Abstract
Background
Out-of-office blood pressure (BP) is recommended for diagnosing hypertension in primary care due to its increased accuracy compared to office BP. Moreover, being diagnosed as hypertensive has previously been linked to lower wellbeing. There is limited evidence regarding the acceptability of out-of-office BP and its impact on wellbeing.
Aim
To assess the acceptability and psychological impact of out-of-office monitoring in people with suspected hypertension.
Design and setting
A pre- and post-evaluation of participants with elevated (≥130 mmHg) systolic BP, assessing the psychological impact of 28 days of self-monitoring followed by ambulatory BP monitoring for 24 hours.
Method
Participants completed standardised psychological measures pre- and post-monitoring, and a validated acceptability scale post-monitoring. Descriptive data were compared using χ2 tests and binary logistic regression. Pre- and post-monitoring comparisons were made using the paired t–test and Wilcoxon signed rank test.
Results
Out-of-office BP monitoring had no impact on depression and anxiety status in 93% and 85% of participants, respectively. Self-monitoring was more acceptable than ambulatory monitoring (n = 183, median 2.4, interquartile range [IQR] 1.9–3.1 versus median 3.2, IQR 2.7–3.7, P<0.01). When asked directly, 48/183 participants (26%, 95% confidence interval [CI] = 20 to 33%) reported that self-monitoring made them anxious, and 55/183 (30%, 95% CI = 24 to 37%) reported that ambulatory monitoring made them anxious.
Conclusion
Out-of-office monitoring for hypertension diagnosis does not appear to be harmful. However, health professionals should be aware that in some patients it induces feelings of anxiety, and self-monitoring may be preferable to ambulatory monitoring.
Keywords: ambulatory monitoring, anxiety, blood pressure, depression, self-monitoring, self-reported
INTRODUCTION
Out-of-office blood pressure (BP) measurement plays an increasing role in the diagnosis and management of hypertension.1,2 Multiple measurements taken by self- or ambulatory monitoring in the patient’s normal environment provide a more accurate estimate of BP, free from the white coat effect and masked hypertension.3 Out-of-office measurements are also a better predictor of long-term prognosis, including cardiovascular events and mortality, compared to measurements taken in the clinician’s office.4,5 Guidelines in the UK and US recommend the use of out-of-office BP measurements to confirm a diagnosis of hypertension.6–8
Although out-of-office BP measurement may offer improved diagnostic accuracy, there is currently limited evidence regarding its acceptability to patients. A systematic review and thematic synthesis for the purposes of ongoing monitoring — rather than diagnosis — found that out-of-office BP measurement empowered patients and enabled them to attribute lifestyle changes to changes in their BP.9 In a cross-sectional survey of patients with and without known hypertension, the acceptability of self-monitoring varied between ethnic groups, a finding which has implications for its implementation, accuracy estimation, and impact on practice.10
The experience of out-of-office monitoring is likely to differ in undiagnosed patients, partly due to the different motivation for self-monitoring (that is, to confirm or disprove their hypertensive status, rather than to improve BP control), as well as differences in familiarity with self-monitoring. Being labelled as hypertensive has previously been linked to lower wellbeing, including anxiety and depression,11 but little is known of whether this is linked to the process of screening or the subsequent diagnosis. The aims of this study were therefore to explore changes in anxiety and depression status, and the acceptability of undertaking out-of-office BP monitoring by patients in primary care suspected of having hypertension.12
METHOD
Study design and participants
GPs from four surgeries identified consecutive patients aged 40–85 years presenting with a single office systolic BP between 130 and 179 mmHg. Those diagnosed with and/or treated for hypertension, atrial fibrillation, autonomic failure, or dementia, or unwilling to monitor their own BP were excluded.
How this fits in
There is an increasing role for out-of-office BP monitoring to diagnose hypertension in primary care, but very little is known about its acceptability and the psychological impact on people with suspected hypertension. In this study, out-of-office BP monitoring had no impact on overall anxiety or depression status using validated scores, but some individuals reported that self-monitoring (26%) and ambulatory monitoring (30%) made them anxious. Self-monitoring was more acceptable than ambulatory monitoring. Out-of-office monitoring for hypertension diagnosis does not appear to be harmful. However, in some patients it induces feelings of anxiety and this should be carefully monitored by health professionals.
Test procedures
Identified patients were invited to a baseline assessment conducted by trained clinic staff to confirm their eligibility, obtain informed consent, and collect baseline data, including a questionnaire.12 Following brief training, participants were asked to monitor their BP at home for 28 days (twice in the morning, twice in the evening) using an automated, bluetooth-enabled BP monitor. After 28 days of self-monitoring, participants returned to the clinic where they were fitted with an ambulatory BP monitor (ABPM) for 24 hours and asked to complete a follow-up questionnaire on its removal.
The psychosocial measures collected via the baseline and follow-up questionnaires were: the hospital anxiety and depression score (HADS), a 14-item scale with half of the items relating to either anxiety or depression;13 the National Institute for Health and Care Excellence (NICE) depression screening tool,14 comprising two questions; and the EQ-5D, which is made up of two components — one describing a person’s health state via scoring five dimensions including anxiety/depression, and the second a self-rated overall health status reported using the visual analogue scale.15 These generic instruments were chosen, rather than those specifically designed for patients with hypertension, as the cohort contained participants who were normotensive and hypertensive. The follow-up questionnaire also contained a validated scale rating the acceptability of aspects of the experience of self- and ambulatory monitoring.16 The questionnaires included space for study participants to write free-text comments.
Data cleaning
The authors included participants who returned both questionnaires in the pre- and post-monitoring comparison of standardised psychological measures. Those who completed the first questionnaire >7 days after their baseline assessment were excluded. For the investigation into acceptability, all participants who returned their follow-up questionnaire and completed all items of the score were eligible.
Analysis
Statistical analyses of the questionnaire data were performed in SPSS (version 24). Comparisons of descriptive data were conducted using χ2 tests for categorical variables and binary logistic regression for continuous variables. Pre- and post-monitoring comparisons were made using the paired t–test and the related samples Wilcoxon signed rank test.
Responses to the HADS items were scored 0–3. A total score of >7 for each subscale was used to define the presence of depression or anxiety,13 while a positive answer to either of the NICE screening tool questions indicated the presence of depression.14 For EQ-5D positive responses, ‘some problems’ and ‘severe problems’ were combined into ‘any problems’ and compared to ‘no problems’.17
The authors compared their acceptability findings to those from previous studies that had used the validated scale.10,16,18 Based on previous studies, the acceptability score was calculated as the average of all 13 individual items, with scoring reversed for the three positively worded items (item 11, ‘It was worth the trouble to get accurate readings’; item 12, ‘I felt in control’; and item 13, ‘A good way to save doctor/nurse time’). The authors used mean scores to enable comparison to the previously published data.
The authors analysed free-text questionnaire answers using a pre-specified framework based on the domains of the validated acceptability scale in order to contextualise the quantitative data.
RESULTS
Pre–post BP monitoring comparison
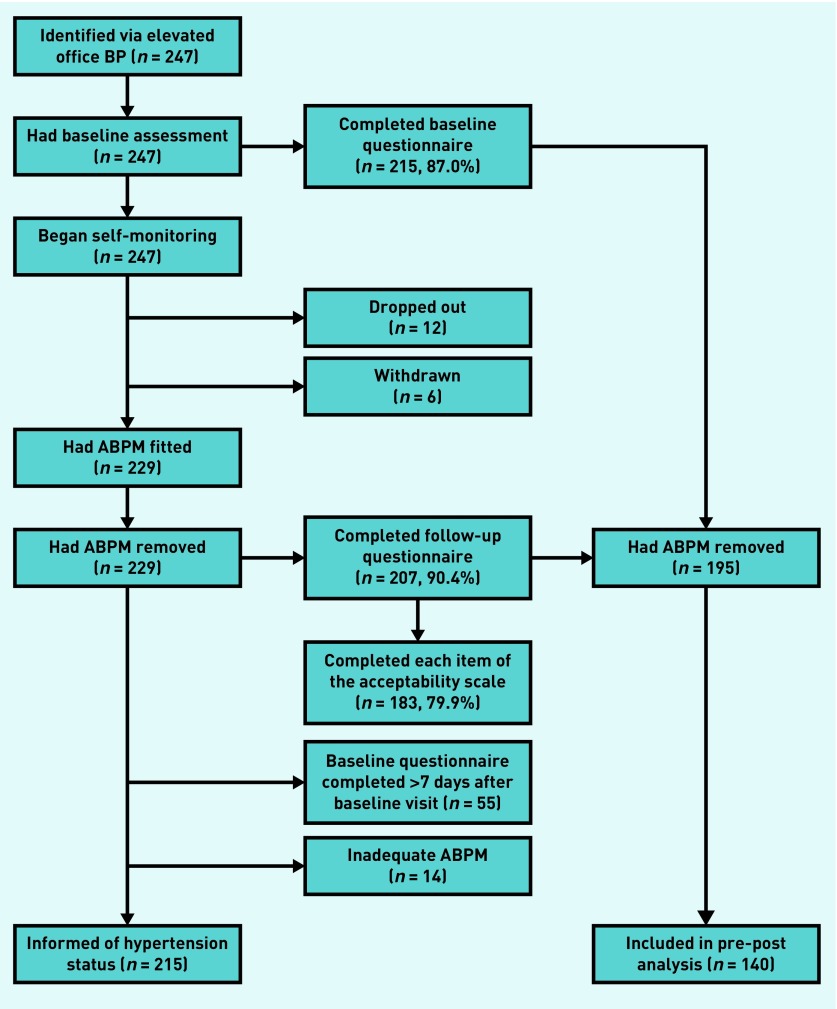
From the total cohort of 247 patients, 140 participants completed both the baseline questionnaire within 7 days of their baseline assessment and the follow-up questionnaire (Figure 1). Participants’ mean age was 57.7 years (standard deviation [SD] 9.8), and 77 (55.0%) were female (Table 1). Older and female participants were more likely to be eligible for inclusion in this analysis (difference in percentage of females +12.9%, P = 0.04, difference in mean age +3.3 years, P = 0.01). There was no significant difference in hypertension status, based on diagnosis via ambulatory BP, between the included and excluded participants (52.7% versus 55.5%, P = 0.69) (Table 1).
Figure 1.
Flow diagram of participants enrolled in the study. ABPM = ambulatory blood pressure monitoring. BP = blood pressure.
Table 1.
Characteristics of study participants
| Total cohort (n= 247) | Pre–post comparisons (n= 140) | Acceptability comparisons (n= 183) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean (SD) | 95% CI | n | Mean (SD) | 95% CI | P-value a | n | Mean (SD) | 95% CI | P-value | |
| Age | 247 | 56.2 (9.8) | 55.0 to 57.5 | 140 | 57.7 (9.8) | 56.0 to 59.3 | 0.01 | 183 | 56.4 (9.7) | 55.0 to 57.8 | 0.37 |
| n | Number (%) | 95% CI of % | n | Number (%) | 95% CI of % | P-value a | n | Number (%) | 95% CI of % | P-value | |
| Female | 247 | 122 (49.4) | 43.2 to 55.6 | 140 | 77 (55.0) | 46.7 to 63.1 | 0.04 | 183 | 90 (49.2) | 42.0 to 56.4 | 0.91 |
| Hypertensiveb | 203 | 109 (53.7) | 46.8 to 60.5 | 131 | 69 (52.7) | 44.1 to 61.1 | 0.69 | 171 | 90 (52.6) | 45.2 to 60.0 | 0.48 |
P-value for comparison with excluded cohort members.
Available for completers of the diagnostic study only (mean daytime ambulatory BP >135 mmHg systolic and/or 85 mmHg diastolic). CI = confidence interval. SD = standard deviation.
Change in depression and anxiety status
Female participants were significantly more likely than males to be classified by HADS as depressed or anxious at baseline or follow-up (Table 2). These findings were replicated across the NICE depression screening tool and the anxiety or depression dimension of EQ-5D (further information is available from the authors on request).
Table 2.
The proportion of cohort members anxious or depressed at baseline and follow-up, assessed using the hospital anxiety and depression scale (HADS)
| Baseline | Follow-up | |||||
|---|---|---|---|---|---|---|
| n | n, % | P-value | n | n, % | P-value | |
| Depressed | ||||||
| Total | 139 | 22 (15.8) | 136 | 14 (10.3) | ||
| Male | 62 | 5 (8.1) | <0.001 | 60 | 2 (3.3) | 0.018 |
| Female | 77 | 17 (22.1) | <0.001 | 76 | 12 (15.8) | 0.018 |
| Anxious | ||||||
| Total | 138 | 48 (34.8) | 137 | 37 (27.0) | ||
| Male | 62 | 13 (21.0) | 0.002 | 61 | 9 (14.8) | 0.004 |
| Female | 76 | 35 (46.1) | 0.002 | 76 | 28 (36.8) | 0.004 |
The HADS depression and anxiety status of most of the 135 participants who had data did not change during the study (Tables 3a and 3b). The status of nine (6.7%, 95% CI = 3.3 to 11.8%) participants classified as depressed at baseline improved, and they were not depressed at follow-up; 15 (11.1%, 95% CI = 6.6 to 17.2%) were recorded as anxious at baseline and not anxious at follow-up, based on HADS. Conversely, one person (0.7%, 95% CI = 0.1 to 3.4%) changed category in the opposite direction to become depressed at follow-up, and five people (3.7%, 95% CI = 1.4 to 7.9%) were categorised as not anxious at baseline and anxious at follow-up.
Table 3a.
Change in HADS depression status (n = 135)
| Baseline | |||||
|---|---|---|---|---|---|
| Not depressed | Depressed | ||||
| n | % (95% CI) | n | % (95% CI) | ||
| Follow-up | Not depressed | 112 | 83.0 (76.0 to 88.6) | 9 | 6.7 (3.3 to 11.8) |
| Depressed | 1 | 0.7 (0.1 to 3.4) | 13 | 9.6 (5.5 to 15.5) | |
CI = confidence interval. HADS = hospital anxiety and depression scale.
Table 3b.
Change in HADS anxiety status (n = 135)
| Baseline | |||||
|---|---|---|---|---|---|
| Not anxious | Anxious | ||||
| n | % (95% CI) | n | % (95% CI) | ||
| Follow-up | Not anxious | 83 | 61.5 (53.1 to 69.4) | 15 | 11.1 (6.6 to 17.2) |
| Anxious | 5 | 3.7 (1.4 to 7.9%) | 32 | 23.7 (17.1 to 31.4) | |
CI = confidence interval. HADS = hospital anxiety and depression scale.
Due to the small sample, it was difficult to assess the characteristics of those whose status improved (24 individuals in total). In terms of the depression subscale, 6/9 (66.7%, 95% CI = 34.8% to 89.6%) were female, and 7/9 (77.8%, 95% CI = 45.6 to 95.1%) were subsequently found not to be hypertensive. For anxiety, 9/15 (60.0%, 95% CI = 35.3% to 81.2%) were female, and 8/15 (53.3%, 95% CI = 31.9% to 79.7%) were subsequently found not to be hypertensive (data not shown).
On average, there was no change in the paired HADS depression subscale score (n = 135, median 0.0, interquartile range [IQR] 0.0–2.0), and a slight improvement in the anxiety subscale score (n = 135, median 1.0, IQR 1.0–4.0) during the period of out-of–office monitoring (data not shown).
Change in EQ-5D
The median score of the self-rated global health status measured using the visual analogue scale of the EQ-5D was 80/100 (IQR 75–90) at baseline, improving to 85 (IQR 75–92) at follow-up (P = 0.05, Wilcoxon rank test); less than the proposed minimal clinically important difference of 10 points.19 There was no significant change in the number of participants reporting problems in mobility, usual activities, and pain dimensions of EQ-5D at follow-up (further information is available from the authors upon request).
Acceptability of self-versus ambulatory monitoring
Participant characteristics
Of the 229 participants that received the follow-up questionnaire, 183 (79.9%) provided complete acceptability data (Figure 1). The mean age of these participants was 56.4 years (SD 9.7), and 90 (49.2%) were female (Table 1). There were no significant differences between these participants and those who failed to provide acceptability data (Table 1).
Quantitative results
Overall, self-monitoring was rated as more acceptable than ambulatory monitoring (Table 4). Cohort members reported that ambulatory monitoring was associated with greater disturbance to home life, sleep, and work, and was more uncomfortable compared to self-monitoring.
Table 4.
Acceptability of different methods of out-of-office blood pressure monitoring (n = 183)
| Self-monitoring | Ambulatory monitoring | Paired difference | ||
|---|---|---|---|---|
| Median score (IQR) | Median score (IQR) | Median (IQR) | P-value | |
| 1. It made me anxious | 2.0 (1.0–5.0) | 2.0 (2.0–5.0) | 0.0 (−1.0–0.0) | 0.13 |
| 2. It disturbs home life or everyday activities | 2.0 (2.0–5.0) | 5.0 (2.0–5.0) | −1.0 (−3.0–0.0) | <0.01 |
| 3. It disturbs sleep | 2.0 (1.0–3.0) | 5.0 (4.0–6.0) | −3.0 (−4.0–0.0) | <0.01 |
| 4. It disturbs work | 2.0 (1.0–4.0) | 4.0 (3.0–5.0) | −1.0 (−3.0– −1.0) | <0.01 |
| 5. It was uncomfortable | 2.0 (2.0–5.0) | 5.0 (3.0–6.0) | −1.0 (−3.0– −1.0) | <0.01 |
| 6. I felt self-conscious | 2.0 (1.0–3.0) | 3.0 (2.0–5.0) | 0.0 (−2.0–0.0) | <0.01 |
| 7. I felt unsure what to do | 2.0 (1.0–2.0) | 2.0 (2.0–2.0) | 0.0 (0.0–0.0) | <0.01 |
| 8. There is a lot of waiting around | 2.0 (2.0–5.0) | 2.0 (2.0–3.0) | 0.0 (0.0–1.0) | 0.06 |
| 9. It worried me knowing my BP | 2.0 (2.0–5.0) | 2.0 (2.0–4.0) | 0.0 (−1.0–1.0) | 0.73 |
| 10. It was difficult to remember to do it | 2.0 (1.0–2.0) | 2.0 (1.0–2.0) | 0.0 (0.0–1.0) | 0.02 |
| 11. It was worth the trouble to get accurate readings | 6.0 (6.0–7.0) | 6.0 (6.0–7.0) | 0.0 (0.0–1.0) | <0.01 |
| 12. I felt in control | 6.0 (4.0–6.0) | 5.0 (4.0–6.0) | 0.0 (0.0–1.0) | <0.01 |
| 13. A good way to save doctor/nurse time | 6.0 (6.0–7.0) | 6.0 (5.0–7.0) | 0.0 (0.0–0.0) | 0.01 |
| Acceptability scorea | 2.4 (1.9–3.1) | 3.2 (2.7–3.7) | −0.6 (−1.2– −0.1) | <0.01 |
Acceptability score is the mean of all 13 individual items, with scoring reversed for the positive items (11: accurate, 12: control, 13: good use of time). Lower scores indicate better acceptability. Ratings: 1 = strongly disagree. 2 = disagree. 3 = disagree slightly. 4 = unsure or not applicable. 5 = agree slightly. 6 = agree. 7 = agree strongly. BP = blood pressure. IQR = interquartile range.
For both measurement techniques, on average the cohort disagreed with the statement ‘it made me anxious’ (median 2.0, IQR 1.0–5.0 for both measurement modalities). However, 48 patients (26.2%, 95% CI = 19.7 to 32.8%), and 55 (30.1%, 95% CI = 23.5 to 36.6%) agreed with the statement to some extent for self- and ambulatory monitoring respectively (that is, scored ≥5). Females were more likely to agree that ambulatory monitoring was anxiety inducing than males (37.8% versus 22.6%, P = 0.03). A similar pattern was observed for self-monitoring, but was not statistically significant (31.1% versus 21.5%, P = 0.14) (data not shown).
In the other dimensions of acceptability investigated there were no statistically significant differences between the scores of males and females for self-monitoring. However, females were more likely to score ambulatory monitoring as making them feel self-conscious (median 4.5, IQR 2.0–6.0 versus median 2.0, IQR 2.0–5.0 for males and females, P<0.01), and less likely to describe themselves as feeling in control (median 5.0, IQR 3.0–6.0 versus median 5.0, IQR 4.0–6.0 for males and females, P = 0.05). Overall, female participants rated ambulatory monitoring as slightly less acceptable than male participants (median 3.3, IQR 2.7–3.9 versus median 3.0, IQR 2.69–3.6, P = 0.09) (data not shown).
When classified by their HADS status at follow-up, anxious cohort members rated both monitoring modalities as less acceptable than their non-anxious counterparts (self-monitoring: median 2.9, IQR 2.2–3.4 versus median 2.3, IQR 1.8–2.8, P<0.01; ambulatory monitoring: median 3.3, IQR 2.9–4.2 versus median 3.1, IQR 2.6–3.7, P = 0.01). A similar pattern was observed among depressed and non-depressed cohort members, though the difference was not statistically significant (further information is available from the authors upon request). Table 5 compares the acceptability findings to those from previously published studies. In each cohort, the mean score was lower (that is, more acceptable) for self-monitored BP than ambulatory BP.
Table 5.
Mean acceptability scores for out-of-office monitoring modalities
| Little 200216 | Wood 201610 | Lindroos 201618a | Present study | |||||
|---|---|---|---|---|---|---|---|---|
| n | Mean (SD) | n | Mean (95% CI) | n | Mean (SD) | n | Mean (SD) | |
| Self-monitoring | 153 | 2.67 (0.90) | 727 | 2.10 (2.0 to 2.2) | 223 | 2.20 (0.70) | 183 | 2.50 (0.83) |
| Ambulatory monitoring | 156 | 3.88 (0.82) | 715 | 2.90 (2.8 to 3.0) | 223 | 3.11 (0.93) | 183 | 3.17 (0.90) |
Altered the wording of item 6 from ‘I felt self-conscious’ to ‘I was more aware of my blood pressure level’. Acceptability score is the mean of all 13 individual items, with scoring reversed for the positive items (11: accurate, 12: control, 13: good use of time). Lower scores indicate better acceptability. CI = confidence interval. SD = standard deviation.
Qualitative results
Box 1 illustrates patients’ experiences of the acceptability of out-of-office BP monitoring. Participants did not provide any free-text comments for three of the categories/questions, namely how self-monitoring made them feel self-conscious, any difficulties they had remembering to self-monitor, or the time-saving benefits for clinicians.
Box 1.
Comments describing the acceptability of out-of-office blood pressure monitoring
|
BP monitoring made me anxious ‘I felt anxious one evening when I had a particularly high [self-monitoring] reading, although the feeling passed quickly.’ (ID229, M, 61 years, Anx−, Dep−) ‘I felt I was wearing a bomb with the 24-hour BP. No doubt the readings should correspond.’ (ID285, F, 58 years, Anx+, Dep+) ’24-hour monitor was very stressful, in my experience. Twice a day home monitoring less so, but still a factor … both systems are, in my view, hard to live with.’ (ID220, M, 60 years, Anx−, Dep−) |
|
BP monitoring disturbs home life/everyday activities ‘A largely enjoyable experience … with the twice-daily [self-monitoring] readings becoming part of everyday life!’ (ID240, M, 73 years, Anx−, Dep−) ‘The timing of morning and evening [self-monitoring readings] has been inconvenient and rushed at times.’ (ID220, M, 60 years, Anx−, Dep−) ‘The 24-hour monitoring was very disruptive … uncomfortable doing household tasks, etc. At one stage, I had to drive the car. I couldn’t stop when the time came for a reading, so very stressful.’ (ID173, F, 75 years, Anx−, Dep−) ‘You can do pilates class with one [the ambulatory monitor]! Takes thought.’ (ID257, F, 48 years, Anx−, Dep−) BP monitoring disturbs sleep ‘I was pleasantly surprised that the night time [ambulatory] monitoring did not disturb me too much.’ (ID001, F, 59 years, Anx−, Dep−) ‘I’m afraid I didn’t last through the night [with the ambulatory monitor]. I found it impossible to sleep, and couldn’t see how BP during a sleepless night could be useful.’ (ID178, F, 64 years, Anx−, Dep−) ‘I had to stop using the 24-hour monitor at 3am in the morning, as I found I could not sleep. Every time it activated, I woke up.’ (ID 110, M, 57 years, Anx−, Dep−) |
|
BP monitoring disturbs work ‘I work as a farm labourer, and found it difficult to work, so I had the day off [to undertake ambulatory monitoring].’ (ID042, M, 61 years, Anx−, Dep−) ‘It would have been inappropriate to wear it [the ambulatory monitor] at work, so I had to arrange to wear it on a Saturday.’ (ID148, F, 56 years, Anx+, Dep−) BP monitoring was uncomfortable ‘I didn’t realise how uncomfortable the 24-hour ABPM would be. I managed to cope, but I imagine some older people would feel quite upset by its intrusiveness.’ (ID083, M, 60 years, Anx+, Dep−) “Could someone invent a BP cuff that fits the shape of the arm, and does it need to be so wide? I had trouble with the cuff and monitor. I thought it was the way I used it, but the GP’s staff had the same trouble as I had.’ (ID261, F, 64 years, Anx−, Dep−) ‘I can’t see any way the [ambulatory] monitor could be made more comfortable or less disturbing. Anyway, it was only 24 hours.’ (ID214, F, 77 years, Anx−, Dep−) |
| BP monitoring made me feel self-conscious — no free-text comments |
|
I was unsure what to do when BP monitoring ‘Both devices threw up error codes, which I was not able to interpret or correct. This worried me that there was something wrong with my BP and/or pulse.’ (ID287, M, 46 years, Anx−, Dep−) |
|
There is a lot of waiting around when BP monitoring ‘I am lazy and casual, and find the BP [self] monitoring tedious and uncomfortable, and takes time which might be used for other things.’ (ID214, F, 77 years, Anx−, Dep−) ‘I had to stop what I was doing to make sure it [the ambulatory monitor cuff] didn’t slip or twist.’ (ID215, F, 40 years, Anx−, Dep+) Knowing my BP when monitoring worried me ‘The fact that you can see your [self-monitoring] results can in itself be worrying, and I wonder if it would be best if people were only told them later.’ (ID152, M, 60 years, Anx−, Dep+) ‘I found the home monitoring very instructive, and noticed how much difference stress or relaxation made to my blood pressure.’ (ID178, F, 64 years, Anx−, Dep−) “I was not able to see the measurements on it [the ambulatory monitor], as it was impossible to get it out from its pouch in time to read it before it disappeared, or it was too dark to see at night.’ (ID192, F, 70 years, Anx−, Dep−) It was difficult to remember to monitor my BP — no free-text comments |
|
It is worth the trouble to get accurate readings ‘I would say taking your blood pressure over the longer period was a much more accurate way to get [a] true reading of someone’s blood pressure than the 24-hour part of the trial.’ (ID150, M, 57 years, Anx−, Dep−) ‘The [self] monitor was so user friendly and completely unobtrusive, apart from 15/20 mins am and pm to use it — which is nothing to get results that might save a life!’ (ID051, F, 66 years, Anx n/a, Dep n/a) ‘I find it very reassuring that my blood pressure from home monitoring seems to be much lower than whenever it has been taken at my GP practice — where I always feel anxious. Hopefully, this will have saved the NHS a long-term prescription!’ (ID177, M, 55 years, Anx−, Dep−) |
|
I felt in control when BP monitoring ‘The [ambulatory] monitor did the job by itself; no question of the wearer being in control.’ (ID214, F, 77 years, Anx−, Dep−) BP monitoring is a good way to save doctor or nurse time — no free-text comments |
Quotes are identified by study ID number, sex, age, and hospital anxiety and depression score. Anx = hospital anxiety and depression score: anxiety subscale at follow-up. BP = blood pressure. Dep = hospital anxiety and depression score: depression subscale at follow-up. F = female. M = male. n/a = status not available. + = present. − = absent.
DISCUSSION
Summary
The authors sought to ascertain the impact of out-of-office monitoring on anxiety and depression status in patients with suspected hypertension, and found both of these remained unaltered for most participants when assessed using standardised, generic measures.
When asked directly about out-of-office monitoring, one-quarter of participants reported that self-monitoring made them feel anxious, and almost one-third reported that ambulatory monitoring, made them feel anxious. On average, self-monitoring was rated as more acceptable than ambulatory monitoring. Females found ambulatory monitoring less acceptable than men.
Out-of-office monitoring for hypertension diagnosis does not appear to be harmful. However, in some patients, it induces feelings of anxiety. Controlled studies using routine diagnostic protocols are needed to confirm the authors’ findings and identify which patient groups are affected.
Strengths and limitations
To the best of the authors’ knowledge, this is the first study to investigate the acceptability and psychological impact of out-of-office BP monitoring for diagnostic purposes using validated measures in a clinically relevant primary care population.
The study is not without limitations. Baseline psychological measures were collected after the participants had been identified as being potentially hypertensive and their GP had suggested participating in the study. This may have elevated baseline anxiety and depression scores, and explain the subsequent fall observed at follow-up. Furthermore, there was no control arm of patients with a raised office BP reading who did not undergo out-of-office-monitoring. Therefore, the authors cannot rule out the effect of regression to the mean.
Perhaps the biggest limitation is that participants underwent home monitoring followed by the 24-hour ABPM, which may have biased their recollections and acceptability scoring. The study collected the patient self-monitored BP readings via a bluetooth connection between the BP monitor and a mobile phone. This additional layer of technology — particularly in rural areas with limited mobile telephone network coverage — may have altered the acceptability of self-monitoring, most likely in a negative direction.
The cohort was predominately white.12 The Blood Pressure in different Ethnic Groups (BPEth) study found that the cross-sectional acceptability of BP monitoring varied between ethnic groups, with patients from minority ethnic groups rating office, ambulatory, and self-monitoring less favourably than white British participants.10 Therefore, these results may be of limited generalisability to patients from ethnic minority groups.
Comparison with existing literature
In the authors’ sample, female participants were more likely to be classified as depressed or anxious across the various measures used, reflecting general population data.20,21
Similarly to the current study, the TASMINH2 trial found that quality of life increased following a period of self-monitoring (and self-titration) by patients with hypertension, though the difference was not statistically significant.22 The trialists also found that anxiety scores did not differ over time, or between arms.
The authors’ finding that self-monitoring is, on the whole, more acceptable than ambulatory monitoring when diagnosing hypertension replicates results previously obtained in secondary care settings. A Scottish study found that 81% of patients preferred self-monitoring over ambulatory monitoring to confirm or exclude hypertension.23 Reasons given by patients were the ability to instantly see their results, being more in control, being less embarrassed in public, and no interference with sleep. Those that preferred ambulatory monitoring liked that it was finished within 1 day. In a cohort of untreated patients of a Greek hypertension outpatient clinic, self-monitoring was more acceptable and preferable to ambulatory monitoring, though both modalities were generally felt to be acceptable, accurate, and convenient.24
The out-of-office BP acceptability scale has been used in three other published studies. It was validated by Little et al in a sample of 200 UK primary care patients recently diagnosed or with poorly controlled hypertension.16 Lindroos et al used it in Finland on 223 participants of a population-based health survey, 27% of whom were receiving antihypertensives,18 while Wood et al studied 770 people, with or without diagnosed hypertension, to explore ethnic differences in acceptability.10
The oldest study16 had the lowest acceptability scores for both ambulatory and self-monitoring, perhaps due to larger, bulkier monitors. The current study, unlike the other cohorts, did not include patients already diagnosed with hypertension and, due to its diagnostic primary aim, patients were required to self-monitor for 28 days. This is longer than the other studies (Lindroos et al 7 days, Little et al duration not reported), and longer than current guideline recommendations.8 This increased measurement burden may have reduced the acceptability of self-monitoring, and may account for the smaller difference observed between the mean scores of the modalities in the present study. Conversely, monitoring for an extended period may have enabled participants to develop a routine, normalising this behaviour and reducing anxiety when attempting to measure their BP, as suggested in the free-text comments.
Implications for research and practice
With approximately one-quarter of participants reporting that self-monitoring made them anxious, further research is needed into how to identify and understand how best to support these patients undergoing out-of-office monitoring for the purposes of hypertension diagnosis. Optimising support would help minimise any psychological harms and maximise adherence. This study could be replicated using an out-of-office diagnostic protocol that resembles current recommended practice (that is, 7-days of self-monitoring with no telemonitoring, or 24-hour ambulatory monitoring).
The NICE hypertension guidelines8 recommend self-monitoring for the diagnosis of hypertension if a patient is unable to tolerate ambulatory blood pressure monitoring. The current results suggest that females find the latter less tolerable and more anxiety inducing, and therefore could be directed towards self-monitoring during diagnosis by their healthcare professional.
Acknowledgments
The authors wish to thank all participants who took part in this study, and participating GP surgeries. This work uses data provided by patients and collected by the NHS as part of their care and support and would not have been possible without access to this data. The NIHR recognises and values the role of patient data, securely accessed and stored, both in underpinning and leading to improvements in research and care.
Funding
This project presents independent research commissioned by the National Institute for Health Research (NIHR) under its Programme Grants for Applied Research funding scheme (RP-PG-0407–10347). Rafael Perera is supported by the NIHR Oxford Biomedical Research Centre. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.
Ethical approval
Ethical approval was granted by the NHS Research Ethics Committee — Oxfordshire Research Ethics Committee B (Reference: 09/H0605/106).
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.Sheppard JP, Schwartz CL, Tucker KL, McManus RJ. Modern management and Diagnosis of Hypertension in the United Kingdom: Home Care and Self-care. Ann Glob Health. 2016;82(2):274–287. doi: 10.1016/j.aogh.2016.02.005. [DOI] [PubMed] [Google Scholar]
- 2.Fletcher BR, Hinton L, Bray EP, et al. Self-monitoring blood pressure in patients with hypertension: an internet-based survey of UK GPs. Br J Gen Pract. 2016. [DOI] [PMC free article] [PubMed]
- 3.Mancia G, Bombelli M, Seravalle G, Grassi G. Diagnosis and management of patients with white-coat and masked hypertension. Nat Rev Cardiol. 2011;8(12):686–693. doi: 10.1038/nrcardio.2011.115. [DOI] [PubMed] [Google Scholar]
- 4.Ward AM, Takahashi O, Stevens R, Heneghan C. Home measurement of blood pressure and cardiovascular disease: systematic review and meta-analysis of prospective studies. J Hypertens. 2012;30(3):449–456. doi: 10.1097/HJH.0b013e32834e4aed. [DOI] [PubMed] [Google Scholar]
- 5.Hansen TW, Kikuya M, Thijs L, et al. Prognostic superiority of daytime ambulatory over conventional blood pressure in four populations: a meta-analysis of 7030 individuals. J Hypertens. 2007;25(8):1554–1564. doi: 10.1097/HJH.0b013e3281c49da5. [DOI] [PubMed] [Google Scholar]
- 6.Siu AL, US Preventive Services Task Force Screening for high blood pressure in adults: US Preventive Services Task Force recommendation statement. Ann Intern Med. 2015;163(10):778–786. doi: 10.7326/M15-2223. [DOI] [PubMed] [Google Scholar]
- 7.Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) Eur Heart J. 2013;34(28):2159–2219. doi: 10.1093/eurheartj/eht151. [DOI] [PubMed] [Google Scholar]
- 8.National Institute for Health and Care Excellence . Hypertension in adults: diagnosis and management. London: NICE; 2016. CG127. https://www.nice.org.uk/guidance/cg127 (accessed 12 Mar 2019) [PubMed] [Google Scholar]
- 9.Fletcher BR, Hinton L, Hartmann-Boyce J, et al. Self-monitoring blood pressure in hypertension, patient and provider perspectives: A systematic review and thematic synthesis. Patient Educ Couns. 2016;99(2):210–219. doi: 10.1016/j.pec.2015.08.026. [DOI] [PubMed] [Google Scholar]
- 10.Wood S, Greenfield SM, Sayeed Haque M, et al. Influence of ethnicity on acceptability of method of blood pressure monitoring: a cross-sectional study in primary care. Br J Gen Pract. 2016. [DOI] [PMC free article] [PubMed]
- 11.Pickering TG. Now we are sick: labeling and hypertension. J Clin Hypertens (Greenwich) 2006;8(1):57–60. doi: 10.1111/j.1524-6175.2005.05121.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nunan D, Thompson M, Heneghan CJ, et al. Accuracy of self-monitored blood pressure for diagnosing hypertension in primary care. J Hypertens. 2015;33(4):755–762. doi: 10.1097/HJH.0000000000000489. discussion 762. [DOI] [PubMed] [Google Scholar]
- 13.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 14.National Institute for Health and Care Excellence . Depression in adults: recognition and management. London: NICE; 2004. CG90. http://www.nice.org.uk/guidance/cg90 (accessed 12 Mar 2019) [PubMed] [Google Scholar]
- 15.EuroQol Group EuroQol — a new facility for the measurement of health-related quality of life. Health Policy. 1990;16(3):199–208. doi: 10.1016/0168-8510(90)90421-9. [DOI] [PubMed] [Google Scholar]
- 16.Little P, Barnett J, Barnsley L, et al. Comparison of acceptability of and preferences for different methods of measuring blood pressure in primary care. BMJ. 2002;325(7358):258–259. doi: 10.1136/bmj.325.7358.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Szende A, Janssen B, Cabases J, editors. Self-Reported Population Health: An International Perspective based on EQ-5D. Dordrecht: Springer; 2014. [PubMed] [Google Scholar]
- 18.Lindroos AS, Jula AM, Puukka PJ, et al. Comparison of Acceptability of Traditional and Novel Blood Pressure Measurement Methods. Am J Hypertens. 2016;29(6):679–83. doi: 10.1093/ajh/hpv167. [DOI] [PubMed] [Google Scholar]
- 19.Luo N, Johnson J, Coons SJ. Using instrument-defined health state transitions to estimate minimally important differences for four preference-based health-related quality of life instruments. Med Care. 2010;48(4):365–371. doi: 10.1097/mlr.0b013e3181c162a2. [DOI] [PubMed] [Google Scholar]
- 20.Crawford JR, Henry JD, Crombie C, Taylor EP. Normative data for the HADS from a large non-clinical sample. Br J Clin Psychol. 2001;40(Pt 4):429–434. doi: 10.1348/014466501163904. [DOI] [PubMed] [Google Scholar]
- 21.Kind P, Dolan P, Gudex C, Williams A. Variations in population health status: results from a United Kingdom national questionnaire survey. BMJ. 1998;316(7133):736–741. doi: 10.1136/bmj.316.7133.736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McManus RJ, Mant J, Bray EP, et al. Telemonitoring and self-management in the control of hypertension (TASMINH2): a randomised controlled trial. Lancet. 2010;376(9736):163–172. doi: 10.1016/S0140-6736(10)60964-6. [DOI] [PubMed] [Google Scholar]
- 23.McGowan N, Padfield PL. Self blood pressure monitoring: a worthy substitute for ambulatory blood pressure? J Hum Hypertens. 2010;24(12):801–806. doi: 10.1038/jhh.2010.15. [DOI] [PubMed] [Google Scholar]
- 24.Nasothimiou EG, Karpettas N, Dafni MG, Stergiou GS. Patients’ preference for ambulatory versus home blood pressure monitoring. J Hum Hypertens. 2014;28(4):224–229. doi: 10.1038/jhh.2013.104. [DOI] [PubMed] [Google Scholar]