1 week, then 25 mg per day for 1 week. Participants weighing less than 50 kg received 1.5 mg per kg bodyweight prednisone for 8 days, then 1 mg per kg for 1 week, then 0.5 mg for 1 week. Group 2: Placebo with an identical appearance to albendazole, plus prednisolone as for Group 1 |
|
| Outcomes | Included in the review: freedom from seizures for 12 months following treatment; mean time seizure‐free following treatment; freedom from cysts 1 month, 6 months and 12 months following treatment; reduction in the number of cysts 1 month, 6 months and 12 months following treatment; deaths due to cysticercosis; all‐cause deaths; adverse events during treatment, and during the first month following treatment | |
| Notes | Location: Ecuador Source of funding: NINDS grant R01‐NS39403. Glaxo/SKB and Acromax Co supplied the active drug and placebo |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Quote: "Patients were allocated to treatment group according to a stratified block randomisation schedule. Two strata were considered: centre (sex centres) and location of the cyst (parenchymal versus extraparenchymal). Permuted blocks of size 4 and 6 were used to balance the treatment allocation within each stratum" Decision: done |
| Allocation concealment? | Low risk | Quote: "The randomisation lists were kept in electronic form on a computer accessible only to the statistician" Decision: done |
| Blinding? All outcomes | Low risk | Quotes: "All other research staff were blinded to the treatment arm"... "double‐blind, placebo controlled trial" Decision: done |
| Incomplete outcome data addressed? All outcomes | Low risk | Of 178 participants, 161 (90%) were followed up and included in the analysis. In addition, 7 died. |
| Free of selective reporting? | Low risk | No evidence of selective reporting |
| Free of other bias? | Low risk | No evidence of other bias |
Cruz 1995.
| Methods | Randomized controlled trial Duration: dates not specified. Participants followed up for 4 months. |
|
| Participants | Number: 61 enrolled, 53 included in the analysis (33 male, 20 female) Inclusion criteria: adults with cystic or encephalitic forms of cerebral cysticercosis ‐ any developmental stage of the parasite, localization parenchymous, subarachnoid, or ventricular Exclusion criteria: patients in a coma or generally poor condition Type of lesion: mixed viable, non‐viable, and both viable and non‐viable |
|
| Interventions | Group 1. Albendazole: 800 mg per day for 8 days Group 2. Albendazole: 800 mg per day for 15 days Group 3. Albendazole: 800 mg per day for 30 days | |
| Outcomes | Included in the review: persistence of cysts at 3 months; number of cysts at baseline and 3 months; symptom change at 3 months; adverse events | |
| Notes | Location: Ecuador Source of funding: partially funded by SmithKline Beecham Pharmaceuticals |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Quote: "...were randomised to one of 3 different treatment groups" Decision: unclear, probably done |
| Allocation concealment? | Unclear risk | Not described Decision: unclear |
| Blinding? All outcomes | Unclear risk | Not described. Participants were treated for different durations, without the use of placebos. Decision: unclear, probably not done |
| Incomplete outcome data addressed? All outcomes | Low risk | Of 61 participants randomized, 53 completed 3 months follow up (87%) |
| Free of selective reporting? | Low risk | No evidence of selected reporting |
| Free of other bias? | Low risk | No evidence of other bias |
Das 2007.
| Methods | Randomized controlled trial Duration: between January 1997 and January 2005 |
|
| Participants | Number: 300 enrolled (178 male, 122 female) Inclusion criteria: adults presenting with recent‐onset seizures, with CT and MRI scan results strongly suggestive of neurocysticercosis and at least 2 lesions with ring enhancement, of which at least 1 was in the vesicular stage, and antibodies against neurocysticercosis detected by ELISA on at least 3 occasions Exclusion criteria: primary seizure disorder, family history of seizure, pre‐existing focal neurological deficit, or any metabolic or hereditary disease Type of lesion: mixed viable and non‐viable |
|
| Interventions | Group 1. 15 mg per kg bodyweight albendazole daily for 14 days, plus 2 mg dexamethasone orally at 8‐hour intervals for 14 days, plus anti‐epileptic drugs at appropriate doses. Dexamethasone tapered off over time. Group 2. Placebo plus anti‐epileptic drugs | |
| Outcomes | Included in the review: seizures, hospital admissions, and resolution of lesions at 3 months, 6 months, 1 year, 2 years, 3 year and 4 years | |
| Notes | Location: India Source of funding: Burdwan Medical College and Hospital |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Quote: "The patients were randomly allocated into two groups" Decision: unclear, probably done |
| Allocation concealment? | Unclear risk | Not described Decision: unclear |
| Blinding? All outcomes | Unclear risk | Placebos used, but blinding not described for investigators and medical staff Decision: unclear |
| Incomplete outcome data addressed? All outcomes | Low risk | 300 randomized, 2 died within 3 months, 298 followed up for 5 years (100% follow up) |
| Free of selective reporting? | Low risk | No evidence of selective reporting |
| Free of other bias? | Low risk | No evidence of other bias |
De Souza 2009.
| Methods | Randomized controlled trial Duration: participants enrolled between May 2002 and October 2003 and followed up for up to 64 months (mean 31 months) |
|
| Participants | Number: 123 enrolled, 103 included in the analysis (59 male, 44 female) Inclusion criteria: all patients presenting with new onset focal or generalized seizures with MRI‐confirmed solitary cysticercal lesion in the brain parenchyma Exclusion criteria: past history of epilepsy, received albendazole or praziquantel in the past, evidence of other lesions on CT or MRI, significant neurological deficits, raised intracranial pressure or seizures refractory to acute treatment Types of lesion: non‐viable |
|
| Interventions | Group 1: Anti‐epileptic drugs only Group 2: Anti‐epileptic drugs plus albendazole 15 mg per kg bodyweight per day for 28 days |
|
| Outcomes | Included in the review: time to becoming seizure‐free; total number of seizures from onset of illness until the last visit; duration of anti‐epileptic drug therapy; number of months seizure free at the last visit; number of months taken off anti‐epileptic drugs at last visit; disappearance of calcification of cysts Not included in the review: types of seizure; mean cyst area; perilesional oedema |
|
| Notes | Location: India Source of funding: Indian Council for Medical Research |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Quote: "The patients were randomised to two groups by means of a random number table" Decision: done |
| Allocation concealment? | Unclear risk | Not described Decision: unclear |
| Blinding? All outcomes | Unclear risk | Not described. Placebos not used Decision: unclear, probably not done |
| Incomplete outcome data addressed? All outcomes | Low risk | Of 123 participants recruited, 103 (84%) had a minimum follow up of 12 months, and so were included. It was stated that the demographic profile, seizure type and MRI findings in the 20 excluded participants did not differ from those included. |
| Free of selective reporting? | Low risk | No evidence of selective reporting |
| Free of other bias? | Low risk | No evidence of other bias |
Del Brutto 1999.
| Methods | Randomized controlled trial Duration: dates not specified |
|
| Participants | Number: 20 enrolled (8 male, 12 female) Inclusion criteria: adults with less than 20 parenchymal brain cysts with no evidence of surrounding inflammation Exclusion criteria: mixed forms of the disease Type of lesion: viable |
|
| Interventions | Group 1. Albendazole: 15 mg per kg for 7 days plus prednisolone 1 mg per kg bodyweight per day, until a few days after the end of the trial Group 2. Praziquantel: 100 mg per kg bodyweight for 1 day, plus 2 mg doses of intravenous dexamethasone administered 6 and 8 hours after the last dose of praziquantel | |
| Outcomes | Included in the review: number of cysts at baseline and 3 months; persistence of cysts at 3 months; persistence of seizures at 6 to 12 months; adverse events associated with treatment Not included in the review: improvement in motor deficit at 6 to 12 months |
|
| Notes | Location: Ecuador Source of funding: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Quote: "...patients were randomly allocated (from a table of random numbers) to one of two treatment groups" Decision: done |
| Allocation concealment? | Unclear risk | Not described Decision: unclear |
| Blinding? All outcomes | Low risk | Quote: "All CT studies were independently reviewed by two experienced radiologists, blinded to the therapy used..." Decision: done |
| Incomplete outcome data addressed? All outcomes | Low risk | 20 participants randomized, all 20 followed up to 6 months (100%) |
| Free of selective reporting? | Low risk | No evidence of selective reporting |
| Free of other bias? | Low risk | No evidence of other bias |
Garcia 1997.
| Methods | Randomized controlled trial Duration: dates not supplied. Participants followed up for 12 months. |
|
| Participants | Number: 55 enrolled (32 male, 23 female) Inclusion criteria: adults with live cysts or nodular enhancing lesions, with or without contrast enhancement, in any part of the brain. Positive immunoblot Exclusion criteria: pregnant or lactating women Type of lesion: viable or mixed (41), non‐viable (9) |
|
| Interventions | Group 1. Albendazole: 400 mg daily for 14 days plus dexamethasone 1.5 mg 3 times daily for 5 days and 0.5 mg 3 times daily for 5 days then 0.5 mg 3 times daily for 2 days Group 2. Albendazole: 400 mg daily for 7 days plus dexamethasone 1.5 mg 3 times daily for 5 days and 0.5 mg 3 times daily for 5 days then 0.5 mg 3 times daily for 2 days | |
| Outcomes | Included in the review: Number of cysts at baseline, 3 months and 1 year; persistence of cysts at 3 months; gastrointestinal symptoms during treatment |
|
| Notes | Location: Peru Source of funding: funded in part by grants number 1‐U01 A135894‐01 from the National Institutes for Health; and from SmithKline Beecham Pharmaceuticals, London, UK |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Quote: "Patients were blindly assigned to one of two treatment groups using a previously assigned randomization schedule" Decision: done |
| Allocation concealment? | Unclear risk | Quote: "Patients were blindly assigned to one of two treatment groups using a previously assigned randomization schedule" Decision: unclear, but probably done |
| Blinding? All outcomes | Unclear risk | Quote: "CT scans were read by an experienced reader, blinded to the therapy used" Decision: done |
| Incomplete outcome data addressed? All outcomes | Low risk | 55 participants randomized, 50 included in the analysis (91%) |
| Free of selective reporting? | Low risk | No evidence of selective reporting |
| Free of other bias? | Low risk | No evidence of other bias |
Garcia 2004.
| Methods | Randomized controlled trial Duration: recruitment between January 1997 and March 1999. Follow up for 6 months. |
|
| Participants | Number: 120 enrolled (61 male, 59 female) Inclusion criteria: adults with fewer than 20 viable parenchymal cysts plus 1 or more seizures in the previous 6 months Exclusion criteria: primary generalized seizures, history of antiparasitic treatment, evidence on CT of other diseases, moderate or severe intracranial hypertension, status epilepticus, focal neurological deficits, unstable vital signs, impending risk of death, or pregnancy. Type of lesion: viable |
|
| Interventions | Group 1. Albendazole: 400 mg every 12 hours and 2 mg dexamethasone every 8 hours for 10 days Group 2. Placebos | |
| Outcomes | Included in the review: recurrence of seizures during months 2 to 30; partial seizures in month 1, months 2 to 12 and months 13 to 30, and following tapering of anti‐epileptic drugs; seizures with generalization in month 1, months 2 to 12 and months 13 to 30, and following tapering of anti‐epileptic drugs; number of cysts at baseline and 6 months; persistence of seizures at 6 months; adverse events associated with treatment | |
| Notes | Location: Peru Source of funding: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Random assignment in blocks of 6 according to a pre‐established list taken from a random‐numbers table |
| Allocation concealment? | Low risk | Randomization performed from remote site by a statistician not otherwise involved in the study. All drugs and placebos were administered by the study personnel, who received them in sealed, opaque, sequentially numbered envelopes |
| Blinding? All outcomes | Low risk | Blinded all study participants and personnel |
| Incomplete outcome data addressed? All outcomes | Low risk | 120 randomized, 116 received study medication, 2 were excluded from the analysis, 14 lost to follow up (100/120 = 83%). The reasons for all withdrawals were clearly documented. |
| Free of selective reporting? | Low risk | No evidence of selective reporting |
| Free of other bias? | Low risk | No evidence of other bias |
Gogia 2003.
| Methods | Randomized controlled trial Duration: recruitment March to July 2000 |
|
| Participants | Number: 72 enrolled (38 male, 34 female) Inclusion criteria: children aged 18 months to 12 years with ring‐enhancing lesions in brain parenchyma, plus seizures without a history of epilepsy Exclusion criteria: tuberculosis, known epilepsy on anti‐epileptic medication, chronic central nervous system disorders. CT scans showing disc, nodular or calcific lesions. Type of lesion: non‐viable |
|
| Interventions | Group 1. Prednisolone: 2 mg per kg for 3 days followed by albendazole 15 mg per kg bodyweight for 28 days Group 2. Prednisolone: 2 mg per kg for 3 days followed by placebo for 28 days | |
| Outcomes | Included in the review: persistence of lesions at 6 months; recurrence of seizures at 6 months Not included in the review: calcification of lesions at 6 months; nodular lesions at 6 months |
|
| Notes | Location: India Source of funding: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Quote: "The enrolled children were randomized using a random number table" Decision: done |
| Allocation concealment? | Low risk | Quote: "...coded as drug A or drug B..." "The drugs were dispensed in coded envelopes" Decision: done |
| Blinding? All outcomes | Low risk | Quote: "The drugs were dispensed in coded envelopes. The investigators and the patients were thus blinded to which drug was being given to which patient. The radiologist responsible for reading the X‐rays was also blinded to the drug therapy" Decision: done |
| Incomplete outcome data addressed? All outcomes | Low risk | 72 participants were randomized; all 72 were followed up for seizure recurrence at 6 months (100%) |
| Free of selective reporting? | Low risk | No evidence of selective reporting |
| Free of other bias? | Low risk | No evidence of other bias |
Gongora‐Rivera 2006.
| Methods | Randomized controlled trial Duration: between November 1999 and January 2001 |
|
| Participants | Number: 36 enrolled (14 male, 22 female) Inclusion criteria: adults with subarachnoid and intraventricular cysticercosis Exclusion criteria: concurrent disease that contraindicated corticosteroid, albendazole allergy, previous cysticidal or surgical treatment for neurocysticercosis in the previous 3 months, pregnant or lactating women, neurological diseases affecting function, unable to attend for regular follow up, Karnofsky score ≤ 50 points Type of lesion: degenerating, viable, or mixed |
|
| Interventions | Group 1. Intravenous dexamethasone: 8 mg every 8 hours for 4 days followed by 15 mg per kg albendazole for 1 day Group 2. Intravenous dexamethasone: 8 mg every 8 hours for 4 days followed by 30 mg per kg albendazole for 1 day | |
| Outcomes | Included in the review: symptom severity score at baseline and 7 days; adverse events associated with treatment Not included in the review: reduction in cyst volume at 90 days |
|
| Notes | Location: Mexico Source of funding: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Quote: "...a computer‐generated randomization plan" Decision: done |
| Allocation concealment? | Low risk | Quote: "The code of the two different albendazole doses was available in sealed envelopes and was not opened until the trial completion" |
| Blinding? All outcomes | Low risk | Quote: "For blinding the pharmaceutical laboratory...provided according to a computer‐generated randomization plan, tablets containing 200 mg or 400 mg albendazole with identical appearance. Neither the patient nor the study staff were aware of treatment assignment" Decision: done |
| Incomplete outcome data addressed? All outcomes | Low risk | Inclusion of randomized participants in the analysis: 36 randomized, 5 did not compete the study (86%). An intention‐to‐treat analysis was also undertaken with similar results obtained. |
| Free of selective reporting? | Low risk | No evidence of selective reporting |
| Free of other bias? | Low risk | No evidence of other bias |
Kalra 2003.
| Methods | Randomized controlled trial Duration: dates not specified. Participants followed up for 6 months. |
|
| Participants | Number: 123 enrolled (65 male, 58 female) Inclusion criteria: children aged 1 to 14 years with seizures plus 1 or 2 ring‐enhancing lesions, excluding intraventricular cysts Exclusion criteria: suspected tuberculosis, intraocular cysts, multiple lesions, disk or calcified lesions, intraventricular cysts, or hydrocephalus Type of lesion: non‐viable |
|
| Interventions | Group 1. Dexamethasone: 0.15 mg per kg bodyweight per day for 5 days plus 15 mg per kg albendazole for 28 days starting on day 3 Group 2. No dexamethasone or albendazole | |
| Outcomes | Included in review: persistence of lesions at 3 months; complete or partial resolution or calcification of lesions at 3 months; seizure recurrence at 3 and 6 months | |
| Notes | Location: India Source of funding: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Quote: "A simple randomization scheme was used for allocation of patients to the treated or control groups" Decision: done |
| Allocation concealment? | Low risk | Quote: "Random assignment code was concealed up to the time of allocation in sealed envelopes labelled with a unique patient number" Decision: done |
| Blinding? All outcomes | High risk | Quote: "Evaluation of CT lesions...was performed by a single radiologist blinded to the treatment assignment and to the clinic outcome" Blinding of participants was not described, and placebos were not used. Abstract refers to an "open trial". Decision: partially done, for radiological outcomes only |
| Incomplete outcome data addressed? All outcomes | High risk | 123 participants randomized, 30 lost to follow up at 3 months (93/123 = 76%). No discussion of the difference between participants available for follow up and those lost to follow up. |
| Free of selective reporting? | Low risk | No evidence of selective reporting |
| Free of other bias? | Low risk | No evidence of other bias |
Kaur 2009.
| Methods | Randomized controlled trial Duration: participants enrolled January to December 2007 and followed up for 6 months |
|
| Participants | Number: 112 enrolled (69 male, 43 female), 103 included in the analysis Inclusion criteria: children aged 1 to 13 years with focal or generalized seizures for less than 3 months, no neuro deficits on clinical examination, and characteristic neuroimaging findings of single, small (< 20 mm) well‐defined lesion with peripheral (ring) or uniform (disc) contrast enhancement with or without surrounding oedema, with minimal or no mass effect, without any midline shift Exclusion criteria: multiple lesions, extra parenchymal neurocysticercosis, focal neurologic deficit, suspected tuberculosis, any active systemic disease, or history of prior antiparasitic treatment Category of lesion: degenerating |
|
| Interventions | Group 1: Albendazole 15 mg per kg bodyweight per day for 7 days, oral prednisolone 2 mg per kg per day for 5 days, plus 75 mg per kg praziquantel for 1 day Group 2: Albendazole 15 mg per kg bodyweight per day for 7 days, oral prednisolone 2 mg per kg per day for 5 days, plus 75 mg per kg placebo for 1 day |
|
| Outcomes | Included in the review: complete resolution of lesion at 1, 3, and 6 months, recurrence of seizures within 6 months, adverse effects of therapy | |
| Notes | Location: India Source of funding: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Quote: "All children were randomized and allocated to either of these two groups using a table of random numbers" Decision: done |
| Allocation concealment? | Low risk | Quote: "Identical looking sachets in strengths of 50, 100, and 200 mg of praziquantel and placebo were prepared...these sachets were coded as group A and B. The code was kept secret and opened only after completion of the study" Decision: done |
| Blinding? All outcomes | Low risk | Quote: "All persons involved in the study including the patient, the clinical investigator and the neuroradiologist were blinded to the random allocation" Decision: done |
| Incomplete outcome data addressed? All outcomes | Low risk | 112 children were enrolled, 9 did not report for follow up, so 103 included in the main analysis (92%) |
| Free of selective reporting? | Low risk | No evidence of selective reporting |
| Free of other bias? | Low risk | No evidence of other bias |
Padma 1994.
| Methods | Randomized controlled trial Duration: dates not specified. Participants followed up for 3 months |
|
| Participants | Number: 75 enrolled (52 male, 23 female) Inclusion criteria: adults and children aged 3.5 to 50 years with epilepsy, parenchymal single small enhancing lesions Exclusion criteria: neurological deficit on examination Type of lesion: non‐viable |
|
| Interventions | Group 1. Albendazole: 15 mg per kg per day for 7 days Group 2. Placebo | |
| Outcomes | Included in the review: complete resolution, partial resolution, and no resolution of lesion at 1 week, 1 month and 3 months | |
| Notes | Location: India Source of funding: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Quote: "Patients were randomly allocated to placebo or albendazole therapy" Decision: unclear, probably done |
| Allocation concealment? | Unclear risk | Not described Decision: unclear |
| Blinding? All outcomes | Low risk | Quote: "CTs were assessed by a neuroradiologist who was not aware of the treatment received by the patient" Placebos were used for participants Decision: done |
| Incomplete outcome data addressed? All outcomes | Low risk | 75 participants randomized, follow‐up data at 3 months available for 68 (91%) |
| Free of selective reporting? | Low risk | No evidence of selective reporting |
| Free of other bias? | Low risk | No evidence of other bias |
Padma 1995.
| Methods | Randomized controlled trial Duration: dates not specified. Participants followed up for 3 months. |
|
| Participants | Number: 29 enrolled (22 male, 7 female) Inclusion criteria: adults and children aged 8 to 50 with multiple cystic lesions suggestive of neurocysticercosis plus neurological signs Exclusion criteria: calcified lesions only Type of lesion: degenerating, viable or mixed (possible to follow the radiological clearance of individual lesions by type) |
|
| Interventions | Group 1. Albendazole: 15 mg per kg per day for 7 days Group 2. Placebo | |
| Outcomes | Included in the review: change in number of lesions at 1 and 3 months; persistence of lesions at 1 week, 1 month, and 3 months Not included in the review: change in oedema at 1 and 3 months |
|
| Notes | Location: India Source of funding: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Quote: "We undertook a randomized, double‐blind, placebo‐controlled study" Decision: unclear, probably done |
| Allocation concealment? | Unclear risk | Not described Decision: unclear |
| Blinding? All outcomes | Low risk | Quote: "...double‐blind, placebo‐controlled study"... "Placebo tablets of similar appearance"..."The CTS scans were assessed...by a neuroradiologist who was not aware of the treatment given" Decision: done |
| Incomplete outcome data addressed? All outcomes | Low risk | 29 randomized, 29 included in the analysis (100%) |
| Free of selective reporting? | Low risk | No evidence of selective reporting |
| Free of other bias? | Low risk | No evidence of selective reporting |
Singhi 2000.
| Methods | Randomized controlled trial Duration: recruitment from 1994 to 1998. Participants followed up for 6 months. |
|
| Participants | Number: 176 included in the analysis, male/female ratio not presented Inclusion criteria: children up to the age of 14 with a single small ring‐enhancing lesion in brain parenchyma Exclusion criteria: none stated Type of lesion: non‐viable |
|
| Interventions | Group 1. Albendazole: 15 mg per kg bodyweight for 28 days plus prednisolone at 2 mg per kg per day for 5 days Group 2. No albendazole or prednisolone | |
| Outcomes | Included in the review: persistence of lesions at month 3 to 6 Not included in the review: lesion size decreased, increased, or remained the same at 3 to 6 months |
|
| Notes | Location: India Source of funding: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Quote: "Children..were chosen at random to receive either albendazole therapy or no specific anticysticeral therapy"..."randomly allocated children" Decision: unclear, probably done |
| Allocation concealment? | Unclear risk | No described Decision: unclear |
| Blinding? All outcomes | Unclear risk | Not described. Placebos not used. Decision: unclear, probably not done. |
| Incomplete outcome data addressed? All outcomes | Unclear risk | Not clear how many participants enrolled and randomized, outcomes data presented for 176 |
| Free of selective reporting? | Low risk | No evidence of selective reporting |
| Free of other bias? | Low risk | No evidence of other bias |
Singhi 2003.
| Methods | Randomized controlled trial Duration: recruitment from June 1999 to June 2000. Participants were followed up for 12 months. |
|
| Participants | Number: 147 randomized, 122 included in the analysis (68 male, 54 female) Inclusion criteria: children with seizures for less than 3 months and up to 3 small enhancing lesions in parenchyma Exclusion criteria: raised intracranial pressure, focal neurological deficit, neurodevelopmental delay, any chronic systemic disease, other lesions on imaging, evidence of tuberculosis Type of lesion: non‐viable |
|
| Interventions | Group 1. Oral prednisolone: 2 mg per kg once daily for 5 days plus 15 mg per kg per day albendazole for 4 weeks starting 2 days after prednisolone started Group 2. Oral prednisolone: 2 mg per kg once daily for 5 days plus 15 mg per kg per day albendazole for 1 week starting 2 days after prednisolone started | |
| Outcomes | Included in the review: persistence of lesions at 1 month; recurrence of seizures within 12 months; epigastric discomfort with treatment Not included in the review: lesion size reduced at 6 months |
|
| Notes | Location: India Source of funding: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Quote: "...they were randomized according to random number tables..." Decision: done |
| Allocation concealment? | Unclear risk | Not described Decision: unclear |
| Blinding? All outcomes | Low risk | Quote: "None of the persons involved in the study (i.e. patient, investigators and neuroradiologist) was aware of this random allocation. The code was opened only after completion of the study" Decision: done |
| Incomplete outcome data addressed? All outcomes | High risk | 147 randomized, 25 excluded due to poor compliance with treatment or inadequate follow up (83% included in the analysis). No discussion of the differences between participants included in the analysis and those excluded. |
| Free of selective reporting? | Low risk | No evidence of selective reporting |
| Free of other bias? | Low risk | No evidence of other bias |
Singhi 2004.
| Methods | Randomized controlled trial Duration: dates not specified |
|
| Participants | Number: 133 enrolled, 110 included in the analysis (66 male, 44 female) Inclusion criteria: children aged 1 to 14 years with seizures for less than 3 months and a single small enhancing lesion in parenchyma Exclusion criteria: history of generalized seizures, neurologic deficit, multiple lesions on CT, or suspected tuberculosis Type of lesion: non‐viable |
|
| Interventions | Group 1. Prednisolone: 2 mg per kg per day for 3 weeks tapering off in the 4th week Group 2. Albendazole: 15 mg per kg per day for 4 weeks Group 3. Albendazole: 15 mg per kg per day for 4 weeks plus prednisolone 2 mg per kg per day | |
| Outcomes | Included in the review: persistence of lesion at 3 and 6 months; recurrence of seizures between weeks 1 and 72, and after withdrawing from antiepilepsy drugs Not included in the review: partial resolution of lesion at 3 and 6 months; disappearance of perilesional oedema at 3 and 6 months |
|
| Notes | Location: India Source of funding: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Quote: "The children were randomly assigned...using random number tables" Decision: done |
| Allocation concealment? | Unclear risk | Not described Decision: unclear |
| Blinding? All outcomes | Unclear risk | Quote: "All CT scans were assessed by a neuroradiologist who was blinded to treatment assignment and to clinical outcome" Blinding not described for participants Decision: unclear, partially done for radiological outcomes |
| Incomplete outcome data addressed? All outcomes | Low risk | 133 participants were randomized, 23 lost to follow up (85% included in the analysis) |
| Free of selective reporting? | Low risk | No evidence of selective reporting |
| Free of other bias? | Low risk | No evidence of other bias |
Sotelo 1988.
| Methods | Randomized controlled trial Duration: dates not specified. Participants were followed up for 4 months. |
|
| Participants | Number: 25 enrolled (16 male, 9 female) Inclusion criteria: adults with parenchymal brain cysticercosis Exclusion criteria: none stated Type of lesion: viable |
|
| Interventions | Group 1. Albendazole: 15 mg per kg per day for 1 month (no steroids) Group 2. Praziquantel: 50 mg per kg per day for 2 weeks (no steroids) Group 3. Steroids and symptomatic treatment only | |
| Outcomes | Included in the review: persistence of cysts at 3 to 4 months; number of cysts at baseline and 3 to 4 months; resolution of symptoms at 3 to 4 months; adverse events associated with treatment | |
| Notes | Location: Mexico Source of funding: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Quote: "Patients were randomly allocated in three groups..." Decision: unclear, probably done |
| Allocation concealment? | Unclear risk | Not described Decision: unclear |
| Blinding? All outcomes | Unclear risk | Not described. Placebos not used. Decision: unclear, probably not done |
| Incomplete outcome data addressed? All outcomes | Low risk | 25 participants enrolled and randomized, 25 included in the analysis (100%) |
| Free of selective reporting? | Low risk | No evidence of selective reporting |
| Free of other bias? | Low risk | No evidence of other bias |
Sotelo 1990.
| Methods | Randomized controlled trial Duration: dates not stated. Participants followed up for 3 months |
|
| Participants | Number: 114 enrolled (67 male, 47 female) Inclusion criteria: adults and children aged 7 to 72 years with parenchymal brain cysts without CT evidence of surrounding inflammation Exclusion criteria: any parenchymal cysticerci surrounded by oedema or showing enhancement after contrast medium administration Type of lesion: viable |
|
| Interventions | Group 1. Praziquantel: 50 mg per kg bodyweight for 15 days Group 2. Praziquantel: 50 mg per kg bodyweight for 8 days Group 3. Albendazole: 15 mg per kg bodyweight for 30 days Group 4. Albendazole: 15 mg per kg bodyweight for 8 days | |
| Outcomes | Included in the review: mean number of cysts before and 3 months after treatment; persistence of lesions after 3 months; over 50% lesions disappeared after 3 months; no resolution after 3 months; adverse events associated with treatment, adverse events severe enough to need steroids; persistence of symptoms after 3 months; improvement in signs and symptoms after 3 months | |
| Notes | Location: Mexico Source of funding: supported by the Secretaria de Salud de Mexico |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Quote: "...patients were randomly allocated to one of four treatment groups" Decision: unclear, probably done |
| Allocation concealment? | Unclear risk | Not described Decision: unclear |
| Blinding? All outcomes | Unclear risk | Quote: "Evaluation of all CT studies was done at the end of the trial by two groups of clinicians and radiologists who were not aware of the treatment group to which the patients had been allocated" Blinding not described for participants, and placebos not used Decision: unclear, partially done for radiological outcomes |
| Incomplete outcome data addressed? All outcomes | Low risk | 114 participants were enrolled and randomized, follow‐up data were available for all 114 (100%) |
| Free of selective reporting? | Low risk | No evidence of selective reporting |
| Free of other bias? | Low risk | No evidence of other bias |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Antoniuk 1991 | Groups not allocated on a random basis, but according to clinical differences |
| Bustos 2006 | No control group |
| Carpio 1995 | Quasi‐randomized |
| Lopez‐Gomez 2001 | Comparisons did not meet the inclusion criteria |
| Marquez‐Caraveo 2004 | No control group |
| Medina 1993 | Unclear whether groups were randomized; unable to contact the author for clarification |
| Proano 2006 | No control group |
| Sanchetee 1994 | No control group |
| Thussu 2008 | Quasi‐randomized |
Characteristics of studies awaiting assessment [ordered by study ID]
Cruz 1991.
| Methods | Randomized or quasi‐randomized controlled trial Duration: dates not supplied. Participants followed up for 3 months |
| Participants | Number: 100 enrolled (45 male, 55 female) Inclusion criteria: adults with diagnosed cerebral cysticercosis ‐ any developmental stage of the parasite, localization parenchymous, subarachnoid, or ventricular Exclusion criteria: none stated Type of lesion: embryonal, encephalitic, cystic, calcified, or mixed |
| Interventions | Group 1. Praziquantel: 50 mg/kg bodyweight daily for 15 days plus 750 mg intravenous dexamethasone over 3 days followed by oral prednisolone every 3 days until day 45 Group 2. Albendazole: 15 mg/ kg for 30 days plus 750 mg intravenous dexamethasone over 3 days followed by oral prednisolone every 3 days until day 45 |
| Outcomes | Persistence of encephalitic lesions at 3 months; persistence of cysts at 3 months; No change, slight improvement, marked improvement, and freedom from headache at 3 months; no change, slight improvement, marked improvement, and freedom from seizures at 3 months; no change, slight improvement, marked improvement, and freedom from raised intracranial pressure at 3 months; no change, slight improvement, marked improvement, and freedom from miscellaneous signs at 3 months |
| Notes | Location: Ecuador Source of funding: partially funded by SmithKline Beecham Pharmaceuticals |
Pretell 2000.
| Methods | Controlled clinical trial Duration: dates not stated, 3 months follow up |
| Participants | Number: 26 (16 males, 10 females) Inclusion criteria: single enhancing lesion in the brain parenchyma Exclusion criteria: pregnancy, other intracranial pathology |
| Interventions | Group 1: Praziquantel 3 doses (25 mg/ kg) at 2‐hour intervals for 1 day Group 2: No antiparasitic therapy |
| Outcomes | Adverse effects of treatment, radiological resolution of lesions |
| Notes | Location: Peru Source of funding: the Food and Drug Administration; the Fogarty Foundation/NIH; NIAID/NIH (USA) |
Takayanagui 1992.
| Methods | Controlled clinical trial Duration: dates not stated, follow up for 6 months |
| Participants | Number: 59 Inclusion criteria: parenchymal non‐enhancing cystic lesions Exclusion criteria: lesions with enhancement, encephalitic cysticercosis, intraventricular cysts |
| Interventions | Group 1: Praziquantel daily doses 50 mg/kg for 21 days Group 2: Albendazole daily doses 20 mg/ kg for 21 days Group 3: No antihelmintic |
| Outcomes | Number of cysts before and 6 months after treatment, adverse events |
| Notes | Location: Brazil Source of funding: not stated |
Characteristics of ongoing studies [ordered by study ID]
Gilman 2007.
| Trial name or title | Randomized study of albendazole in patients with epilepsy due to neurocysticercosis |
| Methods | Randomized controlled trial |
| Participants | Number expected: 120 Inclusion criteria: presence of taenia solium infection as demonstrated by serology and head CT, at least 2 spontaneous seizures within the last 6 months, age 16 to 65 Exclusion criteria: more than 20 cysts, prior therapy for cysticercosis, focal neurological or motor deficits, cranial nerve lesions, history of epilepsy for over 5 years, CT head evidence of: arteriovenous malformations, trauma, cerebral infarcts, haemorrhages, focal disease not attributable to cysticercosis, moderate or severe intracranial hypertension, status epilepticus |
| Interventions | Intervention: Albendazole and dexamethasone for 10 days Control: Placebo for 10 days |
| Outcomes | Recurrence and number of seizures. Persistence and number of cysts. Participants are followed on day 15 and 30, then every 3 months for 3 years. |
| Starting date | May 2000 |
| Contact information | Robert H Gilman, John Hopkins University, USA |
| Study ID | NCT00004403 |
| Notes | Location: USA Registration number: NCT00004403 Source of funding: FDA Office of Orphan Products Development |
Differences between protocol and review
An additional outcome was added: 'resolution of symptoms' as this was an important outcome presented in reports of some of the included trials. An additional category was also added as a control group intervention in the inclusion criteria: 'another dose or duration of anthelmintic', as it became apparent that these comparisons would be important.
Contributions of authors
The selection of trials for inclusion, assessment of methodological quality, and data extraction was undertaken as indicated in the methods of the review. The analyses were undertaken mainly by Katharine Abba, in consultation with the other two authors. All three authors contributed to the discussion and conclusions of the review.
Sources of support
Internal sources
Liverpool School of Tropical Medicine, UK.
Apollo Hospital, Chennai, India.
External sources
Department for International Development, UK.
Declarations of interest
None known.
Unchanged
References
References to studies included in this review
Alarcon 1989 {published data only}
- Alarcon F, Escalante L, Duenas G, Montalvo M, Roman M. Neurocysticercosis: short course of treatment with albendazole. Archives of Neurology 1989;46(11):1231‐6. [DOI] [PubMed] [Google Scholar]
Alarcon 2001 {published data only}
- Alarcon F, Duenas G, Diaz M, Cevallos N, Estrada G. Short course of albendazole therapy for neurocysticercosis: a prospective randomized trial comparing three days, eight days and the control group without albendazole. Revista Ecuatoriana De Neurologia 2001;10:1‐2. [Google Scholar]
Baranwal 1998 {published data only}
- Baranwal AK, Singhi PD, Khandelwal N, Singhi SC. Albendazole therapy in children with focal seizures and single small enhancing computerized tomographic lesions: a randomized, placebo controlled, double‐blind trial. Pediatric Infectious Disease Journal 1998;17(8):696‐700. [DOI] [PubMed] [Google Scholar]
- Baranwal AK, Singhi PD, Khandelwal N, Singhi SC. Morphometry of single small enhancing computed tomographic lesions: outcome and effect of albendazole therapy. Journal of Tropical Pediatrics 2002;48:219‐24. [DOI] [PubMed] [Google Scholar]
- Baranwal AK, Singhi PD, Singhi SC, Khandelwal N. Seizure recurrence and single small enhancing computed tomographic lesions: prognostic factors on long‐term follow‐up. Journal of Child Neurology 2001;6:443‐4. [DOI] [PubMed] [Google Scholar]
Carpio 2008 {published data only}
- Carpio A, Kelvin EA, Bagiella E, Leslie D, Leon P, Andrews H, et al. Effects of albendazole treatment on neurocysticercosis: a randomised controlled trial. Journal of Neurology, Neurosurgery and Psychiatry 2008;79:1050‐5. [DOI] [PubMed] [Google Scholar]
Cruz 1995 {published data only}
- Cruz I, Cruz ME, Carrasco F, Horton J. Neurocysticercosis: optimal dose treatment with albendazole. Journal of Neurological Sciences 1995;133(1‐2):152‐4. [DOI] [PubMed] [Google Scholar]
Das 2007 {published data only}
- Das K, Mondal GP, Banerjee M, Mukherjee BB, Singh OP. Role of antiparasitic therapy for seizures and resolution of lesions in neurocysticercosis patients: an 8 year randomised study. Journal of Clinical Neuroscience 2007;14(12):1172‐7. [DOI] [PubMed] [Google Scholar]
De Souza 2009 {published data only}
- Souza A, Thennarasu K, Yeshraj G, Kovoor JME, Nalini A. Randomized controlled trial of albendazole in new onset epilepsy and MRI confirmed solitary cerebral cysticercal lesion: effect on long‐term seizure outcome. Journal of the Neurological Sciences 2009;276:108‐14. [DOI] [PubMed] [Google Scholar]
Del Brutto 1999 {published data only}
- Brutto OH, Campos X, Sanchez J, Mosquera A. Single‐day praziquantel versus 1‐week albendazole for neurocysticercosis. Neurology 1999;23(52):1079‐81. [DOI] [PubMed] [Google Scholar]
Garcia 1997 {published data only}
- Garcia H, Gilman R, Catacora M, Verastegui M, Gonzalez AE, Tsang VCW, and the Cysticercosis Working Group in Peru. Serologic evolution of neurocysticercosis patients after antiparasitic therapy. Journal of Infectious Diseases 1997;175:486‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia HH, Gilman RH, Horton J, Martinez M, Herrera G, Altamirano J, et al. Albendazole therapy for neurocysticercosis: a prospective double‐blind trial comparing 7 versus 14 days of treatment. Cysticercosis working group in Peru. Neurology 1997;48(5):1421‐7. [DOI] [PubMed] [Google Scholar]
Garcia 2004 {published data only}
- Garcia HH, Pretell EJ, Gilman RH, Martinez SM, Moulton LH, Brutto OH, et al. A trial of antiparasitic treatment to reduce the rate of seizures due to cerebral cysticercosis. New England Journal of Medicine 2004;350(3):249‐58. [DOI] [PubMed] [Google Scholar]
Gogia 2003 {published data only}
- Gogia S, Talukdar B, Choudhury V, Arora BS. Neurocysticercosis in children: clinical findings and response to albendazole therapy in a randomized, double‐blind, placebo controlled trial in newly diagnosed cases. Transactions of the Royal Society of Tropical Medicine and Hygiene 2003;97(4):416‐21. [DOI] [PubMed] [Google Scholar]
Gongora‐Rivera 2006 {published data only}
- Gongora‐Rivera F, Soto‐Hernandez JL, Gonzalez Esquivel D, Cook HJ, Marquez‐Caraveo C, Hernandez Davila R, et al. Albendazole trials at 15 or 30 mg/kg/day for subarachnoid and intraventricular cysticercosis. Neurology 2006;66(3):436‐8. [DOI] [PubMed] [Google Scholar]
Kalra 2003 {published data only}
- Kalra V, Dua T, Kumar V. Efficacy of albendazole and short‐course dexamethasone treatment in children with 1 or 2 ring‐enhancing lesions of neurocysticercosis: a randomised controlled trial. Journal of Pediatrics 2003;143(1):111‐4. [DOI] [PubMed] [Google Scholar]
Kaur 2009 {published data only}
- Kaur S, Singhi P, Singhi S, Khandelwal N. Combination therapy with albendazole and praziquantel versus albendazole alone in children with seizures and single lesion neurocysticercosis. Pediatric Infectious Disease Journal 2009;28(5):403‐6. [DOI] [PubMed] [Google Scholar]
Padma 1994 {published data only}
- Padma MV, Behari M, Misra NK, Ahuja GK. Albendazole in single CT ring lesions in epilepsy. Neurology 1994;44:1344‐6. [DOI] [PubMed] [Google Scholar]
Padma 1995 {published data only}
- Padma MV, Bahari M, Misra NK, Ahuja GK. Albendazole in neurocysticercosis. National Medical Journal of India 1995;8(6):255‐8. [PubMed] [Google Scholar]
Singhi 2000 {published data only}
- Singhi P, Ray M, Singhi S, Khandelwal N. Clinical spectrum of 500 children with neurocysticercosis and response to albendazole therapy. Journal of Child Neurology 2000;15(4):207‐13. [DOI] [PubMed] [Google Scholar]
Singhi 2003 {published data only}
- Singhi P, Dayal D, Khandelwal N. One week versus four weeks of albendazole therapy for neurocysticercosis in children: a randomized, placebo controlled double‐blind trial. Pediatric Infectious Diseases Journal 2003;22(3):268‐72. [DOI] [PubMed] [Google Scholar]
Singhi 2004 {published data only}
- Singhi P, Jain V, Khandelwal N. Corticosteroids versus albendazole for treatment of single small enhancing computed tomographic lesions in children with neurocysticercosis. Journal of Child Neurology 2004;19(5):323‐7. [DOI] [PubMed] [Google Scholar]
Sotelo 1988 {published data only}
- Sotelo J, Escobedo F, Penagos P. Albendazole vs praziquantel for therapy for neurocysticercosis. A controlled trial. Archives of Neurology 1988;45(5):532‐4. [DOI] [PubMed] [Google Scholar]
Sotelo 1990 {published data only}
- Sotelo J, Brutto OH, Penagos P, Escobedo F, Torres B, Rodriguez‐Carbajal J, Rubio‐Donnadieu F. Comparison of therapeutic regimen of anticystercal drugs for parenchymal brain cysticercosis. Journal of Neurology 1990;237:69‐72. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Antoniuk 1991 {published data only}
- Antoniuk SA, Bruck I, Wittig E, Accorsi A. Neurocysticercosis in childhood: II computed tomography of 24 patients according to symptomatic treatment and with praziquantel [Neurocysticercose na infancia: II tomografia computadoriza de 24 pacientes em relacao ao tratamento sintomatico e com praziquantel]. Arquivos de Neuro‐Psiquiatria 1991;49(1):47‐51. [DOI] [PubMed] [Google Scholar]
Bustos 2006 {published data only}
- Bustos JA, Pretell EJ, Llanos‐Zavalaga, Gilman RH, Brutto OH, Garcia HH. Efficacy of a 3‐day course of albendazole treatment in patients with a single neurocysticercosis cyst. Clinical Neurology and Neurosurgery 2006;108:193‐4. [DOI] [PubMed] [Google Scholar]
Carpio 1995 {published data only}
- Carpio A, Santillan F, Leon P, Flores C, Hauser WA. Is the course of neurocysticercosis modified by treatment with antihelminthic agents?. Archives of Internal Medicine 1995;155(18):1982‐8. [PubMed] [Google Scholar]
Lopez‐Gomez 2001 {published data only}
- Lopez‐Gomez M, Castro N, Jung H, Sotelo J, Corona T. Optimization of the single‐day praziquantel therapy for neurocysticercosis. Neurology 2001;57(10):1921‐30. [DOI] [PubMed] [Google Scholar]
Marquez‐Caraveo 2004 {published data only}
- Marquez‐Caraveo C, Gongoro‐Rivera F, Santos Zambrano J, Harnadez R, Soto‐Hernandes JL. Pre‐treatment with corticosteroids and a single cycle of high dose albendazole for subarachnoidal cysticercosis. Journal of Neurology, Neurosurgery and Psychiatry 2004;75:938‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Medina 1993 {published data only}
- Medina MT, Genton P, Montoya MC, Cordova S, Dravet C, Sotelo J. Effect of anticysticercal treatment on the prognosis of epilepsy in neurocysticercosis: a pilot trial. Epilepsia 1993;34(6):1024‐7. [DOI] [PubMed] [Google Scholar]
Proano 2006 {published data only}
- Proano JV, Madrazo I, Avelar F, Lopez‐Felix B, Diaz G, Grijalva I. Medical treatment for neurocysticercosis characterized by giant subarachnoid cysts. New England Journal of Medicine 2001;345:879‐85. [DOI] [PubMed] [Google Scholar]
Sanchetee 1994 {published data only}
- Sanchetee PC, Venkataraman S, Dhamija RM, Roy AK. Albendazole therapy for neurocysticercosis. Journal of the Association of Physicians in India 1994;42(2):116‐7. [PubMed] [Google Scholar]
Thussu 2008 {published data only}
- Thussu A, Chattopadhyay A, Sawhney AMS, Khandelwal N. Albendazole therapy for single small enhancing CT lesions (SSECTL) in the brain in epilepsy. Journal of Neurology, Neurosurgery and Psychiatry 2008;79:272‐5. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Cruz 1991 {published data only}
- Cruz M, Cruz I, Horton J. Albendazole versus praziquantel in the treatment of cerebral cysticercosis: clinical evaluation. Transactions of the Royal Society of Tropical Medicine and Hygiene 1991;85(2):244‐7. [DOI] [PubMed] [Google Scholar]
- Cruz M, Cruz I, Horton J. Clinical evaluation of albendazole and praziquantel in the treatment of cerebral cysticercosis. Southeast Asian Journal of Tropical Medicine and Public Health 1991;22:279‐83. [PubMed] [Google Scholar]
Pretell 2000 {published data only}
- Pretell EJ, Garcia HH, Custodio N, Padilla C, Alvarado M, Gilman RH, et al. Short regimen of praziquantel in the treatment of single brain enhancing lesions. Clinical Neurology and Neurosurgery 2000;102(4):215‐8. [DOI] [PubMed] [Google Scholar]
Takayanagui 1992 {published data only}
- Takayanagui OM, Jardim E. Therapy for neurocysticercosis: comparison between albendazole and praziquantel. Archives of Neurology 1992;49(3):290‐4. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
Gilman 2007 {published data only}
- Randomized study of albendazole in patients with epilepsy due to neurocysticercosis. Ongoing study May 2000.
Additional references
Burneo 2005
- Burneo G. Neurocysticercosis. http:www/eMedicine.com/neuro/topic629.htm (accessed 22 May 2006) 2005.
DeGiorgio 2004
- Giorgio CM, Medina MT, Duron R, Zee C, Escueta SP. Neurocysticercosis. Epilepsy Currents 2004;4(3):107‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Del Brutto 2006
- Brutto OH, Roos KL, Coffey CS, Garcia HH. Meta‐analysis: cysticidal drugs for neurocysticercosis: albendazole and praziquantel. Annals of Internal Medicine 2006;145(1):43‐51. [DOI] [PubMed] [Google Scholar]
Garcia 2002
- Garcia HH, Evans CA, Nash TE, Takayanagui OM, White AC Jr, Botero D, et al. Current consensus guidelines for treatment of neurocysticercosis. Clinical Microbiology Reviews 2002;15(4):747‐56. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jüni 2001
- Jüni P, Altman DG, Egger M. Systematic reviews in health care: assessing the quality of controlled clinical trials. BMJ 2001;323(7303):42‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kossoff 2005
- Kossoff EH. Neurocysticercosis. http:/www.emedicine.com/ped/topic1573.htm>eMedicine (accessed February 2006) 2005.
Lefebvre 2008
- Lefebvre C, Manheimer E, Glanville J. Chapter 6: Searching for studies. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.0 (updated February 2008). The Cochrane Collaboration, 2008. Available from www.cochrane‐handbook.org.
Leite 2000
- Leite JP, Terra‐Bustamante VC, Fernandes RMF, Santos AL, Chimelli L, Sakomoto AC, et al. Calcified neurocysticercosis lesions and postsurgery seizure control in temporal lobe epilepsy. Neurology 2000;55(10):1485‐91. [DOI] [PubMed] [Google Scholar]
Mazumdar 2007
- Mazumdar M, Pandharipande P, Poduri A. Does albendazole affect seizure remission and computed tomography response in children with neurocysticercosis? A systematic review and meta‐analysis. Journal of Child Neurology 2007;22(2):135‐42. [DOI] [PubMed] [Google Scholar]
Murthy 2006
- Murthy JM. Seizures associated with solitary cystericus granuloma: antiepileptic drugs for so long?. Neurology India 2006;54(2):141‐2. [PubMed] [Google Scholar]
Murthy 2007
- Murthy JMK, Rajshekar G. Economic evaluation of seizures associated with solitary cysticercus granuloma. Neurology India 2007;55(1):42‐5. [DOI] [PubMed] [Google Scholar]
Nogales‐Gaete 2006
- Nogales‐Gaete J, Arriagada CM, Salinas RR. Treatment of neurocysticercosis: a review [Tratamiento de la neurocisticercosi: revision critica]. Revista Médica de Chile 2006;134:789‐96. [DOI] [PubMed] [Google Scholar]
Review Manager 5 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.0. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2008.
Roman 2000
- Roman G, Sotelo J, Brutto O, Flissier A, Dumas M, Wadia N, et al. A proposal to declare neurocysticercosis an international reportable disease. Bulletin of the World Health Organization 2000;78(3):399‐406. [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Salinas 1999
- Salinas R, Prasad K. Drugs for treating neurocysticercosis (tapeworm infection of the brain). Cochrane Database of Systematic Reviews 1999, Issue 4. [Art. No.: CD000215. DOI: 10.1002/14651858.CD000215.pub2] [DOI] [PubMed] [Google Scholar]


