Abstract
Objective:
Two decades of empirical research suggest that changes in symptoms are not linear, and many patients gain much of their symptom reduction in one between-sessions interval. Theoretically, such gains are expected to be manifested in the working alliance as well, following a rupture session; however, no study to date has directly examined between-sessions sudden gains in the alliance. In the present study we examined whether ruptures predict subsequent sudden gains in the alliance, which in turn show an effect on outcome that is specific to the treatment in which the alliance is conceptualized as an active mechanism of change.
Method:
In a sample of 241 patient-therapist dyads, patients received either brief relational therapy (BRT), in which the alliance is conceptualized as an active mechanism of change, or cognitive behavioral therapy (CBT), in which it is not. We examined whether patient and therapist reports of ruptures predicted sudden gains in alliance in the subsequent session, and whether early sudden gains in alliance were significantly associated with treatment outcome in BRT vs. CBT.
Results:
Rupture sessions, as reported by therapists but not by patients, predicted a sudden gain in both patient and therapist-reported alliance in the subsequent session. Findings revealed a moderating effect of treatment condition on the association between sudden gains and treatment outcome, in which gains in alliance were associated with better treatment outcome in BRT than in CBT.
Conclusions:
The findings support the potential role of gains in alliance as a specific mechanism of change in BRT vs. CBT.
Keywords: alliance, brief relational therapy, alliance-focused treatment, sudden gain, mechanisms of change
A revolution in psychotherapy research is underway, made possible by careful examination of the process of therapeutic change occurring from one session to the next (Hayes, Laurenceau, Feldman, Strauss, & Cardaciotto, 2007). For many years, studies focused on the change from pre- to post-treatment, but cumulative results over decades of research revealed the richness to be found in the details of the session-to-session process of change. Zooming in on the process of change that unfolds in the course of treatment has revealed phenomena that were formerly hidden from the observation of scientists. Nonlinear patterns of change in symptoms from session to session, such as early rapid response (Ilardi & Craighead, 1994), depression spike (Hayes et al., 2007), and sudden gains (Tang & DeRubeis, 1999) became the focus of empirical investigations, and were found to account for a large portion of total improvement in treatment. Yet, corresponding progress in mechanisms of change continues to lag behind, although such progress seems most natural in light of the empirical literature on non-linear patterns of symptom change. Theoretical literature on some mechanisms of change, such as the working alliance, actually explicitly discusses the importance of focusing on non-linear patterns of development. Contemporary theoretical conceptualizations of the working alliance focus on how ruptures in treatment can evolve, through their successful resolution, into a strengthened alliance (Safran & Muran, 2000). Such improvement in the alliance is conceived as therapeutic in itself and, in treatments like brief relational therapy (BRT), as the direct cause of symptomatic change. In the present study, we adopt the sudden gain methodology, as proposed by Tang and DeRubeis (1999) and as used in numerous studies since then, to investigate such gains in the alliance.
The literature on sudden gains originated in the finding of Tang and DeRubeis (1999) that more than half the total improvement in symptoms of more than a third of the patients was concentrated in one between-sessions interval. Many of these changes were found to be large in magnitude and long-lasting, leading the investigators to suggest that sudden gains in symptoms captured an important process in the patients’ therapeutic change. Since then, numerous studies have implemented the sudden gains methodology to examine the process of changes in symptoms across treatment. These studies revolved around two critical questions: (a) What happened in the session preceding the gain in symptoms (the pre-gain session), which may have increased the chances of a gain? and (b) What are the consequences of the gain in symptoms for treatment outcome?
Studies focusing on the first question suggest that sudden gains in symptoms are the result of theory-specific mechanisms of change (Andrusyna, Luborsky, Pham, & Tang, 2006). For example, sudden gains have been found to be the result of adaptive changes in depression-related core beliefs and schemas in pre-gain sessions in CBT (Tang & DeRubeis, 1999), and of increased insight into maladaptive interpersonal patterns in supportive-expressive treatment (Andrusyna et al., 2006). These changes in core theory-specific mechanisms of change appeared to be the result of therapists’ adequate case conceptualization (Abel, Hayes, Henley, & Kuyken, 2016) and use of therapeutic techniques (Andrusyna et al., 2006).
Studies focusing on the second question reveal that sudden gains in symptoms signify a positive development in treatment resulting in good outcomes even when they occur early in treatment. Sudden gains in symptoms were found not only to predict better outcomes at the end of treatment, but patients who experienced sudden gains in symptoms were significantly less depressed 18 months post-therapy than were those who did not experience sudden gains (Abel et al., 2016; Aderka, Nickerson, Bøe, & Hofmann, 2012; Tang & DeRubeis, 2005; Tang & DeRubeis, 1999). The effects of sudden gains in symptoms on outcome were especially evident in the context of a strong alliance (Wucherpfennig, Rubel, Hofmann, & Lutz, 2017).
Embedded in the perception that change in symptoms may develop non-linearly is the assumption that the mechanisms responsible for such changes are also developing non-linearly. In a previous study, sudden changes within-session were investigated, and were found among 58% of the patients receiving CBT for panic disorder (Weiss, Kivity & Huppert, 2014). These sudden within-session gains were moderately, though not significantly, associated with treatment outcome. The present work is the first to implement the sudden gains methodology to investigate between-sessions changes in process mechanisms of change, using the case of the working alliance as a theoretical framework. The working alliance is commonly defined as the emotional bond established in the therapeutic dyad and the agreement between patient and therapist concerning therapy goals and the tasks necessary to achieve them (Bordin, 1979). The theoretical literature on alliance explicitly discusses the importance of focusing on non-linear patterns of development (Eubanks-Carter, Gorman, & Muran, 2012), though the empirical literature has not yet explored this topic exhaustively. Contemporary theoretical conceptualizations of the working alliance focus on how the process of addressing and resolving ruptures, or problems in the alliance, can lead to a strengthened alliance (Safran & Muran, 2000). Such improvement in the alliance is conceived as therapeutic in itself and, in treatments like brief relational therapy, as the direct cause of symptomatic change.
Recent advances in trial design, notably, session-by-session measurement of the alliance and the use of advanced statistical methods, have made it possible to separate two components of the alliance, trait-like and state-like, each theorized to play a distinct role in treatment (Zilcha-Mano, 2016). The trait-like component of alliance refers to the way in which trait-like characteristics of the patients (and of their therapists), such as their ability to form satisfying relationships with others, affect their ability to create, in treatment, the environment required to conduct any effective treatment. This component is not the one that is theorized to make alliance a mechanism of change in treatment, but rather it may act as a non-specific factor, which is to a large extent a product of the patient’s (and therapist’s) trait-like characteristics. By contrast, the state-like component of alliance refers to alliance as a mechanism of change in itself, with changes in alliance being perceived as the cause of subsequent symptomatic change (Zilcha-Mano, 2017)1. The role of alliance as a mechanism of change in itself is best conceptualized in the theoretical model proposed by Safran and Muran (2000), which has received accumulating empirical support over the years (Muran, 2017; for a meta-analysis, see Eubanks, Safran, & Muran, 2018). This empirically-tested model describes how therapeutic alliance is negotiated through a rupture and repair process, during which therapist and patient collaborate in efforts to improve the alliance, creating state-like changes in it. As the result of such work, gains in alliance are expected, signifying the successful resolution of the ruptures. This process is perceived as the core mechanism of change in BRT, where gains in the alliance signify the successful resolution of ruptures.
The same two questions that advanced the empirical examination of sudden gains in the study of symptomatic change are of great importance in implementing the methodology of sudden gains in the study of the alliance: (a) whether rupture sessions predict subsequent alliance sudden gains. As it is in the literature on sudden gains in symptoms, sudden gains in alliance are not expected to be random but to follow a rupture in the pre-gain session. This is consistent with theoretical conceptualizations of improvements in alliance as products of successful resolution of alliance ruptures (Safran & Muran, 2000); and (b) whether sudden gains in alliance are associated with better treatment outcome. As it is in the literature on sudden gains in symptoms, sudden gains in the alliance are expected to be associated with better treatment outcome. Consistent with the empirically-tested model of rupture resolution processes (Safran & Muran, 1996, 2000), sudden gains in alliance are expected to be associated with better treatment outcome, specifically in treatment where gains in the alliance are expected to be a core mechanism of change (BRT, as opposed to CBT).
In the present study, we address these two questions in a sample of patients receiving either BRT or CBT (Muran et al., 2009; Safran, Muran, Samstag, & Winston, 2005), in which alliance was previously found to be significantly associated with subsequent session outcome (Zilcha-Mano, Muran, Eubanks, Safran, & Winston, 2018; Zilcha-Mano et al., 2016). We examine (a) whether sessions characterized by rupture predict subsequent sudden gains in alliance, and (b) whether sudden gains in alliance are associated with treatment outcome in BRT vs. CBT. In this study, treatment outcome is based on patient rating pre- and post-treatment. Thus, we were able to examine a dyadic effect, in which the perspective of one partner in the dyad serves as the predictor of the perspective of the other partner on outcome (Kivlighan, 2007; Kivlighan, Gelso, Ain, Hummel, & Markin, 2015; Zilcha-Mano et al., 2016): the ability of sudden gains as indicated based on the therapist-rated alliance, to predict patient-rated treatment outcome. We also examined a same-informant effect of the ability of alliance sudden gains, as indicated based on the patient-rated alliance, to predict patient-rated treatment outcome.
Method
Participants
Data of 241 patients, who were assigned to either CBT or BRT were included. The study was approved by the IRB of the relevant institution. Patients were excluded from the study for not meeting the following inclusion criteria: (a) 18–65 years old and (b) English fluency; or for meeting one of the following exclusion criteria: (a) evidence of organic brain syndrome or mental retardation, (b) evidence of psychosis or need for hospitalization, (c) diagnosis of severe major depression or bipolar disorder, (d) evidence of active substance abuse, (f) evidence of active Axis III medical diagnosis, (g) history of violent behavior or impulse control problems, and (h) evidence of active suicidal behavior.
Mean patient age was 42 (SD = 13.54), and 156 participants (64.7%) were female; 74.3% were white, 6.7% black, 5.8% Hispanic, and 13.2% chose the “Other” category or did not answer this question; 58.9% were single, 19.5% married or remarried, 14.5% divorced or separated, and 1.7% widowed; 4% had some high school education, 1.2% were high school graduates, 14.9% had some college education, 38.6% were college graduates, 7% had some post-graduate education, and 29.9% had graduate degrees. At intake, 49.8% met criteria for a primary diagnosis of mood disorder, 21.6% for anxiety disorders, and 4.6% for adjustment disorder. Overall, 46.1% met criteria for multiple Axis I diagnoses and 43.66% had a primary Axis-II personality disorder. The most frequent personality disorders were avoidant (12%), obsessive-compulsive (10%), and not otherwise specified (20.7%).
Treatments and therapists
Two treatment models were used: CBT, which is a schema-focused model that implements strategies such as self-monitoring, cognitive restructuring, behavioral exercises, and experimentation to affect change in symptomatology and belief systems (N = 108, Turner & Muran, 1992), and BRT, also described as an alliance-focused treatment (Safran & Muran, 2000), which is based on an integration of principles derived from intersubjective theories and research on interpersonal process, emotion communication, and rupture resolution and involves ongoing tracking and exploring of patient and therapist interactions (N = 133, Safran & Muran, 2000). Both were manualized and designed to treat patients in a fixed, 30-session, one-session-per-week format. Treatment fidelity, tested using the observer-rated Beth Israel Fidelity Scale (BIFS; Patton et al., 1998; Santangelo et al., 1994), was high for both treatment conditions (Zilcha-Mano et al., 2016). One hundred and eighty-one therapists participated in the study. The mean number of patients treated by each therapist in the current study was 1.32 (SD = 0.59, range: 1–4).
Measures
Working alliance.
We used patient- and therapist-reported alliance to calculate sudden gains. The alliance was assessed after each session using the 12-item version of the Working Alliance Inventory (WAI; Tracey & Kokotovic, 1989). Items were rated on a 7-point Likert scale, ranging from 1 (never) to 7 (always). In the present study, means and standard deviations were as follows: patient- rated alliance level (Mean = 5.82, SD = .96) and therapist-rated alliance level (Mean = 5.13, SD = .87). The internal reliability range across time points was .88-.94 for patients and .83-.93 for therapists. Data from this sample have previously demonstrated the ability of alliance to predict subsequent session outcome (Zilcha-Mano, Muran, Eubanks, Safran, & Winston, 2018; Zilcha-Mano et al., 2016).
Alliance rupture.
We used the single item on rupture from the Post-Session Questionnaire (Muran, Safran, Samstag, & Winston, 1992; Muran et al., 2005, 2009) to measure ruptures in the alliance after each session, for 30 weekly sessions. The one item was answered by both patients (“Did you experience any tension or problem, any misunderstanding, conflict, or disagreement in your relationship with your therapist during the session?”) and therapists (“Did you experience any tension or problem, any misunderstanding, conflict or disagreement, in your relationship with your patient during the session?”) on a Likert scale, ranging from 1 (not at all) to 5 (constantly). In the present study, patient and therapist ratings of ruptures ranged between 1 and 5. Means and standard deviations were as follows: patient-rated ruptures (Mean = 1.35, SD = .80) and therapist-rated ruptures (Mean = 1.59, SD = .92). The use of alliance ruptures as a continuous measure is in line with contemporary theories of alliance ruptures and repair (Eubanks, Muran, & Safran, 2015; Safran & Muran, 2000), and has demonstrated its utility in previous studies (Muran et al., 2009; Tufekcioglu, Muran, Safran, & Winston, 2013).
Treatment outcome and session outcome.
Treatment outcome was assessed based on patient self-report using the Global Severity Index (GSI) of the Symptom Checklist-90-Revised (SCL-90-R: Derogatis & Melisaratos, 1983). We assessed the SCL at two time points: pre- and post-treatment. The internal reliability of the GSI was .86 pre-treatment and .84 post-treatment. Session outcome was assessed after each session based on patient report on the following item: “To what extent are your presenting problems resolved?” (Muran, Safran, Samstag, & Winston, 1992).
Overview of statistical analyses
Identifying sudden gains.
Based on previous literature on alliance, graph inspection following the guidance as it appears in Tang and DeRubeis (1999), and the calculation of clinical significance change, we adjusted the definition of sudden gains in symptoms which was suggested by Tang and DeRubeis (1999), for use with an alliance measure as follows:
Absolute magnitude: gain was at least 0.75 points on the mean WAI score, calculated based on the measure of clinical significance index,2 WAIn – WAIn+1 >= 0.75.
Relative magnitude: gain represented at least 15% of the WAI score of the pre-gain session, WAIn+1 – WAIn >= .15WAIn.3
Relative to alliance fluctuation: the mean difference between the WAI scores of the three sessions before and after the gain was at least 2.78 times greater than the pooled standard deviations of the WAI scores of these two groups of sessions. In other words, the values of the 3 sessions before and 3 sessions after the gain are derived from different distributions. This is comparable to a t-test of the means of the 3 WAI scores before and after the gain. This ensures that the focus is on gains that have a lasting effect, rather than merely on a “get back on track” effect.
Ruptures as predictors of subsequent sudden gains
To examine whether ruptures predicted subsequent sudden gains as identified based on patient- and therapist-reported alliance, we conducted multilevel logistic regression analyses with observations nested within patients, using the SAS PROC GLIMMIX procedure. Adding a third level of analysis (therapists) did not change any of the results. We used patient and therapist reports on ruptures as predictors of gains at the next session, based on both patients’ and therapists’ perspectives. We used a binary variable of the advent of sudden gain at the subsequent session as the dependent variable. In all analyses we controlled for the time in treatment when the gain session occurred.
The moderating effect of treatment condition on the association between sudden gains in alliance early in treatment and treatment outcome
We were interested in examining whether sudden gains in alliance were significantly associated with better treatment outcome in BRT vs CBT. To examine the moderating effect of treatment condition on the association between sudden gains and treatment outcome from pre- to post-treatment, we used linear regression. We repeated our analyses twice, once for gains based on therapist perspective and once based on patient perspective. To reduce the overlap between the time when the predictor (alliance sudden gains) was assessed and the time when treatment outcome was assessed (only at pre- and post-treatment) we took the following steps: (a) we focused only on early sudden gains in alliance, which occur in the first third of treatment (first 10 sessions), and (b) we re-ran the analyses, controlling for early change in session outcome during the first third of treatment (Sessions 1–10). We used that as a proxy for the creation of a temporal relationship between the predictor and treatment outcome.
The equation was as follows:
where error~ N(0,s2), SG = sudden gains.
Results
Preliminary analyses
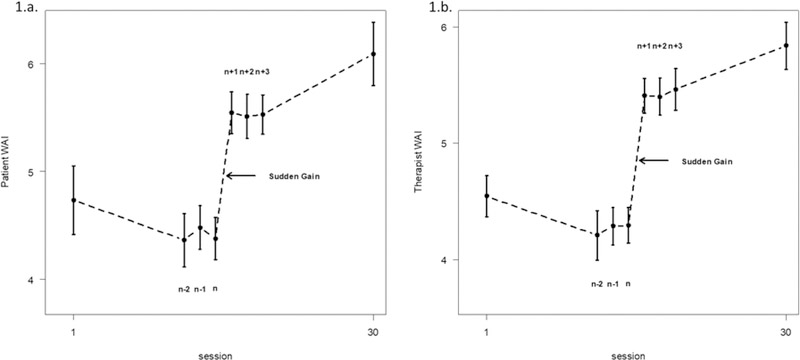
The correlations between patients’ and therapists’ reported ruptures as well as patients’ and therapists’ alliance at the same sessions and the next one ranged between −.18 and −.38. Figure 1 describes the average alliance of three sessions before and after a sudden gain. Of the dyads, 13.7% showed early sudden gains, as indicated by patient-reported alliance, and 14.5% showed early sudden gains as indicated by therapist-reported alliance. No dyad had more than one sudden gain during the first 10 sessions. Focusing on therapist-reported alliance, there were no significant differences in early sudden gains between treatment conditions (χ2(1) = 2.97, p = .08; 18% vs. 10.2% for BRT and CBT, respectively). Focusing on patient-reported alliance, there were significantly more early sudden gains in BRT than in CBT (χ2(1) = 4.75, p = .02; 18% vs. 8.3% for BRT and CBT, respectively). The estimated variance of the therapist’s random effect in the two-level model predicting treatment outcome was not significant (S2 = 0.02, p = 0.35, ICC = .08).
Figure 1.
Average sudden gain in alliance at the sample mean level, based on patients’ alliance self-report (1.a.) and therapists’ alliance self-report (1.b.). Similarly to the original figure by Tang and DeRubeis (1999), the working alliance inventory (WAI) scores shown for sessions n-2, n-1, n, n+1,n+2, and n+3 are the means (± SE) of the corresponding sessions of the patients showing sudden gains in alliance. Adapted from “Sudden gains and critical sessions in cognitive-behavioral therapy for depression,” by Tang, T. Z., & DeRubeis, R. J., 1999, Journal of Consulting and Clinical Psychology, 67.
Ruptures as predictors of subsequent sudden gains
The analyses revealed that therapists’ reports on ruptures at the pre-gain session significantly predicted both their own (RO = 1.33, B = .28, SE = .12, t(3216) = 2.24, p = .02) and their patients’ (RO = 1.50, B = .40, SE = .15, t(2967) = 2.55, p = .01) report on alliance gains at the subsequent session. The findings suggest that greater ruptures were associated with greater chances for subsequent sudden gains. But patients’ reports on ruptures at the pre-gain session did not predict either their own (RO = 1.20, B = .18, SE = .18, t(2976) = 1.03, p = .30) or their therapists’ (RO = 1.26, B = .23, SE = .13, t(2648) = 1.77, p = .07) report on gains at the subsequent session.4
The moderating effect of treatment condition on the association between sudden gains and treatment outcome
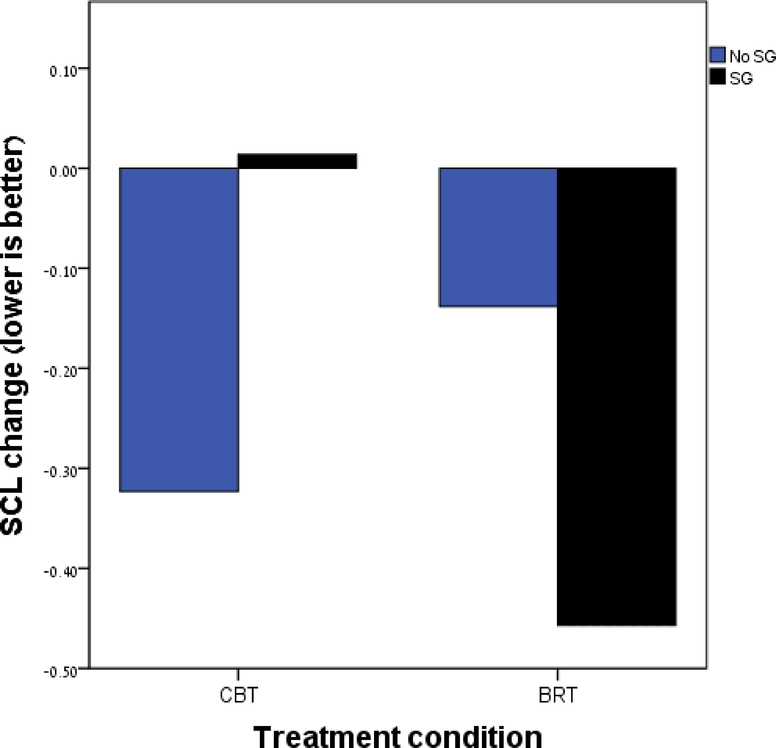
The model examining whether treatment condition moderates the association between sudden gains in alliance, as identified by therapist-reported WAI, and treatment outcome, yielded a significant interaction, B = 0.66, SE = .23, t =2.82, p = .005 (Figure 2). The estimates of the coefficients of the moderation model suggest that early sudden gains were associated with better treatment outcome in BRT (B = −0.32, SE = .15, t = −2.08, p = .03) than in CBT (B = 0.33, SE = .17, t =1.92, p = .06). The explained R2 of the model fit was 7.67%, and the unique contribution of the interaction was 7%. Repeating the analyses controlling for early change in session outcome from the first to the tenth week of treatment resulted in replication of the significant interaction (B = 0.56, SE = .26, t =2.19, p = .03), with stronger association between sudden gains and outcome in BRT than in CBT. The model examining whether treatment condition moderates the association between sudden gains, as identified by patient-reported WAI, and treatment outcome, as reported by the patient, resulted in a non-significant interaction, B = −0.30, SE = .27, t =−1.08, p = .28.5
Figure 2.
The mean of patient-rated treatment outcome stratified by sudden gains (SG) based on therapist-rated alliance, for each treatment condition (brief relational therapy and cognitive behavioral therapy).
Discussion
The concept of sudden gains in symptoms, and the methodology proposed for their assessment, have yielded a prolific body of research. As demonstrated repeatedly in these studies, for many of the patients, treatment does not follow a linear, gradual trajectory. The process of change is more complex and rich, with much of the change occurring for many patients in a single between-sessions interval. To our knowledge, this is the first study to test the applicability of the between-sessions sudden gain methodology to the development of mechanisms of change. The findings suggest that sudden gains in alliance play an important role in treatment, indicating specificity to a treatment in which alliance is perceived to act as a mechanism of change.
Our first question was whether ruptures in the pre-gain session can predict sudden gains in alliance at the next session. The findings suggest that sudden gains in alliance are not random fluctuations but tend to follow a rupture, as perceived by the therapist at the pre-gain session. Similar to the findings regarding sudden gains in symptoms, clear theory-driven predecessors can be detected in the pre-gain sessions that significantly predict the sudden gains in alliance in the subsequent session. Although awaiting a deep investigation into resolution process at the pre-gain or the gain sessions, the present findings suggest that ruptures are crucial for substantial subsequent gains in alliance (although they may not be the only pathway for such gains, Castonguay & Hill, 2012). These findings are consistent with Safran and Muran’s (1996, 2000) conceptualizations of improvements in the alliance as products of successful resolution of ruptures. The findings also support previous arguments regarding the essential role of therapists’ awareness in treatment (Lambert, 2015): therapists’, but not patients’ awareness of ruptures predicted subsequent gains in alliance, as indicated by both patients’ and therapists’ reports.
Our second question was whether sudden gains in alliance are associated with better outcome. We found an association between sudden gains in alliance and outcome, which showed specificity to BRT vs. CBT. This finding is consistent with Safran and Muran’s (1996, 2000) stage-process model of alliance rupture and resolution processes. According to this model, gains in the alliance, which are expected to be a manifestation of successfully resolved ruptures, represent a meaningful change process in BRT. This process may have positive effects on the ability of the individual to negotiate interpersonal needs and take part in a dialogue regarding such needs and therefore result in better treatment outcome. This finding is in some respects consistent with Weiss et al. (2014) which also found no significant effect (though moderate in size) of sudden gains in alliance on outcome in a CBT treatment. However, it is important to note that Weiss et al. (2014) used a different methodology than the between-sessions sudden gains methodology (Tang & DeRubeis, 1999), and tested within-session changes.
The present study, which is the first to implement the between-sessions sudden gains methodology within the theoretical framework of alliance rupture and repair, has the potential to make important contributions to both the literature using the sudden gains methodology, and the literature on the alliance rupture and repair model. On the methodological side, the study supports the potential adequacy of the sudden gains methodology for identifying not only non-linear changes in symptoms but also non-linear changes in mechanisms of change. These findings provide additional validity to the accumulating literature on sudden gains that until now used mostly the same measure to assess sudden gains and treatment outcome, for example, calculating sudden gains based on the Back Depression Inventory (BDI) to predict treatment outcome based on the BDI. The present study tested whether this association still holds when using not only different measures, but even different constructs: a mechanism of change and outcome. In further support of the literature utilizing the methodology of sudden gains, we also used two different perspectives, of the patient and of the therapist, to test a dyadic effect on treatment outcome, a method that is less susceptible to shared variance. Thus, the present study confirms the robustness of the sudden gain methodology.
The study also makes a novel contribution to the field of alliance research. A highly debated issue in the literature on the alliance is whether alliance is a common factor across treatments or a specific mechanism of change (Barber, 2009). One strategy for answering this question is to investigate whether the effect of gains in the alliance on outcome shows specificity to treatment where it is theorized to act as a mechanism of change (such as BRT), compared to treatment where it is not (such as CBT). The present study demonstrates that the association between sudden gains in the alliance and treatment outcome is indeed significantly distinct in the two treatments, and the effect was stronger in BRT. The present finding suggests that state-like changes in the alliance, as manifested in sudden gains, may play different roles and have differential effects on outcome in different treatment conditions. Although meta-analyses failed to support theory-driven predictions about different roles that alliance may fulfill in different treatment (Flückiger, Del Re, Wampold, & Horvath, 2018; Horvath, Del Re, Flückiger, & Symonds, 2011), several studies with patient-level data that were able to look more closely on such differences do show some support for different roles of alliance (Arnow, Steidtmann et al., 2013; Lorenzo-Luaces, Driessen et al., 2017; Snippe, Fleer et al., 2015).
Interestingly, although sudden gains, as indicated by therapist-reported alliance, were a significant predictor of patients-reported outcome in BRT vs. CBT, this was not the case for gains based on patient-reported alliance. Furthermore, it was therapist-reported but not patient-reported rupture that predicted a sudden gain in both patient- and therapist-reported alliance in the subsequent session. These findings may further support the importance of therapist’s awareness for the success of treatment (Lambert, 2015). Therapists’ awareness of ruptures in alliance and their ability to address them may strengthen alliance and improve outcome. These results are consistent with empirical findings on routine outcome monitoring, which demonstrate that alerting therapists to patients’ processes of change is associated with improved outcome for not-on-track patients (Lambert, 2015). Therapists’ awareness of problems and gains in the treatment is essential, at least in treatment where alliance serves as an active ingredient. A thorough investigation on this explanation can shed light on the mechanism underlying previous findings pointing to the importance of therapists adopting a watchful attitude toward changes in the alliance (Chen, Atzil-Slonim, Bar-Kalifa, Hasson-Ohayon, & Refaeli, 2018; Rubel, Bar-Kalifa, Atzil-Slonim, Schmidt, & Lutz, 2018).
Another intriguing finding of the present study is a marginally significant association between sudden gains, as identified by therapist-reported WAI, and treatment outcome—sudden gains in alliance being marginally associated with poorer outcome in CBT. This finding should be interpreted with caution because it is only marginally significant. One potential post hoc explanation concerns the different training the therapists received in the two conditions. The therapists in the BRT condition received training in identifying changes in alliance and building on such changes to create broader changes in the patients’ interpersonal skills. For example, given that BRT therapists are trained to detect ruptures, including subtle withdrawal ruptures in which the patient is overly deferential, they may be better equipped to identify a “pseudo alliance” in which the patient is trying to appease the therapist but does not genuinely agree with the tasks and goals of treatment (Muran et al., 2018). The therapists in the CBT condition did not receive such training. Therefore, they may differ in their ability to accurately detect authentic gains in the alliance (as opposed to pseudo–gains, such as when the patient may react in a deferential and appeasing way after a rupture). CBT therapists may also be less skilled specifically in the process of generalizing the gains in alliance into a broader change in outcome, even if the gains are authentic. According to this post hoc explanation, although the alliance is associated with treatment outcome across theoretical orientations (Flückiger, Del Re, Wampold, & Horvath, 2018), the benefits of the specific patterns of rupture resolution processes may be especially evident in a treatment in which the therapists are specifically trained to make such processes beneficial for therapeutic change. This potential post hoc explanation suggests important directions for future research.
We have little reason to assume that the sudden gains in alliance observed in the present study are mere reflections of sudden gains in symptoms, though this possibility (which we were not able to test using our present data) deserves direct examination. First, previous findings on the present data suggest that session-to-session alliance was not just a product of session progress, but rather a significant predictor of it (Zilcha-Mano et al., 2016). This finding is consistent with other studies showing that strengthening in alliance (Falkenström, Granström, & Holmqvist, 2013; Zilcha-Mano, 2016) and also ruptures in alliance (Larsson, Falkenström, Andersson, & Holmqvist, 2018; Rubel, Zilcha-Mano, Feils-Klaus, & Lutz, 2018) are not merely the by-products of changes in symptoms. Second, in the present study sudden gains in alliance were found to be significantly predicted by alliance ruptures in the previous session. It is less likely that at the very same session of alliance rupture there was also a sudden gain in symptoms, if one sees changes in alliance as the result of sudden gains in symptoms. Third, given the fact that no significant difference in outcome were found between the treatments, and that sudden gains in symptoms were found to be consistent predictors of treatment outcome (Aderka et al., 2012), it is less likely that the BRT treatment showed more sudden gains in symptoms, but rather that sudden gains in alliance are unique mechanisms that explain variability in treatment outcome in BRT compared to CBT.
If replicated in future studies, the present findings provide important support for the therapeutic process theorized and previously tested by Safran and Muran (1996, 2000), which serves as the basis for BRT (Muran et al., 2018), and according to which successful resolution of alliance ruptures, as manifested in strengthening of the alliance, may bring about therapeutic change. Tracking and repairing alliance ruptures and engaging with the patient in meta-communication about this process are expected to increase the patient’s awareness of what is transpiring in the therapeutic relationship. This increased awareness may help the patient, in collaboration with the therapist, to identify and change habitual, self-defeating relational patterns that may contribute to their interpersonal difficulties. The CBT treatment is expected to work through a conceptually different process of change, such as a schema change resulting from implementing such techniques as cognitive restructuring, self-monitoring, behavioral exercises, and experimentation (Turner & Muran, 1992).
The implications of these findings should be considered in light of the limitations of the study. The most important limitation of the present study is the assessment of the treatment outcome, SCL, at only two time points in treatment and only from the patient’s perspective. Thus, we can only approach a correct temporal relationship between sudden gains and treatment outcome, but cannot unequivocally establish such a relationship. To compensate for this limitation, we focused only on early sudden gains and controlled for early changes in session outcome. This solution, of course, has its own limitations, but it enabled us to approximate temporal precedence. Future studies should use session by session treatment outcome, ideally from both patients’ and therapists’ perspectives. Additionally, to capture the whole process of rupture and repair, assessments of repairs, via self-report (Muran et al., 1992) and external observer rating scales (Eubanks, Muran, & Safran, 2015; Safran & Muran, 1996) should be used to investigate whether the effect of rupture on outcome is mediated by resolution processes at the pre-gain or the gain session. This would also make possible the next step in elucidating the effects of therapists’ conscious experience and awareness of ruptures. Finally, the definitions used to identify sudden gains in the present study, derived from the literature on sudden gains and modified to fit the alliance measure, should be further tested and validated in future studies.
To the best of our knowledge, this is the first study to use the methodology of between-sessions sudden gains to investigate changes in the alliance over the course of treatment, and to examine their associations with treatment outcome. The study makes two main important contributions: (a) To the literature on sudden gains methodology, it provides additional validation, demonstrating its robustness even when the sudden gains and outcome are distinct constructs, tested on information supplied by different informants. (b) To the literature on alliance, the study makes a unique contribution to one of the most debated issues in the field of alliance research: the association between gains in alliance and treatment outcome showed specificity to the treatment that theorizes changes in the alliance as a mechanism of change. It is important for future studies to utilize promising frameworks for investigating non-linear change, such as early rapid response (Ilardi & Craighead, 1994), depression spike (Hayes et al., 2007), and sudden gains (Tang & DeRubeis, 1999), to study other theory-specific and common mechanisms of change.
Supplementary Material
Public health significance:
The findings suggest that for many patients much of the improvement in alliance occurs in a single between-sessions interval, following a session in which the therapist reported a rupture. Such alliance gains may show a specific association with treatment outcome in a treatment focusing on the alliance as a core mechanism of change. These findings are consistent with theoretical conceptualizations of gains in alliance as products of the therapists identifying and resolving ruptures, and attest to the important role such a rupture resolution process is expected to play in Brief Relational Therapy.
Acknowledgments
The research was supported by a grant from the National Institute for Mental Health MH071768 (Principal Investigator: J. Christopher Muran).
Footnotes
For a discussion of the potential role of within-patient alliance as an active ingredient in treatment and the potential role of between-patients alliance as a non-specific factor, see Curran and Bauer (2011), and Zilcha-Mano (2016, 2017, 2018).
We computed clinical significance using a mean internal consistency of .88. First session SD was .74. The standard error of measurement for the scale produced .26 (standard error of measurement , and the standard error of the difference between two administrations of the measure was calculated as × .26, or .37. Next, we used 2 times the standard error of the difference as an index of reliable change (e.g., Jacobson & Truax, 1991). Consequently, we identified improvement of at least 0.75 points on the WAI as a gain. This was calculated based on the patient-rated alliance because this information was available only for patients’ rating, and some of the details were missing in the literature regarding the therapist-rated alliance. Though having its own shortcomings, using the same criterion for both patients and therapists enabled us to make the prediction of outcome based on sudden gains comparable between patients and therapists.
The original criterion of 25% relative change is based on the BDI, which is an outcome measure. The BDI was designed to be highly sensitive to changes in symptoms, and it is expected to show a meaningful reduction over the course of treatment. Thus, the 25% reduction criterion was a critical one to remedy the BDI trajectories during treatment. Although the alliance is dynamic in nature, the changes that are expected and documented are much less substantial than the reduction in symptoms, so that less adjustment is required. Following Tang and DeRubeis’s method of identifying the amount of relative reduction to be used as a criterion, we conducted a visual inspection of alliance data, in the absence of any other information about the patients, which resulted in the use of the 15% criterion.
Several post-hoc analyses were conducted to test the stability of the findings beyond different models. The findings replicate the originally reported findings. The models included: (a) a model including both patient-rated ruptures and therapist-rated ruptures in the same model in predicting sudden gains both based on patient-rated alliance and based on therapist-rated alliance; (b) a model including an interaction effect between patient-rated ruptures and therapist-rated ruptures in predicting sudden gains both based on patient-rated alliance and based on therapist-rated alliance; (c) a model including first-, second-, and third-order lags of the patients’ and therapists’ report on ruptures in predicting sudden gains in alliance based on patients’ and therapists’ reported alliance.
Several post-hoc analyses were conducted to test the stability of the findings beyond different models. The findings replicate the originally reported findings. The models included: (a) a model including sudden gains based on both patient-rated alliance and therapist-rated alliance in the same model; (b) a model including control on intake SCL levels; (c) a model including an individual-specific control on session outcome level in the session preceding the gain.
References
- Abel A, Hayes AM, Henley W, & Kuyken W (2016). Sudden Gains in Cognitive – Behavior Therapy for Treatment-Resistant Depression : Processes of Change, 84(8), 726–737. [DOI] [PubMed] [Google Scholar]
- Aderka IM, Nickerson A, Bøe HJ, & Hofmann SG (2012). Sudden gains during psychological treatments of anxiety and depression: A meta-analysis. Journal of Consulting and Clinical Psychology, 80(1), 93–101. [DOI] [PubMed] [Google Scholar]
- Andrusyna TP, Luborsky L, Pham T, & Tang TZ (2006). The mechanisms of sudden gains in supportive–expressive therapy for depression. Psychotherapy Research, 16(5), 526–536. [Google Scholar]
- Arnow BA, Steidtmann D, Blasey C, Manber R, Constantino MJ, Klein DN, … Fisher AJ (2013). The relationship between the therapeutic alliance and treatment outcome in two distinct psychotherapies for chronic depression. Journal of Consulting and Clinical Psychology, 81(4), 627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bordin ES (1979). The generalizability of the psychoanalytic concept of the working alliance. Psychotherapy: Theory, Research & Practice, 16(3), 252. [Google Scholar]
- Castonguay LG, & Hill CE (2012). Transformation in psychotherapy: Corrective experiences across cognitive behavioral, humanistic, and psychodynamic approaches. American Psychological Association. [Google Scholar]
- Chen R, Atzil-Slonim D, Bar-Kalifa E, Hasson-Ohayon I, & Refaeli E (2018). Therapists’ recognition of alliance ruptures as a moderator of change in alliance and symptoms. Psychotherapy Research, 28(4), 560–570. [DOI] [PubMed] [Google Scholar]
- Derogatis LR, & Melisaratos N (1983). The brief symptom inventory: an introductory report. Psychological Medicine, 13(3), 595–605. [PubMed] [Google Scholar]
- Eubanks-Carter C, Gorman BS, & Muran JC (2012). Quantitative naturalistic methods for detecting change points in psychotherapy research: An illustration with alliance ruptures. Psychotherapy Research, 22(6), 621–637. [DOI] [PubMed] [Google Scholar]
- Eubanks CF, Muran JC, & Safran JD (2015). Rupture resolution rating system (3RS): Manual. Unpublished Manuscript, Mount Sinai-Beth Israel Medical Center, New York, NY. [Google Scholar]
- Falkenström F, Granström F, & Holmqvist R (2013). Therapeutic alliance predicts symptomatic improvement session by session. Journal of Counseling Psychology, 60(3), 317. [DOI] [PubMed] [Google Scholar]
- Flückiger C, Del Re AC, Wampold BE, & Horvath AO (2018). The alliance in adult psychotherapy: A meta-analytic synthesis. Psychotherapy Relationships That Work, 3. [DOI] [PubMed] [Google Scholar]
- Hayes AM, Laurenceau J-P, Feldman G, Strauss JL, & Cardaciotto L (2007). Change is not always linear: The study of nonlinear and discontinuous patterns of change in psychotherapy. Clinical Psychology Review, 27(6), 715–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ilardi SS, & Craighead WE (1994). The role of nonspecific factors in cognitive-behavior therapy for depression. Clinical Psychology: Science and Practice, 1(2), 138–155. [Google Scholar]
- Kivlighan DM Jr (2007). Where is the relationship in research on the alliance? Two methods for analyzing dyadic data. Journal of Counseling Psychology, 54(4), 423. [Google Scholar]
- Kivlighan DM Jr, Gelso CJ, Ain S, Hummel AM, & Markin RD (2015). The therapist, the client, and the real relationship: An actor–partner interdependence analysis of treatment outcome. Journal of Counseling Psychology, 62(2), 314. [DOI] [PubMed] [Google Scholar]
- Larsson MH, Falkenström F, Andersson G, & Holmqvist R (2018). Alliance ruptures and repairs in psychotherapy in primary care. Psychotherapy Research, 28(1), 123–136. [DOI] [PubMed] [Google Scholar]
- Lorenzo-Luaces L, Driessen E, DeRubeis RJ, Van HL, Keefe JR, Hendriksen M, & Dekker J (2017). Moderation of the alliance-outcome association by prior depressive episodes: Differential effects in cognitive-behavioral therapy and short-term psychodynamic supportive psychotherapy. Behavior Therapy, 48(5), 581–595. [DOI] [PubMed] [Google Scholar]
- Muran JC (2002). A relational approach to understanding change: Plurality and contextualism in a psychotherapy research program. Psychotherapy Research, 12(2), 113–138. [Google Scholar]
- Muran JC (2017). Confessions of a New York rupture researcher: An insider’s guide and critique. Psychotherapy Research, 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muran JC, Safran JD, Eubanks CF, & Gorman BS (2018). The effect of alliancefocused training on a cognitive-behavioral therapy for personality disorders. Journal of Consulting and Clinical Psychology, 86(4), 384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muran JC, Safran JD, Gorman BS, Samstag LW, Eubanks-Carter C, & Winston A (2009). The relationship of early alliance ruptures and their resolution to process and outcome in three time-limited psychotherapies for personality disorders. Psychotherapy: Theory, Research, Practice, Training, 46(2), 233. [DOI] [PubMed] [Google Scholar]
- Muran JC, Safran JD, Samstag LW, & Winston A (1992). Patient and therapist postsession questionnaires, Version 1992. New York: Beth Israel Medical Center. [Google Scholar]
- Rubel JA, Bar-Kalifa E, Atzil-Slonim D, Schmidt S, & Lutz W (2018). Congruence of therapeutic bond perceptions and its relation to treatment outcome: Within-and between-dyad effects. [DOI] [PubMed]
- Rubel JA, Zilcha-Mano S, Feils-Klaus V, & Lutz W (2018). Session-to-session effects of alliance ruptures in outpatient CBT: Within-and between-patient associations. Journal of Consulting and Clinical Psychology, 86(4), 354. [DOI] [PubMed] [Google Scholar]
- Safran JD, & Muran JC (2000). Resolving therapeutic alliance ruptures: Diversity and integration. Journal of Clinical Psychology, 56(2), 233–243. [DOI] [PubMed] [Google Scholar]
- Safran JD, Muran JC, Samstag LW, & Winston A (2005). Evaluating alliance-focused intervention for potential treatment failures: A feasibility study and descriptive analysis. Psychotherapy: Theory, Research, Practice, Training, 42(4), 512. [Google Scholar]
- Snippe E, Fleer J, Tovote KA, Sanderman R, Emmelkamp PMG, & Schroevers MJ (2015). The therapeutic alliance predicts outcomes of cognitive behavior therapy but not of mindfulness-based cognitive therapy for depressive symptoms. Psychotherapy and Psychosomatics, 84(5), 314–315. [DOI] [PubMed] [Google Scholar]
- Tang TZ, & DeRubeis RJ (1999). Sudden gains and critical sessions in cognitive-behavioral therapy for depression. Journal of Consulting and Clinical Psychology, 67(6), 894. [DOI] [PubMed] [Google Scholar]
- Tang TZ, & DeRubeis RJ (2005). Sudden gains in cognitive-behavioral therapy for depression. Journal of Consulting and Clinical Psychology, 73(1), 168–172. [DOI] [PubMed] [Google Scholar]
- Tufekcioglu S, Muran JC, Safran JD, & Winston A (2013). Personality disorder and early therapeutic alliance in two time-limited therapies. Psychotherapy Research, 23(6), 646–657. [DOI] [PubMed] [Google Scholar]
- Turner AE, & Muran JC (1992). Cognitivebehavioral therapy for personality disorders: A treatment manual. Social and Behavioral Sciences Documents Abstracts, (18). [Google Scholar]
- Weiss M, Kivity Y, & Huppert JD (2014). How does the therapeutic alliance develop throughout cognitive behavioral therapy for panic disorder? Sawtooth patterns, sudden gains, and stabilization. Psychotherapy Research, 24(3), 407–418. [DOI] [PubMed] [Google Scholar]
- Wucherpfennig F, Rubel JA, Hofmann SG, & Lutz W (2017). Processes of Change after a Sudden Gain and Relation to Treatment Outcome-Evidence for an Upward Spiral. Journal of Consulting and Clinical Psychology, 85(12), 1199–1210. [DOI] [PubMed] [Google Scholar]
- Zilcha-Mano S (2016). New analytic strategies help answer the controversial question of whether alliance is therapeutic in itself. World Psychiatry, 15(1), 84–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zilcha-Mano S (2017). Is the alliance really therapeutic? Revisiting this question in light of recent methodological advances. American Psychologist, 72(4), 311. [DOI] [PubMed] [Google Scholar]
- Zilcha-Mano S, Muran JC, Eubanks CF, Safran JD, & Winston A (2018). When therapist estimations of the process of treatment can predict patients rating on outcome: The case of the working alliance. Journal of Consulting and Clinical Psychology, 86(4), 398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zilcha-Mano S, Muran JC, Hungr C, Eubanks CF, Safran JD, & Winston A (2016). The relationship between alliance and outcome: Analysis of a two-person perspective on alliance and session outcome. Journal of Consulting and Clinical Psychology, 84(6), 484. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.