Short abstract
Introduction
Acute stroke unit care, intravenous thrombolysis and endovascular treatment significantly improve the outcome for patients with ischaemic stroke, but data on access and delivery throughout Europe are lacking. We assessed best available data on access and delivery of acute stroke unit care, intravenous thrombolysis and endovascular treatment throughout Europe.
Methods
A survey, drafted by stroke professionals (ESO, ESMINT, EAN) and a patient organisation (SAFE), was sent to national stroke societies and experts in 51 European countries (World Health Organization definition) requesting experts to provide national data on stroke unit, intravenous thrombolysis and endovascular treatment rates. We compared both pooled and individual national data per one million inhabitants and per 1000 annual incident ischaemic strokes with highest country rates. Population estimates were based on United Nations data, stroke incidences on the Global Burden of Disease Report.
Results
We obtained data from 44 European countries. The estimated mean number of stroke units was 2.9 per million inhabitants (95% CI 2.3–3.6) and 1.5 per 1000 annual incident strokes (95% CI 1.1–1.9), highest country rates were 9.2 and 5.8. Intravenous thrombolysis was provided in 42/44 countries. The estimated mean annual number of intravenous thrombolysis was 142.0 per million inhabitants (95% CI 107.4–176.7) and 72.7 per 1000 annual incident strokes (95% CI 54.2–91.2), highest country rates were 412.2 and 205.5. Endovascular treatment was provided in 40/44 countries. The estimated mean annual number of endovascular treatments was 37.1 per million inhabitants (95% CI 26.7–47.5) and 19.3 per 1000 annual incident strokes (95% CI 13.5–25.1), highest country rates were 111.5 and 55.9. Overall, 7.3% of incident ischaemic stroke patients received intravenous thrombolysis (95% CI 5.4–9.1) and 1.9% received endovascular treatment (95% CI 1.3–2.5), highest country rates were 20.6% and 5.6%.
Conclusion
We observed major inequalities in acute stroke treatment between and within 44 European countries. Our data will assist decision makers implementing tailored stroke care programmes for reducing stroke-related morbidity and mortality in Europe.
Keywords: Survey, Europe, acute stroke treatment, health care resources, stroke unit, intravenous thrombolysis, endovascular treatment
Introduction
Stroke is the second most common single cause of death in Europe. It is responsible for more than one million deaths per year and is the leading cause of long-term disability.1,2 Twenty to 35% of stroke patients die within the first month after a stroke, and up to one-third of survivors lose their independence.3,4,5 Consequently, the socioeconomic impact of stroke is considerable: the annual cost of stroke in Europe is estimated to be €45 billion: €20 billion for direct care, €9 billion related to loss of productivity and €16 billion for informal care.1 The burden of stroke differs widely across Europe. Specifically, the incidence and case fatality of stroke in central and eastern European countries remain higher than in northern, western and southern European countries.1,6–9
The main pillars of acute ischaemic stroke treatment are stroke unit (SU) care and treatments promoting revascularisation. SUs, defined as dedicated areas or wards in hospitals open round the clock, where stroke patients are admitted and cared for by a multidisciplinary team including medical, nursing and therapy staff, are most effective in reducing mortality and morbidity.10–12 Since 2002, intravenous thrombolysis (IVT) has been approved in Europe for use in acute stroke treatment.13 In 2015, following randomised controlled trials demonstrating that endovascular treatment (EVT) dramatically improves the outcome of stroke patients with large vessel occlusion in the anterior circulation, European guidelines recommended the use of EVT in comprehensive stroke centres (CSCs).14–16 However, pan-European data on the access to and delivery of SU care, IVT and EVT are lacking.
Therefore, the European Stroke Organisation (ESO), the European Society of Minimally Invasive Neurological Therapy (ESMINT), the European Academy of Neurology (EAN) and the Stroke Alliance for Europe (SAFE) surveyed the access to and delivery rates of acute SU care, IVT and EVT throughout Europe.
Objectives
We aimed to collect national data on access to and delivery rates for acute SU care, IVT and EVT throughout Europe. We compared both pooled data of all countries and individual country rates with highest country rates. We also aimed to estimate the number of SUs necessary to cover the needs of the European population and to calculate how many patients could be treated with IVT and EVT if best practice were to be followed in all European countries.
Methods
Study design and participants
This pan-European study surveyed European chairs of national stroke societies and stroke experts on the access to and delivery rates of acute SU care, IVT and EVT in their countries. The study’s steering committee consisted of 10 representatives from ESO, ESMINT, EAN and SAFE, including at least 1 board member from each society. The survey was pre-announced six months before it started in the ESO, ESMINT, and EAN newsletters. The World Health Organization (WHO)’s definition of the European region as including 51 countries was adopted. Countries with less than 100,000 inhabitants (Monaco, Liechtenstein, Andorra, and San Marino) were excluded, and North Cyprus, which was not listed under the WHO definition, was added. National stroke society chairs were invited to be country coordinators by the steering committee. In the absence of a national stroke or neurological society, national coordinators were selected by the steering committee, following a thorough review of proposals proffered by board members and/or country representatives of ESO, EAN or ESMINT. Each country coordinator was responsible for selecting two additional national stroke experts, one of whom was a neurointerventionalist, whenever possible. Coordinators and experts were responsible for identifying the most reliable and most recent national data sources (i.e. stroke registries, governmental data sources, etc.) to answer the survey questions. In the absence of national or local stroke registries, the coordinator and experts were asked to perform best estimates by consensus, and took full responsibility for the validity of the responses provided. The affiliations of the 44 coordinators and 58 experts are shown in Supplementary Appendix 1.
Data collection
The survey was drafted by the steering committee after a series of meetings, audio conferences and e-mail correspondence. Thereafter, it was externally reviewed by four stroke experts with extensive research skills and proven experience in drafting European stroke surveys (see Acknowledgments and Supplementary Appendix 1). The survey consisted of 64 items (Supplementary Appendix 2). The first section collected information on the professional background of the coordinators and experts. Subsequent sections dealt with stroke care and prehospital stroke care pathways, acute stroke treatment strategies, information on stroke registries and quality control, as well as stroke awareness campaigns. The definition of an acute SU was based on local and/or national definitions. A pilot survey was performed in Austria, Hungary, Poland, Spain and Switzerland to assess feasibility. The survey was performed between 30 October 2016 and 24 February 2017. Collected data were independently reviewed by two authors (RVM, DAS). Whenever there was ambiguity and/or missing or conflicting responses, the steering committee requested clarifications, and final approvals were granted by the steering committee.
Data analyses
Our analyses focused on access to and delivery rates of acute SU care, IVT and EVT as well as the number of centres delivering IVT and EVT. All data were analysed using appropriate descriptive methods. Whenever a response was ‘unknown’, it was eliminated. We calculated crude rates of acute SUs per one million inhabitants using United Nations population estimates (2015 Revision of World Population Prospects),17 with the exception of Serbia, for which estimates from the Statistical Office of the Republic of Serbia were used (not including Kosovo and Metohija). Similar calculations were done for annual numbers of IVT and EVT performed, and number of centres providing IVT and EVT within each country. The annual incidence of ischaemic stroke per country was based on the estimates from the Global Burden of Disease Report (2016).8 These data were used to test the associations between SUs, IVT and EVT rates per million population using Pearson correlation. We calculated the number of acute SUs necessary to reach the defined target of three acute SUs per one million inhabitants or one SU per 1000 annual incident strokes.18,19 We also calculated how many additional patients could be treated if an IVT rate of 18% could be achieved in all countries, and similar calculations were done for patients treated with EVT if an EVT rate of 5% could be achieved in all countries. Both cut-offs were data driven and were based on the next lower whole-numbered value of the three countries with highest rates. The data obtained from the survey were collated and analysed in Microsoft Excel, version 2010 (Microsoft Corporation, Redmond, WA, USA). Selected variables were imported into Stata 14 (StataCorp, College Station, TX, USA) for further analysis.
Best practice
We compared both pooled and individual national data per one million inhabitants and per annual incident ischaemic stroke rates regarding access to and delivery of SU care and IVT and EVT therapies with highest country rates.
Patient involvement
A representative from a patient organisation (SAFE) was involved in all stages of the research project (i.e. generating hypothesis, design of the survey, interpretation of the results and critical revision of the manuscript). This patient representation is intended to insure sufficient integration of the patient perspective, and better dissemination of results to patients and next of kin.
Results
Overall, 44/51 invited countries participated (Supplementary Figure 1). Seven countries did not respond to multiple attempts at contact. The total number of inhabitants in the 44 participating countries was estimated to be 835 million.17 Overall, 22 (50%) surveys were completed by a coordinator and two experts, 9 (20%) by a coordinator and one expert, and 13 (30%) by a coordinator alone.
Acute SUs, IVT hospitals and EVT centres
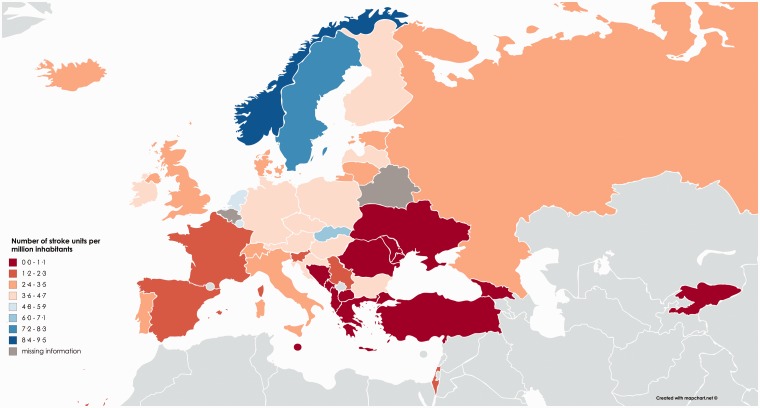
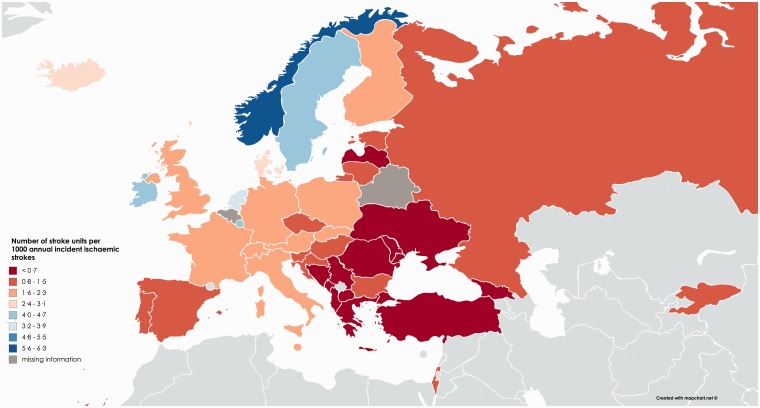
Information on acute SU care was provided for 42/44 countries. National requirements for SUs were defined in 29 countries (68%) and planned in seven countries (16%) (Supplementary Figure 2). Overall, there were 2139 acute SUs in 42 countries, corresponding to a pooled mean of 2.9 SUs per million inhabitants (95% CI; 2.3–3.6) (Table 1, Supplementary Figure 3) and 1.5 (95% CI; 1.1–1.9) per 1000 annual incident ischaemic strokes (Table 2, Supplementary Figure 6). There was a considerable heterogeneity among the 42 countries (Figures 1 and 2). Countries with highest rates had 9.2 acute SUs per one million population and 5.8 per 1000 annual incident ischaemic strokes. Ten countries had less than one acute SU per one million inhabitants.
Table 1.
Absolute and relative numbers per million inhabitants of stroke units, annual number of intravenous thrombolysis treatments (IVT), number of IVT centres, annual number of endovascular treatments (EVT) and EVT centres per country.
| Country | No. of stroke unitsa | Stroke units per million | Annual no. of IVTb | Annual no. of IVT per millionb | No. of IVT centres | IVT centres per million | Annual no. of EVTc | Annual no. of EVT per millionc | No. of EVT centres | No. of EVT centres 24/7 | EVT centres per million |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Albania | 1 | 0.3 | 0 | 0.0 | 0 | 0.0 | 6 | 2.1 | 1 | 0 | 0.3 |
| Austria | 38 | 4.4 | 3000 | 351.1 | 38 | 4.4 | 650 | 76.1 | 11 | 9 | 1.3 |
| Belarus | – | – | – | – | 12 | 1.3 | – | – | 1 | 1 | 0.1 |
| Belgium | – | – | 2250 | 199.1 | – | – | 706 | 62.5 | 17 | 12 | 1.5 |
| Bosnia andHerzegovina | 4 | 1.0 | 150 | 39.4 | 4 | 1.0 | 50 | 13.1 | 1 | 1 | 0.3 |
| Bulgaria | 30 | 4.2 | 296 | 41.4 | 28 | 3.9 | 34 | 4.8 | 4 | – | 0.6 |
| Croatia | 18 | 4.2 | 300 | 70.7 | 20 | 4.7 | 30 | 7.1 | 2 | 1 | 0.5 |
| Czech Republic | 45 | 4.3 | 3800 | 360.4 | 45 | 4.3 | 1063 | 100.8 | 15 | 15 | 1.4 |
| Denmark | 20 | 3.5 | 1632 | 287.9 | 10 | 1.8 | 280 | 49.4 | 3 | 3 | 0.5 |
| Estonia | 4 | 3.0 | 541 | 412.2 | 6 | 4.6 | 109 | 83.0 | 3 | 2 | 2.3 |
| Finland | 21 | 3.8 | 1600 | 290.7 | 21 | 3.8 | 407 | 74.0 | 5 | 5 | 0.9 |
| France | 140 | 2.2 | 8000 | 124.2 | 140 | 2.2 | 4589 | 71.3 | 37 | – | 0.6 |
| Georgia | 2 | 0.5 | 4 | 1.0 | 1 | 0.3 | 0 | 0.0 | 0 | 0 | 0.0 |
| Germany | 295 | 3.7 | 30,000 | 371.8 | 350 | 4.3 | 9000 | 111.5 | 135 | 110 | 1.7 |
| Greece | 5 | 0.4 | 225 | 20.5 | 18 | 1.6 | 40 | 3.7 | 6 | 1 | 0.5 |
| Hungary | 39 | 4.0 | 2000 | 202.9 | 39 | 4.0 | 265 | 26.9 | 6 | 3 | 0.6 |
| Iceland | 1 | 3.0 | 30 | 91.1 | 5 | 15.2 | 0 | 0.0 | 0 | 0 | 0.0 |
| Ireland | 22 | 4.7 | 550 | 117.3 | 24 | 5.1 | 210 | 44.8 | 2 | 1 | 0.4 |
| Israel | 10 | 1.2 | 1200 | 148.8 | 20 | 2.5 | 300 | 37.2 | 9 | 9 | 1.1 |
| Italy | 178 | 3.0 | 8000 | 133.8 | 182 | 3.0 | 1882 | 31.5 | 50 | 16 | 0.8 |
| Kyrgyzstan | 5 | 0.8 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0 | 0.0 |
| Latvia | 7 | 3.6 | 540 | 274.0 | 7 | 3.6 | 95 | 48.2 | 2 | 1 | 1.0 |
| Lithuania | 8 | 2.8 | 699 | 242.8 | 10 | 3.5 | 276 | 95.9 | 6 | 3 | 2.1 |
| Luxembourg | 3 | 5.3 | 30 | 52.9 | 3 | 5.3 | 3 | 5.3 | 1 | – | 1.8 |
| FYROM | 1 | 0.5 | 60 | 28.9 | 1 | 0.5 | 2 | 1.0 | 1 | 0 | 0.5 |
| Malta | 1 | 2.4 | 40 | 95.5 | 2 | 4.8 | 30 | 71.7 | 1 | 1 | 2.4 |
| Montenegro | 0 | 0.0 | 20 | 32.0 | 3 | 4.8 | 0 | 0.0 | 0 | 0 | 0.0 |
| Netherlands | 85 | 5.0 | 4821 | 284.8 | 85 | 5.0 | 1088 | 64.3 | 20 | 20 | 1.2 |
| Northern Cyprus | 2 | 6.4 | 30 | 95.7 | 2 | 6.4 | 20 | 63.8 | 2 | 2 | 6.4 |
| Norway | 48 | 9.2 | 1100 | 211.1 | 49 | 9.4 | 150 | 28.8 | 5 | – | 1.0 |
| Poland | 171 | 4.4 | 6493 | 168.2 | 171 | 4.4 | 175 | 4.5 | 21 | 4 | 0.5 |
| Portugal | 25 | 2.4 | 1516 | 146.5 | 25 | 2.4 | 845 | 81.6 | 9 | 4 | 0.9 |
| Republic of Moldova | 2 | 0.5 | 45 | 11.1 | 2 | 0.5 | 20 | 4.9 | 0 | 0 | 0.0 |
| Romania | 10 | 0.5 | 200 | 10.3 | 10 | 0.5 | 15 | 0.8 | 2 | 0 | 0.1 |
| Russia | 451 | 3.1 | 11,651 | 81.2 | 451 | 3.1 | 260 | 1.8 | 134 | 37 | 0.9 |
| Serbia | 10 | 1.4 | 400 | 56.8 | 20 | 2.8 | 10 | 1.4 | 4 | 3 | 0.6 |
| Slovakia | 36 | 6.6 | 972 | 179.1 | 44 | 8.1 | 385 | 71.0 | 7 | 3 | 1.3 |
| Slovenia | 3 | 1.5 | 400 | 193.5 | 12 | 5.8 | 142 | 69.2 | 1 | 1 | 0.5 |
| Spain | 60 | 1.3 | 5002 | 108.5 | 59 | 1.3 | 2408 | 52.2 | 37 | 35 | 0.8 |
| Sweden | 72 | 7.4 | 2600 | 265.9 | 72 | 7.4 | 390 | 39.9 | 6 | 3 | 0.6 |
| Switzerland | 23 | 2.8 | 1000 | 120.5 | 23 | 2.8 | 626 | 75.4 | 9 | 9 | 1.1 |
| Turkey | 33 | 0.4 | 1480 | 18.8 | 41 | 0.5 | 456 | 5.8 | 21 | 10 | 0.3 |
| Ukraine | 10 | 0.2 | 300 | 6.7 | 27 | 0.6 | 10 | 0.2 | 4 | – | 0.6 |
| United Kingdom | 200 | 3.1 | 10,290 | 159.0 | 200 | 3.1 | 478 | 7.4 | 28 | 2 | 0.1 |
| Total /Mean [95% CI] | 2139 | 2.9[2.3–3.6] | 113,267 | 142.0[107.4–176.7] | 2282 | 3.6[2.7–4.4] | 27,505 | 37.1[26.7–47.5] | 629 | 327 | 0.9[0.6–1.2] |
FYROM: former Yugoslav Republic of Macedonia.
aAccording to the local definition of stroke unit.
bAnnual number of intravenous thrombolysis in 2015 or 2016.
cAnnual number of endovascular treatments (EVT) for acute ischaemic stroke performed in 2016, except Denmark, Sweden and Malta (2015).
Table 2.
Relative numbers of stroke units, annual number of intravenous thrombolysis (IVT) treatments, IVT centres, annual endovascular treatment (EVT) and EVT centres per annual incident ischaemic strokes.a
| Country | Annual no. of incident ischaemic strokesa | Stroke units per 1000 ischaemic strokes | Annual no. of IVTs per 1000 ischaemic strokes | Proportion of stroke patients with IVT (%) | IVT hospitals per 1000 ischaemic strokes | Annual no. of EVTs per 1000 ischaemic strokes | Proportion of ischaemic stroke patients with EVT (%) | EVT centres per 1000 ischaemic strokes |
|---|---|---|---|---|---|---|---|---|
| Albania | 4815 | 0.2 | 0.0 | 0.0 | 0.0 | 1.2 | 0.1 | 0.2 |
| Austria | 16,314 | 2.3 | 183.9 | 18.4 | 2.3 | 39.8 | 4.0 | 0.7 |
| Belarus | 30,056 | – | – | – | 0.4 | – | - | 0.0 |
| Belgium | 19,689 | – | 114.3 | 11.4 | – | 35.9 | 3.6 | 0.9 |
| Bosnia and Herzegovina | 13,580 | 0.3 | 11.0 | 1.1 | 0.3 | 3.7 | 0.4 | 0.1 |
| Bulgaria | 28,869 | 1.0 | 10.3 | 1.0 | 1.0 | 1.2 | 0.1 | 0.1 |
| Croatia | 20,278 | 0.9 | 14.8 | 1.5 | 1.0 | 1.5 | 0.1 | 0.1 |
| Czech Republic | 30,877 | 1.5 | 123.1 | 12.3 | 1.5 | 34.4 | 3.4 | 0.5 |
| Denmark | 8339 | 2.4 | 195.7 | 19.6 | 1.2 | 33.6 | 3.4 | 0.4 |
| Estonia | 3757 | 1.1 | 144.0 | 14.4 | 1.6 | 29.0 | 2.9 | 0.8 |
| Finland | 12,685 | 1.7 | 126.1 | 12.6 | 1.7 | 32.1 | 3.2 | 0.4 |
| France | 87,372 | 1.6 | 91.6 | 9.2 | 1.6 | 52.5 | 5.3 | 0.4 |
| Georgia | 8973 | 0.2 | 0.4 | 0.0 | 0.1 | 0.0 | 0.0 | 0.0 |
| Germany | 171,801 | 1.7 | 174.6 | 17.5 | 2.0 | 52.4 | 5.2 | 0.8 |
| Greece | 22,182 | 0.2 | 10.1 | 1.0 | 0.8 | 1.8 | 0.2 | 0.3 |
| Hungary | 32,335 | 1.2 | 61.9 | 6.2 | 1.2 | 8.2 | 0.8 | 0.2 |
| Iceland | 419 | 2.4 | 71.6 | 7.2 | 11.9 | 0.0 | 0.0 | 0.0 |
| Ireland | 4809 | 4.6 | 114.4 | 11.4 | 5.0 | 43.7 | 4.4 | 0.4 |
| Israel | 7411 | 1.3 | 161.9 | 16.2 | 2.7 | 40.5 | 4.0 | 1.2 |
| Italy | 108,811 | 1.6 | 73.5 | 7.4 | 1.7 | 17.3 | 1.7 | 0.5 |
| Kyrgyzstan | 5238 | 1.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Latvia | 10,282 | 0.7 | 52.5 | 5.3 | 0.7 | 9.2 | 0.9 | 0.2 |
| Lithuania | 12,539 | 0.6 | 55.7 | 5.6 | 0.8 | 22.0 | 2.2 | 0.5 |
| Luxembourg | 700 | 4.3 | 42.9 | 4.3 | 4.3 | 4.3 | 0.4 | 1.4 |
| FYROM | 5939 | 0.2 | 10.1 | 1.0 | 0.2 | 0.3 | 0.0 | 0.2 |
| Malta | 537 | 1.9 | 74.5 | 7.4 | 3.7 | 55.9 | 5.6 | 1.9 |
| Montenegro | 1315 | 0.0 | 15.2 | 1.5 | 2.3 | 0.0 | 0.0 | 0.0 |
| Netherlands | 23,458 | 3.6 | 205.5 | 20.6 | 3.6 | 46.4 | 4.6 | 0.9 |
| Northern Cyprus | – | – | – | – | – | – | – | – |
| Norway | 8230 | 5.8 | 133.7 | 13.4 | 6.0 | 18.2 | 1.8 | 0.6 |
| Poland | 99,397 | 1.7 | 65.3 | 6.5 | 1.7 | 1.8 | 0.2 | 0.2 |
| Portugal | 18,208 | 1.4 | 83.3 | 8.3 | 1.4 | 46.4 | 4.6 | 0.5 |
| Republic of Moldova | 9592 | 0.2 | 4.7 | 0.5 | 0.2 | 2.1 | 0.2 | 0.0 |
| Romania | 79,247 | 0.1 | 2.5 | 0.3 | 0.1 | 0.2 | 0.0 | 0.0 |
| Russia | 538,984b | 0.8 | 21.6 | 2.2 | 0.8 | 0.5 | 0.0 | 0.2 |
| Serbia | 31,632 | 0.3 | 12.6 | 1.3 | 0.6 | 0.3 | 0.0 | 0.1 |
| Slovakia | 16,273 | 2.2 | 59.7 | 6.0 | 2.7 | 23.7 | 2.4 | 0.4 |
| Slovenia | 4629 | 0.6 | 86.4 | 8.6 | 2.6 | 30.7 | 3.1 | 0.2 |
| Spain | 66,594 | 0.9 | 75.1 | 7.5 | 0.9 | 36.2 | 3.6 | 0.6 |
| Sweden | 17,361 | 4.1 | 149.8 | 15.0 | 4.1 | 22.5 | 2.2 | 0.3 |
| Switzerland | 12,896 | 1.8 | 77.5 | 7.8 | 1.8 | 48.5 | 4.9 | 0.7 |
| Turkey | 69,064 | 0.5 | 21.4 | 2.1 | 0.6 | 6.6 | 0.7 | 0.3 |
| Ukraine | 160,904 | 0.1 | 1.9 | 0.2 | 0.2 | 0.1 | 0.0 | 0.0 |
| United Kingdom | 87,594 | 2.3 | 117.5 | 11.7 | 2.3 | 5.5 | 0.5 | 0.3 |
| Total /Mean [95% CI] | 1,913,985 | 1.5[1.1–1.9] | 72.7[54.2–91.2] | 7.3%[5.4–9.1] | 1.9[1.3–2.5] | 19.3[13.5–25.1] | 1.9%[1.3–2.5] | 0.4[0.3–0.5] |
FYROM: former Yugoslav Republic of Macedonia.
aAccording to Global Burden of Disease estimates (2016).8
bAccording to the local experts, the incidence of ischemic stroke is overestimated.
Figure 1.
Choropleth map showing number of stroke units per million population in 42 European countries (mean 2.9, 95% CI 2.3–3.6).
Figure 2.
Choropleth map showing number of stroke units per 1000 annual incident ischaemic strokes in 42 European countries (mean 1.5; 95% CI 1.1–1.9).
Overall, 43/44 countries reported the number of hospitals delivering IVT (Table 1). IVT was performed at 2282 hospitals, corresponding to a mean number of 3.6 (95% CI; 2.7–4.4) IVT hospitals per one million inhabitants and 1.9 (95% CI; 1.3–2.5) per 1000 annual incident ischaemic strokes. Countries with highest rates had 15.2 IVT hospitals per one million population and 11.9 per 1000 annual incident ischaemic strokes.
All countries reported the number of centres delivering EVT (Table 1). EVT was performed at 629 stroke centres, corresponding to a mean number of 0.9 (95% CI; 0.6–1.2) EVT centres per one million inhabitants and 0.4 (95% CI; 0.3–0.5) per 1000 annual incident ischaemic strokes (Table 2). Countries with highest rates had 6.4 EVT centres per one million population and 1.9 per 1000 annual incident ischaemic strokes. Twenty-nine countries had less than one stroke centre capable of performing EVT per one million inhabitants. Centres offering EVT round the clock were provided by 33 countries (Table 1). According to coordinators and experts, the available centres met the needs for EVT in 15/43 countries. In eight of the countries currently lacking full EVT coverage, it was already being planned. In the remaining 20 countries, there were no plans to provide full national access to EVT in the near future. National protocols for EVT were available in 20 countries (Supplementary Table 1 and 2).
IVT
Overall, 43/44 countries provided figures on annual IVTs performed. IVT was not available in 2/44 countries. The number of IVTs performed came from national IVT registries in 26 countries. The remaining countries provided data from national offices of statistics, service reports or estimates made by coordinators and experts. For all countries, data were from the years 2015 or 2016 (Tables 1 and 2).
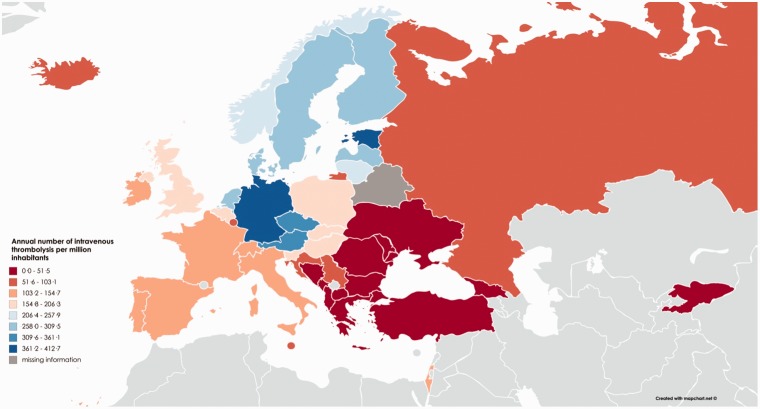
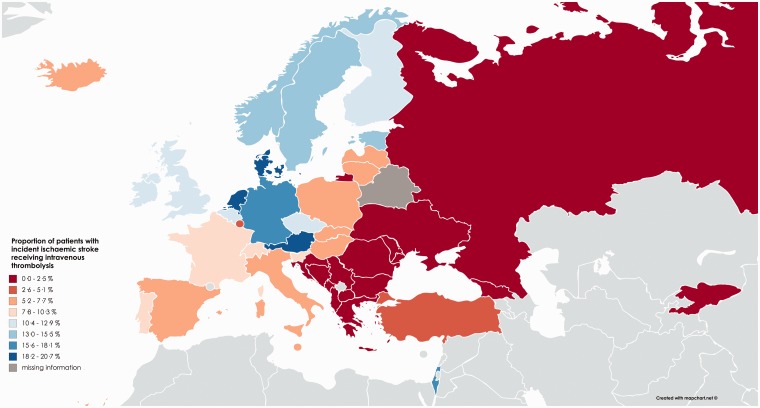
Overall, the total annual number of patients receiving IVT in 43 countries was 113,267. The estimated mean number of IVTs per one million inhabitants for these 43 countries was 142.0 (95% CI; 107.4–176.7) and 72.7 (95% CI; 54.2–91.2) per 1000 annual incident ischaemic strokes, while the highest country rates were 412.2 and 205.5, respectively (Supplementary Figure 4). In 10 countries, the estimated annual numbers of IVT treatments delivered per one million inhabitants were fewer than 50, whereas four countries had rates above 350 (Figure 3). Overall, 7.3% (95% CI; 5.4–9.1) of all patients with an ischaemic stroke in Europe received IVT, whereas 13 countries reported IVT rates of 10% or more (Table 2, Figure 4, Supplementary Figure 7).
Figure 3.
Choropleth map showing contemporary annual rates of intravenous thrombolysis (IVT) per million population in 42 European countries (mean 142.0, 95% CI 107.4–176.7).
Figure 4.
Choropleth map showing contemporary annual estimates of the proportion of patients with incident ischaemic stroke treated with intravenous thrombolysis (IVT) in 42 European countries (mean 7.3%; 95% CI 5.4–9.1).
The two most frequent reasons for not performing IVT were late patient admission (27 countries) and a lack of personnel with stroke expertise on site (15 countries). Other reasons included a lack of immediate access to brain imaging (5 countries), and a lack of a round the clock SU and/or medical laboratory availability in five countries. In Kyrgyzstan, alteplase was scheduled to be approved for the treatment of acute ischaemic stroke treatment in the near future. The cost was singled out as a barrier to providing IVT in four countries. The number of acute SUs per one million population was significantly associated with the number of IVTs delivered per million population (Pearson correlation coefficient 0.54, p = 0.0002) (Supplementary Figure 9).
EVT
EVT was available in 40/44 countries and 39 countries provided figures on annual numbers of EVTs performed. The number of EVTs performed came from national registries in 14 countries. The remaining countries provided data from national offices of statistics, service reports, extrapolation from locally obtained figures or estimates by coordinators and experts. For most countries, data were from 2016 (Tables 1 and 2).
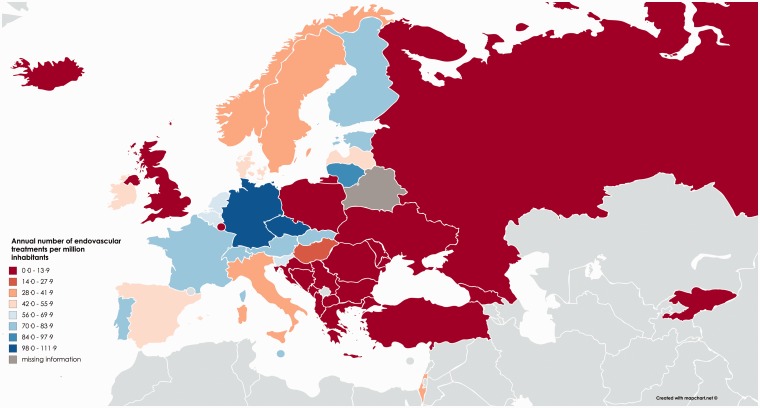
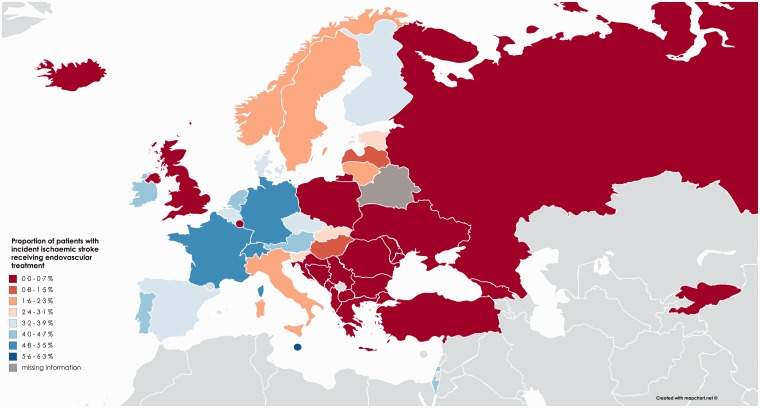
Overall, 27,505 procedures were performed, corresponding to a mean number of 37.1 procedures per one million inhabitants (95% CI; 26.7–47.5) and 19.3 (95% CI; 13.5–25.1) per 1000 annual incident ischaemic strokes, while highest country rates were 111.5 and 55.9, respectively (Supplementary Figure 5 and 8). The annual number of treatments delivered per million inhabitants was fewer than 10 per one million inhabitants in 13 countries, whereas three countries reported EVT rates above 100 per one million (Table 1, Figure 5). Overall, 1.9% (95% CI; 1.3–2.5) of all patients with an ischaemic stroke in Europe received EVT, 15 countries reported EVT rates of 3% or more (Table 2, Figure 6).
Figure 5.
Choropleth map showing contemporary annual rates of endovascular treatments (EVT) for ischaemic stroke per million population in 43 European countries (mean 37.1, 95% CI 26.7–47.5).
Figure 6.
Choropleth map showing contemporary annual estimates of the proportion of patients with incident ischaemic stroke receiving endovascular treatment (EVT) in 42 European countries (mean 1.9%; 95% CI 1.3–2.5).
The most common reasons reported for not providing EVT to all eligible patients were lack of specifically trained personnel (34 countries), lack of facilities (22 countries) and costs (16 countries). Overall, we observed that the number of EVTs delivered per one million population tended to be higher in countries with a greater number of SUs (Pearson correlation coefficient 0.36, p = 0.02).
Discussion
Our study shows that (1) for most European countries, access to and delivery of SUs, IVT and EVT are far below highest country rates and there are considerable inequalities among and within the different countries, (2) only 7.3% of all acute ischaemic stroke patients receive IVT and only 1.9% receive EVT, (3) and there is a significant correlation between the number of SUs per million inhabitants and delivery rates for both IVT and EVT.
Although there has been a dense network of SUs in northern European countries for the past two decades, no such network is present in most eastern and southern European countries. The European Brain Council has recently estimated that only one in three stroke patients in Europe has access to acute SU care.19 We have calculated that, in order to provide three SUs per one million inhabitants across Europe, at least 628 additional SUs would be needed in 20 countries (Table 3), and in order to reach one SU per 1000 annual incident ischaemic strokes, 447 SUs would be necessary in 18 countries. However, these calculations are rough estimates, based on the assumption that existing SUs are equally distributed within countries and that there is a uniform population distribution throughout Europe. In remote rural areas, more SUs might be necessary to meet the needs of the population, whereas in urban areas, high volume SUs can care for more stroke patients. Furthermore, we did not take into consideration the number of beds in the SUs and some SUs are likely to be too small to meet the needs of patients in their area. In line with the results regarding the availability of SUs, the number of EVT centres per country also varies significantly throughout Europe; 28 countries did not reach the benchmark of one CSC per one million inhabitants.20 To achieve this goal, at least 286 more CSCs delivering EVT would be needed in these 28 countries (Table 3). It is also noteworthy that some countries, as Albania, Bulgaria, Greece, Luxembourg, FYROM, Romania, Russia, Serbia and Ukraine, had a very low mean annual number of EVT per CSC. Although we recognise that in some cases this might be accounted by a low but growing case volume in recently created centres in 2016, which was a year of change in many countries regarding the organisation of EVT centres, this also indicates the need to implement basic requirements for CSC.
Table 3.
Estimated number of additional stroke units and comprehensive stroke centres required to achieve three stroke units per one million inhabitants and one comprehensive stroke centre per one million inhabitants, and estimated number of additional treatments with intravenous thrombolysis and endovascular interventions if rates of 18% and 5%, respectively, are to be achieved.
| Country | No. of additional stroke units required | No. of additional comprehensive stroke centres required | No. of additional intravenous thrombolysis treatments per year(target rate 18%) | No. of additional endovascular treatments per year(target rate 5%) |
|---|---|---|---|---|
| Albania | 8 | 2 | 867 | 235 |
| Austria | 0 | 0 | 0 | 166 |
| Belarus | – | 8 | – | – |
| Belgium | – | 0 | 1294 | 278 |
| Bosnia and Herzegovina | 7 | 3 | 2294 | 629 |
| Bulgaria | 0 | 3 | 4900 | 1409 |
| Croatia | 0 | 2 | 3350 | 984 |
| Czech Republic | 0 | 0 | 1758 | 481 |
| Denmark | 0 | 3 | 0 | 137 |
| Estonia | 0 | 0 | 135 | 79 |
| Finland | 0 | 1 | 683 | 227 |
| France | 53 | 27 | 7727 | 0 |
| Georgia | 10 | 4 | 1611 | 449 |
| Germany | 0 | 0 | 924 | 0 |
| Greece | 28 | 5 | 3768 | 1069 |
| Hungary | 0 | 4 | 3820 | 1352 |
| Iceland | 0 | 0 | 45 | 21 |
| Ireland | 0 | 3 | 316 | 30 |
| Israel | 14 | 0 | 134 | 71 |
| Italy | 1 | 10 | 11,586 | 3559 |
| Kyrgyzstan | 13 | 6 | 943 | 262 |
| Latvia | 0 | 0 | 1311 | 419 |
| Lithuania | 1 | 0 | 1558 | 351 |
| Luxembourg | 0 | 0 | 96 | 32 |
| FYROM | 5 | 1 | 1009 | 295 |
| Malta | 0 | 0 | 57 | 0 |
| Montenegro | 2 | 1 | 217 | 66 |
| Netherlands | 0 | 0 | 0 | 85 |
| Northern Cyprus | 0 | 0 | – | – |
| Norway | 0 | 0 | 381 | 262 |
| Poland | 0 | 18 | 11,398 | 4795 |
| Portugal | 6 | 1 | 1761 | 65 |
| Republic of Moldova | 10 | 4 | 1682 | 460 |
| Romania | 49 | 18 | 14,064 | 3947 |
| Russia | 0 | 9 | 85,366a | 26,689a |
| Serbia | 11 | 3 | 5294 | 1572 |
| Slovakia | 0 | 0 | 1957 | 429 |
| Slovenia | 3 | 1 | 433 | 89 |
| Spain | 78 | 9 | 6985 | 922 |
| Sweden | 0 | 4 | 525 | 478 |
| Switzerland | 2 | 0 | 1321 | 19 |
| Turkey | 203 | 58 | 10,952 | 2997 |
| Ukraine | 124 | 41 | 28,663 | 8035 |
| United Kingdom | 0 | 37 | 5477 | 3902 |
| Total | 628 | 286 | 226,662 | 67,347 |
FYROM: former Yugoslav Republic of Macedonia.
aAccording to the local experts, the incidence of ischemic stroke is overestimated.
Governments, health care professionals and stroke specialists should now carefully plan and implement networks of SUs providing IVT and CSCs delivering EVT, taking into account geographical conditions and regional and local characteristics while still being affordable. CSCs will require round the clock stroke physicians with expertise in endovascular stroke management, and fully trained neurointerventionalists with qualifications based on current models of certification.21,22 Too many competing EVT centres will not be cost-effective, will compromise quality and will dilute the expertise of specialists. Universal adoption of a uniform definition of SUs and CSCs together with an appropriate certification process would help to guarantee the achievement of set quality targets throughout Europe.
IVT and EVT
Overall, 7.3% of all patients received IVT and 1.9% EVT. So far, population-based studies on IVT and EVT rates are scarce and there are no established and well-accepted benchmarks for determining what proportion of patients with acute ischaemic stroke should receive IVT and EVT. The burden of stroke report provided thrombolysis rates in national and large regional audits, but the denominator of populations varied between ‘all stroke patients’, ‘all ischaemic stroke patients’, ‘hospitalised stroke patients’, ‘stroke unit patients’ and others, making reliable comparisons impossible.9 Furthermore, using hospitalised stroke patients as the denominator can be misleading, since hospitalisation rates for stroke vary across Europe.9 In the same report, average annual thrombolysis rates per 100,000 population were only provided for 11 countries, within different time frames. The denominators of our survey were the population at risk and the number of incident ischaemic strokes, based on the 2015 Global Burden of Disease Report.8 Highest practice rate for IVT was 20.6%, whereas 13 countries had IVT rates of 10% or more. Highest EVT rates were 5%, with 15 countries achieving 3% or more. The estimated number of additional patients who could be treated with IVT taking 18% as the threshold is 226,662, and the estimated number of additional patients who could be treated with EVT at a threshold of 5% is 67,347 (Table 3). However, these are still rather conservative estimates, since even the IVT and EVT rates in countries with the highest rates can be improved. In Germany, for instance, only 60% of eligible patients were reported to have been treated by IVT in 2012.9 Based on the available evidence from intervention trials and prospective registries for EVT, a recent study in the UK has estimated that approximately 10% of stroke patients admitted to hospital were eligible for EVT.23
Implications
Our findings have implications for the future organisation of acute stroke care in Europe as we have shown in which countries rates of SUs, IVT and EVT are currently below best practice. In 2006, the second Helsingborg Declaration, co-sponsored by the WHO Regional Office for Europe, set new targets for stroke management and care.24 One specific goal for 2015 was that all patients with acute stroke who were potentially eligible for acute, specific treatment, were transferred to hospitals with adequate capacity and expertise to administer treatments – defined as a SU or stroke dedicated area. Our survey shows that many patients still have no access to appropriate acute stroke treatment and a clear action plan to address these inequalities is urgently needed. Therefore, a third Action Plan for Stroke in Europe is currently being drafted to set achievement goals for 2030 and the present survey will provide important information for future health care planning. By increasing the awareness of what needs to change, this knowledge may also be useful for local and national stroke patient and professional organisations, in order to develop tailored approaches that consider the specific barriers faced by national healthcare systems and take the first vital steps to improve overall stroke care. To develop a successful strategy for change, you need to understand the types of barriers faced in healthcare. Using this data, you can consider which barriers and levers may operate in your organisation and which may be relevant to a particular problem. Following careful analysis, it is possible to develop a tailored approach to overcome the barriers, encourage changes in behaviour and ultimately implement guidance.
Strengths and limitations
A major strength of our survey – apart from the large number of participating countries – is that data were mostly based on national stroke registries. Furthermore, the survey questions were answered by experienced stroke and neurointerventional experts. Our survey does, however, have several important limitations: (1) The population density is not reflected in the survey owing to the lack of well-established indicators for each individual European country. (2) Several countries lack prospective stroke registries and coordinators and experts had to use multiple sources of regional and local information to extrapolate national figures. (3) Given the lack of a uniform definition of SUs, some differences in SU rates are likely to be related to differences in definitions. Furthermore, we did not assess the number of patients treated in SUs. (4) Estimated stroke incidence rates of the 2015 Global Burden of Disease Report – the most accepted global data on stroke incidence – might eventually be too high for some countries, while for other countries, rates might be too low. We have therefore presented data both ways, per one million inhabitants and per 1000 annual incident ischaemic strokes. Finally, the methods used to collect information in countries lacking national stroke registries were not standardised and therefore in these cases, data should be seen as exploratory. The development of stroke registries, internal and external audits in those countries should be a goal, in order to improve the quality of data gathered. However, since in most cases this is not expected to happen in the near future, we do believe that communication of those preliminary results provides the opportunity to highlight the need for change and can lead to effective results.
Conclusions
This is the first comprehensive survey on access to and delivery rates of acute SU care, IVT and EVT in Europe. We found major inequalities in treatment of acute stroke patients between and within 44 European countries, and in many countries rates are far below highest country rates, leaving many patients untreated. Individual country level data indicate where access to and delivery of acute stroke care is insufficient or lacking and allows comparison with highest country rates. These data will support governments, health care providers and European politicians to draw up action plans to implement acute stroke treatment, tailored for each European country, in order to reduce stroke-related mortality and morbidity in Europe.
Supplemental Material
Supplemental material, Supplemental appendix for Access to and delivery of acute ischaemic stroke treatments: A survey of national scientific societies and stroke experts in 44 European countries by Diana Aguiar de Sousa, Rascha von Martial, Sònia Abilleira, Thomas Gattringer, Adam Kobayashi, Miquel Gallofré, Franz Fazekas, Istvan Szikora, Valery Feigin, Valeria Caso and Urs Fischer in European Stroke Journal
Supplemental Material
Supplemental material, Supplemental Table for Access to and delivery of acute ischaemic stroke treatments: A survey of national scientific societies and stroke experts in 44 European countries by Diana Aguiar de Sousa, Rascha von Martial, Sònia Abilleira, Thomas Gattringer, Adam Kobayashi, Miquel Gallofré, Franz Fazekas, Istvan Szikora, Valery Feigin, Valeria Caso and Urs Fischer in European Stroke Journal
Acknowledgements
We thank Bo Norrving, Didier Leys, Kennedy Lees, M and Turgut Tatlisumak for their useful comments regarding the questionnaire, data collection methodology and policy implications of this paper. We thank Susan Edith Kaplan for editorial comments.
“ESO ESMINT EAN SAFE Survey on Stroke Care in Europe” collaborators
M Petrela, O Taka, E Enesi (Albania); S Kiechl, M Brainin, F Fazekas (Austria); P Konovalov (Belarus); A Peeters, G Vanhooren, L Defreyne (Belgium); H Haris, M Moranjkic (Bosnia and Herzegovina); S Andonova, I Staikov (Bulgaria); H Budincevic, D Ozretic, B Malojčić (Croatia); A Tomek (Czech Republic); H Iversen, SP Jonhsen (Denmark); J Korv, R Vibo, V Malikov (Estonia); T Sairanen, D Strbian, K Lappalainen (Finland); S Timsit, E Touze, D Leys (France); A Tsiskaridze, I Burduladze (Georgia); M Dichgans, J Röther, J Fiehler (Germany); G Tsivgoulis, E Brountzos (Greece); D Bereczki. C Óváry, I Szikora (Hungary); B Thorarinsson, V Vilmarsson (Iceland); J Harbison (Ireland); N Bornstein, D Tanne, A Horev (Israel); D Toni, S Mangiafico, V Caso (Italy); A Murzaliev, I Lutsenko, A Artykbaev, (Kyrgyzstan); E Miglãne, K Kupcs, I Kikule (Latvia); D Jatuzis, D Rastenyte, M Kurminas (Lithuania); D Ulbricht (Luxembourg); A Arsovska, M Smiceska, E Lickova (The former Yugoslav Republic of Macedonia); M Mallia, R Grech, M Schembri (Malta); V Lisnic, E Manole, E Zota (Moldova); M Cukic (Montenegro); D Dippel, C Majoie, H B van der Worp (Netherlands); S Akpinar (Northern Cyprus); E Berge, Hanne Ellekjær (Norway); A Czlonkowska, W Poncyljusz, A Kobayashi (Poland); E Azevedo, V Tedim-Cruz, M Ribeiro (Portugal); C Tiu (Romania); T Kharitonova (Russia); L Bumbasirevic (Serbia); Z Gdovinova, I Vulev, P Turcani (Slovakia); B Zvan, V Svigelj, Z Milosevic (Slovenia); J Gállego, M Rodríguez Yáñez, E Palacio-Portilla, A Gonzallez Mandly, M Gallofré, S Abilleira, C Gimenez, S Calleja-Puerta, J Marta-Moreno, M Óscar Ayo, A Lago (Spain); M Arnold (Switzerland); M Mazya, T Moreira (Sweden); N Uzuner, L Gungor, O Ozdemir (Turkey); H Rodgers, J Dawson, P White (United Kingdom); Y Flomin, D Shcheglov (Ukraine).
Declaration of Conflicting Interests
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Diana Aguiar de Sousa, Rascha von Martial, Thomas Gattringer, Adam Kobayashi, Miquel Gallofré, Franz Fazekas, Valery Feigin and Valeria Caso: nothing to disclose.
Sònia Abilleira: Co-Principal Investigator of the RACECAT trial (NCT02795962).
Istvan Szikora: First Past President of the European Society of Minimally Invasive Neurological Therapy (ESMINT), investigator in the TREVO Registry, consultant to Medtronic Neurovascular, Stryker Neurovascular, Codman Neurovascular and Sequent Medical, outside the submitted work.
Urs Fischer: Secretary General of the European Stroke Organisation. Received research grants from the Swiss National Science Foundation and the Swiss Heart Foundation. He is principal investigator of the SWITCH trial, the ELAN trial and the SWIFT DIRECT trial. Received consultancy for Medtronic/Covidien.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research received no specific grant from any funding agency in the public, commercial, or not-forprofit sectors.
Ethical approval
Not required.
Informed consent
The lead author (UF) affirms that this manuscript is an honest, accurate and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned have been explained. All authors, external and internal, had full access to all of the data (including statistical reports and tables) in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis.
Guarantor
Urs Fischer is the study guarantor.
Contributorship
Idea and concept: Urs Fischer, Valeria Caso.
Study design: Urs Fischer, Valeria Caso, Diana Aguiar de Sousa, Sònia Abilleira, Thomas Gattringer, Adam Kobayashi, Miquel Gallofré, Franz Fazekas, Istvan Szikora.
Design of the questionnaire: Urs Fischer, Valeria Caso, Diana Aguiar de Sousa, Sònia Abilleira, Thomas Gattringer, Adam Kobayashi, Miquel Gallofré, Franz Fazekas, Istvan Szikora.
Literature search: Diana Aguiar de Sousa, Urs Fischer.
Figures: Diana Aguiar de Sousa.
Data collection: Rascha von Martial, Diana Aguiar de Sousa, Valery Feigin, Urs Fischer.
Data analysis: Rascha von Martial, Diana Aguiar de Sousa.
Data interpretation: Rascha von Martial, Diana Aguiar de Sousa, Urs Fischer, Sònia Abilleira, Thomas Gattringer, Adam Kobayashi, Miquel Gallofré, Franz Fazekas, Istvan Szikora.
Writing: Urs Fischer, Diana Aguiar de Sousa, Valeria Caso.
Editorial comments: Susan Edith Kaplan.
Relevant intellectual inputs to the manuscript: Sònia Abilleira, Rascha von Martial, Thomas Gattringer, Adam Kobayashi, Miquel Gallofré, Franz Fazekas, Istvan Szikora, Valery Feigin.
References
- 1.European Heart Network. European cardiovascular disease statistics. Brussels: European Heart Network, 2017. [Google Scholar]
- 2.Townsend N, Wilson L, Bhatnagar P, et al. Cardiovascular disease in Europe: epidemiological update 2016. Eur Heart J 2016; 37: 3232–3245. [DOI] [PubMed] [Google Scholar]
- 3.Feigin VL, Lawes CM, Bennett DA, et al. Worldwide stroke incidence and early case fatality reported in 56 population-based studies: a systematic review. Lancet Neurol 2009; 8: 355–369. [DOI] [PubMed] [Google Scholar]
- 4.Heuschmann PU, Wiedmann S, Wellwood I, et al. Three-month stroke outcome: the European Registers of Stroke (EROS) investigators. Neurology 2011; 76: 159–165. [DOI] [PubMed] [Google Scholar]
- 5.Truelsen T, Piechowski-Jozwiak B, Bonita R, et al. Stroke incidence and prevalence in Europe: a review of available data. Eur J Neurol 2006; 13: 581–598. [DOI] [PubMed] [Google Scholar]
- 6.Feigin VL, Norrving B, Mensah GA. Global burden of stroke. Circ Res 2017; 120: 439–448. [DOI] [PubMed] [Google Scholar]
- 7.GBD 2015 Mortality and Causes of Death Collaborators. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016; 388: 1459–1544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Feigin VL, Roth GA, Naghavi M, et al. Global burden of stroke and risk factors in 188 countries, during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet Neurol 2016; 15: 913–924. [DOI] [PubMed] [Google Scholar]
- 9.Stevens E, Emmett E, Wang Y, et al. The burden of stroke in Europe. London: Stroke Alliance for Europe, 2017. [Google Scholar]
- 10.Langhorne P, Williams BO, Gilchrist W, et al. Do stroke units save lives? Lancet 1993; 342: 395–398. [DOI] [PubMed] [Google Scholar]
- 11.Jørgensen HS, Nakayama H, Raaschou HO, et al. The effect of a stroke unit: reductions in mortality, discharge rate to nursing home, length of hospital stay, and cost. Stroke 1995; 26: 1178–1182. [DOI] [PubMed] [Google Scholar]
- 12.Indredavik B, Bakke F, Slordahl SA, et al. Stroke unit treatment. 10-year follow-up. Stroke 1999; 30: 1524–1527. [DOI] [PubMed] [Google Scholar]
- 13.Emberson J, Lees KR, Lyden P, et al. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet 2014; 384: 29–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goyal M, Menon BK, van Zwam WH, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet 2016; 387: 1723–1731. [DOI] [PubMed] [Google Scholar]
- 15.Wahlgren N, Moreira T, Michel P, et al. ESO-KSU, ESO, ESMINT, ESNR and EAN Mechanical thrombectomy in acute ischemic stroke: consensus statement by ESO-Karolinska Stroke Update 2014/2015, supported by ESO, ESMINT, ESNR and EAN. Int J Stroke 2016; 11: 134–147. [DOI] [PubMed] [Google Scholar]
- 16.Fiehler J, Cognard C, Gallitelli M, et al. European recommendations on organisation of interventional care in acute stroke (EROICAS). Int J Stroke 2016; 11: 701–716. [DOI] [PubMed] [Google Scholar]
- 17.United Nations, Department of Economic and Social Affairs, Population Division World population prospects: the 2015 revision – key findings and advance tables. United Nations, New York, 2015.
- 18.Warlow C, Sudlow C, Dennis M, et al. Stroke. Lancet 2003; 362: 1211–1224. [DOI] [PubMed] [Google Scholar]
- 19.Quoidbach V, Esposito G, Destrebecq F, et al. Policy white paper towards optimizing research and care for brain disorders. Brussels: European Brain Council, 2017. [Google Scholar]
- 20.Grotta JC, Hacke W. Stroke neurologist's perspective on the new endovascular trials. Stroke 2015; 46: 1447–1452. [DOI] [PubMed] [Google Scholar]
- 21.Ringelstein EB, Müller-Jensen A, Nabavi DG, et al. Comprehensive stroke unit. Nervenarzt 2011; 82: 778–784. [DOI] [PubMed] [Google Scholar]
- 22.Lavine SD, Cockroft K, Hoh B, et al. Training guidelines for endovascular stroke intervention: an international multi-society consensus document. Intervent Neurol 2016; 5: 51–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McMeekin P, White P, Martin AJ, et al. Estimating the number of UK stroke patients eligible for endovascular thrombectomy. Eur Stroke J 2017; 2: 319–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kjellström T, Norrving B, Shatchkute A. Helsingborg declaration 2006 on European stroke strategies. Cerebrovasc Dis 2007; 23: 231–241. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Supplemental appendix for Access to and delivery of acute ischaemic stroke treatments: A survey of national scientific societies and stroke experts in 44 European countries by Diana Aguiar de Sousa, Rascha von Martial, Sònia Abilleira, Thomas Gattringer, Adam Kobayashi, Miquel Gallofré, Franz Fazekas, Istvan Szikora, Valery Feigin, Valeria Caso and Urs Fischer in European Stroke Journal
Supplemental material, Supplemental Table for Access to and delivery of acute ischaemic stroke treatments: A survey of national scientific societies and stroke experts in 44 European countries by Diana Aguiar de Sousa, Rascha von Martial, Sònia Abilleira, Thomas Gattringer, Adam Kobayashi, Miquel Gallofré, Franz Fazekas, Istvan Szikora, Valery Feigin, Valeria Caso and Urs Fischer in European Stroke Journal