Abstract
We surveyed self-reported lifetime health conditions (using National Health and Aging Trends Study questions) and related driving reduction in a large multi-site older driver cohort (n = 2,990) from the AAA Longitudinal Research on Aging Drivers (LongROAD) Study’s baseline assessment. Those reporting reduced driving (n = 337) largely attributed reduction to musculoskeletal (29%), neurologic (13%), and ophthalmologic (10%) conditions. Women reported health condition-related driving reduction more often than men (14% versus 8%, p<.001). Mobility affects well-being; health professionals should consider that health conditions may cause older adults to reduce driving. Gender differences deserve attention in future research and education efforts.
Keywords: Older drivers, driving safety, health conditions, mobility
Mobility within the community is considered an instrumental activity of daily living (IADL), allowing an individual to live independently in the community (Altman, 2014; Roley et al., 2008). Optimal mobility promotes healthy aging by allowing people to access needed goods and services such as groceries and healthcare, to maintain social contacts, and to engage their communities (Satariano et al., 2012). In many areas of the country, travel by car is the only practical transportation option (National Research Council, 2005; Shaheen, Allen, & Liu, 2008). Thus, driving is an IADL that promotes health and independence (Dickerson, Reistetter, Davis, & Monahan, 2011; Dickerson, Reistetter, & Gaudy, 2013).
Many age-related health conditions may impair safe driving ability, including conditions affecting vision, cognition, neck flexibility, lower extremity strength, hearing, and reaction time (American Geriatrics Society & Pomidor, 2016; Choi, Mezuk, & Rebok, 2012; Classen, 2014). Although older drivers are in fewer crashes than their younger counterparts, age-related health conditions and the aging process itself may cause increased frailty in this population, which means older drivers are more likely to be injured in the case of a crash (Bandeen-Roche et al., 2015; Cicchino, 2015).
Many older drivers may reduce their driving (e.g., driving fewer miles or taking fewer trips) for various reasons, including in response to perceived physical, cognitive, or perceptual deficits (Betz & Lowenstein, 2010; Marie Dit Asse, Fabrigoule, Helmer, Laumon, & Lafont, 2014). Along with such perceived conditions, health condition diagnosis may also cause this population to limit their driving (Marshall, 2008). Unfortunately, driving reduction is associated with negative outcomes such as depressive symptoms and decreased life satisfaction (Chihuri et al., 2015; Harrison & Ragland, 2007).
Understanding the causes of driving reduction may help in identifying older adults who will eventually cease driving and may help guide intervention development to prolong safe driving (O’Connor, Edwards, Small, & Andel, 2012). Evidence exists that older adults are more receptive to driving cessation when they can anticipate and plan for this event (Betz, Scott, Jones, & DiGuiseppi, 2016). Health professionals (occupational therapists, physicians, and other providers) play a significant role in such planning by addressing driving safety related to health conditions and medications. Occupational therapists, in particular, play a key role in older driver safety: those with specialized training in driving may conduct comprehensive driving assessments (including a behind-the-wheel portion), while others assess IADLs (Lane et al., 2014). Occupational therapists may also be able to recommend driving rehabilitation services that provide education and assistive devices or driving modifications to help offset the effects of some of these conditions (Lane et al., 2014). Identifying and understanding specific health conditions that influence driving behaviors may help practitioners and families in properly addressing driving reduction and cessation (Betz et al., 2016).
The AAA Longitudinal Research on Aging Drivers (LongROAD) Study offers an opportunity to examine a large multi-site cohort of older drivers in the United States (US). Utilizing these data, we sought to: (1) describe self-reported lifetime prevalence of health conditions among older drivers and (2) examine the effect of these conditions on self-reported driving reductions in the past year.
METHODS
Design and Participants
For this cross-sectional study, we used baseline survey data from the AAA LongROAD Study. An overview of the study and methodology is described in detail elsewhere (Li et al., 2017). The AAA LongROAD Study aims to explore the roles of medical, behavioral, social, technological, and environmental factors in safe driving among older adults. The study enrolled older drivers in sites in five states (Ann Arbor, MI; Baltimore, MD; Cooperstown, NY; Denver, CO; and San Diego, CA). Data collected for the study include: self-reported and objectively-measured health, functioning, and driving behaviors; objective driving data (from a device collecting global positioning, accelerometer measurements, etc.); medical record information, medication history; and state motor vehicle driving records.
For study recruitment, we mailed and emailed invitations to patients registered at primary care clinics affiliated with AAA LongROAD study sites and then called potential participants for additional eligibility screening and recruitment. Inclusion criteria included: being 65–79 years old; possessing a valid driver’s license; driving at least once weekly, on average; no significant cognitive impairment (measured by initial medical chart review at some sites and the Six-Item Screener (Callahan, Unverzagt, Hui, Perkins, & Hendrie, 2002) during telephone screening at all sites) that might impede their ability to give fully informed consent; driving a primary vehicle that was a 1996 model or newer 80% or more of the time; having an accessible and unused OBDII port for installation of a study device to monitor driving; living in the study site area ≥10 months per year with no plans to move within five years; and not married to or living with a current LongROAD participant. Eligible and interested individuals scheduled in-person sessions, during which written informed consent was obtained. Each site’s respective Institutional Review Board gave study approval.
Measures
During in-person sessions, research staff administered questionnaires about health, functioning, and driving. For this analysis, we utilized baseline variables concerning health conditions and related driving reduction. Research staff asked participants: “Have you decreased your driving due to a health problem in the past 12 months?” Then, using a modified version of the National Health and Aging Trends Study questionnaire (Montaquila, Freedman, Edwards, & Kasper, 2012), research staff asked participants if during their lifetimes they had ever had (or their doctor had ever told them that they had) any of 55 health conditions. Participants who responded “yes” to having decreased their driving in the past 12 months were prompted to answer whether any of the specific conditions they had reported had caused them to reduce driving.
Data Management
We entered all project data (except personally-identifiable information, which was maintained at enrollment sites) into a secure web-based system. Research staff stored and managed data in a relational database using Scientific Information Retrieval (SIR/XS) software at the Data Coordinating Center (DCC) at Columbia University Medical Center. The DCC provided fully de-identified, cleaned datasets for analysis.
Analysis
All 2,990 LongROAD study participants were included in this analysis. We grouped health conditions into categories based on organ system (as shown in Table 2). Any conditions affecting more than one organ system were categorized according to the system most likely to directly affect driving (e.g., for deep vein thrombosis, the musculoskeletal category) based on the Clinician’s Guide to Assessing and Counseling Older Drivers and study team discussion (American Geriatrics Society & Pomidor, 2016). We also categorized health conditions affecting multiple organ systems separately if prevalence was high (e.g., cancer). Other, lower frequency conditions affecting more than one organ system were grouped into a “miscellaneous” category.
Table 2.
Self-reported health condition groups and related decreases in driving among those with the condition and among all who had reduced driving for any condition
| Lifetime diagnosis | Decreased driving in past 12 months | |||||||
|---|---|---|---|---|---|---|---|---|
| Self-Reported Condition Groups | n | % | 95% CI | n | %a | 95% CI | %b | 95% CI |
| Musculoskeletal | 2286 | 76.5 | 74.9–78.0 | 96 | 4.2 | 3.4–5.0 | 28.5 | 23.6–33.3 |
| Neurologic | 1315 | 44.0 | 42.2–45.8 | 43 | 3.3 | 2.3–4.2 | 12.8 | 9.2–16.3 |
| Ophthalmologic | 1447 | 48.4 | 46.6–50.2 | 34 | 2.3 | 1.6–3.1 | 10.1 | 6.9–13.3 |
| Cancer | 980 | 32.8 | 31.1–34.5 | 26 | 2.7 | 1.6–3.7 | 7.7 | 4.9–10.6 |
| Cardiovascular | 1930 | 64.5 | 62.8–66.3 | 15 | 0.8 | 0.4–1.2 | 4.5 | 2.2–6.7 |
| Psychologic | 817 | 27.3 | 25.7–28.9 | 7 | 0.9 | 0.2–1.5 | 2.1 | 0.5–3.6 |
| Metabolic | 933 | 31.2 | 29.5–32.9 | 5 | 0.5 | 0.1–1.0 | 1.5 | 0.2–2.8 |
| Respiratory | 584 | 19.5 | 18.1–21.0 | 3 | 0.5 | 0.0–1.1 | 0.9 | 0.0–1.9 |
| Gastrointestinal | 156 | 5.2 | 4.4–6.0 | 1 | 0.6 | 0.0–1.9 | 0.3 | 0.0–0.9 |
| Miscellaneous | 141 | 4.7 | 4.0–5.5 | 1 | 0.7 | 0.0–2.1 | 0.3 | 0.0–0.9 |
| Ear, Nose, & Throat | 33 | 1.1 | 0.7–1.5 | 0 | 0.0 | - | 0.0 | - |
| Genitourinary | 37 | 1.2 | 0.8–1.6 | 0 | 0.0 | - | 0.0 | - |
| Hematologic | 94 | 3.1 | 2.5–3.8 | 0 | 0.0 | - | 0.0 | - |
| Renal | 75 | 2.5 | 2.0–3.1 | 0 | 0.0 | - | 0.0 | - |
Proportion that have decreased driving in the past 12 months due to each condition, among all persons with that condition.
Proportion that have decreased driving in the past 12 months due to each condition, among those that had reduced their driving due to any health condition (n = 337).
Our team described demographic, health, and driving characteristics using percentages with 95% confidence intervals (95%CI) for dichotomous variables or medians with interquartile ranges (IQR) for continuous variables. The data met the assumptions for the Pearson’s chi-squared test (i.e., the data set is sufficiently large and the variables are categorical and independent in nature), so we utilized this statistical test to compare population characteristics to driving reduction based on health condition group.
RESULTS
Table 1 illustrates participant demographics. Of the 2,990 LongROAD study participants, 41.6% were aged 65–69 years, 34.7% were aged 70–74 years, and 23.7% were aged 75–79 at enrollment. More than half (53.0%) were female; most were White and non-Hispanic. Two-thirds were married, and most had at least a bachelor’s degree, owned their home, and had an annual household income ≥$50,000.
Table 1.
Demographic and health characteristics, by reported self-reduction of driving for any health condition in the past 12 months (N = 2990)
| Reduced Driving For Any Condition |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| Characteristic | Total | Yes | No | p | |||||
| n | % | n | % | 95% CI | n | % | 95% CI | ||
| Total | 2990 | 100 | 337 | 11.3 | 10.2–12.5 | 2657 | 88.7 | 87.7–90.0 | -- |
| Age | 0.864 | ||||||||
| 65–69 | 1243 | 41.6 | 138 | 11.1 | 9.4–13.0 | 1105 | 88.9 | 87.0–90.6 | |
| 70–74 | 1037 | 34.7 | 115 | 11.1 | 9.3–13.2 | 922 | 88.9 | 86.8–90.7 | |
| 75–79 | 710 | 23.7 | 84 | 11.8 | 9.6–14.5 | 626 | 88.2 | 85.5–90.4 | |
| Gender | <0.001 | ||||||||
| Male | 1404 | 47.0 | 112 | 8.0 | 6.6–9.6 | 1292 | 92.0 | 90.4–93.4 | |
| Female | 1586 | 53.0 | 225 | 14.2 | 12.5–16.0 | 1361 | 85.8 | 84.0–87.5 | |
| Race | 0.480 | ||||||||
| White | 2616 | 87.5 | 291 | 11.1 | 10.0–12.4 | 2325 | 88.9 | 87.6–90.0 | |
| Black | 213 | 7.1 | 22 | 10.3 | 6.7–15.4 | 191 | 89.7 | 87.6–93.3 | |
| Asian | 72 | 2.4 | 11 | 15.3 | 8.2–26.1 | 61 | 84.7 | 73.9–91.8 | |
| Other | 76 | 2.5 | 10 | 13.2 | 6.8–23.3 | 66 | 86.8 | 76.7–93.2 | |
| Don’t Know/Refused/NA | 13 | 0.4 | 3 | 23.1 | 6.2–54.0 | 10 | 76.9 | 46.0–93.8 | |
| Hispanic | 0.008 | ||||||||
| Yes | 83 | 2.8 | 17 | 20.5 | 12.7–31.0 | 66 | 79.5 | 69.0–87.3 | |
| No | 2794 | 93.4 | 310 | 11.1 | 10.0–12.3 | 2484 | 88.9 | 87.7–90.0 | |
| Education | 0.870 | ||||||||
| ≤Some College | 1062 | 35.5 | 121 | 11.3 | 9.5–13.3 | 941 | 88.7 | 86.7–90.5 | |
| Bachelors | 698 | 23.3 | 82 | 11.7 | 9.4–14.1 | 616 | 88.3 | 85.9–90.7 | |
| ≥Masters | 1221 | 40.8 | 134 | 11.0 | 9.3–12.9 | 1087 | 89.0 | 87.1–90.7 | |
| Living Situation | |||||||||
| Owned Home | 2599 | 86.9 | 290 | 11.2 | 10.0–12.4 | 2309 | 88.8 | 87.6–90.0 | 0.564 |
| Rented Home | 275 | 9.2 | 37 | 13.5 | 9.8–18.2 | 238 | 86.5 | 81.8–90.2 | |
| With Family Member | 60 | 2.0 | 5 | 8.3 | 3.1–19.1 | 55 | 91.7 | 80.9–96.9 | |
| Other | 53 | 1.8 | 5 | 9.4 | 3.5–21.4 | 48 | 90.6 | 78.6–96.5 | |
| Marital Status | 0.383 | ||||||||
| Married/Living with Partner | 1974 | 66.0 | 215 | 10.9 | 9.6–12.4 | 1759 | 89.1 | 87.6–90.4 | |
| Other | 986 | 33.0 | 118 | 12.0 | 10.0–14.2 | 868 | 88.0 | 85.8–90.0 | |
| Income | 0.020 | ||||||||
| ≤$49,999 | 775 | 25.9 | 106 | 13.7 | 11.4–16.3 | 669 | 86.3 | 83.7–88.6 | |
| $50,000-$79,999 | 719 | 24.0 | 69 | 9.6 | 7.6–12.0 | 650 | 90.4 | 88.0–92.4 | |
| $80,000-$99,999 | 431 | 14.4 | 57 | 13.2 | 10.2–16.9 | 374 | 86.8 | 83.1–89.8 | |
| ≥$100,000 | 959 | 35.7 | 95 | 9.9 | 8.1–12.0 | 864 | 90.1 | 88.0–91.9 | |
For lifetime diagnoses of specific health conditions, the highest proportions reported having ever had or been diagnosed with a total of three (12.3%), four (13.9%), or five (12.8%) conditions. Only 2.0% reported having no conditions, with a maximum of 20 diagnoses reported (median: 5; IQR 3–7; data not shown). According to Table 2, which shows self-reported lifetime health condition groups versus driving reduction in the past year, most participants self-reported musculoskeletal (76.5%) or cardiovascular (64.5) diagnoses.
Table 3 highlights specific self-reported lifetime health conditions versus driving reduction in the past year. Overall, 337 (11.3%) participants reported having decreased their driving for any health condition(s) in the past year (see Table 1). Of the most common self-reported health conditions and problems, participants with ‘joint pain or joint swelling’ and ‘other arthritis’ were most likely to report driving reduction (n = 48 and 36, respectively). Among all health categories, musculoskeletal diagnoses were the most common self-reported cause of driving reduction, affecting 28.5% of those who decreased driving. Some musculoskeletal conditions that were often associated with reported driving reduction included hip and knee replacements (8.8% [17 of 194] and 8.4% [26 of 309] of participants, respectively).
Table 3.
Self-reported health conditions and related decreases in driving among those with the condition and among all who had reduced driving for any condition
| Lifetime diagnosis | Decreased driving in past 12 months | |||||||
|---|---|---|---|---|---|---|---|---|
| Self-Reported Condition(s) | n | % | 95% CI | n | %a | 95% CI | %b | 95% CI |
| Musculoskeletal | ||||||||
| Joint pain or joint swelling | 1583 | 52.9 | 51.1–54.7 | 48 | 3 | 2.3–4.0 | 14.2 | 10.8–18.5 |
| Other arthritis | 1555 | 52 | 50.2–53.8 | 36 | 2.3 | 1.6–3.2 | 10.7 | 7.7–14.6 |
| Knee replacement | 309 | 10.3 | 9.3–11.5 | 26 | 8.4 | 5.7–12.2 | 7.7 | 5.2–11.2 |
| Hip replacement | 194 | 6.5 | 5.6–7.4 | 17 | 8.8 | 5.3–13.9 | 5 | 3.1–8.0 |
| Fracture of the hip or forearm | 217 | 7.3 | 6.4–8.3 | 8 | 3.7 | 1.7–7.4 | 2.4 | 1.1–4.8 |
| Peripheral neuropathy | 249 | 8.3 | 7.4–9.4 | 5 | 2 | 0.7–4.9 | 1.5 | 0.5–3.6 |
| Deep vein thrombosis | 110 | 3.7 | 3.1–4.4 | 3 | 2.7 | 0.7–8.4 | 0.9 | 0.2–2.8 |
| Gout | 239 | 8 | 7.1–9.0 | 3 | 1.3 | 0.3–3.9 | 0.9 | 0.2–2.8 |
| Osteoporosis | 453 | 15.2 | 13.9–16.5 | 3 | 0.7 | 0.2–2.1 | 0.9 | 0.2–2.8 |
| Peripheral artery surgery | 30 | 1 | 0.7–1.5 | 2 | 6.7 | 1.2–23.5 | 0.6 | 0.1–2.4 |
| Rheumatoid arthritis | 147 | 4.9 | 4.2–5.7 | 2 | 1.4 | 0.2–5.3 | 0.6 | 0.1–2.4 |
| Other musculoskeletal problem | 30 | 1 | 0.7–1.5 | 1 | 3.3 | 0.2–19.1 | 0.3 | 0.0–1.9 |
| Degenerative bone/joint disease | 12 | 0.4 | 0.2–0.7 | 0 | 0 | -- | 0 | -- |
| Edema | 3 | 0.1 | 0.0–0.3 | 0 | 0 | -- | 0 | -- |
| Knee problem | 9 | 0.3 | 0.2–0.6 | 0 | 0 | -- | 0 | -- |
| Lymphedema | 3 | 0.1 | 0.0–0.3 | 0 | 0 | -- | 0 | -- |
| Neck/back problem | 72 | 2.4 | 1.9–3.0 | 0 | 0 | -- | 0 | -- |
| Shoulder Problem | 26 | 0.9 | 0.5–1.3 | 0 | 0 | -- | 0 | -- |
| Other lower extremity problem | 22 | 0.7 | 0.4–1.1 | 0 | 0 | -- | 0 | -- |
| Other upper extremity problem | 35 | 1.2 | 0.8–1.6 | 0 | 0 | -- | 0 | -- |
| Neurologic | ||||||||
| Vertigo | 385 | 12.9 | 11.7–14.1 | 14 | 3.6 | 2.1–6.2 | 4.2 | 2.4–7.0 |
| Migraine headaches | 360 | 12 | 10.9–13.3 | 8 | 2.2 | 1.0–4.5 | 2.4 | 1.1–4.8 |
| Movement disorder | 118 | 3.9 | 3.3–4.7 | 8 | 6.8 | 3.2–13.3 | 2.4 | 1.1–4.8 |
| Sleep disorders | 598 | 20 | 18.6–21.5 | 7 | 1.2 | 0.5–2.5 | 2.1 | 0.9–4.4 |
| Stroke | 143 | 4.8 | 4.1–5.6 | 7 | 4.9 | 2.3–9.9 | 2.1 | 0.9–4.5 |
| Traumatic brain injury | 59 | 2 | 1.5–2.6 | 4 | 6.8 | 2.2–17.3 | 1.2 | 0.4–3.2 |
| Parkinson’s disease | 22 | 0.7 | 0.5–1.1 | 2 | 9.1 | 1.6–30.6 | 0.6 | 0.1–2.4 |
| Multiple sclerosis | 19 | 0.6 | 0.4–1.0 | 1 | 5.3 | 0.9–25.0 | 0.3 | 0.0–1.9 |
| Seizure disorder | 31 | 1 | 0.7–1.5 | 1 | 3.2 | 0.2–18.5 | 0.3 | 0.0–1.9 |
| Amyotrophic lateral sclerosis | 1 | 0 | -- | 0 | 0 | -- | 0 | -- |
| Brain aneurysm | 5 | 0.2 | 0.1–0.4 | 0 | 0 | -- | 0 | -- |
| Brain surgery | 3 | 0.1 | 0.0–0.3 | 0 | 0 | -- | 0 | -- |
| Brain tumor | 24 | 0.8 | 0.5–1.2 | 0 | 0 | -- | 0 | -- |
| CNS infection | 4 | 0.1 | 0.0–0.4 | 0 | 0 | -- | 0 | -- |
| Cognitive impairment | 11 | 0.4 | 0.2–0.7 | 0 | 0 | -- | 0 | -- |
| Dystonia | 2 | 0.1 | 0.0–0.3 | 0 | 0 | -- | 0 | -- |
| Headache | 2 | 0.1 | 0.0–0.3 | 0 | 0 | -- | 0 | -- |
| Intracranial hemorrhage | 1 | 0 | -- | 0 | 0 | -- | 0 | -- |
| Neuralgia | 4 | 0.1 | 0.0–0.4 | 0 | 0 | -- | 0 | -- |
| Tourette’s syndrome | 1 | 0 | -- | 0 | 0 | -- | 0 | -- |
| Other neurologic problem | 24 | 0.8 | 0.5–12.1 | 0 | 0 | -- | 0 | -- |
| Ophthalmologic | ||||||||
| Cataracts | 1332 | 44.5 | 42.8–46.4 | 29 | 2.2 | 0.0–4.4 | 8.6 | 5.9–12.3 |
| Glaucoma | 255 | 8.5 | 7.6–9.6 | 5 | 2 | 0.7–4.8 | 1.5 | 0.5–3.6 |
| Diabetic retinopathy | 54 | 1.8 | 1.4–2.4 | 1 | 1.9 | 1.5–3.2 | 0.3 | 0.0–1.9 |
| Cornea problem | 7 | 0.2 | 0.1–0.5 | 0 | 0 | -- | 0 | -- |
| Macular problem | 26 | 0.9 | 0.5–1.3 | 0 | 0 | -- | 0 | -- |
| Other visual problem | 20 | 0.7 | 0.4–1.1 | 0 | 0 | -- | 0 | -- |
| Retinal problem | 17 | 0.6 | 0.3–0.9 | 0 | 0 | -- | 0 | -- |
| Cancer | 980 | 32.8 | 31.1–34.5 | 26 | 2.7 | 1.8–3.9 | 7.7 | 5.2–11.2 |
| Cardiovascular | ||||||||
| Myocardial infarction | 198 | 6.6 | 5.8–7.6 | 5 | 2.5 | 0.9–6.1 | 1.5 | 0.5–3.6 |
| Fainting | 166 | 5.6 | 4.8–6.4 | 4 | 2.4 | 0.8–6.4 | 1.2 | 0.4–3.2 |
| High blood pressure | 1688 | 56.5 | 54.7–58.2 | 4 | 0.2 | 0.1–0.6 | 1.2 | 0.4–3.2 |
| Coronary bypass surgery | 114 | 3.8 | 3.2–4.6 | 3 | 2.6 | 0.7–8.1 | 0.9 | 0.2–2.8 |
| Atrial fibrillation | 304 | 10.2 | 9.1–11.3 | 2 | 0.7 | 0.1–2.6 | 0.6 | 0.1–2.4 |
| Coronary angioplasty | 185 | 6.2 | 5.4–7.1 | 1 | 0.5 | 0.0–3.4 | 0.3 | 0.0–1.9 |
| Valve disorder/replacement | 18 | 0.6 | 0.4–1.0 | 1 | 5.6 | 0.8–26.5 | 0.3 | 0.0–1.9 |
| Arrhythmia | 39 | 1.3 | 0.9–1.8 | 0 | 0 | -- | 0 | -- |
| Cardiomyopathy | 14 | 0.5 | 0.3–0.8 | 0 | 0 | -- | 0 | -- |
| Carotid artery surgery | 49 | 1.6 | 1.2–2.2 | 0 | 0 | -- | 0 | -- |
| Coronary heart disease | 14 | 0.5 | 0.3–0.8 | 0 | 0 | -- | 0 | -- |
| Heart surgery | 3 | 0.1 | 0.0–0.3 | 0 | 0 | -- | 0 | -- |
| Hypercholesterolemia | 10 | 0.3 | 0.2–0.6 | 0 | 0 | -- | 0 | -- |
| Vasculitis | 1 | 0 | -- | 0 | 0 | -- | 0 | -- |
| Vessel stenosis/dissection/aneurysm | 17 | 0.6 | 0.3–0.9 | 0 | 0 | -- | 0 | -- |
| Other cardiovascular problem | 13 | 0.4 | 0.2–0.8 | 0 | 0 | -- | 0 | -- |
| Psychologic | ||||||||
| Depression | 584 | 19.5 | 18.1–21.0 | 7 | 1.2 | 0.5–2.6 | 2.1 | 0.9–4.4 |
| Anxiety disorder | 336 | 11.2 | 10.1–12.4 | 3 | 0.9 | 0.2–2.8 | 0.9 | 0.2–2.8 |
| Attention deficit disorder | 31 | 1 | 0.7–1.5 | 1 | 3.2 | 0.2–18.5 | 0.3 | 0.0–1.9 |
| Post-traumatic stress disorder | 89 | 3 | 2.4–3.7 | 1 | 1.1 | 0.1–7.0 | 0.3 | 0.0–1.9 |
| Psychotic disorder | 19 | 0.6 | 0.4–1.0 | 1 | 5.3 | 0.9–25.0 | 0.3 | 0.0–1.9 |
| Attention deficit hyperactivity disorder | 57 | 1.9 | 1.5–2.5 | 0 | 0 | -- | 0 | -- |
| Eating disorders | 1 | 0 | -- | 0 | 0 | -- | 0 | -- |
| Personality disorder | 5 | 0.2 | 0.1–0.4 | 0 | 0 | -- | 0 | -- |
| Substance abuse/alcohol dependency | 81 | 2.7 | 2.2–3.4 | 0 | 0 | -- | 0 | -- |
| Other mental health problem | 1 | 0 | -- | 0 | 0 | -- | 0 | -- |
| Metabolic | ||||||||
| Diabetes mellitus | 483 | 16.2 | 14.9–17.5 | 3 | 0.6 | 0.0–2.0 | 0.9 | 0.2–2.8 |
| Thyroid imbalance | 533 | 17.8 | 13.5–19.3 | 2 | 0.4 | 0.1–1.5 | 0.6 | 0.1–2.4 |
| Adrenal problem | 1 | 0 | -- | 0 | 0 | -- | 0 | -- |
| Diabetes insipidus | 2 | 0.1 | 0.0–0.3 | 0 | 0 | -- | 0 | -- |
| Other metabolic problem | 11 | 0.4 | 0.2–0.7 | 0 | 0 | -- | 0 | -- |
| Respiratory | ||||||||
| Asthma | 368 | 12.3 | 11.2–13.5 | 2 | 0.5 | 0.0–2.2 | 0.6 | 0.1–2.4 |
| Chronic obstructive pulmonary disease | 142 | 4.7 | 4.0–5.5 | 1 | 0.7 | -- | 0.3 | 0.0–1.9 |
| Autoimmune Disease | 2 | 0.1 | 0.0–0.3 | 0 | 0 | -- | 0 | -- |
| Pulmonary embolism | 114 | 3.8 | 3.2–4.6 | 0 | 0 | -- | 0 | -- |
| Other respiratory problem | 27 | 0.9 | 0.6–1.3 | 0 | 0 | -- | 0 | -- |
| Gastrointestinal | ||||||||
| GI injury/surgery | 47 | 1.6 | 1.2–2.1 | 1 | 2.1 | 0.1–12.7 | 0.3 | 0.0–1.9 |
| Liver disease | 21 | 0.7 | 0.4–1.1 | 0 | 0 | -- | 0 | -- |
| Other GI problem | 94 | 3.1 | 2.5–3.9 | 0 | 0 | -- | 0 | -- |
| Ear, Nose, and Throat | ||||||||
| Ear/Hearing problem | 19 | 0.6 | 0.4–1.0 | 0 | 0 | -- | 0 | -- |
| Sinus problem | 5 | 0.2 | 0.1–0.4 | 0 | 0 | -- | 0 | -- |
| Other ENT problem | 8 | 0.3 | 0.3–0.4 | 0 | 0 | -- | 0 | -- |
| Genitourinary | ||||||||
| Bladder problem | 7 | 0.2 | 0.1–0.5 | 0 | 0 | -- | 0 | -- |
| Endometriosis | 2 | 0.1 | 0.0–0.3 | 0 | 0 | -- | 0 | -- |
| GU infection | 2 | 0.1 | 0.0–0.3 | 0 | 0 | -- | 0 | -- |
| Ovarian problem | 4 | 0.1 | 0.0–0.4 | 0 | 0 | -- | 0 | -- |
| Prostate problem | 17 | 0.6 | 0.3–0.9 | 0 | 0 | -- | 0 | -- |
| Other GU problem | 6 | 0.2 | 0.1–0.5 | 0 | 0 | -- | 0 | -- |
| Hematologic | -- | |||||||
| Anemia | 5 | 0.2 | 0.1–0.4 | 0 | 0 | -- | 0 | -- |
| Coagulation disorder | 84 | 2.8 | 2.3–3.5 | 0 | 0 | -- | 0 | -- |
| Neutropenia | 1 | 0 | -- | 0 | 0 | -- | 0 | -- |
| Thrombocytosis | 2 | 0.1 | 0.0–0.3 | 0 | 0 | -- | 0 | -- |
| Other hematologic problem | 2 | 0.1 | 0.0–0.3 | 0 | 0 | -- | 0 | -- |
| Renal | ||||||||
| Chronic renal failure | 47 | 1.6 | 1.1–2.1 | 0 | 0 | -- | 0 | -- |
| Other kidney disease | 32 | 1.1 | 0.7–1.5 | 0 | 0 | -- | 0 | -- |
| Miscellaneous | ||||||||
| Allergies | 9 | 0.3 | 0.2–0.6 | 0 | 0 | -- | 0 | -- |
| Chronic pain | 4 | 0.1 | 0.0–0.4 | 0 | 0 | -- | 0 | -- |
| Scleroderma | 6 | 0.2 | 0.1–0.5 | 0 | 0 | -- | 0 | -- |
| Skin problem | 14 | 0.5 | 0.3–0.8 | 0 | 0 | -- | 0 | -- |
| Systemic lupus erythematosus | 6 | 0.2 | 0.1–0.5 | 0 | 0 | -- | 0 | -- |
| Other infectious condition | 22 | 0.7 | 0.5–1.1 | 0 | 0 | -- | 0 | -- |
| Other systemic problem | 11 | 0.4 | 0.2–0.7 | 0 | 0 | -- | 0 | -- |
| Other miscellaneous problem | 36 | 1.2 | 0.9–1.7 | 0 | 0 | -- | 0 | -- |
Proportion that have decreased driving in the past 12 months due to each condition, among all persons with that condition.
Proportion that have decreased driving in the past 12 months due to each condition, among those that had reduced their driving due to any health condition (n = 337).
Other commonly cited categories of health conditions among those who reduced their driving were neurologic (15.4%) and ophthalmologic (10.4%) health conditions, followed by cancer (7.7%). Common self-reported diagnoses within the cancer category included breast (19.1%, 5 of 26 reduced driving) and colon (15.4%, 4 of 26) cancers. Some health conditions, although rare, led to higher proportions of reported driving reductions in the past year. For example, 9.1% (2 of 22) of participants reporting a lifetime diagnosis of Parkinson’s disease consequently decreased driving in the past year. Other less common conditions reported to cause driving reduction included: traumatic brain injury, affecting 6.8% (4 of 59 reduced driving) of participants; peripheral artery surgery (6.7%, 2 of 30); psychotic disorders (e.g., schizophrenia and bipolar disorder; 5.3%, 1 of 19); and multiple sclerosis (also 5.3%, 1 of 19). Among those reporting driving reduction for health conditions in the past year, 133 participants (39.5%) did not specify conditions that caused them to do so.
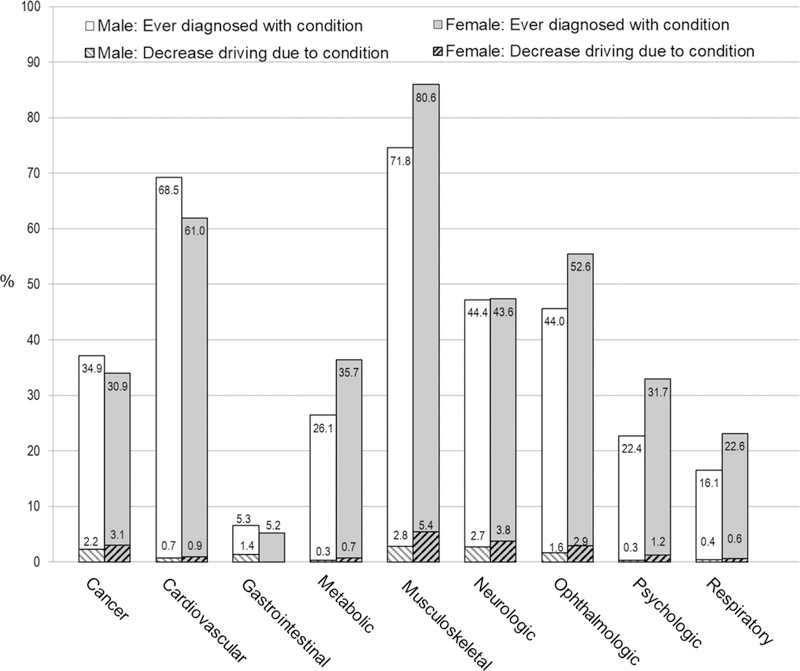
Gender influenced both health condition and driving reduction prevalence (see Figures 1 and 2). Women reported more lifetime medical conditions than men (mean: 5.6 vs 5.1; p <.001) and were more likely to have ophthalmologic, metabolic, psychologic, musculoskeletal, or respiratory condition diagnoses, while men were more likely to have cancer or cardiovascular condition diagnoses. Women were more likely than men to report having reduced their driving due to a health condition in the past year (14.2% versus 8.0%, p <.001; see Table 1), particularly for musculoskeletal or ophthalmologic problems (see Figure 1). Among 1,278 women with musculoskeletal problems, 5.3% reported reducing their driving in the past year due to these conditions; among 1,008 men with musculoskeletal problems, only 2.8% reported such reductions due to these conditions. Similarly, among 830 women with ophthalmologic conditions, 2.9% reported reducing driving in the past year; among the 617 men with ophthalmologic conditions, only 1.6% did so.
Figure 1.
Proportion of participants reporting prior diagnoses (lifetime) and reduced driving (past 12 months), by diagnosis category gender
Condition categories with zero reported reduced driving are not shown.
Figure 2.
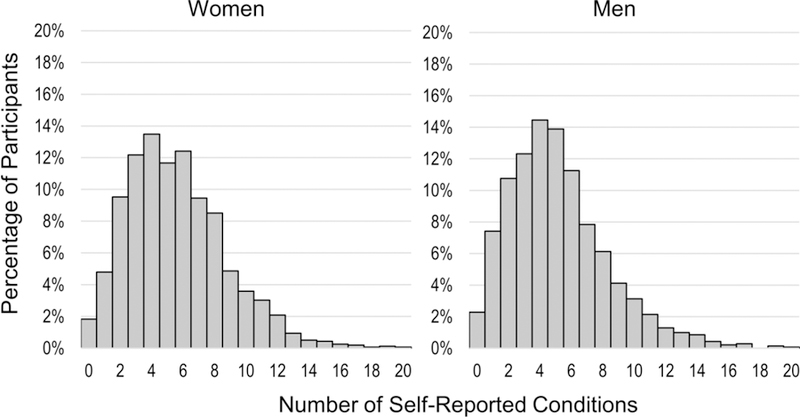
Number of lifetime self-reported health conditions per participant, by gender
DISCUSSION
This cross-sectional study of a large multi-site sample of older drivers yielded three main findings. First, musculoskeletal health conditions were the most prevalent self-reported lifetime diagnoses and were associated with the most reports of driving reductions in the past year. Second, several less common health conditions were also associated with self-reported driving reduction. Finally, in line with prior work, women were more likely than men to report reducing driving due to health conditions (Choi, Adams, & Kahana, 2013; D’Ambrosio, Donorfio, Coughlin, Mohyde, & Meyer, 2008).
Musculoskeletal health conditions (e.g., arthritis), symptoms (joint pain and swelling), and surgeries (hip and knee replacement) were associated with reported driving reduction in this cohort. Such conditions may thus further affect quality of life through reduced mobility (American Geriatrics Society & Pomidor, 2016). Pain medication used for such musculoskeletal conditions may also have confounding effects on reported reduction, as dizziness or other medication side effects might be the primary factors leading to driving adjustment or reduction (Hetland & Carr, 2014). Physical health conditions have previously been documented to require driving restrictions in some individuals, such as the recommended six weeks after knee and hip replacements (Braitman & McCartt, 2008; Ragland, Satariano, & MacLeod, 2004). Other than musculoskeletal conditions, neurologic and ophthalmologic conditions and cancer also were associated with self-reported driving reduction. Past research supports the role of ophthalmologic conditions in driving reduction (American Geriatrics Society & Pomidor, 2016), and some studies have examined the role of cancer on driving habits (Lyman, McGwin, & Sims, 2001; Ragland, Satariano, & MacLeod, 2005; Yuen, Gillespie, Day, Morgan, & Burik, 2007). Considering that some people reduced driving because of this diagnosis, future research should further consider the types of cancer and the mechanisms that may cause this to occur. Additionally, psychologic conditions like depression and anxiety also caused some driving reduction. Clinicians should keep in mind the potential effects of mental illness on driving habits. Other conditions may result in temporary driving restrictions that may also cause older adults to decrease driving. For example, cardiac valve replacement requires 4 weeks of driving restriction, along with other conditions like seizures (3–12 months), stroke/TIA (varying times), and more (American Geriatrics Society & Pomidor, 2016; Fisk, Owsley, & Pulley, 1997; Krauss, Ampaw, & Krumholz, 2001). Clinicians should be mindful of such driving restriction periods and should counsel their patients accordingly.
Some less prevalent health conditions (e.g., Parkinson’s disease, traumatic brain injury) were also associated with high reported rates of driving reduction. Even considering the low prevalence of these conditions, health professionals like occupational therapists tend to be aware of the effects such neurological conditions have on driving through symptoms like lack of awareness or freezing gait (Crizzle et al., 2013; Hassan, King, & Watt, 2015; Pachana & Petriwskyj, 2006). Clinicians should continue to be cognizant of the increased effects of these conditions on older adult driving habits compared to other conditions. It is also important to consider that the LongROAD cohort contained predominantly active, healthy adults without cognitive problems at enrollment. Therefore, it is possible that some of these conditions are more prevalent in the general population than in the LongROAD cohort (ex: Parkinson’s disease: 1.0% versus 0.7% in this cohort) (Tysnes & Storstein, 2017). Additionally, conditions such as diabetes, arrhythmia, sleep disorders, seizure disorders, and depression were all previously documented to have detrimental effects on driving ability (Binns & Camm, 2002; Cox et al., 2006; Hill et al., 2017; Krumholz, 2009; Tregear, Reston, Schoelles, & Phillips, 2009) and were not associated with high rates of reported driving reduction in our sample. Because factors like already-treated or controlled conditions and better-than-average health in LongROAD participants may have confounded this association, future research should examine the potential relationships between newly-diagnosed health conditions and driving reduction.
Our findings have implications for occupational therapists and other health professionals because understanding the effects of health conditions on older adults’ driving ability and providing them with relevant mobility counseling may help older drivers avoid premature driving reductions or cessation (American Geriatrics Society & Pomidor, 2016). Educating practitioners on health condition-related driving reduction may allow them to better prepare older adults and their families for the consequences of driving reduction. Furthermore, disseminating information about the condition-specific mechanisms that may cause driving reduction may help these health professionals to effectively plan interventions that may address such consequences. In general, provision of condition-specific guidelines for practitioners, patients, and families might also be helpful in times of temporary changes (e.g., after joint replacement) (Abbas & Waheed, 2011; Pierson, Earles, & Wood, 2003). For example, the Driving Pathways by Diagnosis Sheets, which provide driving evaluation and therapy recommendations for conditions such as arthritis, Parkinson’s disease, etc. may be a valuable resource for health professionals (Touchinsky, Chew, & Davis, 2014). One study found that although stroke affected driving ability, clinicians were unlikely to counsel stroke patients about driving reduction (Fisk et al., 1997). Also, more general anticipatory guidance about future driving retirement may benefit patients with progressive disorders, such as dementia or Parkinson’s disease.
Finally, although female participants reported having roughly equal amounts of lifetime health condition diagnoses as male participants, they reported higher rates of driving reduction due to health conditions. While this may stem, in part, from differences in age of condition onset or specific condition diagnosis, prior work suggests women are more likely than men to visit and consult a doctor about potential health problems and to reduce driving with age (Choi et al., 2013; Xu & Borders, 2003). Higher rates of driving reduction in women might be attributed to lower confidence in driving ability, which could be exacerbated by health condition diagnosis (Charlton et al., 2006; Meng & Siren, 2012; Siren, Hakamies-Blomqvist, & Lindeman, 2004). Alternatively, men may be overconfident or feel pressured to continue driving as part of a traditional provider role (Brabyn, Schneck, Lott, & Haegerström-Portnoy, 2005; Charlton et al., 2006; Molnar et al., 2014). In recognition of this, health education efforts for older drivers should also focus on increasing self-efficacy around driving behaviors. Premature driving reduction and cessation may cause decreased quality of life, but counseling from a knowledgeable health professional, along with proper treatment and referral to specialists, may deter early driving cessation and resulting detrimental effects (Chihuri et al., 2015; Stressel, Hegberg, & Dickerson, 2014). Tools such as the Assessment of Readiness for Mobility Transition may assist clinicians in individualizing mobility transition services for older adults (Meuser, Berg-Weger, Chibnall, Harmon, & Stowe, 2013).
LIMITATIONS
Limitations include that the LongROAD baseline enrollment assessment did not collect data regarding when participants developed health conditions or how soon after the diagnoses they decreased driving. Future studies will have medical record information available and may be able to address some of these questions. In addition, in some cases, a participant may have not reduced driving in the past year due to a diagnosed health condition because the condition was treated or resolved. For example, nearly half of the study population reported having cataracts, but only 2% of participants limited driving as a result; many participants may have had cataract surgery to restore vision, and therefore driving ability. Through the LongROAD cohort’s longitudinal follow-up, we may better address temporal relationships between health conditions and driving behaviors.
Some health conditions may have been double-counted among participants who decreased driving, due to co-occurrence. For example, 6% (n = 21) of these participants had some combination of ‘joint pain and swelling,’ ‘rheumatoid arthritis’ and ‘other arthritis.’ Of participants who decreased driving, 39% did not report the health condition associated with driving reduction. Thus, the role of health conditions in driving reduction was not fully characterized with these data. Also, this study’s questions only addressed driving reduction because of health conditions. This study did not assess other forms of self-regulation (e.g., avoidance of certain driving conditions) or the reasons for reductions (e.g., recommendation from someone versus self-regulation); future studies will be able to do this utilizing other questions posed to the LongROAD cohort.
Despite its limitations, this study has many strengths. The large multi-state sample enabled identification of conditions of relatively low prevalence that nevertheless commonly resulted in reduced driving. Our study also examined a wide variety of health conditions affecting diverse organ systems. As the AAA LongROAD Study progresses, longitudinal data will build on baseline analysis to further explore issues around health conditions, driving, and driving self-regulation.
CONCLUSION
This study’s findings highlight that older adults may reduce driving for certain health conditions, especially those affecting the musculoskeletal, neurologic, and ophthalmologic systems. Future research should further consider the effects of such health conditions on older adult driving habits. Such research may help health professionals talk about driving reduction with older adults with certain diagnoses and ensure they receive referrals to appropriate services. These steps may help to ensure that older adults do not compromise their independence and mobility and that, given the time to prepare, they may cope better with driving reduction (Betz et al., 2016). As we collect data from this cohort over time, we hope to identify patterns in health condition diagnosis versus driving reduction that may help researchers and health professionals better address this issue in the future.
Acknowledgments
Funding Sources: This research was supported by the AAA Foundation for Traffic Safety (Washington, DC) through the Longitudinal Research on Aging Drivers (LongROAD) Project, by The National Institute on Aging, AFAR, The John A. Hartford Foundation, and The Atlantic Philanthropies under the Paul Beeson Career Development Award Program <number K23AG043123>, and by The Centers for Disease Control and Prevention under Grant 1 R49 <number CE002096>. The contents of the manuscript are solely the responsibility of the authors and do not necessarily reflect the official views of the funding agencies.
Footnotes
Disclosure of Interests: None of the authors has any conflicts of interest to disclose.
Sponsor’s Role: The AAA Foundation was involved in LongROAD study design and manuscript review. They were not involved in subject recruitment, data collection, analysis, or in the decision to publish findings.
REFERENCES
- Abbas G, & Waheed A (2011). Resumption of Car Driving after Total Hip Replacement. Journal of Orthopaedic Surgery, 19(1), 54–56. doi: 10.1177/230949901101900112 [DOI] [PubMed] [Google Scholar]
- Altman BM (2014). Definitions, concepts, and measures of disability. Annals of Epidemiology, 24(1), 2–7. doi: 10.1016/j.annepidem.2013.05.018 [DOI] [PubMed] [Google Scholar]
- American Geriatrics Society, & Pomidor, A. (2016). Clinician’s guide to assessing and counseling older drivers In: National Highway Traffic Safety Administration; Washington, DC. [Google Scholar]
- Bandeen-Roche K, Seplaki CL, Huang J, Buta B, Kalyani RR, Varadhan R, … Kasper JD (2015). Frailty in Older Adults: A Nationally Representative Profile in the United States. The Journals of Gerontology: Series A, 70(11), 1427–1434. doi: 10.1093/gerona/glv133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betz ME, & Lowenstein SR (2010). Driving patterns of older adults: results from the Second Injury Control and Risk Survey. Journal of the American Geriatrics Society, 58(10), 1931–1935. doi:JGS3010 [pii] 10.1111/j.1532-5415.2010.03010.x [DOI] [PubMed] [Google Scholar]
- Betz ME, Scott K, Jones J, & DiGuiseppi C (2016). “Are you still driving?” Meta-synthesis of older adults’ preferences for communication with healthcare providers about driving. Traffic Inj Prev, 17(4), 367–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Binns H, & Camm J (2002). Driving and arrhythmias : The crux of medical fitness to drive is the risk of incapacitating arrhythmias. BMJ : British Medical Journal, 324(7343), 927–928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brabyn JA, Schneck ME, Lott LA, & Haegerström-Portnoy G (2005). Night Driving Self-Restriction: Vision Function and Gender Differences. Optometry and Vision Science, 82(8), 755–764. [DOI] [PubMed] [Google Scholar]
- Braitman KA, & McCartt AT (2008). Characteristics of older drivers who self-limit their driving. Annual Proceedings of the Association for the Advancement of Automotive Medicine, 52, 245–254. [PMC free article] [PubMed] [Google Scholar]
- Callahan CM, Unverzagt FW, Hui SL, Perkins AJ, & Hendrie HC (2002). Six-item screener to identify cognitive impairment among potential subjects for clinical research. Medical Care, 40(9), 771–781. doi: 10.1097/01.MLR.0000024610.33213.C8 [DOI] [PubMed] [Google Scholar]
- Charlton JL, Oxley J, Fildes B, Oxley P, Newstead S, Koppel S, & O’Hare M (2006). Characteristics of older drivers who adopt self-regulatory driving behaviours. Transportation Research Part F-Traffic Psychology and Behaviour, 9(5), 363–373. doi:DOI 10.1016/j.trf.2006.06.006 [DOI] [Google Scholar]
- Chihuri Mielenz T., DiMaggio C, Betz M, DiGuiseppi C, Jones V, & Li G (2015). Driving cessation and health outcomes in older adults Retrieved from https://www.aaafoundation.org/driving-cessation-and-health-outcomes-older-adults-longroad-study [DOI] [PMC free article] [PubMed]
- Choi M, Adams KB, & Kahana E (2013). Self-regulatory driving behaviors: gender and transportation support effects. Journal of Women and Aging, 25(2), 104–118. doi: 10.1080/08952841.2012.720212 [DOI] [PubMed] [Google Scholar]
- Choi M, Mezuk B, & Rebok GW (2012). Voluntary and Involuntary Driving Cessation in Later Life. Journal of Gerontological Social Work, 55(4), 367–376. doi: 10.1080/01634372.2011.642473 [DOI] [PubMed] [Google Scholar]
- Cicchino JB (2015). Why have fatality rates among older drivers declined? The relative contributions of changes in survivability and crash involvement. Accident Analysis and Prevention, 83, 67–73. doi: 10.1016/j.aap.2015.06.012 [DOI] [PubMed] [Google Scholar]
- Classen S (2014). Summary of an evidence based review on interventions for medically at risk older drivers. Occup Ther Health Care, 28(2), 223–228. doi: 10.3109/07380577.2014.896490 [DOI] [PubMed] [Google Scholar]
- Cox DJ, Kovatchev B, Vandecar K, Gonder-Frederick L, Ritterband L, & Clarke W (2006). Hypoglycemia Preceding Fatal Car Collisions. Diabetes Care, 29(2), 467–468. doi: 10.2337/diacare.29.02.06.dc05-1836 [DOI] [PubMed] [Google Scholar]
- Crizzle AM, Classen S, Lanford DN, Malaty IA, Okun MS, Wang Y, … McFarland NR (2013). Postural/Gait and cognitive function as predictors of driving performance in Parkinson’s disease. Journal of Parkinson’s Disease, 3(2), 153–160. doi: 10.3233/JPD-120152 [DOI] [PubMed] [Google Scholar]
- D’Ambrosio LA, Donorfio LK, Coughlin JF, Mohyde M, & Meyer J (2008). Gender differences in self-regulation patterns and attitudes toward driving among older adults. Journal of Women and Aging, 20(3–4), 265–282. [DOI] [PubMed] [Google Scholar]
- Dickerson AE, Reistetter T, Davis ES, & Monahan M (2011). Evaluating Driving as a Valued Instrumental Activity of Daily Living. American Journal of Occupational Therapy, 65(1), 64–75. doi:DOI 10.5014/ajot.2011.09052 [DOI] [PubMed] [Google Scholar]
- Dickerson AE, Reistetter T, & Gaudy JR (2013). The perception of meaningfulness and performance of instrumental activities of daily living from the perspectives of the medically at-risk older adults and their caregivers. Journal of Applied Gerontology, 32(6), 749–764. doi: 10.1177/0733464811432455 [DOI] [PubMed] [Google Scholar]
- Fisk GD, Owsley C, & Pulley LV (1997). Driving after stroke: Driving exposure, advice, and evaluations. Archives of Physical Medicine and Rehabilitation, 78(12), 1338–1345. doi: 10.1016/S0003-9993(97)90307-5 [DOI] [PubMed] [Google Scholar]
- Harrison A, & Ragland DR (2007). Consequences of driving reduction or cessation for older adults. Transportation Research Record: Journal of the Transportation Research Board, 1843/2003, 96–104.
- Hassan H, King M, & Watt K (2015). The perspectives of older drivers on the impact of feedback on their driving behaviours: A qualitative study. Transportation Research Part F: Traffic Psychology and Behaviour, 28, 25–39. doi: 10.1016/j.trf.2014.11.003 [DOI] [Google Scholar]
- Hetland A, & Carr DB (2014). Medications and Impaired Driving: A Review of the Literature. The Annals of pharmacotherapy, 48(4), 494–506. doi: 10.1177/1060028014520882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill LL, Lauzon VL, Winbrock EL, Li G, Chihuri S, & Lee KC (2017). Depression, antidepressants and driving safety. Inj Epidemiol, 4(1), 10. doi: 10.1186/s40621-017-0107-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krauss GL, Ampaw L, & Krumholz A (2001). Individual state driving restrictions for people with epilepsy in the US. Neurology, 57(10), 1780–1785. [DOI] [PubMed] [Google Scholar]
- Krumholz A (2009). Driving Issues in Epilepsy: Past, Present, and Future. Epilepsy Currents, 9(2), 31–35. doi: 10.1111/j.1535-7511.2008.01283.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lane A, Green E, Dickerson AE, Davis ES, Rolland B, & Stohler JT (2014). Driver rehabilitation programs: defining program models, services, and expertise. Occup Ther Health Care, 28(2), 177–187. doi: 10.3109/07380577.2014.903582 [DOI] [PubMed] [Google Scholar]
- Li G, Eby DW, Santos R, Mielenz TJ, Molnar LJ, Strogatz D, … Andrews HF (2017). Longitudinal Research on Aging Drivers (LongROAD): Study design and methods. Injury Epidemiology, 4(1), 22. doi: 10.1186/s40621-017-0121-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyman JM, McGwin G Jr., & Sims RV (2001). Factors related to driving difficulty and habits in older drivers. Accident Analysis and Prevention, 33(3), 413–421. [DOI] [PubMed] [Google Scholar]
- Marie Dit Asse L, Fabrigoule C, Helmer C, Laumon B, & Lafont S (2014). Automobile Driving in Older Adults: Factors Affecting Driving Restriction in Men and Women. Journal of the American Geriatrics Society, 62(11), 2071–2078. doi: 10.1111/jgs.13077 [DOI] [PubMed] [Google Scholar]
- Marshall SC (2008). The role of reduced fitness to drive due to medical impairments in explaining crashes involving older drivers. Traffic Inj Prev, 9(4), 291–298. [DOI] [PubMed] [Google Scholar]
- Meng A, & Siren A (2012). Older Drivers’ Reasons for Reducing the Overall Amount of Their Driving and for Avoiding Selected Driving Situations. Journal of Applied Gerontology, 34(3), NP62–NP82. doi: 10.1177/0733464812463433 [DOI] [PubMed] [Google Scholar]
- Meuser TM, Berg-Weger M, Chibnall JT, Harmon AC, & Stowe JD (2013). Assessment of Readiness for Mobility Transition (ARMT) A Tool for Mobility Transition Counseling With Older Adults. Journal of Applied Gerontology, 32(4), 484–507. [DOI] [PubMed] [Google Scholar]
- Molnar LJ, Charlton JL, Eby DW, Langford J, Koppel S, Kolenic GE, & Marshall S (2014). Factors affecting self-regulatory driving practices among older adults. Traffic Inj Prev, 15(3), 262–272. doi: 10.1080/15389588.2013.808742 [DOI] [PubMed] [Google Scholar]
- National Research Council. (2005). Does the Built Environment Influence Physical Activity?: Examining the Evidence--Special Report 282: Transportation Research Board
- O’Connor ML, Edwards JD, Small BJ, & Andel R (2012). Patterns of level and change in self-reported driving behaviors among older adults: Who self-regulates? The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 67(4), 437–446. doi: 10.1093/geronb/gbr122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pachana NA, & Petriwskyj AM (2006). Assessment of insight and self-awareness in older drivers. Clinical Gerontologist, 30(1), 23–38. [Google Scholar]
- Pierson JL, Earles DR, & Wood K (2003). Brake response time after total knee arthroplasty: when is it safe for patients to drive? The Journal of arthroplasty, 18(7), 840–843. [DOI] [PubMed] [Google Scholar]
- Ragland DR, Satariano WA, & MacLeod KE (2004). Reasons given by older people for limitation or avoidance of driving. Gerontologist, 44(2), 237–244. [DOI] [PubMed] [Google Scholar]
- Ragland DR, Satariano WA, & MacLeod KE (2005). Driving cessation and increased depressive symptoms. Journals of Gerontology. Series A: Biological Sciences and Medical Sciences, 60(3), 399–403. doi:60/3/399 [pii] [DOI] [PubMed] [Google Scholar]
- Roley SS, DeLany JV, Barrows CJ, Brownrigg S, Honaker D, Sava DI, … Youngstrom MJ (2008). Occupational therapy practice framework: domain & practice, 2nd edition. American Journal of Occupational Therapy, 62(6), 625–683. [DOI] [PubMed] [Google Scholar]
- Satariano WA, Guralnik JM, Jackson RJ, Marottoli RA, Phelan EA, & Prohaska TR (2012). Mobility and aging: new directions for public health action. American Journal of Public Health, 102(8), 1508–1515. doi: 10.2105/ajph.2011.300631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaheen S, Allen D, & Liu J (2008). Public transit training: A mechanism to increase ridership among older adults
- Siren A, Hakamies-Blomqvist L, & Lindeman M (2004). Driving Cessation and Health in Older Women. Journal of Applied Gerontology, 23(1), 58–69. doi: 10.1177/0733464804263129 [DOI] [Google Scholar]
- Stressel D, Hegberg A, & Dickerson AE (2014). Driving for adults with acquired physical disabilities. Occup Ther Health Care, 28(2), 148–153. doi: 10.3109/07380577.2014.899415 [DOI] [PubMed] [Google Scholar]
- Touchinsky S, Chew F, & Davis ES (2014). Gaps and pathways project: driving pathways by diagnosis sheets. Occup Ther Health Care, 28(2), 203–206. doi: 10.3109/07380577.2014.903450 [DOI] [PubMed] [Google Scholar]
- Tregear S, Reston J, Schoelles K, & Phillips B (2009). Obstructive Sleep Apnea and Risk of Motor Vehicle Crash: Systematic Review and Meta-Analysis. Journal of Clinical Sleep Medicine : JCSM : Official Publication of the American Academy of Sleep Medicine, 5(6), 573–581. [PMC free article] [PubMed] [Google Scholar]
- Tysnes O-B, & Storstein A (2017). Epidemiology of Parkinson’s disease. Journal of Neural Transmission, 124(8), 901–905. doi: 10.1007/s00702-017-1686-y [DOI] [PubMed] [Google Scholar]
- Xu KT, & Borders TF (2003). Gender, Health, and Physician Visits Among Adults in the United States. American Journal of Public Health, 93(7), 1076–1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuen H, Gillespie M, Day T, Morgan L, & Burik J (2007). Driving behaviors in patients with head and neck cancer during and after cancer treatment: A preliminary report. Head and Neck, 29(7), 675–681. doi: 10.1002/hed.20567 [DOI] [PubMed] [Google Scholar]