Abstract
Purpose
We aim to assess if air pollution levels and climatological factors are associated with hospital admissions for exacerbation of chronic obstructive pulmonary disease (COPD) in Spain from 2004 to 2013.
Methods
We conducted a retrospective study. Information on pollution level and climatological factors were obtained from the Spanish Meteorological Agency and hospitalizations from the Spanish hospital discharge database. A case-crossover design was used to identify factors associated with hospitalizations and in hospital mortality. Postal codes were used to assign climatic and pollutant factors to each patient.
Results
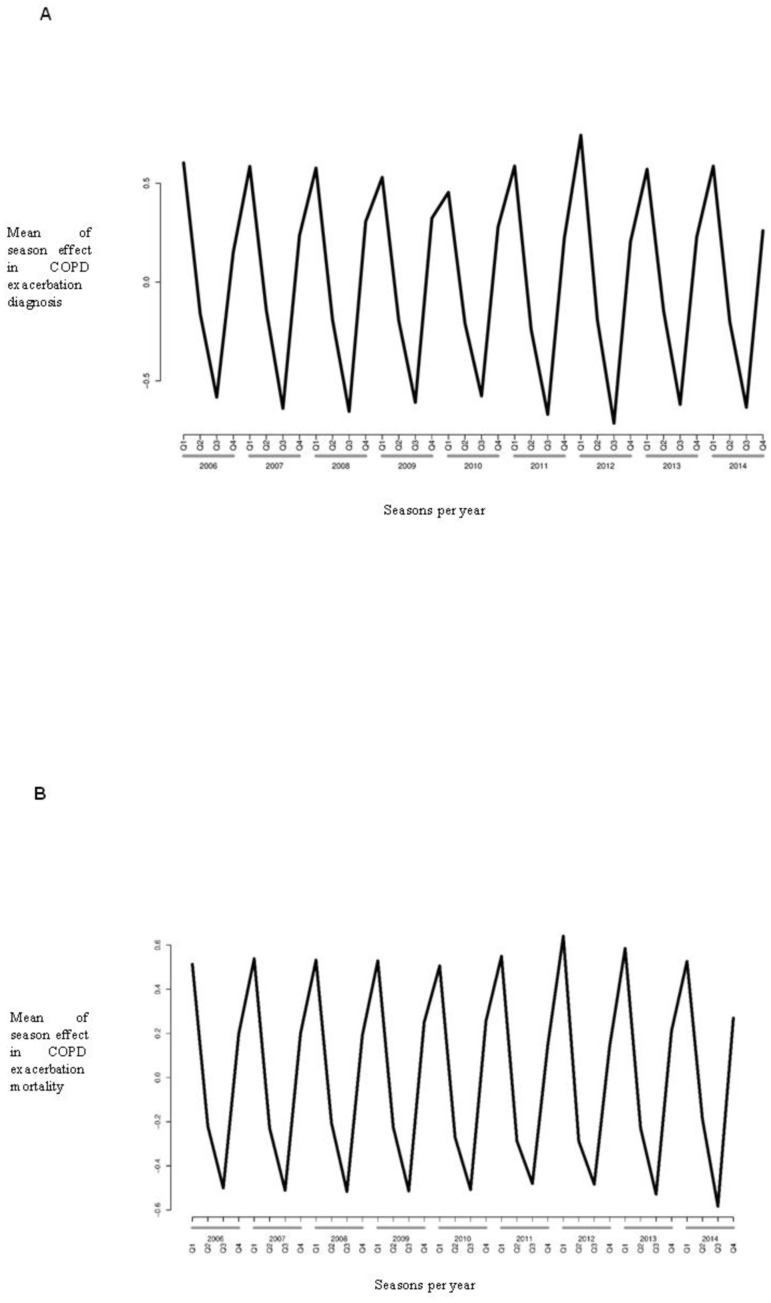
We detected 162,338 hospital admissions for COPD exacerbation. When seasonal effects were evaluated we observed that hospital admissions and mortality were more frequent in autumn and winter. In addition, we found significant associations of temperature, humidity, ozone (O3), carbon monoxide (CO), particulate matter up to 10 μm in size (PM10) and nitrogen dioxide (NO2) with hospital admissions. Lower temperatures at admission with COPD exacerbation versus 1, 1.5, 2 and 3 weeks prior to hospital admission for COPD exacerbation, were associated with a higher probability of dying in the hospital. Other environmental factors that were related to in-hospital mortality were NO2, O3, PM10 and CO.
Conclusions
Epidemiology of hospital admissions by COPD exacerbation was negatively affected by colder climatological factors (seasonality and absolute temperature) and short-term exposure to major air pollution (NO2, O3, CO and PM10).
Introduction
Chronic obstructive pulmonary disease (COPD) is a major cause of health care costs, mortality and morbidity around the world. Exacerbations of existing COPD are a frequent reason for hospital admission and with increased mortality among these patients [1]. Known risk factors for COPD exacerbations include exposures to tobacco, some workplace exposures, and infections by bacteria and virus [2]. Another potential trigger for such exacerbations is short-term exposures to air pollution [3–5].
The evidence regarding the effects of air pollution exposure on COPD exacerbations is still limited. It has been investigated by several studies. Some of them have reported that air pollutions are risk factor for exacerbation or mortality [6–8], while others found not significant associations or relationship only for selected populations [9,10]. However, a recent systematic review and meta-analysis concluded that the risk of COPD exacerbations is significantly increased by short-term exposure to major air pollutants [11].
The mechanisms by which COPD exacerbations can be triggered after exposure to air pollution are not yet fully understood. However, there are several reasonable hypotheses [12]. Particulate matters like particulate matter up to 10 μm in size (PM10) and gaseous pollutants of nitrogen dioxide (NO2) and ozone (O3) can all produce deleterious effects on the respiratory airways such as increased bronchial reactivity [13], airway oxidative stress-induced DNA damage [14,15], pulmonary and systemic inflammation [16–18], amplification of viral infections [19], and reduction in airway cialiary activity [20]. On the other hand, sulfur dioxide (SO2) is a well-known respiratory irritant, with acute respiratory symptoms reported immediately upon exposure to elevated concentrations, and it can also cause bronchoconstriction [2,21].
Extremes of temperature, both cold and heat, have also been associated to excess mortality and morbidity among patients suffering COPD [22]. However, the interaction between temperature and air pollution among COPD patients and the effect such interaction has on the morbidity burden has been poorly investigated so far [23].
We aim to assess if air pollution levels and climatological factors are associated with hospital admissions for exacerbation of chronic obstructive pulmonary disease (COPD) in Spain from 2004 to 2013.
Material and methods
Study population
We conducted a retrospective study. All patients hospitalized in Spain from 1 January 2004 to 31 December 2013 for suffering a COPD exacerbation were included in our investigation. Hospital admissions were extracted from the Spanish National Hospital Discharge data base (Spanish Minimum Basic Data Set, MBDS). Over 97% of all hospitalizations in Spain are included in this database. Details on the MBDS can be found elsewhere [24].
The MBDS variables used for our investigation included; sex, age, dates of hospital admission date of hospital discharge, postal code of the patient, up to 14 diagnosis and 20 procedure codes and outcome at discharge. The 9th edition of the International Classification of Diseases (ICD-9-CM) is used for coding in the MBDS. We excluded patients with a missing postal code.
Environmental data
Information on pollution level and climatological factors were obtained from the Spanish Meteorological Agency (AEMET) (http://www.aemet.es/). As we did not have any individual exposure levels postal codes were used to assign climatic and pollutant factors to each patient using the data provided from the nearest station to the patient’s residence.
The daily data assigned to each patient included, humidity, temperature and the following pollutants PM10, SO2, NO2, O3, and CO, There are around 800 meteorological stations in Spain. The locations of these meteorological stations for each of the 17 Spanish Autonomous Communities can be obtained from the web of the AEMET (http://www.aemet.es/es/eltiempo/observacion).
Outcome variables
We considered the main outcome variable a hospital admission with a primary diagnosis of COPD exacerbation (code 491.21 in the ICD9CM). According to the MBDS methodology for every patient admitted to the hospital, and beside which is the primary diagnosis, those who have been admitted to any hospital in the previous 30 days are considered a readmission. In our study all patients who had an admission in the previous month were deleted from the database so it is not possible to have an overlap with other admission in which COPD was not the primary diagnosis.
Statistical analysis
The statistical methods used have been described in detail in a previous study conducted by our group. [25] Basically the following processes were conducted. To assess the seasonal effect on COPD exacerbation that resulted in a hospital admission the years were divided into quarters. We used a Bayesian model with Poisson distribution to analyze the seasonal effect [26].
To evaluate the effect of each environmental factor on the hospital admissions for COPD exacerbation we used a case-crossover design (CCD) [25, 27, 28] In this design each patient is used as his own control. We considered four time periods before the date of the hospital admission (baseline) for each patient as control periods (1, 1.5, 2 and 3 weeks) as has been described before [29]. In order to avoid the effect of one day with outlier values we calculated the mean for each environmental factor including the day before and after the control periods and for the baseline the two days immediately before. The association between environmental factors and COPD exacerbation admissions was evaluated using conditional logistic regression obtaining odds ratios with their 95%CI using an exact method. To construct each model we introduced the environmental factor under study and afterwards introduced the remaining factors one by one in the model for adjustment. If any of the remaining factor had a significant correlation with the environmental factor under study this factor was excluded from the model.
R statistical package version 3.4.4 (GNU General Public License) was used for all analyses and a p-values <0.05 (two-tailed) was the cut point for significance [30]
Ethical aspects
The study maintains data confidentiality at all times. Given the anonymous and mandatory nature of the database, it was not necessary to obtain informed consent or approval by an ethics committee in accordance with Spanish legislation.
Results
Characteristics of study population
The epidemiological and clinical characteristics of the study population are shown in Table 1. We detected 162,338 hospital admissions for COPD exacerbation. The median age was 75.1 years and 83.5% were male. The most frequent comorbidities were mild diabetes without complication (24.5%), congestive heart failure (19.3%), and renal disease (11.1%).
Table 1. Epidemiological and clinical characteristics of patients admitted to hospital with a COPD exacerbation in Spain from 2004 to 2013.
| Description | Data |
|---|---|
| No. of patients | 162338 |
| Males | 135598 (83.5) |
| Age (years) | 75.15 (10.76) |
| Length of stay (days) | 8.37 (7.73) |
| Charlson index | 2.42 (1.73) |
| In-hospital mortality | 9868 (6.1) |
| Comorbid diseases | |
| Myocardial infarction | 6404 (3.9) |
| Congestive heart failure | 31275 (19.3) |
| Peripheral vascular disease | 9087 (5.6) |
| Cerebrovascular disease | 6680 (4.1) |
| Dementia | 4226 (2.6) |
| Connective tissue disease-rheumatic disease | 2394 (1.5) |
| Peptic ulcer disease | 1177 (0.7) |
| Mild liver disease | 7463 (4.6) |
| Diabetes without complications | 39749 (24.5) |
| Diabetes with complications | 2843 (1.8) |
| Paraplegia and hemiplegia | 453 (0.3) |
| Renal disease | 18063 (11.1) |
| Cancer | 10876 (6.7) |
| Moderate or severe liver disease | 760 (0.5) |
| Metastatic carcinoma | 2593 (1.6) |
Values are expressed as absolute number (percentage) and mean (95% of confidence interval).
Effect of season on admission with COPD exacerbation and in-hospital mortality
When seasonal effects were evaluated using a Bayesian model (Fig 1A), COPD exacerbation admissions were less common in second and third quarter of the year, and more abundant in the last and first quarter of the year. Similar pattern were found in COPD exacerbation -related death (Fig 1B).
Fig 1. Mean of the seasonal effect in admissions for COPD exacerbation (A) and in-hospital mortality (B) in Spain between 2004 and 2013.
Effects of short-term exposure to environmental risk factors on COPD exacerbation hospital admissions and in-hospital mortality
In the bivariate model, significant associations were found for temperature, NO2, O3, PM10 and CO with COPD exacerbation hospital admissions. Using a multi-environmental factor model temperature, humidity, NO2, O3, PM10 and CO remained significantly associated (Table 2).
Table 2. Bivarite and multivariable models results for the associations between environmental factors and COPD exacerbation hospital admissions for study time periods (1, 1.5, 2 and 3 weeks before hospitalization).
| Unadjusted | Adjusted | |||
|---|---|---|---|---|
| Environmental factor (Unit) | OR (95% CI) | p-value | OR (95% CI) | p-value |
| 1 week | ||||
| Temperature (°C) | 0.99 (0.99; 0.99) | <0.001 | 0.99 (0.98; 0.99) | <0.001 |
| Humidity (%) | 0.99 (0.99; 1.00) | 0.117 | 0.99 (0.98; 0.99) | 0.002 |
| NO2 (Bg/m3) | 1.02 (1.01; 1.03) | 0.020 | 1.01 (0.99; 1.03) | 0.229 |
| SO2 (Bg/m3) | 1.00 (0.99; 1.01) | 0.641 | 1.00 (0.99; 1.01) | 0.711 |
| O3 (Bg/m3) | 0.98 (0.98; 0.99) | <0.001 | 0.98 (0.97; 0.99) | <0.001 |
| PM10 (Bg/m3) | 0.99 (0.98; 1.01) | 0.511 | 0.98 (0.97; 0.99) | 0.034 |
| CO (Bg/m3) | 1.04 (1.03; 1.05) | <0.001 | 1.04 (1.02; 1.06) | <0.001 |
| 1.5 weeks | ||||
| Temperature (°C) | 0.99 (0.99; 1.01) | 0.167 | 0.99 (0.99; 0.99) | 0.024 |
| Humidity (%) | 1.00 (0.99; 1.01) | 0.475 | 0.99 (0.99; 1.01) | 0.236 |
| NO2 (Bg/m3) | 0.97 (0.96; 0.98) | <0.001 | 0.97 (0.96; 0.98) | <0.001 |
| SO2 (Bg/m3) | 0.99 (0.99; 1.01) | 0.503 | 1.00 (0.99; 1.01) | 0.908 |
| O3 (Bg/m3) | 0.99 (0.98; 0.99) | <0.001 | 0.98 (0.97; 0.99) | <0.001 |
| PM10 (Bg/m3) | 0.96 (0.95; 0.97) | <0.001 | 0.96 (0.94; 0.97) | <0.001 |
| CO (Bg/m3) | 1.03 (1.02; 1.04) | <0.001 | 1.04 (1.03; 1.06) | <0.001 |
| 2 weeks | ||||
| Temperature (°C) | 0.99 (0.99; 0.99) | <0.001 | 0.99 (0.99; 0.99) | <0.001 |
| Humidity (%) | 0.99 (0.99; 1.01) | 0.440 | 0.99 (0.99; 0.99) | 0.043 |
| NO2 (Bg/m3) | 1.03 (1.01; 1.04) | <0.001 | 1.02 (1.01; 1.04) | 0.002 |
| SO2 (Bg/m3) | 0.99 (0.99; 1.01) | 0.187 | 0.99 (0.99; 1.01) | 0.107 |
| O3 (Bg/m3) | 0.98 (0.97; 0.98) | <0.001 | 0.98 (0.97; 0.99) | <0.001 |
| PM10 (Bg/m3) | 0.99 (0.98; 1.01) | 0.222 | 0.97 (0.96; 0.99) | 0.001 |
| CO (Bg/m3) | 1.05 (1.03; 1.06) | <0.001 | 1.04 (1.03; 1.06) | <0.001 |
| 3 weeks | ||||
| Temperature (°C) | 1.01 (1.01; 1.01) | 0.029 | 1.00 (0.99; 1.00) | 0.206 |
| Humidity (%) | 1.00 (1.00; 1.00) | 0.858 | 1.00 (1.00; 1.00) | 0.650 |
| NO2 (Bg/m3) | 1.03 (1.02; 1.05) | <0.001 | 1.02 (1.01; 1.03) | 0.017 |
| SO2 (Bg/m3) | 0.99 (0.99; 1.00) | 0.715 | 0.99 (0.99; 1.01) | 0.551 |
| O3 (Bg/m3) | 0.97 (0.97; 0.98) | <0.001 | 0.97 (0.97; 0.98) | <0.001 |
| PM10 (Bg/m3) | 1.01 (0.99; 1.02) | 0.452 | 0.98 (0.97; 0.99) | 0.026 |
| CO (Bg/m3) | 1.05 (1.04; 1.06) | <0.001 | 1.05 (1.03; 1.06) | <0.001 |
NO2, nitrogen dioxide; SO2, sulfur dioxide; O3, ozone; PM10, particulate matter up to 10 μg/ m3 in size; CO: carbon monoxide; OR, odds ratio; 95% CI, 95% of confidence interval.
Both CO and NO2 concentrations showed, in general, significant OR values >1. Thus, high concentrations of CO and NO2 at the time of admission when they were taken as control 1.5, 2 and 3 weeks before admission were significantly associated with a higher possibility of COPD exacerbation hospital admission. Concentrations of O3, PM10 showed values of OR <1. Specifically, high concentrations of O3 and PM10 1, 1.5, 2 and 3 weeks before admissions were significantly associated with high probability of COPD exacerbation related hospitalization. Note that associations of humidity and temperature with COPD exacerbation hospitalization only occurred when 1 and 2 weeks were considered as control times; thus, low temperatures at the time of admission, with respect to the corresponding control times, were significantly associated with a greater possibility of hospital admission related to COPD exacerbation. SO2 concentrations were not associated with COPD exacerbation hospital admissions in any of the periods analyzed.
The effects of each environmental factor in the in-hospital mortality after COPD exacerbation are shown in Table 3.
Table 3. Bivarite and multivariable models results for the associations between environmental factors and in hospital mortality after COPD exacerbation hospital admissions for study time periods (1, 1.5, 2 and 3 weeks before hospitalization).
| Unadjusted | Adjusted | |||
|---|---|---|---|---|
| Environmental factor (Unit) | OR (95% CI) | p-value | OR (95% CI) | p-value |
| 1 week | ||||
| Temperature (°C) | 0.98 (0.97; 0.99) | <0.001 | 0.98 (0.97; 0.99) | <0.001 |
| Humidity (%) | 0.99 (0.99; 1.01) | 0.526 | 1.00 (0.99; 1.00) | 0.096 |
| NO2 (Bg/m3) | 0.98 (0.93; 1.04) | 0.567 | 0.98 (0.92; 1.04) | 0.475 |
| SO2 (Bg/m3) | 0.99 (0.97; 1.02) | 0.681 | 1.01 (0.98; 1.04) | 0.516 |
| O3 (Bg/m3) | 0.96 (0.93; 0.99) | 0.011 | 0.95 (0.92; 0.99) | 0.015 |
| PM10 (Bg/m3) | 0.95 (0.90; 1.01) | 0.112 | 0.94 (0.88; 1.00) | 0.051 |
| CO (Bg/m3) | 1.05 (0.99; 1.12) | 0.062 | 1.05 (0.99; 1.12) | 0.099 |
| 1.5 weeks | ||||
| Temperature (°C) | 0.98 (0.98; 0.99) | <0.001 | 0.98 (0.97; 0.99) | <0.001 |
| Humidity (%) | 1.00 (1.00; 1.00) | 0.349 | 1.00 (1.00; 1.00) | 0.959 |
| NO2 (Bg/m3) | 0.91 (0.87; 0.96) | <0.001 | 0.92 (0.87; 0.98) | 0.007 |
| SO2 (Bg/m3) | 0.98 (0.96; 1.01) | 0.183 | 1.00 (0.97; 1.02) | 0.826 |
| O3 (Bg/m3) | 0.97 (0.94; 0.99) | 0.029 | 0.95 (0.91; 0.98) | 0.002 |
| PM10 (Bg/m3) | 0.89 (0.84; 0.94) | <0.001 | 0.89 (0.83; 0.95) | <0.001 |
| CO (Bg/m3) | 1.03 (0.98; 1.08) | 0.226 | 1.04 (0.99; 1.09) | 0.139 |
| 2 weeks | ||||
| Temperature (°C) | 0.99 (0.98; 0.99) | 0.003 | 0.99 (0.98; 0.99) | <0.001 |
| Humidity (%) | 1.00 (0.99; 1.01) | 0.886 | 0.99 (0.99; 1.01) | 0.473 |
| NO2 (Bg/m3) | 0.99 (0.94; 1.04) | 0.626 | 0.99 (0.93; 1.05) | 0.704 |
| SO2 (Bg/m3) | 0.99 (0.96; 1.01) | 0.289 | 0.99 (0.96; 1.02) | 0.427 |
| O3 (Bg/m3) | 0.96 (0.93; 0.99) | 0.006 | 0.96 (0.93; 0.99) | 0.018 |
| PM10 (Bg/m3) | 0.95 (0.89; 1.01) | 0.065 | 0.94 (0.88; 1.00) | 0.053 |
| CO (Bg/m3) | 1.03 (0.98; 1.08) | 0.208 | 1.04 (0.98; 1.09) | 0.198 |
| 3 weeks | ||||
| Temperature (°C) | 0.99 (0.98; 0.99) | 0.012 | 0.99 (0.98; 0.99) | 0.004 |
| Humidity (%) | 1.00 (0.99; 1.00) | 0.767 | 0.99 (0.99; 1.00) | 0.704 |
| NO2 (Bg/m3) | 1.03 (0.98; 1.08) | 0.293 | 1.00 (0.94; 1.06) | 0.946 |
| SO2 (Bg/m3) | 0.99 (0.97; 1.01) | 0.436 | 0.99 (0.97; 1.02) | 0.713 |
| O3 (Bg/m3) | 0.95 (0.92; 0.97) | <0.001 | 0.94 (0.91; 0.98) | 0.001 |
| PM10 (Bg/m3) | 0.97 (0.92; 1.03) | 0.306 | 0.94 (0.88; 1.00) | 0.058 |
| CO (Bg/m3) | 1.06 (1.01; 1.11) | 0.011 | 1.06 (1.01; 1.12) | 0.035 |
NO2, nitrogen dioxide; SO2, sulfur dioxide; O3, ozone; PM10, particulate matter up to 10 μg/ m3 in size; CO: carbon monoxide; OR, odds ratio; 95% CI, 95% of confidence interval.
Lower temperatures at admission with COPD exacerbation versus 1, 1.5, 2 and 3 weeks before hospital admission for COPD exacerbation, increased the risk of in-hospital mortality in both crude and adjusted analysis. Other environmental factors that were related to in-hospital mortality were NO2, O3, PM10 and CO. No significant association between SO2 concentrations and in-hospital mortality in patients admitted for COPD exacerbation were found.
Discussion
Our study provides evidence that the epidemiology of hospital admissions by COPD is associated with environmental factors. We observed an overall seasonal effect as most hospital admissions for COPD exacerbation and in-hospital mortality occurred in the colder seasons (autumn to winter). Moreover, lower temperatures and higher concentrations of atmospheric pollutants significantly increased the incidence of hospitalization and in-hospital mortality.
We also described for all the time periods analyzed a significant association between short-term exposure to concentrations of NO2, O3 and PM10 and hospital admission for COPD exacerbation. Studies conducted in Europe and US agree with us observing the association between hospital admissions for COPD exacerbation and air pollution [31–36]. Additionally in a recent systematic review, Devries et al [2] reported that the incidence of hospitalization and of emergency room visits related to COPD showed a significant increase as the concentration of PM2.5, NO2, and SO2 raised. Another recent meta-analysis confirmed found that short-term exposure to gaseous and particulate pollutants increased the risk of COPD exacerbations significantly, 1% for PM2.5, 2% for NO2, and 0% for O3 for an increment of 10 μg/m3, but 0% for CO per increment of 100 μg/m [3,11]. Moreover, subgroup analysis according to age, study design, location and outcome, obtained similar and significant results.
Exposure to SO2 did not show a significant association with hospital admission for COPD exacerbation in the present study. These findings are consistent with a previous study, in which no effect was identified for SO2 [36]. By contrast, Santus et al [37] found that SO2 increases emergency room admissions for COPD exacerbations. In any case, over the last years the concentrations of SO2 have decreased sharply, as a consequence of cleaner motor vehicles fuels so nowadays NO2, O3 and PM have become the more relevant pollutants from a heath point of view [15].
The current analysis also has found a significant association between higher probability of hospital admissions with COPD exacerbation and lower temperatures at admission. Similar results have been reported by Krachunov et al [38], who reported that the levels of air pollutants were associated with the lower daily mean temperatures. In this way, Almagro et al [39] reported a 4.7% increase in the incidence of hospitalizations per 1 degree decrease in the temperature. Thus, Aga et al [40] observed that the daily number of deaths increased by 0.8%. per 10 μg/m3 increase in PM10. However, the highest risk of mortality among COPD patients is not related to gas pollutants such as NO2 or O3, being particulate matter pollution the strongest factor [41].
Regarding in hospital mortality, we found the highest figures in cold seasons such as autumn and winter. It has been previously reported that deaths from COPD increase significantly during the cold weather found in winter [42], but this is usually considered as a cofactor in the investigation on the effect of atmospheric pollution [43,44]. Agreeing with this conclusion we found that, not only lower temperatures, but also higher NO2, O3, CO and PM10 concentrations in the weeks before the hospital admission for COPD exacerbation, increased the risk of in-hospital mortality.
Nevertheless, several limitations of this study must be considered. First, we did not measure exposure to other environmental agents such as PM2.5, which could also have an influence on hospital admissions for COPD exacerbations. The reason for this is that in Spain the number of stations measuring PM2.5 is much smaller than those measuring PM10, so we have used the latter for our study. Second, we measured exposure levels at the monitoring stations but not at the individuals’ home since we used zip codes not addresses. This is important as some gaseous pollutants from traffic such as NO2 can taper quickly from its source and the patient’s home distance from the monitoring stations is not known. Third, we have not included infections by influenza in Spain in our investigation, and is well known that influenza incidence is associated to temperature and humidity [45]. However, in Spain data on influenza is not available by postal code or even by province and the information is collected only from epidemiological week 40 to week 10 (22 out of 52 weeks). Fifth, in our study population we have a male predominance among COPD patient which is mainly due to secular effects of the tobacco exposure and has been described in previous Spanish investigations [46]. Sixth, we cannot use lag days and test which exposure has the strongest association with the outcome (day 0, day -1, day -2, etc) because as commented in the methods section we decided to use an average value for each environmental factor over a 3-day period. Finally, we don’t have certainty that those hospitalized with COPD exacerbation as their main diagnosis died in the hospital as a consequence of this disease.
In summary, our results showed that epidemiology of hospital admissions by COPD exacerbations was negatively affected by colder climatological factors (absolute temperature, and seasonality) and by the short-term exposure to major air pollution (NO2, O3, CO and PM10).
Abbreviations
- AEMET
Spanish State Meteorological Agency
- CCD
case-crossover design
- CLR
conditional logistic regression
- CO
carbon monoxide
- COPD
chronic obstructive pulmonary disease
- ICD-9-CM
International Classification of Diseases, 9th ed, Clinical Modification
- MBDS
Spanish Minimum Basic Data Set
- MSSSI
Ministry of Health Social Services and Equality
- NHS
National Health System
- NO2
nitrogen dioxide
- O3
ozone
- PM10
particulate matter up to 10 μm in size
Data Availability
We cannot legally distribute the data because the Spanish Ministry of Health, who is the owner of the data, does not allow us to share the data. This is so because when we ask the Ministry of Health for the data using the link: http://www.mscbs.gob.es/estadEstudios/estadisticas/estadisticas/estMinisterio/SolicitudCMBDdocs/Formulario_Peticion_Datos_CMBD.pdf, we must sign an engagement in which we legally compromise to: 1. Under no circumstances to export the entire database or make partial exports that could allow the generation of the same through aggregation or identification of natural persons or reporting units. 2. To destroy the file or data provided and all the copies made of it once elapsed the period of time for which the data is required. In any case all investigators can request the databases using the following contact information: http://www.mscbs.gob.es/estadEstudios/estadisticas/estadisticas/estMinisterio/SolicitudCMBDdocs/Formulario_Peticion_Datos_CMBD.pdf. The same compromises are acquired with the Spanish Meteorological Agency and the databases can be requested using the following contact information: http://www.aemet.es/es/eltiempo/observacion.
Funding Statement
This study forms part of research funded by the FIS (Fondo de Investigaciones Sanitarias—Health Research Fund, Instituto de Salud Carlos III) co-financed by the European Union through the Fondo Europeo de Desarrollo Regional (FEDER, “Una manera de hacer Europa”): grant no. PI16/00564 to RJ. Menarini provided grant support through grant no. HUIL-15/07. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Global initiative for chronic obstructive lung disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease (2018 report). Disponible en: http://www.goldcopd.com. Fecha de acceso: 01/05/2018.
- 2.DeVries R, Kriebel D, Sama S. Low level air pollution and exacerbation of existing copd: a case crossover analysis. Environ Health. 2016; 15 (1):98 10.1186/s12940-016-0179-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Atkinson RW, Kang S, Anderson HR, Mills IC, Walton HA. Epidemiological time series studies of PM2.5 and daily mortality and hospital admissions: a systematic review and meta-analysis. Thorax. 2014; 69 (7):660–5. 10.1136/thoraxjnl-2013-204492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li MH, Fan LC, Mao B, Yang JW, Choi AMK, Cao WJ,et al. Short-term exposure to ambient fine particulate matter increases hospitalizations and mortality in COPD: a systematic review and meta-analysis. Chest. 2016; 149 (2):447–58. 10.1378/chest.15-0513 [DOI] [PubMed] [Google Scholar]
- 5.Bloemsma LD, Hoek G, Smit LAM. Panel studies of air pollution in patients with COPD: Systematic review and meta-analysis. Environ Res. 2016; 151:458–68. 10.1016/j.envres.2016.08.018 [DOI] [PubMed] [Google Scholar]
- 6.Neuberger M, Moshammer H, Rabczenko D. Acute and subacute effects of urban air pollution on cardiopulmonary emergencies and mortality: time series studies in Austrian cities. Int J Environ Res Public Health. 2013; 10 (10):4728–51. 10.3390/ijerph10104728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Peel JL, Tolbert PE, Klein M, Metzger KB, Flanders WD, Todd K, et al. Ambient air pollution and respiratory emergency department visits. Epidemiology. 2005; 16 (2):164–74. [DOI] [PubMed] [Google Scholar]
- 8.Choi J, Oh JY, Lee YS, Min KH, Hur GY, Lee SY, et al. Harmful impact of air pollution on severe acute exacerbation of chronic obstructive pulmonary disease: particulate matter is hazardous. Int J Chron Obstruct Pulmon Dis. 2018; 13:1053–1059. 10.2147/COPD.S156617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xu Z, Yu D, Jing L, Xu X. Air pollution and daily mortality in Shenyang, China. Arch Environ Health. 2000; 55 (2):115–20. 10.1080/00039890009603397 [DOI] [PubMed] [Google Scholar]
- 10.Yang Q, Chen Y, Krewski D, Burnett RT, Shi Y, McGrail KM. Effect of short-term exposure to low levels of gaseous pollutants on chronic obstructive pulmonary disease hospitalizations. Environ Res. 2005; 99 (1):99–105 10.1016/j.envres.2004.09.014 [DOI] [PubMed] [Google Scholar]
- 11.Li J, Sun S, Tang R, Qiu H, Huang Q, Mason TG, et al. Major air pollutants and risk of COPD exacerbations: a systematic review and meta-analysis.Int J Chron Obstruct Pulmon Dis. 2016; 11:3079–3091. 10.2147/COPD.S122282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.MacNee W, Donaldson K. Exacerbations of COPD: environmental mechanisms. Chest. 2000. May;117 (5 Suppl 2):390S–7S. 10.1378/chest.117.5_suppl_2.390s [DOI] [PubMed] [Google Scholar]
- 13.Foster WM, Brown RH, Macri K, Mitchell CS. Bronchial reactivity of healthy subjects: 18–20 h postexposure to ozone. J Appl Physiol (1985). 2000; 89 (5):1804–10. [DOI] [PubMed] [Google Scholar]
- 14.Oh SM, Kim HR, Park YJ, Lee SY, Chung KH. Organic extracts of urban air pollution particulate matter (PM2.5)-induced genotoxicity and oxidative stress in human lung bronchial epithelial cells (BEAS-2B cells). Mutat Res. 2011. August 16; 723 (2):142–51. 10.1016/j.mrgentox.2011.04.003 [DOI] [PubMed] [Google Scholar]
- 15.Ko FW, Hui DS. Air pollution and chronic obstructive pulmonary disease. Respirology. 2012; 17 (3):395–401. 10.1111/j.1440-1843.2011.02112.x [DOI] [PubMed] [Google Scholar]
- 16.Bayram H, Sapsford RJ, Abdelaziz MM, Khair OA. Effect of ozone and nitrogen dioxide on the release of proinflammatory mediators from bronchial epithelial cells of nonatopic nonasthmatic subjects and atopic asthmatic patients in vitro. J Allergy Clin Immunol. 2001; 107 (2):287–94. 10.1067/mai.2001.111141 [DOI] [PubMed] [Google Scholar]
- 17.Happo MS, Salonen RO, Hälinen AI, Jalava PI, Pennanen AS, Dormans JA, et al. Inflammation and tissue damage in mouse lung by single and repeated dosing of urban air coarse and fine particles collected from six European cities. Inhal Toxicol. 2010; 22 (5):402–16. 10.3109/08958370903527908 [DOI] [PubMed] [Google Scholar]
- 18.Budinger GR, McKell JL, Urich D, Foiles N, Weiss I, Chiarella SE, et al. Particulate matter-induced lung inflammation increases systemic levels of PAI-1 and activates coagulation through distinct mechanisms. PLoS One. 2011. 11; 6 (4):e18525 10.1371/journal.pone.0018525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wong CM, Thach TQ, Chau PY, Chan EK, Chung RY, Ou CQ, et al. Part 4. Interaction between air pollution and respiratory viruses: time-series study of daily mortality and hospital admissions in Hong Kong. Res Rep Health Eff Inst. 2010. November;(154):283–362. [PubMed] [Google Scholar]
- 20.Kakinoki Y, Ohashi Y, Tanaka A, Washio Y, Yamada K, Nakai Y, et al. Nitrogen dioxide compromises defence functions of the airway epithelium. Acta Otolaryngol Suppl. 1998; 538:221–6. [PubMed] [Google Scholar]
- 21.Devalia JL, Rusznak C, Herdman MJ, Trigg CJ, Tarraf H, Davies RJ. Effect of nitrogen dioxide and sulphur dioxide on airway response of mild asthmatic patients to allergen inhalation. Lancet. 1994; 344 (8938):1668–71. [DOI] [PubMed] [Google Scholar]
- 22.Hansel NN, McCormack MC, Kim V. The effects of air pollution and temperature on COPD. COPD. 2016; 13 (3):372–9. 10.3109/15412555.2015.1089846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Qiu H, Tan K, Long F, Wang L, Yu H, Deng R, et al. The burden of COPD morbidity attributable to the interaction between ambient air pollution and temperature in Chengdu, China. Int J Environ Res Public Health. 2018; 15 (3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Subdirección General de Desarrollo (2001) Instituto Nacional de Salud. Ministerio de Sanidad y Consumo [http://www.ingesa.msc.es/estadEstudios/documPublica/CMBD-2001.htm] Conjunto Mínimo Básico de Datos Hospitales de Insalud 2001.
- 25.Álvaro-Meca A, Díaz A, de Miguel Díez J, Resino R, Resino S. Environmental Factors Related to Pulmonary Tuberculosis in HIV-Infected Patients in the Combined Antiretroviral Therapy (cART) Era. PLoS One. 2016;11(11):e0165944 10.1371/journal.pone.0165944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rue H, Martino S, Lindgren F, Simpson D, Riebler A. INLA: Functions which allow to perform full Bayesian analysis of latent Gaussian models using Integrated Nested Laplace Approximaxion, 2014. R package version 00–1389624686.
- 27.Maclure M. The case-crossover design: a method for studying transient effects on the risk of acute events. Am J Epidemiol. 1991; 133 (2):144–53. 10.1093/oxfordjournals.aje.a115853 [DOI] [PubMed] [Google Scholar]
- 28.Perz JF, Armstrong GL, Farrington LA, Hutin YJ, Bell BP. The contributions of hepatitis B virus and hepatitis C virus infections to cirrhosis and primary liver cancer worldwide. J Hepatol. 2006; 45 (4):529–38. 10.1016/j.jhep.2006.05.013 [DOI] [PubMed] [Google Scholar]
- 29.Jaakkola JJ. Case-crossover design in air pollution epidemiology. Eur Respir J Suppl. 2003. May; 40:81s–85s. [DOI] [PubMed] [Google Scholar]
- 30.The R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: the R Foundation for Statistical Computing, 2011.
- 31.Zanobetti A, Schwartz J, Dockery DW. Airborne particles are a risk factor for hospital admissions for heart and lung disease. Environ Health Perspect. 2000; 108 (11):1071–7 10.1289/ehp.001081071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dominici F, Peng RD, Bell ML, Pham L, McDermott A, Zeger SL, et al. Fine particulate air pollution and hospital admission for cardiovascular and respiratory diseases. JAMA. 2006; 295 (10):1127–34. 10.1001/jama.295.10.1127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Medina-Ramón M, Zanobetti A, Schwartz J. The effect of ozone and PM10 on hospital admissions for pneumonia and chronic obstructive pulmonary disease: a national multicity study. Am J Epidemiol. 2006; 163 (6):579–88 10.1093/aje/kwj078 [DOI] [PubMed] [Google Scholar]
- 34.Anderson HR, Spix C, Medina S, Schouten JP, Castellsague J, Rossi G, et al. Air pollution and daily admissions for chronic obstructive pulmonary disease in 6 European cities: results from the APHEA project. Eur Respir J. 1997; 10 (5):1064–71. [DOI] [PubMed] [Google Scholar]
- 35.Sauerzapf V, Jones AP, Cross J. Environmental factors and hospitalisation for chronic obstructive pulmonary disease in a rural county of England. J Epidemiol Community Health. 2009; 63 (4):324–8. 10.1136/jech.2008.077024 [DOI] [PubMed] [Google Scholar]
- 36.Fusco D, Forastiere F, Michelozzi P, Spadea T, Ostro B, Arcà M, et al. Air pollution and hospital admissions for respiratory conditions in Rome, Italy. Eur Respir J. 2001; 17 (6):1143–50. [DOI] [PubMed] [Google Scholar]
- 37.Santus P, Russo A, Madonini E, Allegra L, Blasi F, Centanni S, How air pollution influences clinical management of respiratory diseases. A case-crossover study in Milan. Respir Res. 2012; 13:95 10.1186/1465-9921-13-95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Krachunov II, Kyuchukov NH, Ivanova ZI, Yanev NA, Hristova PA, Borisova ED, et al. Impact of air pollution and outdoor temperature on the rate of chronic obstructive pulmonary disease exacerbations. Folia Med (Plovdiv). 2017; 59(4):423–9. [DOI] [PubMed] [Google Scholar]
- 39.Almagro P, Hernandez C, Martinez-Cambor P, Tresserras R, Escarrabill J. Seasonality, ambient temperatures and hospitalizations for acute exacerbation of COPD: a population-based study in a metropolitan area. Int J Chron Obstruct Pulmon Dis. 2015; 10:899–908. 10.2147/COPD.S75710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Aga E, Samoli E, Touloumi G, Anderson HR, Cadum E, Forsberg B, et al. Short-term effects of ambient particles on mortality in the elderly: results from 28 cities in the APHEA2 project. Eur Respir J Suppl. 2003; 40:28s–33s. [DOI] [PubMed] [Google Scholar]
- 41.Sunyer J, Basagaña X. Particles, and not gases, are associated with the risk of death in patients with chronic obstructive pulmonary disease. Int J Epidemiol. 2001; 30 (5):1138–40. 10.1093/ije/30.5.1138 [DOI] [PubMed] [Google Scholar]
- 42.Donaldson GC, Wedzicha JA. The causes and consequences of seasonal variation in COPD exacerbations. Int J Chron Obstruct Pulmon Dis. 2014; 9:1101–10. 10.2147/COPD.S54475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wordley J, Walters S, Ayres JG. Short term variations in hospital admissions and mortality and particulate air pollution. Occup Environ Med. 1997; 54 (2):108–16. 10.1136/oem.54.2.108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kelsall JE, Samet JM, Zeger SL, Xu J. Air pollution and mortality in Philadelphia, 1974–1988. Am J Epidemiol. 1997; 146 (9):750–62. 10.1093/oxfordjournals.aje.a009351 [DOI] [PubMed] [Google Scholar]
- 45.Sooryanarain H, Elankumaran S. Environmental role in influenza virus outbreaks. Annu Rev Anim Biosci. 2015; 3:347–73. 10.1146/annurev-animal-022114-111017 [DOI] [PubMed] [Google Scholar]
- 46.Soriano JB, Ancochea J, Miravitlles M, García-Río F, Duran-Tauleria E, Muñoz L, et al. Recent trends in COPD prevalence in Spain: a repeated cross-sectional survey 1997–2007. Eur Respir J. 2010;36:758–65. 10.1183/09031936.00138409 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
We cannot legally distribute the data because the Spanish Ministry of Health, who is the owner of the data, does not allow us to share the data. This is so because when we ask the Ministry of Health for the data using the link: http://www.mscbs.gob.es/estadEstudios/estadisticas/estadisticas/estMinisterio/SolicitudCMBDdocs/Formulario_Peticion_Datos_CMBD.pdf, we must sign an engagement in which we legally compromise to: 1. Under no circumstances to export the entire database or make partial exports that could allow the generation of the same through aggregation or identification of natural persons or reporting units. 2. To destroy the file or data provided and all the copies made of it once elapsed the period of time for which the data is required. In any case all investigators can request the databases using the following contact information: http://www.mscbs.gob.es/estadEstudios/estadisticas/estadisticas/estMinisterio/SolicitudCMBDdocs/Formulario_Peticion_Datos_CMBD.pdf. The same compromises are acquired with the Spanish Meteorological Agency and the databases can be requested using the following contact information: http://www.aemet.es/es/eltiempo/observacion.