Abstract
Background
Despite the widespread adoption of the transradial approach for elderly patients undergoing percutaneous coronary intervention (PCI) in clinical practice, data on octogenarians in China are still relatively limited. This study sought to compare both the safety and efficacy of transradial intervention (TRI) and transfemoral intervention (TFI) in octogenarians in China.
Methods
We identified 254 octogenarians who underwent PCIs in Fuwai Hospital, Beijing, China between January 1, 2006 and April 30, 2011. TRI was used in 184 patients and TFI was used in 70 patients. Incidence rates of in- hospital and 1-year clinical outcomes were compared between the two groups. Ono-to-one propensity score matching (PSM) was performed to control for potential bias. A total of 48 pairs were matched.
Results
Baseline and procedural characteristics were balanced between the TRI and TFI groups. Patients undergoing TRI had significantly fewer access site complications (10.3% vs. 20.0%, p = 0.040), although this difference did not remain significant in propensity score-matched patients (10.4% vs. 22.9%, p = 0.100). After PSM, the patients undergoing TRI were less likely to have major post-PCI bleeding (0 vs. 12.5%, odds ratio 0.47, 95% confidence interval 0.37-0.58, p = 0.026). There were no statistical differences in the incidence rates of major adverse cardiac events (a composite of cardiac death, myocardial infarction, and target vessel revascularization) and their components both during hospitalization and at 1-year.
Conclusions
Compared with TFI, TRI was safer and more feasible for octogenarians undergoing PCI.
Keywords: Coronary artery disease, Octogenarian, Percutaneous coronary intervention, Transfemoral intervention, Transradial intervention
INTRODUCTION
Transradial interventions (TRI), as opposed to traditional transfemoral intervention (TFI), has been increasingly adopted for percutaneous coronary intervention (PCI) due to its potential advantages. Previous studies have demonstrated fewer access site-related bleeding and vascular complications, shorter length of stay, and better satisfaction in patients undergoing TRI.1-11
Due to extended life expectancy and stagnation of birth rates, our society is aging rapidly. Elderly patients with coronary artery disease represent a growing population who will benefit from PCI. Nevertheless, they have also been reported to have higher risks of access site-related complications, postprocedural bleeding, and mortality.12-15 Several studies have shown the safety and efficacy of TRI in octogenarians,16-19 but data on TRI in octogenarians in China are still limited. Using data from the Fuwai database, a single-center registry based on the largest heart center in the People’s Republic of China, we sought to examine the safety and efficacy of TRI in octogenarians in China.
MATERIALS AND METHODS
Our study population consisted of a consecutive cohort of octogenarians who underwent PCI between January 1, 2006 and April 30, 2011, at Fuwai Hospital in Beijing, China. We identified 254 patients, of whom 184 had TRI and 70 had TFI. The Institutional Review Board of Fuwai Hospital, Peking Union Medical College, approved the study and waived the requirement for informed consent.
The primary endpoints were in-hospital and 1-year major adverse cardiac events (MACE), defined as a composite of cardiac death, myocardial infarction, and target vessel revascularization. Secondary endpoints included each component of in-hospital and 1-year MACE, access site complications, and major bleeding.
Access site complications were defined as local hematoma that prolonged hospital stay, mediastinal hematoma, retroperitoneal hematoma, aneurysm, and arteriovenous fistula. Bleeding was defined according to the Bleeding Academic Research Consortium (BARC) definition,20 and a bleeding event with BARC grade ≥ 3 was considered to indicate major bleeding. Th patients’ baseline, angiographic, and procedural characteristics were obtained from the medical record system and the catheterization laboratory’s database. In-hospital outcomes were validated by medical record review. Follow-up work was performed by trained personnel at Fuwai Hospital via phone visits at 6 months and 1 year after discharge.
Continuous variables were expressed as mean ± standard deviation and compared using the Student’s t test. Categorical variables were described using frequencies and percentages and compared using the chi-square test or Fisher’s exact test, as appropriate. Clinical outcomes between the TRI and TFI groups were analyzed by logistic regression and expressed as odds ratio (OR)/hazard ratio (HR) and 95% confidence interval (CI).
Since treatment decisions in real-world practice are not made based on randomization, 1:1 propensity score matching (PSM) was performed to control for potential bias. Propensity scores were calculated using a logistic regression model with access route as the dependent variable. Independent variables included age; gender; prior history of myocardial infarction (MI), coronary artery bypass grafting (CABG) surgery, PCI, stroke, diabetes mellitus, hypertension, or hyperlipidemia; clinical diagnosis; left ventricular ejection fraction (LVEF) before PCI; hemoglobin level before PCI; creatinine concentration before PCI; use of anticoagulant agents; single-, double-, or triple-vessel lesions; left main disease; lesion type (de novo, intrastent, or restenosis); lesion location (ostial or bifurcation lesion); sheath size; number of treated lesions; number of stents used; and the use of drug-eluting stents. In order to prevent poor matches, the caliper was set as 0.05. A total of 48 pairs were matched, and the C-statistics for the propensity score model was 0.69. The paired t test for continuous variables and paired chi-square test or Fisher’s exact test for categorical variables were then performed within the matched pairs of patients. Data were analyzed according to the intention-to-treat principle (before potential crossover). All statistical analyses were performed using IBM SPSS software, version 22.0 (IBM Corp, Armonk, New York) and a 2-sided p < 0.05 was considered to be significant.
RESULTS
A total of 254 patients underwent PCI between January 1, 2006 and April 30, 2011. TRI was performed in 184 patients (72.4%). The baseline and procedural characteristics of the patients are shown in Tables 1 and 2. Compared with TFI, the patients undergoing TRI had fewer prior MI and CABG and were more likely to have triple-vessel lesions (p < 0.05). They also had higher mean LVEF (mean 60.1% vs. 56.8%, p = 0.004), with 12.0% being lower than 50% (p = 0.617, compared with the TFI group). A ≤ 6F sheath was more frequently used in the TRI patients (98.4% vs. 84.3%, p < 0.001). There were no significant differences between the two groups with regards to other baseline and procedural characteristics. After PSM, all characteristics were well-balanced between the TRI and TFI patients.
Table 1. Baseline characteristics of octogenarians undergoing transradial (TRI) and transfemoral intervention (TFI).
| Characteristics | All patients | Propensity score-matched patients | ||||
| TRI, n = 184 (%) | TFI, n = 70 (%) | p | TRI, n = 48 (%) | TFI, n = 48 (%) | p | |
| Age, year* | 82.1 ± 2.6 | 81.6 ± 1.7 | 0.171 | 81.9 ± 2.2 | 81.7 ± 1.9 | 0.593 |
| Female | 59 (32.1) | 23 (32.9) | 0.904 | 16 (33.3) | 18 (37.5) | 0.670 |
| Medical history of | ||||||
| Myocardial infarction | 41 (22.3) | 27 (38.6) | 0.014 | 16 (33.3) | 18 (37.5) | 0.670 |
| Prior CABG | 2 (1.1) | 16 (22.9) | < 0.001 | 2 (4.2) | 4 (8.3) | 0.677 |
| Prior PCI | 39 (21.2) | 20 (28.6) | 0.214 | 14 (29.2) | 13 (27.1) | 0.820 |
| Stroke | 14 (7.6)0 | 7 (10.0) | 0.813 | 7 (14.6) | 7 (14.6) | 1 |
| Diabetes mellitus | 44 (23.9) | 21 (30.0) | 0.321 | 12 (25.0) | 12 (25.0) | 1 |
| Hypertension | 119 (64.7) | 50 (71.4) | 0.308 | 31 (64.6) | 30 (62.5) | 0.832 |
| Hyperlipidemia | 87 (47.3) | 28 (40.0) | 0.297 | 17 (35.4) | 16 (33.3) | 0.830 |
| Diagnosis | ||||||
| STEMI | 41 (22.3) | 20 (28.6) | 0.294 | 15 (31.2) | 18 (37.5) | 0.519 |
| NSTEMI | 12 (6.5)0 | 4 (5.7) | 0.536 | 3 (6.2) | 3 (6.2) | 1 |
| Unstable angina | 84 (45.7) | 28 (40.0) | 0.418 | 21 (43.8) | 17 (35.4) | 0.404 |
| Stable angina | 44 (23.9) | 18 (25.7) | 0.765 | 8 (16.7) | 10 (20.8) | 0.601 |
| Others | 3 (1.6) | 0 (0) | 0.671 | 1 (2.1) | 0 (0)0. | 1 |
| LVEF, %* | 60.1 ± 9.3 | 56.8 ± 7.6 | 0.004 | 57.2 ± 9.8 | 56.7 ± 7.8 | 0.817 |
| LVEF < 50% | 22 (12.0) | 10 (14.3) | 0.617 | 10 (20.8) | 7 (14.6) | 0.423 |
| Hemoglobin, g/L* | 125.4 ± 15.2 | 125.5 ± 18.8 | 0.971 | 129.6 ± 15.6 | 124.0 ± 19.7 | 0.138 |
| Creatinine, μmol/L* | 90.8 ± 35.1 | 93.9 ± 20.3 | 0.572 | 87.1 ± 21.5 | 93.6 ± 24.2 | 0.272 |
| GP IIb/IIIa usage | 7 (3.8) | 2 (2.9) | 0.715 | 3 (6.2) | 2 (4.2) | 1 |
| LMWH usage | 120 (65.2) | 46 (65.7) | 0.941 | 36 (75.0) | 30 (62.5) | 0.186 |
| Fondaparinux sodium usage | 4 (2.2) | 4 (5.7) | 0.221 | 2 (4.2) | 2 (4.2) | 1 |
CABG, coronary arterial bypass grafting; GP, glycoprotein; LMWH, low molecular weight heparin; LVEF, left ventricle ejection fraction; NSTEMI, non-ST-segment elevation myocardial infarction; PCI, percutaneous coronary intervention; SD, standard deviation; STEMI, ST-segment elevation myocardial infarction.
* Presented as mean ± SD.
Table 2. Angiographic and procedural characteristics of octogenarians undergoing transradial (TRI) and transfemoral intervention (TFI).
| Characteristics | All patients | Propensity score-matched patients | ||||
| TRI, n = 184 (%) | TFI, n = 70 (%) | p | TRI, n = 48 (%) | TFI, n = 48 (%) | p | |
| Procedural success | 181 (98.4) | 70 (100) | 0.563 | 47 (97.9) | 48 (100). | 1 |
| Left main disease | 21 (11.4) | 15 (21.4) | 0.065 | 6 (12.5) | 9 (18.8) | 0.399 |
| Diseased coronary vessels | ||||||
| Single vessel | 37 (20.1) | 10 (14.3) | 0.286 | 6 (12.5) | 5 (10.4) | 0.749 |
| Double vessel | 58 (31.5) | 16 (22.9) | 0.174 | 13 (27.1) | 12 (25.0) | 0.816 |
| Triple vessel | 89 (48.4) | 44 (62.9) | 0.039 | 29 (60.4) | 31 (64.6) | 0.673 |
| Lesion type | ||||||
| De novo | 179 (97.3) | 65 (92.9) | 0.144 | 46 (95.8) | 46 (95.8) | 1 |
| Intra stent | 5 (2.7) | 3 (4.3) | 0.688 | 2 (4.2) | 1 (2.1) | 1 |
| Restenosis | 0 (0) | 2 (2.9) | 0.075 | 0 (0) | 1 (2.1) | 1 |
| Lesion location | ||||||
| Ostial lesion | 22 (12.0) | 8 (11.4) | 0.907 | 11 (22.9) | 5 (10.4) | 0.100 |
| Bifurcation lesion | 60 (32.6) | 21 (30.0) | 0.690 | 12 (25.0) | 11 (22.9) | 0.811 |
| Chronic total occlusion | 22 (12.0) | 5 (7.1) | 0.266 | 7 (14.6) | 4 (8.3) | 0.336 |
| Sheath size ≤ 6F | 181 (98.4) | 59 (84.3) | < 0.001 | 45 (93.8) | 47 (97.9) | 0.617 |
| Number of treated lesion* | 1.3 ± 0.5 | 1.4 ± 0.7 | 0.171 | 1.3 ± 0.5 | 1.4 ± 0.7 | 0.135 |
| Number of stents used* | 1.7 ± 0.8 | 1.7 ± 1.1 | 0.938 | 1.7 ± 0.7 | 1.7 ± 1.1 | 0.829 |
| DES usage | 174 (94.6) | 62 (88.6) | 0.106 | 45 (93.8) | 40 (83.3) | 0.109 |
| Intravascular ultrasound | 10 (5.4)0 | 2 (2.9) | 0.520 | 4 (8.3) | 0 (0) | 0.117 |
| IABP support | 14 (7.6)0 | 7 (10.0) | 0.611 | 4 (8.3) | 3 (6.2) | 1 |
| Total procedure time, minute* | 38.2 ± 22.5 | 41.4 ± 20.2 | 0.303 | 37.3 ± 18.5 | 40.8 ± 19.5 | 0.375 |
| Contrast volume, ml* | 155.8 ± 72.0 | 147.0 ± 63.7 | 0.388 | 158.5 ± 67.0 | 150.9 ± 69.8 | 0.606 |
| Dissection | 1 (0.5) | 1 (1.4) | 0.476 | 0 (0) | 1 (2.1) | 1 |
| Acute thrombosis | 1 (0.5) | 3 (4.3) | 0.065 | 0 (0) | 3 (6.2) | 0.242 |
DES, drug-eluting stents; IABP, intra-aortic balloon pump; SD, standard deviation.
* Presented as mean ± SD.
Six patients (2.4%) failed TRI procedures and were converted to TFI. No patients in the TFI group crossed over to the TRI group. A vascular closure device was used in 30 patients (42.9%) in the TFI group.
Data on bleeding and complications from PCI are shown in Table 3. The incidence rates for BARC ≥ 2 (10.9% vs. 24.3%, p = 0.007) and BARC ≥ 3 (2.7% vs. 10.0%, p = 0.022) post-PCI bleeding were both significantly lower in the TRI group than the TFI group. Moreover, access-site-related major bleeding was less frequently observed among the TRI patients (1.1% vs. 7.1%, p = 0.018). Non-access-site-related major bleeding also tended to be less frequent in the TRI group, but this did not reach statistical significance. The TRI group had fewer access site complications (10.3% vs. 20.0%, p = 0.040). Despite these differences, the transfusion rate was similar between the two groups. In the propensity score-matched patients, rates of BARC ≥ 2 (12.5% vs. 29.2%, p = 0.044) and BARC ≥ 3 (0 vs. 12.4%, p = 0.026) bleeding remained significantly lower, while the rate of access site complications did not (10.4% vs. 22.9%, p = 0.100).
Table 3. Bleeding and complications of octogenarians undergoing transradial (TRI) and transfemoral (TFI) intervention.
| Complications | All patients | Propensity score-matched patients | ||||
| TRI, n = 184 (%) | TFI, n = 70 (%) | p | TRI, n = 48 (%) | TFI, n = 48(%) | p | |
| BARC ≥ 2 bleeding | 20 (10.9) | 17 (24.3) | 0.007 | 6 (12.5) | 14 (29.2) | 0.044 |
| BARC ≥ 3 bleeding | 5 (2.7) | 7 (10.0) | 0.022 | 0 (0) | 6 (12.5) | 0.026 |
| Access-site-related major bleeding | 2 (1.1) | 5 (7.1) | 0.018 | 0 (0) | 4 (8.3) | 0.117 |
| Non-access-site-related major bleeding | 3 (1.6) | 2 (2.9) | 0.618 | 0 (0) | 2 (4.2) | 0.495 |
| Access site complications | 19 (10.3) | 14 (20.0) | 0.040 | 5 (10.4) | 11 (22.9) | 0.100 |
| Local hematoma | 18 (10.3) | 10 (14.2) | 0.306 | 5 (10.4) | 9 (18.8) | 0.247 |
| Mediastinal hematoma | 0 | 0 | 1 | 0 | 0 | 1 |
| Retroperitoneal hematoma | 0 | 2 (2.9) | 0.021 | 0 | 1 (2.1) | 1 |
| Aneurysm | 1 (0.5) | 2 (2.9) | 0.185 | 0 (0) | 1 (2.1) | 1 |
| Arteriovenous fistula | 0 | 0 | 1 | 0 | 0 | 1 |
| Transfusion | 2 (1.1) | 4 (5.7) | 0.051 | 0 (0) | 2 (4.2) | 0.495 |
BARC, bleeding academic research consortium.
The in-hospital outcomes are shown in Table 4. The rates of MACE, cardiac death, myocardial infarction, and target vessel revascularization were similar in the two groups both before and after PSM. However, the TRI patients were less likely to suffer from major bleeding than the TFI patients during the index hospitalization (OR: 0.47, 95% CI: 0.37-0.58, p = 0.026).
Table 4. In-hospital and 1-year outcomes of octogenarians undergoing transradial (TRI) and transfemoral (TFI) intervention.
| Outcomes | All patients | Propensity score-matched patients | ||||||
| TRI, n = 184 (%) | TFI, n = 70 (%) | OR/HR (95% CI) | p | TRI, n = 48 (%) | TFI, n = 48 (%) | OR/HR (95% CI) | p | |
| In-hospital outcomes | ||||||||
| MACE | 10 (5.4) | 7 (10.0) | 0.52 (0.19-1.41) | 0.200 | 4 (8.3) | 5 (10.4) | 0.78 (0.44-1.39) | 1 |
| Cardiac death | 6 (0.4) | 3 (1.1) | 0.56 (0.09-3.44) | 0.535 | 2 (4.2) | 2 (4.2) | 1 (0.37-2.72) | 1 |
| MI | 2 (2.7) | 4 (5.7) | 0.61 (0.21-1.84) | 0.586 | 3 (6.2) | 4 (8.3) | 0.87 (0.44-1.70) | 1 |
| Target vessel revascularization | 4 (2.2) | 2 (2.9) | 0.76 (0.14-4.22) | 0.749 | 0 (0) | 0 (0) | NA | NA |
| Major bleeding | 5 (2.7) | 7 (10.0) | 0.25 (0.08-0.82) | 0.022 | 0 (0) | 6 (12.5) | 0.47 (0.37-0.58) | 0.026 |
| One-year outcomes | ||||||||
| MACE | 8 (4.3) | 5 (7.1) | 0.61 (0.20-1.85) | 0.378 | 6 (12.5) | 5 (10.4) | 1.17 (0.36-3.84) | 0.793 |
| Cardiac death | 4 (2.2) | 5 (7.1) | 0.30 (0.08-1.11) | 0.073 | 3 (6.1) | 5 (10.4) | 0.57 (0.14-2.39) | 0.442 |
| MI | 3 (1.6) | 1 (1.4) | 1.13 (0.12-10.89) | 0.914 | 2 (4.1) | 1 (2.1) | 1.91 (0.17-21.02) | 0.598 |
| Target vessel revascularization | 4 (2.2) | 1 (1.4) | 1.51 (0.17-13.55) | 0.711 | 3 (6.1) | 1 (2.1) | 2.88 (0.30-27.68) | 0.360 |
CI, confidence interval; HR, hazard ratio; OR, odds ratio; MACE, major adverse cardiac events (a composite of cardiac death, myocardial infarction, and target vessel revascularization); MI, myocardial infarction; NA, not applicable.
Follow-up work was completed in all 254 patients with a median follow-up time of 362 days [interquartile range (IQR), 354-365 days] and 363 days (IQR, 356-366 days) for the TRI and TFI groups, respectively. The Kaplan-Meier curves for 1-year clinical outcomes are shown in Figure 1. There were no significant differences between the two groups with regards to 1-year MACE and the components (p > 0.05).
Figure 1.
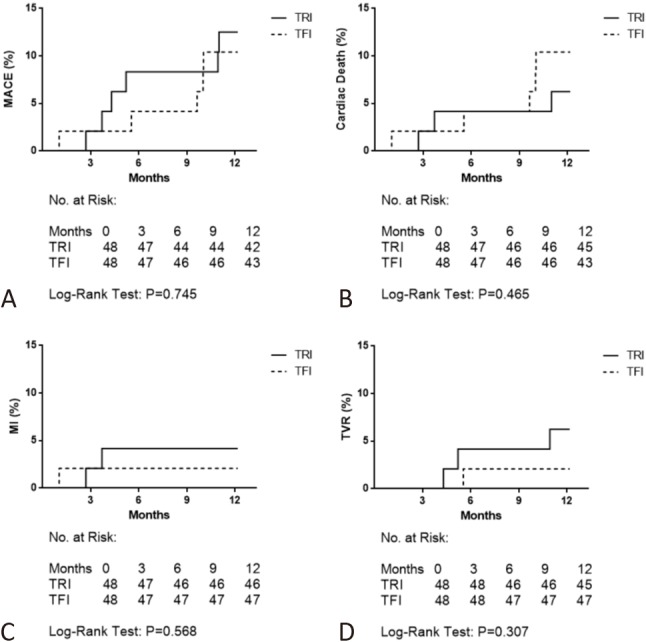
Kaplan-Meier curves for occurrence of MACE (A), cardiac death (B), MI (C), and TVR (D) between groups of TRI and TFI at 1-year in propensity score-matched patients. MACE, major adverse cardiac events (a composite of cardiac death, myocardial infarction, and target vessel revascularization); MI, myocardial infarction; TFI, transfemoral intervention; TRI, transradial intervention; TVR, target vessel revascularization.
DISCUSSION
Due to the advantages of fewer access site-related bleeding and vascular complications, shorter length of stay, and better patient satisfaction, the transradial approach has been widely adopted over the past decade.1-11 The safety and feasibility of TRI in octogenarians have also been reported.16-19 Consistent with these studies, we found that the patients undergoing TRI had fewer access site complications and were less likely to suffer from post-PCI bleeding. After controlling for potential bias using propensity score analysis, they were still less likely to suffer from post-PCI bleeding. There were no statistical differences in the incidence rates of MACE and the components both during hospitalization and at 1-year. Taken together with previous studies which were conducted outside China,16-18 our findings support the current recommendations21,22 for the use of radial artery access in PCI, and add evidence to promote more widespread adoption of TRI in octogenarians.
Compared with their younger counterparts, octogenarians undergoing PCI are at a higher risk of complications, including access site complications.14,23,24 A lower risk of access site complications is considered to be one of the major benefits of TRI, however most of the studies supporting this idea have been conducted in younger populations.25 Coronary artery catheterization from a transradial approach is more technically demanding26,27 and may become even more difficult in octogenarians who have advanced vascular diseases. However, previous studies on TRI versus TFI in octogenarians have all shown positive results. The OCTOPLUS study, a randomized study on TRI versus TFI in octogenarians, showed a significantly lower rate of hematoma in the transradial group.17 Jaffe et al.18 also reported reduced rates of access site bleeding, hematoma, and other vascular complications in octogenarians undergoing TRI. Koutouzis et al.16 found a similar trend of such benefits with the transradial approach, although the difference was not significant. Consistent with previous data, we found that our TRI patients were less likely to suffer from access site complications (10.3% vs. 20.0%, p = 0.040). However, the difference did not remain significant after PSM (10.4% vs. 22.9%, p = 0.100). This lack of significance was probably due to a limited number of propensity score matched patients, because the rate of access site complications was still numerically lower.
Bleeding has been identified as a strong predictor of worst outcomes after PCI.28,29 Several strategies have emerged to reduce the risk of post-PCI bleeding, including pharmacological, technological, and procedural approaches.30 As a procedural approach, TRI has been shown to reduce bleeding in both randomized1,9,11 and observational4,8,10 studies. The updated European guidelines also recommend choosing TRI over TFI for coronary angiography and PCI in order to reduce the incidence of bleeding.31 The physiological reasons for recommending TRI are evident: radial arteries are superficial and readily compressible in clinical practice. Consistent with previous analyses, we found that rates of BARC ≥ 2 and BARC ≥ 3 post-PCI bleeding were significantly lower in the patients undergoing TRI both before and after PSM. TRI was also associated with reduced post-PCI major bleeding (OR: 0.47, 95% CI: 0.37-0.58, p = 0.026). These findings further support the idea that using the transradial approach in octogenarians can lead to improved outcomes after PCI.
Some limitations of this study should be acknowledged. First, it was limited by its nonrandomized nature. Treatment decisions in real-world practice are often made based on prognostic factors rather than results of randomization. Although propensity score matching was performed to control for potential bias, it still cannot be considered a substitute for a randomized prospective study. Second, this study only included data from a single center, although this is the largest and most experienced center in China. Importantly, the benefit of TRI over TFI likely depends on the operators’ experience and their training with the radial technique,26,32,33 both of which may differ from site to site. Thus, the generalizability of our findings to other less-experienced centers remains to be further established.
CONCLUSIONS
In this retrospective study of TRI versus TFI in Chinese octogenarians based on propensity score analysis, TRI showed the advantages of safety and feasibility over TFI. A wider adoption of TRI in octogenarians has the potential to improve outcomes in the treatment of coronary artery diseases.
DECLARATION OF CONFLICT OF INTEREST
All the authors declare no conflict of interest.
REFERENCES
- 1.Jolly SS, Yusuf S, Cairns J, et al. Radial versus femoral access for coronary angiography and intervention in patients with acute coronary syndromes (RIVAL): a randomised, parallel group, multicentre trial. Lancet. 2011;377:1409–1420. doi: 10.1016/S0140-6736(11)60404-2. [DOI] [PubMed] [Google Scholar]
- 2.Yang YJ, Kandzari DE, Gao Z, et al. Transradial versus transfemoral method of percutaneous coronary revascularization for unprotected left main coronary artery disease: comparison of procedural and late-term outcomes. JACC Cardiovasc Interv. 2010;3:1035–1042. doi: 10.1016/j.jcin.2010.09.003. [DOI] [PubMed] [Google Scholar]
- 3.Brueck M, Bandorski D, Kramer W, et al. A randomized comparison of transradial versus transfemoral approach for coronary angiography and angioplasty. JACC Cardiovasc Interv. 2009;2:1047–1054. doi: 10.1016/j.jcin.2009.07.016. [DOI] [PubMed] [Google Scholar]
- 4.Feldman DN, Swaminathan RV, Kaltenbach LA, et al. Adoption of radial access and comparison of outcomes to femoral access in percutaneous coronary intervention an updated report from the National Cardiovascular Data Registry (2007–2012). Circulation. 2013;127:2295–2306. doi: 10.1161/CIRCULATIONAHA.112.000536. [DOI] [PubMed] [Google Scholar]
- 5.Chase AJ, Fretz EB, Warburton WP, et al. Association of the arterial access site at angioplasty with transfusion and mortality: the MORTAL study (Mortality benefit OF Reduced Transfusion after percutaneous coronary intervention via the Arm or Leg). Heart. 2008;94:1019–1025. doi: 10.1136/hrt.2007.136390. [DOI] [PubMed] [Google Scholar]
- 6.Baklanov DV, Kaltenbach LA, Marso SP, et al. The prevalence and outcomes of transradial percutaneous coronary intervention for ST-segment elevation myocardial infarction: analysis from the National Cardiovascular Data Registry (2007 to 2011). J Am Coll Cardiol. 2013;61:420–426. doi: 10.1016/j.jacc.2012.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rao SV, Cohen MG, Kandzari DE, et al. The transradial approach to percutaneous coronary intervention: historical perspective, current concepts, and future directions. J Am Coll Cardiol. 2010;55:2187–2195. doi: 10.1016/j.jacc.2010.01.039. [DOI] [PubMed] [Google Scholar]
- 8.Jin C, Li W, Qiao SB, et al. Costs and benefits associated with transradial versus transfemoral percutaneous coronary intervention in China. J Am Heart Assoc. 2016;5:pii:e002684. doi: 10.1161/JAHA.115.002684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Romagnoli E, Biondi-Zoccai G, Sciahbasi A, et al. Radial versus femoral randomized investigation in ST-segment elevation acute coronary syndrome: the RIFLE-STEACS (Radial Versus Femoral Randomized Investigation in ST-Elevation Acute Coronary Syndrome) study. J Am Coll Cardiol. 2012;60:2481–2489. doi: 10.1016/j.jacc.2012.06.017. [DOI] [PubMed] [Google Scholar]
- 10.Jin C, Xu Y, Qiao S, et al. Comparison of transradial and transfemoral approaches in women undergoing percutaneous coronary intervention in China: a retrospective observational study. Angiology. 2017;68:799–806. doi: 10.1177/0003319716685670. [DOI] [PubMed] [Google Scholar]
- 11.Valgimigli M, Gagnor A, Calabró P, et al. Radial versus femoral access in patients with acute coronary syndromes undergoing invasive management: a randomised multicentre trial. Lancet. 2015;385:2465–2476. doi: 10.1016/S0140-6736(15)60292-6. [DOI] [PubMed] [Google Scholar]
- 12.Feldman DN, Gade CL, Slotwiner AJ, et al. Comparison of outcomes of percutaneous coronary interventions in patients of three age groups (< 60,60 to 80, and > 80 years) (from the New York State Angioplasty Registry). American J Cardiol. 2006;98:1334–1339. doi: 10.1016/j.amjcard.2006.06.026. [DOI] [PubMed] [Google Scholar]
- 13.Assali AR, Moustapha A, Sdringola S, et al. The dilemma of success: percutaneous coronary interventions in patients ≥ 75 years of age—successful but associated with higher vascular complications and cardiac mortality. Cathet Cardiovasc Interv. 2003;59:195–199. doi: 10.1002/ccd.10532. [DOI] [PubMed] [Google Scholar]
- 14.Piper WD, Malenka DJ, Ryan TJ, et al. Predicting vascular complications in percutaneous coronary interventions. Am Heart J. 2003;145:1022–1029. doi: 10.1016/S0002-8703(03)00079-6. [DOI] [PubMed] [Google Scholar]
- 15.Wei CC, Lee SH. Predictors of mortality in elderly patients with non-ST elevation acute coronary syndrome - data from Taiwan Acute Coronary Syndrome Full Spectrum Registry. Acta Cardiol Sin. 2017;33:377–383. doi: 10.6515/ACS20170126A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Koutouzis M, Matejka G, Olivecrona G, et al. Radial vs. femoral approach for primary percutaneous coronary intervention in octogenarians. Cardiovasc Revasc Med. 2010;11:79–83. doi: 10.1016/j.carrev.2009.04.107. [DOI] [PubMed] [Google Scholar]
- 17.Louvard Y, Benamer H, Garot P, et al. Comparison of transradial and transfemoral approaches for coronary angiography and angioplasty in octogenarians (the OCTOPLUS study). Am J Cardiol. 2004;94:1177–1180. doi: 10.1016/j.amjcard.2004.07.089. [DOI] [PubMed] [Google Scholar]
- 18.Jaffe R, Hong T, Sharieff W, et al. Comparison of radial versus femoral approach for percutaneous coronary interventions in octogenarians. Catheter Cardiovasc Interv. 2007;69:815–820. doi: 10.1002/ccd.21021. [DOI] [PubMed] [Google Scholar]
- 19.Lee HW, Cha KS, Ahn J, et al. Comparison of transradial and transfemoral coronary intervention in octogenarians with acute myocardial infarction. Int J Cardiol. 2016;202:419–424. doi: 10.1016/j.ijcard.2015.09.004. [DOI] [PubMed] [Google Scholar]
- 20.Mehran R, Rao SV, Bhatt DL, et al. Standardized bleeding definitions for cardiovascular clinical trials a consensus report from the bleeding academic research consortium. Circulation. 2011;123:2736–2747. doi: 10.1161/CIRCULATIONAHA.110.009449. [DOI] [PubMed] [Google Scholar]
- 21.Windecker S, Kolh P, Alfonso F, et al. 2014 ESC/EACTS Guidelines on myocardial revascularization: The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J. 2014;35:2541–2619. doi: 10.1093/eurheartj/ehu278. [DOI] [PubMed] [Google Scholar]
- 22.Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol. 2011;58:e44–122. doi: 10.1016/j.jacc.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 23.Klein LW, Block P, Brindis RG, et al. Percutaneous coronary interventions in octogenarians in the American College of Cardiology–National Cardiovascular Data Registry: development of a nomogram predictive of in-hospital mortality. J Am Coll Cardiol. 2002;40:394–402. doi: 10.1016/s0735-1097(02)01992-7. [DOI] [PubMed] [Google Scholar]
- 24.Kobayashi Y, Mehran R, Mintz GS, et al. Comparison of in-hospital and one-year outcomes after multiple coronary arterial stenting in patients ≥ 80 years old versus those < 80 years old. Am J Cardiol. 2003;92:443–446. doi: 10.1016/s0002-9149(03)00663-5. [DOI] [PubMed] [Google Scholar]
- 25.Bertrand OF, Bélisle P, Joyal D, et al. Comparison of transradial and femoral approaches for percutaneous coronary interventions: a systematic review and hierarchical Bayesian meta-analysis. Am Heart J. 2012;163:632–648. doi: 10.1016/j.ahj.2012.01.015. [DOI] [PubMed] [Google Scholar]
- 26.Dehghani P, Mohammad A, Bajaj R, et al. Mechanism and predictors of failed transradial approach for percutaneous coronary interventions. JACC Cardiovasc Interv. 2009;2:1057–1064. doi: 10.1016/j.jcin.2009.07.014. [DOI] [PubMed] [Google Scholar]
- 27.Kiemeneij F, Laarman GJ, Odekerken D, et al. A randomized comparison of percutaneous transluminal coronary angioplasty by the radial, brachial and femoral approaches: the access study. J Am Coll Cardiol. 1997;29:1269–1275. doi: 10.1016/s0735-1097(97)00064-8. [DOI] [PubMed] [Google Scholar]
- 28.Doyle BJ, Rihal CS, Gastineau DA, Holmes DR. Bleeding, blood transfusion, and increased mortality after percutaneous coronary intervention: implications for contemporary practice. J Am Coll Cardiol. 2009;53:2019–2027. doi: 10.1016/j.jacc.2008.12.073. [DOI] [PubMed] [Google Scholar]
- 29.Chu CY, Lin TH, Lai WT. The management and prognostic factors of acute coronary syndrome: evidence from the Taiwan Acute Coronary Syndrome Full Spectrum Registry. Acta Cardiol Sin. 2017;33:329–338. doi: 10.6515/ACS20161205A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dauerman HL, Rao SV, Resnic FS, Applegate RJ. Bleeding avoidance strategies: consensus and controversy. J Am Coll Cardiol. 2011;58:1–10. doi: 10.1016/j.jacc.2011.02.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Roffi M, Patrono C, Collet JP, et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J. 2016;37:267–315. doi: 10.1093/eurheartj/ehv320. [DOI] [PubMed] [Google Scholar]
- 32.Ball WT, Sharieff W, Jolly SS, et al. Characterization of operator learning curve for transradial coronary interventions. Circ Cardiovasc Interv. 2011;4:336–341. doi: 10.1161/CIRCINTERVENTIONS.110.960864. [DOI] [PubMed] [Google Scholar]
- 33.Burzotta F, Trani C, Tommasino A, et al. Impact of operator experience and wiring technique on procedural efficacy of trans-radial percutaneous chronic total occlusion recanalization performed by dedicated radialists. Cardiol J. 2013 doi: 10.5603/CJ.a2013.0063. [DOI] [PubMed] [Google Scholar]


