ABSTRACT
As rescue workers are regularly confronted with potentially traumatising on-duty events, they have an increased risk to develop trauma-related mental and physical health impairments, including post-traumatic, depressive, and somatic symptoms. For this high-risk group, it could be of particular importance to experience their occupational burden as manageable, meaningful, and coherent. This mindset – called sense of coherence – may be a potential resilience factor against the development of mental and physical health problems. In a cross-sectional cohort of 102 rescue workers (Mdn(QD)age = 26.0 (8.5), age range: 18−61), including 36 women, we investigated whether higher values on the Revised Sense of Coherence Scale (SOC-R) predicted lower post-traumatic, depressive, and somatic symptoms. In addition, we evaluated the factor structure of the SOC-R using confirmatory factor analyses. Linear regressions indicated that higher SOC-R, but particularly manageability scores were associated with less post-traumatic (β = −.31, p = .009), depressive (β = −.44, p < .001), and somatic symptoms (β = −.36, p = .002). Furthermore, we found that all symptom scores significantly increased with occupational and private-life trauma exposure. The SOC-R’s factor structure was replicated, comprising the three subscales manageability, reflection, and balance. However, the SOC-R’s convergent factor validity was rather low in the present sample. Taken together, a high sense of coherence, and in particular a high manageability conviction, was observed as resilience factors for high-risk groups that are frequently exposed to potentially traumatic events. Future studies might investigate whether strengthening the sense of coherence could be one building block in an effective prevention program for maintaining long-term health in risk groups.
KEYWORDS: Revised sense of coherence scale (SOC-R), resilience, PTSD, depression, somatic symptoms, emergency medical service, occupational stress and health, paramedics, ambulance workers, first responders
PALABRAS CLAVE: Escala del sentido de coherencia revisado (SOC-R), resiliencia, TEPT, depresión, síntomas somáticos, servicio médico de emergencia, estrés laboral y salud, paramédicos, trabajadores de ambulancias primeros respondedores
关键词: 修订版心理一致感量表(SOC-R), 韧性, PTSD, 抑郁, 躯体症状, 紧急医疗服务, 职业压力与健康, 医护人员, 救护人员, 现场应急人员
HIGHLIGHTS
• The Revised Sense of Coherence scale displayed poor convergent factor validity in German rescue workers. • Higher sense of coherence, but particularly the manageability conviction was associated with less mental and physical complaints in rescue workers. • On-duty and private-life trauma exposure were associated with more mental and physical health impairments. • Longitudinal studies are necessary to confirm whether the revised sense of coherence is a prospective resilience factor against stress and trauma in high-risk professions.
Abstract
Debido a que los trabajadores de rescate se enfrentan regularmente con eventos laborales potencialmente traumatizantes, presentan un mayor riesgo de desarrollar trastornos mentales y físicos relacionados con el trauma, incluyendo síntomas postraumáticos, depresivos y somáticos. Para este grupo de alto riesgo sería importante el experimentar su trabajo como manejable, significativo y coherente. Esta perspectiva —llamada sentido de coherencia— podría ser un factor potencial de resiliencia en contra del desarrollo de problemas mentales y físicos. En una cohorte transversal con 102 trabajadores de rescate (Mdn(QD)edad = 26.0 (8.5), rango de edad: 18-61), de los cuáles 36 eran mujeres, investigamos si los valores más altos en la Escala del Sentido de Coherencia Revisada (SOC-R) predijeron menos síntomas postraumáticos, depresivos y somáticos. Además, evaluamos la estructura factorial del SOC-R mediante análisis factoriales confirmatorios. Las regresiones lineales indicaron que las puntuaciones más altas del SOC-R, pero particularmente la capacidad de menejabilidad, se asociaron con menos síntomas postraumáticos (β = −.31, p = .009), depresivos (β = −.44, p <.001) y somáticos (β = −.36, p = .002). Además, encontramos que a mayor la exposición con traumas laborales y privados los puntajes de estos síntomas aumentaron significativamente. La estructura factorial del SOC-R se replicó con sus tres subescalas manejabilidad, reflexión y equilibrio. Sin embargo, la validez del factor convergente del SOC-R era menor en la presente muestra. En general, se observó que un alto sentido de coherencia y, en particular una alta manejabilidad, funcionan como factores de resiliencia en grupos de alto riesgo que con frecuencia están expuestos a eventos potencialmente traumáticos. Estudios futuros deberían investigar si el fortalecimiento del sentido de coherencia podría ser un componente básico en un programa de prevención eficaz para mantener la salud a largo plazo en grupos de riesgo.
Abstract
由于救援人员经常面临可能造成创伤的职业事件,他们发生创伤相关的精神和身体健康损害的风险增加,包括创伤后应激、抑郁和躯体症状。对于这个高风险群体而言,将其职业负担看作为可管理,有意义且一致可能尤为重要。这种被称为心理一致感的心理状态可能是一种潜在的抵御心理和身体健康问题发展的韧性因素。在102名救援人员(Mdn(QD) 年龄= 26.0(8.5),年龄范围:18-61)的横断面队列研究中,包括36名女性。我们考察了修订心理一致感量表(SOC-R)的更高分数是否预测较低的创伤后应激、抑郁和躯体症状。此外,我们使用验证性因子分析评估了SOC-R的因子结构。 线性回归分析表明,较高的SOC-R分数,尤其是可控性得分与较少的创伤后应激(β= −.31,p = .009),抑郁(β= −.44,p <.001)和躯体症状(β = −.36,p = .002)相关。进一步的,我们发现随着职业和个人生活创伤暴露,所有症状评分都显著增加。 SOC-R的因子结构得到重复,包括三个分量表:可管理性,反思和平衡。不过,在本样本中SOC-R的聚合效度相当低。总的来说,高度心理一致性,尤其是高的可控信念,被视为经常暴露于潜在创伤事件的高风险群体的韧性因素。未来的研究可能会调查加强心理一致感是否可以成为有效维持风险群体长期健康的预防计划的一个组成部分。
1. Introduction
Research in cohorts exposed to multiple traumatic event types such as survivors of violent conflict and war, found the risk for post-traumatic stress disorder (PTSD) and depression to increase in a dose–response relationship with the number of traumatic events experienced across lifetime, up to a maximum of 100% under extreme trauma exposure (Comellas et al., 2015; Conrad et al., 2017; Kolassa et al., 2010; Kolassa, Kolassa, Ertl, Papassotiropoulos, & De Quervain, 2010; Mollica, McInnes, Pool, & Tor, 1998). A similarly increased risk to develop PTSD can be assumed in individuals who are regularly confronted with traumatic experiences in the context of their work. Such occupational high-risk groups include firefighters, police officers, and rescue workers.
Rescue workers are confronted with on average 15 different traumatic event types during five years of employment, including the care for severely injured or dying children, family members, friends, colleagues or acquaintances or being themselves attacked or injured during rescue operations (Alexander & Klein, 2001; Declercq, Meganck, Deheegher, & Van Hoorde, 2011; Donnelly & Bennett, 2014; Halpern, Maunder, Schwartz, & Gurevich, 2012; Regehr, Goldberg, & Hughes, 2002; Teegen & Yasui, 2000). There is ample evidence for an increasing prevalence of clinically relevant (often co-morbid) post-traumatic and depressive symptoms as well as accompanying somatic complaints with the number of traumatic events on duty (Aasa, Brulin, Ängquist, & Barnekow-Bergkvist, 2005; Benedek, Fullerton, & Ursano, 2007; Berger et al., 2011; Clohessy & Ehlers, 1999; Donnelly, 2012; Fjeldheim et al., 2014; Fullerton, Ursano, & Wang, 2004; Häller, Michael, & Balmer Koechlin, 2009; Hegg-Deloye et al., 2014; Razik, Ehring, & Emmelkamp, 2013; Skeffington, Rees, & Mazzucchelli, 2017; Teegen & Yasui, 2000; Wild et al., 2016). According to a meta-analysis of Berger et al. (Berger et al., 2011), rescue workers show even higher prevalence rates for PTSD than firefighters and police officers. Not surprisingly, PTSD prevalence in rescue workers is much higher than in the general population, and ranges between 5% and 22% (Bennett, Williams, Page, Hood, & Woollard, 2004; Berger et al., 2011, 2007; Clohessy & Ehlers, 1999; Grevin, 1996; Jonsson, Segesten, & Mattson, 2003; Lowery & Stokes, 2005; Skeffington et al., 2017; van der Ploeg & Kleber, 2003). There is initial evidence that also nonwork-related major life events, but particularly adverse experiences during childhood could lead to considerably elevated concurrent symptom levels in rescue workers (Levy-Gigi et al., 2015; Maunder, Halpern, Schwartz, & Gurevich, 2012; Richter, 2014).
Several factors protecting from the development of mental health problems after trauma in first responders have been identified, among them high levels of perceived (coping) self-efficiency (Heinrichs et al., 2005; Regehr, Hill, Knott, & Sault, 2003), social support (Fjeldheim et al., 2014; Prati & Pietrantoni, 2010; Regehr et al., 2003; Shakespeare-Finch, Rees, & Armstrong, 2015), or the emotion regulation strategy acceptance (Gärtner, Behnke, Conrad, Kolassa, & Rojas, 2019). In addition, Antonovsky proposed a sense of coherence as an important psychological resilience factor (Antonovsky, 1979). In its original form, the sense of coherence encompassed three principal beliefs that a person can have about life and its challenges: First, the perception of the world as logically structured, understandable and thus predictable (comprehensibility). Second, the conviction of having sufficient resources to successfully face the demands of the world (manageability). And thirdly, the conviction that these demands are valuable challenges that exist for a good reason and are worth dealing with (meaningfulness).
Different versions of Antonovsky’s Sense of Coherence Scale (SOC) exist (Antonovsky, 1993). Previous research using either the 9-, 13- or 29-item version found that a higher sense of coherence was associated with, e.g., less severe somatic symptoms in breast cancer patients (Leonhart et al., 2017), less pregnancy-specific distress (Staneva, Morawska, Bogossian, & Wittkowski, 2016), and with higher health-related quality of life in adolescents with heart disease (Wang, Hay, Clarke, & Menahem, 2014).
Yet, the original SOC questionnaires suffered from problems regarding their psychometric properties, including an inconsistent factorial structure and fluctuations with age (Bachem & Maercker, 2016). Due to the concept’s high correlation with broad personality traits, particularly neuroticism (Gruszczyńska, 2014; Kase, Ueno, & Oishi, 2018), its discriminant validity was debated. Recently, Bachem and Maercker (2016) reconceptualised the sense of coherence and introduced the Revised Sense of Coherence Scale (SOC-R). In its revised version, less focus is placed on the structure, predictability, and reasonability of environmental stimuli, but the individual’s general ability to perceive life events as a coherent whole, including both, the good and the bad. Comparable to the original concept it describes a person’s conviction to master life’s adversities, extended by the individual’s ability to see the relatedness and balance between ambiguous life experiences (Bachem & Maercker, 2016). Individuals with a stronger sense of coherence are therefore expected to maintain mental health even if confronted with highly stressful or traumatic events. Accordingly, the authors found negative correlations between the SOC-R and measures for depression and anxiety as well as positive correlations with measures of mental and physical well-being (Bachem & Maercker, 2016). Furthermore, the revised sense of coherence moderates the association between early-life emotional neglect and later-life mental health in a way that individuals with low to moderate scores on the SOC-R showed considerably more mental health problems related to early-life emotional neglect than individuals with higher SOC-R values (Mc Gee, Höltge, Maercker, & Thoma, 2017, 2018).
The aim of this cross-sectional study was to investigate whether the revised sense of coherence is a potential resilience factor against post-traumatic, depressive, and somatic symptoms also in high-risk groups, who are regularly confronted with extreme levels of trauma, such as rescue workers. Thereby, potential covariates, including trauma exposure on duty and in private life across childhood and adulthood as well as (biological) sex, will be considered. In addition, given the relative novelty of the SOC-R, this study aimed at evaluating the questionnaire’s factor structure in a cohort of German rescue workers.
2. Material and methods
2.1. Participants
Participants were recruited from October to December 2016 in two rescue stations of the German Red Cross in Germany. Full data was available from 103 rescue workers. One participant had to be excluded for doubts on the validity of the given answers, i.e., the participant indicated an invariant response pattern in several questionnaires, including the SOC-R. Statistical analyses were therefore based on a total of N = 102 participants (Mdn(QD1)age = 26.0 (8.5) years, range: 18−61), including 36 women. Working experience ranged from one week to 35 years (Mdn(QD) = 3.29 (5.47) years).
2.2. Materials and study procedure
The Ulm University ethics committee approved the study procedures. Study aims and procedures were introduced to the rescue workers during regular further education events. Rescue workers interested in study participation were asked to provide their email address to receive an individual link for participation in an online survey (LimeSurvey, 2017). All participants declared their written informed consent prior to participation. The survey lasted approximately 60 min and included questions on demographic data, questionnaires to assess the experience of traumatic events and childhood maltreatment, clinical screening instruments for PTSD, depression, and somatic symptoms, and instruments to measure a variety of potential risk and resilience factors regarding the development of mental health problems, including the SOC-R. A detailed description of the questionnaires used in this study can be found below.
2.2.1. Sense of coherence
The Revised Sense of Coherence Scale (SOC-R) (Bachem & Maercker, 2016) contains 13 items (e.g., In spite of everything, I can learn from bad experiences). Participants indicated their agreement with each statement on a 5-point Likert scale ranging from 1 (not at all true) to 5 (extremely true), with item 6 being coded reversely. The scale comprises the three subscales manageability, reflection, and balance. For statistical analyses, the sum scores of all items (Cronbach’s α = .76) and the three subscales were calculated (Cronbach’s α = .72, .72, and .63 for manageability, reflection, and balance, respectively).
2.2.2. Occupational trauma exposure
Using a modified and extended version of the Rescue and Emergency Situations Questionnaire (Schoch, 2008), the rescue workers’ exposure to 10 potentially traumatic on-duty event types were assessed, including severe injury or death, taking care of people with special needs (e.g., palliative patients) or difficulties in the interaction with relatives of victims. In addition, participants could add events not included in the event list as free text. Participants indicated whether they had ever been exposed to any of the described mission events or not. The number of experienced potentially traumatic event types represented the occupational trauma exposure.
2.2.3. Private-life trauma exposure
To assess the exposure to traumatic event types in private life from child- to adulthood, we used two questionnaires. First, the German version of the Life Event Checklist for DSM-5 (LEC-5) (Ehring, Knaevelsrud, Krüger, & Schäfer, 2014; Weathers et al., 2013) was used to assess 16 potentially traumatic event types covering the exposure to natural disasters, accidents, interpersonal violence, war, life-threatening illness or injury. Participants were asked whether they had ever experienced any of these events or witnessed how a close relative or friend had experienced any of these events. Each form of exposure was rated as one individual potentially traumatic event type. Participants could also add traumatic event types not included in the event list. Different from the original questionnaire, we excluded the answering option of being confronted on duty and instructed the participants to focus on their private life only, as work-related traumatic events were assessed separately. Participants could also indicate that they had not experienced the event or were insecure whether they had been exposed to it. In this case, the item was rated as nonexposed. Second, childhood maltreatment experiences were assessed with the German 20-item short-version of the Maltreatment and Abuse Chronology of Exposure scale (Teicher & Parigger, 2015) applied as a self-report measure (KERF-20) (Isele, Schauer, Ruf-Leuschner, & Elbert, 2011; Isele et al., 2014). The KERF-20 covers 10 different forms of childhood maltreatment experiences, including sexual abuse, emotional, and physical neglect, as well as physical and emotional abuse through parents or siblings, the experience of violence through peers, and the witness of violence on parents or siblings, respectively. The values of each subscale were added, then interpolated, and finally, the sum score of all subscales was calculated. LEC-5 and KERF-20 sum scores were summarised to represent the individual’s total private-life trauma exposure (cf. Conrad et al., 2017; Wilker et al., 2015).
2.2.4. Post-traumatic symptoms
The German version of the PTSD Checklist for DSM-5 (PCL-5) (Krüger-Gottschalk, Knaevelsrud, Rau et al., 2017; Weathers et al., 2013) was applied. The PCL-5 includes 20 items covering the four PTSD symptom clusters intrusions, avoidance, hyperarousal, and negative alterations in mood and cognition. With regard to the worst traumatic event experienced in private or on duty, participants indicated on a 5-point Likert scale, ranging from 1 (not at all) to 5 (very strong), how much they felt impaired by the described problems (e.g., avoidance of memories, thoughts or emotions related to the traumatic event) during the last month. The sum score of all items was used as a measure for PTSD symptom severity (Cronbach’s α = .91).
2.2.5. Depression symptoms
Depressive symptoms were assessed with the German version of the 9-item depression scale of the Patient Health Questionnaire (PHQ-9) (Kroenke, Spitzer, Williams, & Löwe, 2010; Löwe, Spitzer, Zipfel, & Herzog, 2002). On a 4-point Likert scale ranging from 0 (not at all) to 3 (almost every day), participants indicated how much they felt impaired by symptoms of depression during the past two weeks (e.g., tiredness or feeling of no energy). For statistical analyses, the symptom score of all nine items was calculated (Cronbach’s α = .83).
2.2.6. Somatic symptoms
Physical impairment and sleep disturbances during the last four weeks (e.g., stomach aches; back pain) were assessed with 15 items according to the German version of the Patient Health Questionnaire (PHQ-15) (Kroenke et al., 2010; Löwe et al., 2002). For reasons of comparability between males and females, we excluded the item asking for menstrual pain. The questions were answered on a 3-point Likert scale from 0 (not at all) to 2 (very strong). The sum score of all responses was used in subsequent analyses (Cronbach’s α = .84).
2.3. Statistical analyses
Statistical analyses were performed with SPSS, version 20 (IBM Corp, 2011) and R, version 3.5.1 (R Core Team, 2018). To evaluate the factor structure of the SOC-R we performed confirmatory factor analyses (CFA) using the R package lavaan, version 0.6–3 (Rosseel, 2012). As SOC-R items were not multivariate normally distributed (Energy test: E = 2.01, p < .001), a maximum likelihood estimator (MLR) with robust Huber-White standard errors and an asymptotic Yuan-Bentler test statistic was used (Bentler, 2006, pp. 289-291; Rosseel, 2012, p. 29). We specified a one-factor model including all 13 items and two 3-factor models separating the three subscales manageability, reflection, and balance, as proposed in Bachem and Maercker (2016). The absolute χ2 statistic and the according p-value (p > .05), the relative χ2 statistic (χ2/df < 3), the root mean square error of approximation (RMSEA; ≤ .08), the standardised root mean square residual (SRMR; ≤ .08), and the comparative fit index (CFI; ≥ .95) were used as model fit criteria (Hu & Bentler, 1999). According to the Fornell-Larcker criteria (Fornell & Larcker, 1981), satisfying factor convergence is indicated by an average variance extracted (AVE) larger than .50 and a composite reliability (CR) larger than .70. Satisfying factor discriminability is indicated by an AVE larger than the maximum shared variance (MSV) and a square root of AVE greater than inter-construct correlations (Gaskin, 2016; Hair, Black, Babin, & Anderson, 2010).
Furthermore, we investigated whether the SOC-R and its subscales were associated with lower PTSD, depression, and somatic symptom severity as well as a lower total symptom burden, as an indicator of rescue workers’ overall health status. For the total symptom burden, the symptom severity scores were z-standardised and averaged to a composite score. Due to nonnormality of various study variables, bivariate correlations were computed with Spearman’s ρ rank correlation. Linear regression analyses were conducted to predict the severity of the different symptoms and their composite by the SOC-R or its subscales. All models included occupational and private-life trauma exposure as well as sex as covariates. As model residuals were right-tailed for each outcome variable, all regression models were 5000-times BCa bootstrapped.
3. Results
3.1. Confirmatory factor analysis
The intercorrelation matrix of the SOC-R items (Supplementary Table 1) shows no generally positive correlations of the questionnaire’s items. Within the three factors suggested by Bachem and Maercker (2016), rather weak item intercorrelations were found (manageability: ρ = .22−.45, p ≤ .029; reflection: ρ = .22−.45, p ≤ .025; balance: ρ = .19−.54, p ≤ .051). In addition, significant correlations with items of other factors occurred. Using CFA, we compared the one- and the two three-factor solutions proposed by Bachem and Maercker (2016). As displayed in Table 1, none of the compared solutions reached a satisfactory model fit, with the original three-factor solution (Figure 1) yielding the comparatively best model-to-data adequacy. To further evaluate the adequacy of this solution, we additionally examined the Fornell-Larcker criteria (Table 2). Only AVE = 31−42% of the items’ variance converged on the respective factors. As a result, the composite reliability was rather low for the factors balance and manageability and not satisfactory for the reflection factor (CR ≤ .70). The reflection factor also had a low discriminant validity due to the fact that its items shared less variance with another than with items of the other factors (i.e., AVE < MSV). Taken together, the SOC-R’s three-factor solution was the most adequate structure to presume in the present sample, although the factors’ convergent validity was rather low as a result of the weak item intercorrelations.
Table 1.
Results of confirmatory factor analyses.
| χ2 (df) | p | χ2/df | RMSEA | SRMR | CFI | |
|---|---|---|---|---|---|---|
| One-factor solution | 173.51 (65) | < .001 | 2.67 | .126 [.103, .149] | .113 | .591 |
| Original three-factor solutiona | 89.88 (62) | .012 | 1.45 | .066 [.032, .095] | .081 | .892 |
| Modified three-factor solutionb | 122.03 (62) | < .001 | 1.97 | .098 [.072, .124] | .112 | .763 |
RMSEA = robust root mean square error of approximation with a 90% confidence interval, SRMR = standardized root mean square residual, CFI = robust comparative fit index. aSee Figure 1 for details; bBachem and Maercker (2016) proposed a modified three-factor solution, in which the second and third item were counted to the balance scale instead of the reflection scale.
Figure 1.

Three-factor solution of the Revised Sense of Coherence Scale (SOC-R; Bachem & Maercker, 2016). Values on paths indicate standardised regression coefficients (β) or correlations (r). Italic values on top of the items display the respective proportions of explained item variance, R2
Table 2.
Fornell-Larcker criteria of the preferred three-factor model.
| Model criteria |
Interfactor correlations |
||||||
|---|---|---|---|---|---|---|---|
| CR | AVE | √AVE | MSV | Balance | Reflection | Manageability | |
| Balance | .730 | .420† | .648 | .208 | − | ||
| Reflection | .636† | .309† | .556† | .318† | .149 | − | |
| Manageability | .725 | .348† | .590 | .318 | .456 | .564 | − |
A composite reliability of CR > .70 indicates a sufficient consistency of items within a factor (latent variable); an average variance extracted of AVE > .50 indicates sufficient convergent factor validity (i.e., more than 50% of the items’ variances converged on their common factor); satisfactory discriminant factor validity is given when the maximum shared variance MSV < AVE and when the square root of AVE is greater than the interfactor correlations (i.e., items within factors converge more on their common factor than on another factors). Values indicated with † violate the aforementioned criteria.
3.2. Associations of the SOC-R with post-traumatic, depressive, and somatic symptoms
Bivariate correlations (Supplementary Table 2) indicated that higher SOC-R total scores were associated with less severe somatic and depressive symptoms as well as a lower symptom composite, whereas the negative association with post-traumatic symptoms was not significant. The SOC-R subscale manageability was negatively associated with the severity of all symptom types, whereas there were no significant correlations of the subscales reflection and balance with symptom severity. Overall, occupational and private-life trauma exposure were associated with a substantially increased severity regarding all symptom types. There were medium to high correlations of post-traumatic, somatic, and depressive symptom severity (ρ = .55−.82, p’s < .001).
Table 3 summarises the results of bootstrapped linear regressions performed to test whether higher SOC-R total scale or subscales statistically predicted less severe post-traumatic, somatic, depressive as well as transdiagnostic symptoms (symptom composite score).
Table 3.
Overview of linear regression predicting symptom severity (N = 102).
| Posttraumatic symptoms (PCL-5 sum score) |
Somatic symptoms (PHQ-15 sum score) |
Depressive symptoms (PHQ-9 sum score) |
Transdiagnostic symptom composite score |
|||||
|---|---|---|---|---|---|---|---|---|
| Predictors | β (η2p) | β (η2p) | β (η2p) | β (η2p) | β (η2p) | β (η2p) | β (η2p) | β (η2p) |
| SOC-R | ||||||||
| total score | −.09 (.011) | −.17* (.037) | −.26** (.088) | −.20* (.058) | ||||
| Manageability | −.31** (.101) | −.36** (.131) | −.44*** (.196) | −.43** (.205) | ||||
| Reflection | .13 (.021) | .16 (.032) | .06 (.004) | .13 (.027) | ||||
| Balance | .12 (.019) | .04 (.002) | .09 (.011) | .10 (.015) | ||||
| Occupational trauma exposure | .22** (.056) | .22** (.066) | .36** (.142) | .38*** (.166) | .27** (.093) | .28** (.109) | .33*** (.135) | .34*** (.165) |
| Private-life trauma exposure | .40*** (.172) | .39*** (.172) | .23* (.066) | .24** (.072) | .36*** (.157) | .34*** (.155) | .38*** (.180) | .37*** (.191) |
| Sex† | .18 (.042) | .21* (.056) | .17 (.037) | .20* (.053) | −.05 (.003) | −.02 (.001) | .12 (.020) | .15 (.036) |
| Model statistics | ||||||||
| R2 | .269 | .338 | .260 | .312 | .401 | .339 | .350 | .401 |
| F(df1,df2) | 8.93*** (4,97) | 8.07*** (6,95) | 8.50*** (4,97) | 11.01*** (4,97) | 10.61*** (6,95) | 8.10*** (6,95) | 6.56*** (4,97) | 10.61*** (6,95) |
* p < .05, ** p < .01, *** p < .001, two-tailed; standardised regression coefficient (β), explained variance (R2, η2p). † Positive coefficients indicate more symptoms for women. Detailed results are presented in the Supplementary Tables 3 and 4. All models were 5000 times nonparametrically BCa bootstrapped.
Post-traumatic symptoms were less severe in rescue workers with higher manageability scores (Figure 2(b)), whereas the SOC-R total scale (Figure 2(a)) or other subscales showed no significant association with post-traumatic symptoms. Occupational and private-life trauma exposure as well as female sex were associated with more severe post-traumatic symptoms.
Figure 2.
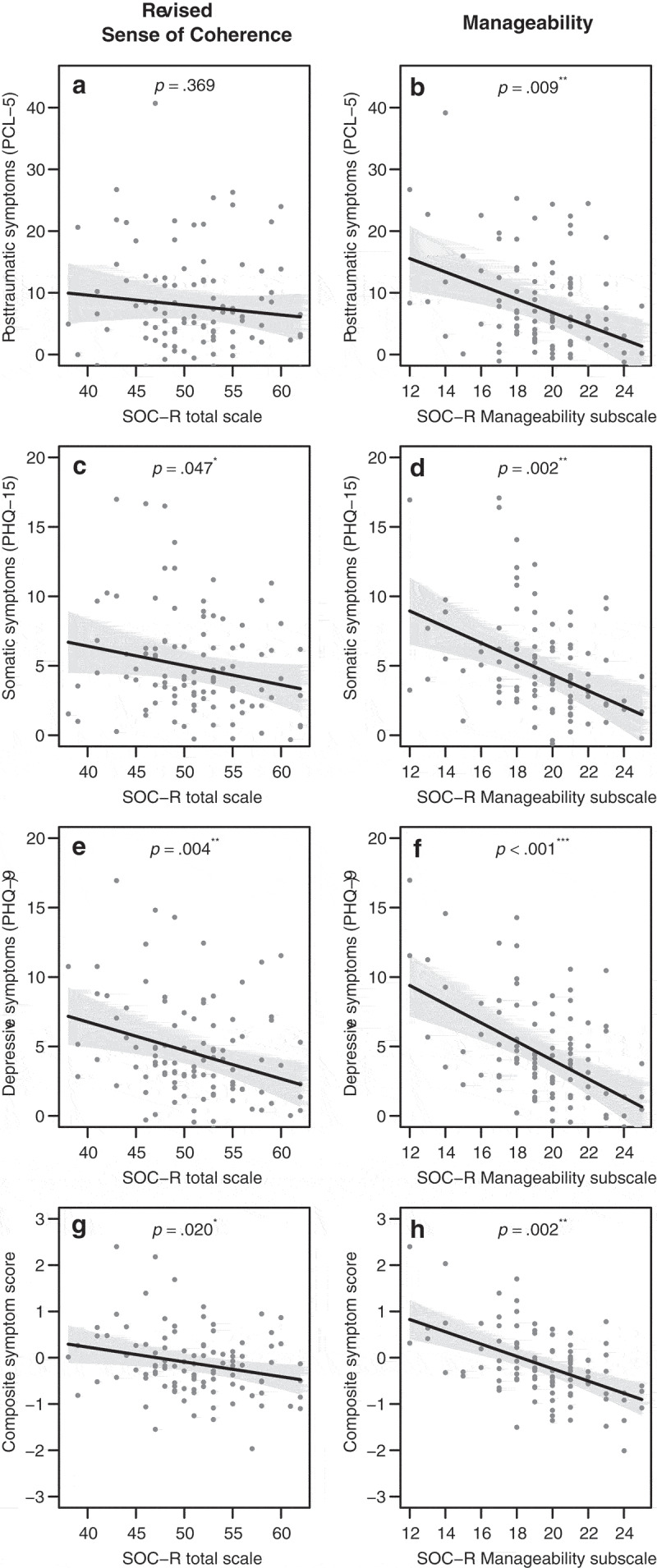
Partial scatter plots displaying the linear regressive associations of the Revised Sense of Coherence Scale (SOC-R; Bachem & Maercker, 2016) total scale with the rescue workers’ (a) post-traumatic symptoms as assessed with the PTSD Checklist for DSM-5 (PCL-5; Krüger-Gottschalk et al., 2017), (c) depressive symptoms as assessed with the Patient Health Questionnaire depression scale (PHQ-9; Löwe et al., 2002), (e) somatic symptoms as assessed with the Patient Health Questionnaire physical symptoms scale (PHQ-15 ; Löwe et al., 2002), and the transdiagnostic symptom composite score (g) as well as the associations of the SOC-R Manageability subscale with (b) post-traumatic symptoms, (d) depressive symptoms, (f) somatic symptoms, and the transdiagnostic symptom composite score (h). Influences of occupational and private-life trauma exposure and sex were considered as covariates. Grey areas indicate 95% confidence intervals.
Somatic symptoms were less severe in rescue workers with higher SOC-R total (Figure 2(c)) and manageability scores (Figure 2(d)), whereas the other SOC-R subscales showed no significant association with somatic symptoms. Occupational and private-life trauma exposure, as well as female sex, were associated with more severe somatic symptoms.
Similarly, depressive symptoms were less severe in rescue workers with higher SOC-R total (Figure 2(e)) and manageability scores (Figure 2(f)), while there were no significant associations of the other SOC-R subscales with depressive symptoms. Again, occupational and private-life trauma exposure were linked to more severe depressive symptoms.
Regarding the symptom composite score, symptom severity was lower in rescue workers with higher SOC-R total (Figure 2(g)) and manageability scores (Figure 2(h)). Again, the other SOC-R subscales had no significant relationship with symptom severity. Occupational and private-life trauma exposure was associated with elevated symptom severity.
The association of female sex with increased symptom severity was inconsistent across the regression models (see Table 3). Group comparison between male and female rescue workers indicated that sex was multiply associated with other variables (Supplementary Table 5). Men were significantly older (d = 1.02, p < .001), had longer work experience (d = 0.63, p = .003), and descriptively, were exposed to more occupational trauma events (d = 0.34, p = .090). Moreover, male rescue workers indicated slightly higher scores than females on the SOC-R total scale (d = 0.42, p = .043), whereas no sex differences were observed for the SOC-R subscales (p’s > .068).
Correlation analyses indicated no dependency of the sense of coherence measures on other covariates, i.e., occupational or private-life trauma exposure, age, working experience or educational level (p’s > .05; see Supplementary Table 2).
4. Discussion
This study aimed at investigating the putative beneficial relationship of the revised sense of coherence with mental and physical health in a cross-sectional sample of German rescue workers. Our results suggest that the revised sense of coherence and particularly its manageability facet could be an important resilience factor protecting the mental and physical health of rescue workers and employees of professions with similar on-duty trauma exposure. Moreover, we confirmed the three-factor structure of the SOC-R in the present sample with restrictions regarding the factors’ convergent validity.
4.1. Factor structure of the SOC-R
CFA indicated the three-factor solution as originally proposed by Bachem and Maercker (2016) as the relatively most appropriate structure for the SOC-R in this sample of rescue workers. The SOC-R total scale was divided into the three subscales manageability, reflection, and balance. The three factors explained a similar amount of variance on the items and yielded a comparably weak model fit as reported in earlier studies (Bachem & Maercker, 2016; Mc Gee et al., 2017). One explanation for the poor model fit could be the low intercorrelation of the SOC-R items. Low correlations of items within factors could also have inflated themodel-fit parameters, in particular RMSEA, SRMR and the χ2 test (Beierl, Bühner, & Heene, 2018; Heene, Hilbert, Draxler, Ziegler, & Bühner, 2011). Inflated model-fit indices may thus erroneously identify unsuitable or unjustifiably complex factor solutions as appropriate (Beierl et al., 2018; Heene et al., 2011). Therefore, we more closely investigated the SOC-R’s factor structure using Fornell-Larcker criteria, revealing that the questionnaire’s items did not homogeneously converge on the respective factors, but showed considerable ‘error’ variances with other factors’ items. This resulted in a rather low convergent factor validity of the SOC-R in the present sample. Due to this, the composite reliability of the SOC-R subscales manageability and balance was in the lower acceptable range, while the composite reliability of the reflection subscale was too low. In sum, our results suggest the SOC-R’s three-factor structure as the relatively most appropriate a-priori solution in rescue workers. However, the SOC-R factors showed a rather low convergent validity which could indicate that the questionnaire items do not adequately represent the theoretically presumed facets of the revised sense of coherence.
4.2. The revised sense of coherence as a potential resilience factor
As the revised sense of coherence was proposed as a potential resilience factor, we investigated the SOC-R’s association with post-traumatic, depressive, and somatic symptoms in this sample of German rescue workers. We identified the manageability subscale as significantly associated with less severe post-traumatic, depressive, and somatic symptoms beyond the influence of occupational and private-life trauma exposure and sex. Manageability accounted for considerable proportions of the variance of the different symptom types (η2p = 10−20%, see Table 3), comparable in size to the negative associations of trauma exposure as an important aetiological transdiagnostic risk factor in rescue workers (Berger et al., 2011; Clohessy & Ehlers, 1999; Hegg-Deloye et al., 2014; Teegen & Yasui, 2000). Furthermore, higher values on the SOC-R total scale were linked to lower depressive and somatic as well as composite symptom levels, whereas our results indicated no association of the SOC-R total scale with less severe post-traumatic symptoms. Thus, in this study, the rescue workers’ conviction to have sufficient resources to successfully manage vicious situations appeared to be the central protective aspect within the sense of coherence against developing clinically relevant mental or physical symptoms. Believing that there are no solutions or strategies for dealing with stressors can trigger negative self-reflective emotions such as despair, hopelessness, shame or even guilt, which have been reported to be linked to an intensification of symptomatology in rescue workers (Avraham, Goldblatt, & Yafe, 2014; Halpern, Gurevich, Schwartz, & Brazeau, 2009; Halpern et al., 2012). Manageability could counteract these beliefs and feelings. The manageability conviction apparently characterises rescue workers who stay resilient even in the face of continuing occupational trauma exposure and after major psychosocial stress and trauma events in private life. In general, our results replicate previous findings indicating a protective effect of the revised sense of coherence and, primarily, its manageability facet against the development of mental diseases (Bachem & Maercker, 2016; Mc Gee et al., 2017, 2018). Moreover, this study is the first to associate the SOC-R with better physical health.
4.3. Occupational and private-life trauma exposure as risk factors
Previous studies indicated that rescue workers face a considerably high risk to develop PTSD and depression as well as physical health complaints as a reaction to frequent exposure to severely stressful or traumatic experiences on duty (Aasa et al., 2005; Benedek et al., 2007; Berger et al., 2011; Clohessy & Ehlers, 1999; Donnelly, 2012; Fjeldheim et al., 2014; Fullerton et al., 2004; Häller et al., 2009; Hegg-Deloye et al., 2014; Razik et al., 2013; Skeffington et al., 2017; Teegen & Yasui, 2000; Wild et al., 2016). In line with this, we found the number of experienced traumatic event types on duty associated with an increased severity of post-traumatic, depressive, and somatic symptoms. There is evidence that private psychosocial stress or trauma events and particularly adverse childhood experiences could also compromise the health of emergency medical service, fire brigade or police personnel or increase their vulnerability to on-duty traumatisation (Levy-Gigi et al., 2015; Maunder et al., 2012; Richter, 2014). Correspondingly, we observed consistently increased transdiagnostic symptom severity in rescue workers who reported more potentially traumatic life-events in adulthood and/or more maltreatment experiences in childhood. Active psychoeducation about the role of traumatic experiences, especially childhood maltreatment, as a vulnerability factor could raise the awareness and willingness of rescue workers to seek professional help when developing mental and physical stress symptoms. Information should already be offered during career counselling and entry to make applicants with a history of (childhood) trauma aware of their particular risk.
4.4. Limitations and future directions
Observed prevalence rates for mental disorder symptoms were in the range of previous studies in the emergency medical service (Berger et al., 2011; Donnelly, 2012; Hegg-Deloye et al., 2014; Sterud, Ekeberg, & Hem, 2006). Highly affected individuals might not have participated in the present study due to current or chronical illness, dismissal or early retirement. This ‘healthy-worker effect’ might have led to an underestimation of effects (Costa, 2003). Moreover, due to the study’s cross-sectional design, the results can only be interpreted correlational. To conclusively investigate the putative role of the sense of coherence as a resilience factor, prospective longitudinal studies are necessary (Mc Gee et al., 2018).
Longitudinal studies are also needed to provide evidence on the dynamic of the revised sense of coherence throughout life. A longitudinal study in older adults found no changes in the SOC-R over the course of one year (Mc Gee et al., 2018). However, the developers of the SOC-R speculated that the sense of coherence could fluctuate with major life events. Being exposed to a high number of critical life events could compromise the sense of coherence, or vice versa, could stimulate the formation of a stronger sense of coherence (Bachem & Maercker, 2016). Longitudinal studies on Antonovsky’s SOC conception found a decrease with negative life events (Volanen, Suominen, Lahelma, Koskenvuo, & Silventoinen, 2007), but particularly in older adults as a reaction to deficits in health and social resources (Silverstein & Heap, 2015). In our sample, however, SOC-R scores were neither associated with the rescue workers’ occupational or private-life trauma exposure, nor with their age or working experience. Moreover, the score distributions corresponded well to the scores of healthy and old adults and were only slightly higher than those observed for bereaved persons (Bachem & Maercker, 2016; Mc Gee et al., 2017). To conclusively investigate possible impacts of multiple trauma exposure on the stability of the SOC-R, future research may employ longitudinal designs in high-risk groups. The sense of coherence is classically understood as a predictor of lower health impairments in reaction to stress and trauma. However, additional research is needed to clarify whether the sense of coherence could be compromised in reaction to the occurrence of mental or physical health problems and whether successful occupational resilience trainings or psychotherapy can improve the individual sense of coherence.
In bereaved persons, significantly lower SOC-R sum scores were observed in women than in men, and a similar trend regarding the subscales (Bachem & Maercker, 2016). We observed equally directed, but small-sized differences in our sample. Further, women reported slightly more severe post-traumatic and somatic symptoms than men. Although this finding is in line with the well-established epidemiological observation that women have a generally increased risk to develop stress-related disorder symptoms (Creamer, Burgess, & Mcfarlane, 2001; de Vries & Olff, 2009; Goldstein et al., 2016; Perkonigg, Kessler, Storz, & Wittchen, 2000), it contradicts previous research in rescue workers reporting a higher PTSD prevalence in men than women (Bennett et al., 2004). Indeed, increased symptom prevalence for female rescue workers appears debatable as female rescue workers were younger in this population, less work experienced, and were – descriptively – exposed to less occupational trauma than their male colleagues. In sum, we refrain from interpreting the sex effects in this occupational cohort, because sex is not only disproportionately distributed but also systematically confounded with relevant occupational-demographic or disorder aetiological factors. Future studies are needed to investigate whether aspects of the revised sense of coherence are differentially used by men and women.
5. Conclusions
This cross-sectional study suggests the revised sense of coherence and particularly, its manageability facet as a possible resilience factor for the mental and physical health of occupationally trauma-exposed populations. We replicated the exposure to potentially traumatic events on-duty or in private life as important risk factors for rescue workers’ health. Comprehensively evaluating the German SOC-R’s psychometric features indicated its three-factor structure as the most appropriate solution in this sample, although poor item-to-factor convergence compromised the factor validity. Future longitudinal studies may investigate the revised sense of coherence as possible prospective resilience factor and may aim at strengthening employees’ manageability perception to help them better cope with their professional demands.
Supplementary Material
Acknowledgments
M.Sc.-Psych. Daniela Conrad received a Ph.D. scholarship from the Hector Fellow Academy and Dipl.-Psych. Alexander Behnke holds a Ph.D. scholarship from the German Academic Scholarship Foundation (Studienstiftung des Deutschen Volkes). We furthermore thank our team of Bachelor and Master students for their support in data collection and data entry.
Note
In case of nonnormally distributed data, the quartile deviation (QD), defined as half of the interquartile deviation, is used as robust alternative for the standard deviation.
Author Contributions
RR, AB, DC, and ITK developed the study concept. RR, DC, and AB conducted the study setup and AB collected the data. AB performed the statistical data analyses. AB drafted the first version of the manuscript supported by DC and under supervision of ITK and RR. AB revised the article according to the reviewers’ comments. All authors contributed to the interpretation of data, critically revised the manuscript, and approved the final version of the paper for submission.
Disclosure statement
No potential conflict of interest was reported by the authors.
Data availability statement
Restrictions apply to the datasets: The datasets for this manuscript are not publicly available because the data may not be passed on or published to third parties outside the research project. The dataset contains sensitive personal and clinical information that might allow identifying individual participants. We do not have the consent of the ethics committee or our participants to grant access to or insight into the collected data.
Supplementary material
Supplemental data for this article can be accessed here.
References
- Aasa U., Brulin C., Ängquist K. A., & Barnekow-Bergkvist M. (2005). Work-related psychosocial factors, worry about work conditions and health complaints among female and male ambulance personnel. Scandinavian Journal of Caring Sciences, 19, 251–12. [DOI] [PubMed] [Google Scholar]
- Alexander D. A., & Klein S. (2001). Ambulance personnel and critical incidents: Impact of accident and emergency work on mental health and emotional well-being. British Journal of Psychiatry, 178, 76–81. [DOI] [PubMed] [Google Scholar]
- Antonovsky A. (1979). Health, stress, and coping. Jossey-Bass social and behavioral science series. San Francisco, CA: Jossey-Bass Inc. [Google Scholar]
- Antonovsky A. (1993). The structure and properties of the Sense of Coherence Scale. Social Science & Medicine, 36, 725–733. [DOI] [PubMed] [Google Scholar]
- Avraham N., Goldblatt H., & Yafe E. (2014). Paramedics’ experiences and coping strategies when encountering critical incidents. Qualitative Health Research, 24, 194–208. [DOI] [PubMed] [Google Scholar]
- Bachem R., & Maercker A. (2016). Development and psychometric evaluation of a revised Sense of Coherence Scale. European Journal of Psychological Assessment, 34, 206–215. [Google Scholar]
- Beierl E. T., Bühner M., & Heene M. (2018). Is that measure really one-dimensional?: Nuisance parameters can mask severe model misspecification when assessing factorial validity. Methodology, 14, 188–196. [Google Scholar]
- Benedek D. M., Fullerton C., & Ursano R. J. (2007). First responders: Mental health consequences of natural and human-made disasters for public health and public safety workers. Annual Review of Public Health, 28, 55–68. [DOI] [PubMed] [Google Scholar]
- Bennett P., Williams Y., Page N., Hood K., & Woollard M. (2004). Levels of mental health problems among UK emergency ambulance workers. Emergency Medicine Journal, 21, 235–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bentler P. M. (2006). EQS 6 structural equations program manual. (6th ed.). Multivariate Software, IncEncino, CA: Multivariate Software, Inc. Retrieved from http://www.econ.upf.edu/~satorra/CourseSEMVienna2010/EQSManual.pdf.. [Google Scholar]
- Berger W., Coutinho E. S. F., Figueira I., Marques-Portella C., Luz M. P., Neylan T. C., … Mendlowicz M. V. (2011). Rescuers at risk: A systematic review and meta-regression analysis of the worldwide current prevalence and correlates of PTSD in rescue workers. Social Psychiatry and Psychiatric Epidemiology, 47, 1001–1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berger W., Figueira I., Maurat A. M., Bucassio É. P., Vieira I., Jardim S. R., … Mendlowicz M. V. (2007). Partial and full PTSD in Brazilian ambulance workers: Prevalence and impact on health and on quality of life. Journal of Traumatic Stress, 20, 637–642. [DOI] [PubMed] [Google Scholar]
- Clohessy S., & Ehlers A. (1999). PTSD symptoms, response to intrusive memories and coping in ambulance service workers. British Journal of Clinical Psychology, 38, 251–265. [DOI] [PubMed] [Google Scholar]
- Comellas R. M., Makhashvili N., Chikovani I., Patel V., McKee M., Bisson J., & Roberts B. (2015). Patterns of somatic distress among conflict-affected persons in the Republic of Georgia. Journal of Psychosomatic Research, 78, 466–471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conrad D., Wilker S., Pfeiffer A., Lingenfelder B., Ebalu T., Lanzinger H., … Kolassa S. (2017). Does trauma event type matter in the assessment of traumatic load? European Journal of Psychotraumatology, 8, 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa G. (2003). Factors influencing health of workers and tolerance to shift work. Theoretical Issues in Ergonomics Science, 4, 263–288. [Google Scholar]
- Creamer M., Burgess P., & Mcfarlane A. C. (2001). Post-traumatic stress disorder: Findings from the Australian national survey of mental health and well-being. Psychological Medicine, 31, 1237–1247. [DOI] [PubMed] [Google Scholar]
- de Vries G.-J., & Olff M. (2009). The lifetime prevalence of traumatic events and posttraumatic stress disorder in the Netherlands. Journal of Traumatic Stress, 22, 259–267. [DOI] [PubMed] [Google Scholar]
- Declercq F., Meganck R., Deheegher J., & Van Hoorde H. (2011). Frequency of and subjective response to critical incidents in the prediction of PTSD in emergency personnel. Journal of Traumatic Stress, 24, 133–136. [DOI] [PubMed] [Google Scholar]
- Donnelly E. (2012). Work-related stress and posttraumatic stress in emergency medical services. Prehospital Emergency Care, 16, 76–85. [DOI] [PubMed] [Google Scholar]
- Donnelly E. A., & Bennett M. (2014). Development of a critical incident stress inventory for the emergency medical services. Traumatology: An International Journal, 20, 1–8. [Google Scholar]
- Ehring T., Knaevelsrud C., Krüger A., & Schäfer I. (2014). The life event checklist for DSM-5, german version. Translated questionnaire, Zentrum für Psychotraumatologie, Hamburg, Germany. Retrieved from http://zep-hh.de/wp-content/uploads/2015/05/PCL-5.pdf
- Fjeldheim C. B., Nöthling J., Pretorius K., Basson M., Ganasen K., Heneke R., … Seedat S. (2014). Trauma exposure, posttraumatic stress disorder and the effect of explanatory variables in paramedic trainees. BMC Emergency Medicine, 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fornell C., & Larcker D. F. (1981). Evaluating structural equation models with unobservable variables and measurement error. Journal of Marketing Research, 18, 39–50. [Google Scholar]
- Fullerton C. S., Ursano R. J., & Wang L. (2004). Acute stress disorder, posttraumatic stress disorder, and depression in disaster or rescue workers. American Journal of Psychiatry, 161, 1370–1376. [DOI] [PubMed] [Google Scholar]
- Gärtner A., Behnke A., Conrad D., Kolassa I.-T., & Rojas R. (2019). Emotion regulation in rescue workers: Differential relationship with perceived work-related stress and stress-related symptoms. Frontiers in Psychology, 9, 2744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaskin J. (2016). Validitymaster, stats tools package. Provo, Utah, USA: Information Systems Department, Brigham Young University. Retrieved from http://statwiki.kolobkreations.com
- Goldstein R. B., Smith S. M., Chou S. P., Saha T. D., Jung J., Zhang H., … Grant B. F. (2016). The epidemiology of DSM-5 posttraumatic stress disorder in the USA: Results from the national epidemiologic survey on alcohol and related conditions-III. Social Psychiatry and Psychiatric Epidemiology, 51, 1137–1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grevin F. (1996). Posttraumatic stress disorder, ego defense, mechanisms, and empathy among urban paramedics. Psychological Reports, 79, 483–495. [DOI] [PubMed] [Google Scholar]
- Gruszczyńska E. (2014). Discriminant validity of sense of coherence vs trait anxiety in explaining emotional state in an experimental task. Psychological Reports, 115, 228–241. [DOI] [PubMed] [Google Scholar]
- Hair J., Black W., Babin B., & Anderson R. (2010). Multivariate data analysis (7th ed.). Upper Saddle River, NJ, USA: Prentice-Hall, Inc. [Google Scholar]
- Häller P., Michael T., & Balmer Koechlin K. (2009). PTBS und komorbide Beschwerden bei Rettungssanitätern. Verhaltenstherapie and Verhaltensmedizin, 30, 403–417. [Google Scholar]
- Halpern J., Gurevich M., Schwartz B., & Brazeau P. (2009). What makes an incident critical for ambulance workers? Emotional outcomes and implications for intervention. Work & Stress, 23, 173–189. [Google Scholar]
- Halpern J., Maunder R. G., Schwartz B., & Gurevich M. (2012). The critical incident inventory: Characteristics of incidents which affect emergency medical technicians and paramedics. BMC Emergency Medicine, 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heene M., Hilbert S., Draxler C., Ziegler M., & Bühner M. (2011). Masking misfit in confirmatory factor analysis by increasing unique variances: A cautionary note on the usefulness of cutoff values of fit indices. Psychological Methods, 16, 319–336. [DOI] [PubMed] [Google Scholar]
- Hegg-Deloye S., Brassard P., Jauvin N., Prairie J., Larouche D., Poirier P., … Corbeil P. (2014). Current state of knowledge of post-traumatic stress, sleeping problems, obesity and cardiovascular disease in paramedics. Emergency Medicine Journal, 31, 242–247. [DOI] [PubMed] [Google Scholar]
- Heinrichs M., Wagner D., Schoch W., Soravia L. M., Hellhammer D. H., & Ehlert U. (2005). Predicting posttraumatic stress symptoms from pretraumatic risk factors: A 2-year prospective follow-up study in firefighters. American Journal of Psychiatry, 162, 2276–2286. [DOI] [PubMed] [Google Scholar]
- Hu L., & Bentler P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6, 1–55. [Google Scholar]
- IBM Corp (2011). IBM SPSS statistics for windows. Armonk, NY: IBM Corp. [Google Scholar]
- Isele D., Schauer M., Ruf-Leuschner M., & Elbert T (2011). Belastende Kindheitserfahrungen (KERF-20-I) – eine komprimierte Interviewversion In M. Schauer, M.Schauer, F.Neuner, & T. Elbert (Eds (Eds), Narrative exposure therapy (net): a short-term treatment for traumatic stress disorders (2nd ed.). Göttingen/Camebridge: Hogrefe & Huber Publishers. [Google Scholar]
- Isele D., Teicher M. H., Ruf-Leuschner M., Elbert T., Kolassa I.-T., Schury K., & Schauer M. (2014). KERF - Ein Instrument zur umfassenden Ermittlung belastender Kindheitserfahrungen: Erstellung und psychometrische Beurteilung der deutschsprachigen MACE (Maltreatment and Abuse Chronology of Exposure) Scale. Zeitschrift für Klinische Psychologie und Psychotherapie, 43, 121–130. [Google Scholar]
- Jonsson A., Segesten K., & Mattson B. (2003). Post-traumatic stress among Swedish ambulance personnel. Emergency Medicine Journal, 20, 79–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kase T., Ueno Y., & Oishi K. (2018). The overlap of sense of coherence and the Big Five personality traits: A confirmatory study. Health Psychology Open, 5, 1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolassa I.-T., Ertl V., Eckart C., Kolassa S., Onyut L. P., & Elbert T. (2010). Spontaneous remission from PTSD depends on the number of traumatic event types experienced. Psychological Trauma: Theory, Research, Practice, and Policy, 2, 169–174. [Google Scholar]
- Kolassa I.-T., Kolassa S., Ertl V., Papassotiropoulos A., & De Quervain D. J.-F. (2010). The risk of posttraumatic stress disorder after trauma depends on traumatic load and the Catechol-O-Methyltransferase Val158Met polymorphism. Biological Psychiatry, 67, 304–308. [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R. L., Williams J. B. W., & Löwe B. (2010). The patient health questionnaire somatic, anxiety, and depressive symptom scales: A systematic review. General Hospital Psychiatry, 32, 345–359. [DOI] [PubMed] [Google Scholar]
- Krüger-Gottschalk A., Knaevelsrud C., Rau H., Dyer A., Schäfer I., Schellong J., & Ehring T (2017). The German version of the Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Psychometric properties and diagnostic utility. BMC Psychiatry, 17(1), 379. https://doi.org/10.1186/s12888-017-1541–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leonhart R., Bancroft E. K., Mitra A., Ardern-Jones A., Castro E., Page E. C., & Eeles R. A. (2017). Physical and psychological correlates of high somatic symptom severity in Chinese breast cancer patients. Psychooncology, 26, 656–663. [DOI] [PubMed] [Google Scholar]
- Levy-Gigi E., Bonanno G. A., Shapiro A. R., Richter-Levin G., Kéri S., & Sheppes G. (2015). Emotion regulatory flexibility sheds light on the elusive relationship between repeated traumatic exposure and posttraumatic stress disorder symptoms. Clinical Psychological Science, 4, 28–39. [Google Scholar]
- LimeSurvey G. (2017). LimeSurvey: An open source survey tool. Hamburg, Germany. Retrieved from http://www.limesurvey.org. [Google Scholar]
- Löwe B., Spitzer R., Zipfel S., & Herzog W (2002). Gesundheitsfragebogen für Patienten (PHQ-D). Komplettversion und Kurzform. Testmappe mit Manual. Germany, Pfizer: Fragebögen , Schablonen. Karlsruhe. [Google Scholar]
- Lowery K., & Stokes M. A. (2005). Role of peer support and emotional expression on posttraumatic stress disorder in student paramedics. Journal of Traumatic Stress, 18, 171–179. [DOI] [PubMed] [Google Scholar]
- Maunder R. G., Halpern J., Schwartz B., & Gurevich M. (2012). Symptoms and responses to critical incidents in paramedics who have experienced childhood abuse and neglect. Emergency Medicine Journal, 29, 222–227. [DOI] [PubMed] [Google Scholar]
- Mc Gee S. L., Höltge J., Maercker A., & Thoma M. V. (2017). Evaluation of the revised Sense of Coherence scale in a sample of older adults: A means to assess resilience aspects. Aging and Mental Health. doi: 10.1080/13607863.2017.1364348 [DOI] [PubMed] [Google Scholar]
- Mc Gee S. L., Höltge J., Maercker A., & Thoma M. V. (2018). Sense of coherence and stress-related resilience: Investigating the mediating and moderating mechanisms in the development of resilience following stress or adversity. Frontiers in Psychiatry, 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mollica R. F., McInnes K., Pool C., & Tor S. (1998). Dose-effect relationships of trauma to symptoms of depression and post-traumatic stress disorder among Cambodian survivors of mass violence. British Journal of Psychiatry, 173, 482–488. [DOI] [PubMed] [Google Scholar]
- Perkonigg A., Kessler R. C., Storz S., & Wittchen H. U. (2000). Traumatic events and post-traumatic stress disorder in the community: Prevalence, risk factors and comorbidity. Acta Psychiatrica Scandinavica, 101, 46–59. [DOI] [PubMed] [Google Scholar]
- Prati G., & Pietrantoni L. (2010). The relation of perceived and received social support to mental health among first responders: A meta-analytic review. American Journal of Community Psychology, 38, 403–417. [Google Scholar]
- R Core Team (2018). R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing. Retrieved from https://www.R-project.org/ [Google Scholar]
- Razik S., Ehring T., & Emmelkamp P. M. G. (2013). Psychological consequences of terrorist attacks: Prevalence and predictors of mental health problems in Pakistani emergency responders. Psychiatry Research, 207, 80–85. [DOI] [PubMed] [Google Scholar]
- Regehr C., Goldberg G., & Hughes J. (2002). Exposure to human tragedy, empathy, and trauma in ambulance paramedics. American Journal of Orthopsychiatry, 72, 505–513. [DOI] [PubMed] [Google Scholar]
- Regehr C., Hill J., Knott T., & Sault B. (2003). Social support, self-efficacy and trauma in new recruits and experienced firefighters. Stress and Health : Journal of the International Society for the Investigation of Stress, 19, 189–193. [Google Scholar]
- Richter S. (2014). Stressbelastung und Stressbewältigung bei haupt- und ehrenamtlichen Einsatzkräften in Rheinland-Pfalz (Doctoral Dissertation). Universität der Bundeswehr, Munich, Germany. Retrieved from https://d-nb.info/1069557307/34. [Google Scholar]
- Rosseel Y. (2012). lavaan: An R package for structural equation modeling. Journal of Statistical Software, 48, 1–36. [Google Scholar]
- Schoch E.(2008). Berufliche Belastung und ihre psychischen Folgen bei Einsatzkräften im Rettungsdienst [Occupational stress and its psychological consequences in emergency service employees] (unpublished diploma thesis). Dep. Clinical Psychology, University of Konstanz. Germany: Konstanz. [Google Scholar]
- Shakespeare-Finch J., Rees A., & Armstrong D. (2015). Social support, self-efficacy, trauma and well-being in emergency medical dispatchers. Social Indicators Research, 123, 549–565. [Google Scholar]
- Silverstein M., & Heap J. (2015). Sense of coherence changes with aging over the second half of life. Advances in Life Course Research, 23, 98–107. [DOI] [PubMed] [Google Scholar]
- Skeffington P. M., Rees C. S., & Mazzucchelli T. (2017). Trauma exposure and post-traumatic stress disorder within fire and emergency services in Western Australia. Australian Journal of Psychology, 69, 20–28. [Google Scholar]
- Staneva A., Morawska A., Bogossian F., & Wittkowski A. (2016). Pregnancy-specific distress: The role of maternal sense of coherence and antenatal mothering orientations. Journal of Mental Health, 25, 387–394. [DOI] [PubMed] [Google Scholar]
- Sterud T., Ekeberg Ø., & Hem E. (2006). Health status in the ambulance services: A systematic review. BMC Health Services Research, 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teegen F., & Yasui Y. (2000). Traumaexposition und posttraumatische Belastungsstörungen bei dem Personal von Rettungsdiensten. Verhaltenstherapie and Verhaltensmedizin, 21, 65–83. [Google Scholar]
- Teicher M. H., & Parigger A. (2015). The ‘Maltreatment and abuse chronology of exposure’ (MACE) scale for the retrospective assessment of abuse and neglect during development. PloS one, 10, 1–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Ploeg E., & Kleber R. J. (2003). Acute and chronic job stressors among ambulance personnel: Predictors of health symptoms. Occupational and Environmental Medicine, 60, i40–i46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volanen S.-M., Suominen S., Lahelma E., Koskenvuo M., & Silventoinen K. (2007). Negative life events and stability of sense of coherence: A five-year follow-up study of Finnish women and men. Scandinavian Journal of Psychology, 48, 433–441. [DOI] [PubMed] [Google Scholar]
- Wang Q., Hay M., Clarke D., & Menahem S. (2014). Associations between knowledge of disease, depression and anxiety, social support, sense of coherence and optimism with health-related quality of life in an ambulatory sample of adolescents with heart disease. Cardiology in the Young, 24, 126–133. [DOI] [PubMed] [Google Scholar]
- Weathers F. W., Blake D. D., Schnurr P. P., Kaloupek D. G., Marx B. P., & Keane T. M (2013). The Life Events Checklist for DSM-5 (LEC-5). National Center for PTSD, U.S. Department of Veterans Affairs, Washington DC, USA. Retrieved May 3, 2017, from http://www.ptsd.va.gov [Google Scholar]
- Weathers F. W., Litz B., Keane T., Palmieri P., Marx B., & Schnurr P (2013). The PTSD checklist for DSM-5 (PCL-5). National Center for PTSD, U.S. Department of Veterans Affairs, Washington DC, USA. [Google Scholar]
- Wild J., Smith K. V., Thompson E., Béar F., Lommen M. J. J., & Ehlers A. (2016). A prospective study of pre-trauma risk factors for post-traumatic stress disorder and depression. Psychological Medicine, 46, 2571–2582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilker S., Pfeiffer A., Kolassa S., Koslowski D., Elbert T., & Kolassa I.-T. (2015). How to quantify exposure to traumatic stress? Reliability and predictive validity of measures for cumulative trauma exposure in a post-conflict population. European Journal of Psychotraumatology, 6, 28306. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Restrictions apply to the datasets: The datasets for this manuscript are not publicly available because the data may not be passed on or published to third parties outside the research project. The dataset contains sensitive personal and clinical information that might allow identifying individual participants. We do not have the consent of the ethics committee or our participants to grant access to or insight into the collected data.


