Abstract
Background
Blended group therapy (bGT) has been investigated a several times for anxiety and depression, but information on patients’ adherence to and therapists’ perception of the novel format is nonexistent. Furthermore, many studies investigated mainly female and highly educated populations, limiting the validity of previous findings.
Objective
This study aimed to reduce the gaps and limitations of the previous findings by evaluating an integrated internet- and mobile-supported bGT format.
Methods
A total of 27 patients diagnosed with major depression (14/27, 52% female and 7/27, 25.9% compulsory education) participated in a 7-week treatment at a university outpatient clinic. Furthermore, 8 novice therapists participated in semistructured interviews and a subsequent cross-validation survey.
Results
Primary symptom reduction was high (d=1.31 to 1.51) and remained stable for the follow-up period. Therapists identified advantages (eg, patient engagement, treatment intensification, and improved therapeutic relation) and disadvantages (eg, increased workload, data issues, and undesired effects) of bGT. The required online guidance time was 10.3 min per patient and week, including guidance on exercises (67% or 6.9 min) and intimate communication (33% or 3.4 min). Concerning patients’ adherence to bGT, tracked completion of all Web-based and mobile tasks was high and comparable with group attendance.
Conclusions
Results suggest high feasibility of bGT in a gender-balanced, moderately educated sample. bGT provides group therapists with tools for individual care, resulting in an optimization of the therapy process, and high completion rates of the implemented bGT elements. The limited work experience of the involved therapists restricts the study findings, and potential drawbacks need to be regarded in the development of future bGT interventions.
Keywords: eHealth, mobile phone, computer-assisted therapy, monitoring, group therapy, depression, professional-patient relations
Introduction
Background
Depression is one of the most prevalent mental disorders and a leading cause of disability. It imposes suffering and high costs on individuals, societies, and health systems [1]. In line with international research priorities [2,3], different forms of mobile- and internet-based interventions constitute innovative and efficient strategies to deliver evidence-based psychological treatments for common mental health disorders [4-8].
Among their most frequent formats, mobile and Web-based interventions offer flexible and anonymous access to mental health services, resulting in low social barriers and low risk of stigmatization [9,10]. Owing to the high degree of automatization, those interventions guarantee standardized treatments to a highly scalable extent. These properties make them attractive for mental health care organizations and have led to the launch of the first routine online clinics [11-13].
However, Web-based and mobile interventions also exhibit limitations as they do not meet all patients’ needs and preferences, and therapist contact usually is restricted to a wide degree. Furthermore, therapeutic guidance frequently is associated with better treatment outcomes and reduced dropout rates [14,15]. Finally, many therapists lack experience with this novel approach and hold more cautious attitudes toward Web-based interventions [16]. Comparable levels of caution and awareness have been found among different interest parties (eg, mental health care providers and policy makers), contributing to a frequently discussed retardation of dissemination efforts [17]. Therefore, it is crucial to gain further insight into therapists’ perception and acceptance of technology-aided treatments.
The techniques developed in the field of Web-based therapy [7,18-21] can also be harnessed to improve existing forms of face-to-face therapy, resulting in a continuum of blended treatments (Figure 1). Within blended interventions (synonymous computer- or mobile-supported interventions), the spectrum of possible applications ranges from adjuncts to psychotherapy [22], which can be applied before, after, or during treatment [23,24], to more integrated forms of therapy in which Web-based or mobile elements and personal sessions are more deeply intertwined into one treatment rationale [25-27]. A growing number of studies show that blended interventions can lead to shortened treatments in which less therapist time is needed to achieve substantial effects [23,26,28]. Simultaneously, Web-based or mobile elements can be deployed to optimize the therapeutic process, to foster transfer, and to boost effects of classical treatments. In this regard, first studies in routine care found additive effects of traditional face-to-face therapy augmented with Web-based therapy elements [29,30].
Figure 1.
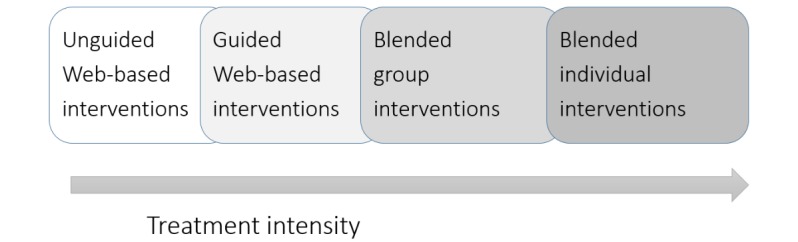
Blends of Web-based and face-to-face therapy.
According to therapists, patients can profit from blended interventions in the form of increased treatment accessibility and flexibility, as well as from the improvement of patients’ self-management and the optimal use of face-to-face sessions [31,32]. Additionally, mental health care providers, policy makers, and other such organizations seem to have a more positive conception of blended therapy compared with pure Web-based therapy [17], and therapists seem to prefer the blended format because it is associated with less risks (eg, diagnostic process) [16]. Among the potential disadvantages of the integrated format, therapists frequently remark that blended therapy is not feasible for all patients and that the format at times could hamper the therapeutic process—in particular, the establishment of the therapeutic alliance [31,32]. Consequently, those issues should be investigated in more detail in patient- and therapist-related studies.
While most blended research focuses on individual therapy [23], less is known about its potential for group therapy. Psychological groups have a broad range of applications in inpatient and outpatient settings [33]; and the spectrum ranges from informational groups, over psychoeducational groups, to group counseling and group psychotherapy [34]. So far, the feasibility and effects of blended group therapy (bGT; synonymous computer- or app-supported group therapy) have been investigated in terms of brief interventions for depression and anxiety. For example, computer-based relaxation, cognitive restructuring, and self-control desensitization have been found to be supportive in the treatment of generalized anxiety disorder (GAD) [35]. Furthermore, first evidence for the efficiency of brief bGT for social anxiety disorder and GAD was found in small comparative trials, leading to significant symptom reductions in a comparably short time period [36,37]. As for depression, several feasibility studies investigated the merits of supportive computer- and mobile-based elements. For example, a tablet-guided behavioral activation (BA) intervention was found to be feasible for the treatment of major depressive disorder [38]. In another study, Aguilera et al found beneficial effects of group therapy augmented with monitoring and text messaging [39]. Furthermore, a brief resource-oriented bGT intervention was developed by our workgroup to address depression by means of a low-threshold, stigma-free treatment strategy. The results revealed high feasibility in terms of client satisfaction and observed between-group treatment effects. Moreover, assessed parameters of treatment adherence (eg, self-reported exercising) indicated high acceptability of bGT elements [40-41]. In a subsequent qualitative investigation (including 13 patients of this study), the use of technology was described as a therapeutic factor, facilitating insight, exercising, and treatment transfer [42].
Objectives
This study wants to carry this work forward by investigating an integrated bGT intervention based on Acceptance and Commitment Therapy (ACT) principles [43], complemented with elements of BA [44]. As in previous studies, patients’ self-reported depressiveness and general health, as well as ACT-specific variables and standardized measures for service satisfaction and usability, were assessed. For the first time, log data were tracked to provide reliable information on completion rates of computer- and mobile-based elements. Focusing on the therapist-related feasibility of bGT, this study includes therapist interviews and a subsequent follow-up survey. As a related aspect, the amount of weekly online guidance was recorded to ascertain therapists’ between-session workload.
Methods
Participants
The trial was preregistered at the German trial register (DRKS Number: DRKS00010888), and the regional ethics committee of the University of Salzburg approved the study procedure. Participants were recruited via a multimodal recruitment strategy by handing out flyers in public health centers and densely populated public areas and by advertisements on depression-related Web pages. After registering on the study platform participants obtained detailed information about the procedure and goals of the study and were asked to give informed consent.
The selection of participants followed 2 steps. Participants were asked to fill out a short screening questionnaire. This included the short version of the Center of Epidemiologic Studies Depression (CES-D) scale [45,46] and additional questions regarding current and past psychological or medical treatment. Participants reporting at least mild levels of depression (CES-D>17) and no suicidal ideation, critical drinking, or past or recent history of severe psychiatric conditions were invited to take part in a diagnostic interview.
Personal clinical interviews were conducted by 3 independent and experienced psychologists, applying the German Mini-Diagnostic Interview for Psychological Disorders (DIPS) [47]. The Mini-DIPS is a 30- to 45-min version of the German DIPS [48], based on the International Classification of Diseases-10 depression criteria. Participants were deemed eligible if the following criteria applied: aged between 18 and 65 years, suffering from mild-to-moderate levels of major depression and/or dysthymia; and/or mild-to-moderate comorbid anxiety, as well as familiarity with the use of personal computers and possession of a smartphone. According to clinical judgement, participants were excluded if they suffered from severe depression (>7 criteria, including main symptoms), severe anxiety disorder, bipolar disorder, any schizoaffective disorder, severe psychiatric and psychotic conditions, substance abuse, suicidal ideation, or if they exhibited low German language and/or computer skills. Participants were also excluded if they currently underwent psychotherapy. Psychiatric medication was tolerated but has been kept constant for at least 3 months before study onset. Figure 2 presents the flowchart demonstrating the recruitment and research procedure in detail.
Figure 2.
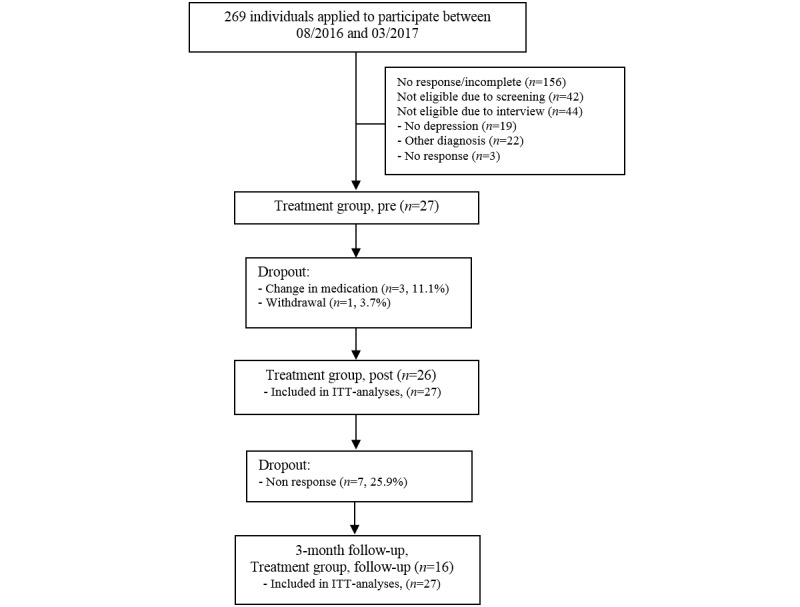
Study flow chart. ITT: intention to treat.
Procedure
After preassessment, participants were provided with access to the internet platform (Minddistrict) and scheduled to one of 2 weekly groups, depending on personal preferences. To provide personal support in case of technical problems, the app-based diary was installed at the end of the first group session. Group meetings lasted 7 weeks, and each session was preceded by a preparatory Web-based module. The therapist gave supportive feedback after completion of a given Web-based session and occasionally gave reminders to participants by sending out prompts via the platform. The app-based diary complemented the blended treatment with a focus on the transfer of previously learned techniques into daily life. Participants were free to logon to the platform after treatment had ended but did no longer receive therapist guidance. As recommended by several guidelines [33], group sessions were held in a double trainer format which lasted 90 min each. One week after the last group session, the Web-based post assessment had to be filled out and follow-up assessment took place 3 months later.
Intervention
The 7 weeks intense group treatment was based on the ACT and BA principles. ACT [43] is one of the several new treatments originating from cognitive behavioral therapy (CBT). The core principles of this contemporary approach can be divided into mindfulness and acceptance techniques (acceptance, cognitive defusion, and self as context) and behavior change techniques (contact with the present moment, values, and committed action). Even though ACT and BA diverge regarding certain theoretical assumptions (ie, proposed mechanisms of action) [49], they also share many communalities (eg, clarification of goals or strong emphasis on behavioral techniques). Therefore, ACT-based behavior change techniques can be complemented by BA principles [50]. The current treatment rationale was recreated based on a previous intervention, merging ACT and BA into one integrated rationale [51]. Detailed information on intervention content and design can be obtained from Table 1 and Figure 3.
Table 1.
Group sessions and computer and multimedia elements of the intervention.
| Week | Web-based module | Group session | App | Workbook |
| 1 | Introduction into mindfulness | Introduction into ACTa, mindfulness | Feature 1: Mindfulness in daily life | List of mindful activities |
| 2 | Natural suffering and suffering through avoidance | Avoidance and acceptance | Feature 2: Acceptance | Acceptance of a difficult situation, topic, character trait, or conflict; Reflection on mindfulness |
| 3 | Defusion | Fusion and defusion | Feature 3: Defusion | Typical examples of defusion |
| 4 | Values, goals, and self-management | Values, mastery, and self-management | Feature 4: Mastery activities | Bull’s-eye exercise; Example and sheet for SMARTb principle; Activity planning |
| 5 | Commitment | Commitment and positive reinforcement | Feature 5a: “Do activities” Feature 5b: “Do not activities” | Determination, ranking, and planning of do- and do not activities; Self-management; Activity planning |
| 6 | Expansion of behavioral activation | Expansion of behavioral activation | Continuation of previous features of the app | Contracts |
| 7 | Review and transfer | Transfer and conclusion | Continuation of previous features of the app | Plan for relapse |
aACT: Acceptance and Commitment Therapy.
bSMART: frequent self-management principle.
Figure 3.
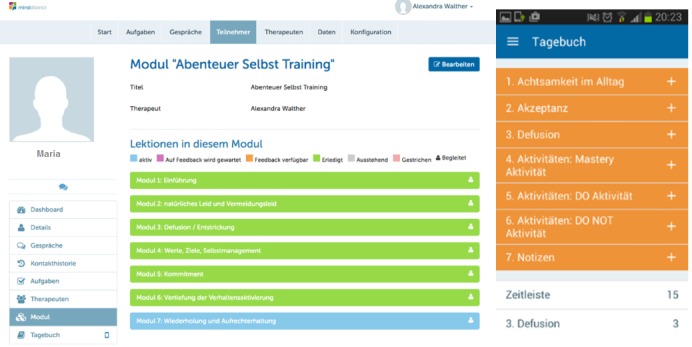
User interfaces of the web-based platform and the smartphone app.
With regard to the use of computer- and mobile-based elements, the patients’ weekly routine consisted of 3 steps. First, a preparatory Web-based module, featuring video clips, text-based tasks, and an asynchronous therapist chat, had to be completed. Afterward, patients received individualized feedback from the assigned therapist (if applicable within 2 days). Second, patients participated in the weekly reunions, which again were partially complemented by modern media (ie, short clips or PowerPoint presentations). As a last step, patients were guided by weekly mobile phone diary tasks, which were scheduled for 7 days following the weekly group session. All reminders and prompts were modifiable according to personal preferences, and wherever possible, therapists were instructed to balance media and personal treatment elements according to patient needs and their professional judgement. If patients did not adhere to the Web-based tasks, therapists were instructed to send out a prompt in the middle of the treatment week and, again, once on the day before the forthcoming group session. If patients complained about the number of reminders, the prompts were reduced or stopped.
Therapists
A total of 8 novice therapists (2 male and 6 female) conducted the groups in a double trainer setting. Of the 8 therapists, 2 finished their master’s degree (MSc) or Doctor of Science in psychology and underwent tertiary training in psychotherapy (CBT), clinical psychology (CBT), or medicine at the time of the intervention. The remaining 5 therapists were in their final year of clinical psychology (MSc) and had clinical experience with conducting classical forms of individual or group therapy, as well as with drafting psychological expert reports. None of the therapists had previous experience with conducting bGT or any other form of Web-based therapy. All participating therapists underwent previous training (minimum 40 hours), including a 6-digital versatile disc ACT-series (ACT in Action) and 2 textbooks [52,53] encompassing sections on difficult situations in the ACT. Therapists also protocolled their weekly group sessions. Adherence to the foreseen treatment course was supported by in- and between-session media and technology elements. Of the 8 therapists, 2 therapists participated in a previous bGT study [41] and 6 participated in this study. At the time of the therapist interviews (3 to 12 months after study end), all except 1 therapist were in tertiary clinical trainings for psychotherapy (3 therapists; CBT and client-centered therapy), clinical psychology (3 therapists; CBT), or medicine (1 therapist).
Outcome Measures
Primary Outcomes
The principal outcome of the study was reduction of depressed mood. It was measured by the short version of the German translation of the CES-D scale [45,46]. This questionnaire measures interactive, cognitive, and somatic symptoms, as well as emotions and motor functions related to depression. The 16 items are rated on a 4-point Likert scale. Any value above 17 is interpreted as critical. The German version’s critical threshold (>17) has high discriminative validity, pointed out by a sensitivity of 90%, a specificity of 87% [45], and an area-under-the-curve value of 0.94 [54]. The reliability of the CES-D has been shown to be high [46]. The Cronbach alpha in this study was .90.
As a more general self-report questionnaire that measures psychological distress, nonspecific current mental health, and the risk of developing psychological disorders, the General Health Questionnaire-12 (GHQ-12 [55]) was used. The questionnaire has shown solid reliability [56] and good intercultural validity [57]. The Cronbach alpha in this study was .84.
Secondary Outcomes
Psychological flexibility (ie, acceptance of unpleasant feelings, worry, and control agendas) is the central psychological construct of the ACT and was measured by the Fragebogen zu Akzeptanz und Handeln II [58]. This is the German version of the Acceptance and Action Questionnaire-II (AAQ-II) by Bond et al [59]. The 7 items are rated on a 7-point Likert scale. The Cronbach alpha of the this study was .89.
Anxiety was measured with the Anxious Thoughts Inventory (AnTi) [60] (German translation [61]). It analyzes 3 dimensions of worry: social worry, physical health worry, and meta-worry (worry about worries). The 22 items are rated on a 4-point Likert scale. The Cronbach alpha in this study was .87.
Finally, worry was measured with the PSWQ-3 [62], a short form of the Penn State Worry Questionnaire [63]. It is a questionnaire that assesses self-reported key aspects of worry in GAD. The 3 items are rated on a 5-point Likert scale. The Cronbach alpha in this study was .74.
Client Satisfaction and System Usability
System usability of applied app and Web elements was measured by the System Usability Scale (SUS) [64]. The SUS is a robust questionnaire with 10 items rated on a 5-point Likert scale. The sum score ranges from 1 to 100. SUS scores >85.5 classify excellent usability; scores ≤85.5 and >71.4 classify as good, scores ≤71.4 and >50.9 as OK, scores ≤50.9 and >35.7 as poor, and scores ≤35.7 and >20.3 as awful [65]. The Cronbach alpha in this study was .78.
The ZUF-8 (Fragebogen zur Patientenzufriedenheit) [66], the German version of the Client Satisfaction Questionnaire-8 [67], was used to assess several aspects of participants’ overall treatment satisfaction. The 8 items are rated on a 4-point Likert scale. The total score can range from 8 to 32, with a cut-off value of 24 [68] to grade a person as dissatisfied. The Cronbach alpha in this study was .94. For the mobile-based app, adherence was defined as more than 3 weekly entries.
Statistical Analyses
SPSS 24 (SPSS Inc) was used to carry out the analyses. Significant differences between pre, post, and follow-up were analyzed by linear mixed models, with compound symmetry as covariance type and restricted maximum likelihood estimation. Missing outcome values were analyzed according to the intention-to-treat (ITT) principle. Individual pre to post changes served as a base for the reliable change indexes (RCIs) [69]. We used internal consistency as a parameter for RCI reliability [70]. The reliable change criteria were 5.87 scale points for the CES-D and 4.87 for the GHQ-12. For the assessment of change, within-group effect sizes were calculated with pooled SD and reported in Cohen d [71]. Power analysis was executed with G*Power [72]. We assumed that the effect size for the secondary outcomes may only lie in the medium range. Thus, an estimated sample size of N=22 was calculated for a medium within-subjects effect size of d=0.65 (alpha error=.05; power beta=.90).
Qualitative Analyses
On the basis of a structured interview guide (Multimedia Appendix 1), audiotaped therapist interviews were conducted by the first author (RS). Interviews lasted between 28 and 56 min (mean 44) and were transcribed by 2 independent psychologists who also analyzed the material obtained. MAXQDA was used to conduct the analysis. Analysts were blind to the outcomes and identity of participants. The qualitative content analysis [73] served as the method of information extraction by applying a deductive extraction based on the addressed research questions. After analyzing one third of the transcript, both psychologists and the first author (RS) jointly revised the code system to reach agreement on the applied coding system. Principal codes closely related to the structured interview guide were then specified into further emerging subthemes. After content analysis, a set of follow-up questions was surveyed anonymously to depict the degree of consensus on particular findings among the interviewed therapists. Of the 30 items, 10 items related to design aspects will be reported in a further publication on bGT design. The complete list of follow-up questions was translated by a bilingual psychologist and is presented in (Multimedia Appendix 2).
Results
Participants
A comprehensive overview of participant characteristics at baseline is provided in Table 2. Men and women were equally represented (52%, 14/27 female,), with a mean age of 37.7 years (SD 13.7), and relatively low levels of education and employment status. Furthermore, 1 patient withdrew from treatment, resulting in a completion rate of 96% (26/27). During the study period, 3 patients reported changes in medication. According to ITT principles, those patients remained in the analyses. Detailed information on participants’ enrolment and participation throughout the study can be seen in Figure 2.
Table 2.
Demographic, behavioral, and clinical characteristics of the sample at pretreatment (N=27).
| Characteristic | Statistics | |
| Age (years), mean (SD) | 37.70 (13.66) | |
| Gender, female n (%) | 14 (51.9) | |
| Education, n (%) | ||
|
|
≥9 years (compulsory school) | 7 (25.9) |
|
|
≥12 years (A level) | 12 (44.4) |
|
|
≥any tertiary education (eg, university) | 8 (29.6) |
| Employment, n (%) | ||
|
|
Full time | 11 (40.7) |
|
|
Part time | 6 (22.2) |
|
|
None/marginally | 5 (18.5) |
|
|
Currently in education | 5 (18.5) |
| Current psychopharmacological treatment, n (%) | 3 (12) | |
| Previous psychotherapeutic treatment, n (%) | 14 (54) | |
| Computer experience, n (%) | ||
|
|
Daily use | 25 (92.6) |
|
|
Weekly use | 2 (7.4) |
| Diagnosis, n (%) | ||
|
|
F32.0 (mild depressive episode), n (%) | 3 (11.1) |
|
|
F32.1 (moderate depressive episode), n (%) | 8 (29.6) |
|
|
F33.0 (recurrent depressive episode, current episode mild), n (%) | 10 (37.0) |
|
|
F33.1 (recurrent depressive episode, current episode moderate), n (%) | 4 (14.8) |
|
|
F33.4 (recurrent depressive disorder, in remission—elevated levels of depression), n (%) | 2 (7.4) |
| Comorbidities, n (%) | ||
|
|
F10.1/2 (harmful use of alcohol/addiction) | 1 (3.7) |
|
|
F40.0 (agoraphobia without panic disorder) | 1 (3.7) |
|
|
F40.1 (social phobia) | 2 (7.4) |
|
|
F40.2 (specific phobia) | 1 (3.7) |
|
|
F41.1 (generalized anxiety disorder) | 3 (11.1) |
|
|
F43.2 (adjustment disorder) | 1 (3.7) |
|
|
F50.2 (bulimia nervosa) | 1 (3.7) |
Primary and Secondary Outcomes
Linear mixed models unveiled significant changes in all outcome measures, and pre- to posteffect sizes for primary outcomes were large to very large (d=1.31 to 1.51). The primary outcome CES-D showed a statistically significant decrease in self-reported depressiveness, with an F value of F2,43.323=18.94, P<.001. For the CES-D, 74% (20/27) of participants exhibited RCIs from pre to post assessment (deteriorations=3.7% [1/27]). Self-reported psychological distress, measured by the GHQ-12, decreased significantly, F2,41.616=12.04, P<.001, and RCI was found in 63% (17/27) of participants (deterioration=0% [0/27]). Estimated means, SDs, effect sizes, and RCIs of both scales are depicted in Table 3.
Table 3.
Means, SDs, effect sizes (Cohen d), and reliable change for primary and secondary outcomes (N=27).
| Questionnaire | Estimated mean (SD) | Effect sizes (estimated mean [95% CI]), pre to post effect size | Reliable change | |||
| Pre | Post | Follow-up | Pre to post RCIa | Pre to follow-up RCI | ||
| CES-Db | 22.44 (5.18) | 13.56 (6.48) | 12.19 (7.94) | 1.51 (0.89 to 2.09) | 74 | 78 |
| GHQ-12c | 16.07 (5.41) | 9.63 (4.39) | 11.94 (7.12) | 1.31 (0.70 to 1.87) | 63 | 52 |
| AAQ-IId | 26.15 (8.87) | 20.71 (8.85) | 18.63 (9.71) | 0.59 (0.02 to 1.14) | —e | — |
| AnTif | 44.33 (10.22) | 36.46 (10.45) | 36.25 (11.59) | 0.72 (0.14 to 1.27) | — | — |
| PSWQ-3g | 7.63 (2.50) | 6.67 (2.76) | 6.50 (2.97) | 0.37 (−0.19 to 0.91) | — | — |
aRCI: reliable change index.
bCES-D: Center for Epidemiological Studies-Depression scale.
cGHQ-12: general health questionnaire (12-item version).
dAAQ-II: Acceptance and Actions Questionnaire.
eNot applicable.
fAnTi: Anxious Thoughts Inventory.
gPSWQ-3: Penn State Worry Questionnaire (ultra-short version).
For applied secondary outcomes, the treatment resulted in less pronounced effects (d=0.38 to d=0.71). The AAQ-II revealed a significant change over time, F2,39.710=10.41, P<.001, and an effect size of d=0.59. A comparable pattern was found with regard to the AnTi, F2,39.450=12.68, P<.001, and d=0.72, and with regard to the PSWQ-3, F2,39.447=4.11, P<.001, and d=0.37. For further information on estimated means, SDs, and effect sizes, see Table 3.
Maintenance of Treatment Effects
After a follow-up period of 3 months, the reduction of self-reported depression (CES-D) remained stable (F1,23.556=29.98; P<.001) and 78% (21/27) of participants exhibited RCI (deteriorations=7.4% [2/27]). With regard to self-reported psychological distress (GHQ-12), participants indicated significant effects from pre to follow-up, F1,22.758=4.82, P=.04, and RCI was found in 52% of participants (14/27) (deteriorations=11.1% [3/27]). Contrary to self-reported depressiveness, treatment effects on psychological distress regressed slightly during the follow-up period. However, these reductions failed to rise above the level of statistical significance (contrast: t26=1.39; P=.17). Stable treatment effects were also found for the 3 secondary outcomes: psychological flexibility (AAQ-II) F1,18.867=12.59, P=.002; anxious thoughts (AnTi) F1,17.771=12.04, P=.003; and worry (PSWQ-3) F1,18.825=4.60, P=.04. Further information can be obtained from Table 3.
Client Satisfaction and System Usability
System usability of applied app and Web elements, measured by the SUS [64], unveiled an average system usability of 65.33 (SD 18.95) of 100 possible scale points. Accordingly, system usability can be classified as OK to good [65]. Participant’s service satisfaction, measured by the ZUF-8 [66], assessed an average satisfaction of mean 26.43 (SD 4.80) on a 32-point scale, indicating “good” client satisfaction. However, according to the weekly documentation of group sessions, group coherence in 1 group was low, and the group climate would have profited from including personality disorders (Cluster A and B) in the diagnostic procedure.
Intervention Usage and Therapeutic Guidance
Besides group attendance=82.4% (5.9/7 sessions), usage of digital elements was high (Figure 4): completion rate of Web-based modules 76% (5.3/7 modules), and 67% (14/21 entries) for the mobile-based diary app. However, the average number of app entries during treatment (mean 33) exhibited great variety (range 0 to 246). The average time therapists spent in the guiding of weekly Web-based modules was mean 10.3 min per patient, including guidance on accomplished exercises (67% or 6.9 min) and lateral patient-therapist communication (33% or 3.4 min). Thus, two-third of the total guidance was dedicated to the supervision of Web-based tasks, whereas intimate patient-to-therapist communication constituted the remaining third. There was a trend toward a reduction of guidance as the study progressed, and the single groups differed in the required guidance time.
Figure 4.
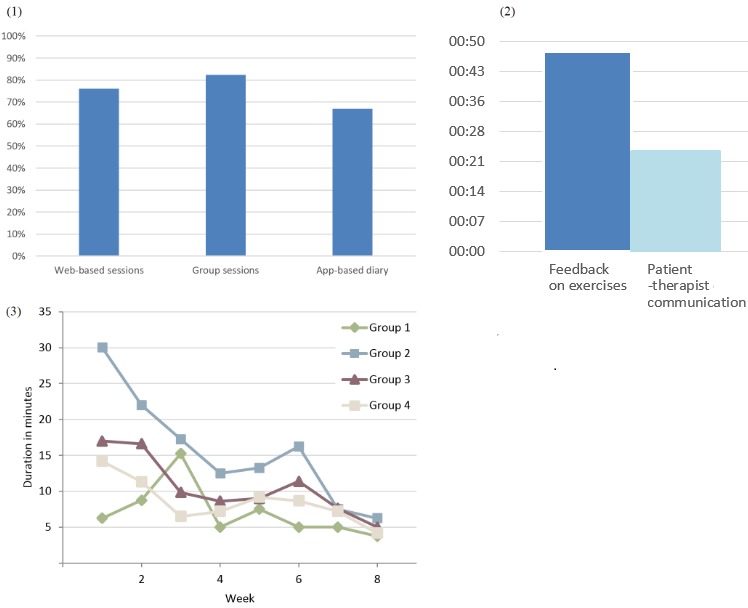
(1) Patients’ completion rates of all intervention elements. (2) Therapists’ average guidance time per patient during entire treatment; a total of 24 min was spent on personal topics, whereas 48 min was spent on feedback on specific exercises. (3) Therapists’ weekly Web-based guidance by single group.
Therapist Interviews and Subsequent Follow-Up Survey
The therapists’ experiences with and attitudes toward bGT can be described as cautiously positive to positive. Important themes concerned the functionality and applicability of bGT and patients’ interaction with the format, as well as the general appraisal of bGT. Table 4 depicts main themes, subthemes, and frequently assigned codes of the interviews. With Cohen kappa=0.49, interrater agreement was sufficiently high. Interview results were subsequently validated by an anonymous follow-up survey, which was based on the content of the interviews (Table 5).
Table 4.
Main themes, subthemes, and frequent codes of therapist interviews.
| Main theme and subtheme | Frequent codes | |
| Advantages | ||
|
|
Patients | Content repeatable; greater learning effect; increased engagement with therapy tasks |
|
|
Therapists | Additional information through monitoring; helpful for younger therapists; guiding thread |
|
|
Interaction | Patients more open (online disinhibition); building relationship through intimate Web-based communication |
| Disadvantages | ||
|
|
General | Additional effort; data security; limited management of acute crisis; predefined treatment course |
|
|
Specific | Effects on group climate and cohesion; sessions overloaded |
| General evaluation | ||
|
|
Positive | Contemporary; suitable for in-patient settings; improved handling with increased routine |
|
|
Negative | Preference toward classic therapy; more training than therapy; technical issues; initial skepticism |
| Web-based communication | ||
|
|
Online reminders | Require organized working style; increase compliance; unwanted effects |
| Online feedback | Important feature; needs to be short in duration | |
| Patients’ differences | ||
|
|
Optional classic treatment path | Adaptation to patient preferences; possible side effects |
|
|
Differences in patients | Not for severe depression; amount of required guidance time; differences in media affinity; requires openness and compliance |
Table 5.
Benefits and drawbacks of blended group therapy (bGT) according to interview follow-up survey (n=8).
| Statementa | Percentages | Mean (SD) | |
|
|
Agree (rather agree) | Disagree (rather disagree) |
|
| I am more open after experience with bGTa | 25 (75) | 0 (0) | 3.25 (0.46) |
| I am more critical after experience with bGTa | 0 (0) | 13 (88) | 1.86 (0.36) |
| I have serious concerns about data safetya | 0 (25) | 25 (50) | 2.00 (0.76) |
| bGT may also be feasible for in-patient treatmenta | 13 (75) | 0 (13) | 3 (0.53) |
| Advantages of more flexible working hours because of Web-based guidancea | 50 (38) | 13 (0) | 3.25 (1.03) |
| Computer elementsb should be used for in-session supporta | 50 (25) | 0 (25) | 3.25 (0.89) |
| Overuse of in-session media can hamper group dynamicsa | 50 (38) | 0 (13) | 3.38 (0.75) |
| Overuse of in-session media did hamper dynamics in my groupsa | 0 (25) | 50 (25) | 1.75 (0.87) |
| Computer elementsc should be used for between-session supporta | 63 (38) | 0 (0) | 3.63 (0.52) |
| Platform prepares patients optimally for group reunionsa | 38 (63) | 0 (0) | 3.38 (0.52) |
| Repeated application of therapy content fosters abilities (CE, app, and session)a | 38 (63) | 0 (0) | 3.38 (0.52) |
| Reminders increased compliance with Web-based tasksa | 13 (75) | 0 (13) | 3.00 (0.53) |
| bGT cannot increase treatment transfera | 0 (13) | 38 (50) | 1.75 (0.71) |
| Reminders did exert a lot of pressure on some patientsa | 13 (50) | 0 (38) | 2.75 (0.71) |
| Additional between-session therapist time needs to be reimburseda | 88 (13) | 0 (0) | 3.88 (0.35) |
| Patients shared additional private concerns over platform (online disinhibition)a,d | 50 (34) | 0 (17) | 3.33 (0.82) |
| Between-session contact made me feel more connected with clientsa,d | 17 (83) | 0 (0) | 3.17 (0.41) |
| Between-session contact does not promote relationship with clienta,d | 0 (0) | 33 (67) | 1.67 (0.52) |
aExact wording is provided in Multimedia Appendix 2.
bSlides and videos.
cPlatform, app, and monitoring.
dOptional questions only applied to 6 therapists.
In the wider perspective, therapists agreed that bGT can have a positive impact on current forms of group therapy and that they had more positive attitudes toward bGT after applying this format. Perceived merits of bGT were augmented monitoring, in addition to patients’ responsiveness to given online reminders in terms of increased treatment adherence. Most therapists agreed that patients would profit from the technology-aided treatment transfer and from the repeated presentation of therapy materials (platform, app, and group sessions). Furthermore, they agreed that Web-based modules would prepare patients for subsequent group reunions. A total of 6 out of 8 therapists reported that particular patients disclosed more openly via private Web-based communication (online disinhibition effect) compared with the group meetings. Individual differences emerged in the preference of particular treatment elements. Although some therapists emphasized the added value of between-session elements, others underpinned the merits of applied in-session tools.
With regard to the potential risks of bGT, a consensus emerged that in-session media should be applied cautiously (eg, overloaded sessions) and that the intervention at times may have hampered some of the desired group dynamics (eg, too little time for discussions). In this context, the preservation of technology-free group sessions was suggested. Furthermore, 2 therapists also advocated a cautious use of Web-based reminders and prompts to prevent less interested patients from feeling overwhelmed or discouraged. During the interview, 1 therapist expressed serious concerns about data safety.
Discussion
Principal Findings
This study investigated the feasibility of a mobile- and Web-supported bGT for depression, with a focus on therapists’ perception of and patients’ adherence to the novel format. High effects on self-reported depressiveness and general health, as well as beneficial effects on ACT-related secondary outcomes, were observed. Effects remained stable over a short follow-up period. Therapist interviews revealed high treatment applicability and perceived benefits concerned treatment availability and monitoring and transfer, as well as the establishment of the therapeutic relation. On an average, therapists spent 10 min per patient per week with online guidance, with decreasing guidance over the course of time and variation between individual groups. Regarding patients’ system usage, participants almost equally engaged in weekly group reunions and Web-based tasks. Usage patterns of the mobile-based diary varied to some extent.
Applied primary outcome measures indicated substantial effects on self-reported depressiveness and general health after the outpatient treatment had ended. Observed effects correspond to earlier bGT depression studies [40,41,74], to benchmarking meta-analyses on group therapy [75-77], and to recent group therapy trials in routine care [78,79]. As guideline-based group CBT usually entails 15- to 20-hour sessions [33], high treatment effects where achieved in a comparably short period of time. Although the most observed effects remained stable, self-reported general health decreased slightly but non significantly at follow-up. To further increase treatment success, different forms of online aftercare [23,24] could easily be integrated into bGT and flexible care solutions, such as discontinuous groups, booster sessions, or online groups [80,81], can be facilitated by bGT. As a related aspect, long-term effects of bGT need to be studied in future trials.
This study adds a first therapist-related perspective to the growing evidence on bGT. Retrospectively, novice therapists described the format as contemporary, featuring patient- and therapist-related, as well as interactional, advantages. They reported patients to engage intensely with the bGT tasks, leading patients to be well prepared for the next group session. Furthermore, they appreciated the format for providing flexible working hours, as well as information about the individual treatment progress. Even though not all therapists were initially fond of the novel format, personal experience increased the self-reported willingness to work with the novel approach [82,83]. As for the perceived disadvantages, therapists mentioned the additional between-session workload and some preferred a more classical format. In this context, some therapists stated that it may be difficult to attract experienced or less-interested therapists and that the treatment had a more training-like character. Furthermore, patients should not feel overwhelmed by the use of technology or the intensity of treatment (eg, reminders).
With regard to the reported improvement of therapeutic alliance, the therapist back-end system allowed personalized feedback on completed tasks (two-third of the time), as well as intimate lateral communication between therapists and clients (one-third of the time). Interviewed therapists appreciated both functionalities, and according to the therapists, patients responded to online prompts, resulting in an increased completion of outstanding therapy tasks. As a last consideration, all therapists that used software with implemented confidential communication (6 out of 8 therapists) reported that some of their patients disclosed more openly via intimate lateral communication. This phenomenon can be classified as a form of the online disinhibition effect [84]. In a previous study, the online disinhibition in bGT seemed to be fostered by the perceived intimacy between the patient and therapist in the absence of an additional audience [42].
As another important feasibility criterion, the amount of additional workload because of Web-based guidance is from particular relevance [85]. Beyond doubt, the time required by therapists depends on the implemented tasks of a given intervention. We found a moderate amount of additional workload in an intervention designed to provide close between-session guidance. Most therapists expected further reductions of required guidance time with a growing routine in conducting bGT. Therapist support is frequently associated with improved treatment adherence and lower dropout rates [15]. Here, bGT can be a reasonable alternative to existing formats, such as Web-based therapy or blended individual therapy.
Treatment flexibility is of particular interest in outpatient groups, as the scheduling of group sessions is usually restricted to evening hours on a specific weekday. On one hand, technology-induced treatment flexibility is appreciated by patients [32,42]. On the other hand, more flexible working hours may also prove to be attractive for certain therapists. Here, increases in flexibility are achieved by moving working hours toward Web-based guidance between sessions. In a double trainer setting with a group size of 8 patients, the expected Web-based guidance for 4 patients takes around 45 min per therapist and week. In this regard, surveyed therapists uniformly emphasized the relevance of reimbursement for Web-based guidance time. Even though this additional workload can easily be compensated by shortening the overall treatment duration [28], such shortenings should be carried out carefully and in accordance with patient needs [86] (eg, time to establish trust in the group).
bGT takes a special position in the field of internet interventions. First, bGT can be a cost-efficient treatment option situated between guided Web-based interventions and blended individual therapy (Figure 1). Compared with Web-based interventions, bGT preserves real-world contact at slightly higher costs. When compared with individual therapy, however, bGT can lead to similar cost savings as known from classical group therapy. Second, group phenomena could be harnessed to support therapist efforts to promote compliance with Web-based tasks [42,87]. Compared with Web-based interventions that sometimes suffer from low adherence rates [15,88], patients engaged to a wide extent in the featured Web-based tasks, as results indicate comparable adherence to group sessions and technology-based elements. Finally, bGT blurs distinctions between individual and group therapy, as it brings a high degree of individualized care to the group format. For example, it opens new ways for intimate patient-to-therapist communication, and it routinely provides therapists with individual information on treatment progress or potential problems [74].
With regard to potential disadvantages of bGT, therapists mentioned that certain participants may feel overwhelmed by the close monitoring of between-session activities or by the number of set reminders. For this reason, the intensity of monitoring and Web-based activities should be adaptable to patient needs. As a second aspect, 2 therapists expressed concerns about data safety. These concerns should be treated with high priority to prevent therapists from being deterred. Third, extensive in-session media use was described as a risk factor, potentially dampening desired group dynamics. Although observable incidences were reported less frequently (Table 5), bGT interventions can profit from a cautious implementation of in-session technology. Fourth, some therapists stated that it may be more difficult to attract experienced or less interested therapists. Thus, incentives seem important to make bGT a workable approach (eg, reimbursement of Web-based guidance time, flexibility of working hours, and balance of work tasks). As a last aspect, 1 therapist mentioned the limited management of acute crisis, which theoretically may be induced by Web-based elements or between-session tasks. Here, technology can provide new ways of emergency management too, for example, by the installation of an emergency button, as seen in a blended app-supported problem-solving treatment for patients with intentional self-harm [89].
This study has several noteworthy strengths and limitations. First, this study adds a first therapist-related perspective to previous findings on bGT [37-42]. Second, it applies a multimodal research strategy (eg, triangulation of quantitative and qualitative methods and implementation of log data) to investigate feasibility in a more holistic way. Third, in accordance with recommendations on the documented use of technology [90], this study provides detailed and objectively measured information on Web-based and mobile app completion rates. Fourth, compared with previous bGT depression studies [40,41] and studies on Web-based interventions [91,92], the current sample composition is more balanced with regard to gender and the level of education. Finally, the study reports deterioration rates and possible risks associated with the novel format.
Among its most important limitations, this study was designed and powered to investigate the feasibility of bGT for depression. The study design, therefore, does not allow any conclusions about technology-induced increases in efficiency or effectiveness. Together with blended individual therapy trials [29,30], future research will have to determine the merits of bGT in terms of augmented treatment effects. Second, many different constellations of blended therapy exist and heterogeneity within the field is high [23]. At hand, findings primarily represent the more integrated forms of blended therapy, whereas less-integrated forms (eg, adjunct Web-based programs) may differ in the therapist’s guidance, the flexibility of treatment, or the intensity of treatment. In this context, bGT concepts for group psychotherapy (>15 to 20 sessions), as well as blends of internet interventions with telegroup therapy [93,94], and discontinuous groups should be developed. Third, even though conducted in an outpatient clinic, the study setting restricts generalizability, as groups were held at an affiliated university center for psychotherapy and counseling, and the sample was self-selected. Therefore, it is probable that clients were more interested in this kind of treatment. Furthermore, the treatment was carried out by novice therapists. Although some study aspects appear less prone to introducing bias (ie, Web-based guidance time or log files), it is likely that novice therapists are more adaptable to innovations. More ample evaluations of therapist views exist in neighboring fields, such as individual blended therapy, tele therapy, and Web-based therapy [16,31,93,94].
Conclusions
This study adds a first therapist perspective to previous research on bGT. Feasibility was supported within a university outpatient setting, treating a demographically balanced sample with a short but intense ACT-based group intervention. Even though the intervention entailed a variety of Web- and app-based elements, the amount of online guidance was manageable, and guidance resulted in more flexible working hours. The Web-based platform was appreciated for the implementation of between-session monitoring and the establishment of therapeutic alliance. According to therapists, compliance with CBT tasks can be fostered by prompts via the Web-based platform, resulting in high adherence rates. Potential negative effects of blending should be regarded in the design and implementation of bGT interventions.
Acknowledgments
This research did not receive any specific grant from funding agencies in the public, commercial, or non-profit sectors.
Abbreviations
- AAQ-II
acceptance and action questionnaire-II
- ACT
Acceptance and Commitment Therapy
- AnTi
Anxious Thoughts Inventory
- BA
Behavioral Activation
- bGT
Blended Group Therapy
- CBT
Cognitive Behavioral Therapy
- CES-D
Center of Epidemiologic Studies Depression
- DIPS
Diagnostic Interview for Psychological Disorders
- GAD
Generalized Anxiety Disorder
- GHQ
General Health Questionnaire
- ITT
intention-to-treat
- PSWQ
Penn State Worry Questionnaire
- RCI
Reliable Change Index
- SUS
System Usability Scale
- ZUF-8
Fragebogen zur Patientenzufriedenheit
Interview guide.
Subsequent questionnaire based on previous therapist-interviews.
Footnotes
Conflicts of Interest: None declared.
References
- 1.Vigo D, Thornicroft G, Atun R. Estimating the true global burden of mental illness. Lancet Psychiatry. 2016 Feb;3(2):171–8. doi: 10.1016/S2215-0366(15)00505-2.S2215-0366(15)00505-2 [DOI] [PubMed] [Google Scholar]
- 2.Tomlinson M, Rudan I, Saxena S, Swartz L, Tsai AC, Patel V. Setting priorities for global mental health research. Bull World Health Organ. 2009 Jun;87(6):438–46. doi: 10.2471/BLT.08.054353. http://www.scielosp.org/scielo.php?script=sci_arttext&pid=S0042-96862009000600012&lng=en&nrm=iso&tlng=en .S0042-96862009000600012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wykes T, Haro JM, Belli SR, Obradors-Tarragó C, Arango C, Ayuso-Mateos JL, Bitter I, Brunn M, Chevreul K, Demotes-Mainard J, Elfeddali I, Evans-Lacko S, Fiorillo A, Forsman AK, Hazo J, Kuepper R, Knappe S, Leboyer M, Lewis SW, Linszen D, Luciano M, Maj M, McDaid D, Miret M, Papp S, Park A, Schumann G, Thornicroft G, van der Feltz-Cornelis C, van Os J, Wahlbeck K, Walker-Tilley T, Wittchen H, ROAMER consortium Mental health research priorities for Europe. Lancet Psychiatry. 2015 Nov;2(11):1036–42. doi: 10.1016/S2215-0366(15)00332-6.S2215-0366(15)00332-6 [DOI] [PubMed] [Google Scholar]
- 4.Andersson G. Internet-delivered psychological treatments. Annu Rev Clin Psychol. 2016;12:157–79. doi: 10.1146/annurev-clinpsy-021815-093006. [DOI] [PubMed] [Google Scholar]
- 5.Cuijpers P, Riper H, Andersson G. Internet-based treatment of depression. Curr Opin Psychol. 2015 Aug;4(4):131–5. doi: 10.1016/j.copsyc.2014.12.026. [DOI] [Google Scholar]
- 6.Păsărelu CR, Andersson G, Bergman Nordgren L, Dobrean A. Internet-delivered transdiagnostic and tailored cognitive behavioral therapy for anxiety and depression: a systematic review and meta-analysis of randomized controlled trials. Cogn Behav Ther. 2017 Dec;46(1):1–28. doi: 10.1080/16506073.2016.1231219. [DOI] [PubMed] [Google Scholar]
- 7.Josephine K, Josefine L, Philipp D, David E, Harald B. Internet- and mobile-based depression interventions for people with diagnosed depression: a systematic review and meta-analysis. J Affect Disord. 2017 Dec 01;223:28–40. doi: 10.1016/j.jad.2017.07.021.S0165-0327(17)30725-5 [DOI] [PubMed] [Google Scholar]
- 8.Rathbone A, Clarry L, Prescott J. Assessing the efficacy of mobile health apps using the basic principles of cognitive behavioral therapy: systematic review. J Med Internet Res. 2017 Dec 28;19(11):e399. doi: 10.2196/jmir.8598. http://www.jmir.org/2017/11/e399/ v19i11e399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Andersson G, Titov N. Advantages and limitations of internet-based interventions for common mental disorders. World Psychiatry. 2014 Feb;13(1):4–11. doi: 10.1002/wps.20083. doi: 10.1002/wps.20083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Emmelkamp P, David D, Beckers T, Muris P, Cuijpers P, Lutz W, Andersson G, Araya R, Banos Rivera RM, Barkham M, Berking M, Berger T, Botella C, Carlbring P, Colom F, Essau C, Hermans D, Hofmann SG, Knappe S, Ollendick TH, Raes F, Rief W, Riper H, Van Der Oord S, Vervliet B. Advancing psychotherapy and evidence-based psychological interventions. Int J Methods Psychiatr Res. 2014 Jan;23(Suppl 1):58–91. doi: 10.1002/mpr.1411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Titov N, Dear BF, Staples LG, Bennett-Levy J, Klein B, Rapee RM, Shann C, Richards D, Andersson G, Ritterband L, Purtell C, Bezuidenhout G, Johnston L, Nielssen OB. MindSpot Clinic: an accessible, efficient, and effective online treatment service for anxiety and depression. Psychiatr Serv. 2015 Oct;66(10):1043–50. doi: 10.1176/appi.ps.201400477. [DOI] [PubMed] [Google Scholar]
- 12.Hedman E, Ljótsson B, Kaldo V, Hesser H, El Alaoui S, Kraepelien M, Andersson E, Rück C, Svanborg C, Andersson G, Lindefors N. Effectiveness of Internet-based cognitive behaviour therapy for depression in routine psychiatric care. J Affect Disord. 2014 Feb;155:49–58. doi: 10.1016/j.jad.2013.10.023.S0165-0327(13)00765-9 [DOI] [PubMed] [Google Scholar]
- 13.Titov N, Dear B, Nielssen O, Staples L, Hadjistavropoulos H, Nugent M, Adlam K, Nordgreen T, Bruvik KH, Hovland A, Repål A, Mathiasen K, Kraepelien M, Blom K, Svanborg C, Lindefors N, Kaldo V. ICBT in routine care: a descriptive analysis of successful clinics in five countries. Internet Interv. 2018 Sep;13:108–15. doi: 10.1016/j.invent.2018.07.006. https://linkinghub.elsevier.com/retrieve/pii/S2214-7829(18)30037-X .S2214-7829(18)30037-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Johansson R, Andersson G. Internet-based psychological treatments for depression. Expert Rev Neurother. 2012 Jul;12(7):861–9. doi: 10.1586/ern.12.63. [DOI] [PubMed] [Google Scholar]
- 15.Richards D, Richardson T. Computer-based psychological treatments for depression: a systematic review and meta-analysis. Clin Psychol Rev. 2012 Jun;32(4):329–42. doi: 10.1016/j.cpr.2012.02.004.S0272-7358(12)00027-X [DOI] [PubMed] [Google Scholar]
- 16.Schuster R, Pokorny R, Berger T, Topooco N, Laireiter AR. The advantages and disadvantages of online and blended therapy: survey study amongst licensed psychotherapists in Austria. J Med Internet Res. 2018 Dec 18;20(12):e11007. doi: 10.2196/11007. http://www.jmir.org/2018/12/e11007/ v20i12e11007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Topooco N, Riper H, Araya R, Berking M, Brunn M, Chevreul K, Cieslak R, Ebert DD, Etchmendy E, Herrero R, Kleiboer A, Krieger T, García-Palacios A, Cerga-Pashoja A, Smoktunowicz E, Urech A, Vis C, Andersson G, E-COMPARED consortium Attitudes towards digital treatment for depression: a European stakeholder survey. Internet Interv. 2017 Jun;8:1–9. doi: 10.1016/j.invent.2017.01.001. https://linkinghub.elsevier.com/retrieve/pii/S2214-7829(16)30044-6 .S2214-7829(16)30044-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ly K, Trüschel A, Jarl L, Magnusson S, Windahl T, Johansson R, Carlbring P, Andersson G. Behavioural activation versus mindfulness-based guided self-help treatment administered through a smartphone application: a randomised controlled trial. BMJ Open. 2014 Jan 09;4(1):e003440. doi: 10.1136/bmjopen-2013-003440. http://bmjopen.bmj.com/cgi/pmidlookup?view=long&pmid=24413342 .bmjopen-2013-003440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ly K, Janni E, Wrede R, Sedem M, Donker T, Carlbring P, Andersson G. Experiences of a guided smartphone-based behavioral activation therapy for depression: a qualitative study. Internet Interv. 2015 Mar;2(1):60–8. doi: 10.1016/j.invent.2014.12.002. [DOI] [Google Scholar]
- 20.Nahum M, Van Vleet TM, Sohal VS, Mirzabekov JJ, Rao VR, Wallace DL, Lee MB, Dawes H, Stark-Inbar A, Jordan JT, Biagianti B, Merzenich M, Chang EF. Immediate Mood Scaler: tracking symptoms of depression and anxiety using a novel mobile mood scale. JMIR Mhealth Uhealth. 2017 Apr 12;5(4):e44. doi: 10.2196/mhealth.6544. http://mhealth.jmir.org/2017/4/e44/ v5i4e44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shen N, Levitan MJ, Johnson A, Bender JL, Hamilton-Page M, Jadad AA, Wiljer D. Finding a depression app: a review and content analysis of the depression app marketplace. JMIR Mhealth Uhealth. 2015 Feb 16;3(1):e16. doi: 10.2196/mhealth.3713. http://mhealth.jmir.org/2015/1/e16/ v3i1e16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Krieger T, Meyer B, Sude K, Urech A, Maercker A, Berger T. Evaluating an e-mental health program ("deprexis") as adjunctive treatment tool in psychotherapy for depression: design of a pragmatic randomized controlled trial. BMC Psychiatry. 2014 Oct 08;14:285. doi: 10.1186/s12888-014-0285-9. https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-014-0285-9 .s12888-014-0285-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Erbe D, Eichert HC, Riper H, Ebert DD. Blending face-to-face and internet-based interventions for the treatment of mental disorders in adults: systematic review. J Med Internet Res. 2017 Dec 15;19(9):e306. doi: 10.2196/jmir.6588. http://www.jmir.org/2017/9/e306/ v19i9e306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ebert D, Tarnowski T, Gollwitzer M, Sieland B, Berking M. A transdiagnostic internet-based maintenance treatment enhances the stability of outcome after inpatient cognitive behavioral therapy: a randomized controlled trial. Psychother Psychosom. 2013;82(4):246–56. doi: 10.1159/000345967.000345967 [DOI] [PubMed] [Google Scholar]
- 25.Kleiboer A, Smit J, Bosmans J, Ruwaard J, Andersson G, Topooco N, Berger T, Krieger T, Botella C, Baños R, Chevreul K, Araya R, Cerga-Pashoja A, Cieślak R, Rogala A, Vis C, Draisma S, van Schaik A, Kemmeren L, Ebert D, Berking M, Funk B, Cuijpers P, Riper H. European COMPARative Effectiveness research on blended Depression treatment versus treatment-as-usual (E-COMPARED): study protocol for a randomized controlled, non-inferiority trial in eight European countries. Trials. 2016 Dec 03;17(1):387. doi: 10.1186/s13063-016-1511-1. https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-016-1511-1 .10.1186/s13063-016-1511-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ly K, Topooco N, Cederlund H, Wallin A, Bergström J, Molander O, Carlbring P, Andersson G. Smartphone-supported versus full behavioural activation for depression: a randomised controlled trial. PLoS One. 2015;10(5):e0126559. doi: 10.1371/journal.pone.0126559. http://dx.plos.org/10.1371/journal.pone.0126559 .PONE-D-14-40400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Urech A, Krieger T, Möseneder L, Biaggi A, Vincent A, Poppe C, Meyer B, Riper H, Berger T. A patient post hoc perspective on advantages and disadvantages of blended cognitive behaviour therapy for depression: A qualitative content analysis. Psychother Res. 2018 Jan 31;:1–13. doi: 10.1080/10503307.2018.1430910. (forthcoming) [DOI] [PubMed] [Google Scholar]
- 28.Thase M, Wright JH, Eells TD, Barrett MS, Wisniewski SR, Balasubramani GK, McCrone P, Brown GK. Improving the efficiency of psychotherapy for depression: computer-assisted versus standard CBT. Am J Psychiatry. 2018 Dec 01;175(3):242–50. doi: 10.1176/appi.ajp.2017.17010089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Berger T, Krieger T, Sude K, Meyer B, Maercker A. Evaluating an e-mental health program ("deprexis") as adjunctive treatment tool in psychotherapy for depression: Results of a pragmatic randomized controlled trial. J Affect Disord. 2018 Dec;227:455–62. doi: 10.1016/j.jad.2017.11.021.S0165-0327(17)31255-7 [DOI] [PubMed] [Google Scholar]
- 30.Zwerenz R, Becker J, Knickenberg RJ, Siepmann M, Hagen K, Beutel ME. Online self-help as an add-on to inpatient psychotherapy: efficacy of a new blended treatment approach. Psychother Psychosom. 2017;86(6):341–350. doi: 10.1159/000481177.000481177 [DOI] [PubMed] [Google Scholar]
- 31.Titzler I, Saruhanjan K, Berking M, Riper H, Ebert DD. Barriers and facilitators for the implementation of blended psychotherapy for depression: a qualitative pilot study of therapists' perspective. Internet Interv. 2018 Jun;12:150–64. doi: 10.1016/j.invent.2018.01.002. https://linkinghub.elsevier.com/retrieve/pii/S2214-7829(17)30090-8 .S2214-7829(17)30090-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.van der Vaart R, Witting M, Riper H, Kooistra L, Bohlmeijer ET, van Gemert-Pijnen LJ. Blending online therapy into regular face-to-face therapy for depression: content, ratio and preconditions according to patients and therapists using a Delphi study. BMC Psychiatry. 2014 Dec 14;14:355. doi: 10.1186/s12888-014-0355-z. https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-014-0355-z .s12888-014-0355-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.DeLucia-Waack J, Kalodner CR, Riva M. Handbook of Group Counseling and Psychotherapy. London, UK: Sage Publications; 2013. [Google Scholar]
- 34.Conyne R. The Oxford Handbook of Group Counseling (Oxford Library of Psychology) Oxford, UK: Oxford University Press; 2011. [Google Scholar]
- 35.Przeworski A, Newman MG. Palmtop computer-assisted group therapy for social phobia. J Clin Psychol. 2004 Feb;60(2):179–88. doi: 10.1002/jclp.10246. [DOI] [PubMed] [Google Scholar]
- 36.Gruber K, Moran PJ, Roth WT, Taylor CB. Computer-assisted cognitive behavioral group therapy for social phobia. Behav Ther. 2001;32(1):155–65. doi: 10.1016/S0005-7894(01)80050-2. [DOI] [Google Scholar]
- 37.Newman MG, Przeworski A, Consoli AJ, Taylor CB. A randomized controlled trial of ecological momentary intervention plus brief group therapy for generalized anxiety disorder. Psychotherapy (Chic) 2014 Jun;51(2):198–206. doi: 10.1037/a0032519. http://europepmc.org/abstract/MED/24059730 .2013-33240-001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Samaan Z, Dennis BB, Kalbfleisch L, Bami H, Zielinski L, Bawor M, Litke K, McCabe K, Whattam J, Garrick L, O'Neill L, Tabak TA, Simons S, Chalmers S, Key B, Vanstone M, Xie F, Guyatt G, Thabane L. Behavioral activation group therapy for reducing depressive symptoms and improving quality of life: a feasibility study. Pilot Feasibility Stud. 2016;2:22. doi: 10.1186/s40814-016-0064-0. https://pilotfeasibilitystudies.biomedcentral.com/articles/10.1186/s40814-016-0064-0 .64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Aguilera A, Bruehlman-Senecal E, Demasi O, Avila P. Automated text messaging as an adjunct to cognitive behavioral therapy for depression: a clinical trial. J Med Internet Res. 2017 Dec 08;19(5):e148. doi: 10.2196/jmir.6914. http://www.jmir.org/2017/5/e148/ v19i5e148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schuster R, Leitner I, Carlbring P, Laireiter A. Exploring blended group interventions for depression: randomised controlled feasibility study of a blended computer- and multimedia-supported psychoeducational group intervention for adults with depressive symptoms. Internet Interv. 2017 Jun;8:63–71. doi: 10.1016/j.invent.2017.04.001. https://linkinghub.elsevier.com/retrieve/pii/S2214-7829(16)30068-9 .S2214-7829(16)30068-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schuster R, Fichtenbauer I, Sparr VM, Berger T, Laireiter AR. Feasibility of a blended group treatment (bGT) for major depression: uncontrolled interventional study in a university setting. BMJ Open. 2018 Mar 12;8(3):e018412. doi: 10.1136/bmjopen-2017-018412. http://bmjopen.bmj.com/cgi/pmidlookup?view=long&pmid=29530905 .bmjopen-2017-018412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schuster R, Sigl S, Berger T, Laireiter AR. Patients' experiences of web- and mobile-assisted group therapy for depression and implications of the group setting: qualitative follow-up study. JMIR Ment Health. 2018 Jul 11;5(3):e49. doi: 10.2196/mental.9613. http://mental.jmir.org/2018/3/e49/ v5i3e49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hayes SC. Acceptance and commitment therapy, relational frame theory, and the third wave of behavioral and cognitive therapies - republished article. Behav Ther. 2016 Nov;47(6):869–85. doi: 10.1016/j.beth.2016.11.006.S0005-7894(16)30094-6 [DOI] [PubMed] [Google Scholar]
- 44.Lejuez CW, Hopko DR, Acierno R, Daughters SB, Pagoto SL. Ten year revision of the brief behavioral activation treatment for depression: revised treatment manual. Behav Modif. 2011 Mar;35(2):111–61. doi: 10.1177/0145445510390929.35/2/111 [DOI] [PubMed] [Google Scholar]
- 45.Hautzinger M, Bailer M. Allgemeine Depressions Skala (ADS). Manual. Weinheim, Germany: Beltz; 1993. [Google Scholar]
- 46.Hautzinger M, Bailer M, Hofmeister D, Keller F. Allgemeine Depressionsskala. Manual (2nd ed.) Göttingen, Germany: Hogrefe; 2012. [Google Scholar]
- 47.Margraf J. [Mini-DIPS: Diagnostic short interview on mental disorders] Berlin, Germany: Springer; 2013. pp. 1–2. [Google Scholar]
- 48.Margraf J, Ehlers A, DiNardo P, Barlow D. [DIPS Diagnostic Interview for Mental Disorders: Interview Guide] Berlin, Germany: Springer; 2013. pp. 1–2. [Google Scholar]
- 49.Kanter JW, Baruch DE, Gaynor ST. Acceptance and commitment therapy and behavioral activation for the treatment of depression: description and comparison. Behav Anal. 2006;29(2):161–85. doi: 10.1007/BF03392129. http://europepmc.org/abstract/MED/22478462 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mazzucchelli T, Kane R, Rees C. Behavioral activation treatments for depression in adults: a meta-analysis and review. Clin Psychology-Sci Pr. 2009;16(4):383–411. doi: 10.1111/j.1468-2850.2009.01178.x. [DOI] [Google Scholar]
- 51.Carlbring P, Hägglund M, Luthström A, Dahlin M, Kadowaki A, Vernmark K, Andersson G. Internet-based behavioral activation and acceptance-based treatment for depression: a randomized controlled trial. J Affect Disord. 2013 Jun;148(2-3):331–7. doi: 10.1016/j.jad.2012.12.020.S0165-0327(12)00853-1 [DOI] [PubMed] [Google Scholar]
- 52.Harris R. [Difficult Situations in Acceptance and Commitment Therapy (ACT)] Germany: Belz; 2014. [Google Scholar]
- 53.Zettle R. ACT for Depression: A Clinician's Guide to Using Acceptance and Commitment Therapy in Treating Depression. Oakland,CA: New Harbinger Publications; 2007. pp. 1–2. [Google Scholar]
- 54.Lehr D, Hillert A, Schmitz E, Sosnowsky N. [ Screening of Depressive Disorders Using the General Depression Scale (ADS-K) and State-Trait Depression Scales (STDS-T)] Diagnostica. 2008 Apr;54(2):61–70. doi: 10.1026/0012-1924.54.2.61. [DOI] [Google Scholar]
- 55.Goldberg D, Williams PA. A users's guide to the General Health Questionnaire. Windsor,UK: NFER-Nelson; 1988. pp. 1–2. [Google Scholar]
- 56.Goldberg DP, Gater R, Sartorius N, Ustun TB, Piccinelli M, Gureje O, Rutter C. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol Med. 1997 Jan;27(1):191–7. doi: 10.1017/s0033291796004242. [DOI] [PubMed] [Google Scholar]
- 57.Schmitz N, Kruse J, Tress W. Psychometric properties of the General Health Questionnaire (GHQ-12) in a German primary care sample. Acta Psychiatr Scand. 1999 Dec;100(6):462–8. doi: 10.1111/j.1600-0447.1999.tb10898.x. [DOI] [PubMed] [Google Scholar]
- 58.Hoyer J, Gloster AT. [Measuring psychological flexibility: the questionnaire on acceptance and action II] Verhaltenstherapie. 2013 Feb 22;23(1):42–44. doi: 10.1159/000347040. [DOI] [Google Scholar]
- 59.Bond FW, Hayes SC, Baer RA, Carpenter KM, Guenole N, Orcutt HK, Waltz T, Zettle RD. Preliminary psychometric properties of the Acceptance and Action Questionnaire-II: a revised measure of psychological inflexibility and experiential avoidance. Behav Ther. 2011 Dec;42(4):676–88. doi: 10.1016/j.beth.2011.03.007.S0005-7894(11)00088-8 [DOI] [PubMed] [Google Scholar]
- 60.Wells A. A multi-dimensional measure of worry: development and preliminary validation of the anxious thoughts inventory. Anxiety Stress Coping. 1994 Jan;6(4):289–99. doi: 10.1080/10615809408248803. [DOI] [Google Scholar]
- 61.Hoyer J. In: AnTI-Anxious Thoughts Inventory-[German version] Rebstock U, editor. Frankfurt, Germany: Universität Frankfurt; 1996. [Google Scholar]
- 62.Berle D, Starcevic V, Moses K, Hannan A, Milicevic D, Sammut P. Preliminary validation of an ultra-brief version of the Penn State Worry Questionnaire. Clin Psychol Psychother. 2011;18(4):339–46. doi: 10.1002/cpp.724. [DOI] [PubMed] [Google Scholar]
- 63.Meyer T, Miller ML, Metzger RL, Borkovec TD. Development and validation of the Penn State Worry Questionnaire. Behav Res Ther. 1990;28(6):487–95. doi: 10.1016/0005-7967(90)90135-6.0005-7967(90)90135-6 [DOI] [PubMed] [Google Scholar]
- 64.Brooke J. Redhatch Consulting Ltd. 1996. [2019-03-04]. SUS: A quickdirty usability scale https://hell.meiert.org/core/pdf/sus.pdf .
- 65.Bangor A, Kortum P, Miller J. Determining what individual SUS scores mean: adding an adjective rating scale. J Usability Stud. 2009;4(3):114–123. http://uxpajournal.org/determining-what-individual-sus-scores-mean-adding-an-adjective-rating-scale/ [Google Scholar]
- 66.Schmidt J, Lamprecht F, Wittmann WW. [Satisfaction with inpatient care. Development of a questionnaire and initial validity studies] Psychother Psychosom Med Psychol. 1989;39:248. https://psycnet.apa.org/record/1991-75702-001 . [PubMed] [Google Scholar]
- 67.Attkisson CC, Zwick R. The client satisfaction questionnaire. Psychometric properties and correlations with service utilization and psychotherapy outcome. Eval Program Plann. 1982;5(3):233–7. doi: 10.1016/0149-7189(82)90074-x.0149-7189(82)90074-X [DOI] [PubMed] [Google Scholar]
- 68.Hannöver W, Dogs C, Kordy H. [Patient satisfaction - a measure of treatment success?] Psychotherapeut. 2000 Sep 25;45(5):292–300. doi: 10.1007/s002780000094. [DOI] [Google Scholar]
- 69.Jacobson NS, Truax P. Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. J Consult Clin Psychol. 1991 Feb;59(1):12–9. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- 70.Lambert MJ, Ogles BM. Using clinical significance in psychotherapy outcome research: the need for a common procedure and validity data. Psychother Res. 2009 Jul;19(4-5):493–501. doi: 10.1080/10503300902849483.914764151 [DOI] [PubMed] [Google Scholar]
- 71.Cohen J. Statistical Power Analysis for the Behavioral Sciences (2nd Edition) Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. pp. 37–42. [Google Scholar]
- 72.Faul F, Erdfelder E, Lang A, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007 May;39(2):175–91. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- 73.Mayring P. Qualitative Content Analysis: Theoretical Foundation, Basic Procedures and Software Solution. Berlin, Germany: Leibniz Insitutute; 2018. [Google Scholar]
- 74.Marmarosh CL. Introduction to special issue: feedback in group psychotherapy. Psychotherapy (Chic) 2018 Dec;55(2):101–104. doi: 10.1037/pst0000178.2018-25950-001 [DOI] [PubMed] [Google Scholar]
- 75.Burlingame GM, Fuhriman A, Mosier J. The differential effectiveness of group psychotherapy: a meta-analytic perspective. Group Dyn. 2003;7(1):3–12. doi: 10.1037/1089-2699.7.1.3. [DOI] [Google Scholar]
- 76.Burlingame GM, Seebeck JD, Janis RA, Whitcomb KE, Barkowski S, Rosendahl J, Strauss B. Outcome differences between individual and group formats when identical and nonidentical treatments, patients, and doses are compared: A 25-year meta-analytic perspective. Psychotherapy (Chic) 2016 Dec;53(4):446–61. doi: 10.1037/pst0000090.2016-58498-004 [DOI] [PubMed] [Google Scholar]
- 77.McDermut W, Miller I, Brown R A. The efficacy of group psychotherapy for depression: a meta analysis and review of the empirical research. Clin Psychol-Sci Pr. 2001;8(1):98–116. doi: 10.1093/clipsy/8.1.98. [DOI] [Google Scholar]
- 78.Delgadillo J, Kellett S, Ali S, McMillan D, Barkham M, Saxon D, Donohoe G, Stonebank H, Mullaney S, Eschoe P, Thwaites R, Lucock M. A multi-service practice research network study of large group psychoeducational cognitive behavioural therapy. Behav Res Ther. 2016 Dec;87:155–161. doi: 10.1016/j.brat.2016.09.010.S0005-7967(16)30167-X [DOI] [PubMed] [Google Scholar]
- 79.Thimm JC, Antonsen L. Effectiveness of cognitive behavioral group therapy for depression in routine practice. BMC Psychiatry. 2014 Oct 21;14:292. doi: 10.1186/s12888-014-0292-x. https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-014-0292-x .s12888-014-0292-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bauer S, Wolf M, Haug S, Kordy H. The effectiveness of internet chat groups in relapse prevention after inpatient psychotherapy. Psychother Res. 2011 Mar;21(2):219–26. doi: 10.1080/10503307.2010.547530.933985701 [DOI] [PubMed] [Google Scholar]
- 81.Nordh M, Vigerland S, Öst LG, Ljótsson B, Mataix-Cols D, Serlachius E, Högström J. Therapist-guided internet-delivered cognitive-behavioural therapy supplemented with group exposure sessions for adolescents with social anxiety disorder: a feasibility trial. BMJ Open. 2017 Dec 14;7(12):e018345. doi: 10.1136/bmjopen-2017-018345. http://bmjopen.bmj.com/cgi/pmidlookup?view=long&pmid=29247101 .bmjopen-2017-018345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Månsson KN, Klintmalm H, Nordqvist R, Andersson G. Conventional cognitive behavioral therapy facilitated by an internet-based support system: feasibility study at a psychiatric outpatient clinic. JMIR Res Protoc. 2017 Aug 24;6(8):e158. doi: 10.2196/resprot.6035. http://www.researchprotocols.org/2017/8/e158/ v6i8e158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kaiser T, Schmutzhart L, Laireiter AR. Attitudes of Austrian psychotherapists towards process and outcome monitoring. Adm Policy Ment Health. 2018 Dec;45(5):765–79. doi: 10.1007/s10488-018-0862-1. http://europepmc.org/abstract/MED/29520535 .10.1007/s10488-018-0862-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Suler J. The online disinhibition effect. Cyberpsychol Behav. 2004 Jun;7(3):321–6. doi: 10.1089/1094931041291295. [DOI] [PubMed] [Google Scholar]
- 85.Kenter R, van de Ven P, Cuijpers P, Koole G, Niamat S, Gerrits R, Willems M, van Straten A. Costs and effects of internet cognitive behavioral treatment blended with face-to-face treatment: results from a naturalistic study. Internet Interv. 2015 Mar;2(1):77–83. doi: 10.1016/j.invent.2015.01.001. [DOI] [Google Scholar]
- 86.Ruwaard J, Kok R. European Health Psychologist. 2015. [2019-03-04]. Wild West eHealth: Time to hold our horses? https://www.ehps.net/ehp/index.php/contents/article/view/765 .
- 87.Ivanov V, Enander J, Mataix-Cols D, Serlachius E, Månsson KN, Andersson G, Flygare O, Tolin D, Rück C. Enhancing group cognitive-behavioral therapy for hoarding disorder with between-session internet-based clinician support: A feasibility study. J Clin Psychol. 2018 Jul;74(7):1092–105. doi: 10.1002/jclp.22589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Christensen H, Griffiths KM, Farrer L. Adherence in internet interventions for anxiety and depression. J Med Internet Res. 2009 Apr 24;11(2):e13. doi: 10.2196/jmir.1194. http://www.jmir.org/2009/2/e13/ v11i2e13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Mackie C, Dunn N, MacLean S, Testa V, Heisel M, Hatcher S. A qualitative study of a blended therapy using problem solving therapy with a customised smartphone app in men who present to hospital with intentional self-harm. Evid Based Ment Health. 2017 Dec;20(4):118–22. doi: 10.1136/eb-2017-102764.eb-2017-102764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Sieverink F, Kelders SM, van Gemert-Pijnen JE. Clarifying the concept of adherence to eHealth technology: systematic review on when usage becomes adherence. J Med Internet Res. 2017 Dec 06;19(12):e402. doi: 10.2196/jmir.8578. http://www.jmir.org/2017/12/e402/ v19i12e402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Lindner P, Nyström MB, Hassmén P, Andersson G, Carlbring P. Who seeks ICBT for depression and how do they get there? Effects of recruitment source on patient demographics and clinical characteristics. Internet Interv. 2015 May;2(2):221–5. doi: 10.1016/j.invent.2015.04.002. [DOI] [Google Scholar]
- 92.Klein JP, Gamon C, Späth C, Berger T, Meyer B, Hohagen F, Hautzinger M, Lutz W, Vettorazzi E, Moritz S, Schröder J. Does recruitment source moderate treatment effectiveness? A subgroup analysis from the EVIDENT study, a randomised controlled trial of an internet intervention for depressive symptoms. BMJ Open. 2017 Jul 13;7(7):e015391. doi: 10.1136/bmjopen-2016-015391. http://bmjopen.bmj.com/cgi/pmidlookup?view=long&pmid=28710212 .bmjopen-2016-015391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Greene CJ, Morland LA, Macdonald A, Frueh BC, Grubbs KM, Rosen CS. How does tele-mental health affect group therapy process? Secondary analysis of a noninferiority trial. J Consult Clin Psychol. 2010 Oct;78(5):746–50. doi: 10.1037/a0020158.2010-19874-015 [DOI] [PubMed] [Google Scholar]
- 94.Marton K, Kanas N. Telehealth modalities for group therapy: comparisons to in-person group therapy. Int J Group Psychother. 2015 Dec 14;66(1):145–50. doi: 10.1080/00207284.2015.1096109. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Interview guide.
Subsequent questionnaire based on previous therapist-interviews.


