Notes
Editorial note
This review is superseded by the published Cochrane Review, Saif‐Ur‐Rahman 2024 [https://doi.org/10.1002/14651858.CD014573], which considers only the oral killed vaccines because the live oral vaccines do not have World Health Organization (WHO) prequalification. Saif‐Ur‐Rahman 2024 also considered only currently available WHO pre‐qualified oral killed cholera vaccines (Dukoral, Shanchol, and Euvichol/Euvichol‐Plus).
Abstract
Background
Cholera is a cause of acute watery diarrhoea which can cause dehydration and death if not adequately treated. It usually occurs in epidemics, and is associated with poverty and poor sanitation. Effective, cheap, and easy to administer vaccines could help prevent epidemics.
Objectives
To assess the effectiveness and safety of oral cholera vaccines in preventing cases of cholera and deaths from cholera.
Search methods
In October 2010, we searched the Cochrane Infectious Disease Group Specialized Register; Cochrane Central Register of Controlled Trials (CENTRAL); MEDLINE; EMBASE; LILACS; the metaRegister of Controlled Trials (mRCT), and the WHO International Clinical Trials Registry Platform (ICTRP) for relevant published and ongoing trials.
Selection criteria
Randomized or quasi‐randomized controlled trials of oral cholera vaccines in healthy adults and children.
Data collection and analysis
Each trial was assessed for eligibility and risk of bias by two authors working independently. Data was extracted by two independent reviewers and analysed using the Review Manager 5 software. Outcomes are reported as vaccine protective efficacy (VE) with 95% confidence intervals (CIs).
Main results
Seven large efficacy trials, four small artificial challenge studies, and 29 safety trials contributed data to this review.
Five variations of a killed whole cell vaccine have been evaluated in large scale efficacy trials (four trials, 249,935 participants). The overall vaccine efficacy during the first year was 52% (95% CI 35% to 65%), and during the second year was 62% (95% CI 51% to 62%). Protective efficacy was lower in children aged less than 5 years; 38% (95% CI 20% to 53%) compared to older children and adults; 66% (95% CI 57% to 73%).
One trial of a killed whole cell vaccine amongst military recruits demonstrated 86% protective efficacy (95% CI 37% to 97%) in a small epidemic occurring within 4 weeks of the 2‐dose schedule (one trial, 1426 participants). Efficacy data is not available beyond two years for the currently available vaccine formulations, but based on data from older trials is unlikely to last beyond three years.
The safety data available on killed whole cell vaccines have not demonstrated any clinically significant increase in adverse events compared to placebo.
Only one live attenuated vaccine has reached Phase III clinical evaluation and was not effective (one trial, 67,508 participants). Two new candidate live attenuated vaccines have demonstrated clinical effectiveness in small artificial challenge studies, but are still in development.
Authors' conclusions
The currently available oral killed whole cell vaccines can prevent 50 to 60% of cholera episodes during the first two years after the primary vaccination schedule. The impact and cost‐effectiveness of adopting oral cholera vaccines into the routine vaccination schedule of endemic countries will depend on the prevalence of cholera, the frequency of epidemics, and access to basic services providing rapid rehydration therapy.
Keywords: Adult; Child; Humans; Administration, Oral; Cholera; Cholera/prevention & control; Cholera Vaccines; Cholera Vaccines/administration & dosage; Cholera Vaccines/adverse effects; Randomized Controlled Trials as Topic; Vaccines, Attenuated; Vaccines, Attenuated/administration & dosage; Vaccines, Attenuated/adverse effects
Plain language summary
Oral vaccines for preventing cholera
Researchers in The Cochrane Collaboration conducted a review of the effect of oral vaccines for preventing cholera. After searching for relevant studies, they identified 48 relevant articles. Their findings are summarized below.
What is cholera and how do vaccines work?
Cholera is a severe form of diarrhoea. People get cholera by drinking water or eating food that has been contaminated with the bacteria (Vibrio cholera). Some people only become mildly ill, but some become extremely unwell with watery diarrhoea and vomiting. These people can become dehydrated very quickly and if untreated 25% to 50% can die.
The disease spreads rapidly in poor communities, especially where there is no sanitation or a lack of clean water. In refugee camps or following natural disasters a cholera epidemic can kill many hundreds of people very quickly.
Oral cholera vaccines work by giving people a small dose of the cholera bacteria to swallow. This dose of bacteria has been killed or changed so that it does not cause diarrhoea but is still able to make the person immune to natural cholera. There are three oral cholera vaccines currently available.
What the research says about the effects of using current oral vaccines
Oral cholera vaccines will decrease your risk of getting cholera if you live somewhere where cholera is common, but they won't remove the risk completely
Oral cholera vaccines probably don't have any major side effects when they are taken, but rare or late complications cannot be excluded.
Summary of findings
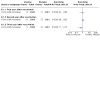
Summary of findings 1. Summary of findings table: Oral killed whole cell vaccines for preventing cholera.
| Oral killed whole cell vaccines for preventing cholera | ||||||
|
Patient or population: Adults and children Settings: Endemic areas Intervention: Killed whole cell vaccines administered orally Comparison: Placebo | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Vaccine efficacy (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Not being vaccinated | Being vaccinated | |||||
| How many people get cholera during the first 2 years after vaccination? | Children aged less than 5 years | VE 38% (20% to 53%) | 29005 (4 studies5) | high1,2,3,4 | Oral cholera vaccine prevents just over one third of cholera illnesses. | |
| 90 per 10,000 | 56 per 10,000 (42 to 72) | |||||
| Older children and adults | VE 66% (57% to 73%) | 214066 (4 studies5) | high1,2,3,4 | Oral cholera vaccine prevents two thirds of cholera illnesses | ||
| 30 per 100,000 | 10 per 100,000 (8 to 13) | |||||
| How long does the protection last? | 3rd year after vaccination; all ages |
VE 30% (2% to 50%) |
58184 (1 study7) |
moderate6 | Oral cholera vaccine is probably less effective in the third year | |
| 30 per 10,000 |
21 per 10,000 (15 to 29) |
|||||
| 4th year after vaccination; all ages |
VE ‐5% (‐84% to 40%) |
56613 (1 study7) |
moderate6 | Oral cholera vaccine is probably ineffective after 4 years | ||
| 30 per 100,000 |
32 per 10,000 (18 to 55) |
|||||
| Are there any side effects? | All ages | 44,924 (14 studies) |
moderate8 | Oral cholera vaccines probably don’t have more side effects than a placebo | ||
| *The basis for the assumed risk (eg the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; VE: Vaccine protective efficacy. | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 No study limitations: Clemens 1988 Bangladesh and Taylor 2000 Peru are individually randomized trials with adequate allocation concealment and blinding. Sur 2009 India is a cluster randomized study, and Trach 1997 is a quasi‐randomized study without allocation concealment. 2 No serious inconsistency: The findings from all three trials (4 comparisons) were remarkably similar and any observed differences between the vaccines is well within the bounds of random error. It should be noted that a protective effect with the most widely available vaccine (WC‐rBS/Dukoral®), given in its recommended schedule of two doses, was not shown until after a booster dose at 10 months. 3 No serious indirectness: The trials are from several endemic countries and include both adults and children. This evidence could reasonably be applied to other endemic settings where the background risk of cholera is known and used to calculate an absolute benefit with vaccination. 4 No serious imprecision: The finding is of a statistically significant benefit with vaccination. The clinical importance will depend on the incidence of cholera in the population. 5 Clemens 1988 Bangladesh: a 3‐arm trial of WC (currently unavailable), WC‐BS (currently unavailable) vs placebo, Taylor 2000 Peru; WC‐rTB (Dukoral®) versus placebo, Trach 1997 Vietnam; vWC (a variant WC vaccine only available in Vietnam) vs placebo, Sur 2009 India; BivWC (Shanchol®) vs placebo. 6 Serious indirectness: The exact vaccines used in this trial are no longer available but the current vaccines are very similar in composition. Downgraded by 1. 7 Only Clemens 1988 Bangladesh followed participants beyond 2‐years. 8 Fourteen studies assessed for side effects during the first 2 weeks after vaccination. No individual side effect has been shown to be more common with the oral cholera vaccine than with placebo. This data cannot exclude rare or late complications. Downgraded by 1.
Background
Description of the condition
Cholera is an acute intestinal infection, caused by the bacterium Vibrio cholerae. Most infected persons do not become ill, although the bacteria are present in the faeces for 7 to 14 days. Over 90% of those who do become ill experience a mild diarrhoeal episode that is indistinguishable from other diarrhoeal illnesses. However, a proportion develop typical cholera symptoms, with sudden onset of profuse watery diarrhoea, usually accompanied by vomiting, which can lead to severe dehydration (WHO 2000a). If untreated, around 25% to 50% of patients with the typical cholera symptoms will die, but if given adequate rehydration treatment the deaths can be reduced to less than 1% (WHO 2000b). In 2005 there were a total of 131,943 reported cases of cholera throughout the world, including 2272 deaths (WHO 2006a). Ninety‐five percent of the reported cases were in Africa, but it is likely that many more cases, both in Africa and elsewhere, went unreported.
V. cholerae is transmitted mainly through the ingestion of faecally contaminated water or food, and can spread rapidly especially where there is poverty, poor hygiene and lack of sanitation. It can lead to serious outbreaks; in 2005 the World Health Organization (WHO) confirmed 49 different outbreaks in 36 countries (WHO 2006a), and in vulnerable populations epidemics can be devastating; in July 1994, in the refugee camps of Goma in Zaire, there were 70,000 cases with 12,000 deaths (Sanchez 1997). More recently, large epidemics have occurred in Zimbabwe (WHO 2009), and Haiti (WHO 2010a).
V. cholerae colonise the gut by attaching themselves to receptors in the mucosa of the upper small intestine (Sack 2004). Pathogenicity is mediated by a toxin, composed of two subunits; A and B. The B subunit is involved in binding the bacteria to the epithelial cell surface. It has no toxic effect, but does stimulate the host's immune response. The soluble A subunit is then released into the mucosal cells and causes hypersecretion of fluids and electrolytes, which lead to the typical symptoms of the disease (Girard 2005). Colonisation of the intestine can be inhibited by host antibodies generated in response to previous infection with V. cholerae.
There are over two hundred distinct serological groups of V. cholerae, classified on the basis of the 'O' antigen present on the cell surface, of which only two are known to cause epidemics: serogroups O1 and O139. V. cholerae O1 can be further classified into two biotypes: classical and El Tor. These in turn can each be divided into three serotypes: Ogawa, Inaba and Hikojima (Heymann 2008). The epidemic strains currently in circulation worldwide are the El Tor biotype of V. cholerae O1, which was first recognised in Indonesia in 1961 and has now spread to many other countries in Asia, Europe, Africa, and Latin America; and the Bengal strain of V. cholerae O139 which began in 1992 in India and Bangladesh, and remains restricted to Asia (WHO 2000b). The classical biotype of V. cholerae O1 is also known to cause epidemics, though these are now uncommon, and non‐O1/non‐O139 strains occasionally cause sporadic cases of gastroenteritis (Heymann 2008).
There is evidence that persons with blood group O have overall lower risk of cholera, but increased susceptibility to severe cholera (Harris 2005). The mechanism for this effect is not known, but it should be taken into account when assessing vaccine effectiveness.
Description of the intervention
Widespread use of cholera vaccines began in the 1960s. The vaccines then in use were composed of whole V. cholerae O1 cells, killed using formalin, phenol or heat, and administered by injection. In the 1970s, these injected whole cell vaccines fell out of favour (Bhadra 1994), as it was perceived that they had a low efficacy (around 50%), provided only short‐term immunity (3 to 6 months), and had an unacceptable rate of side effects. A Cochrane review first published in 1998, however, found that the duration and efficacy of the whole cell injected vaccines may have been underestimated: it was 54% at seven months (based on 18 trials) and 46% at one year (based on 14 trials). Protection waned by the second year in children under five, but persisted into the third year for those over the age of five years (Graves 2010). Nevertheless, injected vaccines are no longer in use or available, and attention is now focused on vaccines administered by the oral route.
Two main types of oral vaccines have been investigated in clinical trials: inactivated vaccines (containing killed whole cells of V. cholerae), and live attenuated vaccines (containing genetically modified, non‐pathogenic strains of V. cholerae). In addition, subunit vaccines have been tested which consist only of cell components (antigens). The live attenuated vaccines are usually given as a single dose, whereas killed whole cell vaccines may require two or three doses at one week intervals to produce an adequate immunological response. Three vaccine formulations are currently available (WHO 2010b):
WC‐rBS (Dukoral®): A monovalent inactivated vaccine containing killed whole cells of V. cholerae O1 plus additional recombinant cholera toxin B subunit. Produced by SBL Vaccine/Crucell, Sweden.
BivWC (Shanchol®): A bivalent inactivated vaccine containing killed whole cells of V. cholerae O1 and V. cholerae O139. Produced by Shantha Biotechnics, India.
BivWC (mORCVAX®): A bivalent inactivated vaccine containing killed whole cells of V. cholerae O1 and V. cholerae O139. Produced by VABIOTECH, Vietnam and only available in Vietnam.
However, there are many other candidate vaccines at various stages of clinical development (Girard 2005).
How the intervention might work
Vaccines work by stimulating immunity against a pathogen which has been killed, attenuated or otherwise rendered incapable of causing disease, in order to prevent or mitigate the effects of infection with the natural pathogen if it subsequently occurs. The route of administration of a vaccine may influence its immunogenicity and acceptability. Oral vaccines have the potential to stimulate local immunity within the mucosa of the gut, preventing the colonisation and multiplication of V. cholerae. Since cholera is transmitted orally, oral vaccines may thus have more direct effect than injected vaccines which stimulate immunity in the blood. Oral vaccines are also potentially easier to administer, more acceptable to patients than injected vaccines, and have a reduced risk of transmitting blood borne infections (Holmgren 2005).
The cholera toxin B subunit contains similar antigens to those found in enterotoxigenic Escherichia coli (ETEC); an important cause of diarrhoea in many parts of the world (Huilan 1991), and the most common cause of diarrhoea in people travelling from industrialised to developing countries (Sack 2004). Oral cholera vaccines may therefore provide significant cross‐protection against ETEC infection and the vaccine is already licensed in many countries for preventing ETEC diarrhoea in travellers. This aspect of cholera vaccine use will be covered by another Cochrane review on vaccines to prevent ETEC.
Why it is important to do this review
Oral vaccines have been licensed in many countries and are currently used mainly by travellers (Hill 2006). However, there has not been a full review of the relative effectiveness of different types of oral vaccine, the duration of their efficacy, or their adverse effects.
These vaccines may also have an important role in preventing cholera in areas where it is endemic, or in the prevention or control of outbreaks in high risk settings. The killed whole cell vaccine (WC/rBS) has been used in crisis situations in Darfur, Sudan (WHO 2006b), and in Aceh, Indonesia in 2005 after the tsunami (WHO 2006c). It has also been evaluated in an endemic situation in Beira, Mozambique in 2003‐2004 (Lucas 2005). The live CVD 103‐HgR vaccine was used during a cholera outbreak in Pohnpei, Federated States of Micronesia in 2000 (Calain 2004).
This review is one of a series of three that replaces a previous Cochrane review 'Vaccines for preventing cholera', which was first published in 1998 and updated in 2001. An updated stable review of injected vaccines (Graves 2010) has now replaced the original cholera vaccines review; it will be accompanied by this review of oral vaccines and a further review assessing the effects of vaccines (including cholera vaccine) on infection with ETEC.
Objectives
To assess the effectiveness and safety of oral cholera vaccines in preventing cases of cholera and deaths from cholera.
Methods
Criteria for considering studies for this review
Types of studies
Randomized or quasi‐randomized controlled trials, including cluster‐randomized trials.
Types of participants
Well adults or children (without symptoms of cholera).
Types of interventions
Intervention
Any vaccine that is designed to prevent cholera and is administered by the oral route.
Control
Placebo, control vaccine, no intervention or different dose or schedule of cholera vaccine.
Types of outcome measures
Primary outcomes
Cases of cholera.
Deaths from cholera.
Secondary outcomes
Cases of severe dehydrating diarrhoea.
Cases of all‐cause diarrhoea.
Deaths from severe dehydrating diarrhoea.
Deaths from all causes.
Serious adverse events leading to hospital admission or death.
Other adverse events.
Search methods for identification of studies
We attempted to identify all relevant studies regardless of language or publication status (published, unpublished, in press, and in progress). The search was conducted in January 2010 and repeated in October 2010.
Electronic searches
Published studies
We searched the following databases using the search terms detailed in Table 2: The Cochrane Infectious Disease Group Specialized Register; the Cochrane Central Register of Controlled Trials (CENTRAL), published in The Cochrane Library; MEDLINE; EMBASE; and LILACS.
1. Detailed Search Strategy.
| Search set | CIDG SR^ | CENTRAL | MEDLINE^^ | EMBASE^^ | LILACS^^ |
| 1 | cholera | cholera | cholera | cholera | cholera |
| 2 | Vaccin* | Vaccin* | Vaccin* | Vaccin$ | Vaccin$ |
| 3 | 1 or 2 | 1 or 2 | 1 or 2 | 1 or 2 | 1 or 2 |
| 4 | CHOLERA VACCINES | CHOLERA VACCINES | CHOLERA‐VACCINE | ||
| 5 | 3 or 4 | 3 or 4 | 3 or 4 | ||
| 6 | Limit 5 to human | Limit 5 to humans |
Ongoing studies
We also searched the metaRegister of Controlled Trials (mRCT) and the WHO International Clinical Trials Registry Platform (ICTRP) for ongoing trials using "cholera" and "vaccin*" as search terms.
Searching other resources
Researchers, organizations, and pharmaceutical companies
We attempted to contact individual researchers working in the field for unpublished and ongoing trials.
Reference lists
We also checked the reference lists of all studies identified by the above methods for any additional studies relevant to this review.
Data collection and analysis
Selection of studies
Two authors (PG, KA or DS) independently screened all citations and abstracts identified by the search strategy for potentially eligible studies. Full reports of those studies deemed eligible were formally assessed for inclusion in the review using a pre‐designed eligibility form based on the inclusion criteria. All reports were scrutinised for evidence of dual publication.
Trials where participants were given an artificial challenge with V. cholerae after vaccination (i.e. by ingesting a standardized dose of bacteria), were included but assessed separately from studies assessing efficacy against natural infection. Trials reporting only safety or adverse event data were included and summarized only if primary outcome data (an efficacy trial) for the same vaccine was already available. Trials testing the vaccine for purposes other than safety or prevention of cholera (for example, for prevention of diarrhoea associated with ETEC, or 'traveller's diarrhoea') were excluded.
Where it was unclear whether a trial should be included we attempted to contact the authors for clarification, and resolved any differences in opinion through discussion. We obtained translated copies of those papers published in languages other than English. The studies which did not meet the criteria for inclusion, and the reasons for their exclusion, are listed in the 'Characteristics of excluded studies' table.
Data extraction and management
For each included trial, two authors (KA, KZ or DS) independently extracted information (using a pre‐tested data extraction form) on the characteristics of the trial (study design, study dates and duration, study location, setting, and source of funding); the participants (the inclusion and exclusion criteria); the intervention (the type of vaccine, type of placebo, dose and immunisation schedule); and the outcomes presented in the papers.
For individually randomized trials, two authors independently extracted the number of participants randomized to each group, and the number experiencing the outcome. Data on the number of doses received and the number of participants lost to follow‐up has been calculated and recorded for each group.
For cluster‐randomized trials, we recorded the number of clusters in the trial, the average (mean) size of clusters, the unit of randomization (e.g. household or institution), and reported estimates of the intracluster correlation coefficient (ICC) for each outcome. If the trial results were adjusted for clustering we extracted the point estimate and the 95% confidence interval (CI), and also the unadjusted data so that we could calculate an adjusted risk ratio to present in a meta‐analysis. Where results were not adjusted for clustering, we extracted the same data as for individually randomized trials, and adjusted the results according to known estimates of the ICC.
Adverse event data has been extracted for each individual type of event wherever possible. Where adverse events were reported for more than one dose, the number of people reporting each side effect after each dose has been recorded. Where trials reported the occurrence of adverse events over time following a single dose, if possible we recorded the proportion of people affected during each time period. If the denominator or total number of people affected for each time period is not clear, then events occurring in the first time period (typically 24 hours) after each dose was recorded.
Where data was missing or incomplete we contacted the authors for clarification. In cases of disagreement we double checked the data extraction and resolved the disagreement through discussion.
Assessment of risk of bias in included studies
Two authors (KZ, KA or DS) independently assessed the risk of bias of the individually randomized trials using the 'The Cochrane Collaboration's tool for assessing the risk of bias' (Higgins 2008). We followed this guidance to assess whether adequate steps had been taken to reduce the risk of bias across six domains: sequence generation; allocation concealment; blinding (of participants, personnel, and outcome assessors); incomplete outcome data; selective outcome reporting; and other sources of bias. For cluster‐randomized trials we also considered the possible effects of particular biases which occur with this study design: recruitment bias, baseline imbalance, loss of clusters, incorrect analysis and comparability to individually randomized trials (Higgins 2008).
For sequence generation and allocation concealment we report the methods used. For blinding we describe who was blinded and the blinding method. For incomplete outcome data we report the percentage and proportion lost to follow up. For selective outcome reporting we state any discrepancies between the methods used and the results in terms of the outcomes measured or the outcomes reported. For other biases we describe any other trial features that we think could have affected the trials result (e.g. if the trial was stopped early). We also report components of study design or conduct which may have introduced any bias specific to cluster‐randomized trials.
We have categorized our judgments as 'yes' (low risk of bias), 'no' (high risk of bias), or 'unclear', and this information has been used to guide the interpretation of the results. Where our judgement for efficacy trials was unclear we attempted to contact the trial authors for clarification and any differences of opinion were resolved through discussion.
The results of this assessment of the risk of bias can be seen in Figure 1.
1.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Measures of treatment effect
All the pre‐specified outcomes were dichotomous data and are presented as risk ratios with 95% CIs.
For the occurrence of cholera and diarrhoea cases, the overall risk ratio (RR) has been converted to vaccine efficacy (or effectiveness where intention‐to‐treat analysis was used) using the formula: % Vaccine Efficacy = (1‐RR) x 100%.
Unit of analysis issues
Trials including more than two comparison groups have been split and analysed as individual pair‐wise comparisons. When conducting meta‐analysis we have ensured that participants and cases in the placebo group were not counted more than once, by dividing the placebo cases and participants evenly between the intervention groups.
Cluster‐randomized trials have only been included in the meta‐analysis after appropriate adjustment for the effect of clustering. The individualized data has been reduced to the 'effective sample size' by dividing the number of events and the number of participants by the 'design effect'. The design effect was calculated as: 1 + (M‐1)ICC; where M = average cluster size and ICC = intracluster correlation coefficient. We used estimates of the ICC as presented in the relevant papers.
Dealing with missing data
If data from the trial reports were insufficient, unclear, or missing, we attempted to contact the trial authors for additional information. If we judged the missing data to render the result uninterpretable we have excluded the data from the meta‐analysis and clearly stated the reason.
The primary analysis is a complete case analysis where the number of evaluable participants at each time point is used as the denominator.
Assessment of heterogeneity
We assessed for heterogeneity between the trials by examining the forest plot to check for overlapping CIs, by using the Chi² test for heterogeneity using a 10% level of significance, and the I² statistic using a value of 50% to represent moderate levels of heterogeneity. A rough guide to interpretation of the I² statistic is given in the Cochrane Handbook section 9.5.2.
Assessment of reporting biases
There were insufficient trials for us to assess the likelihood of small study effects, such as publication bias, by examining the funnel plot for asymmetry.
Data synthesis
We analysed the data using Review Manager 5. Interventions are compared directly using pair‐wise comparisons, and meta‐analysis has been performed, where appropriate, if there was more than one trial for a particular comparison. For outcomes that are measured at different time points we have stratified the analysis by the time point.
We have combined studies using the Mantel‐Haenszel method with the fixed‐effect model. When we have combined the results of trials using different vaccines, or where moderate heterogeneity was detected, we have used the random‐effects model. For comparisons which included both individually and cluster‐randomized studies; we adjusted the data from the cluster‐randomized studies to the 'effective sample size' taking into account the design effect, and then combined the data using the Mantel‐Haenzel method.
If the reported results of cluster‐randomized studies had not been adjusted to take into account the effects of clustering, and we were unable to make these adjustments ourselves, the results are simply reported in tables, and not included in the meta‐analysis.
Subgroup analysis and investigation of heterogeneity
We conducted the following subgroup analyses where data were available: age (adult and child, or age under 5 years and over 5 years), time period of follow up, blood group (group O versus other blood groups), type of vaccine, vaccine regimen used or doses received, and whether the challenge was artificial or natural.
Sensitivity analysis
We intended to conduct a sensitivity analysis to evaluate the possible effects of incomplete outcome data by carrying out a best‐worst case analysis, such that patients who were lost to follow up were assumed to have the event of interest in one sensitivity analysis and then were assumed to not have the event in a second sensitivity analysis. The data to reliably do this were however not available, so the presented data are a complete‐case analysis and represent an assessment of vaccine efficacy, rather than effectiveness.
Results
Description of studies
Results of the search
The search identified 204 references, of which 46 were excluded on abstract alone. Full text copies were obtained of 158 and these were formally assessed using the pre‐stated inclusion criteria. Overall, 110 were excluded for the reasons displayed in the Characteristics of excluded studies table.
Included studies
Forty‐eight individual papers have contributed to this review describing 39 separate trials. Fourteen of these describe efficacy data from seven large scale field trials, four describe small artificial challenge efficacy studies, and 29 contribute only safety data. For further details see the Characteristics of included studies table.
Killed whole cell vaccines
Six trials have evaluated the clinical efficacy of five variations of a killed whole cell vaccine (Clemens 1988 Bangladesh; Sanchez 1994 Peru; Sanchez 1995 Peru; Taylor 2000 Peru; Trach 1997 Viet Nam; Sur 2009 India).
The composition of these vaccines, the dosing schedule, and the population groups included in these trials are shown in Table 3.
2. The vaccine composition, dosing and participants in field trials of killed whole cell vaccines.
|
Vaccine code (Trade name) |
Item | Vaccine composition, dosing and population used in the field trials |
|
WC (not currently available) |
Composition | Three strains of V. cholerae O1:
|
| Dosing schedule | Three doses, at 6 week intervals | |
| Field trial | Clemens 1988 Bangladesh: 41580 participants in primary analysis | |
| Population | Children aged 2‐15 years and women over the age of 15 | |
|
WC‐BS (not currently available) |
Composition | As for WC with additional:
|
| Dosing schedule | Three doses, at 6 week intervals | |
| Field trial | Clemens 1988 Bangladesh: 41,542 participants in primary analysis | |
| Population | Children aged 2‐15 years and women over the age of 15 | |
|
WC/rBS (Dukoral®) |
Composition | As for WC‐BS except 1 mg purified cholera B subunit is replaced with:
|
| Dosing schedule | Two doses, 2 weeks apart Taylor 2000 Peru also gave a booster dose at 10 months | |
| Field trials | Sanchez 1994 Peru: (1426 participants in primary analysis), Sanchez 1995 Peru: (307 participants), Taylor 2000 Peru: (17,799 participants) | |
| Population | Sanchez 1994 Peru and Sanchez 1995 Peru: Military recruits Taylor 2000 Peru: Adults and children aged 2 to 65 years | |
|
vWC (ORCVAX®) |
Composition | Four strains of V. cholerae O1.
As for WC except the2.5 x 1010 formalin‐killedV. cholerae classical Ogawa whole cells (strain Cairo 50) are replaced with:
|
| Dosing schedule | Two doses, 2 weeks apart | |
| Field trial | Trach 1997 Viet Nam: 114879 participants in primary analysis | |
| Population | Adults and children aged > 1 year | |
|
BivWC (Shanchol®) |
Composition | Three strains of V. cholerae O1 plus one strain of V. cholerae O139:
|
| Dosing schedule | Two doses, 2 weeks apart | |
| Field trial | Sur 2009 India: 66,900 participants in primary analysis | |
| Population | Adults and children aged > 1 year, living in Kolkata, India |
WC = killed whole cell, BS = cholera toxin B subunit, rBS = recombinant cholera toxin B subunit, LPS = Lipopolysaccharide, ELISA = Enzyme‐linked immunosorbent assay
The individual vaccines represent step‐wise developments from the original vaccines used in Clemens 1988 Bangladesh to the three vaccines commercially available today.
Two of the field trials used a cluster‐randomized design (Trach 1997 Viet Nam; Sur 2009 India). In order to include these trials in a meta analysis, we have converted the data presented in the original papers to risk ratios, and adjusted for the effect of clustering using the ICC presented in Sur 2009 India. The remaining five trials were individually randomized.
Three of these efficacy trials and 11 additional trials contribute to the safety data for these five vaccines.
Live attenuated vaccines
Only one live attenuated vaccine (CVD 103‐HgR) has reached the stage of large scale field evaluation (Richie 2000 Indonesia). The protective efficacy of two other candidate vaccines: Peru 15 and VC638, has been evaluated in small randomized artificial challenge studies (Cohen 2002; García 2005). The composition, dosing schedule and population groups included in these trials are shown in Table 4.
3. The vaccine composition, dosing and participants in efficacy trials of live attenuated vaccines.
|
Vaccine code (Trade name) |
Item | Vaccine composition, dosing and population used in the field trials |
|
CVD103‐HGR (not currently available) |
Composition |
Richie 2000 Indonesia: 5 x 109 lyophilized organisms of a genetically modified V. cholerae O1 Classical Inaba (569B) Tacket 1999: 2 to 8 x 108 CFU of lyophilized organisms of a genetically modified strain of V. cholerae O1 plus buffer |
| Dosing schedule | A single dose | |
|
Field trial Artificial challenge study |
Richie 2000 Indonesia: 67,508 participants Tacket 1999: 51 participants |
|
| Population |
Richie 2000 Indonesia: Age 2 to 41 years in Jakarta, Indonesia Tacket 1999: Adults aged 18 to 40 in USA |
|
|
Peru15 (not currently available) |
Composition | 5 x 108 CFU of a live attenuated strain of V. cholerae O1 El Tor Inaba plus 200ml CeraVacx buffer (Cera Products, Columbia) |
| Dosing schedule | A single dose | |
| Artificial challenge study | Cohen 2002: 36 participants | |
| Population | Volunteers aged 18 to 40 in USA | |
|
VC638 (not currently available) |
Composition | 1 x 109 CFU of a live attenuated strain of V. cholerae O1 El Tor Ogawa plus buffer |
| Dosing schedule | A single dose | |
| Artificial challenge study | García 2005: 21 participants | |
| Population | Volunteer males aged 8 to 40 in Cuba |
CFU = Colony forming units
An additional 18 trials contributed safety data only to the evaluation of these vaccines.
Excluded studies
Eleven of the excluded trials may be eligible for inclusion in later updates of the review, as the only reason for their exclusion was that no trials assessing the clinical efficacy of these vaccines have been published; we decided to exclude these early‐stage trials because data on safety and tolerability alone is of limited use in practice.
Risk of bias in included studies
Allocation
Efficacy studies
One cluster, quasi‐randomized study (Trach 1997 Viet Nam) used alternate open allocation and three out of the six other efficacy trials did not adequately describe the process of sequence generation or allocation concealment (Richie 2000 Indonesia; Sanchez 1994 Peru; Sanchez 1995 Peru). However, as the effect of unconcealed allocation in vaccine trials is unlikely to be substantial given that all participants are well prior to enrolment, these trials were judged to be at low risk of bias for these criteria.
Safety (and immunogenicity) only studies
Eleven out of the 29 trials only presenting safety data did not adequately describe the process of allocation concealment for us to make a judgement about the risk of bias.
Blinding
Efficacy outcomes
Six of the seven efficacy trials adequately blinded participants and staff involved with the trial (Clemens 1988 Bangladesh; Richie 2000 Indonesia; Taylor 2000 Peru; Sanchez 1994 Peru, Sanchez 1995 Peru; Sur 2009 India). One trial was unblinded (Trach 1997 Viet Nam).
Safety outcomes
Most studies used placebos which were of identical appearance to the vaccine, and could be considered at low risk of bias for safety outcomes. In nine studies the use of a placebo was not adequately described to make a judgement and so were classified as 'unclear'.
Incomplete outcome data
Efficacy studies
Three trials adequately addressed incomplete data for cases of cholera (Taylor 2000 Peru; Sanchez 1994 Peru; Sur 2009 India). In one trial it was unclear whether this had been done, but due to the large sample size and active surveillance system used, this was unlikely to have introduced significant bias (Clemens 1988 Bangladesh). In two trials it was unclear how many participants were lost to follow‐up (Richie 2000 Indonesia; Trach 1997 Viet Nam).
Safety (and immunogenicity) only studies
Safety only studies were generally of only short duration with minimal losses to follow‐up and therefore considered at low risk of bias.
Selective reporting
We found no evidence of selective reporting bias.
Other potential sources of bias
One trial had evidence of possible other bias (Concha 1995). In this trial, 620 individuals who originally consented to participate dropped out because of a political campaign against it.
Effects of interventions
See: Table 1
Killed whole cell vaccines
Clinical efficacy
Six trials have evaluated the clinical efficacy of five variations of a killed whole cell vaccine (Clemens 1988 Bangladesh; Sanchez 1994 Peru; Sanchez 1995 Peru; Taylor 2000 Peru; Trach 1997 Viet Nam; Sur 2009 India).
These vaccines are similar but not identical in composition (see Table 3). Despite the variation in dosing schedules, the protective efficacy against confirmed cholera of all five vaccines is similar in both the first and second years following vaccination. It should however be noted that protective efficacy with the two‐dose schedule of the WC‐rBS vaccine (Dukoral) was not demonstrated in Peru until the second year following a booster dose at 10 months (Taylor 2000 Peru).
The per protocol estimates of protective efficacy as reported in the original papers are shown in Table 4. For comparative purposes we have converted all measures of efficacy to cluster adjusted RRs (Sur 2009 India used rate ratio) and presented these in a forest plot (Year 1 of follow‐up: four trials, 252,887 participants: VE 52%, 95% CI 35% to 65%, I² 49%, Analysis 1.1; Year 2 of follow‐up: three trials, 130,334 participants: VE 61%, 95% CI 50% to 70%, I² 0%, Analysis 1.2).
1.1. Analysis.

Comparison 1: Whole cell vaccines (all types) versus placebo ‐ Primary efficacy outcomes, Outcome 1: Cases of cholera ‐ 1st year of follow up (with meta analysis)
1.2. Analysis.

Comparison 1: Whole cell vaccines (all types) versus placebo ‐ Primary efficacy outcomes, Outcome 2: Cases of cholera ‐ 2nd year of follow up (with meta analysis)
Evidence of protection for time periods of greater than two years after vaccination is only available for the WC and WC‐BS vaccine formulations which are not currently available.
The protective efficacy in children aged less than 5 years was lower than that seen in adults when the data was amalgamated over the first two years of follow‐up (four trials, participants; Age < 5 years: VE 38%, 95% CI 20% to 53%, Age > 5 years: VE 66%, 95% CI 57% to 73%, Analysis 1.5; Figure 2). This data was calculated by summing the number cases of cholera in the first two years, and using the number of participants completing 2‐years of follow‐up as the denominator. A sensitivity analysis using the number of participants completing 1‐year follow‐up as the denominator did not change the result (Analysis 1.6).
1.5. Analysis.

Comparison 1: Whole cell vaccines (all types) versus placebo ‐ Primary efficacy outcomes, Outcome 5: Cases of cholera by age group ‐ First two years of follow‐up
2.

Forest plot of comparison: 1 Whole cell vaccines (all types) versus placebo ‐ Primary efficacy outcomes, outcome: 1.5 Cases of cholera by age group ‐ First two years of follow‐up.
1.6. Analysis.

Comparison 1: Whole cell vaccines (all types) versus placebo ‐ Primary efficacy outcomes, Outcome 6: Cases of cholera by age group ‐ First two years of follow‐up (sensitivity analysis)
Whole cell vaccine (WC: not currently available); three doses given 6 weeks apart
One trial conducted in Bangladesh in 1985 (Clemens 1988 Bangladesh) compared the WC vaccine versus placebo in children aged 2 to 15 years and females aged > 15 years.
Protective efficacy against cholera episodes was established within the first 4‐months after vaccination (one trial, 41,580 participants: VE 52%, 95% CI ‐5% to 78%, Analysis 2.1) and maintained until the third year (Year 1: VE 53%, 95% CI 34% to 66%; Year 2: VE 57%, 95% CI 38% to 70%; Year 3: VE 42%, 95% CI 11% to 62%; Year 4: VE ‐28%, 95% CI ‐137% to 31%, Analysis 2.1). Protective efficacy was lost in the fourth year of follow‐up.
2.1. Analysis.

Comparison 2: Whole cell vaccine (WC) versus placebo ‐ Subgroup analysis, Outcome 1: Cases of cholera by time of follow‐up (3‐dose recipients)
Vaccine efficacy appears to be lower in children age < 5 years (one trial, 41,580 participants; Year 1: Age 2 to 5 years VE 31%, 95% CI ‐9% to 57%; Age > 5 years VE 67%, 95% CI 44% to 80%, Analysis 2.2; Year 2: Age 2 to 5 years VE 24%, 95% CI ‐29% to 55%; Age > 5 years VE 73%, 95% CI 55% to 84%, Analysis 2.3). The difference between vaccine and placebo was not shown to be statistically significant at any time point in this group, although the trend was towards some protection.
2.2. Analysis.

Comparison 2: Whole cell vaccine (WC) versus placebo ‐ Subgroup analysis, Outcome 2: Cases of cholera by age‐group ‐ 1st year of follow‐up (3‐dose recipients)
2.3. Analysis.

Comparison 2: Whole cell vaccine (WC) versus placebo ‐ Subgroup analysis, Outcome 3: Cases of cholera by age‐group ‐ 2nd year of follow‐up (3‐dose recipients)
There was also a statistically significant difference between vaccine and placebo in cases of severe watery diarrhoea of any cause (Year 1: VE 32%, 95% CI 7% to 51%, Analysis 2.5), any watery diarrhoea (Year 1: VE 33%, 95% CI 18% to 46%, Analysis 2.5), and diarrhoea of any cause (Year 1: VE 22%, 95% CI 8% to 35%, Analysis 2.5). There is a trend towards a protective effect against all‐cause death (VE 23%, 95% CI ‐1% to 42%), and death from non‐dysenteric diarrhoea (VE 53%, 95% CI ‐16% to 81%), but these did not reach statistical significance (Analysis 2.6).
2.5. Analysis.

Comparison 2: Whole cell vaccine (WC) versus placebo ‐ Subgroup analysis, Outcome 5: Cases of all cause diarrhoea ‐ 1st year of follow‐up (3‐dose recipients)
2.6. Analysis.

Comparison 2: Whole cell vaccine (WC) versus placebo ‐ Subgroup analysis, Outcome 6: Deaths ‐ 1st year of follow‐up (3‐dose recipients)
Whole cell plus B subunit vaccine (WC‐BS: not currently available); three doses given 6 weeks apart
The same study (Clemens 1988 Bangladesh) also evaluated the WC‐BS vaccine.
Protective efficacy against cholera episodes was similarly demonstrated at 4‐months after vaccination (one trial, 41,542 participants: VE 79%, 95% CI 38% to 93%, Analysis 3.1) but evidence of clinical efficacy was lost in the third year after vaccination (Year 1: VE 62%, 95% CI 46% to 74%; Year 2: VE 58%, 95% CI 40% to 71%; Year 3: 18%, 95% CI ‐21% to 44%; Year 4: 16%, 95% CI ‐66% to 58%, Analysis 3.1).
3.1. Analysis.

Comparison 3: Whole cell vaccine plus B subunit (WC‐BS) versus placebo ‐ Subgroup analysis, Outcome 1: Cases of cholera by time of follow‐up (3‐dose recipients)
Vaccine efficacy again appears to be lower in children age < 5 years (one trial, 41,542 participants; Year 1: Age 2 to 5 years VE 38%, 95% CI ‐1% to 62%; Age > 5 years VE 78%, 95% CI 61% to 87%, Analysis 3.2; Year 2: Age 2 to 5 years VE 47%, 95% CI 3% to 71%; Age > 5 years VE 63%, 95% CI 41% to 76%, Analysis 3.3).
3.2. Analysis.

Comparison 3: Whole cell vaccine plus B subunit (WC‐BS) versus placebo ‐ Subgroup analysis, Outcome 2: Cases of cholera by age‐group ‐ 1st year of follow‐up (3‐dose recipients)
3.3. Analysis.

Comparison 3: Whole cell vaccine plus B subunit (WC‐BS) versus placebo ‐ Subgroup analysis, Outcome 3: Cases of cholera by age‐group ‐ 2nd year of follow‐up (3‐dose recipients)
There was also a statistically significant difference between vaccine and placebo in cases of severe watery diarrhoea of any cause (Year 1: VE 51%, 95% CI 31% to 66%, Analysis 3.5), any watery diarrhoea (Year 1: VE 38%, 95% CI 23% to 50%, Analysis 3.5), and diarrhoea of any cause (Year 1: VE 26%, 95% CI 12% to 38%, Analysis 3.5). All‐cause death and death from non‐dysenteric diarrhoea were also significantly lower in the group given the vaccine (Year 1: All‐cause death: VE 26%, 95% CI 3% to 44%; Deaths from non‐dysenteric diarrhoea: VE 80%, 95% CI 31% to 94%, Analysis 3.6).
3.5. Analysis.

Comparison 3: Whole cell vaccine plus B subunit (WC‐BS) versus placebo ‐ Subgroup analysis, Outcome 5: Cases of all cause diarrhoea ‐ 1st year of follow‐up (3‐dose recipients)
3.6. Analysis.

Comparison 3: Whole cell vaccine plus B subunit (WC‐BS) versus placebo ‐ Subgroup analysis, Outcome 6: Deaths ‐ 1st year of follow‐up (3‐dose recipients)
No statistically significant difference between WC‐BS and WC was demonstrated at any time point, although there was a trend towards increased protection with WC‐BS during the first 8‐months after vaccination (Analysis 4.1).
4.1. Analysis.

Comparison 4: Whole cell vaccine (WC) versus Whole cell vaccine plus B subunit (WC‐BS) ‐ Subgroup analysis, Outcome 1: Cases of confirmed cholera by time of follow‐up (3‐dose recipients)
Whole cell plus recombinant vaccine (WC‐rBS: available as Dukoral®, SBL); two doses given 2 weeks apart +/‐ a booster dose at 10 months
One large trial in the general population (Taylor 2000 Peru), and two smaller trials in military recruits (Sanchez 1994 Peru; Sanchez 1995 Peru) have evaluated the efficacy of the WC‐rBS vaccine ;
Taylor 2000 Peru did not demonstrate any significant difference between vaccine or placebo during the first year (one trial, 17,799 participants: VE ‐4%, 95% CI ‐105% to 48%, Analysis 5.1). However, following a booster dose at 10 months the vaccine was superior to placebo in the second year of follow‐up (1 trial, 14,999 participants: VE 60%, 95% CI 25% to 79%, Analysis 5.2).
5.1. Analysis.

Comparison 5: Whole cell plus recombinant B subunit vaccine (WC‐rBS) versus placebo ‐ Subgroup analysis, Outcome 1: Cases of cholera by age group ‐ 1st year of follow‐up (2 doses)
5.2. Analysis.

Comparison 5: Whole cell plus recombinant B subunit vaccine (WC‐rBS) versus placebo ‐ Subgroup analysis, Outcome 2: Cases of cholera by age group ‐ 2nd year of follow‐up (2 doses plus booster)
In the second year of follow‐up the estimate of vaccine efficacy was highest in those older than 15 years, although there were very few cholera episodes in the youngest age group (one trial, 14,999 participants, Year 2: Age 2‐5 years VE 52%, 95% CI ‐162% to 91%; Age 5 to 15 years VE 47%, 95% CI ‐44% to 80%; Age 16 to 65 years VE 71%, 95% CI 22% to 89%; Analysis 5.2)
Both the small trials in military recruits experienced an outbreak of cholera during or shortly after the vaccination schedule. In Sanchez 1994 Peru the outbreak occurred 2 to 4 weeks after vaccination. A vaccine efficacy of 86% (95% CI 37% to 97%) was demonstrated in those who received the full two dose schedule, but a single dose did not appear protective (one trial, 1563 participants, Analysis 5.3). In Sanchez 1995 Peru the outbreak occurred between the first and second vaccine doses, and vaccine efficacy after one dose approached statistical significance (VE 44%, 95% CI ‐4% to 70%, Analysis 5.3).
5.3. Analysis.

Comparison 5: Whole cell plus recombinant B subunit vaccine (WC‐rBS) versus placebo ‐ Subgroup analysis, Outcome 3: Cases of cholera in military recruits, 4 to 18 weeks follow‐up
Variant whole cell vaccine (vWC: available as ORCVAX®, Vabiotech); two doses given 2 weeks apart
One cluster quasi‐randomized trial evaluated the efficacy of the vWC vaccine with 1‐year follow‐up (Trach 1997 Viet Nam).
Two doses of vaccine were superior to placebo at preventing cholera episodes requiring in‐patient care in all age groups (one trial, 119,033 participants, Age 1 to 5 years VE 68%, 95% CI 14% to 88%, Age > 5 years VE 66%, 95% CI 42% to 80%, authors own figures).
The vaccine was protective against severe and non‐severe cholera episodes (one trial, 119,033 participants, Severe episodes VE 65%, 95% CI 34% to 81%, Non‐severe episodes VE 56%, 95% CI 26% to 74%, authors own figures).
Bivalent whole cell vaccine (BivWC: available as Shanchol®, Shantha Biotechnics); two doses given 2 weeks apart
One cluster‐randomized trial evaluated the efficacy of the BivWC vaccine (Sur 2009 India). Data are presented for two years of follow‐up although the trial is ongoing.
The protective efficacy of the BivWC vaccine was statistically significant during the second but not the first year after vaccination (one trial, 66,900 participants in 3478 clusters: Year 1 VE 45%, 95% CI lower bound ‐5%, Year 2 VE 77%, 95% CI lower bound 55%, authors own figures).
Over two years follow‐up the vaccine was protective in all age groups but lowest in the youngest age group (one trial, 66,900 participants: Age 1 to 4.9 years VE 49%, 95% CI lower bound 6%; Age 5 to 14.9 years VE 87%, 95% CI lower bound 54%; Age > 15 years VE 63%, 95% CI lower bound 23%; authors own figures).
Safety
Whole cell vaccine (WC: not currently available); three doses given 6 weeks apart
Safety data were available from 613 participants. No statistically significant differences were shown between vaccine and placebo after the first or second doses (one trial, 613 participants, Analysis 6.1; Analysis 3.1)
6.1. Analysis.

Comparison 6: Whole cell vaccines (all types) versus placebo ‐ Safety outcomes (first dose), Outcome 1: Adverse events ‐ Whole cell (WC) versus placebo
Whole cell plus B subunit vaccine (WC‐BS: not currently available); three doses given 6 weeks apart
Safety data were available from 631 participants. No statistically significant differences were shown between vaccine and placebo after the first or second doses (one trial, 631 participants, Analysis 6.2; Analysis 3.2)
6.2. Analysis.

Comparison 6: Whole cell vaccines (all types) versus placebo ‐ Safety outcomes (first dose), Outcome 2: Adverse events ‐ Whole cell plus B subunit (WC‐BS) versus placebo
Whole cell plus recombinant vaccine (WC‐rBS: available as Dukoral®, SBL); two doses given 2 weeks apart +/‐ a booster dose at 10 months
Safety data is available on 12,121 participants who received the WC‐rBS vaccine in eight placebo‐controlled randomized trials (Begue 1995; Concha 1995; Hallander 2002; Sanchez 1993a; Sanchez 1995 Peru; Taylor 1999a; Taylor 2000 Peru; Trach 2002). The placebo used in seven of these studies was an oral dose of inactivated E. coli (K12 strain).
The largest study (Taylor 2000 Peru) collected reports of adverse events at the time of the second dose. It found very low levels of symptoms (0.2%), and only the figures for diarrhoea were presented (one study, 10,992 participants, Analysis 6.3). The remaining studies are small. The only statistically significant result was from one study (Sanchez 1995 Peru) which found a higher rate of stomach gurgling after the second dose of vaccine (seven trials, 23,870 participants, Analysis 6.3; Analysis 7.1). The symptoms most commonly reported after taking the vaccine were: stomach gurgling (14%), abdominal pain (9%), headache (5%), and these were generally described as mild.
6.3. Analysis.

Comparison 6: Whole cell vaccines (all types) versus placebo ‐ Safety outcomes (first dose), Outcome 3: Adverse events ‐ Whole cell plus recombinant B subunit (WC‐rBS) versus placebo
7.1. Analysis.

Comparison 7: Whole cell vaccines (all types) versus placebo ‐ Safety outcomes (second dose), Outcome 1: Adverse events ‐ Whole cell plus recombinant B subunit (WC‐rBS) versus placebo
One additional study translated from Chinese (Chen 1996) evaluated the safety of a locally formulated WC‐rBS in 369 schoolchildren and factory workers and reports no significant differences between vaccine and placebo.
Variant whole cell vaccine (vWC: available as ORCVAX®, Vabiotech); two doses given 2 weeks apart
There is no safety data available for this vaccine.
Bivalent whole cell vaccine (BivWC: available as Shanchol®, Shantha Biotechnics); two doses given 2 weeks apart
Safety data is available from 32,190 participants who received the bivalent whole cell vaccine in four randomized controlled trials (Mahalanabis 2008; Anh 2007; Kanungo 2009; Sur 2009 India). The placebo used in all four trials was an oral dose of inactivated E. coli (K12 strain).
The largest study (Sur 2009 India) only collected data passively, encouraging participants to present for medical care, and found very low levels of symptoms (<0.2%). It did however record 51 serious adverse events but with no differences between the vaccine and placebo groups. The remaining three studies are small. No clinically important differences between the vaccine and placebo have been shown (four trials, 67,414 participants, Analysis 6.4; Analysis 7.2). Excluding Sur 2009 India, the symptoms most commonly reported were: abdominal pain (7%), headache (7%), fever (4%), and nausea (3%). These were generally described as mild.
6.4. Analysis.

Comparison 6: Whole cell vaccines (all types) versus placebo ‐ Safety outcomes (first dose), Outcome 4: Adverse events ‐ Bivalent whole cell (BivWC) versus placebo
7.2. Analysis.

Comparison 7: Whole cell vaccines (all types) versus placebo ‐ Safety outcomes (second dose), Outcome 2: Adverse events ‐ Bivalent whole cell (BivWC) versus placebo
Live attenuated vaccines
Efficacy
Only CVD 103‐HgR has been evaluated for clinical efficacy against naturally occurring V. cholera. The other live attenuated vaccines listed here remain in development.
CVD 103‐HgR (not currently available): one dose
CVD 103‐HgR has not been shown to give significant clinical protection from natural cholera infection in any age group (one trial, 67,508 participants, Analysis 8.1; Analysis 8.2), however only one efficacy study has evaluated this vaccine. This study relied on passive surveillance and the number of cholera events was very low (Richie 2000 Indonesia). There was also no difference in all‐cause death, or deaths related to diarrhoea (one study, 67,508 participants, Analysis 8.3; Analysis 8.4).
8.1. Analysis.
Comparison 8: Live attenuated vaccines (all types) versus placebo ‐ Efficacy outcomes, Outcome 1: Cases of cholera following natural infection ‐ CVD 103HgR versus placebo
8.2. Analysis.

Comparison 8: Live attenuated vaccines (all types) versus placebo ‐ Efficacy outcomes, Outcome 2: Severe cholera following natural infection ‐ CVD 103HgR versus placebo
8.3. Analysis.

Comparison 8: Live attenuated vaccines (all types) versus placebo ‐ Efficacy outcomes, Outcome 3: Death from any cause (except motor accidents)
8.4. Analysis.

Comparison 8: Live attenuated vaccines (all types) versus placebo ‐ Efficacy outcomes, Outcome 4: Death from diarrhoea (any organism)
A small artificial challenge study in adult volunteers in the USA (Tacket 1999) did however, demonstrate a protective effect against moderate to severe diarrhoea (one trial, 51 participants: VE 91%, 95% CI 33% to 99%, Analysis 8.5) and any diarrhoea (VE 80%, 95% CI 56% to 91%, Analysis 8.6).
8.5. Analysis.

Comparison 8: Live attenuated vaccines (all types) versus placebo ‐ Efficacy outcomes, Outcome 5: Cases of moderate to severe diarrhoea ‐ following artificial challenge
8.6. Analysis.

Comparison 8: Live attenuated vaccines (all types) versus placebo ‐ Efficacy outcomes, Outcome 6: Cases of any diarrhoea ‐following artificial challenge
Peru 15 (in development): one dose
One artificial challenge study conducted in adult volunteers in the USA (Cohen 2002) showed a protective effect against moderate to severe diarrhoea (one trial, 36 participants: VE 95%, 95% CI 21% to 100%, Analysis 8.5) and any diarrhoea (VE 97%, 95% CI 69% to 100%, Analysis 8.6). Phase III clinical trials are necessary before conclusions on the clinical efficacy of this vaccine can be made.
VC638 (in development): one dose
One small artificial challenge study conducted in adult volunteers in Cuba (García 2005) demonstrated a protective effect against any diarrhoea (one trial, 21 participants: VE 99%, 95% CI 68 % to 100%, Analysis 8.6), but not severe diarrhoea (Analysis 8.5). Phase III clinical trials are necessary before conclusions on the clinical efficacy of this vaccine can be made.
Safety
CVD 103‐HgR (not currently available): one dose
A total of 1970 participants have received CVD 103‐HgR in fifteen included randomized controlled trials (Cryz 1990; Gotuzzo 1993; Kotloff 1992; Lagos 1993; Lagos 1995; Lagos 1999; Migasena 1989a; Perry 1998; Richie 2000 Indonesia; Simanjuntak 1993; Su‐Arehawaratana 1992a; Su‐Arehawaratana 1992b; Suharyono 1992a; Suharyono 1992b; Tacket 1999). The placebo used in 14 of these studies was an oral dose of inactivated E. coli (K12 strain).
No symptom was shown to be statistically more common in those given the vaccine (15 trials, 1970 participants, Analysis 9.1). The commonest reported symptoms following vaccination were: malaise (20% but only recorded in two trials), anorexia (12% but only recorded in three trials), headache (13%), abdominal pain (10%), fever (7%), diarrhoea (5%), vomiting (5%). In general these symptoms are reported to be mild. Su‐Arehawaratana 1992a reports one participant developing diarrhoea after vaccination that required them to seek hospital care.
9.1. Analysis.

Comparison 9: Live attenuated vaccines (all types) versus placebo ‐ Safety outcomes, Outcome 1: Adverse events ‐ CVD 103‐HgR versus placebo
Peru 15 (in development): one dose
A total of 252 participants have received Peru 15 in four randomized controlled trials (Cohen 2002; Qadri 2005; Qadri 2007; Sack 1997). The placebo used in these trials was the buffer given alone.
Headache was the only symptom to be statistically more common with the vaccine (four trials, 419 participants: Headache RR 4.14, 95% CI 1.27 to 13.48, Analysis 9.2). The commonest reported symptoms during the first few days after vaccination were: nausea (18%), loss of energy (15%), loss of appetite (10%), and headache (10%). Other adverse events were uncommon, and all adverse events were described as mild.
9.2. Analysis.

Comparison 9: Live attenuated vaccines (all types) versus placebo ‐ Safety outcomes, Outcome 2: Adverse events ‐ Peru 15 versus placebo
VC638 (in development): one dose
A total of 90 participants have received VC638 in three randomized studies (García 2005; Benítez 1999; Valera 2009). The placebo used in these trials was the buffer given alone.
No symptom was shown to be statistically more common in those given vaccine (three trials, 137 participants, Analysis 9.3). The commonest reported symptoms during the first few days were: stomach gurgling (40%), nausea (33%), abdominal pain (32%), headache (19%), and diarrhoea (13%). Other adverse events were uncommon, and all but one adverse event (a moderate headache) were described as mild.
9.3. Analysis.

Comparison 9: Live attenuated vaccines (all types) versus placebo ‐ Safety outcomes, Outcome 3: Adverse events ‐ VC638 versus placebo
Discussion
Summary of main results
Killed whole cell vaccines
Five variations of a killed whole cell cholera vaccine have been evaluated in large scale clinical trials. The overall vaccine efficacy during the first year was 52% (95% CI 35% to 65%), and during the second year was 61% (95% CI 50% to 70%).
The protective efficacy over 2‐years follow‐up was lower in children aged less than 5 years (VE 38%, 95% CI 20% to 53%), than that seen in older age‐groups (VE 66%, 95% CI 57% to 73%).
Any observed differences in vaccine efficacy between these vaccines is well within the bounds of random error.
Clinical protection against cholera with the older vaccines (WC and WC‐BS) was demonstrated within 4‐months of the primary schedule and persisted as long as the third year after vaccination. This cannot be reliably extrapolated to the currently available vaccines given the changes in both the immunisation schedule and the composition of the vaccines.
Of the currently available vaccines:
A two dose regimen of WC‐rBS (Dukoral®) was not shown to be clinically effective in adults in Peru until after a third booster dose was given at 10 months. One smaller trial in military recruits in Peru, did demonstrate a high protective efficacy in a small epidemic occurring within 4 weeks of the two dose schedule but extrapolation of this result beyond short term follow‐up may be unreliable. Clinical efficacy in children aged less than 5 years has not been demonstrated.
A two dose regimen of BivWC (Shanchol®) is likely to be effective during the first and second years after vaccination though this only reached statistical significance during the second year, and follow‐up in this trial is ongoing. There is a trend towards protection in all age groups but this was not statistically significant in the under 5 year olds.
The Vietnam variation of BivWC (mORCVAX®) has not been formally evaluated in published clinical trials. It contains the same elements as Shanchol but has a different manufacturing process.
Live attenuated vaccines
The live attenuated vaccines remain in development. The only vaccine to reach Phase III clinical trials and licensure in some countries, CVD 103‐HgR, has not been shown to provide a protective effect against clinical cholera episodes; however, it has only been evaluated in one large efficacy trial in which there were few cases in either arm.
Overall completeness and applicability of evidence
The currently available vaccines represent stepwise modifications to the original vaccines developed and studied in Bangladesh in the 1980s. Although changes have occurred in both the composition and the recommended vaccination schedule, they remain similar enough to sensibly combine in a meta‐analysis, and this is confirmed by their remarkably similar efficacies. The efficacy data from these older studies and vaccines therefore remains relevant to the assessment of the WC‐rBS (Dukoral®) and BivWC (Shanchol®) vaccines available today.
The current recommended schedule for WC‐rBS is two doses 2 weeks apart, and three doses 2 weeks apart for children age 2 to 5 years. The two dose schedule (rather than the three doses used in the Bangladesh study) has been adopted based on immunological data, and the observation that two doses of the original WC and WC‐BS vaccines were equally effective to three doses in the Bangladesh study (Clemens 1988 Bangladesh). Unfortunately we have been unable to get access to the data to confirm this finding.
The lack of protective efficacy with a two‐dose schedule seen in the only large scale trial of WC‐rBS (Taylor 2000 Peru) has been discussed in the literature with questions raised about the adequacy and accuracy of the cholera surveillance during the first year of follow‐up (Clemens 2001; Taylor 2001). Reassuringly two doses were protective in the much smaller military trials, but the number of events was low and the period of follow‐up inadequate to make conclusions for the use of the vaccine outside of an acute epidemic situation. Although the two dose schedule of BivWC has been shown to be protective in the first year (though not quite reaching statistical significance), this vaccine is sufficiently different from WC‐rBS to restrict the generalisation of this result.
The primary analysis used in this review is a complete‐case analysis excluding participants who received incomplete vaccine schedules. These findings will therefore tend to overestimate the effectiveness of the vaccine when given outside of trial settings, where vaccine coverage will almost always be considerably less than 100%. This factor should be taken into consideration when planning a cholera vaccination programme.
The best evidence for the use of cholera vaccines in epidemic situations, such as seen in Zimbabwe and Haiti in recent years, comes from the two trials in adult military recruits. Sanchez 1994 Peru demonstrated 86% protective efficacy (95% CI 37% to 97%) in a small epidemic occurring within 4 weeks of the two‐dose schedule of WC‐rBS. The reactive use of cholera vaccines once an epidemic has begun has been further evaluated through case‐control studies (Anh 2011), and modelling exercises (Reyburn 2011), which are outside of the scope of this review (Ryan 2011).
Quality of the evidence
The quality of the evidence was assessed using the GRADE methodology. Overall the quality is moderate to high, meaning that we can have a high degree of confidence in these results, and further research is unlikely to substantially alter the current estimates of protective efficacy. See Summary of findings table 1.
Agreements and disagreements with other studies or reviews
The World Health Organization published a position paper on oral cholera vaccines in 2010 (WHO 2010b). The findings presented here are in broad agreement with this paper.
Authors' conclusions
Implications for practice.
The currently available oral killed whole cell vaccines can prevent 50 to 60% of cholera episodes during the first 2‐years after the primary vaccination schedule. Protective efficacy is unlikely to last more than 3 years and booster doses in line with the manufacturers recommendations will be required.
The impact and cost‐effectiveness of adopting oral cholera vaccines into the routine vaccination schedule of endemic countries will depend on the prevalence of cholera among the community, the frequency of epidemics, and the availability or unavailability of adequate facilities to provide rapid rehydration therapy.
Athough there is currently little high quality evidence for the effect of vaccines in emergency and epidemic situations, It is likely that cholera vaccines would have an important impact on reducing disease in epidemics, especially where access to clean water and sanitation is difficult to achieve.
Implications for research.
The evidence from Peru suggests that countries considering routine vaccination should assess whether the two‐dose primary immunization schedule is adequate in their setting.
What's new
| Date | Event | Description |
|---|---|---|
| 12 January 2024 | Amended | Editorial note added to direct readers to review that supersedes this one. |
History
Protocol first published: Issue 7, 2010 Review first published: Issue 3, 2011
| Date | Event | Description |
|---|---|---|
| 3 August 2011 | Amended | Plain language summary amended. |
Acknowledgements
The editorial base for the Cochrane Infectious Disease Group is funded by the Department for International Development (DFID), UK, for the benefit of developing countries.
Data and analyses
Comparison 1. Whole cell vaccines (all types) versus placebo ‐ Primary efficacy outcomes.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Cases of cholera ‐ 1st year of follow up (with meta analysis) | 4 | 249935 | Risk Ratio (M‐H, Random, 95% CI) | 0.48 [0.35, 0.65] |
| 1.1.1 Whole cell vaccine (WC); 3 doses, 6 weeks apart | 1 | 31162 | Risk Ratio (M‐H, Random, 95% CI) | 0.47 [0.33, 0.69] |
| 1.1.2 Whole cell plus B subunit vaccine (WC‐BS); 3 doses, 6 weeks apart | 1 | 31124 | Risk Ratio (M‐H, Random, 95% CI) | 0.38 [0.25, 0.56] |
| 1.1.3 Whole cell plus recombinant B subunit vaccine (WC‐rBS); 2 doses, 2 weeks apart | 1 | 17799 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.52, 2.05] |
| 1.1.4 Variant whole cell vaccine (vWC); 2 doses, 2 weeks apart | 1 | 111928 | Risk Ratio (M‐H, Random, 95% CI) | 0.36 [0.23, 0.56] |
| 1.1.5 Bivalent whole cell vaccine (BivWC); 2 doses, 2 weeks apart | 1 | 57922 | Risk Ratio (M‐H, Random, 95% CI) | 0.55 [0.26, 1.17] |
| 1.2 Cases of cholera ‐ 2nd year of follow up (with meta analysis) | 3 | 130334 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.30, 0.50] |
| 1.2.1 Whole cell vaccine (WC); 3 doses, 6 weeks apart | 1 | 30011 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.28, 0.65] |
| 1.2.2 Whole cell plus B subunit vaccine (WC‐BS); 3 doses, 6 weeks apart | 1 | 30008 | Risk Ratio (M‐H, Random, 95% CI) | 0.42 [0.28, 0.63] |
| 1.2.3 Whole cell plus recombinant B subunit vaccine (WC‐rBS); 2 doses, 2 weeks apart plus booster at 10 months | 1 | 14997 | Risk Ratio (M‐H, Random, 95% CI) | 0.40 [0.21, 0.75] |
| 1.2.4 Variant whole cell vaccine (vWC); 2 doses, 2 weeks apart | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 1.2.5 Bivalent whole cell vaccine (BivWC); 2 doses, 2 weeks apart | 1 | 55318 | Risk Ratio (M‐H, Random, 95% CI) | 0.22 [0.11, 0.48] |
| 1.3 Cases of cholera ‐ 3rd year of follow up (with meta analysis) | 1 | 58174 | Risk Ratio (M‐H, Random, 95% CI) | 0.70 [0.50, 0.98] |
| 1.3.1 Whole cell vaccine (WC); 3 doses, 6 weeks apart | 1 | 29114 | Risk Ratio (M‐H, Random, 95% CI) | 0.59 [0.36, 0.97] |
| 1.3.2 Whole cell plus B subunit vaccine (WC‐BS); 3 doses, 6 weeks apart | 1 | 29060 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.51, 1.29] |
| 1.3.3 Whole cell plus recombinant B subunit vaccine (WC‐rBS); 2 doses, 2 weeks apart plus booster at 10 months | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 1.3.4 Variant whole cell vaccine (vWC); 2 doses, 2 weeks apart | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 1.3.5 Bivalent whole cell vaccine (BivWC); 2 doses, 2 weeks apart | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 1.4 Cases of cholera ‐ 4th year of follow up (with meta analysis) | 1 | 56613 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.60, 1.84] |
| 1.4.1 Whole cell vaccine (WC); 3 doses, 6 weeks apart | 1 | 28357 | Risk Ratio (M‐H, Random, 95% CI) | 1.28 [0.59, 2.76] |
| 1.4.2 Whole cell plus B subunit vaccine (WC‐BS); 3 doses, 6 weeks apart | 1 | 28256 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.37, 1.91] |
| 1.4.3 Whole cell plus recombinant B subunit vaccine (WC‐rBS); 2 doses, 2 weeks apart plus booster at 10 months | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 1.4.4 Variant whole cell vaccine (vWC); 2 doses, 2 weeks apart | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 1.4.5 Bivalent whole cell vaccine (BivWC); 2 doses, 2 weeks apart | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 1.5 Cases of cholera by age group ‐ First two years of follow‐up | 4 | 243071 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.33, 0.56] |
| 1.5.1 Age < 5 years | 4 | 29005 | Risk Ratio (M‐H, Random, 95% CI) | 0.62 [0.47, 0.80] |
| 1.5.2 Age > 5 years | 4 | 214066 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.27, 0.43] |
| 1.6 Cases of cholera by age group ‐ First two years of follow‐up (sensitivity analysis) | 4 | 248140 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.33, 0.56] |
| 1.6.1 Age < 5 years | 4 | 29773 | Risk Ratio (M‐H, Random, 95% CI) | 0.62 [0.47, 0.80] |
| 1.6.2 Age > 5 years | 4 | 218367 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.27, 0.43] |
1.3. Analysis.

Comparison 1: Whole cell vaccines (all types) versus placebo ‐ Primary efficacy outcomes, Outcome 3: Cases of cholera ‐ 3rd year of follow up (with meta analysis)
1.4. Analysis.

Comparison 1: Whole cell vaccines (all types) versus placebo ‐ Primary efficacy outcomes, Outcome 4: Cases of cholera ‐ 4th year of follow up (with meta analysis)
Comparison 2. Whole cell vaccine (WC) versus placebo ‐ Subgroup analysis.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Cases of cholera by time of follow‐up (3‐dose recipients) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1.1 First four months after vaccination | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1.2 First year after vaccination | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1.3 Second year after vaccination | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1.4 Third year after vaccination | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1.5 Fourth year after vaccination | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.2 Cases of cholera by age‐group ‐ 1st year of follow‐up (3‐dose recipients) | 1 | 41580 | Risk Ratio (M‐H, Random, 95% CI) | 0.48 [0.23, 0.98] |
| 2.2.1 Age 2 to 5 years | 1 | 7730 | Risk Ratio (M‐H, Random, 95% CI) | 0.69 [0.43, 1.09] |
| 2.2.2 Age > 5 years | 1 | 33850 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.20, 0.54] |
| 2.3 Cases of cholera by age‐group ‐ 2nd year of follow‐up (3‐dose recipients) | 1 | 40017 | Risk Ratio (M‐H, Random, 95% CI) | 0.45 [0.16, 1.25] |
| 2.3.1 Age 2 to 5 years | 1 | 7419 | Risk Ratio (M‐H, Random, 95% CI) | 0.76 [0.45, 1.29] |
| 2.3.2 Age > 5 years | 1 | 32598 | Risk Ratio (M‐H, Random, 95% CI) | 0.27 [0.16, 0.45] |
| 2.4 Cases of cholera by blood group ‐ First 2 years of follow‐up (3‐dose recipients) | 1 | 41580 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.45 [0.36, 0.58] |
| 2.4.1 Blood Group O | 1 | 13465 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.53 [0.37, 0.76] |
| 2.4.2 All other blood groups | 1 | 28115 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.41 [0.29, 0.56] |
| 2.5 Cases of all cause diarrhoea ‐ 1st year of follow‐up (3‐dose recipients) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.5.1 Severe watery diarrhoea | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.5.2 Any watery diarrhoea | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.5.3 Any diarrhoea | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.6 Deaths ‐ 1st year of follow‐up (3‐dose recipients) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.6.1 All cause deaths | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.6.2 Deaths from non‐dysenteric diarrhoea (adult females only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
2.4. Analysis.

Comparison 2: Whole cell vaccine (WC) versus placebo ‐ Subgroup analysis, Outcome 4: Cases of cholera by blood group ‐ First 2 years of follow‐up (3‐dose recipients)
Comparison 3. Whole cell vaccine plus B subunit (WC‐BS) versus placebo ‐ Subgroup analysis.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Cases of cholera by time of follow‐up (3‐dose recipients) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1.1 First four months after vaccination | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1.2 First year after vaccination | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1.3 Second year after vaccination | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1.4 Third year after vaccination | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1.5 Fourth year after vaccination | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.2 Cases of cholera by age‐group ‐ 1st year of follow‐up (3‐dose recipients) | 1 | 41542 | Risk Ratio (M‐H, Random, 95% CI) | 0.38 [0.14, 1.03] |
| 3.2.1 Age 2 to 5 years | 1 | 7558 | Risk Ratio (M‐H, Random, 95% CI) | 0.62 [0.38, 1.01] |
| 3.2.2 Age > 5 years | 1 | 33984 | Risk Ratio (M‐H, Random, 95% CI) | 0.22 [0.13, 0.39] |
| 3.3 Cases of cholera by age‐group ‐ 2nd year of follow‐up (3‐dose recipients) | 1 | 40014 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.29, 0.60] |
| 3.3.1 Age 2 to 5 years | 1 | 7273 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.53 [0.29, 0.96] |
| 3.3.2 Age > 5 years | 1 | 32741 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.37 [0.23, 0.59] |
| 3.4 Cases of cholera by blood group ‐ First 2 years of follow‐up (3‐dose recipients) | 1 | 41542 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.40 [0.31, 0.51] |
| 3.4.1 Blood Group O | 1 | 13453 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.33, 0.70] |
| 3.4.2 All other blood groups | 1 | 28089 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.24, 0.48] |
| 3.5 Cases of all cause diarrhoea ‐ 1st year of follow‐up (3‐dose recipients) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.5.1 Severe watery diarrhoea | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.5.2 Any watery diarrhoea | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.5.3 Any diarrhoea | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.6 Deaths ‐ 1st year of follow‐up (3‐dose recipients) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.6.1 All cause deaths | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.6.2 Deaths from non‐dysenteric diarrhoea (adult females only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
3.4. Analysis.

Comparison 3: Whole cell vaccine plus B subunit (WC‐BS) versus placebo ‐ Subgroup analysis, Outcome 4: Cases of cholera by blood group ‐ First 2 years of follow‐up (3‐dose recipients)
Comparison 4. Whole cell vaccine (WC) versus Whole cell vaccine plus B subunit (WC‐BS) ‐ Subgroup analysis.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Cases of confirmed cholera by time of follow‐up (3‐dose recipients) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.1.1 First four months after vaccination | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.1.2 Four to eight months after vaccination | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.1.3 First year after vaccination | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.1.4 Second year after vaccination | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.1.5 Third year after vaccination | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.1.6 Fourth year after vaccination | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.2 Cases of cholera by age‐group ‐ 1st year of follow‐up (3‐dose recipients) | 1 | 82085 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.80, 1.55] |
| 4.2.1 Age 2 to 5 years | 1 | 7628 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.65, 1.86] |
| 4.2.2 Age > 5 years | 1 | 33820 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.48 [0.77, 2.85] |
| 4.2.3 Eight to 12 months after vaccination | 1 | 40637 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.53, 1.60] |
| 4.3 Cases of cholera by age‐group ‐ 2nd year of follow‐up (3‐dose recipients) | 1 | 40007 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.66, 1.55] |
| 4.3.1 Age 2 to 5 years | 1 | 7344 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.44 [0.77, 2.71] |
| 4.3.2 Age > 5 years | 1 | 32663 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.40, 1.33] |
| 4.4 Cases of cholera by blood group, First 2 years of follow‐up (3‐dose recipients) | 1 | 41448 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.14 [0.85, 1.54] |
| 4.4.1 Blood group O | 1 | 13422 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.72, 1.68] |
| 4.4.2 Any other blood group | 1 | 28026 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.19 [0.79, 1.79] |
| 4.5 Cases of all cause diarrhoea ‐ 1st year of follow‐up (3‐dose recipients) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.5.1 Severe watery diarrhoea | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.5.2 Any watery diarrhoea | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.5.3 Any diarrhoea | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.6 Deaths ‐ 1st year of follow‐up (3‐dose recipients) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.6.1 All cause deaths | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.6.2 Deaths from non‐dysenteric diarrhoea (adult females only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
4.2. Analysis.

Comparison 4: Whole cell vaccine (WC) versus Whole cell vaccine plus B subunit (WC‐BS) ‐ Subgroup analysis, Outcome 2: Cases of cholera by age‐group ‐ 1st year of follow‐up (3‐dose recipients)
4.3. Analysis.

Comparison 4: Whole cell vaccine (WC) versus Whole cell vaccine plus B subunit (WC‐BS) ‐ Subgroup analysis, Outcome 3: Cases of cholera by age‐group ‐ 2nd year of follow‐up (3‐dose recipients)
4.4. Analysis.

Comparison 4: Whole cell vaccine (WC) versus Whole cell vaccine plus B subunit (WC‐BS) ‐ Subgroup analysis, Outcome 4: Cases of cholera by blood group, First 2 years of follow‐up (3‐dose recipients)
4.5. Analysis.

Comparison 4: Whole cell vaccine (WC) versus Whole cell vaccine plus B subunit (WC‐BS) ‐ Subgroup analysis, Outcome 5: Cases of all cause diarrhoea ‐ 1st year of follow‐up (3‐dose recipients)
4.6. Analysis.

Comparison 4: Whole cell vaccine (WC) versus Whole cell vaccine plus B subunit (WC‐BS) ‐ Subgroup analysis, Outcome 6: Deaths ‐ 1st year of follow‐up (3‐dose recipients)
Comparison 5. Whole cell plus recombinant B subunit vaccine (WC‐rBS) versus placebo ‐ Subgroup analysis.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 5.1 Cases of cholera by age group ‐ 1st year of follow‐up (2 doses) | 1 | 17799 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.52, 2.05] |
| 5.1.1 Age 2 to 5 years | 1 | 2368 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.91 [0.44, 34.90] |
| 5.1.2 Age 6 to 15 years | 1 | 6782 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.22, 2.19] |
| 5.1.3 Age 16 to 65 years | 1 | 8649 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.37, 2.60] |
| 5.2 Cases of cholera by age group ‐ 2nd year of follow‐up (2 doses plus booster) | 1 | 14997 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.40 [0.21, 0.75] |
| 5.2.1 Age 2 to 5 years | 1 | 2040 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.09, 2.62] |
| 5.2.2 Age 6 to 15 years | 1 | 6049 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.53 [0.20, 1.44] |
| 5.2.3 Age 16 to 65 years | 1 | 6908 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.29 [0.11, 0.78] |
| 5.3 Cases of cholera in military recruits, 4 to 18 weeks follow‐up | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5.3.1 Cases of cholera ‐ Occurring after the second dose | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5.3.2 Cases of cholera ‐ Occurring between the first and second dose | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Comparison 6. Whole cell vaccines (all types) versus placebo ‐ Safety outcomes (first dose).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 6.1 Adverse events ‐ Whole cell (WC) versus placebo | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1.1 Abdominal pain | 1 | 613 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.17 [0.80, 1.70] |
| 6.1.2 Severe abdominal pain | 1 | 613 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.51 [0.09, 2.77] |
| 6.1.3 Diarrhoea | 1 | 613 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.50 [0.95, 2.36] |
| 6.1.4 Watery diarrhoea | 1 | 613 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.46 [0.75, 2.84] |
| 6.1.5 Subjective fever | 1 | 613 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.77 [0.86, 3.65] |
| 6.1.6 Nausea | 1 | 613 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.92 [0.83, 4.46] |
| 6.1.7 Vomiting | 1 | 613 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.39 [0.62, 9.15] |
| 6.1.8 Other symptoms requiring bedrest | 1 | 613 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.06, 16.28] |
| 6.2 Adverse events ‐ Whole cell plus B subunit (WC‐BS) versus placebo | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.2.1 Abdominal pain or stomach cramps | 1 | 631 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.17 [0.80, 1.70] |
| 6.2.2 Severe abdominal pain | 1 | 631 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.09, 2.62] |
| 6.2.3 Diarrhoea | 1 | 631 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.35 [0.85, 2.13] |
| 6.2.4 Watery diarrhoea | 1 | 631 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.31 [0.67, 2.57] |
| 6.2.5 Subjective fever | 1 | 631 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.14 [0.52, 2.51] |
| 6.2.6 Nausea | 1 | 631 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.45 [0.60, 3.50] |
| 6.2.7 Vomiting | 1 | 624 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.21 [0.46, 3.22] |
| 6.2.8 Other symptoms requiring bedrest | 1 | 631 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.06, 15.37] |
| 6.3 Adverse events ‐ Whole cell plus recombinant B subunit (WC‐rBS) versus placebo | 7 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 6.3.1 Abdominal pain or stomach cramps | 6 | 2878 | Risk Ratio (M‐H, Random, 95% CI) | 1.11 [0.70, 1.74] |
| 6.3.2 Stomach gurgling | 3 | 1219 | Risk Ratio (M‐H, Random, 95% CI) | 1.16 [0.90, 1.49] |
| 6.3.3 Diarrhoea | 7 | 23870 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.73, 1.49] |
| 6.3.4 Fever | 4 | 941 | Risk Ratio (M‐H, Random, 95% CI) | 0.31 [0.08, 1.26] |
| 6.3.5 Nausea | 4 | 2213 | Risk Ratio (M‐H, Random, 95% CI) | 1.41 [0.32, 6.13] |
| 6.3.6 Vomiting | 4 | 2049 | Risk Ratio (M‐H, Random, 95% CI) | 1.46 [0.40, 5.33] |
| 6.3.7 Headache | 4 | 2488 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.37, 1.40] |
| 6.3.8 Loss of appetite | 2 | 390 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.17, 3.18] |
| 6.3.9 Dizziness | 1 | 1313 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.41, 2.69] |
| 6.3.10 Any adverse event | 2 | 21616 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.71, 1.28] |
| 6.3.11 Any serious adverse event | 2 | 21133 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 6.3.12 Other | 1 | 624 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.35, 2.29] |
| 6.4 Adverse events ‐ Bivalent whole cell (BivWC) versus placebo | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.4.1 Diarrhoea | 4 | 67414 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.42, 1.55] |
| 6.4.2 Abdo pain | 4 | 67414 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.63, 1.88] |
| 6.4.3 Gas | 1 | 160 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.19, 2.22] |
| 6.4.4 Loss of appetite | 3 | 514 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.20 [0.35, 4.13] |
| 6.4.5 Nausea | 4 | 67414 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.38, 1.67] |
| 6.4.6 Vomiting | 4 | 67414 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.57, 2.21] |
| 6.4.7 Fever | 4 | 67414 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.62 [0.84, 3.10] |
| 6.4.8 Headache | 3 | 514 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.55, 1.75] |
| 6.4.9 General ill feeling | 3 | 514 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.70 [0.61, 4.77] |
| 6.4.10 Rash | 1 | 66900 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.64 [0.27, 9.83] |
| 6.4.11 Weakness | 1 | 66900 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.27 [0.03, 2.45] |
| 6.4.12 Itch | 1 | 66900 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.29 [0.34, 31.58] |
| 6.4.13 Cough | 1 | 66900 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.15, 7.77] |
| 6.4.14 Dizziness | 1 | 66900 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.07, 17.51] |
Comparison 7. Whole cell vaccines (all types) versus placebo ‐ Safety outcomes (second dose).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 7.1 Adverse events ‐ Whole cell plus recombinant B subunit (WC‐rBS) versus placebo | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.1.1 Abdominal pain or stomach cramps | 5 | 2061 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.69, 1.32] |
| 7.1.2 Stomach gurgling | 2 | 556 | Risk Ratio (M‐H, Fixed, 95% CI) | 7.82 [4.36, 14.03] |
| 7.1.3 Diarrhoea | 5 | 2061 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.20 [0.70, 2.05] |
| 7.1.4 Fever | 4 | 896 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.19 [0.34, 4.20] |
| 7.1.5 Nausea | 3 | 1438 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.26, 4.06] |
| 7.1.6 Vomiting | 4 | 1859 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.13 [0.54, 8.44] |
| 7.1.7 Headache | 3 | 1674 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.26 [0.79, 1.99] |
| 7.1.8 Loss of appetite | 2 | 387 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.80 [0.36, 129.27] |
| 7.1.9 Dizziness | 1 | 1165 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.79 [0.54, 42.75] |
| 7.1.10 Any adverse event | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 7.1.11 Any serious adverse event | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 7.1.12 Other | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 7.2 Adverse events ‐ Bivalent whole cell (BivWC) versus placebo | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.2.1 Diarrhoea | 4 | 67397 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.17 [0.53, 2.57] |
| 7.2.2 Abdo pain | 4 | 67397 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.41 [0.64, 3.12] |
| 7.2.3 Gas | 1 | 155 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.68 [0.12, 3.93] |
| 7.2.4 Loss of appetite | 3 | 497 | Risk Ratio (M‐H, Fixed, 95% CI) | 9.12 [0.50, 166.49] |
| 7.2.5 Nausea | 4 | 67397 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.08 [1.12, 22.92] |
| 7.2.6 Vomiting | 4 | 67397 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.41, 2.01] |
| 7.2.7 Fever | 4 | 67397 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.46, 2.04] |
| 7.2.8 Headache | 3 | 497 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.24 [0.59, 2.62] |
| 7.2.9 General ill feeling | 3 | 497 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.22 [0.36, 4.15] |
| 7.2.10 Rash | 1 | 66900 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.37 [0.01, 8.96] |
| 7.2.11 Weakness | 1 | 66900 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 7.2.12 Itch | 1 | 66900 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 7.2.13 Cough | 1 | 66900 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 7.2.14 Dizziness | 1 | 66900 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
Comparison 8. Live attenuated vaccines (all types) versus placebo ‐ Efficacy outcomes.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 8.1 Cases of cholera following natural infection ‐ CVD 103HgR versus placebo | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 8.1.1 First year after vaccination | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 8.1.2 Second year after vaccination | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 8.1.3 Third year after vaccination | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 8.2 Severe cholera following natural infection ‐ CVD 103HgR versus placebo | 1 | 67508 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.58 [0.61, 4.07] |
| 8.3 Death from any cause (except motor accidents) | 1 | 67508 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.83, 1.28] |
| 8.4 Death from diarrhoea (any organism) | 1 | 67508 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.26, 2.17] |
| 8.5 Cases of moderate to severe diarrhoea ‐ following artificial challenge | 3 | 108 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.08 [0.02, 0.34] |
| 8.5.1 CVD 103HgR | 1 | 51 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.09 [0.01, 0.67] |
| 8.5.2 Peru 15 | 1 | 36 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.05 [0.00, 0.79] |
| 8.5.3 VC638 | 1 | 21 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.15 [0.01, 2.86] |
| 8.6 Cases of any diarrhoea ‐following artificial challenge | 3 | 108 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.14 [0.07, 0.28] |
| 8.6.1 CVD 103HgR | 1 | 51 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.20 [0.09, 0.44] |
| 8.6.2 Peru 15 | 1 | 36 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.07 [0.01, 0.52] |
| 8.6.3 VC638 | 1 | 21 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.05 [0.00, 0.80] |
Comparison 9. Live attenuated vaccines (all types) versus placebo ‐ Safety outcomes.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 9.1 Adverse events ‐ CVD 103‐HgR versus placebo | 12 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 9.1.1 Diarrhoea | 12 | 3320 | Risk Ratio (M‐H, Random, 95% CI) | 1.09 [0.81, 1.47] |
| 9.1.2 Fever | 8 | 2516 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.57, 1.23] |
| 9.1.3 Vomiting | 9 | 2866 | Risk Ratio (M‐H, Random, 95% CI) | 1.22 [0.84, 1.79] |
| 9.1.4 Nausea | 3 | 1474 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.67, 1.80] |
| 9.1.5 Seizure | 1 | 1077 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 9.1.6 Itching | 1 | 1077 | Risk Ratio (M‐H, Random, 95% CI) | 2.00 [0.61, 6.61] |
| 9.1.7 Rash | 3 | 1489 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.26, 3.49] |
| 9.1.8 Abdominal pain | 7 | 2155 | Risk Ratio (M‐H, Random, 95% CI) | 1.12 [0.86, 1.46] |
| 9.1.9 Headache | 3 | 1243 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [0.91, 1.58] |
| 9.1.10 Anorexia | 3 | 478 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.48, 2.36] |
| 9.1.11 Malaise | 2 | 434 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.61, 1.26] |
| 9.1.12 Borborygmus | 1 | 81 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.59, 1.35] |
| 9.1.13 Liquid stools | 1 | 81 | Risk Ratio (M‐H, Random, 95% CI) | 1.37 [0.33, 5.72] |
| 9.2 Adverse events ‐ Peru 15 versus placebo | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 9.2.1 Loss of appetite | 1 | 59 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.16, 2.55] |
| 9.2.2 Loss of energy | 1 | 59 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.42 [0.32, 6.41] |
| 9.2.3 Abdominal cramps | 3 | 369 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.92 [0.62, 13.82] |
| 9.2.4 Headache | 3 | 349 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.14 [1.27, 13.48] |
| 9.2.5 Vomiting | 2 | 299 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.01 [0.26, 96.01] |
| 9.2.6 Nausea | 1 | 59 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.66 [0.38, 7.26] |
| 9.2.7 Diarrhoea | 3 | 369 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.44 [0.12, 48.45] |
| 9.2.8 Gas | 1 | 70 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.27 [0.10, 53.81] |
| 9.2.9 Fever | 2 | 310 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 9.2.10 Respiratory symptoms | 1 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.25, 3.47] |
| 9.2.11 Gastrointestinal symptoms | 1 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.50 [0.72, 3.14] |
| 9.3 Adverse events ‐ VC638 versus placebo | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 9.3.1 Abdominal pain | 3 | 137 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.94 [0.94, 4.02] |
| 9.3.2 Nausea | 1 | 36 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.00 [0.56, 28.40] |
| 9.3.3 Diarrhoea | 3 | 137 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.05 [0.65, 6.48] |
| 9.3.4 Headache | 3 | 137 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.30 [0.83, 6.36] |
| 9.3.5 General discomfort | 1 | 36 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.60 [0.13, 50.25] |
| 9.3.6 Borborygmus | 3 | 137 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.23 [0.77, 1.95] |
| 9.3.7 Vomiting | 2 | 101 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.05, 24.33] |
| 9.3.8 Fever | 2 | 101 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 9.3.9 Heartburn | 1 | 56 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.23, 4.40] |
| 9.3.10 Malaise | 1 | 56 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
Comparison 10. Live attenuated CVD 103‐HgR vaccine versus placebo ‐ Subgroup analysis.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 10.1 Cases of cholera by age group (age 2‐5 years) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 10.1.1 First year after vaccination | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 10.1.2 Second year after vaccination | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 10.1.3 Third year after vaccination | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 10.2 Cases of confirmed cholera attending healthcare facilities (age over 5 years) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 10.2.1 First year after vaccination | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 10.2.2 Second year after vaccination | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 10.2.3 Third year after vaccination | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 10.3 Cases of cholera within four years and five months, by blood group | 1 | 67508 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.54, 1.24] |
| 10.3.1 Blood group O | 1 | 24303 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.60 [0.34, 1.08] |
| 10.3.2 All other blood groups | 1 | 43205 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.15 [0.63, 2.10] |
| 10.4 Any diarrhoea following artifical challenge, by blood group | 1 | 51 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.17 [0.07, 0.43] |
| 10.4.1 Blood group O | 1 | 23 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.30 [0.13, 0.73] |
| 10.4.2 Blood group non‐O | 1 | 28 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.08 [0.01, 0.54] |
| 10.5 Moderate or severe diarrhoea due to V. cholerae after artificial challenge, by blood group | 1 | 51 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.12 [0.02, 0.64] |
| 10.5.1 Blood group O | 1 | 23 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.13 [0.02, 1.00] |
| 10.5.2 Blood group non‐O | 1 | 28 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.10 [0.01, 1.72] |
| 10.6 Additional adverse event data | 0 | Other data | No numeric data |
10.1. Analysis.

Comparison 10: Live attenuated CVD 103‐HgR vaccine versus placebo ‐ Subgroup analysis, Outcome 1: Cases of cholera by age group (age 2‐5 years)
10.2. Analysis.

Comparison 10: Live attenuated CVD 103‐HgR vaccine versus placebo ‐ Subgroup analysis, Outcome 2: Cases of confirmed cholera attending healthcare facilities (age over 5 years)
10.3. Analysis.

Comparison 10: Live attenuated CVD 103‐HgR vaccine versus placebo ‐ Subgroup analysis, Outcome 3: Cases of cholera within four years and five months, by blood group
10.4. Analysis.

Comparison 10: Live attenuated CVD 103‐HgR vaccine versus placebo ‐ Subgroup analysis, Outcome 4: Any diarrhoea following artifical challenge, by blood group
10.5. Analysis.

Comparison 10: Live attenuated CVD 103‐HgR vaccine versus placebo ‐ Subgroup analysis, Outcome 5: Moderate or severe diarrhoea due to V. cholerae after artificial challenge, by blood group
10.6. Analysis.
Comparison 10: Live attenuated CVD 103‐HgR vaccine versus placebo ‐ Subgroup analysis, Outcome 6: Additional adverse event data
| Additional adverse event data | |||
| Study | Adverse event monitoring | Adverse events reporting | Results |
| Kotloff 1992 | Monitored daily for 7 days | Data presented in an unusable form | 'Among volunteers who experienced symptoms, the complaints were mild'. 'All episodes of fever were low grade. No subject exceeded the minimum definition of diarrhea (four stools within 24 h) or vomiting (one episode of emesis) or met these criteria for more than 1 day'. |
| Migasena 1989a | Seen daily for 5 days | Text summary only | 'No significant adverse reactions, including fever, diarrhea, vomiting, anorexia, or abdominal cramps were observed in any participant during the 7‐day period of observation'. |
| Perry 1998 | Seen daily for 6 days after each inoculation of vaccine or placebo | Data presented is from a crossover trial where all participants took vaccine and placebo 12 days apart | 'No significant difference was seen in reported diarrhoea, fever or vomiting following vaccine or placebo'. |
| Su‐Arehawaratana 1992a | Monitored daily for 7 days | Numerical data is only provided for diarrhoea | 'No increased rate of diarrhoeal episodes or other gastrointestinal adverse reactions was observed among vaccine than among placebo recipients'. |
| Su‐Arehawaratana 1992b | Monitored daily for seven days after each dose | Numerical data is only provided for diarrhoea | 'No increased rate of diarrhoeal episodes or other gastrointestinal adverse reactions was observed among vaccine than among placebo recipients'. |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Anh 2007.
| Study characteristics | ||
| Methods | Design: A randomized controlled trial (individually randomized) Trial dates and duration: Enrollment from May to June 2005; follow‐up for 28 days |
|
| Participants | Sample size: 153 participants enrolled Inclusion criteria: Age 18 to 40 years, healthy male and non‐pregnant females, written informed consent Exclusion criteria: History of diarrhoea, anti‐diarrhoeal or antibiotic use during the past week, history of diarrhoea and abdominal pain lasting for 2 weeks during the past 6 months |
|
| Interventions | Vaccine: Bivalent killed whole‐cell vaccine (BivWC; mORCVAX, VABIOTECH) Placebo: Heat‐killed E. coli K12 strain All participants were randomized to receive 2 doses, at an interval of 14 days. |
|
| Outcomes |
Included in review:
Not included in the review:
|
|
| Notes | Location: SonLa Province, Northwest Vietnam Setting: Source of funding: The Bill and Melinda Gates Foundation through the Diseases of Most Impoverished Program administered by the International Vaccine Institute, and the Swedish International Development Cooperation Agency. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: 'A randomization list was prepared by a statistician who otherwise was not involved in the study. Randomization numbers were generated in blocks of four' |
| Allocation concealment (selection bias) | Low risk | Comment: See other comments, no further description. |
| Blinding (performance bias and detection bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Blinding (performance bias and detection bias) Safety outcomes | Low risk | Quote: 'The reformulated vaccine and the placebo were packaged as liquid formulations in identical vials containing five 1.5‐ml doses'. 'A physician who was unaware of the study agent received by the subject conducted a structured interview regarding the subjects...symptoms'. |
| Incomplete outcome data (attrition bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Incomplete outcome data (attrition bias) Safety outcomes | Low risk | Comment: Nine participants (5.9%) did not receive the second dose of vaccine; 5 were found ineligible and 4 lost to follow‐up. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No evidence of other bias |
Begue 1995.
| Study characteristics | ||
| Methods | Design: Randomized controlled trial (individual randomization) Duration and dates (field work): March 1993 |
|
| Participants | Sample size: 624 received the first dose of vaccine, 541 received 2 doses Inclusion criteria: Persons aged 2 to 65 years Exclusion criteria: pregnancy |
|
| Interventions | Vaccine: Killed whole‐cell vaccine plus recombinant cholera toxin subunit (WC‐rBS; Dukoral®, SBL, Sweden) Placebo: Inactived E. coli K12 suspension Vaccine and placebo were administered along with freshly prepared antacid solution. Two doses were given two weeks apart. |
|
| Outcomes |
Included in the review:
Not included in the review:
|
|
| Notes | Location: outskirts of Lima, Peru Setting: Small community of 300 families. Source of funding: US Naval Medical Research and Development Command |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "..administer the vaccine or placebo according to a pre‐randomized list" Comment: Unclear description but probably low risk of bias |
| Allocation concealment (selection bias) | Low risk | Comment: Not described but probably low risk of bias |
| Blinding (performance bias and detection bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Blinding (performance bias and detection bias) Safety outcomes | Low risk | Quote: 'Inactivated Escherichia coli K12, identical in appearance to the vaccine, was used as placebo, and was administered orally in the above antacid solution, and in a double blinded manner.' |
| Incomplete outcome data (attrition bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported as an outcome |
| Incomplete outcome data (attrition bias) Safety outcomes | Low risk | Comment: No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No evidence of other bias |
Benítez 1999.
| Study characteristics | ||
| Methods | Design: Randomized controlled trial (individually randomized) Duration and dates (field work): Not stated |
|
| Participants | Sample size: 56 (this paper describes 4 separate small trials with different doses of VC638. A total of 42 received vaccine and 14 placebo) Inclusion criteria: Age 18 to 40 years, male students or workers, good health, informed consent. Exclusion criteria: Recent history of diarrhoeal disease or cholera vaccination, taking medication at the time of recruitment. |
|
| Interventions | Vaccine: VC638 ‐ A live attenuated strain of V. cholerae O1 El Tor Ogawa
Placebo: Buffer alone |
|
| Outcomes |
Included in review:
Not included in the review:
|
|
| Notes | Location: La Lisa of Havana, Cuba Setting: Institute of Tropical Medicine Source of funding: None stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: Not described as randomised though it seems unlikely that this was not done. |
| Allocation concealment (selection bias) | Low risk | Quote: 'The clinical investigator assigned a letter to each volunteer. The code was kept by the monitor till the end of the experiment and analysis of all samples'. |
| Blinding (performance bias and detection bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Blinding (performance bias and detection bias) Safety outcomes | Low risk | Quote: 'The placebo consisted of bicarbonate buffer alone and was indistinguishable from the vaccine preparation. To ensure double‐blinding, identical flasks, containing either inoculum or placebo, were coded by an outside monitor'. |
| Incomplete outcome data (attrition bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Incomplete outcome data (attrition bias) Safety outcomes | Low risk | Comment: No losses recorded during the monitoring of adverse events |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No evidence of any other bias |
Chen 1996.
| Study characteristics | ||
| Methods | Design: Randomized controlled trial (individually randomized) Duration and dates (field work): Jun 1993 to Jan 1994 |
|
| Participants | Sample size: 369 Inclusion criteria: Students from the primary and secondary school, and factory workers of Jiu‐Fu area, Guang‐Zhou. Exclusion criteria: A history of cholera, or acute diarrhoea in the past 2 weeks. |
|
| Interventions | Vaccine 1: Killed whole‐cell vaccine plus recombinant cholera toxin B subunit (locally formulated)
Vaccine 1: Killed whole‐cell vaccine plus recombinant cholera toxin B subunit (locally formulated)
Placebo: Buffer alone |
|
| Outcomes |
Included in review:
Not included in the review:
|
|
| Notes | Location: Jiu‐Fu Area in Guang‐Zhou city Setting: Source of funding: National 638 funds and fund from the Academy of Guang‐Dong Province |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Labelled as 'Randomized', no further details. |
| Allocation concealment (selection bias) | Unclear risk | None described. |
| Blinding (performance bias and detection bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy is not reported |
| Blinding (performance bias and detection bias) Safety outcomes | Unclear risk | Described as 'double‐blind'. No further details |
| Incomplete outcome data (attrition bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy is not reported |
| Incomplete outcome data (attrition bias) Safety outcomes | Low risk | No losses to follow‐up reported |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No evidence of other bias |
Clemens 1987.
| Study characteristics | ||
| Methods | Design: Randomized controlled trial (individual randomization) Trial dates and duration: 1984, with short‐term follow‐up |
|
| Participants | Sample size: 1,257 enrolled and took first dose of vaccine or placebo, 1051 received two doses, and 898 received third doses Inclusion criteria: Children aged 2 to 15 years and women aged over 15 years. Exclusion criteria: Pregnancy, people too ill to leave their beds on the day of the vaccination |
|
| Interventions | Vaccine 1: Killed whole cell plus purified cholera B subunit vaccine (WC‐BS) Vaccine 2: Killed whole cell vaccine (WC) Placebo 1: Heat‐inactivated E. coli K12 strain Placebo 2: Distilled water |
|
| Outcomes |
Included in the review:
Not included in the review:
|
|
| Notes |
Location: Matlab, Bangladesh Setting: Community, within a health and demographic surveillance site Source of funding: United States Agency for International Development (USAID); the government of Japan; the Swedish Agency for Research Cooperation with Developing Countries, and the World Health Organization. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "randomly assigned" Comment: Unclear description but probably low risk of bias |
| Allocation concealment (selection bias) | Low risk | Quote: "Each of the agents, labelled only as W,X,Y or Z" Comment: Allocation concealed |
| Blinding (performance bias and detection bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Blinding (performance bias and detection bias) Safety outcomes | Low risk | Quote: "..study physicians who were kept unaware of the identities of agents received by subjects.." |
| Incomplete outcome data (attrition bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Incomplete outcome data (attrition bias) Safety outcomes | Low risk | Comment: No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No evidence of other bias |
Clemens 1988 Bangladesh.
| Study characteristics | ||
| Methods | Design: Randomized controlled trial (individual randomization) Trial dates and duration: Vaccination January to March 1985; follow‐up 5 years Surveillance: Passive surveillance system at diarrhoea treatment centres serving the study population. |
|
| Participants | Number of participants: 89,596 received at least one dose of vaccine or placebo, 62,285 ingested three complete doses Inclusion criteria: children aged 2‐15 years and women over the age of 15 Exclusion criteria: Pregnancy, illness requiring bed rest |
|
| Interventions | Vaccine 1: Killed whole cell plus purified cholera B subunit vaccine (WC‐BS) Vaccine 2: Killed whole cell vaccine (WC) Placebo: Escherichia coli K12 strain placebo (K12) All subjects were randomized to receive three doses, at 6 week intervals. All doses were ingested with antacid. |
|
| Outcomes |
Included in review:
Cases of diarrhoea and cholera were only included in the analysis if they occurred at least 14 days after the third dose of vaccine or placebo. Not included in the review:
|
|
| Notes | Location: Matlab, Bangladesh Setting: Surveillance study area, served by three diarrhoea treatment centres. Source of funding: Bill and Melinda Gates Foundation; U.S. National Institutes of Health; U.S. National Science Foundation; Swedish International Development Cooperation Agency; governments of Korea, Japan and Kuwait, USAID, Word Health Organization |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote:"After computerisation of the census, we assigned every person in the eligible age‐gender categories to letters A, B or C, using simple randomisation" |
| Allocation concealment (selection bias) | Low risk | Quote: "The agents were identified only by the letters A, B and C" Comment: Allocation concealed |
| Blinding (performance bias and detection bias) Efficacy outcomes | Low risk | Quote: "During the conduct of the study, the identities of these letter...were unknown to all persons connected with the trial in Bangladesh" |
| Blinding (performance bias and detection bias) Safety outcomes | Low risk | As above |
| Incomplete outcome data (attrition bias) Efficacy outcomes | Low risk | Comment: Attrition between the first and third doses was high: 30.5%. The protective effect is reported as being similar in those who only received two doses, so these losses are unlikely to have introduced significant bias. |
| Incomplete outcome data (attrition bias) Safety outcomes | Low risk | Comment: There was no missing data for adverse events. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting. |
| Other bias | Low risk | No evidence of other bias. |
Cohen 2002.
| Study characteristics | ||
| Methods | Design: Randomized controlled trial (individual randomization) Trial dates and duration: 2000‐2001 |
|
| Participants | Number of participants: 59 (36 included in the challenge study) Inclusion criteria: Age 18 to 40 years, informed consent, and judged likely to comply with the study requirements. Exclusion criteria: Clinically significant abnormalities on urinalysis, full blood count, serum hepatic transaminases, glucose, creatine, urea nitrogen, electrolytes or ECG. Travel to cholera endemic areas in the previous 5 years, history of cholera or ETEC challenge, recent antibiotic use, abnormal stool pattern, regular laxative use, failure to pass psychological screening, allergy to tetracycline or ciprofloxacin, pregnant or breastfeeding, HIV‐positive, hep B‐positve, hep C‐postive, stool culture positive for enteric pathogen. |
|
| Interventions | Vaccine: Peru 15 ‐ a live attenuated strain of V. cholerae O1 El Tor Inaba plus 200 ml CeraVacx buffer (Cera Products, Columbia) Placebo: 200ml CeraVacx buffer (Cera Products, Columbia) Challenge: Three months after vaccination, willing participants were given artificial challenge with 105 CFU of virulent V. cholerae 01 El Tor Inaba Strain N16961, prepared from a standardised frozen inoculum |
|
| Outcomes |
Included in the review:
Participants who went on to receive artificial challenge were also monitored for diarrhoea, and positive stool culture with the challenge strain; on an inpatient basis.
Not included in the review:
|
|
| Notes | Location: USA Setting: Volunteer study. Outpatient phase for adverse events, inpatients phase for response to artificial challenge Sources of funding: National Institutes of Health, General Clinical Research Centres Program |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: ‘sequence generated by SAS PROC PLAN’. |
| Allocation concealment (selection bias) | Low risk | Comment: The randomization code generated off‐site and study blinded until after analysis |
| Blinding (performance bias and detection bias) Efficacy outcomes | Low risk | Quote: ‘Investigators did not know the vaccine status of all volunteers until the data was locked and the code was broken after the challenge was completed’ |
| Blinding (performance bias and detection bias) Safety outcomes | Low risk | Quote: 'Volunteers were randomly assigned to groups in a double‐blind manner....A study nurse who was unaware of the group assignment reviewed the (symptom) diary'. |
| Incomplete outcome data (attrition bias) Efficacy outcomes | High risk | Comment: The loss of participants between randomisation and the challenge study (39%) could introduce significant bias. |
| Incomplete outcome data (attrition bias) Safety outcomes | Low risk | Comment: The data was complete for the three days of adverse event monitoring |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No evidence of other bias |
Concha 1995.
| Study characteristics | ||
| Methods | Design: Randomized controlled trial (cluster randomized by household) Duration: Two months, January and February 1992 |
|
| Participants | Sample size: 1313 received an initial dose of vaccine or placebo, 1165 received two doses. Inclusion criteria: People between the ages of 12 months and 64 years who have resided in the study area for at least two months. Exclusion criteria: Confirmed or possible pregnancy, illness requiring bed rest, known mental illness or incapacity to give informed consent, diarrhoea at the time either of the two vaccine doses were administered. |
|
| Interventions | Vaccine: Killed whole‐cell vaccine plus recombinant cholera toxin subunit (WC‐rBS; Dukoral®, SBL, Sweden) Placebo: killed whole cells of E. coli K12. Both vaccine and placebo were administered with a buffer solution. Two doses were given, two weeks apart. |
|
| Outcomes |
Included in the review:
Not included in the review:
|
|
| Notes | Location: Los Olivios, Barraquilla, Colombia Setting: Households in a poor neighbourhood Source of funding: Pan American Health Organization and World Health Organization. Vaccine donated by the National Bacteriological Laboratory in Stockholm, Sweden. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Households were randomly selected to receive either vaccine or placebo" Comment: The method of sequence generation is unclear |
| Allocation concealment (selection bias) | Low risk | Quote: "the vaccination team knew the two only as 'vaccine A and 'vaccine B' |
| Blinding (performance bias and detection bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy is not reported |
| Blinding (performance bias and detection bias) Safety outcomes | Low risk | Quote: "Both agents were administered double‐blind; the vaccination team know the two only as "vaccine A" and "vaccine B"....nurses, who .. were unaware of how the agent were distributed..record any..symptoms" |
| Incomplete outcome data (attrition bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Incomplete outcome data (attrition bias) Safety outcomes | Low risk | Comment: No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | High risk | Comment: 620 individuals who originally consented to participate dropped out of the study because of a political campaign against it. |
Cryz 1990.
| Study characteristics | ||
| Methods | Design: Randomized controlled trial (individually randomized) Trial dates and duration: Study dates not given; follow‐up 21 days |
|
| Participants | Sample size: 50 enrolled Inclusion criteria: Age 21 to 45 years, healthy, informed consent Exclusion criteria: None stated |
|
| Interventions | Vaccine: CVD 103‐HgR live attenuated vaccine containing:
Placebo: 5 x 108 CFU of heat‐killed E. coli K12 strain |
|
| Outcomes |
Included in review:
Not included in the review:
|
|
| Notes | Location: Switzerland Setting: Not stated Source of funding: None stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as 'randomised', no further details given. |
| Allocation concealment (selection bias) | Unclear risk | None described |
| Blinding (performance bias and detection bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Blinding (performance bias and detection bias) Safety outcomes | Low risk | Quote: 'A coded sachet containing either vaccine or placebo was mixed with the buffer solution and immediately ingested.', 'The appearance of the placebo was identical to that of the vaccine.' |
| Incomplete outcome data (attrition bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Incomplete outcome data (attrition bias) Safety outcomes | Low risk | Comment: No losses are reported during the first week of adverse event surveillance |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No evidence of other bias |
García 2005.
| Study characteristics | ||
| Methods | Design: Randomized controlled study with artificial challenge (Individually randomized) Trial dates and duration: Dates not stated; artifical challenge took place 1 month after vaccination |
|
| Participants | Sample size: 45 (21 in challenge study) Inclusion criteria: Age 18 to 40 years, volunteer male workers among the western scientific community, good health, informed consent. Exclusion criteria: Recent history of diarrhoeal disease or cholera vaccination, taking any medication at the time of recruitment, any abnormality in clinical laboratory tests (complete blood count, chemistry panel, HIV and Hep C virus antibodies, Hep B virus antigen), stool cultures positive for an enteric pathogen, recent antibiotic use, or psychological incompatibility with accepting quarantine conditions |
|
| Interventions | Vaccine: VC638 ‐ A live attenuated strain of V. Cholerae O1 El Tor Ogawa
Placebo: Buffer alone Artificial challenge: 7 x 105 CFU of fully virulent El Tor Ogawa strain 3008 (orally). |
|
| Outcomes |
Included in review:
Not included in the review:
|
|
| Notes | Location: Havana Cuba Setting: Inpatient trials unit, Institute of Tropical Medicine Source of funding: None stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: Described as 'Randomized', no further details given |
| Allocation concealment (selection bias) | Unclear risk | Comment: None described. |
| Blinding (performance bias and detection bias) Efficacy outcomes | Unclear risk | Comment: Described as 'double blind', no further details given. |
| Blinding (performance bias and detection bias) Safety outcomes | Unclear risk | Comment: Described as 'double blind', no further details given. |
| Incomplete outcome data (attrition bias) Efficacy outcomes | High risk | Comment: The loss of participants between randomisation and the challenge study (47%) could introduce significant bias. |
| Incomplete outcome data (attrition bias) Safety outcomes | Low risk | Comment: The data was complete as participants for the three days of adverse event monitoring |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No evidence of other bias |
Gotuzzo 1993.
| Study characteristics | ||
| Methods | Design: A randomized controlled trial (individually randomized) Duration: Vaccination from Sept to Dec 1991; follow‐up 28 days |
|
| Participants | Sample size: 241 enrolled Inclusion criteria: Adults aged 18 to 38 years Exclusion criteria: Pregnancy, antibiotics or diarrhoea within the previous 72 h, previous cholera vaccine. |
|
| Interventions | Vaccine 1: CVD 103‐HgR live attenuated vaccine containing:
Vaccine 2: CVD 103‐HgR live attenuated vaccine containing:
Placebo: 5 x 108 cells of heat‐killed E. coli K‐12 strain |
|
| Outcomes |
Included in review:
Not included in the review:
|
|
| Notes | Location: Peru Setting: 2 groups: high socioeconomic group: medical students and physicians from the Facultad de Medicina, Universidad Peruana Cayetano Heredia, and a low socioeconomic group: selected from Canto Grande, a periurban slum community with poor water and sanitation. Source of funding: National Institute of Allergy and Infectious Diseases (NIAID) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: Described as 'randomized', no further details given. |
| Allocation concealment (selection bias) | Low risk | Quote: 'Eligible adults were administered coded preparations sequentially labelled A, B, or C, two of which contained the vaccine and the other a placebo'. |
| Blinding (performance bias and detection bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Blinding (performance bias and detection bias) Safety outcomes | Low risk | Quote: 'Double‐blind clinical follow‐up was maintained for 7 days following vaccination'. |
| Incomplete outcome data (attrition bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Incomplete outcome data (attrition bias) Safety outcomes | Low risk | Comment: No losses to follow up are reported |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No evidence of other bias |
Hallander 2002.
| Study characteristics | ||
| Methods | Design: Randomized controlled trial (individually randomized) Duration: Enrolled; follow‐up 28 days |
|
| Participants | Sample size: 249 Inclusion criteria: Age 1 to 12 years, permanent resident in study area, informed consent, good health Exclusion criteria: None stated |
|
| Interventions | Vaccine Killed whole‐cell vaccine plus recombinant cholera toxin subunit (WC‐rBS; Dukoral®, SBL, Sweden) Placebo: heat‐killed E. coli K‐12 strain (C 600) All participants were randomized to receive 2 doses, 14 days apart |
|
| Outcomes |
Included in review:
Not included in the review:
|
|
| Notes | Location: León, Nicaragua Setting: Source of funding: None declared *This paper contained the details of three individual trials: OCV‐023, OCV‐024 and OCV‐028. OCV‐023 and OCV‐024 were excluded from this review as they used a variation on this vaccine for which no primary efficacy data is available. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: Described as 'randomized', no further details given. |
| Allocation concealment (selection bias) | Unclear risk | Comment: None described. |
| Blinding (performance bias and detection bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Blinding (performance bias and detection bias) Safety outcomes | Unclear risk | Comment: None described. |
| Incomplete outcome data (attrition bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Incomplete outcome data (attrition bias) Safety outcomes | Low risk | Comment: No losses described |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No evidence of other bias |
Kanungo 2009.
| Study characteristics | ||
| Methods | Design: A randomized controlled trial (individually randomized) Trial dates and duration: Enrollment from June to August 2007; follow‐up for 28 days |
|
| Participants | Sample size: 160 patients stratified into adults and children Inclusion criteria: Age 18 to 40 years for adult study, 1 to 18 years for children, healthy male and non‐pregnant females, written informed consent Exclusion criteria: Abdominal pain, loss of appetite, nausea, general ill feeling or vomiting within the past 24 h, any diarrhoea within 6 weeks of enrolment, diarrhoea or abdominal pain lasting more than 2 weeks in the past 6 months, antibiotics in the past 2 weeks, anti‐diarrhoeal medication or acute disease in the past week, history of serious chronic disease or an immunocompromising condition or therapy |
|
| Interventions | Vaccine: Bivalent killed whole‐cell vaccine (BivWC: SHanchol®, Shantha Biotechnics) Placebo: Heat killed E. coli K12 strain All subjects were randomized to receive 2 doses, at an interval of 14 days. All doses were administered via an oral syringe and offered water. |
|
| Outcomes |
Included in review:
Not included in the review:
|
|
| Notes | Location: Kolkata, India Setting: The clinical trial unit of the National Institute of Cholera and Enteric Diseases (NICED) Source of funding: the Bill and Melinda Gates Foundation through the Diseases of the Most Impoverished Program and the Cholera Vaccine Initiative, and the governments of Korea, Kuwait and Sweden through the International Vaccine Institute |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: 'Separate randomization lists for the two age groups were prepared by a statistician in the IVI who was otherwise not involved in the study. Randomization was performed in blocks of four using Visual Fortran 5.0 (Digital USA)'. |
| Allocation concealment (selection bias) | Low risk | Quote: 'Vials were labeled with four‐letter codes... the identities of the codes were only known to Shantha staff who labeled the vials and who were otherwise not involved in the study', 'Eligible subjects were assigned to receive either vaccine or placebo according to the randomization list. Subjects were assigned sequentially to a number in the randomization list'. |
| Blinding (performance bias and detection bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Blinding (performance bias and detection bias) Safety outcomes | Low risk | Quote: 'Study staff and participants were unaware of the identity of the codes during the study period'. |
| Incomplete outcome data (attrition bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Incomplete outcome data (attrition bias) Safety outcomes | Low risk | Comment: Five participants (3.1%) were lost to follow‐up between the first and second doses. Four withdrew consent and one was found to be ineligible. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No evidence of other bias |
Kotloff 1992.
| Study characteristics | ||
| Methods | Design: Randomized controlled cross‐over trial (individually randomized) Duration: Study dates not given; follow‐up 28 days |
|
| Participants | Sample size: 94 enrolled Inclusion criteria: Age 18 to 40 years, college students, informed consent Exclusion criteria: Previously lived in a cholera endemic area, antibiotic therapy in previous 2 weeks |
|
| Interventions | Vaccine: CVD 103‐HgR live attenuated vaccine containing:
Placebo: 5 x 108 CFU of heat‐killed E. coli K12 strain All participants were randomized to receive one dose with crossover to receive the alternative arm after 8 days. |
|
| Outcomes |
Included in review:
Not included in the review:
|
|
| Notes | Location: Maryland, USA Setting: College students Source of funding: Swiss Serum and Vaccine Institute |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: 'In a double‐blind fashion, subjects were randomly allocated to receive a single dose'. |
| Allocation concealment (selection bias) | Unclear risk | Comment: None described |
| Blinding (performance bias and detection bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Blinding (performance bias and detection bias) Safety outcomes | Low risk | Quote: 'The blind was maintained through analysis of data'. |
| Incomplete outcome data (attrition bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Incomplete outcome data (attrition bias) Safety outcomes | Low risk | Comment: No losses to follow up are reported |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No evidence of other bias |
Lagos 1993.
| Study characteristics | ||
| Methods | Design: A randomized controlled trial (individually randomized) Duration: Vaccination took place Nov to Dec 1991; follow‐up 7 days. |
|
| Participants | Sample size: 81 enrolled Inclusion criteria: Age 18 to 35 years, male conscripts of the Chilean Air Force, employees of the Roberto del Rio Hospital, and medical students of the university of Chile, informed consent Exclusion criteria: Antibiotics or diarrhoea during the previous week, signs or symptoms of any acute disease, any type of chronic ailment |
|
| Interventions | Vaccine: CVD 103‐HgR live attenuated vaccine containing:
Placebo: 5 x 109 heat‐killed E. coli K12 strain (C600) All participants were randomized to receive one dose |
|
| Outcomes |
Included in review:
Not included in the review:
|
|
| Notes | Location: Chile Setting: Source of funding: None stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: Not described. |
| Allocation concealment (selection bias) | Low risk | Quote: 'The codes were kept in confidential archives at the Swiss Institute of Sera and Vaccines...until the end of the serological analysis'. |
| Blinding (performance bias and detection bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Blinding (performance bias and detection bias) Safety outcomes | Low risk | Quote: 'All observations were made using the double‐blind methodology'. |
| Incomplete outcome data (attrition bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Incomplete outcome data (attrition bias) Safety outcomes | Low risk | Comment: All participants are included in the adverse event data. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective outcome reporting |
| Other bias | Low risk | No other bias detected |
Lagos 1995.
| Study characteristics | ||
| Methods | Design: Randomized controlled trial (individually randomized) Duration: Study dates not given; follow‐up 8 days |
|
| Participants | Sample size: 349 enrolled Inclusion criteria: Age 5 to 9 years, from public schools in a low‐socioeconomic‐level community Exclusion criteria: Fever, antibiotic therapy, or chronic disease |
|
| Interventions | Vaccine: CVD 103‐HgR live attenuated vaccine containing:
Placebo: Heat‐killed E. coli K12 strain All participants were randomized to receive one dose |
|
| Outcomes |
Included in review:
Not included in the review:
|
|
| Notes | Location: Santiago, Chile Setting: Source of funding: The World Health Organization and NIAID |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: Described as 'randomized', no further details given. |
| Allocation concealment (selection bias) | Low risk | Quote: 'Lyophilized vaccine and placebo were contained in randomized coded aluminum foil sachets. The code remained unbroken until the clinical study, including serology, was completed'. |
| Blinding (performance bias and detection bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Blinding (performance bias and detection bias) Safety outcomes | Low risk | Quote: 'Double‐blind clinical follow‐up to detect adverse reactions was maintained daily for 8 days after the single oral immunization'. |
| Incomplete outcome data (attrition bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Incomplete outcome data (attrition bias) Safety outcomes | Low risk | Comment: No losses recorded during adverse event monitoring |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No evidence of other bias |
Lagos 1999.
| Study characteristics | ||
| Methods | Design: Randomized controlled trial (individually randomized) Trial dates and duration: June 1995 to Nov 1997; follow‐up 28 days |
|
| Participants | Sample size: 312 enrolled Inclusion criteria: Age 3 to 17 months, normal medical history, parental consent Exclusion criteria: Signs and symptoms of acute illness, antibiotic therapy or diarrhoea in previous 2 days |
|
| Interventions | Vaccine: CVD 103‐HgR live attenuated vaccine containing:
Placebo: 5 x 108 CFU of heat‐killed E. coli K12 strain Participants were initially randomized to receive vaccine or placebo. After 14 days all participants in both groups received a dose of vaccine |
|
| Outcomes |
Included in review:
Not included in the review:
|
|
| Notes | Location: Santiago, Chile Setting: Well‐baby clinics at a semi‐rural ambulatory health centre. Source of funding: The World Health Organization and NIAID |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: 'For the first dose one‐half were randomly allocated in double blind fashion to receive a dose of vaccine' |
| Allocation concealment (selection bias) | Low risk | Quote: 'The sachets of test product were packed as individual treatments consisting of two sachets labeled with the same number followed by the letter A or B, indicating the appropriate sachet for the first and second dose of the immunization regimen', 'Each subject received the treatment number matching his/her study identification number'. |
| Blinding (performance bias and detection bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Blinding (performance bias and detection bias) Safety outcomes | Low risk | Comment: Described as 'double‐blind'. |
| Incomplete outcome data (attrition bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Incomplete outcome data (attrition bias) Safety outcomes | Unclear risk | Comment: All randomised participants completed the follow‐up for adverse events following the first dose |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No evidence of other bias |
Mahalanabis 2008.
| Study characteristics | ||
| Methods | Design: Randomized controlled trial (individually randomized) Trial dates and duration: Enrollment from Aug to Oct 2005; follow‐up for 28 days |
|
| Participants | Sample size: 201 participants stratified into adults and children Inclusion criteria: Age 18 to 40 years for adult study, 1 to 17 years for children, healthy male and non‐pregnant females, written informed consent Exclusion criteria: Abdominal pain, vomiting, loss of appetite, generalized ill‐feeling or nausea during the preceding 24 hours, diarrhoea or history of anti‐diarrhoeal or antibiotic use during the past week, history of diarrhoea and abdominal pain lasting for more than 2 weeks during the past 6 months |
|
| Interventions | Vaccine: Bivalent killed whole‐cell vaccine (BivWC: Shanchol®, Shantha Biotechnics) Placebo: Heat‐killed E. coli K12 strain All subjects were randomized to receive 2 doses, at an interval of 14 days. All doses were administered via an oral syringe and offered water. |
|
| Outcomes | No evidence of other bias | |
| Notes | Location: Kolkata, India Setting: Clinical trial ward of the Infectious Diseases Hospital Source of funding: The Bill and Melinda Gates Foundation through the Diseases of Most Impoverished Program administered by the International Vaccine Institute, and the Swedish International Development Cooperation Agency |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: 'Separate randomization lists for adults and children were prepared by a statistician in IVI who was otherwise not involved in the study. Randomization numbers were generated in blocks of 8 using the program Visual Fortran 5.0. (Digital, USA)'. |
| Allocation concealment (selection bias) | Low risk | Quote: 'Study agents were coded using 8 letters (4 for vaccine and 4 for placebo) in the adult trial and 8 different letters in the pediatric trial. Only the code letters on the vials identified the study agents as vaccine or placebo. The codes were revealed to the researchers once recruitment, data collection, and laboratory analyses were complete' |
| Blinding (performance bias and detection bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Blinding (performance bias and detection bias) Safety outcomes | Low risk | Quote: 'All study personnel and participants were blinded to treatment assignment during the duration of the study'. |
| Incomplete outcome data (attrition bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Incomplete outcome data (attrition bias) Safety outcomes | Low risk | Comment: Three randomized participants (2.5%) were excluded from the adverse event follow‐up, one who declined the first dose and two who received the wrong allocation for the second dose |
| Selective reporting (reporting bias) | Low risk | No evidence of selective outcome reporting |
| Other bias | Low risk | No evidence of other bias |
Migasena 1989a.
| Study characteristics | ||
| Methods | Design: A randomized controlled study (individually randomized) Duration: Datesnot given; follow‐up 5 days |
|
| Participants | Sample size: 24 enrolled Inclusion criteria: Healthy adults age 20 to 30 years, informed consent Exclusion criteria: None stated |
|
| Interventions | Vaccine: CVD 103‐HgR live attenuated vaccine containing:
Placebo: 5 x 108 heat‐killed E. coli K12 strain (C600) On day 5 all participants began a 5‐day course of tetracycline. |
|
| Outcomes |
Included in review:
Not included in the review:
|
|
| Notes | Location: Thailand Setting: Vaccine Trial Centre in the Faculty of Tropical Medicine. Source of funding: |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: Described as 'randomized', no further details given. |
| Allocation concealment (selection bias) | Low risk | Quote: 'The study was carried out in double‐blind fashion without the volunteers, the nursing staff, or the clinical investigators knowing the identity of the contents of the packets. A four‐letter code for the packets was employed as an extra precaution to maintain double blindness'. |
| Blinding (performance bias and detection bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Blinding (performance bias and detection bias) Safety outcomes | Low risk | See above |
| Incomplete outcome data (attrition bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Incomplete outcome data (attrition bias) Safety outcomes | Low risk | Comment: No losses are reported |
| Selective reporting (reporting bias) | Low risk | No evidence of selective outcome reporting |
| Other bias | Low risk | No other sources of bias identified |
Perry 1998.
| Study characteristics | ||
| Methods | Design: Randomized controlled cross‐over trial (individually randomized) Trial dates and duration: Dates not stated, cross‐over after 12 days. |
|
| Participants | Number of participants: 76 Inclusion criteria: Clinically healthy commercial sex workers and students aged 18 to 50 years. Half were HIV‐positive and half were age and sex matched HIV‐negative. Exclusion criteria: Pregnancy; clinical symptoms of AIDS; previous cholera vaccination; reported having previously had cholera; taken antibiotics within the previous 4 days; current diarrhoea or other acute illness |
|
| Interventions | vaccine: CVD 103‐HgR live attenuated vaccine containing:
Placebo: Lactate and aspartame only (these are also constituents of the vaccine) On day 12 those who initially received the placebo now received the vaccine, and vice versa. |
|
| Outcomes |
Included in the review:
Not included in the review:
|
|
| Notes | Location: Mali Setting: Not clear Source of funding:WHO Global Programme on Vaccines, National Institute of Allergy and Infectious Diseases, Centre for Vaccine Development, University of Maryland School of Medicine |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: Described as 'randomized', no further details given |
| Allocation concealment (selection bias) | Unclear risk | Comment: Not described |
| Blinding (performance bias and detection bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Blinding (performance bias and detection bias) Safety outcomes | Low risk | Quote: 'identically appearing placebo packets' |
| Incomplete outcome data (attrition bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Incomplete outcome data (attrition bias) Safety outcomes | Low risk | Comment: Four (6%) participants were lost to follow‐up during the study |
| Selective reporting (reporting bias) | Low risk | No evidence of selective outcome reporting |
| Other bias | Low risk | No other sources of bias identified |
Qadri 2005.
| Study characteristics | ||
| Methods | Design: Randomized controlled trial (individually randomized) Trial dates and duration: Dates not stated, follow‐up 21 days |
|
| Participants | Number of participants: 70 Inclusion criteria: Age 18 to 45 years, healthy, willing to participate, informed consent Exclusion criteria: Any chronic disease or recent illness, immunosuppressive conditions during the past 6 months, pregnancy, diarrhoeal illness in the last 6 weeks, febrile illness in the last week or antibiotics in the last 2 weeks, history of any enteric vaccine given in the last month, stool samples positive for any enteric pathogen, food handlers and those cooking for or looking after infants and young children |
|
| Interventions | Vaccine: Peru 15 ‐ a live attenuated strain of V. cholerae 01 El Tor Inaba (AVANT Immunotherapeutics Inc, US) containing:
Placebo: Buffer only All participants were given doxycycline for four days on day 6 to clear the vaccine strain. |
|
| Outcomes |
Included in the review:
Not included in the review:
|
|
| Notes | Location: Dhaka, Bangladesh Setting: Participants recruited from an urban slum, close to inpatient and outpatient facilities of ICCDR,B Source of funding: Diseases of the Most Impoverished Program, Bill and Melinda Gates Foundation, International Vaccine Institute |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: 'Randomization was performed by the International Vaccine Institute, South Korea'. |
| Allocation concealment (selection bias) | Unclear risk | Comment: None described. |
| Blinding (performance bias and detection bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Blinding (performance bias and detection bias) Safety outcomes | Unclear risk | Comment: Described as 'double‐blind'. No further details given. |
| Incomplete outcome data (attrition bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Incomplete outcome data (attrition bias) Safety outcomes | Low risk | Comment: No losses to follow‐up during the 4 days of adverse event reporting |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting. |
| Other bias | Low risk | No other bias identified |
Qadri 2007.
| Study characteristics | ||
| Methods | Trial design: Randomized controlled trial (individually randomized) Trial dates and duration: Dates not stated, follow‐up 21 days |
|
| Participants | Number of participants: 240 Inclusion criteria: age 9 months to 5 years, healthy, parental consent Exclusion criteria: Any chronic disease; any recent illness; any illness or treatment causing immunosuppression in the last 9 months; diarrhoeal illness in the last two weeks; febrile illness in the last week; any enteric vaccine given in the last month; stool samples positive for any enteric pathogen |
|
| Interventions | Vaccine 1: Full dose Peru 15 ‐ a live attenuated strain of V. cholerae 01 El Tor Inaba (AVANT Immunotherapeutics Inc, US)
Vaccine 2: Reduced dose Peru 15 ‐ a live attenuated strain of V. cholerae 01 El Tor Inaba (AVANT Immunotherapeutics Inc, US)
Placebo: Buffer only All participants were given erythromycin for four days on day 6 to clear the vaccine strain. |
|
| Outcomes |
Included in the review:
Not included in the review:
|
|
| Notes | Location: Dhaka, Bangladesh Setting: Participants recruited from an urban slum, close to inpatient and outpatient facilities of ICCDR,B Source of funding: Bill and Melinda Gates Foundation |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: 'Randomization was carried out by the International Vaccine Institute and sent to the vaccine formulation team.' |
| Allocation concealment (selection bias) | Low risk | Quote: 'The vaccine formulation team prepared and blinded the vaccine and the placebo according to the randomization list'. |
| Blinding (performance bias and detection bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Blinding (performance bias and detection bias) Safety outcomes | Low risk | Quote: 'The results were analyzed sequentially in the order in which they had been completed and unblinded.' |
| Incomplete outcome data (attrition bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Incomplete outcome data (attrition bias) Safety outcomes | Low risk | Comment: Follow‐up for adverse events was 100%. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective outcome reporting |
| Other bias | Low risk | No other bias identified |
Richie 2000 Indonesia.
| Study characteristics | ||
| Methods | Design: Randomized controlled trial (individually randomized) Trial dates and duration: July 1993 to Dec 1997, 4 years Surveillance: Passive surveillance conducted through four North Jakarta hospitals distributed across the study area. |
|
| Participants | Sample size: 67,508 Inclusion criteria: Persons aged 2 to 41 years living in the study area. Exclusion criteria: Pregnancy, plans to move out of the study area, diagnosis of cancer |
|
| Interventions | Vaccine: CVD 103‐HgR live attenuated vaccine containing:
Placebo: 5 x 108 heat‐killed E. coli K12 strain (C600) |
|
| Outcomes |
Included in the review:
Not included in the review:
|
|
| Notes | Location: 65 communities in North Jakarta, Indonesia Setting: Poor communities with poor sanitation and relative high cholera incidences Source of funding: World Health Organization, National Institute of Allergy and Infectious Diseases, the Swiss Serum and Vaccine Institute, Berne. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A randomized trial" Comment: Method of randomization unclear |
| Allocation concealment (selection bias) | Low risk | Quote: "Vaccine..and placebo ..were contained in identical, numbered packets" |
| Blinding (performance bias and detection bias) Efficacy outcomes | Low risk | Quote: "Surveillance data collected included..vaccine number. ..Patients with diarrhoea who did not state that they were participants in the study were also included in the surveillance." |
| Blinding (performance bias and detection bias) Safety outcomes | Low risk | Quote: "a double‐blind nested study of adverse events was conducted.." |
| Incomplete outcome data (attrition bias) Efficacy outcomes | Unclear risk | Comment: No mention of the numbers of people who moved out of the area and were therefore lost of follow up. |
| Incomplete outcome data (attrition bias) Safety outcomes | Low risk | Comment: No loss to follow up |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No evidence of other bias |
Sack 1997.
| Study characteristics | ||
| Methods | Design: Randomized controlled trial (individually randomized) Trial dates and duration: Dates not given, 21 days follow‐up |
|
| Participants | Number of participants: 50 in outpatient study (a smaller inpatient study is also reported but included no outcomes relevant to this review) Inclusion criteria: Age 18 to 50 years, healthy, willing to participate, informed consent Exclusion criteria: chronic illness, immunosuppressive condition, abnormal stool pattern, significant abnormality in screening laboratory hematology and chemistry tests, HIV +ve, hepatitis B surface antigen +ve, pregnancy, travel to a cholera endemic area within 5 years, receipt of cholera vaccine, history of cholera infection or vaccination, previous participation in a cholera or ETEC vaccine trial, use of antibiotics within 7 days of vaccination, food handlers or close contact with children under age 5 |
|
| Interventions | Vaccine 1: Full dose Peru 15 ‐ a live attenuated strain of V. cholerae 01 El Tor Inaba
Vaccine 2: Reduced dose Peru 15 ‐ a live attenuated strain of V. cholerae 01 El Tor Inaba (AVANT Immunotherapeutics Inc, US)
Placebo: Buffer only |
|
| Outcomes |
Included in the review:
Not included in the review:
|
|
| Notes | Location: USA Setting: Students or employee volunteers at John Hopkins University and Hospital Source of funding: National Institute Health, Virus Research Institute |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: Described as 'Randomized'. No further details given. |
| Allocation concealment (selection bias) | Unclear risk | Comment: None described |
| Blinding (performance bias and detection bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Blinding (performance bias and detection bias) Safety outcomes | Low risk | Quote: 'Volunteers were randomized to receive either a 109 or 108 CFU or a placebo in a double‐masked manner', 'To protect the masked code, some volunteers were assigned to 1 or 0.1 mL of placebo'. |
| Incomplete outcome data (attrition bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Incomplete outcome data (attrition bias) Safety outcomes | Low risk | Comment: No losses are described during the adverse event monitoring. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No evidence of other bias |
Sanchez 1993a.
| Study characteristics | ||
| Methods | Design:A randomized 2 x 2 factorial controlled trial (individually randomized) Duration: Enrolled during October 1991; follow‐up 28 days |
|
| Participants | Sample size: 186 enrolled and randomized to four groups* Inclusion criteria: Age 18 to 44 years Exclusion criteria: Pregnancy or planned pregnancy, diarrhoea or fever within the past 5 days, recent use of antimotility or antibacterial agent, foodhandler, chronic gastrointestinal disorder. |
|
| Interventions | Vaccine: Killed whole‐cell vaccine plus recombinant cholera toxin subunit (WC‐rBS; Dukoral®, SBL, Sweden) Placebo: Buffer alone All participants were randomized to receive 2 doses, at 11 to 16 days apart |
|
| Outcomes |
Included in review:
Not included in the review:
|
|
| Notes | Location:USA Setting: Military personnel Source of funding: None stated * A further single arm study involving 74 participants is reported in this paper but excluded from this review |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: Described as 'randomized', no further details given. |
| Allocation concealment (selection bias) | Unclear risk | Comment: None described. |
| Blinding (performance bias and detection bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Blinding (performance bias and detection bias) Safety outcomes | Unclear risk | Comment: None described. |
| Incomplete outcome data (attrition bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Incomplete outcome data (attrition bias) Safety outcomes | Low risk | Comment: 6 participants did not receive the second dose as they were unavailable |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No evidence of other bias |
Sanchez 1994 Peru.
| Study characteristics | ||
| Methods | Design: Randomized controlled trial (individual block randomization in groups of 10) Duration: Enrolled January to March 1994, follow‐up to June 1994 Surveillance: Passive surveillance through clinics within the military training centres where the study was conducted |
|
| Participants | Sample size: 1563 enrolled, 1426 received 2 doses of vaccine or placebo Inclusion criteria: 17‐65 years volunteers, available for three months Exclusion criteria: Previous cholera vaccination |
|
| Interventions | Vaccine: Killed whole‐cell vaccine plus recombinant cholera toxin subunit (WC‐rBS; Dukoral®, SBL, Sweden) Placebo: Heat ‐inactivated E. coli K12 strain Vaccine and placebo were given with freshly prepared antacid solution. Two doses were given, 7 to 14 days apart. |
|
| Outcomes |
Included in the review:
Not included in the review:
|
|
| Notes | Location: Lima, Peru Setting: Military training centres Source of funding: Not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was done in blocks of 10 to ensure equal study groups" Comment: Unclear description but probably done |
| Allocation concealment (selection bias) | Low risk | Quote: "Each bottle was identified with a unique code number; vaccine and placebo bottles were pre‐coded" |
| Blinding (performance bias and detection bias) Efficacy outcomes | Low risk | Quote: "The placebo....in a concentration identical in turbidity and appearance to the vaccine preparation" Plus see above |
| Blinding (performance bias and detection bias) Safety outcomes | Unclear risk | Not applicable as safety data is not reported |
| Incomplete outcome data (attrition bias) Efficacy outcomes | High risk | Comment: Subjects lost to follow‐up after the second dose were assumed to contribute half the period to the denominator analysis. Mentioned that losses to follow‐up were similar in both groups. Cases of cholera which occurred in participants between study doses were excluded from the primary analysis. |
| Incomplete outcome data (attrition bias) Safety outcomes | Unclear risk | Not applicable as safety data is not reported |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No evidence of other bias |
Sanchez 1995 Peru.
| Study characteristics | ||
| Methods | Design: Randomized controlled trial (individually randomized) Trial dates and duration: February 1992, 4 weeks Surveillance: Passive surveillance for diarrhoea was performed at the single military medical clinic, where all cases were evaluated. |
|
| Participants | Sample size: 346 enrolled and received first dose, 307 received two full doses Inclusion criteria: Male Hispanics aged 17‐23 years, informed consent Exclusion criteria: Major illness at the time of vaccination, previous cholera vaccine |
|
| Interventions | Vaccine: Killed whole‐cell vaccine plus recombinant cholera toxin subunit (WC‐rBS; Dukoral®, SBL, Sweden) Placebo: suspension of heat‐inactivated E. coli K12 strain Vaccines were given with a buffer solution. Two doses were given two weeks apart. |
|
| Outcomes |
Included in the review:
Not included in the review:
|
|
| Notes | Location: Ancon, Peru Setting: Military training centre Source of funding: US Army and Navy medical departments(?) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: 'randomly allocated' Comment: Method of randomization not adequately described but probably done |
| Allocation concealment (selection bias) | Low risk | Quote: "Each bottle was identified with one of 2 letters; vaccine and placebo preparations were pre‐coded" |
| Blinding (performance bias and detection bias) Efficacy outcomes | Low risk | Quote: 'suspension of heat‐inactivated E coli K12 strain, with same appearance as vaccine'. |
| Blinding (performance bias and detection bias) Safety outcomes | Low risk | See above |
| Incomplete outcome data (attrition bias) Efficacy outcomes | Low risk | Comment: All participants remained in the study area and were included in the analysis. Identification of cases through passive surveillance, with clinical data collected from all participants with diarrhoea. |
| Incomplete outcome data (attrition bias) Safety outcomes | Low risk | Comment: No loss to follow‐up |
| Selective reporting (reporting bias) | High risk | Comment: The report states adverse event data were collected for three days after each dose but only symptoms within 24 hours are presented |
| Other bias | Low risk | No evidence of other bias |
Simanjuntak 1993.
| Study characteristics | ||
| Methods | Trial design: Randomized controlled trial ‐ initially randomized in pairs one to each treatment arm, later changed to individual randomization. Trial dates and duration and dates: 1991 to 1992 |
|
| Participants | Number of participants: 303 Inclusion criteria: Children aged 24 to 59 months Exclusion criteria: Chronic health problem, receiving antibiotic therapy, acute illness on the scheduled day of vaccination |
|
| Interventions | Vaccine: CVD 103‐HgR live attenuated vaccine containing:
Placebo:
Both were given with aspartame sweetener and a buffer. |
|
| Outcomes |
Included in the review:
Not included in the review:
|
|
| Notes | Location: North Jakarta, Indonesia Setting: Villages Source of funding:Consultative group on vaccine development of the national vaccine programme, USA, National Institute of Allergy and Infectious Diseases, US Naval Medical Research and Command |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: Described as randomized. Codes generated by the manufacturer. |
| Allocation concealment (selection bias) | Low risk | Quote: 'Coded preparations looked identical and were only identified by the codes ‘N’ or ‘O’' |
| Blinding (performance bias and detection bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Blinding (performance bias and detection bias) Safety outcomes | Low risk | Quote: 'The clinical follow‐up as well as the administration of the vaccine was double‐blind with neither the clinical staff, the patient or their parents knowing the identity of the preparation'. |
| Incomplete outcome data (attrition bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Incomplete outcome data (attrition bias) Safety outcomes | Low risk | Comment: No losses during adverse event follow‐up are noted. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No evidence of other bias |
Su‐Arehawaratana 1992a.
| Study characteristics | ||
| Methods | Trial design: Randomized controlled trial (individually randomized) Trial dates and duration: February 1988 |
|
| Participants | Number of participants: 206 (in study 1), Inclusion criteria: Thai soldiers aged 18 to 26, who volunteered for the study Exclusion criteria: Previous parenteral inactivated whole cell vaccine |
|
| Interventions | Vaccine: CVD 103‐HgR live attenuated vaccine containing:
Placebo: 5 x 108 CFU inactivated E. coli K12 |
|
| Outcomes |
Included in the review:
Not included in the review:
|
|
| Notes | Location: Thailand Setting: Field study using volunteers Sources of funding: National Institutes of Health, Swiss Serum and Vaccine Institute, US Agency for International Development |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: Described as 'randomised', no further details |
| Allocation concealment (selection bias) | Unclear risk | Comment: None described |
| Blinding (performance bias and detection bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Blinding (performance bias and detection bias) Safety outcomes | Unclear risk | Comment: None described |
| Incomplete outcome data (attrition bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Incomplete outcome data (attrition bias) Safety outcomes | Low risk | Comment: No losses are reported |
| Selective reporting (reporting bias) | Low risk | No evidence of selective outcome reporting |
| Other bias | Low risk | No other bias identified |
Su‐Arehawaratana 1992b.
| Study characteristics | ||
| Methods | Trial design: Randomized controlled crossover trial. Trial dates and duration: June 1991 |
|
| Participants | Number of participants: 120 Inclusion criteria: Volunteers and Thai soldiers aged 18 to 26 Exclusion criteria: None stated |
|
| Interventions | Vaccine: CVD 103‐HgR live attenuated vaccine containing:
Placebo: 5 x 108 CFU inactivated E. coli K12 The trial had 6 arms with each arm crossing over to receive the alternative dose or placebo on day 7 All doses were given with buffer and aspartame sweetener |
|
| Outcomes |
Included in the review:
Not included in the review:
|
|
| Notes | Location: Thailand Setting: Field study using volunteers Sources of funding: National Institutes of Health, Swiss Serum and Vaccine Institute, US Agency for International Development |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: Described as 'randomized', no further details |
| Allocation concealment (selection bias) | Unclear risk | Comment: None described |
| Blinding (performance bias and detection bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Blinding (performance bias and detection bias) Safety outcomes | Unclear risk | Comment: Described as 'double blind', no further details. |
| Incomplete outcome data (attrition bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Incomplete outcome data (attrition bias) Safety outcomes | Low risk | Comment: No losses are reported |
| Selective reporting (reporting bias) | Low risk | No evidence of selective outcome reporting |
| Other bias | Low risk | No other bias identified |
Suharyono 1992a.
| Study characteristics | ||
| Methods | Trial design: Randomized controlled trial (4 arms) Trial dates and duration: February to March 1990 |
|
| Participants | Number of participants: 274 Inclusion criteria: Children aged 5 to 9 years. Witten parental consent. Only one child per family was eligible to take part. Exclusion criteria: Having a chronic health disorder; receiving antibiotic therapy; acute illness on the scheduled day of vaccination |
|
| Interventions | Vaccine: CVD 103‐HgR live attenuated vaccine containing:
Placebo: 5 x 108 CFU inactivated E. coli K12 strain |
|
| Outcomes |
Included in the review:
Not included in the review:
|
|
| Notes | Location: North Jakarta, Indonesia Setting: Small rural village, vaccinated at village health office Source of funding: Consultative group on vaccine development of the national vaccine programme, USA, National Institute of Allergy and Infectious Diseases, Naval Medical Research unit 2, Jakarta, United States Agency for International Development |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: ‘Randomly allocated to one of the four letter‐coded groups according to a computer‐generated randomization sequence’ |
| Allocation concealment (selection bias) | Low risk | Quote: 'Vaccine and placebo packets indistinguishable and identified only by a colour‐coded letter'. |
| Blinding (performance bias and detection bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Blinding (performance bias and detection bias) Safety outcomes | Low risk | Quote: 'The clinical follow‐up as well as the administration of the vaccine was double‐blind with neither the clinical staff, the patient or their parents knowing the identity of the preparation'. |
| Incomplete outcome data (attrition bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Incomplete outcome data (attrition bias) Safety outcomes | Low risk | Comment: No losses reported. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No evidence of other bias |
Suharyono 1992b.
| Study characteristics | ||
| Methods | Trial design: Randomized controlled trial (individually randomized) Trial dates and duration: Sept to Oct 1990 |
|
| Participants | Number of participants: 140 Inclusion criteria: As for Suharyono 1992a Exclusion criteria: As for Suharyono 1992a |
|
| Interventions | Vaccine: CVD 103‐HgR live attenuated vaccine containing:
Placebo: 5 x 108 CFU inactivated E. coli K12 strain |
|
| Outcomes | As for Suharyono 1992a | |
| Notes | Location: As for Suharyono 1992a Setting: Source of funding: As for Suharyono 1992a |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: 'the child was allocated to receive one of the nine treatment groups, according to a randomised sequence' Comment: Study A in the same paper used a computer to generate the sequence. |
| Allocation concealment (selection bias) | Low risk | Comment: Only clearly described for study A but probably done. |
| Blinding (performance bias and detection bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Blinding (performance bias and detection bias) Safety outcomes | Low risk | Quote: 'The clinical follow‐up as well as the administration of the vaccine was double‐blind with neither the clinical staff, the patient or their parents knowing the identity of the preparation'. |
| Incomplete outcome data (attrition bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Incomplete outcome data (attrition bias) Safety outcomes | Low risk | Comment: No losses to follow up are reported |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No evidence of other bias |
Sur 2009 India.
| Study characteristics | ||
| Methods | Design: Randomized controlled trial (cluster randomization) Dates and duration: Vaccination July to September 2006; An interim analysis after 2 years of follow‐up Surveillance: Passive surveillance through nine diarrhoea clinics established in the study area, two hospitals serving the study area, and encouragement to private medical practitioners to refer to the treatment centres. Method of adjustment for clustering: Robust sandwich variance estimates |
|
| Participants | Sample size: 3933 clusters (107,774 individuals) were randomized. 69,328 individuals received at least one dose of vaccine or placebo. The primary analysis includes 66,900 participants who received 2 doses of the vaccine. Inclusion criteria: Age > 1 year, written informed consent Exclusion criteria: Pregnancy |
|
| Interventions | Vaccine: Bivalent killed whole‐cell vaccine (BivWC: Shanchol®, Shantha Biotechnics) Placebo: Heat killed E. coli K12 strain All subjects were randomized to receive 2 doses, at a minimum interval of 14 days. All doses were administered via an oral syringe. |
|
| Outcomes |
Included in review:
Not included in the review: |
|
| Notes | Location: Kolkata, India Setting: Surveillance study area, served by 9 study clinics, private practitioners and 2 hospitals. Source of funding: Bill and Melinda Gates Foundation; Swedish International Development Cooperation Agency; governments of South Korea, Sweden and Kuwait |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: 'An external statistician, who was masked to the identities of the codes, used an SAS version 9.1 computer algorithm to randomly assign dwellings to the four codes in a 1:1:1:1 ratio within each of the strata'. |
| Allocation concealment (selection bias) | Low risk | Quote: 'The vials were labelled with one of four letters, two each for vaccine and placebo. Project staff and study participants were unaware of the identities of the codes'. |
| Blinding (performance bias and detection bias) Efficacy outcomes | Low risk | Quote: 'The vaccine and placebo were identical in appearance' |
| Blinding (performance bias and detection bias) Safety outcomes | Low risk | See above |
| Incomplete outcome data (attrition bias) Efficacy outcomes | Low risk | Comment: Attrition between the first and second doses of vaccine were low: 3.6% vaccine group vs 3.4% placebo group. |
| Incomplete outcome data (attrition bias) Safety outcomes | High risk | Comment: Safety data was collected passively with participants requested to present to medical services. Consequently the incidence of adverse event reporting is very low and likely to be an underestimate. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No evidence of other bias |
Tacket 1999.
| Study characteristics | ||
| Methods | Design: Randomized controlled trial (individually randomized) with challenge study Trial dates and duration: Dates not stated; challenge study was undertaken 3 months after vaccination |
|
| Participants | Sample size: 85 (51 included in challenge study) Inclusion criteria: Age 18 to 40, healthy, informed consent. Exclusion criteria: clinically significant abnormalities on urinalysis, complete blood count, serum hepatic transaminases, glucose, creatinine, blood urea nitrogen, electrolytes, or electrocardiogram, travel to a cholera endemic area in the previous 5 years, abnormal stool pattern or regular use of laxatives, failure to pass a psychological examination, allergy to tetracycline or ciprofloxacin, history of cholera or enterotoxigenic E. coli challenge, history of recent antibiotic use, pregnancy or nursing, positive serology for HIV, hepatitis B antigen, or hepatitis B, stool culture positive for an enteric pathogen |
|
| Interventions | Vaccine: CVD 103‐HgR live attenuated vaccine containing:
Placebo: heat‐inactivated E. coli K12 plus buffer Challenge: 105 organisms of V. cholerae O1 El Tor Inaba (N16961) |
|
| Outcomes |
Included in review:
Not included in the review:
|
|
| Notes | Location: Baltimore and Cincinatti, USA Setting: Hospital Source of funding: National Institute of Allergy and Infectious Diseases, and the Swiss Serum and Vaccine Institute |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: 'For those of blood group O and non‐O within each clinical center, subjects were randomized in blocks of four (two to receive vaccine and two to receive placebo) by using SAS PROC PLAN'. |
| Allocation concealment (selection bias) | Low risk | Quote: 'The code was held by the study sponsor until the database was complete and unalterable'. |
| Blinding (performance bias and detection bias) Efficacy outcomes | Low risk | Quote: 'When suspended in the buffer solution, the placebo was identical in appearance to the vaccine suspension'. |
| Blinding (performance bias and detection bias) Safety outcomes | Low risk | Quote: 'When suspended in the buffer solution, the placebo was identical in appearance to the vaccine suspension'. |
| Incomplete outcome data (attrition bias) Efficacy outcomes | High risk | Comment: The artificial challenge study included only 60% of those given the vaccine. |
| Incomplete outcome data (attrition bias) Safety outcomes | Low risk | Comment: No participants were lost to follow‐up or excluded during the initial 3 days. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective outcome reporting |
| Other bias | Low risk | No other bias identified. |
Taylor 1999a.
| Study characteristics | ||
| Methods | Design: Randomized controlled trial (individually randomized) Duration: Enrollment from Jan to Feb 1995; follow‐up for 28 days |
|
| Participants | Sample size: 216 enrolled Inclusion criteria: Age 2 to 64 years and residing in the study area, informed consent Exclusion criteria: None stated. |
|
| Interventions | Vaccine: Killed whole‐cell vaccine plus recombinant cholera toxin subunit (WC‐rBS; Dukoral®, SBL, Sweden) Placebo: Heat killed E. coli K12 strain All participants were randomized to receive 2 doses, at a minimum interval of 14 days. All doses were administered via pumps designed to deliver the correct dose |
|
| Outcomes |
Included in review:
Not included in the review:
|
|
| Notes | Location: Flores de Villa, southern Lima Setting: Source of funding: The U.S. Army Medical Material and Development Command. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: 'Vaccination teams were assigned to a section of households using pre‐randomized forms to enter adults and children in the study'. |
| Allocation concealment (selection bias) | Low risk | Quote: 'Each bottle was identified with a unique number; vaccine and placebo preparations were pre‐coded'. |
| Blinding (performance bias and detection bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Blinding (performance bias and detection bias) Safety outcomes | Low risk | Quote: 'The participants and the persons who assessed side effects were blinded to the vaccine code'. 'The placebo consisted of a suspension of heat‐inactivated E. coli K12 strain (SBL Vaccin AB) in a concentration that matched the turbidity and appearance of the vaccine preparation'. |
| Incomplete outcome data (attrition bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Incomplete outcome data (attrition bias) Safety outcomes | Low risk | Comment: 12 participants were lost to follow‐up between doses. Reasons for drop‐out were not given but follow‐up in the 3 days after each dose was complete. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No evidence of any other bias |
Taylor 2000 Peru.
| Study characteristics | ||
| Methods | Design: Randomized controlled trial (individually randomized) Duration: 1993 to 1995 Surveillance: Active surveillance in the community through twice weekly visits to each household |
|
| Participants | Sample size: 21,924 received the first dose, 17,799 received the second dose, and 14,997 received the booster dose. Inclusion criteria: Aged 2 to 65 years old and residing in the vaccine trial area. Exclusion criteria: None stated. |
|
| Interventions | Vaccine: Killed whole‐cell vaccine plus recombinant cholera toxin subunit (WC‐rBS; Dukoral®, SBL, Sweden) Placebo: Heat‐inactivated E. coli K12 strain Vaccine or placebo were given as two doses two weeks apart, followed by a third dose 10 months later. |
|
| Outcomes |
Included in the review:
Not included in the review:
|
|
| Notes | Location: Pampas de San Juan de Miraflores, in the southern outskirts of Lima, Peru. Setting: 36 poor marginal neighbourhoods, with a nearby hospital, 4 health posts and 40 neighbourhood rehydration units. Source of funding: US Army Medical Materiel and Development Command, Fort Detrick, Maryland |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The trial area was divided into 4 quadrants (A to D), and every eligible person was randomly assigned a vaccine code of 1 or 9 to give a total of 8 possible codes" Comment: Sequence generation unclear but probably low risk |
| Allocation concealment (selection bias) | Low risk | Quote:"During the study, the vaccine codes were kept locked by.. who was not involved in the study; the codes were not known to any person conducting the trial" |
| Blinding (performance bias and detection bias) Efficacy outcomes | Low risk | Quote: "Suspension of heat‐inactivated Escherichia coli K12 strain in a concentration that matched the turbidity and appearance of the vaccine preparation." plus see above |
| Blinding (performance bias and detection bias) Safety outcomes | Low risk | See above |
| Incomplete outcome data (attrition bias) Efficacy outcomes | Low risk | Comment: Attrition between the first and second doses was high: 18.8% overall. As well as the per protocol analysis, the authors conducted an intention to treat analysis which did not significantly alter the result |
| Incomplete outcome data (attrition bias) Safety outcomes | High risk | Comment: Adverse events from the first dose were recorded only for those attending for a second dose. This method is likely to underestimate the true incidence of adverse events if those experiencing a significant event after the first dose are more likely to drop‐out. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No evidence of other bias |
Trach 1997 Viet Nam.
| Study characteristics | ||
| Methods | Design: Quasi‐randomized controlled trial (alternate allocation, clustered by household) Duration: Vaccination started December 1992, follow‐up to December 1993 Surveillance: Passive surveillance through community health centres, polyclinics and hospitals serving the study area Method of adjustment for clustering: Logistic regression models with generalised estimating equations |
|
| Participants | Sample size: 134,453 individuals, 22,653 households Inclusion criteria: Residents aged one year or older Exclusion criteria: None |
|
| Interventions | Vaccine: Variant killed whole cell vaccine (vWC; National Institute of Hygiene and Epidemiology, Vietnam) Control: No vaccine Two doses were given with a two week interval between them. |
|
| Outcomes |
Included in the review:
|
|
| Notes | Location: Hue, central Vietnam Setting: city community served by 19 health centres, four polyclinics and one regional hospital. Sources of funding: Ministry of Health Vietnam, Swedish Agency for Research Cooperation, World Health Organization, USA National Institute of Child Health and Human Development |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: 'Each household.. was given a serial number. Even‐numbered households were assigned the vaccine, and odd numbered households were assigned no vaccine'. Comment: Alternate allocation is unlikely to significantly bias a vaccine trial |
| Allocation concealment (selection bias) | Low risk | Comment: Alternate allocation, concealment not possible, but unlikely to introduce significant bias. |
| Blinding (performance bias and detection bias) Efficacy outcomes | High risk | Quote: 'open field trial' |
| Blinding (performance bias and detection bias) Safety outcomes | Unclear risk | Not applicable ‐ not included as an outcome |
| Incomplete outcome data (attrition bias) Efficacy outcomes | High risk | Comment: No mention of the participants who may have moved out of the area and therefore been lost to follow up. Cases identified through passive surveillance at the polyclinics and hospitals. |
| Incomplete outcome data (attrition bias) Safety outcomes | Unclear risk | Not applicable as safety data not reported |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No evidence of any other bias |
Trach 2002.
| Study characteristics | ||
| Methods | Design: A 3‐arm randomized controlled trial (individually randomized) Trial dates and duration: Dates not stated, follow‐up 28 days |
|
| Participants | Sample size: 71 in adult study, 70 in child study (from included study arms) Inclusion criteria: Adult study: Age 17 to 25 years, Hanoi residents. Child study: Age 1‐12 years, attending an elementary school or day care centre in Hanoi Exclusion criteria: Diarrhoea during the preceding week, chronic or recurrent abdominal pain or diarrhoea, pregnancy, steroids or other immunosuppressive medications, antibiotics, or known to have HIV or another immunosuppressive condition |
|
| Interventions | Vaccine 1: Killed whole‐cell vaccine plus recombinant cholera toxin subunit (WC‐rBS; Dukoral®, SBL, Sweden) Vaccine 2: A bivalent vaccine containing: 5 x 1010 formalin‐killed V. cholerae 01 Inaba, El Tor biotype cells (strain Phil 6973); 2.5 x 1010 heat‐killed V. cholerae O1 Ogawa, classical biotype cells (strain Cairo 50); 2.5 x 1010 formalin‐killed V. cholerae O1 Inaba, classical biotype cells (strain 569B); 2.5 x 1010 heat‐killed V. cholerae O1 Inaba, classical biotype cells (strain Cairo 48);and 5 x 1010 formalin‐killed V. cholerae O139 (strainAI4456): This arm was excluded as the included strains are different from both the vWC vaccine and the BivWC vaccines with efficacy data Placebo: heat‐killed E. coli K12 strain |
|
| Outcomes |
Included in review:
Not included in the review:
|
|
| Notes | Location: Hanoi, Vietnam Setting: Source of funding: Swedish Agency for Cooperation with Developing Countries; the National Institute of Child Health and Human Development, National Institutes ofHealth, USA; the World Health Organization; and the Diseases of the Most Impoverished Programme, funded by the Bill and Melinda Gates Foundation. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: 'Consenting eligible subjects in blocks of eight were randomly allocated' Comment: Description is unclear but probably done |
| Allocation concealment (selection bias) | Low risk | Quote: 'The vials with the agent for each group were labelled with one of two code letters'. 'The codes were kept secret from all persons involved in the study until freezing of the data set.' |
| Blinding (performance bias and detection bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy outcomes are not reported |
| Blinding (performance bias and detection bias) Safety outcomes | Low risk | Quote: 'The two vaccines and the placebo were packaged as liquid formulations in identical vials'. |
| Incomplete outcome data (attrition bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy outcomes are not reported |
| Incomplete outcome data (attrition bias) Safety outcomes | Low risk | Comment: Only three participants were lost to follow‐up between doses, although the reasons are not stated. |
| Selective reporting (reporting bias) | High risk | Comment: Nausea was not assessed in the children's study |
| Other bias | Low risk | No other source of bias identified |
Valera 2009.
| Study characteristics | ||
| Methods | Design: Randomized controlled trial (individually randomized) Duration and dates (field work): |
|
| Participants | Sample size: 36 Inclusion criteria: Age 18 to 40 years, volunteers working in the scientific community, healthy, informed consent. Exclusion criteria: Previous history of clinically significant diarrhoea or cholera vaccination, receiving medication at the time of recruitment. |
|
| Interventions | Vaccine: VC638 ‐ A live attenuated strain of V. cholerae O1 El Tor Ogawa (Final Institute, Havana)
Placebo: Buffer alone All participants received 300mg of doxycycline on day 5. |
|
| Outcomes |
Included in review:
Not included in the review:
|
|
| Notes | Location: Havana, Cuba Setting: Unit for Isolation of Biological Risks at Tropical Medicine Institute Source of funding: None stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: Described as 'randomized', no further details given. |
| Allocation concealment (selection bias) | Low risk | Quote: 'Vaccine and placebo vials were packaged and coded at random with identical appearance. The code remained unbroken until the end of the study' |
| Blinding (performance bias and detection bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Blinding (performance bias and detection bias) Safety outcomes | Low risk | Comment: See above |
| Incomplete outcome data (attrition bias) Efficacy outcomes | Unclear risk | Not applicable as efficacy not reported |
| Incomplete outcome data (attrition bias) Safety outcomes | Low risk | Comment: No losses during the adverse event monitoring stage |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | No evidence of any other bias |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Ahmed 2006 | Non‐cholera vaccine, no cholera outcomes (abstract) |
| Ahren 1993 | Non‐comparative study. |
| Albert 2003 | A non‐comparative study, all children received the same vaccine (abstract) |
| Ali 2005 | Relates to Clemens 1988 Bangladesh. No additional data relevant to this review. |
| Ali 2008 | Relates to Clemens 1988 Bangladesh. No additional data relevant to this review. |
| Anonymous 1968 | Injectable vaccine |
| Anonymous 1973a | Injectable vaccine |
| Anonymous 1973b | Injectable vaccine |
| Azurin 1967 | Injectable cholera vaccine |
| Azurin 1971 | Injectable cholera vaccine |
| Benenson 1968a | Injectable cholera vaccine |
| Benenson 1968b | Injectable cholera vaccine |
| Bergquist 1997 | Intranasal vaccination (abstract) |
| Black 1986 | Non‐randomized study |
| Black 1987 | Non‐randomized study |
| Burgasov 1976 | Injectable cholera vaccine |
| Bwanga 1984 | Not randomized |
| Cash 1974 | Non‐randomized study |
| Cavailler 2006 | Non‐randomized study |
| Chaicumpa 1998 | Non‐randomized, immunological outcomes only |
| Chongsa‐nguan 1988 | Safety data presented but no trials assess the efficacy of this type of vaccine (lipopolysaccharide) |
| Chongsa‐nguan 1991 | Compared two new vaccine candidates for which efficacy data is not currently available |
| Ciznar 1989 | Not a human study (abstract) |
| Clemens 1986 | Immunological outcomes only |
| Clemens 1988 | Relates to Clemens 1988 Bangladesh. No additional data relevant to this review. |
| Clemens 1989a | Relates to Clemens 1988 Bangladesh. No additional data relevant to this review. |
| Clemens 1989b | Relates to Clemens 1988 Bangladesh. No additional data relevant to this review. |
| Clemens 1990 | Relates to Clemens 1988 Bangladesh. No additional data relevant to this review. |
| Clemens 1991 | Relates to Clemens 1988 Bangladesh. No additional data relevant to this review. |
| Clemens 1992a | Refers to Clemens 1988, no new data relevant to this review |
| Clemens 1992b | Relates to Clemens 1988 Bangladesh. No additional data relevant to this review. |
| Clemens 1995 | Relates to Clemens 1988 Bangladesh. No additional data relevant to this review. |
| Cohen 1999 | No vaccine was given (abstract) |
| Cohen 2000 | Non‐cholera vaccine, no cholera outcomes |
| Cooper 2000 | Non‐comparative study, all participants received the same vaccine |
| Cooper 2001 | Non‐comparative study, all participants received the same vaccine |
| Coster 1995 | The paper contains two very small studies. Study 1 is excluded as it has no placebo group. Study 2 is excluded as it was not randomized. |
| Cryz 1992 | No control group. |
| Cryz 1995 | No efficacy data for this vaccine (CVD 103‐HgR‐Ty21a) |
| Das 1967 | Injectable cholera vaccine |
| Dearlove 1992 | Non‐cholera vaccine (abstract) |
| Durham 1998 | Relates to Clemens 1988 Bangladesh. No additional data relevant to this review. |
| Emch 2006 | Relates to Clemens 1988 Bangladesh. No additional data relevant to this review. |
| Emch 2007 | Relates to Clemens 1988 Bangladesh. No additional data relevant to this review. |
| Emch 2009 | Relates to Clemens 1988 Bangladesh. No additional data relevant to this review. |
| Forrest 1991 | A new vaccine candidate for which efficacy data is not currently available |
| Ganguly 1975 | Immunological outcomes only |
| Gateff 1975 | Injectable cholera vaccine |
| Glass 1989 | Immunological outcomes only |
| Glenn 2007 | Non‐cholera vaccine, no cholera outcomes (abstract) |
| Graves 2000 | A Cochrane Review (abstract) |
| Gray 1989 | Not relevant (abstract) |
| Gupta 1998 | Injectable cholera vaccine |
| Hall 2001 | Non‐cholera vaccine, no cholera outcomes (abstract) |
| Holmgren 1989 | Relates to Clemens 1988 Bangladesh. No additional data relevant to this review. |
| Holmgren 1992 | Relates to Clemens 1988 Bangladesh. No additional data relevant to this review. |
| Hotomi 1998 | Intranasal vaccination (abstract) |
| Islam 2008 | Not an RCT; a willingness to pay study |
| Jertborn 1984 | Not randomized |
| Jertborn 1986 | Retrospective, non‐comparative study. |
| Jertborn 1988 | Retrospective study. |
| Jertborn 1992 | This small study (41 participants) compared the safety and immunogenicity of the WC‐BS and WC‐rBS vaccines. As there was no placebo group we could not include the data. |
| Jertborn 1993 | Immunogenicity data only |
| Jertborn 1994 | Not randomized |
| Jertborn 1996 | Non‐randomised study. |
| Jertborn 1998 | Non‐cholera vaccine, no cholera outcomes |
| Jertborn 2001 | Not cholera vaccine |
| Johansson 2001 | Nasal and intravaginal vaccination (abstract) |
| Johansson 2004 | Nasal and intravaginal vaccination (abstract) |
| Jones 2004 | A summary of included studies |
| Karlsen 2003 | All participants received the same vaccine (abstract) |
| Kenner 1995 | Not randomized |
| Kilhamn 1998 | All participants received the same vaccine (abstract) |
| Kim 2008 | A willingness to pay study (abstract) |
| Kirk 2005 | A case‐control study (abstract) |
| Koenig 1998 | Non‐cholera vaccine, no cholera outcomes (abstract) |
| Kollaritsch 1996 | No efficacy data for this vaccine (CVD 103‐HgR‐Ty21a) |
| Kollaritsch 1997 | All participants received the same vaccine (abstract) |
| Kozlowski 1999 | Not a relevant comparison. Randomized to oral, intranasal and vaginal vaccination. (abstract) |
| Langevin‐Perriat 1988 | Immunological data only |
| Lastre 2002 | Immunological outcomes only |
| Lelikov 1974 | Injectable cholera vaccine |
| Levine 1984 | Not randomized |
| Levine 1988a | Not randomized |
| Levine 1988b | Not randomized |
| Lewis 1993 | Not randomized (on abstract) |
| Leyten 2005 | No relevant outcomes |
| Lopez 2008 | Not an RCT. A review (abstract) |
| Losonsky 1993 | Not randomized |
| Losonsky 1996 | Not randomized |
| Lucas 2005 | A case‐control study |
| Lucas 2007 | A willingness to pay study (abstract) |
| Mahalanabis 2009 | No efficacy data for this vaccine (VA1.3) |
| Martell 2009 | Non‐cholera vaccine, no cholera outcomes |
| María Garcia 2005 | This paper describes multiple small comparative studies (9 volunteers in each treatment arm) with different modifications and dosing of potential vaccine strains including VC638. We were unable to incorporate any of this data. |
| McCormack 1969 | Injectable vaccine |
| Migasena 1988 | Non‐randomized study |
| Migasena 1989b | Contains only safety and immunogenicity data. Excluded as no group received placebo. |
| Migasena 1989c | No efficacy study available for these vaccines |
| Mitra 1990 | No cholera vaccine was given. (Abstract) |
| Mosley 1968 | Injectable vaccine |
| Mosley 1969a | Injectable vaccine |
| Mosley 1969b | Injectable vaccine |
| Mosley 1970 | Injectable vaccine |
| Mosley 1972 | Injectable vaccine |
| Mosley 1973 | Injectable vaccine |
| Nimbkar 1975 | Immunological outcomes only |
| Olsson 2006 | Not an RCT (abstract) |
| Oseasohn 1965 | Injectable vaccine |
| Paineau 2008 | No vaccine given (abstract) |
| Pal 1980 | Injectable vaccine |
| Peltola 1977 | Intracutaneous vaccine (abstract) |
| Peltola 1989 | Trial assesses oral cholera vaccine for preventing travellers diarrhoea, not cholera. |
| Peltola 1991 | No cholera outcomes relevant to this review |
| Philippines 1965 | Injectable cholera vaccine |
| Pitisuttithum 2001 | No cholera vaccine was given. A study to validate an artificial cholera challenge model |
| Qadri 2003 | Not cholera vaccine |
| Qadri 2004 | All participants received the same vaccine |
| Qadri 2006 | Non‐cholera vaccine, no cholera outcomes (abstract) |
| Quiding‐Jarbrink 2001 | All participants received the same vaccine |
| Rao 2002 | Not an RCT (Abstract) |
| Rudin 1998 | Not an appropriate comparison group; oral versus nasal vaccination (abstract) |
| Rudin 1999 | Not an appropriate comparison group; oral versus nasal vaccination (abstract) |
| Sack 1991 | Relates to Clemens 1988 Bangladesh. No additional data relevant to this review. |
| Sack 2007 | Refers to Clemens 1988, no new data relevant to this review |
| Sanchez 1993b | Data on adverse effects not presented in usable form. |
| Sanchez 1994 | A preliminary report from Taylor 2000 Peru. Contains no additional data. |
| Saroso 1978 | Injectable cholera vaccine |
| Savarino 1998 | Non‐cholera vaccine, no cholera outcomes |
| Savarino 1999 | Non‐cholera vaccine, no cholera outcomes |
| Savarino 2002 | Non‐cholera vaccine, no cholera outcomes |
| Sommer 1973 | Randomized controlled study, but vaccine given after exposure to cholera in family members |
| SonLa 2007 | Non‐comparative study |
| Stellfeld 2004 | A review article. Not an RCT |
| Sumarokov 1974 | Injectable vaccine (abstract) |
| Sumarokov 1978 | No clinical efficacy data is available for this vaccine. Oral tablet containing choleragen toxoid, Ogawa and Inaba O‐antigens and Vibrio cholerae exoenzymes. |
| Sumarokov 1990 | No clinical efficacy data is available for this vaccine. Oral tablet containing choleragen toxoid, Ogawa and Inaba O‐antigens and Vibrio cholerae exoenzymes. |
| Sumarokov 1991 | No clinical efficacy data is available for this vaccine. Oral tablet containing choleragen toxoid, Ogawa and Inaba O‐antigens and Vibrio cholerae exoenzymes. |
| Sumarokov 1993 | No clinical efficacy data is available for this vaccine. Oral tablet containing choleragen toxoid, Ogawa and Inaba O‐antigens and Vibrio cholerae exoenzymes. |
| Suntharasamai 1992 | No vaccine given |
| Svennerholm 1981 | No cholera vaccine given (abstract) |
| Svennerholm 1984 | No efficacy data for this vaccine (B subunit alone) |
| Tacket 1992 | Not randomized |
| Tacket 1995a | No vaccine given |
| Tacket 1995b | No efficacy data for this vaccine (CVD 112) |
| Tacket 1998 | No efficacy data for this vaccine (CVD 112) |
| Taylor 1994 | No efficacy data for these vaccines (Peru 14, Peru 5, Peru 3) |
| Taylor 1997 | No efficacy data for this vaccine (CVD 103‐HgR/CVD112) |
| Taylor 1999b | No efficacy data for this vaccine (CVD 103‐HgR/CVD112) |
| Thiem 2006 | Case control study |
| Von Seidlein 2007 | A study of a fingerprint recognition system used during a cholera vaccine trial. Contains no relevant outcomes. |
| Wassen 2005 | Vaginal vaccination (abstract) |
| Wassen 2006 | Vaginal vaccination (abstract) |
| Wasserman 1993 | Immunogenicity data only |
| Wassén 1996 | Intravaginal vaccination (abstract) |
| Wiedermann 2000 | Non cholera vaccine, no cholera outcomes |
Differences between protocol and review
Since the publication of the original review, several changes have occurred in standard Cochrane methodology which were not in the original review. Notably; the method of assessing risk of bias has changed, and summary of findings tables incorporating the GRADE methodology for assessing the quality of evidence have been added. The current methodology for these additions is described in the methods section.
Contributions of authors
This review is an update of a previous review (Graves 2001). The protocol was revised with input from KA, KZ, FQ, PG and DS. The search results were screened by KA, PG and DS. KA, KZ and DS extracted data. KA wrote the first draft which was revised by DS with additional input from all authors.
Sources of support
Internal sources
No sources of support provided
External sources
Department for International Development, UK
Declarations of interest
We certify that we have no affiliations with or involvement in any organisation or entity with a direct financial interest in the subject matter of the review (e.g. employment, consultancy, stock ownership, honoraria, expert testimony).
Edited (no change to conclusions)
References
References to studies included in this review
Anh 2007 {published data only}
Begue 1995 {published data only}
- Begue RE, Castellares G, Ruiz R, Hayashi KE, Sanchez JL, Gotuzzo E, Oberst RB, Taylor DN, Svennerholm A-M. Community-based assessment of safety and immunogenicity of the whole cell plus recombinant b subunit (WC/rBS) oral cholera vaccine in Peru. Vaccine 1995;13(7):691-4. [DOI] [PubMed] [Google Scholar]
Benítez 1999 {published data only}
- Benítez JA, García L, Silva A, García H, Fando R, Cedré B, et al. Preliminary assessment of the safety and immunogenicity of a new CTXPhi-negative, hemagglutinin/protease-defective El Tor strain as a cholera vaccine candidate. Infection and Immunity 1999;67(2):539-45. [DOI] [PMC free article] [PubMed]
Chen 1996 {published data only}
- Chen Q, Yu S, Wang Y. [Community trial for safety and immunogenicity of oral-administered lyophilized rBS-WC cholera vaccine]. Zhonghua yu fang yi xue za zhi [Chinese journal of preventive medicine] 1996;30(6):330-3. [PubMed]
Clemens 1987 {published data only}
- Clemens JD, Stanton BF, Chakraborty J, Sack DA, Khan MR, Huda S, et al. B subunit-whole cell and whole cell-only oral vaccines against cholera: studies on reactogenicity and immunogenicity. Journal of Infectious Diseases 1987;155(1):79-85. [DOI] [PubMed] [Google Scholar]
Clemens 1988 Bangladesh {published data only}
- Clemens JD, Harris JR, Sack DA, Chakraborty J, Ahmed F, Stanton BF, et al. Field trial of oral cholera vaccine in Bangladesh: results from one year of follow-up. Journal of Infectious Diseases 1988;158(1):60-9. [DOI] [PubMed] [Google Scholar]
- Clemens JD, Harris JR, Sack DA, Chakraborty J, Ahmed F, Stanton BF, et al. Field trial of oral cholera vaccines in Bangladesh. Southeast Asian Journal of Tropical Medince and Public Health 1988;19(3):417-422. [PubMed] [Google Scholar]
- Clemens JD, Sack DA, Chakraborty J, Rao MR, Ahmed F, Harris JR, et al. Field trial of oral cholera vaccines in Bangladesh: evaluation of anti-bacterial and anti-toxic breast-milk immunity in repsonse to ingestion of the vaccines. Vaccine 1990;8:469-72. [DOI] [PubMed] [Google Scholar]
- Clemens JD, Sack DA, Harris JR, Chakraborty J, Khan MR, Huda S, et al. ABO blood groups and cholera: new observations on specificity of risk and modifications of vaccine efficacy. Journal of Infectious Diseases 1989;159(4):770-3. [DOI] [PubMed] [Google Scholar]
- Clemens JD, Sack DA, Harris JR, Chakraborty J, Khan MR, Stanton BF, et al. Field trial of oral cholera vaccines in Bangladesh. Lancet 1986;2(8499):124-7. [DOI] [PubMed] [Google Scholar]
- Clemens JD, Sack DA, Harris JR, Chakraborty J, Khan MR, Stanton BF, et al. Impact of b subunit killed whole-cell and killed whole-cell-only oral vaccines against cholera upon treated diarrhoeal illness and mortality in an area endemic for cholera. Lancet 1988;1(8599):1375-9. [DOI] [PubMed] [Google Scholar]
- Clemens JD, Sack DA, Harris JR, Loon F, Chakraborty J, Ahmed F, et al. Field trial of oral cholera vaccines in Bangladesh: results from three-year follow-up. Lancet 1990;335(8684):270-73. [DOI] [PubMed] [Google Scholar]
- Loon FPL, Clemens JD, Chakraborty J, Rao MR, Kay BA, Sack DA, et al. Field trial of inactivated oral cholera vaccines in Bangladesh: results from 5 years of follow-up. Vaccine 1996;14(2):162-6. [DOI] [PubMed] [Google Scholar]
Cohen 2002 {published data only}
- Cohen MB, Giannella RA, Bean J, Taylor DN, Parker S, Hoeper A, et al. Randomized, controlled human challenge study of the safety, immunogenicity, and protective efficacy of a single dose of Peru-15, a live attenuated oral cholera vaccine. Infection and immunity 2002;70(4):1965-70. [DOI] [PMC free article] [PubMed]
Concha 1995 {published data only}
- Concha A, Giraldo A, Castaneda E, Martinez M, la Hoz F, Rivas F, et al. Safety and immunogenicity of oral killed whole cell recombinant B subunit cholera vaccine in Barranquilla, Colombia. [Seguridad e immunogenicidad de la vacuna anticolera de celulas enteras muertas y de la subunidad B recombinante de la tozina en Barranquilla, Colombia]. Bol Of Sanit Panam 1995;119(2):103-12. [Google Scholar]
- Concha A, Giraldo A, Castañeda E, Martínez M, la Hoz F, Rivas F, et al. Safety and immunogenicity of oral killed whole cell recombinant B subunit cholera vaccine in Barranquilla, Colombia. Bulletin of the Pan American Health Organization 1995;29(4):312-21. [PubMed]
Cryz 1990 {published data only}
García 2005 {published data only}
- García L, Jidy MD, García H, Rodríguez BL, Fernández R, Año G, et al. The vaccine candidate Vibrio cholerae 638 is protective against cholera in healthy volunteers. Infection and Immunity 2005;73(5):3018-24. [DOI] [PMC free article] [PubMed]
Gotuzzo 1993 {published data only}
- Gotuzzo E, Butron B, Seas C, Penny M, Ruiz R, Losonsky G, et al. Safety, immunogenicity, and excretion pattern of single-dose live oral cholera vaccine CVD 103-HgR in Peruvian adults of high and low socioeconomic levels. Infection and Immunity 1993;61(9):3994-7. [DOI] [PMC free article] [PubMed]
Hallander 2002 {published data only}
Kanungo 2009 {published data only}
- Kanungo S, Paisley A, Lopez AL, Bhattacharya M, Manna B, Kim DR, et al. Immune responses following one and two doses of the reformulated, bivalent, killed, whole-cell, oral cholera vaccine among adults and children in Kolkata, India: a randomized, placebo-controlled trial. Vaccine 2009;27(49):6887-93. [DOI] [PubMed]
Kotloff 1992 {published data only}
- Kotloff KL, Wasserman SS, O'Donnell S, Losonsky GA, Cryz SJ, Levine MM. Safety and immunogenicity in North Americans of a single dose of live oral cholera vaccine CVD 103-HgR: results of a randomized, placebo-controlled, double-blind crossover trial. Infection and Immunity 1992;60(10):4430-2. [DOI] [PMC free article] [PubMed]
Lagos 1993 {published data only}
- Lagos R, Avendaño A, Horwitz I, Prado V, Ferreccio C, Sotomayor V, et al. [Tolerance and immunogenicity of an oral dose of CVD 103-HgR, a live attenuated Vibrio cholerae 01 strain: a double-blind study of Chilean adults]. Revista médica de Chile 1993;121(8):857-63. [PubMed]
Lagos 1995 {published data only}
- Lagos R, Avendaño A, Prado V, Horwitz I, Wasserman S, Losonsky G, et al. Attenuated live cholera vaccine strain CVD 103-HgR elicits significantly higher serum vibriocidal antibody titers in persons of blood group O. Infection and Immunity 1995;63(2):707-9. [DOI] [PMC free article] [PubMed]
Lagos 1999 {published data only}
Mahalanabis 2008 {published data only}
- Mahalanabis D, Lopez AL, Sur D, Deen J, Manna B, Kanungo S, et al. A randomized, placebo-controlled trial of the bivalent killed, whole-cell, oral cholera vaccine in adults and children in a cholera endemic area in Kolkata, India. PLoS ONE 2008;3(6):e2323. [DOI] [PMC free article] [PubMed]
Migasena 1989a {published data only}
- Migasena S, Pitisuttitham P, Prayurahong B, Suntharasamai P, Supanaranond W, Desakorn V, et al. Preliminary assessment of the safety and immunogenicity of live oral cholera vaccine strain CVD 103-HgR in healthy Thai adults. Infection and Immunity 1989;57(11):3261-4. [DOI] [PMC free article] [PubMed]
Perry 1998 {published data only}
- Perry RT, Plowe CV, Koumaré B, Bougoudogo F, Kotloff KL, Losonsky GA, et al. A single dose of live oral cholera vaccine CVD 103-HgR is safe and immunogenic in HIV-infected and HIV-noninfected adults in Mali. Bulletin of the World Health Organization 1998;76(1):63-71. [PMC free article] [PubMed]
Qadri 2005 {published data only}
- Qadri F, Chowdhury MI, Faruque SM, Salam MA, Ahmed T, Begum YA, et al. Randomized, controlled study of the safety and immunogenicity of Peru-15, a live attenuated oral vaccine candidate for cholera, in adult volunteers in Bangladesh. The Journal of Infectious Diseases 2005;192(4):573-9. [DOI] [PubMed]
Qadri 2007 {published data only}
Richie 2000 Indonesia {published data only}
- Punjabi N, Simanjuntak C, Richie E, Sidharta Y, et al. Large scale, randomized, double blind, placebo controlled field trial to assess the efficacy of a single dose of live oral cholera vaccine CVD 103-HgR. [abstract]. American Journal of Tropical Medicine and Hygiene 1998;59(3 Suppl):249-50. [Google Scholar]
- Richie E, Punjabi NH, Sidharta Y, Peetosutan K, Sukander M, Wasserman SS, et al. Efficacy trial of single dose live oral vaccine CVD 103-HgR in North Jakarta, Indonesia, a cholera endemic area. Vaccine 2000;18:2399-410. [DOI] [PubMed] [Google Scholar]
Sack 1997 {published data only}
Sanchez 1993a {published data only}
Sanchez 1994 Peru {published data only}
- Sanchez JL, Vasquez B, Begue RE, Meza R, Castellares G, Cabezas C, et al. Protective efficacy of oral whole-cell/recombinant-b-subunit cholera vaccine in Peruvian military recruits. Lancet 1994;344(8932):1273-76. [DOI] [PubMed] [Google Scholar]
Sanchez 1995 Peru {published data only}
- Sanchez JL, Hayashi KE, Kruger HF, Meza R, English CK, Vidal W, et al. Immunological response to vibrio cholerae 01 infection and an oral cholera vaccine among Peruvians. Transactions of the Royal Society of Tropical Medicine and Hygiene 1995;89(5):542-5. [DOI] [PubMed] [Google Scholar]
Simanjuntak 1993 {published data only}
- Simanjuntak CH, O'Hanley P, Punjabi NH, Noriega F, Pazzaglia G, Dykstra P, et al. Safety, immunogenicity, and transmissibility of single-dose live oral cholera vaccine strain CVD 103-HgR in 24- to 59-month-old Indonesian children. The Journal of Infectious Diseases 1993;168(5):1169-76. [DOI] [PubMed]
Su‐Arehawaratana 1992a {published data only}
Su‐Arehawaratana 1992b {published data only}
- Su-Arehawaratana P, Singharaj P, Taylor DN, Hoge C, Trofa A, Kuvanont K, et al. Safety and immunogenicity of different immunization regimens of CVD 103-HgR live oral cholera vaccine in soldiers and civilians in Thailand. The Journal of Infectious Diseases 1992;165(6):1042-8. [DOI] [PubMed] [Google Scholar]
Suharyono 1992a {published data only}
Suharyono 1992b {published data only}
- Suharyono, Simanjuntak C, Witham N, Punjabi N, Heppner DG, Losonsky G, et al. Safety and immunogenicity of single-dose live oral cholera vaccine CVD 103-HgR in 5-9-year-old Indonesian children. Lancet 1992;340(8821):689-94. [DOI] [PubMed] [Google Scholar]
Sur 2009 India {published data only}
Tacket 1999 {published data only}
- Tacket CO, Cohen MB, Wasserman SS, Losonsky G, Livio S, Kotloff K, et al. Randomized, double-blind, placebo-controlled, multicentered trial of the efficacy of a single dose of live oral cholera vaccine CVD 103-HgR in preventing cholera following challenge with Vibrio cholerae O1 El tor inaba three months after vaccination. Infection and Immunity 1999;67(12):6341-5. [DOI] [PMC free article] [PubMed]
Taylor 1999a {published data only}
Taylor 2000 Peru {published data only}
- Taylor DN, Cardenas V, Sanchez JL, Begue RE, Gilman R, Bautista C, et al. Two-year study of the protective efficacy of the oral whole cell plus recombinant B subunit cholera vaccine in Peru. Journal of Infectious Diseases 2000;181:1667-73. [DOI] [PubMed] [Google Scholar]
Trach 1997 Viet Nam {published data only}
- Trach DD, Clemens JD, Ke NT, Thuy HT, Son ND, Canh DG, et al. Field trial of a locally produced, killed, oral cholera vaccine in Vietnam. Lancet 1997;349(9047):231-5. [DOI] [PubMed] [Google Scholar]
Trach 2002 {published data only}
- Trach DD, Cam PD, Ke NT, Rao MR, Dinh D, Hang PV, et al. Investigations into the safety and immunogenicity of a killed oral cholera vaccine developed in Viet Nam. Bulletin of the World Health Organization 2002;80(1):2-8. [PMC free article] [PubMed]
Valera 2009 {published data only}
References to studies excluded from this review
Ahmed 2006 {published data only}
Ahren 1993 {published data only}
- Ahren C, Wenneras C, Holmgren J, Svennerholm A-M. Intestinal antibody response after oral immunization with a prototype cholera B subunit-colonization factor antigen enterotoxigenic escherichia coli vaccine. Vaccine 1993;11(9):929-34. [DOI] [PubMed] [Google Scholar]
Albert 2003 {published data only}
Ali 2005 {published data only}
- Ali M, Emch M, Seidlein L, Yunus M, Sack DA, Rao M, et al. Herd immunity conferred by killed oral cholera vaccines in Bangladesh: a reanalysis. Lancet 2005;366(9479):44-9. [DOI] [PubMed] [Google Scholar]
Ali 2008 {published data only}
- Ali M, Emch M, Yunus M, Sack D, Lopez AL, Holmgren J, Clemens J. Vaccine protection of Bangldeshi infants and young children against cholera: implications and for vaccine deployment and person-to-person transmission. Pediatric Infectious Disease Journal 2008;27(1):33-7. [DOI] [PubMed] [Google Scholar]
Anonymous 1968 {published data only}
- Anonymous. A controlled field trial of the effectiveness of various doses of cholera El Tor vaccine in the Philippines. Bulletin of the World Health Organization 1968;38(6):917-23. [PMC free article] [PubMed]
Anonymous 1973a {published data only}
- Anonymous. A controlled field trial of the effectiveness of monovalent classical and El Tor cholera vaccines in the Philippines. Bulletin of the World Health Organization 1973;49(1):13-9. [PMC free article] [PubMed]
Anonymous 1973b {published data only}
- Anonymous. A controlled field trial on the effectiveness of the intradermal and subcutaneous administration of cholera vaccine in the Philippines. Bulletin of the World Health Organization 1973;49(4):389-94. [PMC free article] [PubMed]
Azurin 1967 {published data only}
- Azurin JC, Cruz A, Pesigan TP, Alvero M, Camena T, Suplido R, et al. A controlled field trial of the effectiveness of cholera and cholera El Tor vaccines in the Philippines. Bulletin of the World Health Organization 1967;37(5):703-27. [PMC free article] [PubMed]
Azurin 1971 {published data only}
- Azurin JC, Alvero M. Cholera incidence in a population offered cholera vaccination: comparison of cooperative and uncooperative groups. Bulletin of the World Health Organization 1971;44(6):815-9. [PMC free article] [PubMed]
Benenson 1968a {published data only}
- Benenson AS, Joseph PR, Oseasohn RO. Cholera vaccine field trials in east Pakistan. 1. Reaction and antigenicity studies. Bulletin of the World Health Organization 1968;38(3):347-57. [PMC free article] [PubMed]
Benenson 1968b {published data only}
- Benenson AS, Mosley WH, Fahimuddin M, Oseasohn RO. Cholera vaccine field trials in east Pakistan. 2. Effectiveness in the field. Bulletin of the World Health Organization 1968;38(3):359-72. [PMC free article] [PubMed]
Bergquist 1997 {published data only}
- Bergquist C, Johansson EL, Lagergard T, Holmgren J, Rudin A. Intranasal vaccination of humans with recombinant cholera toxin B subunit induces systemic and local antibody responses in the upper respiratory tract and the vagina. Infection and Immunity 1997;65(7):2676-84. [DOI] [PMC free article] [PubMed]
Black 1986 {published data only}
- Black RE, Levine MM, Clements ML, Young CR, Svennerholm A-M, Holmgren J, Germanier R. Oral immunization with killed whole vibrio and B subunit or procholeragenoid combination cholera vaccines: immune response and protection from V.chlolerae challenge. In: Kuwahara S, Peirce NF, editors(s). Advances in Research on Cholera and Related Diarrheas. Vol. 3. Tokyo: KTK Scientific Publications, 1986:271-5. [Google Scholar]
Black 1987 {published data only}
- Black RE, Levine MM, Clements ML, Young CR, Svennerholm A-M, Holmgren J. Protective efficacy in humans of killed whole-vibrio oral cholera vaccine with and without the B subunit of cholera toxin. Infection and Immunity 1987;55(5):1116-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Burgasov 1976 {published data only}
- Burgasov PN, Sumarokov AA, Lelikov VL, Marcuk LM, Fedenev VG, Dzaparidze MN, et al. Comparative study of reactions and serological response to cholera vaccines in a controlled field trial conducted in the USSR. Bulletin of the World Health Organization 1976;54(2):163-70. [PMC free article] [PubMed]
Bwanga 1984 {published data only}
- Bwanga M. [Initial controlled clinical trials of an oral anticholera vaccine during the cholera epidemic in the district of Malemba-Nkulu (Shaba-Zaire)]. Bulletin de la Société de pathologie exotique et de ses filiales 1984;77(1):13-6. [PubMed]
Cash 1974 {published data only}
- Cash RA, Music SI, Libonati JP, Schwartz AR, Hornick RB. Live oral cholera vaccine: evaluation of the clinical effectiveness of two strains in humans. Infection and Immunity 1974;10(4):762-4. [DOI] [PMC free article] [PubMed]
Cavailler 2006 {published data only}
Chaicumpa 1998 {published data only}
- Chaicumpa W, Chongsa-nguan M, Kalambaheti T, Wilairatana P, Srimanote P, Makakunkijcharoen Y et al. Immunogenicity of liposome-associated and refined antigen oral cholera vaccine in Thai volunteers. Vaccine 1998;16(7):678-84. [DOI] [PubMed] [Google Scholar]
Chongsa‐nguan 1988 {published data only}
- Chongsa-nguan M, Chaicumpa W, Ruangkunaporn Y, Looareesuwan S. Immunogenicity of two formulations of oral cholera vaccines in Thai volunteers. Vaccine 1991;9(1):53-9. [DOI] [PubMed] [Google Scholar]
Chongsa‐nguan 1991 {published data only}
Ciznar 1989 {published data only}
Clemens 1986 {published data only}
- Clemens JD, Jertborn M, Sack D, Stanton B, Holmgren J, Khan MR, Huda S. Effect of neutralization of gastric acid on immune responses to an oral b subunit, killed whole-cell cholera vaccine. Journal of Infectious Diseases 1986;154(1):175-8. [DOI] [PubMed] [Google Scholar]
Clemens 1988 {published data only}
- Clemens JD, Sack DA, Harris JR, Chakraborty J, Neogy PK, Stanton B, et al. Cross-protection by B subunit-whole cell Cholera vaccine against diarrhea associated with heat-labile toxin-producing enterotoxigenic escherichia coli: results of a large-scale field trial. Journal of Infectious Diseases 1988;158(2):372-7. [DOI] [PubMed] [Google Scholar]
Clemens 1989a {published data only}
- Clemens JD, Harris JR, Kay BA, Chakraborty J, Sack DA, Ansaruzzaman M, et al. Oral cholera vaccines containing B-subunit-killed whole cells and killed whole cells only. II. Field evaluation of cross-protection against other members of the vibrionaceae family. Vaccine 1989;7(2):117-20. [DOI] [PubMed] [Google Scholar]
Clemens 1989b {published data only}
- Clemens JD, Stanton BF, Harris JR, Chakraborty J, Dack DA, Rao MR, et al. Exclusion of clinically atypical or microbiologically mixed diarrhoeal episodes from outcome events in a field trial of oral cholera vaccines. International Journal of Epidemiology 1989;18(2):440-5. [DOI] [PubMed] [Google Scholar]
Clemens 1990 {published data only}
- Clemens JD, Sack DA, Chakraborty J, Rao MR, Ahmed F, Harris JR, et al. Field trial of oral cholera vaccines in Bangladesh: evaluation of anti-bacterial and anti-toxic breast-milk immunity in repsonse to ingestion of the vaccines. Vaccine 1990;8:469-72. [DOI] [PubMed] [Google Scholar]
Clemens 1991 {published data only}
- Clemens JD, Loon F, Sack DA, Chakraborty J, Rao MR, Ahmed F, et al. Field trial of oral cholera vaccines in Bangladesh: serum vibriocidal and antitoxic antibodies as markers of the risk of cholera. Journal of Infectious Diseases 1991;163:1235-42. [DOI] [PubMed] [Google Scholar]
Clemens 1992a {published data only}
Clemens 1992b {published data only}
- Clemens JD, Sack DA, Rao MR, Chakraborty J, Khan MR, Kay B, et al. Evidence that inactivated oral cholera vaccines both prevent and mitigate vibrio cholerae 01 infections in a cholera-endemic area. Journal of Infectious Diseases 1992;166:1029-34. [DOI] [PubMed] [Google Scholar]
Clemens 1995 {published data only}
- Clemens J, Rao M, Sack D, Ahmed F, Khan MR, Chakraborty J, et al. Impaired immune response to natural infection as a correlate of vaccine failure in a field trial of killed oral cholera vaccines. American Journal of Epidemiology 1995;142(7):759-64. [DOI] [PubMed] [Google Scholar]
Cohen 1999 {published data only}
- Cohen MB, Giannella RA, Losonsky GA, Lang DR, Parker S, Hawkins JA, et al. Validation and characterization of a human volunteer challenge model for cholera by using frozen bacteria of the new Vibrio cholerae epidemic serotype, O139. Infection & Immunity 1999;67(12):6346-9. [DOI] [PMC free article] [PubMed]
Cohen 2000 {published data only}
- Cohen D, Orr N, Haim M, Ashkenazi S, Robin G, Green MA, et al. Safety and immunogenicity of two different lots of the oral, killed enterotoxigenic escherichia coli-cholera toxin B subunit vaccine in young Isreali adults. Infection and Immunology 2000;68(8):4492-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cooper 2000 {published data only}
Cooper 2001 {published data only}
- Cooper PJ, Chico M, Sandoval C, Espinel I, Guevara A, Levine MM, et al. Human infection with Ascaris lumbricoides is associated with suppression of the interleukin-2 response to recombinant cholera toxin B subunit following vaccination with the live oral cholera vaccine CVD 103-HgR. Infection and Immunity 2001;69(3):1574-80. [DOI] [PMC free article] [PubMed]
Coster 1995 {published data only}
Cryz 1992 {published data only}
- Cryz Jr SJ, Levine MM, Losonsky G, Kaper JB, Althaus B. Safety and immunogenicity of a booster dose of Vibrio cholerae CVD 103-HgR live oral cholera vaccine in Swiss adults. Infection and Immunity 1992;60(9):3916-7. [DOI] [PMC free article] [PubMed]
Cryz 1995 {published data only}
- Cryz SJ, Que JU, Levine MM, Wiedermann G, Kollaritsch H. Safety and immunogenicity of a live oral bivalent typhoid fever (Salmonella typhi Ty21a)-cholera (Vibrio cholerae CVD 103-HgR) vaccine in healthy adults. Infection and Immunity 1995;63(4):1336-9. [DOI] [PMC free article] [PubMed]
Das 1967 {published data only}
- Das Gupta A, Sinha R, Shrivastava DL, De SP, Taneja BL, Rao MS, et al. Controlled field trial of the effectiveness of cholera and cholera El Tor vaccines in Calcutta. Bulletin of the World Health Organization 1967;37(3):371-85. [PMC free article] [PubMed]
Dearlove 1992 {published data only}
Durham 1998 {published data only}
- Durham LK, Longini IM Jr, Halloran ME, Clemens JD, Nizam A, Rao M. Estimation of vaccine efficacy in the presence of waning: application to cholera vaccines. American Journal of Epidemiology 1998;147(10):948-59. [DOI] [PubMed] [Google Scholar]
Emch 2006 {published data only}
- Emch M, Ali M, Park JK, Yunus M, Sack DA, Clemens JD. Relationship between neighbourhood-level killed oral cholera vaccine coverage and protective efficacy: evidence for herd immunity. International Journal of Epidemiology. 2006;35(4):1044-50. [DOI] [PubMed] [Google Scholar]
Emch 2007 {published data only}
- Emch M, Ali M, Acosta C, Yunus M, Sack DA, Clemens JD. Efficacy calculation in randomized trials: global or local measures? Health Place 2007;13(1):238-48. [DOI] [PubMed] [Google Scholar]
Emch 2009 {published data only}
- Emch M, Ali M, Root ED, Yunus M. Spatial and environmental connectivity analysis in a cholera vaccine trial. Social science & medicine (1982) 2009;68(4):631-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Forrest 1991 {published data only}
Ganguly 1975 {published data only}
- Ganguly R, Clem LW, Bencic Z, Sinha R, Sakazaki R, Waldman RH. Antibody response in the intestinal secretions of volunteers immunized with various cholera vaccines. Bulletin of the World Health Organization 1975;52(3):323-30. [PMC free article] [PubMed] [Google Scholar]
Gateff 1975 {published data only}
- Gateff C, Dodin A, Wiart J. [A comparison of the serological effects of classical cholera vaccine and of purified fraction vaccine, with or without simultaneous yellow fever vaccine (author's transl)]. Annales de microbiologie 1975;126(2):231-46. [PubMed]
Glass 1989 {published data only}
- Glass RI, Svennerholm A-M, Stoll BJ, Khan MR, Huda S, Huq MI, Holmgren J. Effects of undernutrition on infection with vibrio cholerae 01 and on response to oral cholera vaccine. Pediatric Infectious Disease Journal 1989;8(2):105-9. [PubMed] [Google Scholar]
Glenn 2007 {published data only}
- Glenn GM, Villar CP, Flyer DC, Bourgeois AL, McKenzie R, Lavker RM, et al. Safety and immunogenicity of an enterotoxigenic Escherichia coli vaccine patch containing heat-labile toxin: use of skin pretreatment to disrupt the stratum corneum. Infection and Immunity 2007;75(5):2163-70. [DOI] [PMC free article] [PubMed]
Graves 2000 {published data only}
- Graves P, Deeks J, Demicheli V, Pratt M, Jefferson T. Vaccines for preventing cholera. Cochrane Database of Systematic Reviews 2001, Issue 1. Art. No: CD000974. Art. No: CD000974. [DOI: Art. No.: CD000974. DOI: 10.1002/14651858.CD000974] [Google Scholar]
Gray 1989 {published data only}
Gupta 1998 {published data only}
- Gupta RK, Taylor DN, Bryla DA, Robbins JB, Szu SC. Phase 1 evaluation of Vibrio cholerae O1, serotype Inaba, polysaccharide-cholera toxin conjugates in adult volunteers. Infection and Immunity 1998;66(7):3095-9. [DOI] [PMC free article] [PubMed]
Hall 2001 {published data only}
- Hall ER, Wierzba TF, Ahren C, Rao MR, Bassily S, Francis W, et al. Induction of systemic antifimbria and antitoxin antibody responses in Egyptian children and adults by an oral, killed enterotoxigenic Escherichia coli plus cholera toxin B subunit vaccine. Infection and Immunity 2001;69(5):2853-7. [DOI] [PMC free article] [PubMed]
Holmgren 1989 {published data only}
- Holmgren J, Clemens J, Sack DA, Sanchez J, Svennerholm A-M. Oral immunization against cholera. Current Topics in Microbiology and Immunology 1989;146:197-204. [DOI] [PubMed] [Google Scholar]
Holmgren 1992 {published data only}
- Holmgren J, Svennerholm AM, Jertborn M, Clemens J, Sack DA, Salenstedt R, et al. An oral B subunit: whole cell vaccine against cholera. Vaccine 1992;10(13):911-4. [DOI] [PubMed] [Google Scholar]
Hotomi 1998 {published data only}
Islam 2008 {published data only}
Jertborn 1984 {published data only}
Jertborn 1986 {published data only}
- Jertborn M, Svennerholm A-M, Holmgren J. Saliva, breast milk, and serum antibody responses as indirect measures of intestinal immunity after oral cholera vaccination or natural disease. Journal of Clinical Microbiology 1986;24(2):203-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jertborn 1988 {published data only}
- Jertborn M, Svennerholm A-M, Holmgren J. Five-year immunologic memory in Swedish volunteers after oral cholera vaccination. Journal of Infectious Diseases 1988;157(2):374-7. [DOI] [PubMed] [Google Scholar]
Jertborn 1992 {published data only}
- Jetborn M, Svennerholm A-M, Holmgren J. Safety and immunogenicity of an oral recombinant cholera b subunit-whole cell vaccine in Swedish volunteers. Vaccine 1992;10(2):130-2. [DOI] [PubMed] [Google Scholar]
Jertborn 1993 {published data only}
Jertborn 1994 {published data only}
Jertborn 1996 {published data only}
- Jetborn M, Svennerholm A-M, Holmgren J. Intestinal and systemic immune responses in human after oral immunization with a bivalent b subunit-01/0139 whole cell cholera vaccine. Vaccine 1996;14(15):1459-65. [DOI] [PubMed] [Google Scholar]
Jertborn 1998 {published data only}
Jertborn 2001 {published data only}
- Jertborn M, Ahren C and Svennerholm AM. Dose-dependent circulating immunoglobin A antibody-secreting cell and serum antibody responses in Swedish volunteers to an oral inactivated enterotoxigenic Escherichia coli vaccine. Clinical and Diagnostic Laboratory Immunology 2001;8(2):424-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Johansson 2001 {published data only}
- Johansson EL, Wassen L, Holmgren J, Jertborn M, Rudin A. Nasal and vaginal vaccinations have differential effects on antibody responses in vaginal and cervical secretions in humans. Infection and Immunity 2001;69(12):7481-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Johansson 2004 {published data only}
Jones 2004 {published data only}
- Jones T. Peru-1 5 (AVANT). Current Opinion in Investigational Drugs 2004;5(8):887-91. [PubMed]
Karlsen 2003 {published data only}
- Karlsen TH, Sommerfelt H, Klomstad S, Andersen PK, Strand TA, Ulvik RJ, et al. Intestinal and systemic immune responses to an oral cholera toxoid B subunit whole-cell vaccine administered during zinc supplementation. Infection and Immunity 2003;71(7):3909-13. [DOI] [PMC free article] [PubMed]
Kenner 1995 {published data only}
Kilhamn 1998 {published data only}
- Kilhamn J, Jertborn M, Svennerholm AM. Kinetics of local and systemic immune responses to an oral cholera vaccine given alone or together with acetylcysteine. Clinical and Diagnostic Laboratory Immunology 1998;5(2):247-50. [DOI] [PMC free article] [PubMed]
Kim 2008 {published data only}
Kirk 2005 {published data only}
- Kirk MD, Kiedrzynski T, Johnson E, Elymore A, Wainiqolo I. Risk factors for cholera in Pohnpei during an outbreak in 2000: lessons for Pacific countries and territories. Pacific Health Dialog 2005;12(2):17-22. [PubMed]
Koenig 1998 {published data only}
- Koenig MA, Roy NC, McElrath T, Shahidullah M, Wojtyniak B. Duration of protective immunity conferred by maternal tetanus toxoid immunization: Further evidence from Matlab, Bangladesh. American Journal of Public Health 1998;88(6):903-7. [DOI] [PMC free article] [PubMed]
Kollaritsch 1996 {published data only}
- Kollaritsch H, Furer E, Herzog C, Wiedermann G, Que JU, Cryz SJ. Randomized, double-blind placebo-controlled trial to evaluate the safety and immunogenicity of combined Salmonella typhi Ty21a and Vibrio cholerae CVD 103-HgR live oral vaccines. Infection and Immunity 1996;64(4):1454-7. [DOI] [PMC free article] [PubMed]
Kollaritsch 1997 {published data only}
- Kollaritsch H, Que JU, Kunz C, Wiedermann G, Herzog C, Cryz SJ. Safety and immunogenicity of live oral cholera and typhoid vaccines administered alone or in combination with antimalarial drugs, oral polio vaccine, or yellow fever vaccine. The Journal of Infectious Diseases 1997;175(4):871-5. [DOI] [PubMed]
Kozlowski 1999 {published data only}
Langevin‐Perriat 1988 {published data only}
Lastre 2002 {published data only}
- Lastre M, Del Campo J, Cedre B, Valmaseda T, Garcia L, Bracho G, Serrano T, Fando R, Sierra G, Perez O. Mucosal IgA anti-lipopolysaccharide antibodies induced by 638 oral live attenuated candidate vaccine. Immunologia 2002;21(1):3-9. [Google Scholar]
Lelikov 1974 {published data only}
- Lelikov VL, Sumarokov AA, Ivanov NR, Fedenev VG, Poliakov KA. [Study of the immunogenicity and immunological effectiveness of choleragen anatoxin (data from a controlled epidemiological experiment). I. The characteristics of choleragen anatoxin compared wiht corpuscular cholera vaccines administered by syringe and by using a jet injector]. Zhurnal mikrobiologii, epidemiologii, i immunobiologii 1974;(11):25-30. [PubMed]
Levine 1984 {published data only}
- Levine MM, Black RE, Clements MLet al. Evaluation in humans of attenuated Vibrio cholerae El Tor Ogawa strain Texas Star-SR as a live oral vaccine. Infection and Immunity 1984;43(2):515-22. [DOI] [PMC free article] [PubMed]
Levine 1988a {published data only}
- Levine MM, Kaper JB, Herrington D, Losonsky G, Morris JG, Clements ML, et al. Volunteer studies of deletion mutants of Vibrio cholerae O1 prepared by recombinant techniques. Infection and Immunity 1988;56(1):161-7. [DOI] [PMC free article] [PubMed]
Levine 1988b {published data only}
Lewis 1993 {published data only}
Leyten 2005 {published data only}
- Leyten EM, Soonawala D, Schultsz C, Herzog C, Ligthelm RJ, Wijnands S, et al. Analysis of efficacy of CVD 103-HgR live oral cholera vaccine against all-cause travellers' diarrhoea in a randomised, double-blind, placebo-controlled study. Vaccine 2005;23(43):5120-6. [DOI] [PubMed] [Google Scholar]
Lopez 2008 {published data only}
Losonsky 1993 {published data only}
- Losonsky GA, Tacket CO, Wasserman SS, Kaper JB, Levine MM. Secondary Vibrio cholerae-specific cellular antibody responses following wild-type homologous challenge in people vaccinated with CVD 103-HgR live oral cholera vaccine: Changes with time and lack of correlation with protection. Infection and Immunity 1993;61(2):729-33. [DOI] [PMC free article] [PubMed]
Losonsky 1996 {published data only}
- Losonsky GA, Yunyongying J, Lim V, Reymann M, Yu Leong Lim, Wasserman SS, et al. Factors influencing secondary vibriocidal immune responses: Relevance for understanding immunity to cholera. Infection and Immunity 1996;64(1):10-5. [DOI] [PMC free article] [PubMed]
Lucas 2005 {published data only}
Lucas 2007 {published data only}
Mahalanabis 2009 {published data only}
María Garcia 2005 {published data only}
- María García H, Año G, Cedré B, Valmaseda T, Maestre JL, Díaz M, et al. [Selection of attenuated Vibrio cholerae strains to obtain oral attenuated candidate vaccines against cholera]. Revista cubana de medicina tropical 2005;57(2):92-104. [PubMed]
Martell 2009 {published data only}
- Martell BA, Orson FM, Poling J, Mitchell E, Rossen RD, Gardner T, et al. Cocaine vaccine for the treatment of cocaine dependence in methadone-maintained patients: a randomized, double-blind, placebo-controlled efficacy trial. Arch Gen Psychiatry 2009;66(10):1116-23. [DOI] [PMC free article] [PubMed]
McCormack 1969 {published data only}
- McCormack WM, Rahman AS, Chowdhury AK, Mosley WH, Phillips RA. Report of the 1966-67 cholera vaccine field trial in rural East Pakistan. 3. The lack of effect of prior vaccination or circulating vibriocidal antibody on the severity of clinical cholera. Bulletin of the World Health Organization 1969;40(2):199-204. [PMC free article] [PubMed]
Migasena 1988 {published data only}
- Migasena S, Pitisuttitham P, Supanaranond W, Desakorn V, Prayurahong B, Suntharasamai, P. Reactogenicity and immunogenicity of oral cholera vaccine in Thai volunteers. Souteast Asian Journal of Tropical Medicine and Public Health 1988;19(3):423-8. [PubMed] [Google Scholar]
Migasena 1989b {published data only}
- Migasena S, Desakorn V, Suntharasamai P, Pitisuttitham P, Prayurahong B, Supanaranond W, et al. Immunogenicity of two formulations of oral cholera vaccine comprised of killed whole vibrios and the B subunit of cholera toxin. Infection and Immunity 1989;57(1):117-20. [DOI] [PMC free article] [PubMed]
Migasena 1989c {published data only}
- Migasena S, Pitisuttitham P, Suntharasamai P, Prayurahong B, Supanaranond W, Desakorn V, et al. Comparison of the reactivities and immunogenicities of procholeragenoid and the B subunit of cholera toxin in Thai volunteers. Infection and Immunity 1989;57(7):1942-5. [DOI] [PMC free article] [PubMed]
Mitra 1990 {published data only}
Mosley 1968 {published data only}
- Mosley WH, Benenson AS, Barui R. A serological survey for cholera antibodies in rural east Pakistan. 2. A comparison of antibody titres in the immunized and control populations of a cholera-vaccine field-trial area and the relation of antibody titre to cholera case rate. Bulletin of the World Health Organization 1968;38(3):335-46. [PMC free article] [PubMed]
Mosley 1969a {published data only}
- Mosley WH, McCormack WM, Ahmed A, Chowdhury AK, Barui RK. Report of the 1966-67 cholera vaccine field trial in rural East Pakistan. 2. Results of the serological surveys in the study population--the relationship of case rate to antibody titre and an estimate of the inapparent infection rate with Vibrio cholerae. Bulletin of the World Health Organization 1969;40(2):187-97. [PMC free article] [PubMed]
Mosley 1969b {published data only}
- Mosley WH, McCormack WM, Fahimuddin M, Aziz KM, Rahman AS, Chowdhury AK, et al. Report of the 1966-67 cholera vaccine field trial in rural East Pakistan. I. Study design and results of the first year of observation. Bulletin of the World Health Organization 1969;40(2):177-85. [PMC free article] [PubMed]
Mosley 1970 {published data only}
- Mosley WH, Woodward WE, Aziz KM, Rahman AS, Chowdhury AK, Ahmed A, et al. The 1968-1969 cholera-vaccine field trial in rural East Pakistan. Effectiveness of monovalent Ogawa and Inaba vaccines and a purified Inaba antigen, with comparative results of serological and animal protection tests. The Journal of Infectious Diseases 1970;121:Suppl 121:1-9. [DOI] [PubMed]
Mosley 1972 {published data only}
- Mosley WH, Aziz KM, Mizanur Rahman AS, Alauddin Chowdhury AK, Ahmed A, Fahimuddin M. Report of the 1966-67 cholera vaccine trial in rural East Pakistan. Bulletin of the World Health Organization 1972;47(2):229-38. [PMC free article] [PubMed]
Mosley 1973 {published data only}
- Mosley WH, Aziz KM, Rahman AS, Chowdhury AK, Ahmed A. Field trials of monovalent Ogawa and Inaba cholera vaccines in rural Bangladesh--three years of observation. Bulletin of the World Health Organization 1973;49(4):381-7. [PMC free article] [PubMed]
Nimbkar 1975 {published data only}
- Nimbkar YS, Karbhari RS, Cherian S, Chanderkar NG, Bhamaria RP, Ranadive PS, et al. Antibody response to two cholera vaccines in volunteers. Progress in Drug Research 1975;19:544-62. [PubMed] [Google Scholar]
Olsson 2006 {published data only}
Oseasohn 1965 {published data only}
Paineau 2008 {published data only}
Pal 1980 {published data only}
- Pal SC, Deb BC, Sen Gupta PG, De SP, Sircar BK, Sen D, et al. A controlled field trial of an aluminum phosphate-adsorbed cholera vaccine in Calcutta. Bulletin of the World Health Organization 1980;58(5):741-5. [PMC free article] [PubMed]
Peltola 1977 {published data only}
- Peltola H, Ruutu P, Palomäki H, Kaukinen K, Aho K. [Intracutaneous vaccination technic with less side effects against typhoid and cholera]. Duodecim; lääketieteellinen aikakauskirja 1977;93(7):431-8. [PubMed]
Peltola 1989 {published data only}
- Peltola H, Siitonen A, Kyronseppa H, Simula I, Mattila L, Oksanen P, et al. Prevention of travellers' diarrhoea by oral b-subunit/whole-cell cholera vaccine. Lancet 1991;338:1285-9. [DOI] [PubMed] [Google Scholar]
Peltola 1991 {published data only}
Philippines 1965 {published data only}
- Philippines Cholera Committee. A controlled field trial of the effectiveness of cholera and cholera El Tor vaccines in the Philippines. Preliminary report. Bulletin of the World Health Organization 1965;32(5):603-25. [PMC free article] [PubMed]
Pitisuttithum 2001 {published data only}
Qadri 2003 {published data only}
- Qadri F, Ahmed T, Ahmed F, Bradley Sack R, Sack DA, Svennerholm AM. Safety and immunogenicity of an oral, inactivated enterotoxigenic Escherichia coli plus cholera toxin B subunit vaccine in Bangladeshi children 18-36 months of age. Vaccine 2003;2(21):19-20. [DOI] [PubMed] [Google Scholar]
Qadri 2004 {published data only}
Qadri 2006 {published data only}
- Qadri F, Ahmed T, Ahmed F, Begum YA, Sack DA, Svennerholm AM. Reduced doses of oral killed enterotoxigenic Escherichia coli plus cholera toxin B subunit vaccine is safe and immunogenic in Bangladeshi infants 6-17 months of age: dosing studies in different age groups. Vaccine 2006;24(10):1726-33. [DOI] [PubMed]
Quiding‐Jarbrink 2001 {published data only}
- Quiding-Jarbrink M, Lonroth H, Ahlstedt I, Holmgren J, Svennerholm AM. Human gastric B cell responses can be induced by intestinal immunisation. Gut 2001;49(4):512-8. [DOI] [PMC free article] [PubMed]
Rao 2002 {published data only}
Rudin 1998 {published data only}
- Rudin A, Johansson EL, Bergquist C, Holmgren J. Differential kinetics and distribution of antibodies in serum and nasal and vaginal secretions after nasal and oral vaccination of humans. Infection and Immunity 1998;66(7):3390-6. [DOI] [PMC free article] [PubMed]
Rudin 1999 {published data only}
- Rudin A, Riise GC, Holmgren J. Antibody responses in the lower respiratory tract and male urogenital tract in humans after nasal and oral vaccination with cholera toxin B subunit. Infection and Immunity 1999;67(6):2884-90. [DOI] [PMC free article] [PubMed]
Sack 1991 {published data only}
- Sack DA, Clemens JD, Huda S, Harris JR, Khan MR, Chakraborty J, et al. Antibody responses after immunization with killed oral cholera vaccines during the 1985 vaccine field trial in Bangladesh. Journal of Infectious Diseases 1991;164(2):407-11. [DOI] [PubMed] [Google Scholar]
Sack 2007 {published data only}
Sanchez 1993b {published data only}
- Sanchez JL, Trofa AF, Taylor DN, Kuschner RA, DeFraites RF, Craig SC, et al. Safety and immunogenicity of the oral, whole cell/recombinant b subunit cholera vaccine in North American volunteers. Journal of Infectious Diseases 1993;167(6):1446-9. [DOI] [PubMed] [Google Scholar]
Sanchez 1994 {published data only}
- Sanchez J, Begue R, Gaillour A, Cardenas V, et al. Feasibility of an efficacy trial of the whole cell plus recombinant B subunit (WC/rBS) oral cholera vaccine in Lima, Peru. [abstract]. AmericanJournal of Tropical Medicine and Hygiene 1994;51:216.
Saroso 1978 {published data only}
- Saroso JS, Bahrawi W, Witjaksono H, Budiarso RL, Brotowasisto, Bencic Z, et al. A controlled field trial of plain and aluminium hydroxide-adsorbed cholera vaccines in Surabaya, Indonesia, during 1973--75. Bulletin of the World Health Organization 1978;56(4):619-27. [PMC free article] [PubMed]
Savarino 1998 {published data only}
- Savarino SJ, Brown FM, Hall E, Bassily S, Youssef F, Wierzba T, Peruski L, El-Masry NA, Safwat M, Rao M, Jertborn M, Sevennerholm A-M, Lee YJ, Clemens JD. Safety and immunogenicity of an oral, killed enterotoxigenic E.coli-cholera toxin B subunit vaccine in Egyptian adults.. J Infect Dis 1998;177:796-9. [DOI] [PubMed] [Google Scholar]
Savarino 1999 {published data only}
Savarino 2002 {published data only}
- Savarino SJ, Hall ER, Bassily S, Wierzba TF, Youssef FG, Peruski LF, et al. Introductory evaluation of an oral, killed whole cell vaccine in trial to avoid misclassification. Pediatric Infectious Disease Journal 2002;21(4):322-30. [DOI] [PubMed] [Google Scholar]
Sommer 1973 {published data only}
- Sommer A, Khan M, Mosley WH. Efficacy of vaccination of family contacts of cholera cases. Lancet 1973;1(814):1230-2. [DOI] [PubMed] [Google Scholar]
SonLa 2007 {published data only}
- SonLa Study Group. Using a fingerprint recognition system in a vaccine trial to avoid misclassification. Bulletin of the World Health Organisation 2007;85(1):64-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stellfeld 2004 {published data only}
- Stellfeld M. [Dukoral. Oral vaccine against cholera]. Ugeskr Laeger 2004;166(47):4251-3. [PubMed]
Sumarokov 1974 {published data only}
- Sumarokov AA, Lelikov VL, Dzhaparidze MN, Karaeva LT, Derteva II. Study of the immunogenicity and immunological effectiveness of choleragen anatoxin (data from a controlled epidemiological experiment). II. The characteristics of choleragen anatoxin immunogenicity compared with corpuscular cholera vaccines administered by syringe and by using a jet injector [zuchenie reaktogennosti i immunologichesko éffektivnosti kholerogena-anatoksina (materialy kontroliruemogo épidemiologicheskogo opyta). Soobshchenie II. Kharakteristika immunogennosti kholerogena-anatoksina v sravnenii s korpuskuliarnymi kholernymi vaktsinami pri ikh vvedenii shpritsem i s pomoshch]. Zhurnal mikrobiologii, epidemiologii, i immunobiologii 1974;(11):31-7. [PubMed]
Sumarokov 1978 {published data only}
- Sumarokov AA, Ivanov NR, Lelikov VL, Dzhaparidze MN, Karaeva LT, Derteva II, et al. Reactogenic properties and immunological efficacy of oral cholera chemical vaccine in a limited controlled revaccination trial in volunteers. Zhurnal Mikrobiologii, Epidemiologii i Immunobiologii 1978;12:87-92. [PubMed] [Google Scholar]
Sumarokov 1990 {published data only}
- Sumarokov AA, Ivanov NR, Dzhaparidze MN, Reznikov IuB, Rystsova EA, Nikitina GP, et al. [The determination of the optimal inoculation dose of an oral cholera chemical bivalent vaccine in a controlled experiment]. Zhurnal mikrobiologii, epidemiologii, i immunobiologii 1990;(12):55-62. [PubMed]
Sumarokov 1991 {published data only}
- Sumarokov AA, Ivanov NR, Dzhaparidze MN, Rystsova EA, Reznikov IuB, Matusevich LIa, et al. [The characteristics of the reactogenicity and immunological activity of a new cholera bivalent chemical vaccine based on the results of controlled trials]. Zhurnal mikrobiologii, epidemiologii, i immunobiologii 1991;(7):55-8. [PubMed]
Sumarokov 1993 {published data only}
- Sumarokov AA, Dzhaparidze MN, Eliseev IuIu, Nikitina GP, Poliakov KA, Kazakova ES, et al. [The determination of the optimal inoculation dose of an oral cholera bivalent chemical vaccine in a controlled trial of the vaccination of children and adolescents]. Zhurnal mikrobiologii, epidemiologii, i immunobiologii 1993;(5):55-60. [PubMed]
Suntharasamai 1992 {published data only}
Svennerholm 1981 {published data only}
Svennerholm 1984 {published data only}
- Svennerholm AM, Gothefors L, Sack DA, Bardhan PK, Holmgren J. Local and systemic antibody responses and immunological memory in humans after immunization with cholera B subunit by different routes. Bulletin of the World Health Organization 1984;62(6):909-18. [PMC free article] [PubMed]
Tacket 1992 {published data only}
Tacket 1995a {published data only}
- Tacket CO, Losonsky G, Nataro JP, Wasserman SS, Cryz SJ, Edelman R, et al. Extension of the volunteer challenge model to study South American cholera in a population of volunteers predominantly with blood group antigen O. Transactions of the Royal Society of Tropical Medicine and Hygiene 1995;89(1):75-7. [DOI] [PubMed]
Tacket 1995b {published data only}
Tacket 1998 {published data only}
- Tacket CO, Taylor RK, Losonsky G, Lim Y, Nataro JP, Kaper JB, et al. Investigation of the roles of toxin-coregulated pili and mannose- sensitive hemagglutinin pili in the pathogenesis of Vibrio cholerae O139 infection. Infection and Immunity 1998;66(2):692-5. [DOI] [PMC free article] [PubMed]
Taylor 1994 {published data only}
Taylor 1997 {published data only}
- Taylor DN, Tacket CO, Losonsky G, Castro O, Gutierrez J, Meza R, et al. Evaluation of a bivalent (CVD 103-HgR/CVD 111) live oral cholera vaccine in adult volunteers from the United States and Peru. Infection and Immunity 1997;65(9):3852-6. [DOI] [PMC free article] [PubMed]
Taylor 1999b {published data only}
- Taylor DN, Sanchez JL, Castro JM, Lebron C, Parrado CM, Johnson DE, et al. Expanded safety and immunogenicity of a bivalent, oral, attenuated cholera vaccine, CVD 103-HgR plus CVD 111, in United States military personnel stationed in Panama. Infection and Immunity 1999;67(4):2030-4. [DOI] [PMC free article] [PubMed]
Thiem 2006 {published data only}
- Thiem VD, Deen JL, Seidlein L, Canh do D, Anh DD, Park JK, et al. Long-term effectiveness against cholera of oral killed whole-cell produced in Vietnam. Vaccine 2006;24(20):4297-303. [DOI] [PubMed] [Google Scholar]
Von Seidlein 2007 {published data only}
- Von Seidlein L, Vu DT, Dang DA, Do GC, Puri M, Gupta V, et al. Using a fingerprint recognition system in a vaccine trial to avoid misclassification. Bulletin of the World Health Organization 2007;85(1):64-7. [DOI] [PMC free article] [PubMed]
Wassén 1996 {published data only}
Wassen 2005 {published data only}
- Wassen L, Jertborn M. Kinetics of local and systemic immune responses after vaginal immunization with recombinant cholera toxin B subunit in humans. Clinical and Diagnostic Laboratory Immunology 2005;12(3):447-52. [DOI] [PMC free article] [PubMed]
Wassen 2006 {published data only}
- Wassen L, Jertborn M. Influence of exogenous reproductive hormones on specific antibody production in genital secretions after vaginal vaccination with recombinant cholera toxin B subunit in humans. Clinical and Vaccine Immunology 2006;13(2):202-7. [DOI] [PMC free article] [PubMed]
Wasserman 1993 {published data only}
Wiedermann 2000 {published data only}
- Wiedermann G, Kollaritsch H, Kundi M, Svennerholm AM, Bjare U. Double-blind, randomized, placebo controlled pilot study evaluating efficacy and reactogenicity of an oral ETEC B-subunit-inactivated whole cell vaccine against travelers' diarrhea (preliminary report). Journal of Travel Medicine 2000;7(1):27-9. [DOI] [PubMed]
Additional references
Anh 2011
- Anh DD, Lopez AL, Thiem VD, Grahek SL, Duong TN, Park JK, et al. Use of Oral Cholera Vaccines in an Outbreak in Vietnam: A Case Control Study. PLoS Neglected Tropical Diseases 2011;5(1):e1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bhadra 1994
- Bhadra RK, Dasgupta U, Das J. Cholera vaccine: developmental strategies and problems. Indian Journal of Biochemistry and Biophysics 1994;31:441-48. [PubMed] [Google Scholar]
Calain 2004
- Calain P, Chaine J-P, Johnson E, Hawley M-L, O'Leary MJ, Oshitani H, et al. Can oral cholera vaccination play a role in controlling a cholera outbreak? Vaccine 2005;22(19):2444-51. [DOI] [PubMed] [Google Scholar]
Clemens 2001
- Clemens JD, Sack DA. Misleading Negative Findings in a Field Trialof Killed, Oral Cholera Vaccine in Peru (Comment). Journal of Infectious Diseases 2001;183:1306-8. [DOI] [PubMed] [Google Scholar]
Girard 2005
- Girard MP, Steele D, Chaignat C-L, Kieny MP. A review of vaccine research and development: human enteric infections. Vaccine 2005;24(15):2732-50. [DOI] [PubMed] [Google Scholar]
Graves 2001
- Graves P, Deeks J, Demicheli V, Pratt M, Jefferson T. Vaccines for preventing cholera. Cochrane Database of Systematic Reviews 2001, Issue 1. Art. No: CD000974. [DOI: 10.1002/14651858.CD000974] [DOI] [Google Scholar]
Graves 2010
- Graves P, Deeks J, Demicheli V, Jefferson T. Vaccines for preventing cholera: killed whole cell or other subunit vaccines (injected). Cochrane Database of Systematic Reviews 2010, Issue 1. Art. No: CD000974. [DOI: 10.1002/14651858.CD000974] [DOI] [PMC free article] [PubMed] [Google Scholar]
Harris 2005
- Harris JB, Khan AI, LaRocque RC, Dorer DJ, Chowdhury F, Faruque ASG, et al. Blood Group, Immunity, and Risk of Infection with Vibrio cholerae in an Area of Endemicity. Infection and Immunity 2005;73(11):7422-7427. [DOI] [PMC free article] [PubMed] [Google Scholar]
Heymann 2008
- Heyman DL. Control of Communicable Diseases Manual. 19th edition. Washington: American Public Health Association, 2008. [Google Scholar]
Higgins 2008
- Higgins JPT, Altman DG (editors). Cochrane Handbook of Systematic Reviews of Intervention. Version 5.0.0. The Cochrane Collaboration, 2008. [Google Scholar]
Hill 2006
- Hill DR, Ford R, Lallo DG. Oral cholera vaccines: use in clinical practice. Lancet infectious diseases 2006;6:361-573. [DOI] [PubMed] [Google Scholar]
Holmgren 2005
- Holmgren J, Adamson J, Anjuere F, Clemens J, Czerkinsky C, Flack C-F et al. Mucosal adjuvants and anti-infection and anti-immunopathology vaccines based on cholera toxin, cholera toxin B subunit and CpG DNA. Immunology letters 2005;97(2):181-188. [DOI] [PubMed] [Google Scholar]
Huilan 1991
- Huilan S, Zhen LG, Mathan MM, Mathew MM, Olarte J, Espejo R et al. Etiology of acute diarrhoea among children in developing countries: a multicentre study in five countries. Bulletin of the World Health Organization 1991;69:549-55. [PMC free article] [PubMed] [Google Scholar]
Lucas 2005
- Lucas ME, Deen JL, Seidlein L, Wang XY, Ampuero J, Puri M et al. Effectiveness of mass cholera vaccination in Beira, Mozambique. New England Journal of Medicine 2005;352(8):757-67. [DOI] [PubMed] [Google Scholar]
Review Manager 5 [Computer program]
- Review Manager (RevMan). Version 5.0. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2008.
Reyburn 2011
- Reyburn R, Deen JL, Grais RF, Bhattacharya S, Sur D, Lopez AL, et al. The case for reactive mass oral cholera vaccinations. PLoS Neglected Tropical Diseases 2011;5(1):e952. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ryan 2011
- Ryan ET. The cholera pandemic, still with us after half a century: time to rethink. PLoS Neglected Tropical Diseases 2011;5(1):e1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sack 2004
- Sack DA, Sack RB, Nair GB, Siddique AK. Cholera. Lancet 2004;363:223-33. [DOI] [PubMed] [Google Scholar]
Sanchez 1997
- Sanchez J, Taylor DN. Cholera. Lancet 1997;349:1825-30. [DOI] [PubMed] [Google Scholar]
Taylor 2001
- Taylor DN, Sanchez J, Cardenas V, Gilman RE, Sadoff J. Misleading negative findings in a field trial of killed, oral cholera vaccine in Peru (Authors reply). Journal of Infectious Diseases 2001;183:1308-9. [DOI] [PubMed] [Google Scholar]
WHO 2000a
- World Health Organization. Fact Sheet No. 103: Cholera. http://www.who.int/mediacentre/factsheets/fs107/en/ Revised March 2000.
WHO 2000b
- World Health Organization Department of Communicable Disease Surveillance and Response. WHO report on global surveillance of epidemic-prone infectious diseases. http://www.who.int/csr/resources/publications/surveillance/en/cholera.pdf 2000;Chapter 4:39-43.
WHO 2006a
- World Health Organization. Cholera 2005. Weekly epidemiological record 2006;81:297-308. [Google Scholar]
WHO 2006b
- World Health Organization Global Task Force on Cholera Control. Oral cholera vaccine use in complex emergencies: what next? Report of a WHO meeting, Cairo, Egypt 14-16 December 2005;WHO/CDS/NTD/IDM/2006.2.
WHO 2006c
- World Health Organization. The use of two-dose oral vaccine in the context of major natural disaster: report of a mass vaccination campaign in Aceh Province, Indonesia 2005. http://www.who.int/topics/cholera/publications/final_tsunami.pdf 2006.
WHO 2009
- WHO. Outbreak News: Cholera, Zimbabwe - update. Weekly Epidemiological Record 2009;84:109-10. [Google Scholar]
WHO 2010a
- WHO. Outbreak news: Cholera, Haiti – update. Weekly Epidemiological Record 2010;85:489-90. [Google Scholar]
WHO 2010b
- WHO. Cholera vaccines:WHO position paper. Weekly Epidemiological Record 2010;85:117-28. [Google Scholar]


