Abstract
Scarce data are available on the quality of life and psychosocial distress of patients with multiple endocrine neoplasia type 2 (MEN2), a genetic cancer syndrome caused by RET germline mutations. Carriers of RET mutations can face several challenges, including fear for the future, guilt for transmission of a germline mutation to an offspring, side effects of cancer treatment, coping behaviors in the face of a chronic and frequently incurable cancer, and difficulties in access to adequate health care. We have addressed the effects of genetic testing on the quality of life of patients with MEN2 and the lifelong physical and psychosocial challenges experienced by these patients. We have also suggested strategies to minimize the burden of living with this chronic condition and the perspectives on future studies to improve the health-related quality of life of the patients.
Keywords: quality of life, MEN2, medullary thyroid carcinoma, pheochromocytoma, hyperparathyroidism
Multiple endocrine neoplasia type 2 (MEN2) is a familial cancer syndrome caused by RET germline mutations [1, 2]. According to the revised American Thyroid Association guidelines for the management of medullary thyroid carcinoma (MTC), MEN2 should be divided into two syndromes: MEN2A and MEN2B. MEN2A includes four phenotypic variants: the classical form associated with MTC pheochromocytoma and primary hyperparathyroidism, MEN2A associated with cutaneous lichen amyloidosis, MEN2 associated with Hirschsprung disease, and isolated familial MTC. MEN2B is associated with early and aggressive MTC, pheochromocytoma, and a recognizable phenotype, including marfanoid body habitus, narrow long facies, and generalized ganglioneuromatosis of the digestive tract. In contrast to MEN2A, 75% of the patients with MEN2B will present with a de novo RET mutation (75%) [3].
Soon after the discovery that RET mutations cause MEN2, genetic testing became available, which improved the precision of identifying gene carriers and allowed for earlier prophylactic surgery and better chances of curing MTC [1, 2]. Despite the clear benefit of genetic testing, being a carrier of a tumor-predisposing gene mutation can result in considerable psychological distress and uncertainties toward family life, work life, and access to, and the financing of, lifelong medical treatments. Furthermore, the reduction in health-related quality of life (HR-QOL) due to chronic metastatic disease or treatment-related complications has been observed in these patients [4]. The present report has focused on the quality of life (QOL) of patients with MEN2 and strategies for patients to cope with this genetic cancer syndrome.
1. Methods
We conducted a literature review using PubMed search on the subject of QOL for patients with MEN2 and the psychological distress associated with genetic testing and treatment. The following search terms were used: MEN2 OR multiple endocrine neoplasia type 2 AND quality of life, MEN2 OR multiple endocrine neoplasia type 2 AND psychosocial, (MEN2 OR multiple endocrine neoplasia type 2 AND distress, and preimplantation and MEN2. The search found 28 studies, of which 7 were included in the present report. The other reports were unrelated to QOL for patients with MEN2 and were excluded. We also used the American Thyroid Association and National Comprehensive Cancer Network guidelines (available at: www.nccn.org). Because the reported data are scarce, we did not use a restriction for the year of publication.
2. Effect of Genetic Testing
Patients with cancer frequently have psychosocial problems, and survivors of cancer are approximately twice as likely to report medication use for anxiety and depression [5, 6]. Among the challenges faced by these patients are issues involving adjustment to illness, family conflict, economic burden, and worsening of HR-QOL.
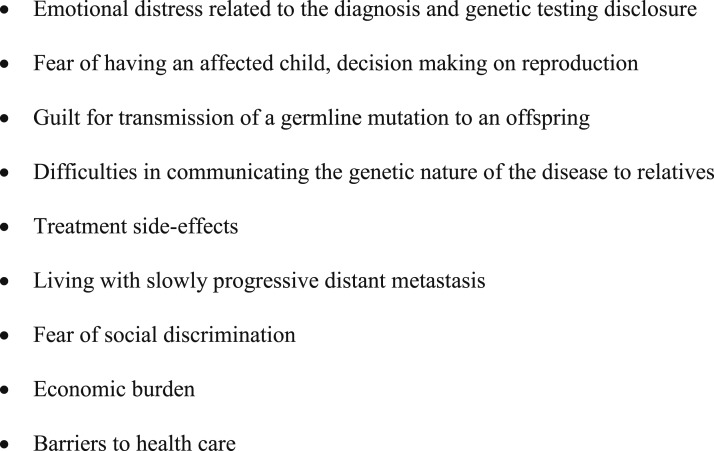
In addition to the burden associated with a cancer diagnosis, patients with MEN2 face further psychosocial problems, including stigmatization by positive mutation carrier status, fear of having an affected child, guilt for transmission of a germline mutation to offspring, living with slowly progressive distant metastasis, fear of social discrimination, and barriers to adequate health care (Fig. 1) [5, 7].
Figure 1.
Challenges faced by patients with MEN2.
Few reported studies have focused on the effects of genetic testing. Those that have were conducted using different strategies to evaluate psychological distress, including semidirected interviews, QOL questionnaires, and psychometric scales (Table 1).
Table 1.
HR-QOL Tools Used in MEN2
| Name of Measurement | Type | Purpose of Investigation | Investigator |
|---|---|---|---|
| Semistructured interviews and questionnaires | Specific for the study | Genetic testing | Grosfeld et al. [8], 1996 |
| HADS and SQLP | General | Genetic testing | Freyer et al. [9], 1999 |
| Semistructured interview | Specific for the study | Genetic testing | Grosfeld et al. [10], 2000 |
| STAI, SDS, UCL, SCL90 | General | ||
| Semidirected interview | Specific for the study | All aspects | Rodrigues et al. [4], 2017 |
| HADS | General | ||
| EORTC QLQ-C30 | Cancer specific | ||
| MINI-MAC | Cancer specific | ||
| PROMIS-29 | Chronic diseases | All aspects | Mongelli et al. [11], 2018a |
Abbreviations: PROMIS-29, Patient-Reported Outcomes Measurement Information System 29-item profile measure; SCL90, Symptom Checklist 90; SDS, Zung Self-Rating Depression Scale; SQLP, subjective quality of life profile; STAI, Spielberger Trait Anxiety Inventory; UCL, Utrecht Coping List.
This study included only patients with MEN2A.
In 1996, Grosfeld et al. [8] reported the results from a seminal study evaluating the psychosocial consequences of RET genetic analysis. The investigation was performed before the genetic test and 2 weeks and 1 year after disclosure of the test results. A total of 87 individuals, including proband and family members, underwent a semistructured interview and questionnaire (Symptom Checklist 90), before and after disclosure of the DNA analysis results. At baseline, most of the participants were very optimistic and believed that the test would permit better medical care and avoid burdensome clinical examinations and did not expect to endure suffering in the case of an unfavorable result. However, the parents were already apprehensive regarding the possibility of having a carrier child, which could result in social discrimination, and were also concerned about future reproduction decision-making. In the first evaluation after disclosure of the test results, 43% were anxious and 37% presented with somatic and depressive complaints. In addition, they related difficulties in communicating about the genetic nature and complexity of the disease to individuals outside the family. The initial feeling on receiving an unfavorable result was associated with relief owing to the better understanding about the risks associated with the disease. One year after test disclosure, a reduction to <20% for some psychosomatic complaints was observed. In contrast, family members without a RET mutation referred to being relieved but also demonstrated feelings of isolation, guilt, and concern about their affected relatives [8].
A subsequent study performed at two French centers evaluated the psychosocial effects of genetic testing for 77 individuals with MTC or at risk of MTC [9]. The individuals completed two questionnaires, including the hospital anxiety and depression scale (HADS) and subjective QOL profile. The cohort included 40 patients with RET-negative MTC, 20 patients with confirmed hereditary MTC, 15 RET mutation carriers awaiting surgery, and 2 relatives with RET-negative findings. No difference in the HADS score was observed between those with sporadic versus familial MTC. In contrast, the subjective QOL profile indicated a greater level of dissatisfaction for the carriers of a RET mutation (average score of 52 for noncarriers and 41 for carriers with a germline mutation; P = 0.01). Specifically, lower levels of satisfaction were observed regarding relationships in general (P = 0.002), people’s attitudes toward them (P = 0.003), medical follow-up (P = 0.015), the decision to have children (P = 0.02), and relationships with family (P = 0.007). Independent of carrier status, family life and medical environment were the most important issues affecting the QOL of these individuals [9]. The group of young patients with a RET mutation presented with the best scores for expectations for favorable changes, a reason not investigated in their study [9] but likely owing to a greater fighting spirit, which was observed in another study by Rodrigues et al. [4].
The study by Rodrigues et al. [4] also documented the stigmatization and burden of being a mutation carrier. Their cross-sectional study assessed 43 patients with MEN2 with ≥1 year of follow-up data available after the genetic diagnosis. The patients had had cured or stable MTC and could have had pheochromocytoma or primary hyperparathyroidism. The median follow-up period was 10.6 ± 8.2 years (range, 1 to 33 years). These patients underwent qualitative and quantitative psychological assessments using semidirected interviews, HADS, the European Organization for Research and Treatment of Cancer QOL questionnaire C30 (EORTC QLQ-C30), and the scale of mental adjustment to cancer (MINI-MAC). During the semidirected interviews, 31 patients (72%) affirmed being afraid of death after receiving the genetic diagnosis. A total of 30 patients (70%) had children and received genetic counseling, all except for 1 of these patients agreed to test their children. The results showed that 17 parents had at least one RET mutation-positive child, 6 parents had mutation-negative children, and 1 parent was waiting for the results. One third of parents (6 of 17) expressed feelings of blame for having transmitted the genetic mutation to their children. However, during the qualitative psychological interviews, such feelings were strongly present in most of the parents with a child carrying a RET mutation, with higher scores for insomnia (P = 0.004), dyspnea (P = 0.005), anxious preoccupation (P = 0.008), and weakness-discouragement (P = 0.049) compared with the patients who had no children or had children with negative mutations. In addition, lower scores were observed for the cognitive (P = 0.001), emotional (P = 0.028), and physical (P = 0.038) functioning of patients with RET mutation-positive children. This fact was attributed to a process of cognitive avoidance, a common coping mechanism of these patients that could have influenced their answers during the semidirected interviews, obscuring the feelings of guilt for most of the parents [4].
In the report by Grey and Winter [7] based heavily on patients’ records from the Association for Multiple Endocrine Neoplasia Disorders, the emotional distress related to transmission of a germline mutation to the offspring also surfaces as an important issue faced by carriers and their families. There is no doubt that the individual’s perception toward the genetic result will depend on several variables, including temperament, social and financial circumstances, disease severity, and family dynamics. Some individuals believed that mutation presence represented a greater pressure on the couple’s relationship. Others thought that the family bond was strengthened, and others affirmed that previous emotional problems had resurfaced. Another issue that has become evident with carriers diagnosed during childhood, who now are adults ready to start a family, is the decision on whether to have children and the ethical issues related to preimplantation genetic diagnosis. In that report [7], one patient’s quote exemplifies this ethical dilemma: “I really felt strange about the idea of selecting my child; if someone had done that to me, I wouldn’t have been born.”
Preimplantation genetic diagnosis involves in vitro fertilization and genetic analysis of the embryo before implantation, allowing couples to avoid the risk of transmitting a genetic condition to future offspring. It has been considered for patients with severe diseases and high penetrance such as MEN1 and MEN2 [12]. However, as demonstrated in a study involving 370 patients with a variety of hereditary cancer syndromes at the University of Texas M. D. Anderson Cancer Center, patients with MEN2 were the least likely to consider preimplantation genetic diagnosis because carriers can now be identified and prophylactic thyroidectomy performed, thereby significantly reducing the morbidity and mortality related to MTC [13].
3. Effect of the Disease and Its Treatment in QOL
Living with MEN2 poses challenges encompassing the disease itself and its treatment-related complications. In patients with MEN2, MTC will usually be indolent and associated with prolonged survival. However, patients with slowly progressive distant metastatic disease can face disease complications, such as diarrhea, flushing, and pain, which will negatively affect their global health status [4]. Furthermore, those patients who develop pheochromocytoma and primary hyperparathyroidism can experience symptoms related to these conditions [7].
In addition to the disease itself, patients with MEN2 will often experience treatment-related morbidities. Because MTC frequently involves the cervical lymph nodes, lymph node dissection, in addition to total thyroidectomy, will often be required. Depending on the extension of lymph node dissection, a number of complications can arise, in addition to permanent hypothyroidism, including hypoparathyroidism, recurrent larynx nerve palsy, and spinal accessory nerve dysfunction, each associated with a myriad of symptoms that affect QOL [3]. Patients with progressive metastatic disease will be treated with tyrosine kinase inhibitors, which have been commonly associated with several adverse events that can affect QOL. Furthermore, patients with bilateral pheochromocytoma requiring bilateral adrenalectomy are at risk of developing symptoms related to hypoadrenalism [7]. Despite the clear presence of several disease- and treatment-related morbidities observed in the routine clinical management of these patients, clinical studies investigating the psychological effect of living with MEN2 and its treatment-related comorbidities are lacking; however, it is reasonable to believe that it can be associated with lower HR-QOL.
The study by Rodrigues et al. [4] investigated not only the psychological distress, but also disease-related issues that affect QOL. The investigators included 43 patients with MEN2 with long-term follow-up (mean, 10.6 ± 8.2 years; range, 1 to 33 years). These patients were evaluated using semidirected interviews with the HADS, EORTC QLQ-C30, and MINI-MAC scales. All patients had MTC (no evidence of disease or stable or slowly progressive disease), 18 (42%) had had pheochromocytoma, 12 (28%) had postoperative hypoparathyroidism, and 12 (28%) had adrenal insufficiency after bilateral adrenalectomy. A total of 26 patients had a RET codon 634 mutation (61%), 13 patients had a RET codon 620 mutation (30%), 3 patients had a RET codon 804 mutation, and 1 patient had a codon 918 mutation. Overall distress was present in 46% of the patients, with high scores (>8) for depression and anxiety symptoms in 26% and 42% of the patients, respectively. Eleven patients (25%) required individual psychotherapy. Patients who were better informed about the disease presented with lower mean score values for depression and anxiety and higher scores for role, cognitive, and emotional functioning.
In terms of global health, most patients were in satisfactory global health when assessed using the EORTC QLQ-C30 for both physical and emotional aspects (mean score, 68.1 ± 22.3 from a maximum of 100). However, it was clear that social (mean score, 81.4 ± 28.9) and physical (mean score, 79.3 ± 21.2) functioning was better than emotional functioning (59.7 ± 32.8). No differences in HR-QOL were observed between patients with and without postoperative hypoparathyroidism; however, the number of patients was small. Using the MINI-MAC scale, a scale of mental adjustment to cancer that evaluates how the individual copes with the disease, what was observed was that patients with adrenal insufficiency and patients who had undergone several neck surgeries had the highest score of “fighting spirit,” which is a positive attitude toward the disease and relates to adherence to treatment and to investigational procedures. However, overall, patients presented with a high level of resignation and acceptance of the disease. Another coping mechanism frequently observed was cognitive avoidance, meaning that outside the medical office, they prefer to forget about the disease. Cognitive avoidance was strongest in the group of patients with RET mutation-positive children, as discussed in the previous section. In summary, in this cohort of patients with longstanding stable and asymptomatic disease, the most important factors associated with psychosocial distress and QOL reduction were having children with a RET mutation and the fear of disease recurrence or progression [4].
A recent study that evaluated QOL in patients with MEN2A included 45 patients recruited from a support group for individuals living with all types of multiple endocrine neoplasias (American Multiple Endocrine Neoplasia Support). The inclusion criteria were individuals aged ≥18 years with a physician-given diagnosis of MEN2A, who were living in the United States. Each individual completed a HR-QOL questionnaire, the Patient-Reported Outcomes Measurement Information System 29-item profile measure, a National Institutes of Health–funded diagnostic measure of physical, mental, and social health in adults living with chronic conditions. These individuals with MEN2A reported worse QOL in all seven domains addressed—anxiety, depression, fatigue, pain, physical functioning, sleep disturbance, and ability to participate in social roles compared with the general US population. Moreover, compared with individuals with other chronic conditions, they reported physical functioning scores similar to those of patients with MEN1, major depressive disorder, and neuroendocrine tumors and better physical functioning compared with patients with congestive heart failure, chronic obstructive pulmonary disease, and rheumatoid arthritis. However, the scores for the fatigue levels were as high as the scores observed in patients with major depressive disorder and congestive heart failure and greater than those observed for patients with chronic obstructive pulmonary disease and rheumatoid arthritis. Despite showing worse HR-QOL for patients with MEN2A compared with the US normative data and similar to that of patients with chronic diseases, it is unclear whether the inclusion of any patient with MEN2A, possibly encompassing patients with advanced MTC, symptomatic pheochromocytoma, and uncontrolled treatment-related complications, might have affected the answers of these patients [11].
4. How to Minimize the Effects on QOL
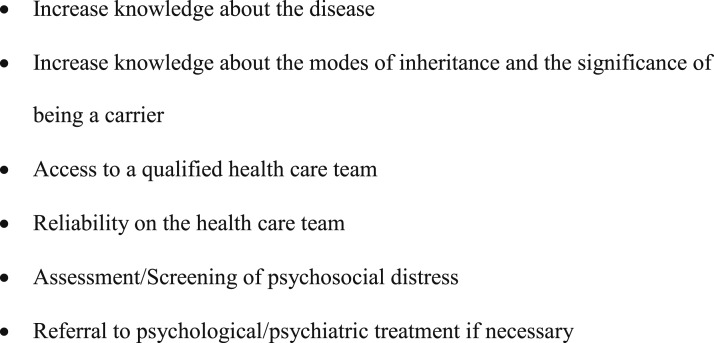
Some strategies are available that can be implemented by health care professionals to help patients with MEN2 cope with the disease. First, providing a good understanding of the disease and its mode of inheritance has been shown to reduce the levels of depression and anxiety symptoms [4]. Second, before genetic testing, patients should understand the meaning of being a carrier and the psychosocial implications of DNA testing. Third, those with unfavorable test outcomes might require more attention by the medical team, including the genetic counseling team [10]. In these cases, the parents of children with a RET mutation should be carefully evaluated and offered psychological support if necessary (Fig. 2) [4, 7]. Patients should understand that an early diagnosis and treatment will minimize the morbidity and affect the prognosis favorably. This information will help patients in coping with the disease and their acceptance of medical treatments. Additionally, adequate postoperative replacement therapy will improve the well-being of these patients. Moreover, it is also important to teach patients who have undergone bilateral adrenalectomy how to proceed in emergency situations [7].
Figure 2.
Strategies to cope with HR-QOL tools used in MEN2.
Assessing the psychological distress at early stages and monitoring it throughout the follow-up period will help to identify patients in need of psychological and/or psychiatric treatment [4]. Finally, whenever possible, patients should be treated in centers of expertise in this complex disease [5, 7], and participation in support groups such as the Association for Multiple Endocrine Neoplasia Disorders (American Multiple Endocrine Neoplasia Support) will undoubtedly help patients and relatives cope with the disease [7]. Sharing and comparing experiences with other patients and families with similar problems can reduce the feelings of isolation, allow individual and social concerns to be addressed, ease the anxiety related to the threat of future problems, such as a new medical diagnosis and interventions, and can help identify the availability of new treatments [4].
A strong medical team–patient relationship is critical for the emotional support of these patients. Physicians, psychologists, and genetic counselors should motivate patients to gain insight into the nature of the disease, providing time for them to ask questions and resolve their doubts. It is important that patients obtain their knowledge about the disease, genetic transmission, potential treatment, and outcomes from their medical team and from recognized patient support groups to avoid misleading information obtained from digital media. It is also important that children receive age-appropriate information in a friendly and caring way [14].
The information obtained from the present report should be eye-opening to the medical team involved in the care of patients with MEN2. Although we have shown the negative psychosocial effect of being a carrier of a cancer hereditary syndrome and the anxiety toward future suffering, we have also clearly demonstrated the power that the medical team has to modify these feelings. It has been shown that after the initial effects of an unfavorable result from genetic testing, a good understanding about the disease and available treatments, in addition to the support of a reliable and experienced medical team, has been associated with a substantial reduction in psychosomatic complaints [8].
5. Conclusions and Perspectives
Despite the association with a substantial psychosocial impact, RET genetic testing has allowed for an earlier diagnosis of MTC and pheochromocytoma, thereby reducing or avoiding MEN2-related morbidities and mortality. For most patients, the initial effect of diagnosis seems to ameliorate over time, especially if patients have the opportunity to work through the emotional effects of being a carrier of a hereditary syndrome.
The important issues faced by these patients also include the guilt of transmitting a mutation to their children and the constant fear of recurrence or progression of MTC. Therefore, it is important that these patients be cared for by a multidisciplinary medical team able to provide information about the disease, specialized medical care, and good psychological support.
Acknowledgments
Disclosure Summary: The authors have nothing to disclose.
Glossary
Abbreviations:
- EORTC QLQ-C30
European Organization for Research and Treatment of Cancer QOL questionnaire C30
- HADS
hospital anxiety and depression scale
- HR-QOL
health-related quality of life
- MEN2
multiple endocrine neoplasia type 2
- MTC
medullary thyroid carcinoma
- QOL
quality of life
References and Notes
- 1. Mulligan LM, Kwok JB, Healey CS, Elsdon MJ, Eng C, Gardner E, Love DR, Mole SE, Moore JK, Papi L, Ponder MA, Telenius H, Tunnacliffe A, Ponder BAJ. Germ-line mutations of the RET proto-oncogene in multiple endocrine neoplasia type 2A. Nature. 1993;363(6428):458–460. [DOI] [PubMed] [Google Scholar]
- 2. Hofstra RM, Landsvater RM, Ceccherini I, Stulp RP, Stelwagen T, Luo Y, Pasini B, Höppener JWM, van Amstel HKP, Romeo G, Lips CJM, Buys CHCM. A mutation in the RET proto-oncogene associated with multiple endocrine neoplasia type 2B and sporadic medullary thyroid carcinoma. Nature. 1994;367(6461):375–376. [DOI] [PubMed] [Google Scholar]
- 3. Wells SA Jr, Asa SL, Dralle H, Elisei R, Evans DB, Gagel RF, Lee N, Machens A, Moley JF, Pacini F, Raue F, Frank-Raue K, Robinson B, Rosenthal MS, Santoro M, Schlumberger M, Shah M, Waguespack SG; American Thyroid Association Guidelines Task Force on Medullary Thyroid Carcinoma. Revised American Thyroid Association guidelines for the management of medullary thyroid carcinoma. Thyroid. 2015;25(6):567–610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rodrigues KC, Toledo RA, Coutinho FL, Nunes AB, Maciel RMB, Hoff AO, Tavares MC, Toledo SPA, Lourenço DM Jr. Assessment of depression, anxiety, quality of life, and coping in long-standing multiple endocrine neoplasia type 2 patients. Thyroid. 2017;27(5):693–706. [DOI] [PubMed] [Google Scholar]
- 5. National Comprehensive Cancer Network NCCN clinical practice guidelines in oncology (NCCN guidelines) for distress management. Available at: www.nccn.org version 2. Accessed 1 October 2018. [DOI] [PMC free article] [PubMed]
- 6. Hawkins NA, Soman A, Buchanan Lunsford N, Leadbetter S, Rodriguez JL. Use of medications for treating anxiety and depression in cancer survivors in the United States. J Clin Oncol. 2017;35(1):78–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Grey J, Winter K. Patient quality of life and prognosis in multiple endocrine neoplasia type 2. Endocr Relat Cancer. 2018;25(2):T69–T77. [DOI] [PubMed] [Google Scholar]
- 8. Grosfeld FJ, Lips CJ, Ten Kroode HF, Beemer FA, Van Spijker HG, Brouwers-Smalbraak GJ. Psychosocial consequences of DNA analysis for MEN type 2. Oncology (Williston Park). 1996;10(2):141–146; discussion 146, 152, 157. [PubMed] [Google Scholar]
- 9. Freyer G, Dazord A, Schlumberger M, Conte-Devolx B, Ligneau B, Trillet-Lenoir V, Lenoir GM. Psychosocial impact of genetic testing in familial medullary-thyroid carcinoma: a multicentric pilot-evaluation. Ann Oncol. 1999;10(1):87–95. [DOI] [PubMed] [Google Scholar]
- 10. Grosfeld FJ, Lips CJ, Beemer FA, Blijham GH, Quirijnen JM, Mastenbroek MP, ten Kroode HF. Distress in MEN 2 family members and partners prior to DNA test disclosure: multiple endocrine neoplasia type 2. Am J Med Genet. 2000;91(1):1–7. [DOI] [PubMed] [Google Scholar]
- 11. Mongelli MN, Peipert BJ, Goswami S, Helenowski I, Yount SE, Sturgeon C. Quality of life in multiple endocrine neoplasia type 2A compared with normative and disease populations. Surgery. 2018;164(3):546–552. [DOI] [PubMed] [Google Scholar]
- 12. Chen S, Li S, Zhang J, Zhang L, Chen Y, Wang L, Jin L, Hu Y, Qi X, Huang H, Xu C. Preimplantation genetic diagnosis of multiple endocrine neoplasia type 2A using informative markers identified by targeted sequencing. Thyroid. 2018;28(3):281–287. [DOI] [PubMed] [Google Scholar]
- 13. Rich TA, Liu M, Etzel CJ, Bannon SA, Mork ME, Ready K, Saraiya DS, Grubbs EG, Perrier ND, Lu KH, Arun BK, Woodard TL, Schover LR, Litton JK. Comparison of attitudes regarding preimplantation genetic diagnosis among patients with hereditary cancer syndromes. Fam Cancer. 2014;13(2):291–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lips CJ, Höppener JW, Van Nesselrooij BP, Van der Luijt RB. Counselling in multiple endocrine neoplasia syndromes: from individual experience to general guidelines. J Intern Med. 2005;257(1):69–77. [DOI] [PubMed] [Google Scholar]