INTRODUCTION
Hand infections are a common problem among the population and carry significant morbidity.1,2 Deep hand infection such as flexor sheath infections are surgical emergencies and require prompt referral to prevent permanent disability. A misdiagnosis of flexor sheath infection can potentially lead to severe stiffness, deformity, or amputation of the digit.2
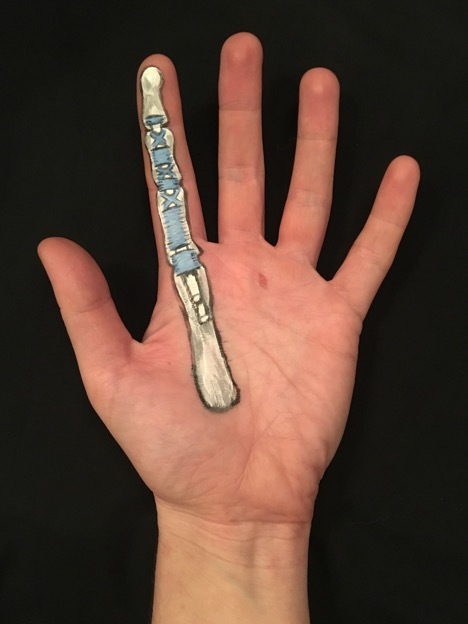
This article presents an unusual case of a 22-year-old with a chronic intermittent history of swelling and pain to the right middle finger (RMF). Although the history was slightly atypical, examination findings identified the Kanavel cardinal signs of tendon sheath infection (Figure 1).
Figure 1.

Flexor sheath infection of the right middle finger from a patient with a drill puncture wound.
CASE REPORT
A 22-year-old male left hand-dominant joiner presented to his GP with severe pain in the RMF. He was awoken the previous night by pain and swelling in his RMF. He was unable to attend work due to the severity of pain in his finger. The pain was constant, worse with movement, and relieved by analgesia (co-codamol and naproxen). He had no history of exacerbating factors, recent trauma, or systemic upset. He reported a glass injury to this finger 22 months previously.
He complained of several similar episodes of pain and swelling to the RMF over the past few years. These episodes usually lasted for 1–2 weeks then spontaneously self-resolved. This episode was more severe than previous episodes, which prompted him to seek medical advice from his GP. His past medical history included mild asthma managed with Qvar® (beclometasone diproprionate) and salbutamol inhalers.
Examination revealed an RMF that was grossly swollen with tenderness on palpation of the flexor tendon from the distal palmar crease up to the distal interphalangeal joint and tenderness on passive extension. There was no heat or redness. He had a single callus over the proximal phalangeal joint of the RMF stemming from his occupation (the site of previous glass injury). He had normal vital signs and was afebrile.
Given his recurrent symptoms, atraumatic history, and increasing severity, his GP made an urgent outpatient referral (the authors’ trust currently aims to see urgent referrals within 2 weeks of referral) to the combined orthopaedic/plastic surgery hand team requesting physiotherapy review for this presumed severe intermittent tendonitis of the RMF. An on-call hand consultant was checking urgent referrals on the afternoon the referral arrived and noted a number of concerning features in a very well documented and thorough GP referral. A decision was made to contact the patient and ask him to attend the local emergency department immediately for a clinical review. Clinical examination confirmed the presence of all four Kanavel signs and he was diagnosed with an RMF flexor sheath infection. He received urgent intravenous flucloxacillin and was taken to the operating theatre the same evening, where exploration of the RMF revealed frank pus within the flexor sheath. This was washed out, and he remained an inpatient while he received 24 hours of intravenous antibiotics. Microbiology culture and sensitivity swabs were taken intra-operatively, which showed no growth of bacteria. He was discharged 2 days after admission with 5 further days of antibiotic therapy and referral to hand therapy to ensure good mobilisation of the digit.
DISCUSSION
Flexor sheath infections, also known as infected tenosynovitis, are a relatively common infection of the hand with a prevalence ranging from 2.5% to 9.4% of hand infections.3 If misdiagnosed, flexor sheath infections can lead to serious, life-threatening consequences. Digital flexor sheaths are a closed continuous synovial system that invest the flexor digitorum profundus and flexor digitorum superficialis (Figure 2). Flexor sheath infections are caused by direct inoculation due to trauma, contiguous spread from adjacent tissues, or via haematogenous spread. Common injuries include animal bites, puncture wounds, IV drug use, and wounds exposed to fresh/saltwater. Such injuries, if associated with severe tenderness, should raise a high suspicion of flexor tenosynovitis.4 Flexor sheath infections initially begin with exudative fluid within the tendon sheath, followed by the development of purulent fluid. Bacterial overgrowth within the synovial sheath leads to increased fluid and pressure, leading to ischaemia, and resulting in a septic necrosis of the tendon sheath and surrounding structures. If left untreated, complications may include soft tissue necrosis, osteomyelitis, and necrotising fasciitis. There are four cardinal signs of flexor tenosynovitis, which are also known as the Kanavel signs:
an exquisite tenderness over the course of the sheath and limited to the sheath;
the finger sits in a resting flexed posture;
an exquisite pain on extending the finger, more marked at the proximal end; and
a fusiform swelling of the whole finger.5
Figure 2.
Picture demonstrating the anatomical location and structure of the flexor sheath. Flexor sheath is composed of annular (ring) pulleys and cruciate (cross) pulleys. The pulleys are identified as A1, A2, C1, A3, C2, A4, C3, and A5.
The presence of all four Kanavel signs predicts a high sensitivity (91–97%) for flexor tenosynovitis.6 The earliest sign is often pain on passive extension,3 with a later sign being tenderness along the flexor sheath suggesting progression of the infection more proximally. Unlike most severe infections, fever is frequently absent (only 17%).3
Management of suspected flexor tenosynovitis in the community involves elevation to reduce swelling and urgent referral to the local hand surgery department. Inpatient management involves broad-spectrum antibiotic therapy and urgent surgery to debride tissues and irrigate the tendon sheath.3
This patient presented with an atypical history of RMF pain and swelling. A thorough examination by his GP revealed the Kanavel signs of flexor sheath infection and, although the diagnosis was not initially clear, the detailed referral raised the suspicions of the duty hand consultant who requested immediate surgical assessment and intervention.
In summary, flexor sheath infections are an important hand condition and all GPs should be aware of this condition and the potential consequences of missing these infections. The history may not always be typical, but if there are clinical features on examination, including the Kanavel signs, urgent same-day referral to a hand service should be considered.
POINTS OF INTEREST
The Kanavel cardinal signs of flexor sheath infection are a finger held in slight flexion, fusiform swelling of the affected digit, tenderness along the flexor tendon sheath, and pain with passive extension of the digit.
A suspicion of flexor sheath infection warrants urgent referral to a hand unit.
Acknowledgments
Thanks to Megan Anderson for creating and providing images.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Patient consent
The patient gave consent for publication of this case report.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.Patel DB, Emmanuel NB, Stevanovic MV, et al. Hand infections: anatomy, types and spread of infection, imaging findings, and treatment options. Radiographics. 2014;34(7):1968–1986. doi: 10.1148/rg.347130101. [DOI] [PubMed] [Google Scholar]
- 2.Giladi AM, Malay S, Chung KC. A systematic review of the management of acute pyogenic flexor tenosynovitis. J Hand Surg Eur Vol. 2015;40(7):720–728. doi: 10.1177/1753193415570248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pang H-N, Teoh L-C, Yam AK, et al. Factors affecting the prognosis of pyogenic flexor tenosynovitis. J Bone Joint Surg Am. 2007;89(8):1742–1748. doi: 10.2106/JBJS.F.01356. [DOI] [PubMed] [Google Scholar]
- 4.Nikkhah D, Rodrigues J, Osman K, Dejager L. Pyogenic flexor tenosynovitis: one year’s experience at a UK hand unit and a review of the current literature. Hand Surg. 2012;17(2):199–203. doi: 10.1142/S0218810412500190. [DOI] [PubMed] [Google Scholar]
- 5.Kanavel A. Infections of the hand. Philadelphia, PA: Lea & Febiger; 1912. [Google Scholar]
- 6.Kennedy CD, Lauder AS, Pribaz JR, Kennedy SA. Differentiation between pyogenic flexor tenosynovitis and other finger infections. Hand (N Y) 2017;12(6):585–590. doi: 10.1177/1558944717692089. [DOI] [PMC free article] [PubMed] [Google Scholar]


