Short abstract
Introduction
The purpose of this study is to investigate which factors are associated with physiotherapy provision to hospitalised stroke patients.
Methods
Data were analysed for stroke patients admitted to hospital in England and Wales between April 2013 and March 2017 recorded on the Sentinel Stroke National Audit Programme (SSNAP) national stroke register. Associations between different patient factors, and applicability for and intensity of physiotherapy were measured using multi-level logistic and regression models.
Findings: Data from 306,078 patients were included on the SSNAP register. Median age was 77 years (IQR 67–85) and 84.7% of patients with completed stroke severity data had a mild-moderate stroke. In all, 85.2% of patients recorded on SSNAP were deemed applicable for physiotherapy. Applicability for physiotherapy was 47% higher among thrombolysed patients (aOR 1.47, 95% CI 1.40–1.54), 36% lower in those with severe pre-morbid disability (aOR 0.64, 95% CI 0.58–0.71) and more than 2.5-fold higher among patients admitted to hospitals with greater availability of early supported discharge (aOR 2.62, 95% CI 1.28–5.37). Patients who were younger, male, had less pre-morbid disability, lower stroke severity, sustained an infarction, received thrombolysis, and had fewer medical complications were more likely to receive more intensive physiotherapy post-stroke.
Conclusion
Several patient and service organisational factors are associated with physiotherapy provision to stroke patients, some of which may not be justifiable. Physiotherapists should be aware of these factors when planning and delivering physiotherapy as well as any possible biases associated with physiotherapy provision to patients post-stroke.
Keywords: SSNAP, stroke, physiotherapy, rehabilitation, stroke unit, intensity
Introduction
Stroke is one of the most common causes of death and disability globally.1,2 Due to the high burden caused by stroke, there is a strong argument to implement early interventions designed to optimise recovery after stroke. It is accepted that patients who receive organised inpatient stroke unit care are more likely to be alive, independent and living at home one year after a stroke compared to patients cared for on general medical wards.3 Physiotherapy, a recognised core component of stroke care, aims to optimise physical function post-stroke.4 Whilst there is evidence to suggest that intensive, repetitive, task-orientated physiotherapy results in improved functional outcomes post-stroke,4 it is not clear from the literature which aspects of physiotherapy, such as session frequency or length, result in improved outcomes. It is also unclear how patients with different characteristics respond to these aspects of physiotherapy. If this evidence was available, physiotherapy sessions could be individually tailored to a patient’s clinical presentation to optimise recovery.
Previous studies have investigated whether different factors influence the amount of physiotherapy patients receive post-stroke. These factors included patient demographics, such as age and gender,5–9 as well as stroke characteristics, particularly stroke severity and its associated neurological impairments (limb weakness, walking ability and neglect).8–15 However, these studies analysed data from either very small patient samples or larger patient samples with limited details of physiotherapy provision. As such, findings from these studies may not be generalisable to the wider stroke population or clinically useful to aid understanding of physiotherapy provision post-stroke. Other factors that could influence physiotherapy provision that have not been previously investigated include stroke subtype (ischaemic or haemorrhagic), use of thrombolysis, co-morbidities and post-discharge therapy support. Therefore, investigating these factors with a larger patient sample and with more detail regarding physiotherapy provision is warranted.
The aim of this study was to identify which factors are associated with physiotherapy provision to hospitalised stroke patients using a large national stroke patient register. As this register records data on applicability for physiotherapy, total number of physiotherapy minutes provided to patients and physiotherapy intensity, the study had three main hypotheses related to these aspects:
As applicability for physiotherapy would be primarily determined by clinical need for physiotherapy, there would be no difference in applicability based on age, gender, stroke type (ischaemic or haemorrhagic), presence of medical complications or availability of early supported discharge (ESD) rehabilitation, but there would be lower applicability if patients presented with very mild or very severe stroke severity, high levels of pre-morbid disability, and had very short lengths of hospital stay (LOS).
As more physiotherapy minutes in hospital would be primarily determined by a greater need for physiotherapy to optimise physical function, there would be no difference in receiving more physiotherapy minutes based on age, gender, stroke type, or presence of medical complications but patients with greater stroke severity, lower pre-morbid disability, longer LOS and lower ESD availability would receive more physiotherapy minutes.
As physiotherapy intensity would be primarily determined by a patient’s ability to participate in rehabilitation, there would be no difference in receiving more intensive physiotherapy based on gender or ESD availability but patients with younger age, lower pre-morbid disability and stroke severity, having an infarct and having fewer medical complications would receive more intensive physiotherapy.
Methods
Data sources and case ascertainment
Data were collected from the Sentinel Stroke National Audit Programme (SSNAP), the national stroke register of England, Wales and Northern Ireland. SSNAP includes patients treated in hospital with acute ischaemic stroke or primary intracerebral haemorrhage. All acute admitting hospitals participate, and data are entered by the clinical teams treating the patient onto a secure webtool with real time data validations to ensure data quality. Permission to collect patient data without explicit consent was granted by the Ethics and Confidentiality Committee of the National Information Governance Board. Overall case ascertainment in SSNAP for hospitalised stroke is estimated to be 90–95%.16 The study cohort included patients in England and Wales aged ≥16 treated in hospital with acute ischaemic stroke or primary intracerebral haemorrhage between 1 April 2013 and 31 March 2017.
In the UK, inpatient stroke care is funded through the public health service (National Health Service) and delivered by medical, nursing and therapy staff. Therapy treatment is determined by the treating therapist following patient assessment rather than by the physician. Whilst SSNAP records data for all therapies (physiotherapy, occupational therapy, and speech and language therapy), only physiotherapy data were analysed in this study. SSNAP records data on the date and time of first physiotherapy assessment, number of days physiotherapy was provided, and total number of physiotherapy minutes provided over a patient’s hospital stay. SSNAP does not record details of therapy treatment (e.g. session content, number of staff treating patients).
In this study, physiotherapy provision was defined as:
applicability for physiotherapy at any point during a patient’s inpatient stay
total number of physiotherapy minutes provided to a patient during their inpatient stay
intensity of physiotherapy provided to the patient
Physiotherapy applicability
Applicability for physiotherapy is defined as whether the patient, following an initial physiotherapy assessment, requires physiotherapy at any time during their hospital admission. Whilst applicability for physiotherapy is decided by the individual physiotherapists or clinical teams treating the patient, patients with no neurological deficits, no limitations of physical function or who require end of life care upon arrival to hospital are usually considered to be not applicable for physiotherapy. The adjusted likelihoods of being deemed applicable for physiotherapy were estimated by fitting multilevel logistic regression models with random intercepts to take account of clustering at the hospital level. Models were adjusted for age, sex, pre-stroke disability (measured using the modified Rankin Scale score, mRS), prior comorbidities, stroke onset whilst already an inpatient, stroke severity, stroke type and treatment with thrombolysis, urinary tract infection (UTI) or pneumonia within the first seven days of stroke, LOS, and availability of ESD. Stroke severity was measured using the admission National Institutes of Health Stroke Scale (NIHSS) score and analysis was restricted to the 83% of patients with a fully completed NIHSS score. ESD availability for each patient was estimated as the proportion of patients discharged to a stroke specialised ESD service for each admitting hospital. Age, LOS, and NIHSS were included as restricted cubic splines with five knots due to the non-linearity of these variables. The variables included in each model were determined a priori as reducing the number of variables included in each model was not necessary due to the large dataset.
Total physiotherapy minutes
The log-transformed number of physiotherapy minutes received by patients considered applicable for physiotherapy was estimated by fitting linear regression models, using the clustered sandwich estimator to take account of clustering at the hospital level. Models were adjusted for age, sex, pre-stroke disability, prior comorbidities, stroke onset whilst already an inpatient, stroke severity, stroke type and treatment with thrombolysis, UTI or pneumonia within the first seven days of stroke, LOS, and ESD availability. Age, ESD availability, LOS and NIHSS were included as restricted cubic splines with five knots due to the non-linearity of these variables.
Physiotherapy intensity
Physiotherapy intensity was measured as the total number of physiotherapy minutes provided divided by the patient’s overall LOS, for patients deemed applicable for physiotherapy. The log of intensity was estimated by fitting linear regression models, using the clustered sandwich estimator to take account of clustering at the hospital level. Models were adjusted for age, sex, pre-stroke disability, prior comorbidities, stroke onset whilst already an inpatient, stroke severity, stroke type and treatment with thrombolysis, UTI or pneumonia within the first seven days of stroke, and ESD availability discharge. Age, ESD availability, and NIHSS were included as restricted cubic splines with five knots due to the non-linearity of these variables.
Sensitivity analyses
Sensitivity analyses were performed for missing data according to different predefined populations including excluding patients who died in hospital within seven days of arrival and measuring stroke severity categorically as either groups of the fully completed NIHSS, or level of consciousness where NIHSS was incomplete.
STROBE statement
As recommended in the writing of observational research, the STROBE statement was used to guide the reporting of this observational study.17
Statistical software
Analyses were carried out using Stata 14 MP.
Results
Patient characteristics
Data from 306,078 patients were recorded on SSNAP between 1 April 2013 and 31 March 2017 (Table 1). Median age was 77 years (IQR 67–85) and 246,479 (80.5%) of patients were functionally independent prior to their stroke (mRS 0–2). Data from patients with a completed NIHSS score (n = 253,672) were included in the regression analyses and 84.7% of patients had a mild or moderate stroke (NIHSS <16).
Table 1.
Patient characteristics recorded on SSNAP.
| Patient characteristics on SSNAP | n (%) |
|---|---|
| Age | |
| <60 | 43,694 (14.3) |
| 60–69 | 49,392 (16.1) |
| 70–79 | 81,329 (26.6) |
| 80–89 | 96,926 (31.7) |
| >90 | 34,737 (11.3) |
| Gender | |
| Female | 152,005 (49.7) |
| Male | 154,073 (50.3) |
| Pre-morbid mRS | |
| 0 | 169,632 (55.4) |
| 1 | 45,700 (14.9) |
| 2 | 31,147 (10.2) |
| 3 | 35,418 (11.6) |
| 4 | 18,660 (6.1) |
| 5 | 5521 (1.8) |
| Stroke Subtype | |
| Infarction | 267,819 (87.5) |
| Intracerebral haemorrhage | 38,259 (12.5) |
| Admission NIHSS Categorya | |
| 0 | 17,224 (6.8) |
| 1–4 | 109,247 (43) |
| 5–9 | 58,860 (23.2) |
| 10–15 | 29,636 (11.7) |
| 16–20 | 17,894 (7.1) |
| 21–42 | 20,811 (8.2) |
mRS: Modified Rankin Scale; NIHSS: National Institutes of Health Stroke Scale.
aNIHSS category only listed if fully completed; n = 253,672.
Applicability for physiotherapy
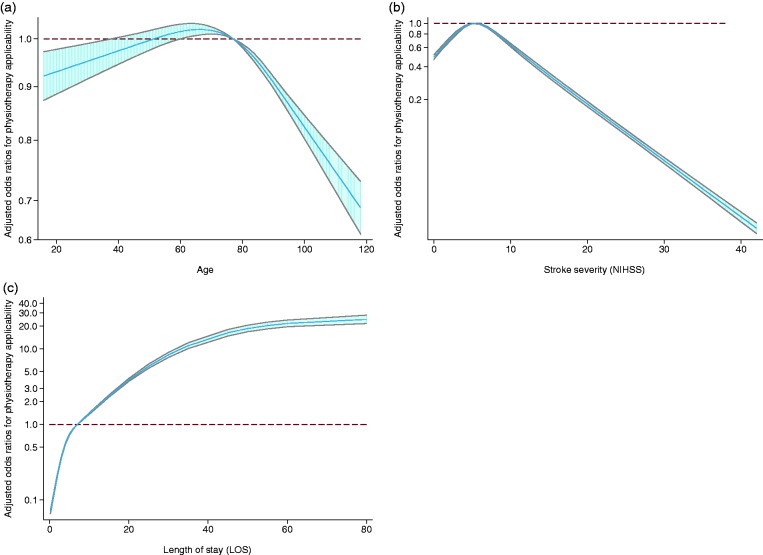
In all, 85.2% of patients registered on the SSNAP register were considered applicable for physiotherapy (Figure 1, Table 2). As hypothesised, patients with very mild or very severe stroke severity, severe pre-morbid disability and shorter LOS (<7 days) were deemed less applicable for physiotherapy. In addition, approximately 12.5% of patients developed a medical complication within the first seven days of hospitalisation and there was no difference in applicability for physiotherapy if a patient had a medical complication in the first seven days of hospitalisation.
Figure 1.
Adjusted odds of applicability for physiotherapy according to (a) age, (b) stroke severity, and (c) length of stay.
Table 2.
Adjusted odds of applicability for physiotherapy according to different patient and service factors.
| Applicability for physiotherapyn = 252,758. Clusters = 205 hospitals |
||
|---|---|---|
| Outcome | Adjusted Odds Ratio | 95% Confidence Interval |
| Age | See spline diagram | |
| Sex | 1.03 | 1.01–1.06 |
| Stroke subtype (infarction without thrombolysis as reference) | ||
| Infarction with thrombolysis | 1.47 | 1.40–1.54 |
| Intracerebral haemorrhage | 0.56 | 0.53–0.58 |
| Pre-morbid mRS (mRS=0 as reference) | ||
| 1 | 1.10 | 1.06–1.15 |
| 2 | 1.09 | 1.03–1.14 |
| 3 | 1.02 | 0.96–1.06 |
| 4 | 0.87 | 0.81–0.93 |
| 5 | 0.64 | 0.58–0.71 |
| UTI or pneumonia in the first seven days | 1.06 | 0.99–1.11 |
| Co-morbidities | ||
| Congestive heart failure | 0.98 | 0.92–1.04 |
| Hypertension | 1.05 | 1.02–1.08 |
| Atrial fibrillation | 0.95 | 0.92–0.99 |
| Diabetes | 1.02 | 0.99–1.06 |
| Prior stroke/transient ischaemic attack | 1.02 | 0.99–1.06 |
| Stroke onset while already an inpatient | 0.61 | 0.56–0.65 |
| Admitting hospital’s availability of ESD | 2.62 | 1.28–5.37 |
| Stroke severity | See spline diagram | |
| Length of stay | See spline diagram | |
| Intercept | 0.23 | 0.17–0.31 |
ESD: early supported discharge.
Contrary to our hypothesis, there were differences in applicability based on age, gender, stroke type and availability of ESD. Patients aged between 70 and 80 had the highest adjusted odds of applicability, with younger and older patients having lower odds. Male patients were slightly more likely to be considered applicable for physiotherapy compared to female patients, but this difference was not seen when data for patients who died within seven days of hospital arrival were excluded (aOR 1.01 95% CI 0.98–1.04, p = 0.403). Compared to patients with non-thrombolysed ischaemic stroke, patients with haemorrhagic stroke were less likely and patients with thrombolysed ischaemic stroke were more likely to be considered applicable for physiotherapy. There was a much higher likelihood of a patient being considered applicable for physiotherapy if the hospital patients were admitted to have greater availability of ESD.
Total physiotherapy minutes
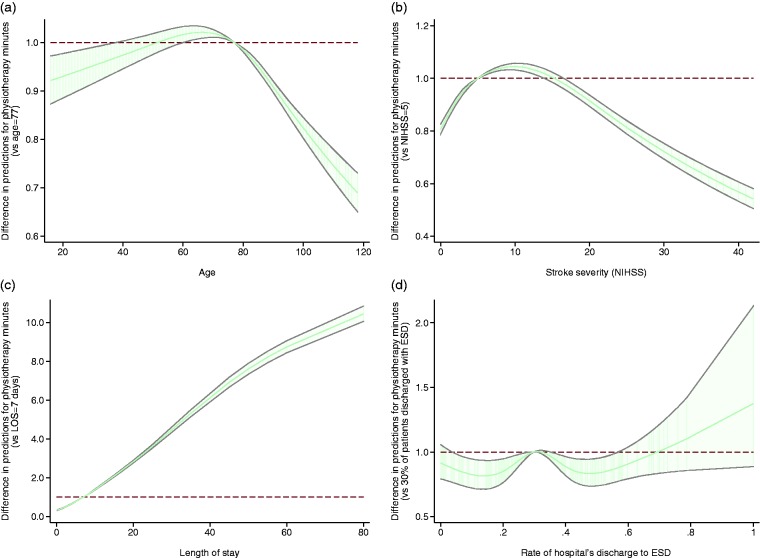
As hypothesised, there was no difference in receiving more physiotherapy minutes based on stroke type, although patients with thrombolysed ischaemic stroke were more likely to receive more physiotherapy minutes than patients who were not thrombolysed (Figure 2, Table 3). As LOS increased, the likelihood of receiving more physiotherapy minutes significantly increased (p < 0.001). Patients with increasing levels of pre-morbid disability (mRS > 1) received less physiotherapy minutes.
Figure 2.
Regression coefficients for total physiotherapy minutes according to (a) age, (b) stroke severity, (c) length of stay and (d) availability of early supported discharge.
Table 3.
Regression coefficients for log total physiotherapy minutes according to different patient and service factors.
| Total physiotherapy minutes (log)n = 218,629. Clusters = 204 hospitals |
||
|---|---|---|
| Outcome | Regression Coefficient | 95% Confidence Interval |
| Age | See spline diagram | |
| Sex | 0.03 | 0.02–0.04 |
| Stroke subtype (infarction without thrombolysis as reference) | ||
| Infarction with thrombolysis | 0.08 | 0.06–0.10 |
| Intracerebral haemorrhage | 0.00 | −0.01 to 0.02 |
| Pre-morbid mRS (mRS=0 as reference) | ||
| 1 | −0.01 | −0.04 to 0.02 |
| 2 | −0.04 | −0.07 to −0.01 |
| 3 | −0.10 | −0.14 to −0.06 |
| 4 | −0.22 | −0.25 to 0.18 |
| 5 | −0.39 | −0.44 to −0.33 |
| UTI or pneumonia in first 7 days | −0.05 | −0.07 to −0.02 |
| Co-morbidities | ||
| Congestive heart failure | −0.01 | −0.05 to 0.03 |
| Hypertension | 0.04 | 0.02–0.05 |
| Atrial fibrillation | −0.04 | −0.05 to −0.03 |
| Diabetes | −0.00 | −0.01 to 0.01 |
| Prior stroke/transient ischaemic attack | −0.02 | −0.03 to −0.01 |
| Stroke onset while already an inpatient | −0.11 | −0.14 to −0.08 |
| Stroke severity | See spline diagram | |
| Admitting hospital’s availability of ESD | See spline diagram | |
| Length of stay | See spline diagram | |
| Intercept | 3.07 | 2.92–3.23 |
ESD: early supported discharge.
Contrary to our hypothesis, there were differences in physiotherapy minutes received based on age, gender, stroke severity, presence of medical complications and ESD availability. Male patients were slightly more likely to receive more physiotherapy minutes than female patients and patients aged between 60 and 80 were more likely to receive more physiotherapy minutes compared to patients younger and older than this age bracket (p < 0.001). Patients who developed a medical complication within the first seven days of hospitalisation received slightly fewer physiotherapy minutes. Patients admitted to hospitals with mid-range ESD referral rates (around 30–35% of patients discharged with ESD) received the most minutes, while patients admitted to hospital with lower (<25%) or higher (>40%) referral rates received less minutes. Patients with moderate stroke severity were more likely to receive more physiotherapy minutes compared to other levels of stroke severity.
Intensity of physiotherapy
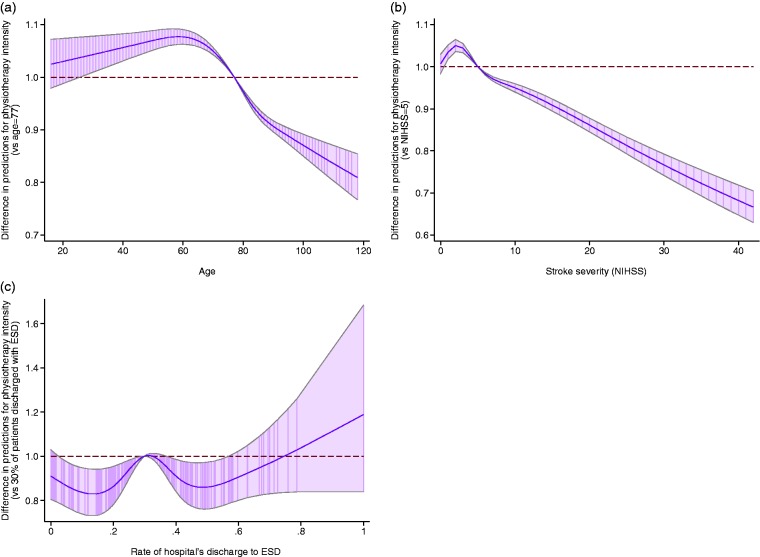
As hypothesised, younger patients, patients with lower pre-morbid disability and stroke severity, having an infarct and having few medical complications received more intensive physiotherapy (Figure 3, Table 4).
Figure 3.
Regression coefficients for physiotherapy intensity according to (a) age, (b) stroke severity, and (c) availability of early supported discharge.
Table 4.
Regression coefficients for log physiotherapy intensity according to different patient and service factors.
| Physiotherapy intensity (log)n = 218655. Clusters = 204 hospitals |
||
|---|---|---|
| Outcome | Regression Coefficient | 95% Confidence Interval |
| Age | See spline diagram | |
| Sex | 0.04 | 0.03–0.05 |
| Stroke subtype (infarction without thrombolysis as reference) | ||
| Infarction with thrombolysis | 0.09 | 0.07–0.11 |
| Intracerebral haemorrhage | −0.06 | −0.07 to −0.04 |
| Pre-morbid mRS (mRS=0 as reference) | ||
| 1 | −0.03 | −0.05 to 0.00 |
| 2 | −0.06 | −0.09 to −0.02 |
| 3 | −0.08 | −0.12 to −0.04 |
| 4 | −0.12 | −0.16 to −0.09 |
| 5 | −0.11 | −0.16 to −0.06 |
| UTI or pneumonia in first 7 days | −0.13 | −0.15 to −0.10 |
| Co-morbidities | ||
| Congestive heart failure | −0.02 | −0.06 to 0.02 |
| Hypertension | 0.03 | 0.02 to 0.04 |
| Atrial fibrillation | −0.03 | −0.05 to −0.02 |
| Diabetes | −0.02 | −0.03 to −0.01 |
| Prior stroke/transient ischaemic attack | −0.01 | −0.02 to −0.00 |
| Stroke onset while already an inpatient | −0.19 | −0.22 to −0.17 |
| Stroke severity | See spline diagram | |
| Admitting hospital’s availability of ESD | See spline diagram | |
| Length of stay | – | – |
| Intercept | 0.41 | 0.29 to 0.52 |
ESD: early supported discharge.
Contrary to our hypothesis, there were differences in physiotherapy based on gender and ESD availability. Male patients were slightly more likely to receive more intensive physiotherapy than female patients. Patients admitted to hospitals with mid-range ESD referral rates (around 30–35% of patients discharged with ESD) received the most intensive physiotherapy, while patients admitted to hospital with lower (<25%) or higher (>40%) referral rates received less intensive physiotherapy.
Discussion
This is the largest study to date reporting factors associated with physiotherapy provision to hospitalised stroke patients. Findings suggest that most patients registered on the SSNAP database were considered applicable for physiotherapy and that age, gender, stroke type, pre-morbid disability, stroke severity, presence of medical complication, LOS and ESD availability influenced physiotherapy provision. Due to the large sample size of stroke patients included in the analyses and the number of stroke units entering data into the SSNAP database, study results may be considered generalisable to the wider stroke population.
Previous studies investigating associations of age and physiotherapy provision to stroke patients have demonstrated mixed results.5–8 It is recognised that increasing age is associated with a higher number of co-morbidities,18 which have been demonstrated to reduce functional outcome post-stroke18,19 and may influence participation in physiotherapy. This finding may explain why age was associated with total physiotherapy minutes and intensity in our study, but it is less clear why age influenced applicability for physiotherapy. Additionally, studies analysing the influence of gender on physiotherapy provision have demonstrated mixed results.7–9 In our study, male patients were statistically more likely to receive more physiotherapy minutes and more intensive physiotherapy to female patients, after adjusting for other factors. However, the effect size between male and female patients was small and therefore may not be clinically significant. Whilst evidence suggests female patients may have more severe stroke and are older than male patients at stroke onset,20 stroke severity and age were adjusted for in the regression models. It is possible that other factors not accounted for in the analyses could be responsible for this gender difference, such as frailty, which tends to be higher in females than males.21,22 As frailty includes low physical activity levels and self-reported exhaustion, this may influence participation in physiotherapy and contribute to the study’s findings. However, as applicability for physiotherapy should be based on clinical need for physiotherapy, these findings on age and gender warrant further investigation.
This study demonstrated that increasing pre-morbid disability and stroke severity were associated with the provision of less physiotherapy minutes and less intensive physiotherapy. These findings contrast with other studies examining the effect of stroke severity on therapy provision, which found that patients with more severe stroke generally received more physiotherapy than patients with milder stroke.8,10,11,13 However, these studies were conducted with much smaller patient samples than the current study and two of these studies only analysed data over 1–2 days of patients’ hospital stay as opposed to their whole hospital stay.8,13 Notable in our study is that patients with very severe stroke received significantly less intensive physiotherapy than patients with moderate and severe stroke. Previous research has found that stroke unit physiotherapists tailor the length and frequency of physiotherapy sessions according to a patient’s ability to tolerate physiotherapy.23 Physiotherapists were more likely to offer shorter yet more frequent physiotherapy sessions for patients who could participate in therapy for short periods of time. Therefore, patients with very severe stroke may only receive very short but frequent physiotherapy sessions based on reduced participation in therapy. However, it is not clear if the beliefs of the treating physiotherapist also influence physiotherapy provision according to stroke severity. For example, physiotherapists may be less likely to provide intensive physiotherapy to optimise function if they perceive that patients with severe stroke have limited rehabilitation potential. Further qualitative research is required to explore this area in more detail.
Other factors associated with physiotherapy intensity included stroke type and post-stroke complications. It is recognised that patients with haemorrhagic stroke are more likely to have increased levels of drowsiness than patients with ischaemic stroke24 and therefore may tolerate less intensive physiotherapy requiring active participation compared to patients with ischaemic stroke. Interestingly, patients with ischaemic stroke who were thrombolysed were considered more applicable for physiotherapy and received more intensive physiotherapy than patients with ischaemic stroke not thrombolysed. Whilst not investigated in this study, this may be due to a reduction in stroke severity post-thrombolysis, which our study has shown is associated with patients receiving more physiotherapy minutes and more intensive physiotherapy. Another possible reason is that patients who are thrombolysed may be perceived to have a better prognosis than those not thrombolysed and therefore physiotherapists may be more likely to consider these patients applicable for physiotherapy. However, this information is not recorded on SSNAP. Like patients with haemorrhagic stroke, patients who develop post-stroke infections may tolerate less intensive physiotherapy due to medical instability or reduced exercise tolerance than patients with no post-stroke complications.
In this study, patients admitted to hospitals with mid-range ESD referral rates received the most physiotherapy minutes and intensive physiotherapy compared to low and high referral rates. It is not entirely clear why this pattern was seen as it could be argued that low ESD availability would mean patients would stay in hospital for longer to receive more physiotherapy. As SSNAP does not record data on reason for ESD referral, this finding warrants further investigation.
This study has some limitations. First, as SSNAP data analysed in this study are from hospitals across England and Wales, individual stroke unit practice may vary from these results and physiotherapists should consider this nationally generated information with reference to their own areas. Second, physiotherapy minutes are self-reported by individual stroke services and different physiotherapists may record different session components on SSNAP, although detailed guidance is provided by SSNAP to limit this variability. It is also recognised that self-reported estimations of session length can be inaccurate due to overestimation of total time engaged in rehabilitation.25 However, a generalised overestimation of physiotherapy provision should not affect the results as all services may be overestimating consistently. Third, data are collected on the total number of minutes and days of physiotherapy provision across a patient’s hospital stay. We cannot say whether there were variations in physiotherapy intensity on a daily basis or if patients received multiple sessions on some days. It has been reported that stroke unit physiotherapists may reduce the amount of physiotherapy before withdrawing physiotherapy for patients not making gains with physiotherapy.23 However, SSNAP data does not provide this level of detail. Finally, whilst possible reasons for the results have been identified within the discussion, SSNAP does not record more detailed information about other factors that may influence the physiotherapy provision, such as staffing levels. Therefore, it is not exactly clear why reported differences in physiotherapy provision occurred. Further exploratory work is required to more fully understand differences in physiotherapy provision across a patient’s hospital stay. This should enable physiotherapists to carefully consider a patient’s individual presentation and tailor physiotherapy sessions accordingly to maximise recovery.
Supplemental Material
Supplemental material, Supplementary material for Physiotherapy provision to hospitalised stroke patients: Analysis from the UK Sentinel Stroke National Audit Programme by Mark P McGlinchey, Lizz Paley, Alex Hoffman, Abdel Douiri and Anthony G Rudd in European Stroke Journal
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical approval
Permission to collect patient data without explicit consent was granted by the Ethics and Confidentiality Committee of the National Information Governance Board, United Kingdom.
Informed consent
Not applicable.
Guarantor
MM.
Contributorship
MM contributed to the study conception, study design and manuscript production; LP was involved in study design, statistical analysis and critical review of the manuscript; AH contributed to the study design and critical review of manuscript; AD took part in the statistical analysis and critical review of manuscript; AR took part in the critical review of manuscript.
References
- 1.GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017; 390: 1151–1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.GBD 2016 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017; 390: 1260–1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stroke Unit Trialists’ Collaboration. Organised inpatient (stroke unit) care for stroke. Cochrane Database Systematic Rev 2013; 9: CD000197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Veerbeek JM, van Wegen E, van Peppen R, et al. What is the evidence for physical therapy poststroke? A systematic review and meta-analysis. PLoS ONE 2014; 9: e87987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bhalla A, Grieve R, Tilling K, et al. Older stroke patients in Europe: stroke care and determinants of outcome. Age Ageing 2004; 33: 618–624. [DOI] [PubMed] [Google Scholar]
- 6.Saposnik G, Black SE, Hakim A, et al. Age disparities in stroke quality of care and delivery of health services. Stroke 2009; 40: 3328–3335. [DOI] [PubMed] [Google Scholar]
- 7.McKevitt C, Coshall C, Tilling K, et al. Are there inequalities in the provision of stroke care? Analysis of an inner-city stroke register. Stroke 2005; 36: 315–320. [DOI] [PubMed] [Google Scholar]
- 8.Cosgrave L, Bernhardt H, Churilov L, et al. Gender and being born overseas influences the amount of acute stroke therapy. J Rehabil Med 2013; 45: 130–136. [DOI] [PubMed] [Google Scholar]
- 9.Arrich J, Mullner M, Lalouschek W, et al. Influence of socioeconomic status and gender on stroke treatment and diagnostics. Stroke 2008; 39: 2066–2072. [DOI] [PubMed] [Google Scholar]
- 10.Brocklehurst JC, Andrews K, Richards B, et al. How much physical therapy for patients with stroke? Br Med J 1978; 1: 1307–1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wade DT, Skilbeck CE, Hewer RL, et al. Therapy after stroke: amounts, determinants and effects. Int Rehabil Med 1984; 6: 105–110. [DOI] [PubMed] [Google Scholar]
- 12.Bode RK, Heinemann AW, Semik P, et al. Patterns of therapy activities across length of stay and impairment levels: peering inside the “black box” of inpatient stroke rehabilitation. Arch Phys Med Rehabil 2004; 85: 1901–1908. [DOI] [PubMed] [Google Scholar]
- 13.Bernhardt J, Chan J, Nicola I, et al. Little therapy, little physical activity: rehabilitation within the first 14 days of organized stroke unit care. Acta Derm Venereol 2007; 39: 43–48. [DOI] [PubMed] [Google Scholar]
- 14.Wolfe C, Taub N, Woodrow J, et al. Patterns of acute stroke care in three districts of southern England. J Epidemiol Commun Health 1993; 47: 144–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cumming TB, Plummer-D’Amato P, Linden T, et al. Hemi-spatial neglect and rehabilitation in acute stroke. Arch Phys Med Rehabil 2009; 90: 19313–1936. [DOI] [PubMed] [Google Scholar]
- 16.Bray BD, Cloud GC, James MA, et al. Weekly variation in health-care quality by day and time of admission: a nationwide, registry-based, prospective cohort study of acute stroke care. Lancet 2016; 388: 170–177. [DOI] [PubMed] [Google Scholar]
- 17.von Elm E, Egger M, Altman DG. Strengthening the reporting of observational studies in epidemiology (StroBE) statement: guidelines for reporting observational studies. BMJ 2007; 335: 806–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Karatepe AG, Gunaydin R, Kaya T, et al. Co-morbidity in patients after stroke: impact on functional outcome. J Rehabil Med 2008; 40: 831–835. [DOI] [PubMed] [Google Scholar]
- 19.Bushnell CD, Lee J, Duncan PW, et al. Impact of co-morbidities on ischemic stroke outcomes in women. Stroke 2008; 39: 2138–2140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Appelros P, Stegmayr B, Terent A. Sex differences in stroke epidemiology: a systematic review. Stroke 2009; 40: 1082–1090. [DOI] [PubMed] [Google Scholar]
- 21.Syddall H, Roberts HC, Evandrou M, et al. Prevalence and correlates of frailty among community-dwelling older men and women: findings from the Hertfordshire Cohort Study. Age Ageing 2010; 39: 197–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alexandre T, Corona L, Brito T, et al. Gender differences in the incidence and determinants of components of the frailty phenotype among older adults. J Aging Health 2018; 30: 190–212. [DOI] [PubMed] [Google Scholar]
- 23.McGlinchey MP, Davenport S. Exploring the decision-making process in the delivery of physiotherapy in a stroke unit. Disabil Rehabil 2015; 37: 1277–1284. [DOI] [PubMed] [Google Scholar]
- 24.Birenbaum D. Emergency neurological care of strokes and bleeds. J Emerg Trauma Shock 2010; 3: 52–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kaur G, English C, Hillier S. Physiotherapists systematically overestimate the amount of time stroke survivors spend engaged in active therapy rehabilitation: an observational study. J Physiother 2013; 59: 45–51. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Supplementary material for Physiotherapy provision to hospitalised stroke patients: Analysis from the UK Sentinel Stroke National Audit Programme by Mark P McGlinchey, Lizz Paley, Alex Hoffman, Abdel Douiri and Anthony G Rudd in European Stroke Journal