Abstract
Self-myofascial release (SMR) is an alternative therapy believed to increase myofascial mobility by exciting muscles and increasing blood flow to the treated area. Previous literature suggest SMR produces conflicting results on performance, muscle activation, range of motion (ROM), and recovery. This study was designed to utilize SMR on a fatigued individual prior to exercise and measure its’ effects on muscle activation, ROM, and perceived recovery compared to a dynamic warm-up session. The findings could help develop an efficient warm-up protocol for resistance-trained individuals. Electromyography (EMG) measured muscle activation of the rectus femoris (RF) and the gluteus maximus (GM), while a bluetooth goniometer assessed knee ROM during a submaximal back-squat. Eleven resistance trained participants (estimated squat 1RM 163% body weight) completed four total sessions of testing with sessions 1 and 3 solely used to induce muscle fatigue. In a counterbalanced design, participants during sessions 2 and 4 received either a dynamic standardized warm-up, or a SMR warm-up. Participants performed 10 repetitions of the back-squat at 70% estimated 1RM load. Peak and mean muscle activation of both muscles, knee ROM, and participants’ perceived recovery was measured during the submaximal repetitions during sessions 2 and 4. Results indicated no significant differences between the dynamic warm-up and SMR warm-up among muscle activation, knee ROM, and participants perceived recovery (p > 0.05). In resistance trained squatters, coaches/trainers can prescribe SMR or a dynamic warm-up/stretching routine for results indicated no differences in perceived recovery, muscle activation, or squat depth.
Keywords: Foam Rolling, electromyography, flexibility, muscle soreness
INTRODUCTION
The squat is a fundamental daily movement that is required for individuals to perform everyday activities such as getting out of a chair, picking up objects, and most all sporting activities (17). According to Duehring et al., it is a key form of exercise shown to increase performance in strength and conditioning (6). Self-myofascial release (SMR) is a type of massage therapy often used to treat muscle pain and stiffness by applying pressure on the thin fascia tissue surrounding the muscle. Previous literature suggests SMR relaxes the contracted muscles by inducing a Golgi tendon organ (GTO) reflex. In theory, SMR causes tension to a fatigued muscles. This in turn causes the GTO reflex to initiate a relaxation or inhibition to the tensed muscle via the peripheral nervous system (7,9,12). Literature also has stated SMR improves fatigued muscles by increasing blood flow which transports essential hormones throughout the body to aide in recovery to the damage site (7,9,12). In combination of both mechanisms, the relaxation of the muscles and increase in blood flow are two benefits most commonly associated with SMR, though results are conflicting.
Previous research has shown benefits to SMR using a foam or stick roller, and the topic has gained popularity over recent years with more research emerging (2). Montiero et al. (16) reported that self-massage on the anterior thigh resulted in a statistically greater range of motion (ROM) in both hip extension and flexion. Further research by Jay et al. (11) suggests that a form of SMR directly following exercise reduces the self-perceived intensity of muscle soreness following exercise known as delayed onset muscle soreness (DOMS). Previously, treatments the following days were an effective way to relieve DOMS (14) measured with a Perceived Recovery Scale (PRS) to quantitatively analyze and assess the rate of DOMS following exercise (13). However, these results are not always conclusive as Fleckenstein et al. (7) concluded, effects of SMR are based on individual variability. Electromyography (EMG) is a device used to measure motor unit activation and can aid in tracking changes in fatigue and recovery during activities such as a squat, deadlift, and other dynamic movements (5,10,12). Bradbury-Squires et al. (2) suggests evidence that foam rolling treatment can be used to increase neuromuscular efficiency, allowing an individual to perform the same tasks without using as much muscle activation measured via EMG.
To further understand the effects of SMR treatment, researchers must compare each measured movement from a baseline measurement. Couture et al. (3) failed to compare their results to any sort of baseline, which could have caused a lack of statistical significance. Although there is differing opinions on what the optimal volume is for SMR treatment, no significant data indicates a gold standard for best results. There is a trend however in studies, while not significant, that SMR produces greater results as the volume or time of treatment increases (2). It is impossible to truly utilize the treatment of self-myofascial release without knowing the outcomes and how to optimize results. Previous literature utilizing SMR treatments have also instructed the participants being examined to SMR roll themselves. This is a potential error as studies have found it is difficult to know the validity of the results without controlling for the time and pressure of the treatment, creating a potential flaw in previous protocols (15,19).
Therefore, the purpose of this study was to observe the effects of SMR treatment compared to a dynamic stretching warm-up on mean and peak muscle activation of the rectus femoris (RF) and gluteus maximus (GM), knee ROM, and perceived recovery during a back squat in a fatigued state. A secondary purpose was to examine how to efficiently and effectively complete a warm up prior to a resistance training protocol, and how to examine SMR affects an individual’s pre/post treatment. It was hypothesized that the SMR treatment would result in improvements of knee ROM and perceived recovery via a PRS, with little to no change in peak or mean muscle activation of the RF and GM muscles.
METHODS
Participants
A power analysis performed by G*POWER 3.1.9.2 (Universitat Kiel, Germany) indicated 11 participants were needed with a power of 0.80, an effect size of 0.8, and an α= 0.05. Eleven highly trained healthy males (176.4±7.5 cm, 84.1±10.2 kgs, 29.4±4.3 yrs) participated in this study, and had lifting experience for 6 months minimum, 2x/week. Participants signed an informed consent and were verbally informed of all procedures prior to testing. A University Institutional Review Board approved this study.
Protocol
A counterbalanced within subjects design was used to measure all dependent variables. Participants completed 4 sessions approximately one hour in length. Session 1 included a familiarization trial with the exercises tested, and a lower body strength training session designed with hopes to induce DOMS. Session 2 consisted of testing and recording muscle activation via EMG, knee ROM, and perceived recovery during a parallel back squat. Session 3 was identical to session 1, a lower body strength training day. Lastly, session 4 was identical to session 2, but in a counterbalanced order receiving either the SMR treatment or traditional dynamic warm-up. Sessions 1 and 2 took place 24 hours apart, along with sessions 3 and 4; while sessions 2 and 3 were spaced by a week. A detailed description of each session are shown in Table 1.
Table 1.
Experimental Design. Flow chart illustrates participants tasks. EMG measured on the RF and GM.
| Day 1 | Day 2 | Day 3 | Day 4 |
|---|---|---|---|
| Standard Warm Up | Standard Warm Up | Standard Warm Up | Standard Warm Up |
| 5 Minute Bike | 5 Minute Bike | 5 Minutes Bike | 5 Minute Bike |
| 15 Back Squat Reps | 15 Back Squat Reps | 15 Back Squat Reps | 15 Back Squat Reps |
| 15 Hip Extension Reps | 15 Hip Extension Reps | 15 Hip Extension Reps | 15 Hip Extension Reps |
| ½ receive 2 mins of SMR | ½ receive 2 mins of SMR | ||
| No SMR=straight to testing | No SMR=straight to testing | ||
| Block 1 | Block 1 | ||
| 3×3 Heavy Back Squat | 3×3 Heavy Back Squat | ||
| 3×10 Back Squat @70%1RM | 3×10 Back Squat @70%1RM | ||
| Block 2 | Testing | Block 2 | Testing |
| 4X10 Box Jump | MVIC of RF and GM | 4×10 Box Jump | MVIC of RF and GM |
| 4×10 SL Weighted Box | 1×10 @70%1RM Back Squat | 4×10 SL Weighted Box | 1×10 @70%1RM Back Squat |
| PRS, EMG and Knee ROM recorded | PRS, EMG and Knee ROM recorded | ||
| Block 3 | Block 3 | ||
| 4×10/ea Lunges (Weighted) | 4×10/ea Lunges (Weighted) | ||
| 4×10/ea Hip Extensions | 4×10/ea Hip Extension | ||
During sessions 2 and 4, participants peak and mean muscle activation was measured via surface EMG (Trigno; Delsys, Natick, MA, USA) of the GM and RF during a submaximal back squat. Placement of the EMG electrode on the GM was exactly halfway on the line between the sacral vertebrae and the greater trochanter, while the sensor on the RF was halfway on the line between the anterior spina iliaca superior and the superior part of the patella. All of the locations and placements of the EMG electrodes followed the guidelines of the SENIAM project (9). Electrodes sat directly on the skin with no interference. Skin was shaved and cleaned to rid the skin of any hair or dead skin on their dominant leg, assessed by which leg they would kick a ball. An Electric goniometer (Delsys Trigno) was used to test ROM at the knee joint during sessions 2 and 4. SMR treatments used the Body Stick (The Stick, model number HD-2400, Atlanta, GA, USA). Lastly, a PRS scale ranging from 1 to 10 measured participants perceived recovery prior to exercise (13).
During sessions 2 and 4, following EMG electrode placement, Maximum Voluntary Isometric Contractions (MVICs) were performed on the RF and GM. The MVIC for the GM was performed by having the participant lay flat on the table with their dominant leg bent at a 90-degree angle. The participant pressed the foot vertically maximally against an immovable object for three seconds (4). The MVIC for the RF placed participants on the edge of a table, both legs hanging off the edge, then instructed to use their dominant leg in knee extension against an immovable object for three seconds (4). The SMR treatment consisted of 2 minutes of heavy pressure performed by the researchers on the RF and GM. SMR treatments were performed by the same primary investigator on all days to prevent error of not being consistent between participants.
The participants that were not receiving SMR that day went straight from the warm up to the testing. Lastly, following the warm-up, participants performed 10 repetitions of the back squat at 70% estimated 1RM load using a National Strength and Conditioning Association training load chart (8).
EMG Signal Processing
EMG signals were full-wave rectified and smoothed using a root-mean-square (RMS) method. A Band pass filter was applied at (low/high pass cut offs) 20–450Hz (20). The mean and peak RMS muscle activity signals during repetitions 4–7 were normalized to the peak muscle activity during the MVIC’s of the (RF) and (GM) (20). The total lift included the eccentric and concentric contraction.
Statistical Analysis
A counterbalanced within participants study design was used. Pre/post measurements of mean and peak GM and RF muscle activation, PRS, and knee ROM were measured with six separate paired samples t-test. An alpha of 0.05, Beta of 0.2, and power of 0.8 were used for all statistical analysis performed using SPSS (version 25, SPSS Inc, Chicago, IL, USA). Two participants muscle activity were removed for the statistical analysis for the peak and mean RF due to the data being ≥2 standard deviations from the mean.
RESULTS
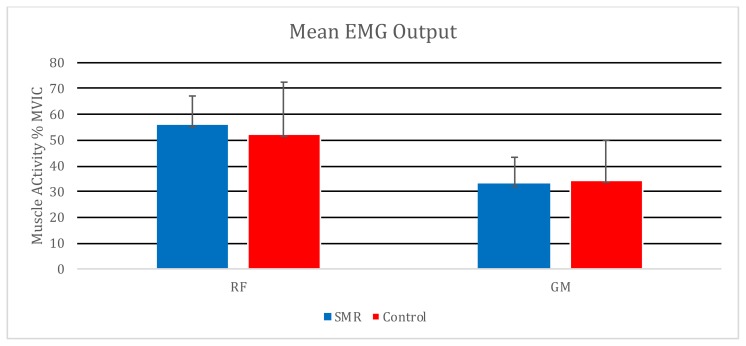
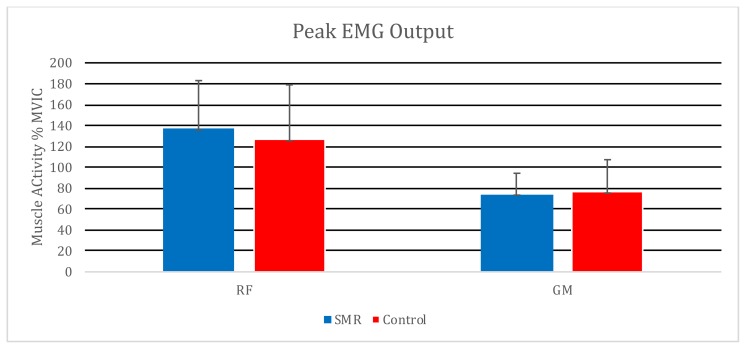
No significant differences were found in peak RF muscle activation, t (9) = −.951, p = 0.366, d = −0.301, or mean RF muscle activation, t (9) = −0.913, p = 0.385, d = −0.289. Further, no significant differences were found in peak GM muscle activation, t (10) = 0.200, p = 0.846, d = 0.060, or mean GM muscle activation, t (10) = 0.301, p = 0.770, d = 0.090.
Recovery did not statistically differ between groups via PRS, t (10) = −1.158, p = 0.274, d = −0.349 (No Treatment Mean = 5.22 ± 1.75, SMR Group Mean = 5.91± 1.81). Lastly, ROM of the knee did not statistically differ among participants, t (10) = 1.191, p = 0.852, d = 0.057 (No Treatment Group Mean = 110.73 ± 11.03, SMR Group Mean = 110.20 ± 12.36).
DISCUSSION
This study examined how SMR treatment prior to back squatting would affect knee ROM, peak and mean muscle activation of the RF and GM, and perceived recovery via a PRS during the back squat exercise. The outcomes indicated a failed hypothesis due to lack of significance of SMR improving knee ROM or perceived recovery. However, our hypothesis was correct regarding no expected difference in mean or peak muscle activation between SMR treatment and dynamic warm- up of the GM and RF muscles.
Previous studies have indicated mixed outcomes regarding SMR treatment on recovery. For example, Fleckenstein et al. indicated no significant effect of foam rolling on reducing muscle fatigue following exercise (7). It was concluded the effects of foam rolling depend on the individual, and there is no constant outcome when it comes to its effect on DOMS. The lack of consistency with the results from using SMR corresponds with the outcomes in the current study. While there were some participants that showed a trend in increased recovery via PRS, overall there was no significant data that allowed for the conclusion that SMR can be confidently relied on to reduce DOMS and increase recovery post exercise.
On the contrary, MacDonald et al. (14) found a significant difference in knee range of motion from implementing the use of a foam roller. A main difference between the current study, and MacDonald et al. that lead to contrasting results could be MacDonald et al. tested recreationally trained resistance trainers classified as moderately active. The current study however examined highly experienced lifters who were extremely well trained. Participants stated subjectively to be highly familiar with squatting and exercising under extreme fatigue. This could have led to the lack of difference in perceived recovery between the SMR and dynamic warm-up group in the current study. Having trained individuals may have caused the SMR treatment to not play as big of role in affecting ROM, muscle activation, and perceived recovery measurements. Other related studies that found significance between SMR and ROM, for the most part, used a weighted lunge to assess ROM rather than a back squat (14,18). The difference in the lunge vs. the back squat movement could impact knee ROM results, due to the participants familiarity with squatting to the same depth during each repetition. While both the lunge and squat are lower body compound movements, they differ in movement mechanics, making it difficult to compare results (8).
If muscle activity is measured across multiple days of testing, EMG data must be normalized to a set reference point. It is possible the MVIC’s performed across two days of testing were not ideal due to the lack of consistency throughout the testing, and the unfamiliarity of the movement. Comparing data to a different normalization method, such as a dynamic task like a 1RM or submaximal repetition, might reduce EMG error and standard deviation across multiple days of testing (1). Future studies should examine more long-term chronic effects of SMR treatment. Furthermore, future research, a similar design and protocol using less trained individuals could lead to more positive outcomes of SMR. Having highly trained individuals who are used to performing a back squat in a fatigued state might make it harder to indicate a difference in variables due to the muscle memory developed over their time training fatigued. Lastly, future studies should compare different volumes of SMR. If an ideal time or pressure of SMR can be identified, it would become easier to use and prescribe to increase performance variables.
In conclusion, the findings of this study indicate SMR did not improve knee ROM during a back squat, and perceived recovery following a heavy resistance training session. Furthermore, mean and peak muscle activity of the GM and RF did not differ between the SMR and dynamic warmup protocol.
Figure 1.
Mean muscle activation during a 10-rep back squat at 70% of the participants estimated 1RM. RF = Rectus Femoris GM = Gluteus Maximus
Figure 2.
Peak muscle activation during a 10-rep back squat at 70% of the participants estimated 1RM. RF = Rectus Femoris GM = Gluteus Maximus
REFERENCES
- 1.Ball N, Scurr J. Electromyography normalization methods for high-velocity muscle actions: review and recommendations. J App Biomech. 2013;29(5):600–608. doi: 10.1123/jab.29.5.600. [DOI] [PubMed] [Google Scholar]
- 2.Bradbury-Squires DJ, Noftall JC, Sullivan KM, Behm DG, Power KE, Button DC. Roller-massager application to the quadriceps and knee-joint range of motion and neuromuscular efficiency during a lunge. J Athl Train. 2015;50(2):133–140. doi: 10.4085/1062-6050-49.5.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Couture G, Karlik D, Glass SC, Hatzel BM. The effect of foam rolling duration on hamstring range of motion. Open Orthop J. 2015;9:450–455. doi: 10.2174/1874325001509010450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cutter NC, Kevorkian CG. Handbook of manual muscle testing. 1st ed. New York, NY: McGraw-Hill; 1999. [Google Scholar]
- 5.De Luca CJ. The use of surface electromyography in biomechanics. J App Biomech. 1997;13(2):135–163. [Google Scholar]
- 6.Duehring MD, Feldman CR, Ebben WP. Strength and conditioning practices of United States high school strength and conditioning coaches. J Strength Cond Res. 2009;23(8):2188–2203. doi: 10.1519/JSC.0b013e3181bac62d. [DOI] [PubMed] [Google Scholar]
- 7.Fleckenstein J, Wilke J, Vogt L, Banzer W. Preventive and regenerative foam rolling are equally effective in reducing fatigue-related impairments of muscle function following exercise. J Sports Sci Med. 2017;16(4):474–479. [PMC free article] [PubMed] [Google Scholar]
- 8.Haff GG, Triplett NT, editors. Essentials of strength training and conditioning. 4th ed. Champaign, IL: Human Kinetics; 2015. [Google Scholar]
- 9.Hermens HJ, Freriks B, Merletti R, Stegeman D, Blok J, Rau G, Disselhorst-Klug C, Hägg G. Roessingh Research and Development. 2000. European recommendations for surface electromyography: results of the SENIAM project. [Google Scholar]
- 10.Isear JJ, Erickson JC, Worrell TW. EMG analysis of lower extremity muscle recruitment patterns during an unloaded squat. Med Sci Sports Exerc. 1997;29(4):532–539. doi: 10.1097/00005768-199704000-00016. [DOI] [PubMed] [Google Scholar]
- 11.Jay K, Sundstrup E, Søndergaard SD, Behm D, Brandt M, Særvoll CA, Jakobsen MD, Andersen LL. Specific and cross over effects of massage for muscle soreness: randomized controlled trial. Int J Sports Phys Ther. 2014;9(1):82–91. [PMC free article] [PubMed] [Google Scholar]
- 12.Korak JA, Paquette MR, Fuller DK, Caputo JL, Coons JM. Muscle Activation Patterns of Lower-Body Musculature Among 3 Traditional Lower-Body Exercises in Trained Women. J Strength Cond Res. 2018;32(10):2770–2775. doi: 10.1519/JSC.0000000000002513. [DOI] [PubMed] [Google Scholar]
- 13.Laurent CM, Green JM, Bishop PA, Sjökvist J, Schumacker RE, Richardson MT, Curtner-Smith M. A practical approach to monitoring recovery: development of a perceived recovery status scale. J Strength Cond Res. 2011;25(3):620–628. doi: 10.1519/JSC.0b013e3181c69ec6. [DOI] [PubMed] [Google Scholar]
- 14.MacDonald GZ, Penney MD, Mullaley ME, Cuconato AL, Drake CD, Behm DG, Button DC. An acute bout of self-myofascial release increases range of motion without a subsequent decrease in muscle activation or force. J Strength Cond Res. 2013;27(3):812–821. doi: 10.1519/JSC.0b013e31825c2bc1. [DOI] [PubMed] [Google Scholar]
- 15.Monteiro ER, Škarabot J, Vigotsky AD, Brown AF, Gomes TM, Novaes JD. Acute effects of different self-massage volumes on the FMS™ overhead deep squat performance. Int J Sports Phys Ther. 2017;12(1):94–104. [PMC free article] [PubMed] [Google Scholar]
- 16.Monteiro ER, Vigotsky AD, Novaes JD, Škarabot J. Acute effects of different anterior thigh self-massage on hip range-of-motion in trained men. Int J Sports Phys Ther. 2018;13(1):104–113. [PMC free article] [PubMed] [Google Scholar]
- 17.Myer GD, Kushner AM, Brent JL, Schoenfeld BJ, Hugentobler J, Lloyd RS, Vermeil A, Chu DA, Harbin J, McGill SM. The back squat: a proposed assessment of functional deficits and technical factors that limit performance. Strength Cond J. 2014;36(6):4–27. doi: 10.1519/SSC.0000000000000103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Phillips J, Diggin D, King DL, Sforzo GA. Effect of varying self-myofascial release duration on subsequent athletic performance. J Strength Cond Res. 2018 doi: 10.1519/JSC.0000000000002751. (Epub doi: 10.1519) [DOI] [PubMed] [Google Scholar]
- 19.Sağiroğlu İ, Kurt C, Pekünlü E, Özsu İ. Residual effects of static stretching and self-myofascial-release exercises on flexibility and lower body explosive strength in well-trained combat athletes. Isokinet Exerc Sci. 2017;25(2):135–141. [Google Scholar]
- 20.Yavuz H, Erdağ D, Amca AM, Aritan S. Kinematic and EMG activities during front and back squat variations in maximum loads. J Sports Sci. 2015;33:1058–1066. doi: 10.1080/02640414.2014.984240. [DOI] [PubMed] [Google Scholar]